Abstract
Methotrexate-associated lymphoproliferative disorders (MTX-LPDs) with diffuse large B-cell lymphoma (DLBCL) pathology present with high rates of spontaneous regression after methotrexate (MTX) termination, especially in Epstein-Barr virus-encoded RNA (EBER)-positive cases. DLBCL with adrenal involvement is known for an extremely dismal prognosis. However, the prognosis of adrenal DLBCL in the context of MTX-LPD is unknown. We herein report two EBER-positive adrenal DLBCL MTX-LPD patients who achieved long-term remissions of 22 and 40 months with MTX termination alone. Both patients are doing well with no relapse at the time of reporting. Unlike adrenal DLBCL in general, adrenal involvement may not be a poor prognostic factor when restricted to DLBCL MTX-LPDs.
Keywords: OIIA-LPDs, MTX-LPDs, primary adrenal lymphoma, PAL, EBER
Introduction
Other iatrogenic immunodeficiency-associated lymphoproliferative disorders (OIIA-LPDs) are defined by the 2017 WHO classification as lymphoid proliferations or lymphomas that arise in patients receiving immunosuppressants for various conditions other than in the post-transplantation setting (1). Methotrexate (MTX) is the most common of these immunosuppressants that cause OIIA-LPDs, and such cases are often referred to as methotrexate-associated lymphoproliferative disorders (MTX-LPDs). MTX is the upfront drug of choice for rheumatoid arthritis patients, and an aging population leading to more patients with rheumatoid arthritis has resulted in an increase in patients with MTX-LPDs (2).
We herein report two MTX-LPD cases presenting as diffuse large B-cell lymphoma (DLBCL) with adrenal involvement that achieved long-term remission with MTX termination alone. In general, the prognosis of DLBCL with adrenal involvement is extremely poor (3), but we report that this may not apply when restricted to adrenal DLBCL of MTX-LPDs.
Case Reports
Case 1
A 77-year-old woman with rheumatoid arthritis treated with oral MTX therapy for more than 20 years developed systemic lymphadenopathy, multiple lung lesions, and bilateral adrenal tumors in November 2018. The patient presented with a fever of 38.5°C and an Eastern Cooperative Oncology Group performance status score of 1. LDH was elevated at 541 U/L. A right cervical lymph node biopsy and lung lesion biopsy were carried out, and DLBCL was diagnosed from both sites (stage IV, IPI: high). Clinical findings suggestive of central nervous system (CNS) invasion were absent. Immunohistochemistry showed that the DLBCL was positive for CD20, Epstein-Barr virus-encoded RNA (EBER), and LMP1 and negative for CD3, CD5, CD10, and Epstein-Barr virus nuclear protein 2 (EBNA2). A fluorescence in situ hybridization (FISH) analysis showed no MYC split signal and no IgH/BCL2 fusion signal.
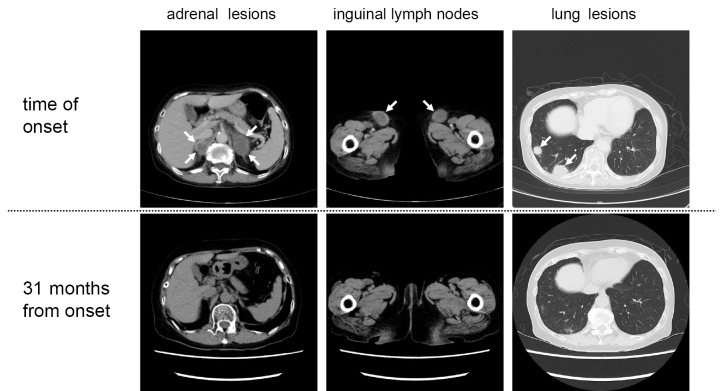
MTX administration was terminated from November 2018, and computed tomography (CT) performed 1 month later showed an approximately 50% size reduction of the DLBCL lesions. The DLBCL lesions continued to regress, and CT performed 12 and 31 months later showed complete remission (Fig. 1). The patient remains well at present with no recurrence 40 months from MTX termination.
Figure 1.
Case 1: CT scans before and after methotrexate termination.
Case 2
A 68-year-old woman who had been on oral MTX therapy for 8 years was found to have bilateral adrenal tumors and lung lesions on CT. LDH was elevated at 1,301 U/L. An adrenal tumor biopsy was carried out in the beginning of June 2020, and DLBCL was diagnosed (stage IV, IPI: high). Clinical findings suggestive of CNS invasion were absent. Immunohistochemistry showed that the DLBCL was positive for CD20, EBER, LMP1, and EBNA2 and negative for CD3, CD5, and CD10. A FISH analysis showed no MYC split signal.
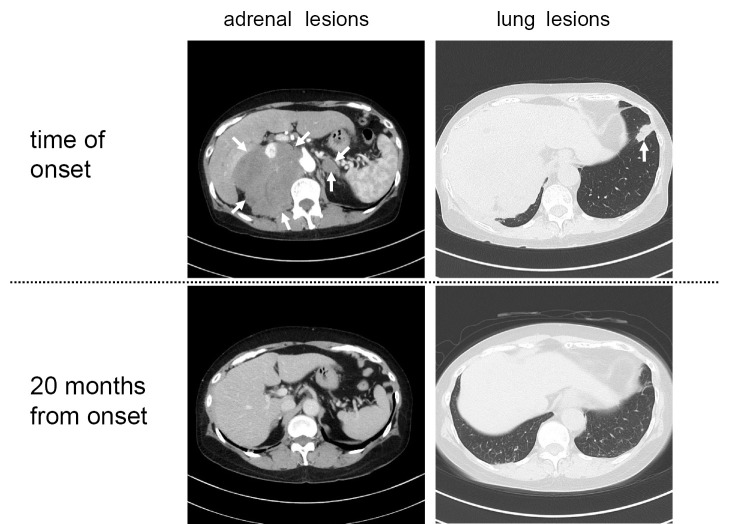
MTX was terminated, and CT performed 3 weeks later showed regression of the tumors, while follow-up CT performed 4 and 20 months later showed complete remission (Fig. 2). The patient remains well with no DLBCL recurrence at 22 months from MTX termination.
Figure 2.
Case 2: CT scans before and after methotrexate termination.
Discussion
We describe two adrenal MTX-LPD patients with DLBCL pathology who achieved long-term remissions of 22 and 40 months with MTX termination alone.
Adrenal DLBCL in general has been reported to present with an extremely poor prognosis. In a systematic review by Rashidi et al. including 187 adrenal lymphoma patients (of whom information on the outcome was available in 149), the 3-, 6-, and 12-month survival rates were reported to be low at 67%, 46%, and 20%, respectively (3). However, prognosis of adrenal DLBCL in the context of MTX-LPD is unknown. There are only two case reports of MTX-LPDs involving the adrenal glands, of which one had pathology of Hodgkin-like lesions and one DLBCL (Table) (4,5). The DLBCL case achieved complete remission with MTX termination alone, but information on the long-term follow up was not provided. We herein report for the first time the long-term follow-up and sustained remission of two adrenal DLBCL MTX-LPD patients requiring no chemotherapy, suggesting that adrenal DLBCL may not have a dismal prognosis when restricted to MTX-LPDs.
Table.
Characteristics of Patients with MTX-associated Lymphoproliferative Disorders with Adrenal Involvement Described in the Literature.
| Reference | sex | age | lymphoma type | stage | EBER status | duration of MTX administration | sites of lymphoma at onset | response after MTX termination | outcome |
|---|---|---|---|---|---|---|---|---|---|
| (4) | M | 70 | Hodgkin- | IE | Positive | 8 years | Right adrenal lesion | Adrenal | No relapse at |
| like | lymphoma | 1 year after tumor | |||||||
| lesions | completely | resection and | |||||||
| resected before | MTX termination | ||||||||
| MTX termination | |||||||||
| (5) | F | 72 | DLBCL | IV | Positive | 12 years | Bilateral adrenal | CR | Maintains CR at |
| lesions | 6 months from | ||||||||
| biopsy | |||||||||
| Case 1 | F | 77 | DLBCL | IV | Positive | >20 years | Systemic | CR | Maintains CR at |
| lymphadenopathy, | 40 months from | ||||||||
| lung lesions, bilateral | MTX termination | ||||||||
| adrenal lesions | |||||||||
| Case 2 | F | 68 | DLBCL | IV | Positive | 8 years | Lung lesions, | CR | Maintains CR at |
| bilateral adrenal | 22 months from | ||||||||
| lesions | MTX termination |
CR: complete remission, DLBCL: diffuse large B-cell lymphoma, F: female, M: male, MTX: methotrexate
MTX-LPDs are most commonly DLBCL or classic Hodgkin's lymphoma (cHL), accounting for 35-60% and 12-25% of cases, respectively (1). In a large, retrospective, single-center study by Kurita et al., regression of MTX-LPDs was seen with MTX termination alone in 31 of 70 DLBCL patients (44%) and 2 of 19 cHL patients (11%). In line with this, the median progression-free survival was 20 months for DLBCL and 5 months for cHL (6). EBER is positive in approximately 40% of MTX-LPDs (1). Kurita et al. reported that EBER positivity significantly correlated with a better progression-free survival (PFS) in DLBCL MTX-LPD patients (6). Other investigators have demonstrated that EBER positivity correlates with an increased incidence of spontaneous regression of MTX-LPDs after MTX cessation (4,5,7). The two cases in the current report were both EBER-positive DLBCLs, so spontaneous regression and sustained remission were well-foreseeable events, due to the fact that they were MTX-LPDs. However, since adrenal DLBCL is known to generally have an extremely poor and aggressive disease course, whether or not the two cases would both have an optimal outcome was very questionable.
EBV-positive DLBCL MTX-LPDs typically correspond to EBV latency type II (LMP1-positive, EBNA2-negative, EBER-positive) or else EBV latency type III (LMP1-positive, EBNA2-positive, EBER-positive) (6,8). Regarding the present patients, Case 1 corresponded to EBV latency type II, and Case 2 corresponded to latency type III.
Adrenal lymphoma is very rare, and Singh et al. reported that among 241 cases of non-Hodgkin's lymphoma, only 4 patients (1.6%) had adrenal involvement, all of whom had DLBCL pathology (9). Many adrenal lymphoma cases in the literature are described as “primary adrenal lymphoma (PAL),” but whether or not the two cases presented here would be classified as PAL is a matter of debate, as different investigators have used different arbitrary definitions of PAL. Rashidi et al. used a relaxed definition of PAL as a histologically proven lymphoma with unilateral or bilateral adrenal involvement, no history of lymphoma elsewhere, and adrenal lesions being unequivocally dominant when other sites were involved (3). Conversely, investigators like Zhou et al. used much stricter criteria for PAL, requiring histologically proven unilateral or bilateral adrenal lymphoma without nodal involvement, the absence of leukemic blood picture, and a lack of involvement of other organs for at least six months after the diagnosis (10). The two cases presented here may meet the criteria for PAL established by Rashidi et al. but would not meet those established by Zhou et al. We therefore refrained from using the term PAL and merely described these cases as “adrenal DLBCL” or “adrenal involvement.”
In conclusion, adrenal DLBCL in general has an exceptionally poor prognosis, but this may not be true in the context of DLBCL MTX-LPD. Providing patients with information on disease-specific life-expectancies is an important part of informed consent, but from our observations, DLBCL MTX-LPD with or without adrenal involvement may have similar outcomes. The accumulation of more cases is needed to confirm our findings.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Gaulard P, Swerdlow SH, Harris NL, Sundstrom CS, Jaffe ES. Other iatrogenic immunodeficiency-associated lymphoproliferative disorders. In: WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Swerdlow SH, Campo E, Harris NLet al. , Eds. IARC Press, Lyon, 2017: 462-464. [Google Scholar]
- 2. Ishigaki S, Masaoka T, Kameyama H, et al. Methotrexate-associated lymphoproliferative disorder of the stomach presumed to be mucosa-associated lymphoid tissue lymphoma. Intern Med 57: 3249-3254, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rashidi A, Fisher SI. Primary adrenal lymphoma: a systematic review. Ann Hematol 92: 1583-1593, 2013. [DOI] [PubMed] [Google Scholar]
- 4. Ohkura Y, Shindoh J, Haruta S, et al. Primary adrenal lymphoma possibly associated with Epstein-Barr virus reactivation due to immunosuppression under methotrexate therapy. Medicine (Baltimore) 94: e1270, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hanai S, Kobayashi K, Kawashima I, Ichijo M, Nakagomi D. Disappearance of bilateral adrenal tumours: immunodeficiency-associated lymphoproliferative disorder in a patient with rheumatoid arthritis. Rheumatology (Oxford) 60: e255-e257, 2021. [DOI] [PubMed] [Google Scholar]
- 6. Kurita D, Miyoshi H, Ichikawa A, et al. Methotrexate-associated lymphoproliferative disorders in patients with rheumatoid arthritis: clinicopathologic features and prognostic factors. Am J Surg Pathol 43: 869-884, 2019. [DOI] [PubMed] [Google Scholar]
- 7. Kaji D, Kusakabe M, Sakata-Yanagimoto M, et al. Retrospective analyses of other iatrogenic immunodeficiency-associated lymphoproliferative disorders in patients with rheumatic diseases. Br J Haematol 195: 585-594, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fujimoto K, Hatanaka KC, Hatanaka Y, et al. Association of Epstein-Barr virus with regression after withdrawal of immunosuppressive drugs and subsequent progression of iatrogenic immunodeficiency-associated lymphoproliferative disorders in patients with autoimmune diseases. Hematol Oncol 38: 799-807, 2020. [DOI] [PubMed] [Google Scholar]
- 9. Singh D, Kumar L, Sharma A, Vijayaraghavan M, Thulkar S, Tandon N. Adrenal involvement in non-Hodgkin's lymphoma: four cases and review of literature. Leuk Lymphoma 45: 789-794, 2004. [DOI] [PubMed] [Google Scholar]
- 10. Zhou L, Peng W, Wang C, Liu X, Shen Y, Zhou K. Primary adrenal lymphoma: radiological; pathological, clinical correlation. Eur J Radiol 81: 401-405, 2012. [DOI] [PubMed] [Google Scholar]