Abstract
In recent years, due to the aging of the population, the number of dental patients with comorbidities such as hypertension and diabetes has increased. Although it has been reported that these patients are increasingly developing medical emergencies during their dental treatments, many dental providers still do not possess the skills to manage medical emergencies appropriately. Simulation training is essential to improve this situation however, there is no report describing how to conduct an effective simulation in detail for dental office medical emergencies. The purpose of this review is to provide information on simulations that is effective and practical. The authors will highlight the key characteristics for providing effective simulation trainings, such as the selection of simulators, simulation locations, instructors, debriefings, methods for evaluating educational effectiveness, and the use of telesimulation as a method for simulation training due to the global COVID-19 pandemic. In addition, this review provides recommendations on tailoring an ideal simulation training course for those who wish to create one. The authors hope that this review will promote the spread of effective simulation training and in turn, contribute to improving the medical safety of dental patients.
Keywords: Simulation training, Medical emergency, High-fidelity manikin, In situ simulation, Debriefing, Telesimulation
1. Introduction
In recent years, many countries around the world are facing population aging, and the number of elderly people with various comorbidities such as hypertension, diabetes, and heart disease is increasing. In addition, it has been reported that the frequency of medical emergencies during dental treatments has increased due to the growing number of patients receiving long-term drug administration and the tendency for dental appointments to be prolonged [1], [2], [3], [4].
In a survey of 2704 dentists in North America, 13,836 medical emergencies occurred over a 10-year period with vasovagal syncope as the predominant type of medical emergency, followed by mild allergic reaction, postural hypotension, and hyperventilation [5]. In a survey of 620 German dentists, 57 % experienced up to three medical emergencies and 36 % experienced up to ten emergencies in one year. In addition, vasovagal syncope was the most common medical emergency, followed by hypertensive crises, seizures, and hypoglycemic episodes [6]. In a three-year survey of 1504 French dentists, 74.4 % faced some medical emergencies and 23 % requested emergency medical services. Vasovagal syncope was also reported to be the most common, occurring about twice a year [7]. A survey of General Dental Practitioners in Great Britain reported that one medical emergency occurred every 4.5 years in England and Wales, and one occurred every 3.6 years in Scotland. [8]. A 6-year survey at the Griffith University Dental Clinic in Australia reported that the frequency of medical emergency was 0.037 %, with vasovagal syncope followed by hypoglycemia and foreign body ingestion [9]. A survey in Japanese university hospitals dentistry published after 2010 reported the frequency of medical emergencies; these values were 0.0031–0.012 % with vasovagal syncope being the most common. This is in agreement with reports from other countries [10], [11]. Based on these reports, although the frequency of medical emergency is low, it can be inferred that most dental providers will encounter situations where they need to deal with medical emergencies several times throughout their careers. Therefore, dental providers need to be able to manage medical emergencies appropriately to ensure patient safety.
Are dental providers sufficiently prepared for medical emergencies? In a survey of 182 dental interns in India, 63 % responded that they had the ability to deal with unconscious patients [12]. On the other hand, in a survey of 153 dental students and dental interns in Saudi Arabia, only 37 % responded they were confident in managing medical emergencies [13]. A survey of 498 dentists in Croatia regarding pediatric medical emergencies found that 45 %−64.9 % of dentists did not have sufficient capacity to deal with medical emergencies such as an asthmatic shock, angina pectoris, hypo/hyperglycemia, epileptic episode, breathing obstruction, vasovagal syncope, and anaphylactic shock. In addition, 20.5 % of dentists experienced failure to make proper diagnosis when faced with medical emergencies [14]. In the authors’ study of Japanese dental providers (i.e. dentists and dental hygienists), only 14 % and 6 % of the respondents were confident in the treatment of vasovagal syncope and anaphylaxis, respectively [15]. Thus, most dental providers lack confidence when managing medical emergencies however, preparing them through appropriate training may improve their confidence. Dental providers cannot acquire the skills needed to manage medical emergencies using real patients [16]. Therefore, introduction of simulation training to improve knowledge and skills in medical emergencies management can be used to solve this situation [1]. An advantage of simulation training is that it allows learners to repeatedly practice medical emergencies management without putting patients at risk. Simulation training also improves the knowledge, task acquisition, and equipment as well as drug familiarity of individual learners. In addition, it contributes to the development of leadership and closed-loop communication when participating as a team [17].
Simulation training has various advantages as described above and should be actively introduced into the education for various medical emergency management to dental providers. Since to date, there is no report describing how to conduct an effective simulation in detail for dental office medical emergencies, the purpose of this review is to provide information on simulations that is effective and practical. This review introduces simulation training for medical emergencies in the dental setting conducted in Japan as well as throughout the world and explain the ideal simulations based on the authors’ experience.
2. Methods
2.1. Type of review
Narrative review.
2.2. Search strategy
Two electronic databases were used to conduct the literature search: PubMed (for the English literature) and Ichushi-Web (for the Japanese literature). The following keywords were employed for the search strategy.
PubMed: (Simulation AND Dental AND Emergency), (Training AND Dental AND "Medical Emergency"), ("High-fidelity Simulation" AND Dental AND Emergency).
The following filters were applied to the PubMed search: Humans and English.
Ichushi-Web: (Dentistry AND "Sudden Change" AND Simulation), (Dentistry AND "Cardiopulmonary Resuscitation" AND Education).
The following filters were applied to the Ichushi-Web search: Excludes meeting abstracts.
Publications from 2000 to 2023 were included (last search date: 6 January 2023). Duplicate articles were detected and excluded. The abstracts were then checked and only publications that fit the purpose of this review were selected.
3. Simulation training for medical emergencies in the dental setting provided in Japan
In Japan’s Model Core Curriculum in Dental Education for dental students published by the Ministry of Education, Culture, Sports, Science and Technology, dental students are required to be able to explain medical emergencies during dental treatment as well as the mechanisms of action and indications for emergency drug [18]. In the Achievement Goals for Dental Residents published by the Ministry of Health, Labor, and Welfare, dental residents are required to acquire knowledge, attitudes, and skills related to medical emergency management in order to perform dental treatments safely [19]. To achieve these goals, many simulation trainings for medical emergencies are provided for dental providers in Japan, primarily by university dental schools. However, many of these reports are written in Japanese and hence, it is difficult for readers outside of Japan to comprehend and appreciate the simulation training being conducted in Japan. Therefore, this section provides an overview of medical emergencies simulation done in Japan, focusing on simulation resources and evaluation methods. Details of the simulation training are shown in Table 1.
Table 1.
Simulation training for medical emergencies provided in Japan.
| Author, year | University / Clinic | Learners / Research subjects | Instructors / Supervisors | Simulators | Medical emergencies to be learned | Evaluation methods of educational effect | Remarks |
|---|---|---|---|---|---|---|---|
| Ito, 2006 [20] | Kyushu University | Dental residents | Dental anesthesiologist | CPR manikin | Cardiac arrest, foreign body airway obstruction | Questionnaire | |
| Kishimoto et al., 2018 [15] | Osaka Dental University | Dentists, dental hygienists, nurses, dental students | Dental anesthesiologist | CPR manikin, simulation app | Vasovagal syncope, anaphylaxis | Practical test with checklist, questionnaire with a 5-point Likert scale | |
| Kubo, 2021 [33] | Private dental clinic | Dental clinic staff | Not listed | VR contents | Hyperventilation, anaphylaxis | Practical test with checklist, oral examination, written test | Introduction to the developed VR simulation training |
| Matsuura, 2018 [31] | Tokyo Dental College | Dental students | Dental anesthesiologist | simulation app | Vasovagal syncope, anaphylaxis, cardiac arrest, ischemic heart disease | Questionnaire | |
| Matsuura et al., 2009 [27] | Tokyo Dental College | Not listed | Dental anesthesiologist | CPR manikin | Cardiac arrest | Practical test with skill reporting system | Introduction to the developed evaluation system |
| Morimoto, 2006 [22] | Osaka University | Dentists, oral surgeons, dental hygienists, nurses, laboratory technicians | Dental anesthesiologist | CPR manikin, high-fidelity manikin | Cardiac arrest, foreign body airway obstruction | Not listed | Introduction to the BLS and ICLS training at the university hospital |
| Nogami et al., 2016 [28] | Fukuoka Dental College | Dentists with BLS healthcare provider | AHA BLS instructor | CPR manikin | Cardiac arrest | Practical test with skill reporting system | Simulation only for skill evaluation |
| Sakuma et al., 2005 [25] | Osaka Dental University | Dentists, dental hygienists, dental technicians, nurses, dental students, office workers | Dental anesthesiologist with AHA ACLS provider | CPR manikin | Cardiac arrest, foreign body airway obstruction | Pratical test | Introduction to the BLS training at the university hospital |
| Sakuma et al., 2005 [29] | Osaka Dental University | Dentists | Dental anesthesiologist with AHA ACLS provider | High-fidelity manikin, Intubation Manikin | Cardiac arrest | Pratical test | Introduction to the ICLS training at the university hospital |
| Sakuma et al., 2020 [26] | Osaka Dental University | Dentists, dental students, dental hygiene students | Dental anesthesiologist with AHA ACLS provider | CPR manikin | Cardiac arrest, foreign body airway obstruction | Practical test with checklist | Introduction to the BLS training at the university hospital |
| Sanuki et al., 2016 [32] | Nagasaki University | Dental students | Dental anesthesiologist | Simulation app | Vasovagal syncope, hyperventilation, local anesthetic toxicity, anaphylaxis | 100 mm visual analog scale | |
| Takahashi, 2006 [23] | The Nippon Dental University | Dental students, dental residents | Dental anesthesiologist, surgeon, internist, nurse | CPR manikin | Cardiac arrest | Pratical test | Introduction to the BLS and ICLS training at the university hospital |
| Takano, 2006 [21] | Tsurumi University | Dentists, dental hygienists, dental technicians, nurses, pharmacists, laboratory technicians, nutritionists, office workers | Dental anesthesiologist, oral surgeon | CPR manikin | Cardiac arrest, foreign body airway obstruction | Pratical test, written test, questionnaire | Introduction to the BLS training at the university hospital |
| Tanaka et al., 2006 [24] | Hiroshima University | Dental and medical residents | Dental anesthesiologist, emergency doctor, nurse, paramedic | CPR manikin, high-fidelity manikin | Cardiac arrest, foreign body airway obstruction | Questionnaire | |
| Tanzawa et al., 2013 [30] | Showa University | Dental students | Dentist | Robot patient | vasovagal syncope, adrenal hypersensitivity | Practical test with checklist, questionnaire | Simulation only for skill evaluation |
ACLS, advanced cardiovascular life support; AHA, American Heart Association; BLS, basic life support; CPR, cardiopulmonary resuscitation; ICLS, immediate cardiac life support: VR, virtual reality
3.1. Simulators
Many reports on medical emergency simulations from Japanese university dental schools were related to Basic Life Support (BLS), and simple cardiopulmonary resuscitation (CPR) manikins were commonly used as simulators [20], [21], [22], [23], [24], [25], [26]. A high-fidelity manikin capable of pulse palpation, blood pressure measurement, and electrocardiogram monitoring is not required for the purpose of performing BLS, including chest compressions, rescue breathing, and AED use. Tokyo Dental College [27] and Fukuoka Dental College [28] used the Skill Reporting System combined with CPR manikins. They reported that this system could evaluate the depth and speed of chest compressions, chest rise during rescue breathing, and was useful for feedback to learners. Osaka University [22] and Osaka Dental University [29] held an Immediate Cardiac Life Support course for dentists using high-fidelity manikin such as HeartSim (Laerdal Medical, Stavanger, Norway). Learners were able to learn advanced resuscitation procedures such as tracheal intubation and defibrillation by using high-fidelity manikins. Showa University has developed a robot patient to assess the ability of dental students to deal with vasovagal syncope and adrenal hypersensitivity [30]. Due to how this robot could move its tongue, jaw, neck, arms, eyeballs, etc., and can also perform vomiting reflex, saliva secretion, and conversation, it reproduces very realistic environments in which medical emergencies may occur. However, the purchase of high-fidelity manikin and the development of robot patients are costly.
The use of apps from smartphones and tablets have been adopted by some universities instead of humanoid simulators. Tokyo Dental College [31] and Nagasaki University [32] used the vital sign simulation app known as SimMon (Castle Andersen ApS, Hillerød, Denmark) to provide simulation trainings for vasovagal syncope, anaphylaxis, cardiac arrest, etc. for dental students. However, there is a concern that it is difficult to acquire skills on a screen-based simulation using apps. The authors have developed a simulation course for vasovagal syncope and anaphylaxis with combination of CPR manikin and SimMon, and have provided it to dental providers such as dentists and dental hygienists. In the case of a medical emergency, the blood pressure, heart rate, arterial oxygen saturation, electrocardiogram, respiratory rate, etc. could be adjusted using SimMon. Therefore, the authors reported that it was effective in improving skills and self-confidence of dental providers for medical emergency management [15]. In addition, SimMon is inexpensive (costing around 30 USD as of January 2023), which is a great advantage for disseminating simulation training to many dental providers.
In recent years, simulation training using virtual reality (VR) technology has been developed in Japan. Kubo (a private dental clinic) used a 360-degree camera to create educational VR contents based on scenarios of hyperventilation syndrome and anaphylaxis during dental treatments [33]. Individuals can learn the diagnosis and treatment of these medical emergencies through images on the head mount display. With the introduction of VR technology, individuals can also learn medical emergency management in an environment resembling on-the-job training. This is a simulation training method that is expected to further develop in the future.
3.2. Instructors
There are 29 university dental schools in Japan, all of which have dental anesthesiology departments. Dental anesthesiologists in these department are usually in charge of general anesthesia and intravenous sedation for oral surgery and dental treatment for children and people with disabilities. In addition, they also deal with medical emergencies during dental treatments. Due to their clinical experience, dental anesthesiologists are primarily in charge of medical emergency simulation courses at each university [15], [20], [21], [22], [23], [24], [25], [26], [27], [29], [31], [32]. The Japanese Dental Society of Anesthesiologist certifies dentists in Japan through the Japanese Board of Dental Anesthesiologist (JBDA) and board certified dental anesthesiology specialist (BCDAS). JBDA certification requirements consist of more than 200 cases of general anesthesia, more than 50 cases of intravenous sedation, and passing a written and an oral exam. BCDAS certification requires experience of more than 500 dental anesthesia cases as well as passing a written and an oral exam [34]. Many dental anesthesiologists in Japan hold these qualifications; they are specialists in medical emergency management. Instructor quality is critical to delivering effective simulation training [15]. Therefore, in Japan, it is desirable for dental anesthesiologists, who are also experts in medical emergency management, to hold the roles of instructors for medical emergency simulation courses. Although some dental anesthesiologists have sufficient clinical experience, they may not be familiar with simulation education, such as the instructional methods and simulator operation.
For BLS-specific simulation training, procedures are standardized by guidelines such as the American Heart Association thus, even those who are not directly involved in dental care can provide sufficient instructions. From this point of view, emergency doctors, surgeons, internists, nurses, and paramedics are also in charge of BLS instructions for dental providers [23], [24].
3.3. Evaluation methods of educational effect
Both the educational and assessment components are essential for simulation training [17]. When simulation training is provided, it should be evaluated on whether it has an educational effect on the learners. However, many of the reports on simulation training in Japan have only described the contents and details of the developed courses [21], [22], [23], [25], [26], [27], [29], [33] with few studies having scientifically evaluated the educational effects, such as reporting statistical results. The authors conducted simulation training based on scenarios of vasovagal syncope and anaphylaxis that occurred during dental treatments and evaluated skills of the learners using a checklist. As a result, the score of the checklist significantly increased after the simulation training, suggesting that the medical emergency diagnosis and treatment skills of dental providers improved [15]. Objective skill evaluation using a checklist is the basis of evaluating educational effectiveness, and the authors believe that this process is essential to provide effective simulations. Nogami et al. [28]. assessed dentists' long-term BLS skills, and Tanzawa et al. [30]. assessed dental students' skills to deal with vasovagal syncope and adrenal hypersensitivity using a checklist. In both reports, simulations were conducted only for the skill evaluation of the subjects, and were not aimed at developing educational methods.
As a method of evaluating educational effectiveness other than evaluating skills, Sanuki et al. used the 100 mm Visual Analog Scale (VAS) to assess learners' confidence in understanding and managing medical emergencies. They reported that simulation improved the confidence of dental students, as their VAS scores on self-confidence increased significantly after simulation training using SimMon [32]. The authors introduced a questionnaire with a five-point Likert scale to assess the confidence of dental providers in diagnosis and treatment of medical emergencies before and after the simulation [15]. It is difficult to completely eliminate the learner's subjectivity in the evaluation of educational effects using VAS or questionnaires. However, by introducing these, it becomes possible to evaluate learners' individual perceptions for the value of simulation training.
4. Simulation training for medical emergencies in the dental setting provided throughout the world
This section provides an overview of medical emergencies simulation in countries other than Japan. Details of the simulation training are shown in Table 2.
Table 2.
Simulation training for medical emergencies provided throughout the world.
| Author, year | Country | University / Hospital | Learners / Research subjects | Instructors / Supervisors | Simulators | Location | Medical emergencies to be learned | Debriefing | Evaluation methods of educational effect | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|
| Balmer, 2008 [46] | UK | Liverpool University | Dental students | Dentist with ACLS instructor, ACLS instructor, ACLS provider | CPR manikin, choking manikin, high-fidelity manikin | Dental operatory | Choking, bradyarrhythmias, tachyarrhythmias, cardiac arrest, myocardial infarction, anaphylaxis, panic attack, asthma, respiratory arrest, hypoglycemia, epilepsy, drug overdose | No (feedback only) | Practical test with checklist, written test, questionnaire | |
| Balmer et al., 2008 [16] | UK | Liverpool University | Dentists, dental care professionals | Instructors with extensive experience in both ACLS teaching and dentistry | High-fidelity manikin, airway simulator | Four rooms set up for simulation | Choking, bradyarrhythmias, tachyarrhythmias, cardiac arrest, myocardial infarction, anaphylaxis, panic attack, asthma, respiratory arrest, hypoglycemia, epilepsy, drug overdose | No (feedback only) | Questionnaire | Three of the four simulation rooms have dental chairs, and the remaining one mimics a waiting room |
| Bilich et al., 2015 [41] | USA | Eastern Washington University | Dental hygiene students | Faculty members after taking faculty development course | High-fidelity manikin | Dental operatory | Myocardial infarction, allergy, stroke, asthma, hypoglycemia | Yes | Practical test with checklist | This is a retrospective study |
| Breuer et al., 2016 [40] | Germany | Friedrich-Alexander University Erlangen-Nürnberg | Dental students | Staff from Department of Anesthesiology and Emergency Medicine | High-fidelity manikin | Waiting room | Cardiac arrest | No | Practical test with checklist | Simulation only for skill evaluation |
| Brooks-Buza et al., 2011 [44] | USA | Wayne State University | Pediatric dental residents, dental assistants | Faculty from Department of Emergency Medicine | High-fidelity manikin | Dental operatory | Bradycardia, tachycardia, cardiac arrest | Yes | Practical test with checklist | |
| Castillo et al., 2017 [38] | USA | Winthrop-University | Dental residents | Not listed | High-fidelity manikin, standardized patient | Simulation center | Stroke, cardiac arrest | Yes | Questionnaire with a 6-point Likert scale | |
| Hadfield et al., 2018 [37] | UK | Cardiff University | Dentists, dental nurses | Anesthesiologists, dentists and nurses with many years of experience in simulation education | High-fidelity manikin | Dental operatory, Simulation center | Airway obstruction, anaphylaxis, hypoglycaemia, myocardial ischemia, asthma | Yes | Questionnaire | |
| Kalsi et al., 2013 [42] | UK | John Radcliffe Hospital | Oral and maxillofacial surgery residents | Simulation center faculty member | High-fidelity manikin | Simulation center | Opioid overdose, acute coronary syndrome, asthma, pulmonary embolism, anaphylaxis, left ventricular failure, pre-eclampsia | Yes | Questionnaire with a 10-point Likert scale | |
| Manton et al., 2021 [35] | USA | Ohio State University | Dental residents | Faculty from Division of Oral and Maxillofacial Surgery and Dental Anesthesiology, dental anesthesiology residents, trained simulationists | High-fidelity manikin, airway manikin, IV/intraosseous access trainer, standardized patient | Dental operatory, waiting room | Vasovagal syncope, seizure, hypo/hyperglycemic crisis, stroke, choking, aspiration, hyperventilation, anaphylaxis, local anesthesia toxicity, asthma, bronchospasm, bradyarrhythmias,tachyarrhythmias, hypertensive crisis, acute coronary syndrome, cardiac arrest, etc. | Yes | Practical test with checklist | |
| Marti et al., 2019 [50] | USA | University of Michigan | Dental students | Faculty from School of Dentistry and Emergency Medicine Depertment | Manikin | Not listed | Altered consciousness, chest pain, drug-related emergencies, unconsciousness, respiratory distress, cardiac arrest | Yes | Practical test with checklist, questionnaire | Detailed information about the manikin was not listed |
| Newby et al., 2010 [45] | Australia | University of Melbourne | Dental students | Dentist, qualified medical simulation educator | High-fidelity manikin | Dental operatory | Vasovagal syncope, hyperventilation, asthma, upper airway obstruction, hypoglycemia, anaphylaxis, chest pain, cardiac arrest | Yes | Practical test, written test, questionnaire with a 5-point Likert scale | |
| Roy et al. [36]., 2018 | France | University of Nantes | Dental students | Not listed | High-fidelity manikin | Simulation center | Airway obstruction, seizure, allergies, vasovagal syncope, asthma, chest pain, cardiac arrest | Yes | Practical test with checklist, questionnaire with a 10-point Likert scale | |
| Rubin et al., 2017 [39] | USA | New York Presbyterian/Weill Cornell Medicine | Dental residents | Course director, simulation center technician | High-fidelity manikin | Simulation center | Hyperventilation, vasovagal syncope, tachycardia, hypertension, hypoglycemia, asthma, anaphylaxis, loal anesthetic toxicity, aspiration, stroke, seizure, angina pectoris, myocardial infarction, cardiac arrest, etc. | Yes | Questionnaire with a 5-point Likert scale | |
| Sopka et al., 2012 [49] | Germany | RWTH Aachen University | Dental students | Certified ERC Advanced Life Support-Instructors, faculty from Department of Anesthesiology and Emergency Medicine | Not listed | Not listed | Cardiac arrest | No (feedback only) | Questionnaire with 6- or 10-point Likert scale | |
| Tan, 2011 [43] | USA | University of Colorado Denver | Pediatric dental residents, dental assistants | Pediatric dental faculty members after taking faculty development course, faculty from Department of Anesthesiology | High-fidelity manikin | Simulation center | Anaphylaxis, laryngospasm, sedative medication overdose, cardiac arrhythmia, cardiac arrest | Yes | Questionnaire with a 4-point Likert scale |
ACLS, advanced cardiovascular life support; CPR, cardiopulmonary resuscitation; ERC, European Resuscitation Council
4.1. Simulators
Most of the simulation training in Japan focuses on BLS. Meanwhile, in other countries predominantly in North America and Europe, simulation training is also widely provided for medical emergencies other than cardiac arrest, such as vasovagal syncope, anaphylaxis, hypoglycemia, and acute coronary syndrome. Therefore, high-fidelity manikins are used as simulators to reproduce complex patient symptoms, vital signs, and electrocardiogram changes at the time of medical emergencies [16], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46]. For example, the high-fidelity manikin SimMan 3 G (Laerdal Medical) can reproduce coughing, snoring, stridor, breathing difficulty, vomiting, etc. [36]. PediaSim Emergency Care simulator (Medical Education Technologies, Inc., Sarasota, FL, USA) can reproduce blink, breath sounds with chest wall movements, heart sounds with central and peripheral pulses, exhibit physiological reactions to drugs, etc. [43]. To provide effective simulation training, it is important to reproduce a realistic clinical setting [15], [45] thus, the use of high-fidelity manikins is very useful for this purpose. On the other hand, barriers to introducing a high-fidelity manikin include the high purchase cost and the extensive time required to learn how to operate it [15], [35], [41]. In addition, it has been reported that even with a high-fidelity manikin, it is difficult to reproduce physiological reactions such as cyanosis, flushing, clamminess, and seizures depending on the model [39]. However, these physiological reactions may be reproduced as technology advances, especially using VR technology.
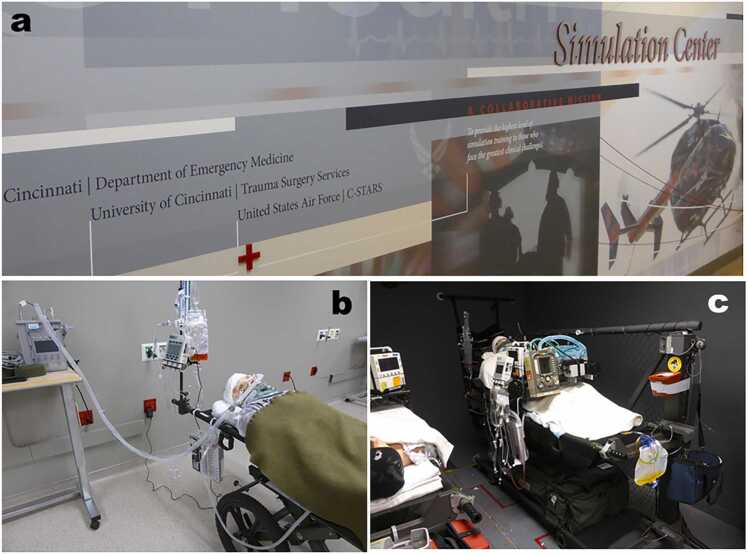
4.2. Simulation location
To reproduce realistic clinical settings, the location of the simulation training is as important as the choice of the simulator. Many of the simulations were performed in dental examination rooms in dental clinics or hospitals [35], [37], [41], [44], [45]. Thus, simulation-based education conducted in the clinical environment where learners usually work, rather than in dedicated training centers, is called in situ simulation [47]. For example, in military trauma training, the US Air Force has collaborated with the University of Cincinnati to provide in situ simulation for critical care air transport teams. Team members including critical care trained physicians, nurses, and respiratory therapists participated in simulation training for trauma management at the Center for Sustainment of Trauma and Readiness Skills (C-STARS) (Fig. 1), and even participated in simulations aboard military transport aircraft C-130 during training flights [48]. It has been reported that in situ simulation allows dental providers to learn in a familiar environment, resulting in a more realistic experience and performance [37]. Brooks-Buza et al. reported that in situ simulation using a high-fidelity simulator can evaluate both the performance of learners and the clinical emergency response system. Through in situ simulation training, they uncovered system-based problems, such as the lack of necessary equipment in clinics and the inability of existing wireless systems to work [44]. Thus, in situ simulation has many advantages and should be adopted as much as possible for effective simulation training.
Fig. 1.
Center for Sustainment of Trauma and Readiness Skills (C-STARS) at the University of Cincinnati Medical Center, Cincinnati, USA. The entrance of C-STARS (a). High-fidelity Manikins used for trauma management simulation (b and c). The room shown in (c) is a special one that can reproduce the brightness of the cabin and the loud engine noise during flight to conduct simulation training in an environment that mimics the cabin of a transport aircraft.
Other than in situ simulation, there have been reports on simulations conducted at simulation centers owned by universities or hospitals [36], [37], [38], [39], [42], [43]. The simulation center is a facility dedicated to medical simulation, and it is possible to use the rooms that reproduce hospital wards, ICU, operating rooms, dental examination rooms, etc. These settings may be better learning environments for individuals learning highly specialized skills, such as medical emergencies during sedation [37] as well as providing simulations for oral surgery residents who work in hospital wards and operating rooms [42].
4.3. Instructors/Supervisors
Since there are very few dental anesthesiologists in countries other than Japan, anesthesiologists, emergency doctors [37], [40], [43], [44], [49], [50], and dentists with advanced cardiovascular life support instructor qualifications [16], [46] have acted as instructors or supervisors for simulation training. It has been reported that simulation center faculty members [42] and technicians [39] participated in the simulation to operate the high-fidelity manikin properly. In addition, trained simulationists [35] and qualified medical simulation educators [45], who are specialists in simulation education, also participated to support the education for learners.
There are some reports that a faculty development course was implemented for faculty members for the purpose of training appropriate educators. Tan gave a lecture on adult learning theories and debriefing techniques to pediatric dental faculty members before conducting simulation training for pediatric dental residents to learn the management of medical emergencies during sedation. [43]. Bilich et al. reported that an experienced faculty member conducted the training for faculty members with the aim of appropriately evaluating skills using a checklist and promoting group debriefing [41]. Preparation, support, and feedback from the faculty members are important and is the key to successful simulation [39]. Therefore, a faculty development course is considered very useful.
In summary, an effective simulation can be performed in countries other than Japan by clinically experienced doctors and/or medical simulation experts in collaboration with dental faculty members, and by introducing a faculty development course prior to the course.
4.4. Debriefing
In simulations conducted in various countries predominantly in North America and Europe, debriefing sessions are provided after scenario-based simulation training [35], [36], [37], [38], [39], [41], [42], [43], [44], [45], [50]. Debriefing is defined as an interactive, bidirectional, and reflective discussion, or conversation between learners or between learners and facilitators [51]. Debriefing provides an opportunity for learners to reflect on the strengths and weaknesses of their performance, thus enhancing team performance and ultimately improving patient outcomes [17]. Feedback, which is often confused with debriefing, is defined as information provided to learners for the purpose of modifying their thinking and/or behavior to improve future performance [51]. Thus, feedback is a one-way transmission of information to the learners and is different from debriefing, which is a two-way discussion. Debriefing is more desirable than simple feedback for effective simulation training.
4.5. Evaluation methods of the educational effect
The authors’ report was the only study in Japan that conducted a practical test after simulation training and evaluated skills using a checklist [15]. However, there are many reports using checklist to assess skills in countries other than Japan [35], [36], [40], [41], [44], [46], [49]. Only a few studies have prospectively compared checklist scores between a simulation group versus a control group (without simulation training) to scientifically evaluate educational effects [35], [36]. Manton et al. evaluated management skills for anaphylaxis or acute coronary syndrome in dental residents. They reported that the average checklist score (out of 128 points) was significantly higher at 90.9 in the simulation group compared to 61.2 in the control group [35]. Roy et al. evaluated management skills for airway obstruction, seizure, allergies, vasovagal syncope, asthma, and chest pain in dental students. The overall checklist score was significantly higher in the simulation group than in the control group and concluded that simulation training using a high-fidelity manikin was useful [36].
As an evaluation method for educational effectiveness other than the checklist, there have been many reports where questionnaires instead were provided to learners [36], [37], [38], [39], [42], [43], [45], [46], [49], [50]. Regarding the questionnaire items, rather than simply asking the learners to freely state their opinions, most reports adopted the Likert scale in order to quantify the learners' confidence after simulation training, their satisfaction with the course, and the effectiveness of the course [36], [38], [39], [42], [43], [45], [49]. For example, Rubin et al. used a five-point Likert scale (from 1 = strongly disagree to 5 = strongly agree) in their questionnaire and reported that the overall course rating was 4.91 ± 0.33 (Mean± SD), indicating that it was highly effective [39].
5. Telesimulation training during the COVID-19 pandemic
The recent global COVID-19 pandemic has had a significant impact on simulation training. Due to the lack of personal protective equipment as well as the need for social distancing, the trend for medical simulation training has shifted from traditional in-person simulation to telesimulation training utilizing various virtual platforms [52]. Telesimulation is defined as the process of using telecommunication and simulation resources to provide education, training, and assessment to off-site learners [53]. This section introduces medical education using telesimulation and explains the pros and cons of telesimulation.
5.1. Medical education using telesimulation in the world
Mikrogianakis et al. connected hospitals in Toronto, Canada and Gaborone, Botswana via Skype videoconferencing software (Skype Limited, Luxembourg) and provided telesimulation training using intraosseous insertion simulators prepared at both facilities. Pediatricians in Toronto remotely instructed physicians in Botswana on the intraosseous insertion technique, resulting in improved scores on learners' written tests. In addition, the questionnaire showed improved confidence in learners handling the device. The intraosseous insertion skills of the learners evaluated by both on-site and off-site evaluators using a checklist showed no difference in scores thus, it was reported that accurate evaluation can be achieved via Skype [54]. By using Skype, multiple hospitals in Ontario, Canada were able to provide anesthesiologists with simulation training for the ultrasound-guided supraclavicular brachial plexus block using a high-fidelity ultrasound simulation machine. Skills were evaluated by both on-site and off-site evaluators using a checklist, and in both evaluations, scores significantly increased after the course compared to before the course. Furthermore, the questionnaire showed that the telesimulation improved learners' confidence in their skills. Moreover, most of the learners indicated that they would recommend the course to their colleagues, suggesting it was a highly satisfying educational method [55]. In addition, the usefulness of telesimulation has been reported in various medical education such as neonatal resuscitation training [56], mass casualty incident training [57], difficult airway management and local anesthetic toxicity management [58], evaluation of laparoscopic performance [59], patient assessment including the interpretation of vital signs and laboratory data [60], and instructor training and faculty development [61].
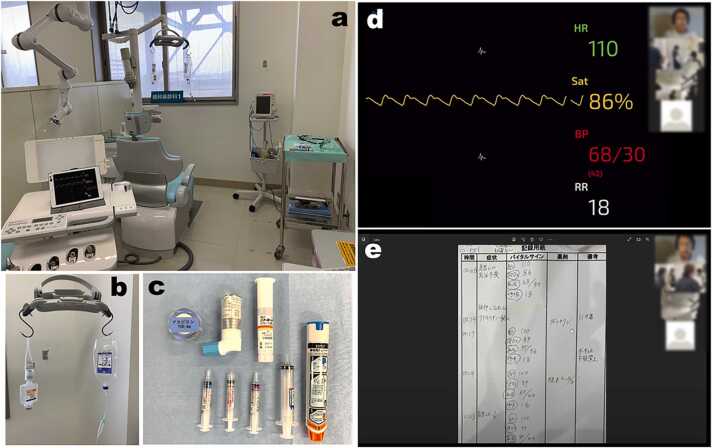
Since 2021, the authors have introduced telesimulation for the management of medical emergencies in the dental settings and are providing it to the dental clinic staff (Fig. 2). The authors' facility (Niigata University) and the dental clinic were connected by Zoom (Zoom Video Communications, Inc., San Jose, CA, USA), and the BCDAS remotely provided simulation training based on vasovagal syncope and anaphylaxis scenarios for dentists and dental hygienists. From the questionnaire given to participants after the course, many answered that the scenario-based telesimulation was very useful, suggesting that it was a favorable educational method for the learners [62].
Fig. 2.
Telesimulation training for medical emergencies in the dental setting. An example of an off-site simulation environment (a). Simulated infusion set and drugs required for simulation (b and c). Scenario-based simulation via Zoom (Zoom Video Communications, Inc., San Jose, CA, USA). Simulated patient's vital signs are reproduced using the simulation app SimMon (Castle Andersen ApS, Hillerød, Denmark) (d). Debriefing after scenario-based simulation (e).
5.2. The pros and cons of telesimulation
The advantage of introducing telesimulation is that it reduces the time and cost of travel for both educators and learners [59], [63]. Furthermore, by reducing the burden of time and cost for the learners, participating in simulations will be more accessible thereby leading to the wide spread of simulation training [64]. In addition, videoconferencing software can be used to easily connect learners and educators around the world allowing various clinical skills and knowledge to be shared. It is also expected to promote international collaboration [63]. Above all, with the spread of COVID-19 worldwide, the introduction of telesimulation is a huge advantage in that it can substantially reduce contact between people. Regarding the educational effect of telesimulation, learners' neonatal resuscitation knowledge scores significantly increased after the course [56], and as mentioned above, the ultrasound-guided supraclavicular brachial plexus block skill has been improved after the course. [55]. In addition, in studies that evaluated inter-rater reliability when evaluating the learners' skills on-site and off-site using a checklist, scores assessed off-site have been reported to be as reliable as on-site [55], [59]. Therefore, it is inferred that the learners are evaluated appropriately in the telesimulation as well as in-person simulation, and that educational effect can be obtained.
On the other hand, some concerns about the introduction of telesimulation have been reported. The most common issues are technical problems, such as unreliable internet connectivity, low bandwidth, issues with the software, etc., which can cause the interruptions of video and audio during simulation training [65]. There have been some reports of video and audio disconnection during the course, although it was only for a short period of time [55], [58], [62]. Therefore, it is essential for instructors and management staff to have adequate technology to troubleshoot these problems [52]. Another concern is that the introduction of telesimulation requires various resources such as simulators, computers, video conferencing software, and screens [57], [63]. In particular, when it is necessary to prepare both on-site and off-site simulators, more simulators are required compared to in-person simulations, which increases operating costs. Furthermore, in telesimulation, it has been reported that the quality of supervision and feedback from the educators may deteriorate due to the physical distance between the educator and the learner [56].
6. Ideal simulation training to learn the management of medical emergencies
This section summarizes the key characteristics of an ideal and tailored simulation training model that can be useful for those who wish to create a simulation training course for the management of medical emergencies in the dental setting.
For the simulators, it should be selected according to the educational purpose. For example, a simple CPR manikin is sufficient for BLS training. On the other hand, the use of a high-fidelity manikin is useful when targeting various medical emergencies other than cardiac arrest. If the cost of a high-fidelity manikin is a barrier, combining a CPR manikin with an app such as SimMon will enable the reproduction of realistic clinical settings at a low cost [15]. Regarding instructors, in Japan, it is desirable that dental anesthesiologists who have qualifications such as JBDA and BCDAS oversee instructions. If the dental anesthesiologist has little experience in simulation education, then the authors recommend running courses in collaboration with simulation education experts. If a dental anesthesiologist is not available (such as in a country other than Japan), the authors believe that the quality of the course can be maintained by having anesthesiologists or emergency doctors manage the course with dental faculty members. Regarding the location of the simulation, it is ideal to introduce in situ simulation, that is, to hold it in a dental clinic or hospital dental examination room. It is also important to provide learners with time to reflect by setting up a debriefing session after each scenario-based simulation training. Both educational and assessment components are important for simulation [17]. Thus, the process of evaluating the educational effect on learners after providing simulation education is essential. Therefore, it is strongly recommended to evaluate each learner's skills using a checklist at the end of the simulation course, and to evaluate their self-confidence and satisfaction by a questionnaire using the Likert scale. Finally, depending on the spread of COVID-19, introducing telesimulation should be considered as an option. By adopting these key characteristics for simulation training mentioned above, the authors believe that it is possible to provide effective simulations for dental providers to learn the management of medical emergencies.
7. Future perspective and conclusion
This review has outlined the several simulation methods for the management of medical emergencies that are being provided around the world, introduced a telesimulation that has been attracting attention in recent years due to the global COVID-19 pandemic, and proposed an ideal simulation training model. However, there are still issues to be considered. First, little has been reported about how long skills acquired through simulation are retained. Most of the studies presented in this review conducted skill assessments immediately after the simulation and evaluated only short-term educational effects. Skills inevitably decline with the passage of time after the simulation. Thus, it is essential to join a refresher course to maintain these learned skills. In the future, it is necessary to perform research from the perspective of long-term educational effects. Second, the educational effect of the authors’ medical emergency training course with telesimulation is unclear. The authors have reported that a course with telesimulation is technically feasible, but the authors have not evaluated its educational effects as a study [62]. Since the need for telesimulation is expected to increase in the future, this should be evaluated as soon as possible.
Simulation training is the only method dental providers can learn to manage the medical emergencies without putting patients at risk. The contents in each section contain many tips for providing effective simulations, and the authors are confident that it would be useful for the readers. The authors hope that this review will promote the spread of effective simulation training and, in turn, contribute to improving the safety of dental patients.
Conflict of Interest
None.
Acknowledgements
The authors would like to thank Dr. Taishi Nago at Faith Dental Office for his cooperation in holding the telesimulation training. We also wish to thank Ms. Crystal Mai for English editing.
Footnotes
Scientific field of dental science: Dental Anesthesiology
References
- 1.Vaughan M., Park A., Sholapurkar A., Esterman A. Medical emergencies in dental practice – management requirements and international practitioner proficiency. A scoping review. Aust Dent J. 2018;63:455–466. doi: 10.1111/adj.12649. [DOI] [PubMed] [Google Scholar]
- 2.Greenwood M. Medical emergencies in dental practice. Prim Dent J. 2014;3:4–5. doi: 10.1308/205016814812136002. [DOI] [PubMed] [Google Scholar]
- 3.Carvalho R.M., Costa L.R., Marcelo V.C. Brazilian dental students' perceptions about medical emergencies: a qualitative exploratory study. J Dent Educ. 2008;72:1343–1349. [PubMed] [Google Scholar]
- 4.Clark M.S., Wall B.E., Tholström T.C., Christensen E.H., Payne B.C. A twenty-year follow-up survey of medical emergency education in U.S. dental schools. J Dent Educ. 2006;70:1316–1319. [PubMed] [Google Scholar]
- 5.Malamed S.F. Knowing your patients. J Am Dent Assoc. 2010;141(Suppl 1):3S–7S. doi: 10.14219/jada.archive.2010.0350. [DOI] [PubMed] [Google Scholar]
- 6.Müller M.P., Hänsel M., Stehr S.N., Weber S., Koch T. A state-wide survey of medical emergency management in dental practices: incidence of emergencies and training experience. Emerg Med J. 2008;25:296–300. doi: 10.1136/emj.2007.052936. [DOI] [PubMed] [Google Scholar]
- 7.Collange O., Bildstein A., Samin J., Schaeffer R., Mahoudeau G., Féki A., et al. Prevalence of medical emergencies in dental practice. Resuscitation. 2010;81:915–916. doi: 10.1016/j.resuscitation.2010.03.039. [DOI] [PubMed] [Google Scholar]
- 8.Atherton G.J., McCaul J.A., Williams S.A. Medical emergencies in general dental practice in Great Britain. Part 1: their prevalence over a 10-year period. Br Dent J. 1999;186:72–79. doi: 10.1038/sj.bdj.4800023. [DOI] [PubMed] [Google Scholar]
- 9.Zachar J.J., Reher P. Frequency and characteristics of medical emergencies in an Australian dental school: a retrospective study. J Dent Educ. 2022;86:574–580. doi: 10.1002/jdd.12859. [DOI] [PubMed] [Google Scholar]
- 10.Kishimoto N., Seo K. Dental anesthesiology education for learning how to manage sudden changes in dental clinic patients. J Jpn Dent Assoc. 2021;74:105–114. [Google Scholar]
- 11.Obata K., Naito H., Yakushiji H., Obara T., Ono K., Nojima T., et al. Incidence and characteristics of medical emergencies related to dental treatment: a retrospective single-center study. Acute Med Surg. 2021;8 doi: 10.1002/ams2.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elanchezhiyan S., Elavarasu S., Vennila K., Renukadevi R., Mahabob M.N., Sentilkumar B., et al. Awareness of dental office medical emergencies among dental interns in southern India: an analytical study. J Dent Educ. 2013;77:364–369. [PubMed] [Google Scholar]
- 13.Albelaihi H.F., Alweneen A.I., Ettish A., Alshahrani F.A. Knowledge, attitude, and perceived confidence in the management of medical emergencies in the dental office: a survey among the dental students and interns. J Int Soc Prev Community Dent. 2017;7:364–369. doi: 10.4103/jispcd.JISPCD_414_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Čuković-Bagić I., Hrvatin S., Jeličić J., Negovetić Vranić D., Kujundžić Tiljak M., Pezo H., et al. General dentists' awareness of how to cope with medical emergencies in paediatric dental patients. Int Dent J. 2017;67:238–243. doi: 10.1111/idj.12286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kishimoto N., Mukai N., Honda Y., Hirata Y., Tanaka M., Momota Y. Simulation training for medical emergencies in the dental setting using an inexpensive software application. Eur J Dent Educ. 2018;22:e350–e357. doi: 10.1111/eje.12301. [DOI] [PubMed] [Google Scholar]
- 16.Balmer M.C., Longman L.P. A practical skill one day medical emergencies course for dentists and DCPs. Br Dent J. 2008;204:453–456. doi: 10.1038/sj.bdj.2008.300. [DOI] [PubMed] [Google Scholar]
- 17.Ritt R.M., Bennett J.D., Todd D.W. Simulation training for the office-based anesthesia team. Oral Maxillofac Surg Clin North Am. 2017;29:169–178. doi: 10.1016/j.coms.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Ministry of Education, Culture, Sports, Science and Technology. Model Core Curriculum in Dental Education (2016 revised edition). (In Japanese). Accessed July 21, 2022. https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjIqvaajrj1AhUIfnAKHVq7DokQFnoECAYQAQ&url=https%3A%2F%2Fwww.mext.go.jp%2Fcomponent%2Fa_menu%2Feducation%2Fdetail%2F__icsFiles%2Fafieldfile%2F2018%2F06%2F15%2F1325989_29_02.pdf&usg=AOvVaw2R2iHyPd5qkYUr-skb5p1P
- 19.Ministry of Health, Labor and Welfare. Achievement Goals for Dental Residents. (In Japanese). Accessed July 21, 2022. https://www.mhlw.go.jp/topics/bukyoku/isei/shikarinsyo/gaiyou/kanren/sekou/toutatsu.html
- 20.Ito S. Action for emergency life support in Kyusyu University Hospital Dental Center. J Jpn Dent Soc Anesth. 2006;34:135–139. [Google Scholar]
- 21.Takano K. A program of the lecture and training for the resuscitation to students and hospital staff in Tsurumi University. J Jpn Dent Soc Anesth. 2006;34:140–142. [Google Scholar]
- 22.Morimoto Y. Emergency resuscitation training at the Osaka University Dental Hospital. J Jpn Dent Soc Anesth. 2006;34:143–145. [Google Scholar]
- 23.Takahashi S. Update and future on training of emergency life support. J Jpn Dent Soc Anesth. 2006;34:146–148. [Google Scholar]
- 24.Tanaka Y., Taguchi N., Ogawa T. A project of ICLS introduction in dentist clinical training -SBOs: ICLS simulation course- J Jpn Dent Educ Assoc. 2006;22:155–160. [Google Scholar]
- 25.Sakuma Y., Hashimoto K., Kato Y., Sugioka S., Momota Y., Yamashita T., et al. Research on practice based education for emergency resuscitation -initial report: the preparation and implementation of BLS training curriculum- J Jpn Dent Soc Anesth. 2005;33:264–272. [Google Scholar]
- 26.Sakuma Y., Kato Y., Momota Y. Basic life support education at Osaka Dental University Dental School -a report of 15 years of outcomes- J Osaka Dent Univ. 2020;54:199–203. [Google Scholar]
- 27.Matsuura N., Ichinohe T., Kawada E., Kaneko Y. Development of evaluation system for cardiopulmonary resuscitation skill training using IT support. J Jpn Dent Soc Anesth. 2009;37:183–186. [Google Scholar]
- 28.Nogami K., Taniguchi S., Ichiyama T. Rapid deterioration of basic life support skills in dentists with basic life support healthcare provider. Anesth Prog. 2016;63:62–66. doi: 10.2344/0003-3006-63.2.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sakuma Y., Hashimoto K., Sugioka S., Momota Y., Kan Y., Yamashita T., et al. Research on practice based education for emergency resuscitation -part 2: immediate cardiac life support education- J Jpn Dent Soc Anesth. 2005;33:439–442. [Google Scholar]
- 30.Tanzawa T., Futaki K., Kurabayashi H., Goto K., Yoshihama Y., Hasegawa T., et al. Medical emergency education using a robot patient in a dental setting. Eur J Dent Educ. 2013;17:e114–e119. doi: 10.1111/j.1600-0579.2012.00770.x. [DOI] [PubMed] [Google Scholar]
- 31.Matsuura N. Development of a clinical training education system using ICT support. J Tokyo Dent Coll Soc. 2018;118:300–303. [Google Scholar]
- 32.Sanuki T., Komasawa N., Kurata S., Ayuse T. Efficacy of simulation application SimMon for emergency response training. Am J Emerg Med. 2016;34:927–928. doi: 10.1016/j.ajem.2016.02.044. [DOI] [PubMed] [Google Scholar]
- 33.Kubo K. Trial application of virtual reality in dental anesthesiology education. J Clin Anesth (Jpn) 2021;45(Suppl):339–347. [Google Scholar]
- 34.The Japanese Dental Society of Anesthesiology. Specialist. Accessed July 21, 2022. http://kokuhoken.net/jdsa/english/specialist.html
- 35.Manton J.W., Kennedy K.S., Lipps J.A., Pfeil S.A., Cornelius B.W. Medical emergency management in the dental office (MEMDO): a pilot study assessing a simulation-based training curriculum for dentists. Anesth Prog. 2021;68:76–84. doi: 10.2344/anpr-67-04-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roy E., Quinsat V.E., Bazin O., Lesclous P., Lejus-Bourdeau C. High-fidelity simulation in training dental students for medical life-threatening emergency. Eur J Dent Educ. 2018;22:e261–e268. doi: 10.1111/eje.12284. [DOI] [PubMed] [Google Scholar]
- 37.Hadfield A., Thompson S., Hall J., Diaz-Navarro C. Perception of simulation training in emergencies for dental sedation practitioners. Clin Teach. 2018;15:52–56. doi: 10.1111/tct.12626. [DOI] [PubMed] [Google Scholar]
- 38.Castillo J., Kutzin J., Agoglia K., Janicke P., Milligan Z., Scott J. An innovative clinical skills "Boot Camp" for dental medicine residents. J Med Educ Curric Dev. 2017;4 doi: 10.1177/2382120517710018. 2382120517710018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rubin M.E., Hansen H.J. An emergency simulation course in a postdoctoral general dentistry program: the New York Presbyterian/Weill Cornell medicine experience. J Dent Educ. 2017;81:1345–1350. doi: 10.21815/JDE.017.094. [DOI] [PubMed] [Google Scholar]
- 40.Breuer G., Knipfer C., Huber T., Huettl S., Shams N., Knipfer K., et al. Competency in managing cardiac arrest: a scenario-based evaluation of dental students. Acta Odontol Scand. 2016;74:241–249. doi: 10.3109/00016357.2015.1042782. [DOI] [PubMed] [Google Scholar]
- 41.Bilich L.A., Jackson S.C., Bray B.S., Willson M.N. High-fidelity simulation: preparing dental hygiene students for managing medical emergencies. J Dent Educ. 2015;79:1074–1081. [PubMed] [Google Scholar]
- 42.Kalsi A.S., Higham H., McKnight M., Dhariwal D.K. Simulation training for dental foundation in oral and maxillofacial surgery - a new benchmark. Br Dent J. 2013;215:571–576. doi: 10.1038/sj.bdj.2013.1143. [DOI] [PubMed] [Google Scholar]
- 43.Tan G.M. A medical crisis management simulation activity for pediatric dental residents and assistants. J Dent Educ. 2011;75:782–790. [PubMed] [Google Scholar]
- 44.Brooks-Buza H., Fernandez R., Stenger J.P. The use of in situ simulation to evaluate teamwork and system organization during a pediatric dental clinic emergency. Simul Health. 2011;6:101–108. doi: 10.1097/SIH.0b013e3182070f9d. [DOI] [PubMed] [Google Scholar]
- 45.Newby J.P., Keast J., Adam W.R. Simulation of medical emergencies in dental practice: development and evaluation of an undergraduate training programme. Aust Dent J. 2010;55:399–404. doi: 10.1111/j.1834-7819.2010.01260.x. [DOI] [PubMed] [Google Scholar]
- 46.Balmer M.C. A dental undergraduate course for the management of medical emergencies in dental practice. Eur J Dent Educ. 2008;12:239–246. doi: 10.1111/j.1600-0579.2008.00525.x. [DOI] [PubMed] [Google Scholar]
- 47.Martin A., Cross S., Attoe C. The use of in situ simulation in healthcare education: current perspectives. Adv Med Educ Pr. 2020;11:893–903. doi: 10.2147/AMEP.S188258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thorson C.M., Dubose J.J., Rhee P., Knuth T.E., Dorlac W.C., Bailey J.A., et al. Military trauma training at civilian centers: a decade of advancements. J Trauma Acute Care Surg. 2012;73(Suppl 5):S483–S489. doi: 10.1097/TA.0b013e31827546fb. [DOI] [PubMed] [Google Scholar]
- 49.Sopka S., Biermann H., Druener S., Skorning M., Knops A., Fitzner C., et al. Practical skills training influences knowledge and attitude of dental students towards emergency medical care. Eur J Dent Educ. 2012;16:179–186. doi: 10.1111/j.1600-0579.2012.00740.x. [DOI] [PubMed] [Google Scholar]
- 50.Marti K., Sandhu G., Aljadeff L., Greene R., Lesch A.B., Le J.M., et al. Simulation-based medical emergencies education for dental students: a three-year evaluation. J Dent Educ. 2019;83:973–980. doi: 10.21815/JDE.019.084. [DOI] [PubMed] [Google Scholar]
- 51.Sawyer T., Eppich W., Brett-Fleegler M., Grant V., Cheng A. More than one way to debrief: a critical review of healthcare simulation debriefing methods. Simul Health. 2016;11:209–217. doi: 10.1097/SIH.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 52.Diaz M.C.G., Walsh B.M. Telesimulation-based education during COVID-19. Clin Teach. 2021;18:121–125. doi: 10.1111/tct.13273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McCoy C.E., Sayegh J., Alrabah R., Yarris L.M. Telesimulation: an innovative tool for health professions education. AEM Educ Train. 2017;1:132–136. doi: 10.1002/aet2.10015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mikrogianakis A., Kam A., Silver S., Bakanisi B., Henao O., Okrainec A., et al. Telesimulation: an innovative and effective tool for teaching novel intraosseous insertion techniques in developing countries. Acad Emerg Med. 2011;18:420–427. doi: 10.1111/j.1553-2712.2011.01038.x. [DOI] [PubMed] [Google Scholar]
- 55.Burckett-St Laurent D.A., Cunningham M.S., Abbas S., Chan V.W., Okrainec A., Niazi A.U. Teaching ultrasound-guided regional anesthesia remotely: a feasibility study. Acta Anaesthesiol Scand. 2016;60:995–1002. doi: 10.1111/aas.12695. [DOI] [PubMed] [Google Scholar]
- 56.Mileder L.P., Bereiter M., Wegscheider T. Telesimulation as a modality for neonatal resuscitation training. Med Educ Online. 2021;26:1892017. doi: 10.1080/10872981.2021.1892017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McCoy C.E., Alrabah R., Weichmann W., Langdorf M.I., Ricks C., Chakravarthy B., et al. Feasibility of telesimulation and Google glass for mass casualty triage education and training. West J Emerg Med. 2019;20:512–519. doi: 10.5811/westjem.2019.3.40805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Beissel A., Lilot M., Bauer C., Beaulieu K., Hanacek C., Desebbe O., et al. A trans-atlantic high-fidelity mannequin based telesimulation experience. Anaesth Crit Care Pain Med. 2017;36:239–241. doi: 10.1016/j.accpm.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 59.Choy I., Fecso A., Kwong J., Jackson T., Okrainec A. Remote evaluation of laparoscopic performance using the global operative assessment of laparoscopic skills. Surg Endosc. 2013;27:378–383. doi: 10.1007/s00464-012-2456-4. [DOI] [PubMed] [Google Scholar]
- 60.Ray J.M., Wong A.H., Yang T.J., Buck S., Joseph M., Bonz J.W., et al. Virtual telesimulation for medical students during the COVID-19 pandemic. Acad Med. 2021;96:1431–1435. doi: 10.1097/ACM.0000000000004129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gross I.T., Whitfill T., Auzina L., Auerbach M., Balmaks R. Telementoring for remote simulation instructor training and faculty development using telesimulation. BMJ Simul Technol Enhanc Learn. 2020;7:61–65. doi: 10.1136/bmjstel-2019-000512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kishimoto N., Nguyen B.H., Tran S.D., Seo K. Telesimulation training applying flipped classroom in the dental clinic for medical emergencies. J Dent Anesth Pain Med. 2021;21:179–181. doi: 10.17245/jdapm.2021.21.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nelsen B.R., Chen Y.K., Lasic M., Bader A.M., Arriaga A.F. Advances in anesthesia education: increasing access and collaboration in medical education, from E-learning to telesimulation. Curr Opin Anaesthesiol. 2020;33:800–807. doi: 10.1097/ACO.0000000000000931. [DOI] [PubMed] [Google Scholar]
- 64.Hayden E.M., Khatri A., Kelly H.R., Yager P.H., Salazar G.M. Mannequin-based telesimulation: increasing access to simulation-based education. Acad Emerg Med. 2018;25:144–147. doi: 10.1111/acem.13299. [DOI] [PubMed] [Google Scholar]
- 65.Roach E., Okrainec A. Telesimulation for remote simulation and assessment. J Surg Oncol. 2021;124:193–199. doi: 10.1002/jso.26505. [DOI] [PubMed] [Google Scholar]