Abstract
Background and objective
Chronic obstructive pulmonary disease (COPD) and heart failure (HF) mutually increase the risk of being present in the same patient, especially if older. Whether or not this coexistence may be associated with a worse prognosis is debated. Therefore, employing data derived from the REPOSI register, we evaluated the clinical features and outcomes in a population of elderly patients admitted to internal medicine wards and having COPD, HF or COPD + HF.
Methods
We measured socio-demographic and anthropometric characteristics, severity and prevalence of comorbidities, clinical and laboratory features during hospitalization, mood disorders, functional independence, drug prescriptions and discharge destination. The primary study outcome was the risk of death.
Results
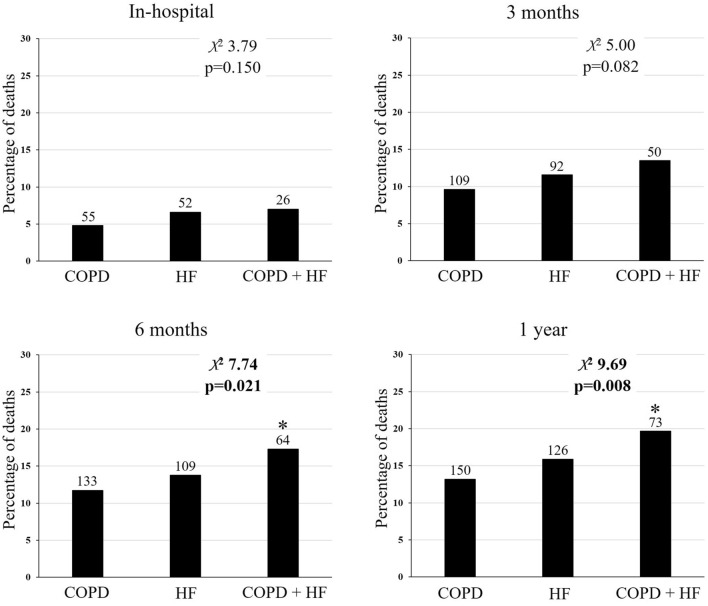
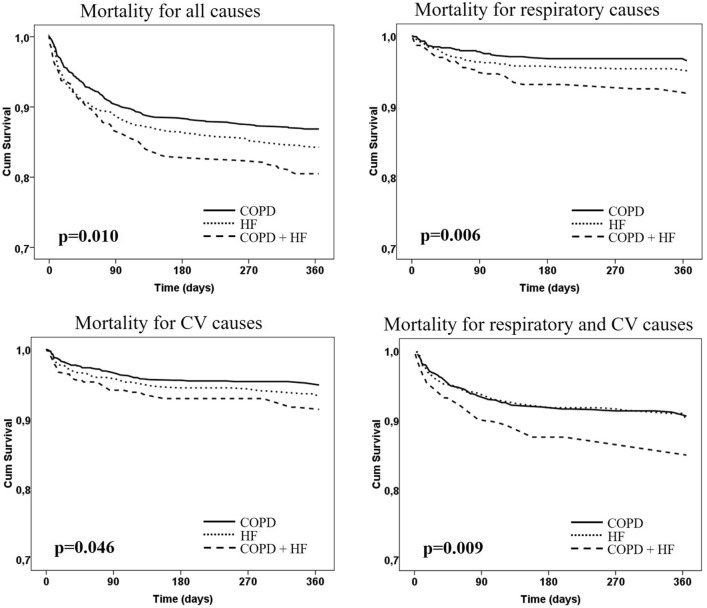
We considered 2,343 elderly hospitalized patients (median age 81 years), of whom 1,154 (49%) had COPD, 813 (35%) HF, and 376 (16%) COPD + HF. Patients with COPD + HF had different characteristics than those with COPD or HF, such as a higher prevalence of previous hospitalizations, comorbidities (especially chronic kidney disease), higher respiratory rate at admission and number of prescribed drugs. Patients with COPD + HF (hazard ratio HR 1.74, 95% confidence intervals CI 1.16–2.61) and patients with dementia (HR 1.75, 95% CI 1.06–2.90) had a higher risk of death at one year. The Kaplan–Meier curves showed a higher mortality risk in the group of patients with COPD + HF for all causes (p = 0.010), respiratory causes (p = 0.006), cardiovascular causes (p = 0.046) and respiratory plus cardiovascular causes (p = 0.009).
Conclusion
In this real-life cohort of hospitalized elderly patients, the coexistence of COPD and HF significantly worsened prognosis at one year. This finding may help to better define the care needs of this population.
Keywords: Chronic obstructive pulmonary disease, Heart failure, Multimorbidity, Mortality, Prognosis, Hospital cure
Introduction
Chronic obstructive pulmonary disease (COPD) and heart failure (HF) are prevalent clinical conditions among older patients [1], frequently coexisting in the same multimorbid individual [2]. Compared with a general population, patients with COPD are more than twofold likely to have a cardiovascular disease [3], while approximately 1 in 7 patients with heart failure, even those with preserved ejection fraction, have concomitant COPD [4]. Smoking habits and chronic systemic inflammation are commonly shared risk and mechanistic factors [5], and advanced age may increase the prevalence of this association. In a real-life setting of internal medicine and geriatric wards and in a cohort of elderly patients with multimorbidity, inpatients with COPD had a higher prevalence of HF (29%) than those without (18%) [6].
Although management and treatment differ, breathlessness may make it difficult to diagnose and distinguish COPD from HF [7]. Studies comparing these two diseases for some clinical outcomes focus on exciting considerations on similarities and differences, but findings often disagree. Taken separately, COPD and HF had a similar risk of hospitalization and death at three years in an outpatient setting [8]. However, when COPD and HF occur together, their coexistence may be associated with a worse outcome than either condition alone [9–11], suggesting a dangerous interaction between the two diseases [12], even in the context of a very long follow-up of community-dwelling elderly subjects [13]. Such an additive prognostic effect seems to vary in the literature according to the selection criteria employed for the different index patient populations, being slightly more evident in COPD with HF [9, 14] than in HF with COPD [15]. In the latter category of outpatients, the coexistence of other comorbidities (such as chronic kidney disease, anemia or diabetes) makes this association less strong [15]. Similarly, data from a long-term registry of the European Society of Cardiology Heart Failure show that in hospitalized HF patients, the concomitant presence of COPD did not increase significantly the risk of all-cause mortality at one-year [16]. On the other hand, in a recent meta-analysis including 18 studies (6 post-hoc analyses of randomized controlled trials and 12 observational studies), COPD, if present in HF patients was associated with a 24% increased risk for all-cause mortality but not for cardiovascular mortality [17]. Thus, further evidence is needed concerning the role that COPD and HF may have in the same patient.
The association between COPD and HF has been generally evaluated in outpatients and hospitalized patients in the context of specialized care settings, pneumological or cardiological. Such a two-cohort approach (e.g., starting from patients with a well-known/prevalent disease with or without another less-known/secondary disease) allows to observe only an added effect to the original cohort [9, 15–17]. However, less information is available in other settings, particularly in the real life of internal medicine wards, characterized by a holistic approach to hospitalized elderly patients and multiple chronic conditions, thus allowing an accurate evaluation of the relative weight of each condition. With this background and gaps of knowledge, our working hypothesis was that only the coexistence of both diseases in the same patient would influence clinical outcome. Therefore, we chose to describe clinical features, hospital care and outcomes of elderly inpatients with COPD, HF or both admitted to internal medicine and geriatric hospital wards participating in the REPOSI registry.
Methods
Study population
This retrospective cross-sectional study analyzed data from the REPOSI registry in the recruitment years spanning from 2010 to 2018. REPOSI, an independent registry run by the Italian Society of Internal Medicine (SIMI), the Mario Negri Institute for Pharmacological Research and the IRCCS Foundation Maggiore Policlinico Hospital, involved a network of internal medicine and geriatric wards in order to collect data on polypharmacy in elderly patients often affected by multiple diseases [18]. The registry design is accessible on the related website [19]. Patients 65 years or older who gave informed consent and were admitted to Internal or Geriatric Medicine wards during the four index weeks chosen for recruitment each year (in February, June, September and December) were eligible for REPOSI. During each index week, data concerning socio-demographic details, the main reason for admission and comorbidities, diagnoses, drug treatment, clinical events during hospitalization and outcome were recorded in at least ten consecutively enrolled patients from each ward. In addition, data on mortality or any new hospitalization were collected by a telephone interview performed by a physician three and twelve months after hospital discharge.
Subjects were referred to as having COPD or HF if a disease diagnosis was reported in medical charts or the diagnosis was made at hospital admission, according to the codes reported in the International Classification of Diseases system (ICD-9), 9th Edition. We considered the ICD-9 codes 491.x, 492.x, and all subsequent subcodes to define patients with COPD and the ICD-9 code 428.x and all subsequent subcodes to define patients with HF. Patients with both conditions were considered as a separate group (COPD + HF). Other comorbidities related to specific ICD-9 codes were reported (see Appendix).
Measurements and outcomes
In the three diagnosis groups (COPD, HF, COPD + HF), we collected socio-demographic and anthropometric variables such as age, sex, body mass index (BMI), marital status, living arrangement, low-income work, years of education and need for a caregiver in the activities of daily living. Moreover, variables concerning a previous institutionalization or hospitalization, smoking and alcohol habits’, severity and comorbidity impact as assessed by the Cumulative Illness Rating Scale-CIRS [20, 21] and the prevalence of the more common diseases (hypertension, hypercholesterolemia, coronary artery disease, atrial fibrillation, peripheral arterial disease, diabetes, chronic kidney disease, osteoporosis, dementia, depression, cancer) were also collected.
On admission, we evaluated the following characteristics: body temperature, systolic and diastolic blood pressure, heart and respiratory rate, laboratory data (fasting glucose, creatinine, hemoglobin, erythrocytes, mean corpuscular volume, leukocytes, platelets, cholesterol, albumin, prothrombin time), oxygen saturation by pulse oximetry (SpO2), presence of pressure ulcers or need for a urinary catheter, cognitive status and mood disorders (by the Short Blessed Test-SBT [22] and the Geriatric Depression Scale-GDS [23], respectively). Furthermore, functional independence (by the Barthel Index-BI [24]), drug prescriptions (at admission, during hospitalization, at three months and one-year follow-up) and the place of destination at discharge were also evaluated.
The primary outcome was the risk of death, evaluated during hospitalization and follow-ups at three, six, and twelve months. The risk of death has been considered for all causes, respiratory causes only, cardiovascular causes only and respiratory and cardiovascular causes together. Other outcomes were duration of hospital stay and readmission rate (at three months and one-year follow-up).
Statistical analysis
A preliminary Shapiro–Wilk test was performed. Data having a non-normal distribution have been reported as numbers (percentages) for categorical variables and medians [1st quartile; 3rd quartile] for continuous variables. Categorical variables were compared using the chi square test or the Freeman-Halton extension of Fisher’s exact test [25], while continuous variables were assessed by the non-parametric Kruskal–Wallis H or Mann–Whitney U tests, as appropriate.
Cox proportional hazard regression models were used to predict the risk of death for all causes [26]. The hazard ratio (HR) and 95% confidence intervals (CI) were calculated. Time-to-event variables were analyzed using Kaplan–Meier survival curves; the Gehan–Breslow–Wilcoxon test was applied due to its ability to emphasize early between-group differences [27].
All analyses were performed using IBM SPSS, version 25.0 (IBM Corp., Armonk, NY, USA) and a p-value of < 0.05 has been considered statistically significant.
Results
Our study population considered 2,343 hospitalized patients, of whom 1,154 (49%) were those with COPD, 813 (35%) with HF and 376 (16%) with COPD + HF. The general characteristics of the study population are reported in Table 1. Differences were found among the three study groups: as compared to COPD patients, HF patients were older, with more females, had more frequent previous hospitalisations and such comorbidities as arterial hypertension, atrial fibrillation, diabetes and chronic kidney disease, as well as the need of a caregiver. HF patients had lower smoking and alcohol habits than COPD patients. On the other hand, patients with COPD + HF (in comparison to COPD alone) were older with more comorbidities (atrial fibrillation, diabetes and chronic kidney disease); while in comparison to HF, they were more frequently males with a higher prevalence of current and former smoking status and alcohol habits. Moreover, patients with COPD + HF had more previous hospitalisations and comorbidities (as assessed by CIRS) than COPD or HF.
Table 1.
General characteristics of the study population
| Variables | COPD (N = 1,154) |
HF (N = 813) |
COPD + HF (N = 376) |
p-Value |
|---|---|---|---|---|
| Age, years (N = 2,343) | 80 [74; 85] | 82 [77; 87] ** | 82 [76; 87] ** | < 0.001 |
| Sex, male (N = 2,343) | 713 (62) | 350 (43) ** | 230 (61) §§ | < 0.001 |
| BMI, kg∙m2 (N = 2,037) | 25.5 [22.7; 28.7] | 25.9 [22.8; 29.4] | 26 [23; 29.6] | 0.108 |
| Regions of enrollment (N = 2,324) | 0.965 | |||
| Northern Italy | 616 (54) | 430 (54) | 198 (53) | |
| Center Italy | 215 (19) | 156 (19) | 68 (18) | |
| Southern Italy | 316 (27) | 217 (27) | 108 (29) | |
| Marital status, married or widow (N = 2,251) | 1007 (90) | 708 (91) | 325 (91) | 0.737 |
| Living arrangement, alone/partner/sons (N = 2,229) | 257 (23)/528 (48)/145 (13) | 168 (22)/330 (43)/153 (20) * | 84 (23)/148 (41)/64 (18) | 0.006 |
| Low-income work (N = 1,714) | 672 (80) | 504 (84) | 234 (86) * | 0.044 |
| Years of education, mean (95% CI) (N = 2,042)# | 7.2 (6.9—7.4) | 6.9 (6.7—7.3) | 6.5 (6.1—6.9) * § | 0.014 |
| Caregiver (N = 2,300) | 631 (56) | 510 (64) ** | 234 (63) * | < 0.001 |
| Partner/sons/other (N = 1,363) | 229 (36)/274 (44)/124 (20) | 127 (25)/270 (54)/106 (21) ** | 80 (34)/105 (45)/48 (21) § | 0.001 |
| Previously institutionalized (N = 2,329) | 66 (5.8) | 55 (6.8) | 20 (5.4) | 0.534 |
| Previously hospitalized (N = 2,056) | 428 (43) | 362 (51) * | 206 (61) ** § | < 0.001 |
| Smoking habit, former/current (N = 2,276) | 576 (51)/187 (17) | 267 (34)/33 (4.2) ** | 200 (54)/41 (11) * §§ | < 0.001 |
| Pack/year (N = 842) | 39 [20; 55] | 27.5 [12.37; 44.25] ** | 37.5 [20; 61.25] §§ | < 0.001 |
| Alcohol habit, former/current (N = 2,249) | 173 (16)/406 (36) | 96 (12)/216 (28) ** | 48 (14)/128 (35) § | < 0.001 |
| CIRS-SI (N = 2,341) | 1.69 [1.53; 1.92] | 1.69 [1.53; 2] | 1.85 [1.69; 2.08] ** §§ | < 0.001 |
| CIRS-CI (N = 2,341) | 3 [2; 5] | 3 [2; 5] | 4 [3; 5] ** §§ | < 0.001 |
| Arterial hypertension (N = 2,342) | 907 (79) | 688 (85) * | 312 (83) | 0.003 |
| Hypercholesterolemia (N = 2,343) | 61 (5.3) | 42 (5.2) | 22 (5.9) | 0.883 |
| CAD (N = 2,343) | 278 (24) | 193 (24) | 108 (29) | 0.142 |
| Atrial fibrillation (N = 2,343) | 287 (25) | 356 (44) ** | 162 (43) ** | < 0.001 |
| PAD (N = 2,343) | 64 (5.5) | 32 (3.9) | 23 (6.1) | 0.168 |
| Diabetes (N = 2,343) | 312 (27) | 263 (32) * | 139 (37) ** | < 0.001 |
| Chronic kidney disease (N = 2,343) | 268 (23) | 295 (36) ** | 164 (44) **§ | < 0.001 |
| Osteoporosis (N = 2,343) | 98 (8.5) | 55 (6.8) | 22 (5.9) | 0.153 |
| Dementia (N = 2,343) | 90 (7.8) | 70 (8.6) | 23 (6.1) | 0.330 |
| Depression (N = 2,343) | 83 (7.2) | 47 (5.8) | 18 (4.8) | 0.185 |
| Cancer (N = 1,311) | 74 (12) | 55 (11) | 33 (15) | 0.259 |
Data are shown as numbers of patients (percentage) or medians [1st quartile; 3rd quartile]. Percentages are calculated for non-missing data
In bold are significant variables
COPD indicates Chronic Obstructive Pulmonary Disease, HF heart failure, BMI body mass index, CIRS-SI and CIRS-CI Cumulative Illness Rating Scale, severity and comorbidity index, respectively, CAD coronary artery disease, PAD peripheral arterial disease
* and **p < 0.05 and p < 0.001 versus COPD
§ and §§ p < 0.05 and p < 0.001 versus HF
# Values of medians [25°–75° percentiles] were 5 [5, 8] in all three groups, not descriptive of differences
Functional, clinical and laboratory variables are illustrated in Table 2. At admission, patients with COPD + HF had lower values of SpO2 than those with HF, while the respiratory rate was higher in COPD + HF patients as compared to COPD and HF only. Values of SBT for cognitive status were higher in HF (in comparison to COPD), while values of GDS for mood disorders were higher in HF and COPD + HF compared to COPD only. The measure of functional independence (evaluated by BI, ad admission, during hospitalization and three months post-discharge) was worse in patients with HF only and COPD + HF as compared to COPD. Compared with COPD and HF alone, drug prescriptions (at admission, discharge and three months follow-up) were higher in COPD + HF. The need for a urinary catheter was lower in COPD.
Table 2.
Functional, clinical and laboratory data
| Variables | COPD | HF | COPD + HF | p-Value |
|---|---|---|---|---|
| Body temperature, °C (N = 2,196) | 36.2 [36; 36.8] | 36.1 [36; 36.6] * | 36 [36; 36.7] | 0.028 |
| Systolic blood pressure, mmHg (N = 2,332) | 130 [120; 140] | 130 [110; 140] * | 125 [110; 140] ** | 0.001 |
| Diastolic blood pressure, mmHg (N = 2,331) | 70 [65; 80] | 70 [60; 80] * | 70 [63.75; 80] | 0.003 |
| Heart rate, bpm (N = 2,319) | 80 [70; 90] | 80 [70; 90] | 80 [70; 90] | 0.222 |
| Respiratory rate, bpm (N = 1,127) | 18 [16; 22] | 18 [15; 22] * | 20 [16; 24] * §§ | < 0.001 |
| Fasting glucose, mg/dL (N = 2,258) | 111 [92; 142] | 115 [95; 149] | 113.5 [96; 150] | 0.053 |
| Creatinine, mg/dL (N = 2,321) | 1.01 [0.8; 1.4] | 1.2 [0.9; 1.78] ** | 1.3 [0.95; 1.78] ** | < 0.001 |
| Hemoglobin, mg/dL (N = 2,328) | 12.1 [10.5; 13.6] | 11.4 [9.8; 13] ** | 12 [10.6; 13.3] §§ | < 0.001 |
| Erythrocytes, million cells per mcL (N = 2,307) | 4.18 [3.64; 4.61] | 4 [3.49; 4.5] ** | 4.1 [3.7; 4.6] § | 0.001 |
| Mean corpuscular volume, fL (N = 2,312) | 89.9 [85; 94] | 89.85 [83; 94] | 90 [85; 95] | 0.099 |
| Leukocytes, cells per microliter (× 103/μL) (N = 2,319) | 8.58 [6.5; 11.6] | 8.16 [6.25; 10.73] | 8.5 [6.4; 11.4] | 0.060 |
| Platelets (cells per microliter) (× 103/μL) (N = 2,323) | 222 [170; 282.5] | 214 [164; 282.5] | 225 [160; 279.5] | 0.616 |
| Cholesterol (mg/dL) (N = 1,626) | 154 [126; 186] | 144 [118; 178] ** | 152 [123.75; 174] | < 0.001 |
| Albumin, gr/dL (N = 1,417) | 3.4 [3; 3.8] | 3.3 [2.97; 3.6] * | 3.3 [2.9; 3.8] | 0.019 |
| Prothrombin time—INR (N = 2,144) | 1.1 [1; 1.25] | 1.2 [1.05; 1.76] ** | 1.16 [1.02; 1.6] ** | < 0.001 |
| SpO2, % (N = 1,795) | 95 [92; 97] | 96 [94; 97] * | 95 [92; 97] §§ | < 0.001 |
| Pressure ulcers (any stages) (N = 1,742) | 25 (2.9) | 30 (5) | 12 (4.4) | 0.118 |
| Need for urinary catheter (N = 2,284) | 322 (29) | 375 (47) ** | 171 (46) ** | < 0.001 |
| Short Blessed Test score (N = 2,010) | 8 [2; 14] | 9 [4; 16] * | 9 [4; 16] | 0.020 |
| Geriatric Depression Scale score (N = 1,841) | 1 [0; 2] | 1 [1; 2] * | 2 [1; 3] * | 0.006 |
| Barthel index | ||||
| At admission (N = 1,822) | 88 [60.75; 100] | 80 [51; 95] ** | 77.5 [52; 92] ** | < 0.001 |
| During hospitalization (N = 2,180) | 84 [52; 98] | 75 [39; 93] ** | 72.5 [39.75; 91.25] ** | < 0.001 |
| At 3-month follow-up (N = 1,162) | 86 [62; 98] | 82 [52; 97] * | 80 [57; 93] * | 0.006 |
| At 12-month follow-up (N = 300) | 79 [51; 91] | 75 [36.5; 95] | 77.5 [55.5; 91.5] | 0.961 |
| Drugs prescriptions (number of drugs) | ||||
| At admission (N = 2,335) | 6 [4; 8] | 7 [5; 9] ** | 8 [6; 10] ** §§ | < 0.001 |
| At discharge (N = 2,001) | 9 [6; 12] | 9 [7; 12] * | 11 [7; 14] ** §§ | < 0.001 |
| At 3-month follow-up (N = 1,326) | 7 [4; 10] | 7 [6; 10] * | 8 [6; 11] ** | < 0.001 |
| At 12-month follow-up (N = 361) | 6 [3; 9] | 7 [4; 9] | 9 [6; 12] ** § | < 0.001 |
| Length of hospital stay, days (N = 2,162) | 10 [7; 15] | 10 [7; 15] | 10 [7.25; 14] | 0.836 |
| Destination at discharge (N = 1,596) | 0.207 | |||
| Home | 734 (92) | 480 (88) | 233 (92) | |
| Nursing home | 31 (3.9) | 36 (6.6) | 12 (4.7) | |
| Rehabilitation | 24 (3) | 22 (4) | 8 (3.1) | |
| Palliative care | 7 (0.9) | 8 (1.5) | 1 (0.4) | |
| Readmission at 3 months (N = 2,044) | 154 (15) | 98 (14) | 52 (16) | 0.645 |
| Readmission at 12 months (N = 1,946) | 178 (18) | 107 (16) | 65 (22) | 0.098 |
Data are shown as numbers of patients (percentage) or medians [1st quartile; 3rd quartile]. Percentages are calculated for non-missing data.
In bold are significant variables
COPD indicates Chronic Obstructive Pulmonary Disease, HF heart failure, SpO2 oxygen saturation by pulse oximetry
* and **p < 0.05 and p < 0.001 versus COPD
§ and §§p < 0.05 and p < 0.001 versus HF
Table 3 reports the univariate and multivariate-adjusted Cox regression models predicting the risk of death for all causes at one year. In the univariate analysis, variables significantly increasing the risk of death were: the presence of COPD + HF (reference: COPD), age ≥ 85 years, male sex, underweight (reference: normal weight), a CIRS-CI value ≥ 3, the presence of coronary artery disease, chronic kidney disease, dementia, cancer, a SBT score ≥ 10, a GDS score > 2, and a BI ≤ 40. The overweight and current smokers (versus former) were demonstrated to have a lower risk of death. The multivariate-adjusted model confirmed a statistically significant and independent risk of worse prognosis for patients with COPD + HF (HR 1.74; 95% CI 1.16–2.61; p = 0.008) and those with dementia (HR 1.75; 95% CI 1.06–2.90; p = 0.030).
Table 3.
Univariate and multivariate-adjusted Cox regression models predicting the risk of death for all causes at one year
| Univariate | Multivariate-adjusted | ||||
|---|---|---|---|---|---|
| HR | p-Value | HR | p-Value | ||
| COPD | 1 | 1 | |||
| HF | 1.22 (0.96–1.55) | 0.102 | 1.13 (0.77–1.65) | 0.541 | |
| COPD + HF | 1.54 (1.16–2.03) | 0.003 | 1.74 (1.16–2.61) | 0.008 | |
| Age, ≥ 85 years | 1.82 (1.47–2.25) | < 0.001 | |||
| Male | 1.36 (1.09–1.69) | 0.005 | |||
| Normal weight | 1 | ||||
| Underweight | 1.95 (1.41–2.69) | < 0.001 | |||
| Overweight | 0.72 (0.52–0.99) | 0.045 | |||
| Smoking habit, current (versus former) | 0.61 (0.40–0.92) | 0.019 | |||
| CIRS-CI ≥ 3 | 1.66 (1.29–2.14) | < 0.001 | |||
| Presence of coronary artery disease | 1.27 (1.009–1.60) | 0.042 | |||
| Presence of chronic kidney disease | 1.40 (1.12–1.74) | 0.002 | |||
| Presence of dementia | 2.18 (1.61–2.95) | < 0.001 | 1.75 (1.06–2.90) | 0.030 | |
| Presence of cancer | 1.95 (1.39–2.73) | < 0.001 | |||
| Overt cognitive impairment (SBT score ≥ 10) | 1.91 (1.49–2.45) | < 0.001 | |||
| Probable depression (GDS score > 2) | 1.38 (1.02–1.85) | 0.033 | |||
| Clinically significant disability (BI ≤ 40) | 2.66 (2.07–3.41) | < 0.001 | |||
The multivariate model has been adjusted for anthropometric variables, smoking habit, comorbidities, overt cognitive impairment, probable depression and clinically significant disability
COPD indicates Chronic Obstructive Pulmonary Disease, HF heart failure, HR hazard ratio, CIRS-CI Cumulative Illness Rating Scale, comorbidity index, SBT short blessed test, GDS geriatric depression scale, BI Barthel index
In bold are significant variables
The Hosmer and Lemeshow Test for the multivariate adjusted model was p = 0.877
Figure 1 reported the distribution of survivors/deaths in the three groups of patients. Deaths were significantly more numerous in COPD + HF in the follow-up of six months and one year (χ2 7.74, p = 0.021 and χ2 9.69, p = 0.008, respectively). In addition, the Kaplan–Meier curves of the three study groups (Fig. 2) showed a stratified and statistically significant higher risk of mortality for all causes (p = 0.010 at Gehan–Breslow–Wilcoxon test), respiratory causes (p = 0.006), cardiovascular causes (p = 0.046) and respiratory and cardiovascular causes (p = 0.009).
Fig. 1.
Percentage of deaths during hospitalization and in the follow-up of 3 and 6 months and one year. *p < 0.05 versus COPD. Numbers over black bars represent the absolute number of deaths
Fig. 2.
Kaplan–Meier curves. The analysis has been performed with the Gehan–Breslow–Wilcoxon test. CV indicates cardiovascular
Discussion
An elderly patient with COPD or HF represents a prototype to evaluate chronicity and disease progression, and the internist as a hospitalist is the physician that should typically exercise a holistic approach to complexity [28]. In a large population of elderly patients admitted to internal medicine wards, our findings demonstrate that the coexistence of both diseases in the same patients is associated with clinical peculiarities, particularly a worse prognosis in the context of a follow-up of one year. Therefore, a synergic association may be hypothesized.
The burden of chronicity is globally becoming a major challenge for health care systems. Thus, the identification of the varied clinical characteristics may help to better focus on the health policy administrative-economic efforts, higher health care resource utilization and costs [29], highlighting the possibility for a multidisciplinary and integrated care plan of cure. Our study reinforces these considerations by comparing patients with COPD, HF or COPD + HF. Although some aspects reported herewith are well known, such as the specific phenotypic characteristics of HF patients (prevalently older females in comparison to COPD), we found that the burden of care was progressively higher from COPD to HF, reaching the maximal impact in patients having both the diseases. In them, there were a high number of previous hospitalizations, comorbidities with a peculiar prevalence of chronic kidney disease and also a higher number of drugs prescriptions at admission, discharge and follow-up. All these data identify a clinical subset with a worse mortality prognosis for all causes, evident after 6 months and significant at 1 year (Table 3 and Figures).
Patients with COPD + HF represent clinically complex patients with different phenotypes, in whom baseline variables as sex, age and associated comorbidities have a different pattern of expression. In general, COPD and HF have a higher prevalence in men and women, respectively [30, 31]. However, in the present cohort, patients with both conditions had a sex-specific prevalence similar to COPD alone [32]. Age is a significant risk factor for most chronic diseases and multimorbidity is dramatically present in older patients [33]. The multimorbidity profile of these diseases in the aging process has been studied from a network perspective, revealing that in patients with COPD + HF the number of concomitant chronic conditions is substantially higher than that found in the general population [32]. The burden of comorbidities, shown by selectively higher values of CIRS-SI and CIRS-CI in our patients with COPD + HF, may be of help to direct prevention and management strategies. Of note, the trend in diabetes prevalences (27%, 32% and 37% in COPD, HF, and COPD + HF patients, respectively), along with a higher and significant difference in chronic kidney (44% in patients with COPD + HF) suggests a link among these chronic conditions, all mediated by dysmetabolism and low-grade chronic inflammation [34]. Furthermore, in the last few years HF has been consistently associated with the presence of clonal hemopoiesis of indeterminate potential (CHIP), a common age-related phenomenon characterized by the presence of somatic mutations in clonal leukocytes that are able to drive an aberrant inflammatory response [35]. Recently, also COPD has been associated with CHIP [36], which may therefore be a common ground for COPD and HF that warrants further studies to elucidate the potential pathophysiological link between the two conditions. Nonetheless, the simultaneous presence of both diseases highlights a population of elderly people with a higher morbidity burden, usually associated with a greater risk of polypharmacy [37] and higher use of healthcare services [38, 39]. This aspect is in line with the higher number of drugs prescribed (at admission, discharge and follow-up) (Table 2) and the prevalence of previous hospitalizations (Table 1) in our patients with COPD + HF.
Prognosis in COPD + HF patients has been evaluated in different settings. Although several studies described a worsening effect of COPD and HF when coexisting in the same patient [9, 13, 15–17], data on hospitalized and elderly patients are scarce and do not confirm this finding [16]. However, the methodology of these studies, focused on a reference population (either COPD or HF) in which the additive effect of the other disease was evaluated, is likely to be the reason for discordant results, because these studies were carried out in pulmonological (COPD) or cardiological (HF) subspecialty settings and, thus, with varying diagnostic accuracy and treatment appropriateness [40]. Moreover, they generally considered only two groups (e.g., COPD vs COPD + HF or HF vs HF + COPD), likely missing the comprehensive multimorbidity context typical of elderly patients as well as the opportunity to observe an interaction effect and the relative weight of both diseases (COPD plus HF) in the same patient. As compared to the existing knowledge, including very recent studies still based on administrative data from outpatients initially selected for a single disease (COPD) [41], the novelty of our study consists into the peculiar internal medicine dataset of elderly hospitalized patients, where we could perform a real-life evaluation by a head-to-head comparison of the three different conditions (COPD, HF and COPD plus HF). This allowed us to evaluate any single difference among them, as well as to distinguish their burden effect on the outcomes. Of note, there were no differences in one-year mortality between COPD and HF alone, while mortality was significantly higher in patients with both diseases. Furthermore, the length of hospital stay was similar in the three groups, confirming that the hospitalization burden was similar. Throughout the entire follow-up period, we noted that although mortality rates during hospitalization and at three months were higher in patients with COPD + HF, this difference became statistically significant (versus COPD) only at six months and one year, perhaps owing to the long-term chronicity and complexity of these patients. Albeit not statistically significant, prognosis seems to be better for COPD alone than for HF alone [9, 15]. In the latter category, older age and a higher prevalence of other comorbidities (atrial fibrillation, diabetes and chronic kidney disease) might explain this result. Finally, in patients with COPD + HF, the higher risk of death was confirmed in the multivariate model adjusted for other common risk factors potentially influencing prognosis, such as anthropometric variables, smoking habit, comorbidities, cognitive impairment, depression and clinically significant disability. This finding again highlights the several possible interactions and synergisms between COPD and HF [12] that did worsen the overall patient prognosis. In our stratification survival analyses, patients with COPD + HF had a worse mortality rate for all causes and respiratory or cardiovascular causes (Fig. 2). The presence of dementia, a predictor of death in elderly patients [42], was independently associated with mortality at one year.
The major strengths of the present study are the large and real-life cohort of elderly patients recruited and the novelty of an approach based upon the evaluation of these distinct patient categories. As for the limitations, we should mention the retrospective nature of the analyses derived from a dataset registry, the relatively short follow-up (one year), and the lack of precise spirometric data confirming the persistent airflow limitation of COPD patients. This limitation, which on the other hand is common to most of the studies published in the field, could have induced a an overdiagnosis of COPD mainly based on clinical findings and historical informations [43]. With this caution in mind, this retrospective analysis demonstrates that hospitalized elderly patients with COPD and HF have a worse prognosis than those with COPD or HF alone. This finding may help to plan and tailor therapeutic and management interventions for these patients.
Acknowledgements
Investigators and co-authors of the REPOSI (REgistro POliterapie SIMI, Società Italiana di Medicina Interna) Study. Group are as follows: Steering Committee—Pier Mannuccio Mannucci (Chair) (Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milano), Alessandro Nobili (co-chair) (Istituto di Ricerche Farmacologiche Mario Negri IRCCS, Milano), Giorgio Sesti (Presidente SIMI), Antonello Pietrangelo (Direttore CRIS – SIMI), Francesco Perticone (Università Magna Grecia Policlinico Mater Domini, Catanzaro), Francesco Violi (Policlinico Umberto I, Roma), Salvatore Corrao (ARNAS Civico, Di Cristina, Benfratelli, DiBiMIS, Università di Palermo, Palermo), Alessandra Marengoni (Spedali Civili di Brescia, Brescia), Mauro Tettamanti, Luca Pasina, Carlotta Franchi (Istituto di Ricerche Farmacologiche Mario Negri IRCCS, Milano). Clinical Data Monitoring and Revision: Carlotta Franchi, Alessio Novella, Mauro Tettamanti, Gabriella Miglio (Istituto di Ricerche Farmacologiche Mario Negri IRCCS, Milano). Database Management and Statistics: Mauro Tettamanti, Alessia Antonella Galbussera, Ilaria Ardoino, Alessio Novella (Istituto di Ricerche Farmacologiche Mario Negri IRCCS, Milano).
Investigators—Domenico Prisco, Elena Silvestri, Giacomo Emmi, Alessandra Bettiol, Irene Mattioli (Azienda Ospedaliero Universitaria Careggi Firenze, SOD Medicina Interna Interdisciplinare); Gianni Biolo, Michela Zanetti, Giacomo Bartelloni, Michele Zaccari, Massimiliano Chiuch (Azienda Sanitaria Universitaria Integrata di Trieste, Clinica Medica Generale e Terapia Medica); Massimo Vanoli, Giulia Grignani, Edoardo Alessandro Pulixi (Azienda Ospedaliera della Provincia di Lecco, Ospedale di Merate, Lecco, Medicina Interna); Matteo Pirro, Graziana Lupattelli, Vanessa Bianconi, Riccardo Alcidi, Alessia Giotta, Massimo R. Mannarino (Azienda Ospedaliera Santa Maria della Misericordia, Perugia, Medicina Interna, Angiologia Malattie da Arteriosclerosi); Domenico Girelli, Fabiana Busti, Giacomo Marchi (Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Medicina Generale e Malattie Aterotrombotiche e Degenerative); Mario Barbagallo, Ligia Dominguez, Vincenza Beneduce, Federica Cacioppo (Azienda Ospedaliera Universitaria Policlinico Giaccone Policlinico di Palermo, Palermo, Unità Operativa di Geriatria e Lungodegenza); Salvatore Corrao, Giuseppe Natoli, Salvatore Mularo, Massimo Raspanti, Christiano Argano, Federica Cavallaro (A.R.N.A.S. Civico, Di Cristina, Benfratelli, Palermo, UOC Medicina Interna ad Indirizzo Geriatrico- Riabilitativo); Marco Zoli, Maria Laura Matacena, Giuseppe Orio, Eleonora Magnolfi, Giovanni Serafini, Angelo Simili, Mattia Brunori, Ilaria Lazzari, Angelo Simili (Azienda Ospedaliera Universitaria Policlinico S. Orsola-Malpighi, Bologna, Unità Operativa di Medicina Interna Zoli); Maria Domenica Cappellini, Giovanna Fabio, Margherita Migone De Amicis, Giacomo De Luca, Natalia Scaramellini, Valeria Di Stefano, Simona Leoni, Sonia Seghezzi, Alessandra Danuto Di Mauro, Diletta Maira, Marta Mancarella (Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milano, Unità Operativa Medicina Interna IA); Tiziano Lucchi, Paolo Dionigi Rossi, Marta Clerici, Simona Leoni, Alessandra Danuta Di Mauro, Giulia Bonini, Federica Conti, Silvia Prolo, Maddalena Fabrizi, Miriana Martelengo, Giulia Vigani, Paola Nicolini (Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milano, Geriatria); Antonio Di Sabatino, Emanuela Miceli, Marco Vincenzo Lenti, Martina Pisati, Lavinia Pitotti, Donatella Padula, Valentina Antoci, Ginevra Cambiè (IRCCS Policlinico San Matteo di Pavia, Pavia, Clinica Medica I, Reparto 11); Roberto Pontremoli, Valentina Beccati, Giulia Nobili, Giovanna Leoncini, Jacopo Alberto, Federico Cattaneo (IRCCS Azienda Ospedaliera Universitaria San Martino-IST di Genova, Genova, Clinica di Medicina Interna 2); Luigi Anastasio, Lucia Sofia, Maria Carbone (Ospedale Civile Jazzolino di Vibo Valentia, Vibo Valentia, Medicina Generale); Francesco Cipollone, Maria Teresa Guagnano, Ilaria Rossi, Emanuele Valeriani, Damiani D’Ardes, Lucia Esposito, Simona Sestili, Ermanno Angelucci (Ospedale Clinicizzato SS. Annunziata, Chieti, Clinica Medica); Gerardo Mancuso, Daniela Calipari, Mosè Bartone (Ospedale Giovanni Paolo II Lamezia Terme, Catanzaro, Unità Operativa Complessa Medicina Interna); Giuseppe Delitala, Maria Berria, Alessandro Delitala (Azienda ospedaliera-universitaria di Sassari, Clinica Medica); Maurizio Muscaritoli, Alessio Molfino, Enrico Petrillo, Antonella Giorgi, Christian Gracin, Giovanni Imbimbo (Policlinico Umberto I, Sapienza Università di Roma, Medicina Interna e Nutrizione Clinica Policlinico Umberto I); Giuseppe Zuccalà, Gabriella D’Aurizio (Policlinico Universitario A. Gemelli, Roma, Roma, Unità Operativa Complessa Medicina d'Urgenza e Pronto Soccorso)Giuseppe Romanelli, Alessandra Marengoni, Andrea Volpini, Daniela Lucente, Francesca Manzoni, Annalisa Pirozzi, Alberto Zucchelli (Unità Operativa Complessa di Medicina I a indirizzo geriatrico, Spedali Civili, Montichiari, Brescia); Antonio Picardi, Umberto Vespasiani Gentilucci, Paolo Gallo, Chiara Dell’Unto (Università Campus Bio- Medico, Roma, Medicina Clinica-Epatologia); Giuseppe Bellelli, Maurizio Corsi, Cesare Antonucci, Chiara Sidoli, Giulia Principato, Alessandra Bonfanti, Hajnalka Szabo, Paolo Mazzola, Andrea Piazzoli, Maurizio Corsi (Università degli studi di Milano-Bicocca Ospedale S. Gerardo, Monza, Unità Operativa di Geriatria); Franco Arturi, Elena Succurro, Bruno Tassone, Federica Giofrè (Università degli Studi Magna Grecia, Policlinico Mater Domini, Catanzaro, Unità Operativa Complessa di Medicina Interna); Maria Grazia Serra, Maria Antonietta Bleve (Azienda Ospedaliera "Cardinale Panico" Tricase, Lecce, Unità Operativa Complessa Medicina); Antonio Brucato, Teresa De Falco, Enrica Negro, Martino Brenna, Lucia Trotta, Giovanni Lorenzo Squintani (ASST FatebenefratelliSacco, Milano, Medicina Interna); Maria Luisa Randi, Fabrizio Fabris, Irene Bertozzi, Giulia Bogoni, Maria Victoria Rabuini, Tancredi Prandini, Francesco Ratti, Chiara Zurlo, Lorenzo Cerruti, Elisabetta Cosi (Azienda Ospedaliera Università di Padova, Padova, Clinica Medica I); Roberto Manfredini, Benedetta Boari, Alfredo De Giorgi, Ruana Tiseo, Giulia Marta Viglione, Caterina Savriè (Azienda OspedalieraUniversitaria Sant'Anna, Ferrara, Unità Operativa Clinica Medica); Giuseppe Paolisso, Maria Rosaria Rizzo, Claudia Catalano, Irene Di Meo (Azienda Ospedaliera Universitaria della Seconda Università degli Studi di Napoli, Napoli, VI Divisione di Medicina Interna e Malattie Nutrizionali dell'Invecchiamento); Claudio Borghi, Enrico Strocchi, Eugenia Ianniello, Mario Soldati, Silvia Schiavone, Alessio Bragagni, Francesca Giulia Leoni, Valeria De Sando, Sara Scarduelli, Michela Cammarosano, Ilenia Pareo (Azienda Ospedaliera Universitaria Policlinico S. Orsola-Malpighi, Bologna, Unità Operativa di Medicina Interna Borghi); Carlo Sabbà, Francesco Saverio Vella, Patrizia Suppressa, Giovanni Michele De Vincenzo, Alessio Comitangelo, Emanuele Amoruso, Carlo Custodero, Giuseppe Re, Andrea Schilardi, Francesca Loparco (Azienda Ospedaliero-Universitaria Consorziale Policlinico di Bari, Bari, Medicina Interna Universitaria C. Frugoni); Luigi Fenoglio, Andrea Falcetta, Alessia Valentina Giraudo, Salvatore D’Aniano (Azienda Sanitaria Ospedaliera Santa Croce e Carle di Cuneo, Cuneo, S. C. Medicina Interna); Anna L. Fracanzani, Silvia Tiraboschi, Annalisa Cespiati, Giovanna Oberti, Giordano Sigon, Felice Cinque (Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milano, UOC Medicina Generale ad Indirizzo Metabolico); Flora Peyvandi, Raffaella Rossio, Giulia Colombo, Pasquale Agosti, Erica Pagliaro, Eleonora Semproni (Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milano, Medicina Interna 2, Ematologia non tumorale e Coagulopatie); Canetta Ciro, Valter Monzani, Valeria Savojardo, Giuliana Ceriani, Christian Folli (Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milano, Medicina Interna Alta Intensità di Cure); Francesco Salerno, Giada Pallini (IRCCS Policlinico San Donato e Università di Milano, San Donato Milanese, Medicina Interna); Fabrizio Montecucco, Luciano Ottonello, Lara Caserza, Giulia Vischi, Salam Kassem, Luca Liberale (IRCCS Ospedale Policlinico San Martino e Università di Genova, Genova, Clinica Medica 1, Medicina Interna e Specialità Mediche); Nicola Lucio Liberato, Tiziana Tognin (ASST di Pavia, UOSD Medicina Interna, Ospedale di Casorate Primo, Pavia); Francesco Purrello, Antonino Di Pino, Salvatore Piro (Ospedale Garibaldi Nesima, Catania, Unità Operativa Complessa di Medicina Interna); Renzo Rozzini, Lina Falanga, Maria Stella Pisciotta, Francesco Baffa Bellucci, Stefano Buffelli, Camillo Ferrandina, Francesca Mazzeo, Elena Spazzini, Giulia Cono, Giulia Cesaroni (Ospedale Poliambulanza, Brescia, Medicina Interna e Geriatria); Giuseppe Montrucchio, Paolo Peasso, Edoardo Favale, Cesare Poletto, Carl Margaria, Maura Sanino (Dipartimento di Scienze Mediche, Università di Torino, Città della Scienza e della Salute, Torino, Medicina Interna 2 Unità Indirizzo d'Urgenza); Francesco Violi, Ludovica Perri (Policlinico Umberto I, Roma, Prima Clinica Medica); Luigina Guasti, Francesca Rotunno, Luana Castiglioni, Andrea Maresca, Alessandro Squizzato, Leonardo Campiotti, Alessandra Grossi, Roberto Davide Diprizio, Francesco Dentali (Università degli Studi dell'Insubria, Ospedale di Circolo e Fondazione Macchi, Varese, Medicina e Geriatria); Marco Bertolotti, Chiara Mussi, Giulia Lancellotti, Maria Vittoria Libbra, Matteo Galassi, Yasmine Grassi, Alessio Greco, Elena Bigi, Elisa Pellegrini, Laura Orlandi, Giulia Dondi, Lucia Carulli (Università di Modena e Reggio Emilia, Azienda Ospedaliero-Universitaria di Modena; Ospedale Civile di Baggiovara, Unità Operativa di Geriatria); Angela Sciacqua, Maria Perticone, Rosa Battaglia, Raffaele Maio, Aleandra Scozzafava, Valentino Condoleo, Tania Falbo, Lidia Colangelo; Marco Filice, Elvira Clausi (Università Geriatriche); Vincenzo Stanghellini, Eugenio Ruggeri, Sara del Vecchio, Ilaria Benzoni (Dipartimento di Scienze Mediche e Chirurgiche, Unità Operativa di Medicina Interna, Università degli Studi di Bologna/Azienda Ospedaliero- Universitaria S.Orsola-Malpighi, Bologna); Andrea Salvi, Roberto Leonardi, Giampaolo Damiani (Spedali Civili di Brescia, U.O. 3a Medicina Generale); Gianluca Moroncini, William Capeci, Massimo Mattioli, Giuseppe Pio Martino, Lorenzo Biondi, Pietro Pettinari, Monica Ormas, Emanuele Filippini, Devis Benfaremo, Roberto Romiti (Clinica Medica, Azienda Ospedaliera UniversitariaOspedali Riuniti di Ancona); Riccardo Ghio, Anna Dal Col (Azienda Ospedaliera Università San Martino, Genova, Medicina III); Salvatore Minisola, Luciano Colangelo, Mirella Cilli, Giancarlo Labbadia (Policlinico Umberto I, Roma, SMSC03Medicina Interna F e Malattie Metaboliche dell'osso); Antonella Afeltra, Benedetta Marigliano, Maria Elena Pipita (Policlinico Campus Biomedico Roma, Roma, Medicina Clinica); Pietro Castellino, Luca Zanoli, Alfio Gennaro, Agostino Gaudio, Samuele Pignataro (Azienda Ospedaliera Universitaria Policlinico – V. Emanuele, Catania, Dipartimento di Medicina); Francesca Mete, Miriam Gino (Ospedale degli Infermi di Rivoli, Torino, Medicina Interna)Guido Moreo, Silvia Prolo, Gloria Pina (Clinica San Carlo Casa di Cura Polispecialistica, Paderno Dugnano, Milano, Unità Operativa di Medicina Generale Emilio Bernardelli); Alberto Ballestrero, Fabio Ferrando, Roberta Gonella, Domenico Cerminara, Paolo Setti, Chiara Traversa, Camilla Scarsi (Clinica Di Medicina Interna ad Indirizzo Oncologico, Azienda Ospedaliera Università San Martino di Genova); Bruno Graziella, Stefano Baldassarre, Salvatore Fragapani, Gabriella Gruden (Medicina Interna III, Ospedale S. Giovanni Battista Molinette, Torino); Franco Berti, Giuseppe Famularo, Patrizia Tarsitani (Azienda Ospedaliera San Camillo Forlanini, Roma, Medicina Interna II); Roberto Castello, Michela Pasino (Ospedale Civile Maggiore Borgo Trento, Verona, Medicina Generale e Sezione di Decisione Clinica); Marcello Giuseppe Maggio Gian Paolo Ceda, Simonetta Morganti, Andrea Artoni, Margherita Grossi (Azienda Ospedaliero Universitaria di Parma, U.O.C Clinica Geriatrica); Stefano Del Giacco, Davide Firinu, Giulia Costanzo, Giacomo Argiolas, Giovanni Paoletti, Francesca Losa (Policlinico Universitario Duilio Casula, Azienda Ospedaliero-Universitaria di Cagliari, Cagliari, Medicina Interna, Allergologia ed Immunologia Clinica); Giuseppe Montalto, Anna Licata, Filippo Alessandro Montalto, Angelo Rizzo (Azienda Ospedaliera Universitaria Policlinico Paolo Giaccone, Palermo, UOC di Medicina Interna); Francesco Corica, Giorgio Basile, Antonino Catalano, Federica Bellone, Concetto Principato (Azienda Ospedaliera Universitaria Policlinico G. Martino, Messina, Unità Operativa di Geriatria); Lorenzo Malatino, Benedetta Stancanelli, Valentina Terranova, Salvatore Di Marca, Rosario Di Quattro, Lara La Malfa, Rossella Caruso (Azienda Ospedaliera per l'Emergenza Cannizzaro, Catania, Clinica Medica Università di Catania); Patrizia Mecocci, Carmelinda Ruggiero, Virginia Boccardi (Università degli Studi di Perugia-Azienda Ospedaliera S.M. della Misericordia, Perugia, Struttura Complessa di Geriatria); Tiziana Meschi, Andrea Ticinesi, Antonio Nouvenne (Azienda Ospedaliera Universitaria di Parma, U.O Medicina Interna e Lungodegenza Critica); Pietro Minuz, Luigi Fondrieschi, Giandomenico Nigro Imperiale, Sarah Morellini (Azienda Ospedaliera Universitaria Verona, Policlinico GB Rossi, Verona, Medicina Generale per lo Studio ed il Trattamento dell’Ipertensione Arteriosa); Mario Pirisi, Gian Paolo Fra, Daniele Sola, Mattia Bellan (Azienda Ospedaliera Universitaria Maggiore della Carità, Medicina Interna 1); Roberto Quadri, Erica Larovere, Marco Novelli (Ospedale di Ciriè, ASL TO4, Torino, S.C. Medicina Interna); Emilio Simeone, Rosa Scurti, Fabio Tolloso (Ospedale Spirito Santo di Pescara, Geriatria); Roberto Tarquini, Alice Valoriani, Silvia Dolenti, Giulia Vannini (Ospedale San Giuseppe, Empoli, USL Toscana Centro, Firenze, Medicina Interna I); Riccardo Volpi, Pietro Bocchi, Alessandro Vignali (Azienda Ospedaliera Universitaria di Parma, Clinica e Terapia Medica); Sergio Harari, Chiara Lonati, Federico Napoli, Italia Aiello (Divisione di Medicina Interna, Multimedica IRCSS, Milano); Francesco Purrello, Antonino Di Pino (Ospedale GaribaldiNesima – Catania, U.O.C Medicina Interna); Teresa Salvatore, Lucio Monaco, Carmen Ricozzi (Policlinico Università della Campania L. Vanvitelli, UOC Medicina Interna); Alberto Pilotto, Ilaria Indiano, Federica Gandolfo (Ente Ospedaliero Ospedali Galliera Genova, SC Geriatria Dipartimento Cure Geriatriche, Ortogeriatria e Riabilitazione)Franco Laghi Pasini, Pier Leopoldo Capecchi (Azienda Ospedaliera Universitaria Senese, Siena, Unità Operativa Complessa Medicina 2); Ranuccio Nuti, Roberto Valenti, Martina Ruvio, Silvia Cappelli, Alberto Palazzuoli (Azienda Ospedaliera Università Senese, Siena, Medicina Interna I); Mauro Bernardi, Silvia Li Bassi, Luca Santi, Giacomo Zaccherini (Azienda Ospedaliera Policlinico Sant’Orsola-Malpighi, Bologna, Semeiotica Medica Bernardi); Vittorio Durante, Daniela Tirotta, Giovanna Eusebi (Ospedale di Cattolica, Rimini, Medicina Interna); Marco Cattaneo, Maria Valentina Amoruso, Paola Fracasso, Cristina Fasolino (Azienda ospedaliera San Paolo, Milano, Medicina III); Moreno Tresoldi, Enrica Bozzolo, Sarah Damanti (IRCCS Ospedale San Raffaele – Milano, Medicina Generale e delle Cure Avanzate); Massimo Porta, Miriam Gino (AOU Città della Salute e della Scienza di Torino – Torino, Medicina Interna 1U).
Appendix
ICD-9 Codes
Hypertension: 40.x
Hypercholesterolemia 272.0
Coronary artery disease: 411.1, 413.x, 414.8, 414.9
Atrial fibrillation: 427.31
Peripheral artery disease 440.2.x, 440.4.x, 443.9.x
Diabetes: 250.x
Chronic kidney disease: 585.x
Osteoporosis: 733.0, 733.01
Dementia: 290.x, 294.1
Depression: 296.2, 296.3, 311.0
Cancer: 14.x, 15.x, 16.x, 17.x, 18.x, 19.x, 20.x
x: refers to all the subsequent subcodess
Funding
Open access funding provided by Università degli Studi di Verona within the CRUI-CARE Agreement.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Human and animal rights statement
The study was conducted according to Good Clinical Practice guidelines and the Declaration of Helsinki. The study was approved by the Ethical Committee of the IRCCS Ca’ Granda Maggiore Policlinico Hospital Foundation of Milan and by the ethics committees of the participating centres.
Conflict of Interest
The authors declare they have no financial interests.
Footnotes
The members of “REPOSI Investigators” are listed in Acknowledgements section.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ernesto Crisafulli, Email: ernesto.crisafulli@univr.it.
REPOSI Investigators:
Pier Mannuccio Mannucci, Giorgio Sesti, Antonello Pietrangelo, Francesco Perticone, Francesco Violi, Salvatore Corrao, Alessandra Marengoni, Mauro Tettamanti, Luca Pasina, Carlotta Franchi, Pier Mannuccio Mannucci, Alessandro Nobili, Giorgio Sesti, Antonello Pietrangelo, Francesco Perticone, Francesco Violi, Salvatore Corrao, Alessandra Marengoni, Mauro Tettamanti, Luca Pasina, Carlotta Franchi, Carlotta Franchi, Alessio Novella, Mauro Tettamanti, Gabriella Miglio, Mauro Tettamanti, Alessia Antonella Galbussera, Ilaria Ardoino, Alessio Novella, Domenico Prisco, Elena Silvestri, Giacomo Emmi, Alessandra Bettiol, Irene Mattioli, Gianni Biolo, Michela Zanetti, Giacomo Bartelloni, Michele Zaccari, Massimiliano Chiuch, Massimo Vanoli, Giulia Grignani, Edoardo Alessandro Pulixi, Matteo Pirro, Graziana Lupattelli, Vanessa Bianconi, Riccardo Alcidi, Alessia Giotta, Massimo R. Mannarino, Domenico Girelli, Fabiana Busti, Giacomo Marchi, Mario Barbagallo, Ligia Dominguez, Vincenza Beneduce, Federica Cacioppo, Salvatore Corrao, Giuseppe Natoli, Salvatore Mularo, Massimo Raspanti, Christiano Argano, Federica Cavallaro, Marco Zoli, Maria Laura Matacena, Giuseppe Orio, Eleonora Magnolfi, Giovanni Serafini, Angelo Simili, Mattia Brunori, Ilaria Lazzari, Angelo Simili, Maria Domenica Cappellini, Giovanna Fabio, Margherita Migone De Amicis, Giacomo De Luca, Natalia Scaramellini, Valeria Di Stefano, Simona Leoni, Sonia Seghezzi, Alessandra Danuto Di Mauro, Diletta Maira, Marta Mancarella, Tiziano Lucchi, Paolo Dionigi Rossi, Marta Clerici, Simona Leoni, Alessandra Danuta Di Mauro, Giulia Bonini, Federica Conti, Silvia Prolo, Maddalena Fabrizi, Miriana Martelengo, Giulia Vigani, Paola Nicolini, Antonio Di Sabatino, Emanuela Miceli, Marco VincenzoLenti, Martina Pisati, Lavinia Pitotti, Donatella Padula, Valentina Antoci, Ginevra Cambiè, Roberto Pontremoli, Valentina Beccati, Giulia Nobili, Giovanna Leoncini, Jacopo Alberto, Federico Cattaneo, Luigi Anastasio, Lucia Sofia, Maria Carbone, Francesco Cipollone, Maria Teresa Guagnano, Ilaria Rossi, Emanuele Valeriani, Damiani D’Ardes, Lucia Esposito, Simona Sestili, Ermanno Angelucci, Gerardo Mancuso, Daniela Calipari, Mosè Bartone, Giuseppe Delitala, Maria Berria, Alessandro Delitala, Maurizio Muscaritoli, Alessio Molfino, Enrico Petrillo, Antonella Giorgi, Christian Gracin, Giovanni Imbimbo, Giuseppe Zuccalà, Gabriella D’Aurizio, Giuseppe Romanelli, Alessandra Marengoni, Andrea Volpini, Daniela Lucente, Francesca Manzoni, Annalisa Pirozzi, Alberto Zucchelli, Antonio Picardi, Umberto Vespasiani Gentilucci, Paolo Gallo, Chiara Dell’Unto, Giuseppe Bellelli, Maurizio Corsi, Cesare Antonucci, Chiara Sidoli, Giulia Principato, Alessandra Bonfanti, Hajnalka Szabo, Paolo Mazzola, Andrea Piazzoli, Maurizio Corsi, Franco Arturi, Elena Succurro, Bruno Tassone, Federica Giofrè, Maria Grazia Serra, Maria Antonietta Bleve, Antonio Brucato, Teresa De Falco, Enrica Negro, Martino Brenna, Lucia Trotta, Giovanni Lorenzo Squintani, Maria Luisa Randi, Fabrizio Fabris, Irene Bertozzi, Giulia Bogoni, Maria Victoria Rabuini, Tancredi Prandini, Francesco Ratti, Chiara Zurlo, Lorenzo Cerruti, Elisabetta Cosi, Roberto Manfredini, Benedetta Boari, Alfredo Giorgi, Ruana Tiseo, Giulia Marta Viglione, Caterina Savriè, Giuseppe Paolisso, Maria Rosaria Rizzo, Claudia Catalano, Irene Di Meo, Claudio Borghi, Enrico Strocchi, Eugenia Ianniello, Mario Soldati, Silvia Schiavone, Alessio Bragagni, Francesca Giulia Leoni, Valeria Sando, Sara Scarduelli, Michela Cammarosano, Ilenia Pareo, Carlo Sabbà, Patrizia Suppressa, Giovanni Michele De Vincenzo, Alessio Comitangelo, Emanuele Amoruso, Carlo Custodero, Giuseppe Re, Andrea Schilardi, Francesca Loparco, Luigi Fenoglio, Andrea Falcetta, Alessia Valentina Giraudo, Salvatore D’Aniano, Anna L Fracanzani, Silvia Tiraboschi, Annalisa Cespiati, Giovanna Oberti, Giordano Sigon, Felice Cinque, Flora Peyvandi, Raffaella Rossio, Giulia Colombo, Pasquale Agosti, Erica Pagliaro, Eleonora Semproni, Canetta Ciro, Valter Monzani, Valeria Savojardo, Giuliana Ceriani, Christian Folli, Francesco Salerno, Giada Pallini, Fabrizio Montecucco, Luciano Ottonello, Lara Caserza, Giulia Vischi, Salam Kassem, Luca Liberale, Nicola Lucio Liberato, Tiziana Tognin, Francesco Purrello, Antonino Di Pino, Salvatore Piro, Renzo Rozzini, Lina Falanga, Maria Stella Pisciotta, Francesco Baffa Bellucci, Stefano Buffelli, Camillo Ferrandina, Francesca Mazzeo, Elena Spazzini, Giulia Cono, Giulia Cesaroni, Giuseppe Montrucchio, Paolo Peasso, Edoardo Favale, Cesare Poletto, Carl Margaria, Maura Sanino, Francesco Violi, Ludovica Perri, Luigina Guasti, Francesca Rotunno, Luana Castiglioni, Andrea Maresca, Alessandro Squizzato, Leonardo Campiotti, Alessandra Grossi, Roberto Davide Diprizio, Francesco Dentali, Marco Bertolotti, Chiara Mussi, Giulia Lancellotti, Maria Vittoria Libbra, Matteo Galassi, Yasmine Grassi, Alessio Greco, Elena Bigi, Elisa Pellegrini, Laura Orlandi, Giulia Dondi, Lucia Carulli, Angela Sciacqua, Maria Perticone, Rosa Battaglia, Raffaele Maio, Aleandra Scozzafava, Valentino Condoleo, Tania Falbo, Lidia Colangelo, Marco Filice, Elvira Clausi, Vincenzo Stanghellini, Eugenio Ruggeri, Sara del Vecchio, Ilaria Benzoni, Andrea Salvi, Roberto Leonardi, Giampaolo Damiani, Gianluca Moroncini, William Capeci, Massimo Mattioli, Giuseppe Pio Martino, Lorenzo Biondi, Pietro Pettinari, Monica Ormas, Emanuele Filippini, Devis Benfaremo, Roberto Romiti, Riccardo Ghio, Anna Dal Col, Salvatore Minisola, Luciano Colangelo, Mirella Cilli, Giancarlo Labbadia, Antonella Afeltra, Benedetta Marigliano, Maria Elena Pipita, Pietro Castellino, Luca Zanoli, Alfio Gennaro, Agostino Gaudio, Samuele Pignataro, Francesca Mete, Miriam Gino, Guido Moreo, Silvia Prolo, Gloria Pina, Alberto Ballestrero, Fabio Ferrando, Roberta Gonella, Domenico Cerminara, Paolo Setti, Chiara Traversa, Camilla Scarsi, Bruno Graziella, Stefano Baldassarre, Salvatore Fragapani, Gabriella Gruden, Franco Berti, Giuseppe Famularo, Patrizia Tarsitani, Roberto Castello, Michela Pasino, Marcello Giuseppe Maggio, Gian PaoloCeda, Simonetta Morganti, Andrea Artoni, Margherita Grossi, Stefano Del Giacco, Davide Firinu, Giulia Costanzo, Giacomo Argiolas, Giovanni Paoletti, Francesca Losa, Giuseppe Montalto, Anna Licata, Filippo Alessandro Montalto, Angelo Rizzo, Francesco Corica, Giorgio Basile, Antonino Catalano, Federica Bellone, Concetto Principato, Lorenzo Malatino, Benedetta Stancanelli, Valentina Terranova, Salvatore Di Marca, Rosario Di Quattro, Lara La Malfa, Rossella Caruso, Patrizia Mecocci, Carmelinda Ruggiero, Virginia Boccardi, Tiziana Meschi, Andrea Ticinesi, Antonio Nouvenne, Pietro Minuz, Luigi Fondrieschi, Giandomenico NigroImperiale, Sarah Morellini, Mario Pirisi, Gian Paolo Fra, Daniele Sola, Mattia Bellan, Roberto Quadri, Erica Larovere, Marco Novelli, Emilio Simeone, Rosa Scurti, Fabio Tolloso, Roberto Tarquini, Alice Valoriani, Silvia Dolenti, Giulia Vannini, Riccardo Volpi, Pietro Bocchi, Alessandro Vignali, Sergio Harari, Chiara Lonati, Federico Napoli, Italia Aiello, Francesco Purrello, Antonino Di Pino, Teresa Salvatore, Lucio Monaco, Carmen Ricozzi, Alberto Pilotto, Ilaria Indiano, Federica Gandolfo, Franco Laghi Pasini, Pier LeopoldoCapecchi, Ranuccio Nuti, Roberto Valenti, Martina Ruvio, Silvia Cappelli, Alberto Palazzuoli, Mauro Bernardi, Silvia Li Bassi, Luca Santi, Giacomo Zaccherini, Vittorio Durante, Daniela Tirotta, Giovanna Eusebi, Marco Cattaneo, Maria Valentina Amoruso, Paola Fracasso, Cristina Fasolino, Moreno Tresoldi, Enrica Bozzolo, Sarah Damanti, Massimo Porta, and Miriam Gino
References
- 1.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 2.Vanfleteren LE, Spruit MA, Franssen FM. Tailoring the approach to multimorbidity in adults with respiratory disease: the NICE guideline. Eur Respir J. 2017;49(2):1601696. doi: 10.1183/13993003.01696-2016. [DOI] [PubMed] [Google Scholar]
- 3.Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(8):631–639. doi: 10.1016/S2213-2600(15)00241-6. [DOI] [PubMed] [Google Scholar]
- 4.Mooney L, Hawkins NM, Jhund PS, Redfield MM, Vaduganathan M, Desai AS, Rouleau JL, Minamisawa M, Shah AM, Lefkowitz MP, Zile MR, Van Veldhuisen DJ, Pfeffer MA, Anand IS, Maggioni AP, Senni M, Claggett BL, Solomon SD, McMurray JJV. Impact of chronic obstructive pulmonary disease in patients with heart failure with preserved ejection fraction: insights from PARAGON-HF. J Am Heart Assoc. 2021;10(23):e021494. doi: 10.1161/JAHA.121.021494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Miguel DJ, Chancafe Morgan J, Jiménez GR. The association between COPD and heart failure risk: a review. Int J Chron Obstruct Pulmon Dis. 2013;8:305–312. doi: 10.2147/COPD.S31236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Argano C, Scichilone N, Natoli G, Nobili A, Corazza GR, Mannucci PM, Perticone F, Corrao S, REPOSI Investigators Pattern of comorbidities and 1-year mortality in elderly patients with COPD hospitalized in internal medicine wards: data from the RePoSI Registry. Intern Emerg Med. 2021;16(2):389–400. doi: 10.1007/s11739-020-02412-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pellicori P, Cleland JGF, Clark AL. Chronic obstructive pulmonary disease and heart failure: a breathless conspiracy. Heart Fail Clin. 2020;16(1):33–44. doi: 10.1016/j.hfc.2019.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Beghé B, Fabbri LM, Garofalo M, Schito M, Verduri A, Bortolotti M, Stendardo M, Ruggieri V, Fucili A, Sverzellati N, Della Casa G, Maietti E, Clini EM, Boschetto P. Three-year hospitalization and mortality in elderly smokers with chronic obstructive pulmonary disease or chronic heart failure. Respiration. 2019;97(3):223–233. doi: 10.1159/000492286. [DOI] [PubMed] [Google Scholar]
- 9.Smith MC, Wrobel JP. Epidemiology and clinical impact of major comorbidities in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2014;9:871–888. doi: 10.2147/COPD.S49621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Londoño KL, Formiga F, Chivite D, Moreno-Gonzalez R, Migone De Amicis M, Corbella X. Prognostic influence of prior chronic obstructive pulmonary disease in patients admitted for their first episode of acute heart failure. Intern Emerg Med. 2018;13(3):351–357. doi: 10.1007/s11739-018-1820-3. [DOI] [PubMed] [Google Scholar]
- 11.Ehteshami-Afshar S, Mooney L, Dewan P, Desai AS, Lang NN, Lefkowitz MP, Petrie MC, Rizkala AR, Rouleau JL, Solomon SD, Swedberg K, Shi VC, Zile MR, Packer M, McMurray JJV, Jhund PS, Hawkins NM. Clinical characteristics and outcomes of patients with heart failure with reduced ejection fraction and chronic obstructive pulmonary disease: insights from PARADIGM-HF. J Am Heart Assoc. 2021;10(4):e019238. doi: 10.1161/JAHA.120.019238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev. 2018;27(149):180057. doi: 10.1183/16000617.0057-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Testa G, Cacciatore F, Bianco A, Della-Morte D, Mazzella F, Galizia G, Gargiulo G, Curcio F, Liguori I, Sabusco A, Rengo F, Bonaduce D, Abete P. Chronic obstructive pulmonary disease and long-term mortality in elderly subjects with chronic heart failure. Aging Clin Exp Res. 2017;29(6):1157–1164. doi: 10.1007/s40520-016-0720-5. [DOI] [PubMed] [Google Scholar]
- 14.Carter P, Lagan J, Fortune C, Bhatt DL, Vestbo J, Niven R, Chaudhuri N, Schelbert EB, Potluri R, Miller CA. Association of cardiovascular disease with respiratory disease. J Am Coll Cardiol. 2019;73(17):2166–2177. doi: 10.1016/j.jacc.2018.11.063. [DOI] [PubMed] [Google Scholar]
- 15.van Deursen VM, Urso R, Laroche C, Damman K, Dahlström U, Tavazzi L, Maggioni AP, Voors AA. Comorbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail. 2014;16(1):103–111. doi: 10.1002/ejhf.30. [DOI] [PubMed] [Google Scholar]
- 16.Canepa M, Straburzynska-Migaj E, Drozdz J, Fernandez-Vivancos C, Pinilla JMG, Nyolczas N, Temporelli PL, Mebazaa A, Lainscak M, Laroche C, Maggioni AP, Piepoli MF, Coats AJS, Ferrari R, ESC-HFA Heart Failure Long-Term Registry Investigators Characteristics, treatments and 1-year prognosis of hospitalised and ambulatory heart failure patients with chronic obstructive pulmonary disease in the European Society of Cardiology Heart Failure Long-Term Registry. Eur J Heart Fail. 2018;20(1):100–110. doi: 10.1002/ejhf.964. [DOI] [PubMed] [Google Scholar]
- 17.Xu S, Ye Z, Ma J, Yuan T. The impact of chronic obstructive pulmonary disease on hospitalization and mortality in patients with heart failure. Eur J Clin Invest. 2021;51(1):e13402. doi: 10.1111/eci.13402. [DOI] [PubMed] [Google Scholar]
- 18.Mannucci PM, Nobili A, Pasina L, REPOSI Collaborators (REPOSI is the acronym of REgistro POliterapie SIMI, Società Italiana di Medicina Interna) Polypharmacy in older people: lessons from 10 years of experience with the REPOSI register. Intern Emerg Med. 2018;13(8):1191–1200. doi: 10.1007/s11739-018-1941-8. [DOI] [PubMed] [Google Scholar]
- 19.The REPOSI registry of multimorbidity and polypharmacy: https://smc-media.eu/web/reposi/. Accessed 29 May 2020
- 20.Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16(5):622–626. doi: 10.1111/j.1532-5415.1968.tb02103.x. [DOI] [PubMed] [Google Scholar]
- 21.Salvi F, Miller MD, Grilli A, Giorgi R, Towers AL, Morichi V, Spazzafumo L, Mancinelli L, Espinosa E, Rappelli A, Dessì-Fulgheri P. A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalised elderly patients. J Am Geriatr Soc. 2008;56(10):1926–1931. doi: 10.1111/j.1532-5415.2008.01935.x. [DOI] [PubMed] [Google Scholar]
- 22.Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry. 1983;140(6):734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- 23.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 24.Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 25.Freeman GH, Halton JH. Note on exact treatment of contingency, goodness of fit and other problems of significance. Biometrika. 1951;38(1–2):141–149. doi: 10.1093/biomet/38.1-2.141. [DOI] [PubMed] [Google Scholar]
- 26.Collett D. Modelling survival data in medical research. London: Chapman and Hall; 1994. [Google Scholar]
- 27.Mike V, Stanley KE, editors. Statistics in medical research: methods and issues, with applications in cancer research. NY, USA: Wiley; 1982. [Google Scholar]
- 28.Corrao S, Natoli G, Nobili A, Mannucci PM, Pietrangelo A, Perticone F, RePoSI Investigators Argano C Comorbidity does not mean clinical complexity: evidence from the RePoSI register. Intern Emerg Med. 2020;15(4):621–628. doi: 10.1007/s11739-019-02211-3. [DOI] [PubMed] [Google Scholar]
- 29.Schwab P, Dhamane AD, Hopson SD, Moretz C, Annavarapu S, Burslem K, Renda A, Kaila S. Impact of comorbid conditions in COPD patients on health care resource utilisation and costs in a predominantly Medicare population. Int J Chron Obstruct Pulmon Dis. 2017;12:735–744. doi: 10.2147/COPD.S112256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lam CSP, Arnott C, Beale AL, Chandramouli C, Hilfiker-Kleiner D, Kaye DM, Ky B, Santema BT, Sliwa K, Voors AA. Sex differences in heart failure. Eur Heart J. 2019;40(47):3859–3868c. doi: 10.1093/eurheartj/ehz835. [DOI] [PubMed] [Google Scholar]
- 31.Ntritsos G, Franek J, Belbasis L, Christou MA, Markozannes G, Altman P, Fogel R, Sayre T, Ntzani EE, Evangelou E. Gender-specific estimates of COPD prevalence: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:1507–1514. doi: 10.2147/COPD.S146390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carmona-Pírez J, Poblador-Plou B, Díez-Manglano J, Morillo-Jiménez MJ, Marín Trigo JM, Ioakeim-Skoufa I, Gimeno-Miguel A, Prados-Torres A. Multimorbidity networks of chronic obstructive pulmonary disease and heart failure in men and women: evidence from the EpiChron Cohort. Mech Ageing Dev. 2021;193:111392. doi: 10.1016/j.mad.2020.111392. [DOI] [PubMed] [Google Scholar]
- 33.Divo MJ, Celli BR, Poblador-Plou B, Calderón-Larrañaga A, de-Torres JP, Gimeno-Feliu LA, Bertó J, Zulueta JJ, Casanova C, Pinto-Plata VM, Cabrera-Lopez C, Polverino F, Carmona Píréz J, Prados-Torres A, Marin JM; EpiChron-BODE Collaborative Group. Chronic Obstructive Pulmonary Disease (COPD) as a disease of early aging: Evidence from the EpiChron Cohort. PLoS One. 2018;13(2):e0193143. 10.1371/journal.pone.0193143. [DOI] [PMC free article] [PubMed]
- 34.Li Z, Zhao H, Wang J. Metabolism and chronic inflammation: the links between chronic heart failure and comorbidities. Front Cardiovasc Med. 2021;8:650278. doi: 10.3389/fcvm.2021.650278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jaiswal S, Ebert BL. Clonal hematopoiesis in human aging and disease. Science. 2019 doi: 10.1126/science.aan4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miller PG, Qiao D, Rojas-Quintero J, Honigberg MC, Sperling AS, Gibson CJ, Bick AG, Niroula A, McConkey ME, Sandoval B, Miller BC, Shi W, Viswanathan K, Leventhal M, Werner L, Moll M, Cade BE, Barr RG, Correa A, Cupples LA, Gharib SA, Jain D, Gogarten SM, Lange LA, London SJ, Manichaikul A, O'Connor GT, Oelsner EC, Redline S, Rich SS, Rotter JI, Ramachandran V, Yu B, Sholl L, Neuberg D, Jaiswal S, Levy BD, Owen CA, Natarajan P, Silverman EK, van Galen P, Tesfaigzi Y, Cho MH, Ebert BL, COPDGene Study Investigators National heart, lung, and blood institute trans-omics for precision medicine consortium. Association of clonal hematopoiesis with chronic obstructive pulmonary disease. Blood. 2022;139(3):357–368. doi: 10.1182/blood.2021013531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Menditto E, Gimeno Miguel A, Moreno Juste A, Poblador Plou B, Aza Pascual-Salcedo M, Orlando V, González Rubio F, Prados TA. Patterns of multimorbidity and polypharmacy in young and adult population: Systematic associations among chronic diseases and drugs using factor analysis. PLoS ONE. 2019;14(2):e0210701. doi: 10.1371/journal.pone.0210701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rinne ST, Liu CF, Wong ES, Hebert PL, Heidenreich P, Bastian LA, Au DH. Organisational structure for chronic heart failure and chronic obstructive pulmonary disease. Am J Manag Care. 2016;22(3):e82–e87. [PubMed] [Google Scholar]
- 39.Palladino R, Tayu Lee J, Ashworth M, Triassi M, Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing. 2016;45(3):431–435. doi: 10.1093/ageing/afw044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Güder G, Störk S. COPD and heart failure: differential diagnosis and comorbidity. Herz. 2019;44(6):502–508. doi: 10.1007/s00059-019-4814-7. [DOI] [PubMed] [Google Scholar]
- 41.Gulea C, Zakeri R, Quint JK. Differences in outcomes between heart failure phenotypes in patients with coexistent chronic obstructive pulmonary disease: a cohort study. Ann Am Thorac Soc. 2022;19(6):971–980. doi: 10.1513/AnnalsATS.202107-823OC. [DOI] [PubMed] [Google Scholar]
- 42.Marengoni A, Corrao S, Nobili A, Tettamanti M, Pasina L, Salerno F, Iorio A, Marcucci M, Bonometti F, Mannucci PM, SIMI Investigators In-hospital death according to dementia diagnosis in acutely ill elderly patients: the REPOSI study. Int J Geriatr Psychiatry. 2011;26(9):930–936. doi: 10.1002/gps.2627. [DOI] [PubMed] [Google Scholar]
- 43.Diab N, Gershon AS, Sin DD, Tan WC, Bourbeau J, Boulet LP, Aaron SD. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(9):1130–1139. doi: 10.1164/rccm.201804-0621CI. [DOI] [PubMed] [Google Scholar]