Abstract
Psychosocial factors are related to immune, viral, and vaccination outcomes. Yet, this knowledge has been poorly represented in public health initiatives during the COVID-19 pandemic. This review provides an overview of biopsychosocial links relevant to COVID-19 outcomes by describing seminal evidence about these associations known prepandemic as well as contemporary research conducted during the pandemic. This focuses on the negative impact of the pandemic on psychosocial health and how this in turn has likely consequences for critically relevant viral and vaccination outcomes. We end by looking forward, highlighting the potential of psychosocial interventions that could be leveraged to support all people in navigating a postpandemic world and how a biopsychosocial approach to health could be incorporated into public health responses to future pandemics.
Keywords: viral susceptibility, psychosocial factors, vaccine efficacy, psychosocial stress, social connection, loneliness, COVID-19
Highlights
Prepandemic evidence links psychosocial factors to viral and vaccination outcomes.
Early evidence reported during the COVID-19 pandemic is consistent with these prior findings.
To better support people during future public health crises, we need structural-level policy changes that take a biopsychosocial approach as well as increased access to individual-level psychosocial interventions.
Tweet
Could psychology have made the pandemic better? Read here for critical information on how our minds impact COVID-19 outcomes such as viral susceptibility, severity, and effective vaccination responses, and how biopsychosocial interventions might protect our future health.
Psychosocial factors are defined as intersecting social, environmental, and cultural influences on individual thoughts, behaviors, and emotions (APA Dictionary of Psychology, 2022). Examples include depressive and anxiety symptoms, stress, loneliness, socioeconomic standing, and discrimination. The role that these psychosocial factors play in predicting susceptibility to viral infections and outcomes has been the subject of decades of scientific research (e.g., Cohen, 2021). However, during the COVID-19 pandemic, this evidence was notably absent from public discourse and was not explicitly drawn upon in the formation of public health policy. Yet, this research has considerable and continued relevance to the COVID-19 pandemic and beyond. These psychosocial factors have been repeatedly shown to influence physiological parameters relevant to infectious disease including inflammation (Muscatell et al., 2020; Rosenblat et al., 2014; Smith et al., 2020; Uchino et al., 2018), general immune protection (Avitsur et al., 2009; Segerstrom & Miller, 2004), the likelihood of viral infection after virus exposure (Falagas et al., 2010), symptom severity (O’Connor et al., 2021), and vaccine efficacy (Pedersen et al., 2009). The present review highlights the importance of these influences on pandemic outcomes. We argue that our understanding is incomplete if we focus solely on whether or not individuals get exposed to COVID-19. Instead, we must understand the complex interactions between the virus, ourselves, and our social environments to inform policy decisions for future pandemics.
This review serves as a companion article to an Association of Psychological Science task force event held in January 2022, which discussed evidence on biopsychosocial determinants of viral susceptibility, recovery, and vaccine responses relevant to COVID-19 and future pandemics.1 This review synthesizes key evidence and discussions from that event, highlighting what was known prior to the COVID-19 pandemic, evidence that emerged during the pandemic, and recommendations for the future.
Psychosocial Factors and COVID-19
Why Care About Psychosocial Factors in the Context of the COVID-19 Pandemic?
Worldwide Psychosocial Health Was Adversely Affected by the COVID-19 Pandemic
Prepandemic estimates placed the worldwide prevalence of anxiety and depressive disorders at 3.6% and 4.4% respectively (World Health Organization, 2017). Although not a perfect comparison, multiple systematic reviews conducted during the pandemic indicated substantial rises in psychological health concerns with estimates suggesting between 14–48% of adults worldwide experienced depressive symptoms, 6–51% experienced anxiety, and 14–50% experienced distress (Chekole & Abate, 2021; Necho et al., 2021; Xiong et al., 2020), with similar increases observed among children (Samji et al., 2022). Meta-analyses have further shown increased prevalence and severity of loneliness (Ernst et al., 2022). Collectively, this evidence demonstrates that the COVID-19 pandemic and resulting stay-at-home orders, changes in routines, and fear and unknowns about contracting the virus placed a significant burden on individuals’ psychosocial health (Holman et al., 2020), which may have been exacerbated among people experiencing personal loss or vicarious trauma through media exposures (Thompson et al., 2022). Although worsening psychosocial health is an important outcome itself, what is often overlooked is the concurrent impact psychosocial factors may have on immunity and the possible implications for viral outcomes.
Prepandemic We Knew Psychosocial Factors Impacted Immunity and Viral Outcomes
Systematic reviews and meta-analyses examining associations between a range of psychosocial factors (such as loneliness, positive and negative emotions) and immunity have consistently demonstrated moderate-to-large effects on enumerative and functional immunological measures (Marsland et al., 2007; Segerstrom & Miller, 2004; Zorrilla et al., 2001). For example, a seminal meta-analytic review of over 300 articles concluded that there was robust evidence that psychological stress impacts immunity, with consistent evidence for associations between chronic stressors relevant to the pandemic (e.g., loss of control, bereavement, isolation) and the suppression of both cellular and humoral measures of immunity (Segerstrom & Miller, 2004). Psychosocial factors have been further correlated with viral susceptibility, with one systematic review finding 41 of 44 studies reported at least one statistically significant association between psychosocial variables and risk for acute respiratory tract infections (Falagas et al., 2010).
Considering psychosocial factors through a broader societal lens, socioeconomic disadvantage, which is a chronic and uncontrollable psychosocial stressor, has been associated with increased risk for upper respiratory infections during prior influenza pandemics (Mamelund et al., 2021; Rutter et al., 2012) as well as higher hospitalization rates (Levy et al., 2013). Lower socioeconomic status (SES) is thought to confer risk for poorer immune outcomes through a variety of factors, including increased exposure to financial stress, negative affect, and less access to coping resources (Gallo & Matthews, 2003). Relatedly, people of color from historically marginalized groups have an elevated risk of infections, including higher rates of tuberculosis among Black Americans and immigrants in the United States (Stewart et al., 2018) and among indigenous people internationally (Tollefson et al., 2013). Many have argued that structural and interpersonal racial discrimination may underlie such associations (Paradies et al., 2015).
Some of the most rigorous evidence supporting the causal influence of psychosocial factors on viral outcomes comes from experimental viral challenge studies. In these investigations, healthy participants are exposed to standardized doses of viruses, including common cold and seasonal coronaviruses, before being quarantined. Serological and clinical measurements are then taken to determine infection status and symptom severity. A series of such studies have shown, that negative emotions, stressful life events, everyday perceived stress, isolation, and conflict, measured prior to virus exposure, can increase viral susceptibility and symptom severity (see Cohen, 2021). Furthermore, these effects may vary depending on social contextual factors as illustrated by Wiley and colleagues (2022), who found that Black Americans were less likely to benefit from the protective effects of positive psychological factors (e.g., self-esteem) on upper respiratory illness compared to White Americans. This suggests people from marginalized groups of color may experience diminished benefits from psychological resources that otherwise enhance immunity and protect against infection (Marsland et al., 2007).
Evidence Associating Psychosocial Factors With COVID-19 Outcomes
In an early prospective cohort study of over 400,000 people in the United Kingdom, people with a history of psychiatric disorder were around 1.5 times more likely to be diagnosed or hospitalized with COVID-19 and twice as likely to die (Yang et al., 2020). Since then, other large cohort studies have shown similar associations (e.g., Fond et al., 2021; Taquet et al., 2021). Associations between psychological distress and COVID-19 infection and severity have also been reported in student samples (Vedhara et al., 2022) and the general population (Ayling et al., 2022).
Considering social influences on COVID-19 outcomes, an early review of SES and COVID-19 infections in the United Kingdom and the United States found that lower SES was related to greater risk of infection and severity (Wachtler et al., 2020), which may reflect financial strain, housing insecurity, and poorer air quality that may accompany socioeconomic disadvantage (Rozenfeld et al., 2020). Similarly, two recent reviews reported that Black and Hispanic individuals experienced higher rates of infection, hospitalization, and COVID-19-related mortality compared to their White peers (Mackey et al., 2021; Mude et al., 2021) and another study found that more racially segregated U.S. counties had higher infection and mortality rates than more integrated counties (Torrats-Espinosa, 2021). Along with racial discrimination and segregation, higher rates of COVID-19 morbidity and mortality among people of color could be due to greater perseveration regarding finances and contracting (and dying from) the virus (Williams et al., 2022). Although further evidence is needed, early evidence shows that, as with other viral infections, susceptibility to and severity of COVID-19 is associated with psychosocial factors.
Prepandemic We Knew Psychosocial Factors Were Related to Vaccination Responses
Given that psychosocial factors can influence immunity, and vaccination relies on the body mounting an appropriate immune response, there has been a long-standing interest in the association between psychosocial factors and vaccination outcomes.
Prepandemic, many observational studies demonstrated an association between negative emotional states (including stress, depressive symptoms, and negative affect) and reduced antibody responses to a range of vaccinations including influenza (Pedersen et al., 2009) and Hepatitis B (Marsland et al., 2006). Psychological stress has been the most widely investigated psychosocial factor in this context, with meta-analytic evidence demonstrating a small-to-moderate negative association between stress and vaccine-specific antibody responses, particularly among older adults (Pedersen et al., 2009) and caregivers (Kiecolt-Glaser et al., 1996; Vedhara et al., 1999). Furthermore, evidence from studies measuring positive mood finds significant associations in the opposite direction (Ayling et al., 2018; Marsland et al., 2006).
Studies have also examined the impact of loneliness on vaccine responses with Pressman and colleagues (2005) finding that loneliness and small social network size were associated with poor antibody responses to influenza vaccination among first-year college students. Other work has focused on contextual social features such as race and SES. For example, children of lower SES had poorer antibody responses to several childhood vaccines (Hoes et al., 2018). Stetler and colleagues (2006) also found lower influenza vaccine antibody responses among Black adults randomized to recall experiences of racial discrimination prior to vaccination as compared to participants in a control condition who were not primed to recall such experiences. Results from meta-analyses support these findings with evidence of small, but significant positive associations of social integration and perceptions of social support with the magnitude of antibody response to vaccination (Uchino et al., 2020).
This observational evidence is supported by a small number of experimental studies that have attempted to enhance vaccine outcomes by employing psychological interventions, so-called psychological adjuvants. In a recent systematic review, Vedhara and colleagues (2019) concluded there was early evidence to suggest that psychological interventions may enhance antibody responses to vaccination but larger and more rigorous trials are needed.
Evidence Associating Psychological Factors and SARS-CoV2 Vaccination Responses
Although evidence supports the influence of psychosocial factors on antibody responses to vaccination, to date limited research has examined this in the context of SARS-CoV-2 vaccines, although we are aware of several studies that are underway. One of the few published studies in this area is of 676 adults from an ongoing UK-based longitudinal study who had antibodies measured following a single dose of the COVID-19 vaccine. The authors found that less social cohesion was associated with lower antibody responses, and this was in part mediated by feelings of loneliness (Gallagher et al., 2022). However, they did not examine whether effects differed by vaccine type. Nonetheless, this mirrors prepandemic work that found greater loneliness and small social network size to predict poorer antibody response to influenza vaccination among first-year college students (Pressman et al., 2005).
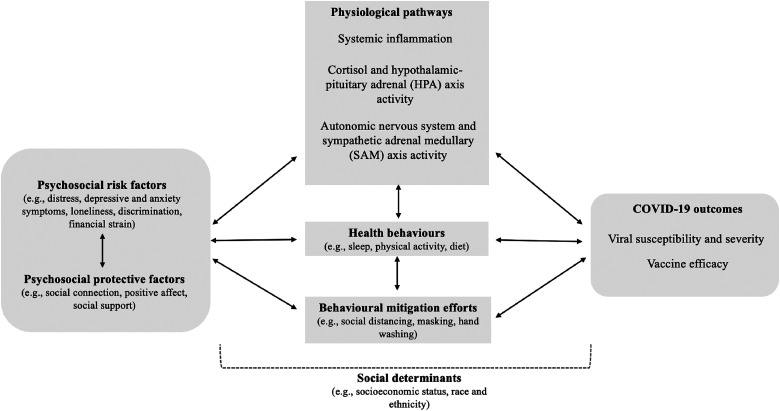
In summary, decades of research have shown that psychosocial factors influence viral susceptibility and vaccine efficacy, with early COVID-19 research following a similar pattern. These psychosocial factors are thought to impact COVID-19 viral susceptibility and vaccine efficacy through a variety of interacting biobehavioral pathways. This includes systemic inflammation, autonomic and neuroendocrine functioning, and health behaviors that may have been disrupted by public health policies to mitigate the spread of the virus. These pathways are illustrated in Figure 1 and described in the supplemental file.2
Figure 1.
Psychosocial factors may relate to COVID-19 through interacting physiological, health behavior, and behavioral mitigation pathways that may differ depending on socioeconomic status, race, and ethnicity.
Moving Forward, What Could Be Done Differently?
Many public health initiatives created to mitigate the spread of COVID-19 were well intentioned and dramatically reduced the spread of COVID-19 and excess deaths. Nevertheless, along with losing loved ones and fears about the virus, these mitigation efforts may have had unintended consequences for psychosocial well-being and in turn, viral and vaccine outcomes. Unfortunately, as can be seen from the above, many of these consequences were entirely predictable, with ample prepandemic evidence demonstrating that psychosocial factors influence viral and vaccine outcomes. Yet, prior findings relating to biopsychosocial relationships in this context appear to have been largely overlooked when formulating public health policy responses. While we cannot change the past, in the following sections we look forward, considering what steps could be taken to address similar oversights in the future.
Inclusion of Psychosocial Risk Factors in Public Health Models
The evidence outlined above illustrates that a range of psychosocial factors should be considered as risk factors for viral complications in the same way that other risk factors (e.g., chronic health conditions, age) are routinely considered in formulating public health policy and interventions. Importantly, these psychosocial risk factors need to be recognized not as static risks but as bidirectional and dynamic contextual factors that may influence public health policies. In the context of COVID-19, different groups of people experienced varying levels of exposure to the virus itself and susceptibility to the negative psychosocial consequences associated with mitigation efforts. This was evident among people with past or current mental health difficulties, from lower SES backgrounds, or from marginalized racial and ethnic groups. Moving forward, it is essential we acknowledge these differences and properly address these vulnerabilities. Below we discuss the potential benefits that could be achieved through psychosocial interventions implemented in tandem with (versus in place of) public policies to address structural and environmental determinants of health inequalities (e.g., paid sick and parental leave, livable wages) to achieve health equity.
Promoting Psychosocial Interventions and Tools
Interventions that reduce loneliness and manage distress while enhancing connection, positive affect, and coping could be used in tandem with established pandemic regulations (e.g., social distancing) to buffer the negative health consequences of mitigation efforts. For example, Fischer et al. (2020) synthesized over 30 meta-analyses examining interventions individuals could use during the pandemic to manage anxiety, depressive symptoms, stress, and promote well-being. Self-guided therapeutic approaches (e.g., mindfulness, cognitive-behavioral therapy), multicomponent and activity-based interventions (e.g., music, physical activity), and certain positive psychological interventions (e.g., gratitude, compassion-based) were the most effective for improving psychological health, but dose effects of these interventions were inconsistent.
Loneliness has also been identified as a useful point of intervention due to the widespread disruption of social networks caused by pandemic restrictions. Parks and Boucher (2020) conducted an 8-week randomized control trial of a digital positive psychological intervention platform on loneliness among U.S. adults. Among participants who completed more activities, those in the intervention reported significantly greater improvements in loneliness compared to those in the placebo control. Similarly, meta-analytic findings from Bertuzzi and colleagues (2021) found that psychological support interventions reduced distress and burnout among health care workers and informal caregivers while increasing their self-efficacy and well-being regardless of the type of intervention (e.g., music therapy, psychoeducation).
As the above demonstrates, numerous psychosocial interventions could be drawn upon to potentially decrease distress and improve social connectedness during future public health crises. Their use could potentially leverage the relationship between psychosocial factors with viral and vaccination outcomes to reduce individual and societal burdens from infection. However, many of these interventions have not been considered in a pandemic context or in relation to viral and vaccine outcomes. We also note the considerable potential of behavioral interventions, given behavioral factors are often closely entwined with psychosocial factors. A full discussion of behavioral interventions goes beyond the scope of the present article but we provide some brief discussion of their potential benefit in the supplemental file.3
Considering implementation, it is critical to target and codesign interventions with populations that are especially susceptible to negative health outcomes during the pandemic, including healthcare workers, individuals experiencing psychological distress due to pandemic restrictions or infection in themselves or a loved one, and individuals with existing mental health conditions that may be exacerbated by mitigation efforts or infection (Inchausti et al., 2020). Further research has identified groups at greater risk for isolation and loneliness, including those with poorer health, lower income, and who live alone (O'sullivan et al., 2021), who may benefit from intervention. As such, policymakers could follow a proportionate universalism approach whereby psychosocial interventions are delivered universally to all people during future health crises but modified in terms of intensity depending on people's needs.
Promoting Change in Public Health
There is also a pressing need to move toward a greater recognition of a biopsychosocial model of health to prepare for future health crises. This includes medical training acknowledging how the body and mind are intimately connected, that these associations are dynamic and unfold across time and development, and must be considered in the context of socioeconomic and racial inequalities in health. Simplistic models of disease that separate mind and body or that overlook the psychosocial environment are incomplete and will continue to dominate public health policies if we do not make a paradigm shift. Thus, as a research community, we need to better convey our science in a way that reaches experts in other disciplines in order to establish collaborations. This includes holding cross-disciplinary conferences, implementing interdisciplinary coursework into our training programs, and building connections with policymakers and stakeholders in government.
Moreover, it is critical for researchers to conduct methodologically rigorous research using probability-based representative samples of individuals to reinforce that psychological research should, and can be, better integrated into public health initiatives in response to future pandemics. To this end, funding lines should be created to fund studies that examine (a) efficiently delivering biopsychosocial interventions tailored toward vulnerable groups, especially during health crises, (b) keeping communities properly informed regarding pandemic regulations and illness rates by working with media outlets to improve accuracy, and (c) developing theoretical models that address emerging health crises (as opposed to relying on old models that may generalize to pandemic circumstances). Such funding could integrate different health psychology experts into teams that make major decisions during epidemics and pandemics. Having a diverse set of health knowledge and viewing health from a biopsychosocial lens will help prepare us for future threats by being proactive versus reactive in the face of future crises. Finally, and perhaps most importantly, researchers need to make our science more accessible to the public and use community-led research to inform the development and adaptation of biopsychosocial interventions. Our research is less effective if we cannot reach the populations that our interventions are intended to benefit or if we leave out the voices of the people for whom our interventions are developed.
Ultimately, the best response to health events such as the COVID-19 pandemic is one that is equally spearheaded by the public, policymakers, and scientific community. Organizations such as the World Health Organization, National Health Services, Centers for Disease Control (CDC), National Institutes of Health, and major psychological organizations (e.g., Association for Psychological Science, International Society for Behavioral Medicine, Academy of Behavioral Medicine Research) must work in tandem with state- and community-level entities to foster collaborations and develop holistic, multilevel approaches to addressing psychosocial risk factors for viral and vaccine outcomes so that we are better prepared for future health crises.
Supplemental Material
Supplemental material, sj-docx-1-bbs-10.1177_23727322221145308 for Psychology Meets Biology in COVID-19: What We Know and Why It Matters for Public Health by Emily J. Jones, Kieran Ayling, Cameron R. Wiley and Adam W.A. Geraghty, Amy L. Greer, Julianne Holt-Lunstad, Aric A. Prather, Hannah M.C. Schreier, Roxane Cohen Silver, Rodlescia S. Sneed, Anna L. Marsland, Sarah D. Pressman, Kavita Vedhara in Policy Insights from the Behavioral and Brain Sciences
Acknowledgments
This article was written as part of the Association for Psychological Sciences’ Global Collaboration on COVID-19. We want to thank Dr. Andy DeSoto, Ms. Emily Proppe, and all who contributed to the collaboration. For details of contributors please see: https://www.psychologicalscience.org/psychology-biology-covid-19.
The event recording can be viewed here: https://bit.ly/3fUmAuK
The supplemental file can be found here: https://osf.io/7yjmx/?view_only=8fd04f409d8344af8b0ad1677349794f
The supplemental file can be found here: https://osf.io/7yjmx/?view_only=8fd04f409d8344af8b0ad1677349794f
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Emily J. Jones https://orcid.org/0000-0001-8176-9185
Supplemental Material: Supplemental material for this article is available online.
References
- APA Dictionary of Psychology (2022). Retrieved 9 November 2022, fromhttps://dictionary.apa.org/
- Avitsur R., Powell N., Padgett D. A., Sheridan J. F. (2009). Social interactions, stress, and immunity. Immunology and Allergy Clinics, 29(2), 285–293. https://doi.org/10.1016/j.iac.2009.02.006 [DOI] [PubMed] [Google Scholar]
- Ayling K., Fairclough L., Tighe P., Todd I., Halliday V., Garibaldi J., Royal S., Hamed A., Buchanan H., Vedhara K. (2018). Positive mood on the day of influenza vaccination predicts vaccine effectiveness: A prospective observational cohort study. Brain, Behavior, and Immunity, 67, 314–323. 10.1016/j.bbi.2017.09.008 [DOI] [PubMed] [Google Scholar]
- Ayling K., Jia R., Coupland C., Chalder T., Massey A., Broadbent E., Vedhara K. (2022). Psychological predictors of self-reported COVID-19 outcomes: Results from a prospective cohort study. Annals of Behavioral Medicine, 56(5), 484–497. 10.1093/abm/kaab106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertuzzi V., Semonella M., Bruno D., Manna C., Edbrook-Childs J., Giusti E. M., Castelnuovo G., Pietrabissa G. (2021). Psychological support interventions for healthcare providers and informal caregivers during the COVID-19 pandemic: A systematic review of the literature. International Journal of Environmental Research and Public Health, 18(13), Article 6939. 10.3390/ijerph18136939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chekole Y. A., Abate S. M. (2021). Global prevalence and determinants of mental health disorders during the COVID-19 pandemic: A systematic review and meta-analysis. Annals of Medicine and Surgery, 68, Article 102634. 10.1016/j.amsu.2021.102634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. (2021). Psychosocial vulnerabilities to upper respiratory infectious illness: Implications for susceptibility to coronavirus disease 2019 (COVID-19). Perspectives on Psychological Science, 16(1), 161–174. 10.1177/1745691620942516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst M., Niederer D., Werner A. M., Czaja S. J., Mikton C., Ong A. D., Rosen T., Brähler E., Beutel M. E. (2022). Loneliness before and during the COVID-19 pandemic: A systematic review with meta-analysis. American Psychologist, 77(5), 660–677. https://doi.org/10.1037/amp0001005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falagas M., Karamanidou C., Kastoris A., Karlis G., Rafailidis P. (2010). Psychosocial factors and susceptibility to or outcome of acute respiratory tract infections. The International Journal of Tuberculosis and Lung Disease, 14(2), 141–148. [PubMed] [Google Scholar]
- Fischer R., Bortolini T., Karl J. A., Zilberberg M., Robinson K., Rabelo A., Gemal L., Wegerhoff D., Nguyễn T. B. T., Irving B. (2020). Rapid review and meta-meta-analysis of self-guided interventions to address anxiety, depression, and stress during COVID-19 social distancing. Frontiers in Psychology, 11, 563876. 10.3389/fpsyg.2020.563876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fond G., Nemani K., Etchecopar-Etchart D., Loundou A., Goff D. C., Lee S. W., Lancon C., Auquier P., Baumstarck K., Llorca P.-M., Yon D. K., Boyer L. (2021). Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: A systematic review and meta-analysis. JAMA Psychiatry, 78(11), 1208–1217. 10.1001/jamapsychiatry.2021.2274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher S., Howard S., Muldoon O. T., Whittaker A. C. (2022). Social cohesion and loneliness are associated with the antibody response to COVID-19 vaccination. Brain, Behavior, and Immunity, 103, 179–185. 10.1016/j.bbi.2022.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo L. C., Matthews K. A. (2003). Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin, 129(1), Article 10. 10.1037/0033-2909.129.1.10 [DOI] [PubMed] [Google Scholar]
- Hoes J., Boef A. G. C., Knol M. J., de Melker H. E., Mollema L., van der Klis F. R. M., Rots N. Y., van Baarle D. (2018). Socioeconomic status is associated with antibody levels against vaccine preventable diseases in the Netherlands. Frontiers in Public Health, 6, Article 209, 1–9. 10.3389/fpubh.2018.00209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman E., Thompson R., Garfin D., Silver R. (2020). The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Science Advances, 6(42). https://doi.10.1126/sciadv.abd5390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inchausti F., MacBeth A., Hasson-Ohayon I., Dimaggio G. (2020). Psychological intervention and COVID-19: What we know so far and what we can do. Journal of Contemporary Psychotherapy, 50(4), 243–250. 10.1007/s10879-020-09460-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser J. K., Glaser R., Gravenstein S., Malarkey W. B., Sheridan J. (1996). Chronic stress alters the immune response to influenza virus vaccine in older adults. Proceedings of the National Academy of Sciences, 93(7), 3043–3047. 10.1073/pnas.93.7.3043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy N. S., Nguyen T. Q., Westheimer E., Layton M. (2013). Disparities in the severity of influenza illness: A descriptive study of hospitalized and nonhospitalized novel H1N1 influenza–positive patients in New York city: 2009–2010 influenza season. Journal of Public Health Management and Practice, 19(1), 16–24. 10.1097/PHH.0b013e31824155a2 [DOI] [PubMed] [Google Scholar]
- Mackey K., Ayers C. K., Kondo K. K., Saha S., Advani S. M., Young S., Spencer H., Rusek M., Anderson J., Veazie S., Smith M., Kansagara D. (2021). Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths. Annals of Internal Medicine, 174(3), 362–373. 10.7326/M20-6306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamelund S.-E., Shelley-Egan C., Rogeberg O. (2021). The association between socioeconomic status and pandemic influenza: Systematic review and meta-analysis. PLOS ONE, 16(9), Article e0244346. 10.1371/journal.pone.0244346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsland A. L., Cohen S., Rabin B. S., Manuck S. B. (2006). Trait positive affect and antibody response to hepatitis B vaccination. Brain, Behavior, and Immunity, 20(3), 261–269. 10.1016/j.bbi.2005.08.009 [DOI] [PubMed] [Google Scholar]
- Marsland A. L., Pressman S., Cohen S.. (2007). Postive affect and immune function. In R. Ader (Ed.), Psychoneuroimunology (4th ed., Vol. 2, pp. 761–779). San Diego, CA: Elsevier.
- Mude W., Oguoma V. M., Nyanhanda T., Mwanri L., Njue C. (2021). Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: A systematic review and meta-analysis. Journal of Global Health, 11, 05015. 10.7189/jogh.11.05015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscatell K. A., Brosso S. N., Humphreys K. L. (2020). Socioeconomic status and inflammation: A meta-analysis. Molecular Psychiatry, 25(9), 2189–2199. 10.1038/s41380-018-0259-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Necho M., Tsehay M., Birkie M., Biset G., Tadesse E. (2021). Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. International Journal of Social Psychiatry, 67(7), 892–906. 10.1177/00207640211003121 [DOI] [PubMed] [Google Scholar]
- O’Connor D. B., Thayer J. F., Vedhara K. (2021). Stress and health: A review of psychobiological processes. Annual Review of Psychology, 72, 663–688. 10.1146/annurev-psych-062520-122331 [DOI] [PubMed] [Google Scholar]
- O’sullivan R., Burns A., Leavey G., Leroi I., Burholt V., Lubben J., Holt-Lunstad J., Victor C., Lawlor B., Vilar-Compte M. (2021). Impact of the COVID-19 pandemic on loneliness and social isolation: A multi-country study. International Journal of Environmental Research and Public Health, 18(19), Article 9982. 10.3390/ijerph18199982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradies Y., Ben J., Denson N., Elias A., Priest N., Pieterse A., Gupta A., Kelaher M., Gee G. (2015). Racism as a determinant of health: A systematic review and meta-analysis. PloS One, 10(9), Article e0138511. 10.1371/journal.pone.0138511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks A. C., Boucher E. M. (2020). Positive psychological interventions (PPIs) in the age of COVID-19: On the potential impact of digital PPIs on loneliness. The Journal of Positive Psychology, 15(5), 569–571. 10.1080/17439760.2020.1789715 [DOI] [Google Scholar]
- Pedersen A. F., Zachariae R., Bovbjerg D. H. (2009). Psychological stress and antibody response to influenza vaccination: A meta-analysis. Brain, Behavior, and Immunity, 23(4), 427–433. 10.1016/j.bbi.2009.01.004 [DOI] [PubMed] [Google Scholar]
- Pressman S. D., Cohen S., Miller G. E., Barkin A., Rabin B. S., Treanor J. J. (2005). Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychology, 24(3), Article 297. 10.1037/0278-6133.24.3.297 [DOI] [PubMed] [Google Scholar]
- Rosenblat J. D., Cha D. S., Mansur R. B., McIntyre R. S. (2014). Inflamed moods: A review of the interactions between inflammation and mood disorders. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 53, 23–34. 10.1016/j.pnpbp.2014.01.013 [DOI] [PubMed] [Google Scholar]
- Rozenfeld Y., Beam J., Maier H., Haggerson W., Boudreau K., Carlson J., Medows R. (2020). A model of disparities: Risk factors associated with COVID-19 infection. International Journal for Equity in Health, 19(1), 1–10. 10.1186/s12939-020-01242-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter P. D., Mytton O. T., Mak M., Donaldson L. J. (2012). Socio-economic disparities in mortality due to pandemic influenza in England. International Journal of Public Health, 57(4), 745–750. 10.1007/s00038-012-0337-1 [DOI] [PubMed] [Google Scholar]
- Samji H., Wu J., Ladak A., Vossen C., Stewart E., Dove N., Long D., Snell G. (2022). Mental health impacts of the COVID-19 pandemic on children and youth–a systematic review. Child and Adolescent Mental Health, 27(2), 173–189. 10.1111/camh.12501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segerstrom S. C., Miller G. E. (2004). Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychological Bulletin, 130(4), Article 601. 10.1037/0033-2909.130.4.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K. J., Gavey S., Riddell N. E., Kontari P., Victor C. (2020). The association between loneliness, social isolation and inflammation: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 112, 519–541. 10.1016/j.neubiorev.2020.02.002 [DOI] [PubMed] [Google Scholar]
- Stetler C., Chen E., Miller G. E. (2006). Written disclosure of experiences with racial discrimination and antibody response to an influenza vaccine. International Journal of Behavioral Medicine, 13(1), 60–68. 10.1207/s15327558ijbm1301_8 [DOI] [PubMed] [Google Scholar]
- Stewart R. J., Tsang C. A., Pratt R. H., Price S. F., Langer A. J. (2018). Tuberculosis—United States, 2017. Morbidity and Mortality Weekly Report, 67(11), 317–323. 10.15585/mmwr.mm6711a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J. R., Harrison P. J. (2021). Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. The Lancet Psychiatry, 8(2), 130–140. 10.1016/S2215-0366(20)30462-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R. R., Jones N. M., Freeman A. M., Holman E. A., Garfin D. R., Silver R. C. (2022). Psychological responses to US statewide restrictions and COVID-19 exposures: A longitudinal study. Health Psychology, 41(11), 817. 10.1037/hea0001233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tollefson D., Bloss E., Fanning A., Redd J., Barker K., McCray E. (2013). Burden of tuberculosis in indigenous peoples globally: A systematic review. The International Journal of Tuberculosis and Lung Disease, 17(9), 1139–1150. 10.5588/ijtld.12.0385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torrats-Espinosa G. (2021). Using machine learning to estimate the effect of racial segregation on COVID-19 mortality in the United States. Proceedings of the National Academy of Sciences, 118(7), Article e2015577118. 10.1073/pnas.2015577118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino B., Trettevik R., Kent de Grey R., Cronan S., Hogan J., Baucom B. (2018). Social support, social integration, and inflammatory cytokines: A meta-analysis. Health Psychology, 37(5), 462–471. 10.1037/hea0000594 [DOI] [PubMed] [Google Scholar]
- Uchino B. N., Landvatter J., Zee K., Bolger N. (2020). Social support and antibody responses to vaccination: A meta-analysis. Annals of Behavioral Medicine, 54(8), 567–574. 10.1093/abm/kaaa029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vedhara K., Ayling K., Jia R., Fairclough L., Morling J. R., Ball J. K., Knight H., Blake H., Corner J., Denning C., Bolton K., Jackson H., Coupland C., Tighe P. (2022). Relationship between anxiety, depression, and susceptibility to severe acute respiratory syndrome coronavirus 2 infection: Proof of concept. The Journal of Infectious Diseases, 225(12), 2137–2141. 10.1093/infdis/jiac006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vedhara K., Ayling K., Sunger K., Caldwell D. M., Halliday V., Fairclough L., Avery A., Robles L., Garibaldi J., Welton N. J. (2019). Psychological interventions as vaccine adjuvants: A systematic review. Vaccine, 37(25), 3255–3266. 10.1016/j.vaccine.2019.04.091 [DOI] [PubMed] [Google Scholar]
- Vedhara K., Cox N. K., Wilcock G. K., Perks P., Hunt M., Anderson S., Lightman S. L., Shanks N. M. (1999). Chronic stress in elderly carers of dementia patients and antibody response to influenza vaccination. The Lancet, 353(9153), 627–631. 10.1016/S0140-6736(98)06098-X [DOI] [PubMed] [Google Scholar]
- Wachtler B., Michalski N., Nowossadeck E., Diercke M., Wahrendorf M., Santos-Hövener C., Lampert T., Hoebel J. (2020). Socioeconomic inequalities and COVID-19 – A review of the current international literature. Journal of Health Monitoring, 5(Suppl. 7), 3–17. 10.25646/7059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiley C. R., Blevins K. M., Cohen S., Pressman S. D. (2022). Do positive psychological factors equally predict resistance to upper respiratory infections in African and European Americans? Psychological Science, 33(9), 1509–1521. 10.1177/09567976221083322 [DOI] [PubMed] [Google Scholar]
- Williams D. P., Jones N. M., Holman E. A. (2022). Racial and ethnic differences in perseverative cognition at the onset of the COVID-19 pandemic. Social Science & Medicine, 306, 115105. 10.1016/j.socscimed.2022.115105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2017). Depression and other common mental disorders: Global health estimates. World Health Organization. [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L. M., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H., Chen W., Hu Y., Chen Y., Zeng Y., Sun Y., Ying Z., He J., Qu Y., Lu D. (2020). Pre-pandemic psychiatric disorders and risk of COVID-19: A UK Biobank cohort analysis. The Lancet Healthy Longevity, 1(2), e69–e79. 10.1016/S2666-7568(20)30013-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorrilla E. P., Luborsky L., McKay J. R., Rosenthal R., Houldin A., Tax A., McCorkle R., Seligman D. A., Schmidt K. (2001). The relationship of depression and stressors to immunological assays: A meta-analytic review. Brain, Behavior, and Immunity, 15(3), 199–226. 10.1006/brbi.2000.0597 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-bbs-10.1177_23727322221145308 for Psychology Meets Biology in COVID-19: What We Know and Why It Matters for Public Health by Emily J. Jones, Kieran Ayling, Cameron R. Wiley and Adam W.A. Geraghty, Amy L. Greer, Julianne Holt-Lunstad, Aric A. Prather, Hannah M.C. Schreier, Roxane Cohen Silver, Rodlescia S. Sneed, Anna L. Marsland, Sarah D. Pressman, Kavita Vedhara in Policy Insights from the Behavioral and Brain Sciences