Abstract
Background
In the aftermath of the COVID-19 pandemic, medical students and residents in the U.S. and globally have gained more exposure to teledermatology, both for the purposes of clinical practice and education.
Objective
We conducted a systematic review to assess outcomes from teledermatology interventions for dermatology trainees in the U.S. and globally in accordance with Preferred Reporting Items for Systematic Reviews (PRISMA).
Methods
We searched MEDLINE, EMBASE, Web of Science, and Cochrane CENTRAL for articles written in English and published database inception to November 20, 2022.
Results
In total, 15 studies met the inclusion criteria. Outcomes reported ranged broadly from resident-provider concordance rates, diagnostic accuracy in comparison to control groups, number of patients seen, and self-reported satisfaction and improvement. Generally, studies indicated high satisfaction rates and improvement in educational outcomes among medical students, residents, and other trainees in the global health setting.
Limitations
Because of the heterogeneity of study design and outcomes reported, meta-analysis could not be performed.
Conclusion
Teledermatology can be successfully deployed for clinical care and education domestically and in the global health setting.
Key words: global health, international dermatology education, teledermatology, virtual curriculum
Capsule Summary.
-
•
Our systematic review of teledermatology interventions for dermatology trainees in the United States and globally shows high rates of satisfaction, improvement, and concordance.
-
•
Global teledermatology education is a promising area for furthering virtual training as an effective and cost-efficient option for trainees.
Introduction
In the aftermath of the COVID-19 pandemic, medical students and trainees have gained more exposure to teledermatology, both for the purposes of clinical practice and education. Medical students rarely receive adequate dermatology experience in core rotations or during preclinical years. When 0.3% of medical schools’ curricula are dedicated to dermatology,1 it follows that many students report unfamiliarity with managing basic dermatologic conditions.2 Given that >35% of patients reporting to primary care providers have dermatologic complaints, there is a need for new modalities for dermatologic education.3,4
In the case of residents, teledermatology was a means to sustain education during the COVID-19 pandemic. While a majority of programs have adopted a predominantly online didactic curriculum, the literature indicates mixed reviews on the effectiveness of online curricula in comparison to live, in-person teaching.5 Furthermore, several programs have introduced resident-led teledermatology clinics and multi-provider visits, wherein both resident and attending interface with patients from remote areas to formulate assessments and plans for treatment.6,7 Surveys indicate that residents are generally interested in teledermatology education but are usually limited by a lack of resources or experience. Residency programs have expressed interest and indicated that telemedicine would be helpful in evaluating residents.8,9
The need for teledermatology in education is perhaps most acute in the setting of global health, where surveys indicate that research efforts and funding are severely lacking in comparison to the burden of skin disease. Designing scalable teledermatological interventions could prove to be rewarding in addressing the need to provide dermatological care to underserved regions in a cost-effective manner.10,11 In this systematic review, we assess outcomes from teledermatology interventions for dermatology trainees in the United States and globally.
Methods
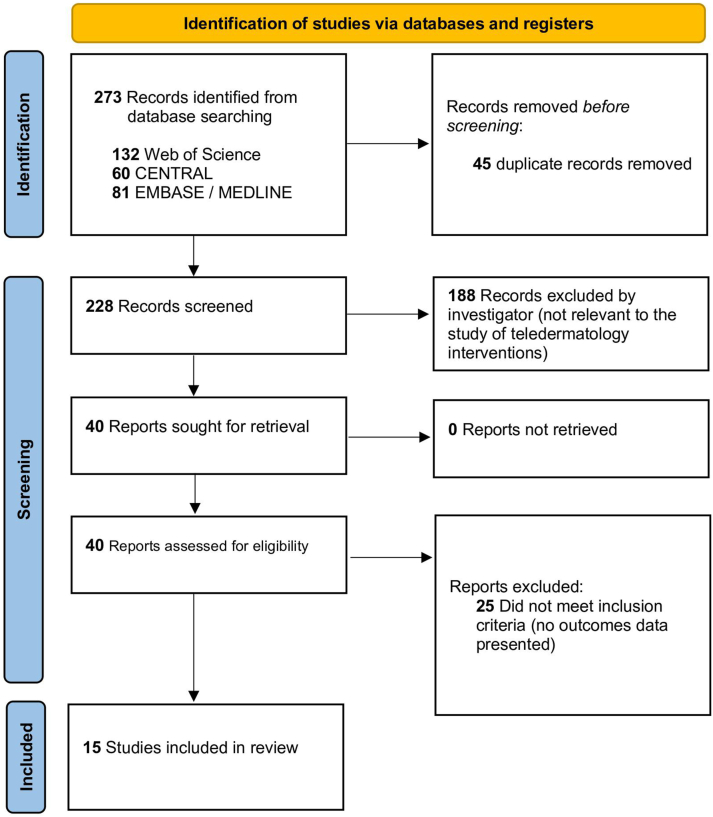
We registered our study protocol with the International Prospective Register of Systematic Reviews. We developed search queries (supplement, available via Mendeley at https://doi.org/10.17632/6j85rx62pm.2) specific to Ovid MEDLINE, Ovid EMBASE, Web of Science, and Cochrane CENTRAL databases for all articles written in English and published from database inception to November 30, 2022. We included all articles that discussed quantitative or self-reported outcomes from teledermatology interventions. We excluded all articles that lacked relevance or did not discuss outcomes data. References of all articles deemed eligible were screened for additional relevant articles (Fig 1).
Fig 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for systematic review.
We extracted the following data from the included studies: mode of intervention, target audience, names of institutions involved, number of trainees involved, names of countries involved, and outcomes data provided (ie, resident-provider concordance rates, diagnostic accuracy in comparison to control groups, number of patients seen, and self-reported satisfaction and improvement). Two authors (R.R.R. and H.A.P) independently evaluated articles for selection and performed data extraction. Disagreements were reviewed by the third independent author, B.K.S. All included studies were subject to methodological quality analysis per Joanna Briggs Institute critical appraisal checklist for cross-sectional studies (supplemental table 1 available via Mendeley at https://doi.org/10.17632/6j85rx62pm.2). This systematic review was conducted per the guidelines prescribed by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (supplement, available via Mendeley at https://doi.org/10.17632/6j85rx62pm.2).
Results
Our systematic review synthesizes findings from 15 studies. Among all studies, 8 discussed teledermatology intervention in resident education, 4 in medical education, and 5 in the global health setting.
Teledermatology in resident education
For interventions targeting resident education, outcomes ranged broadly from resident-provider concordance rates, diagnostic accuracy compared with control groups, number of patients seen, and self-reported satisfaction and improvement.
Evaluating residents by measuring resident-provider concordance rates is a common educational outcome metric, with 3 studies reporting this outcome. In one study, 7 dermatology residents participated in 280 eConsults, reviewed by the dermatology faculty at the University of Miami Miller School of Medicine. Faculty overall and partial agreement with resident responses increased over time for the resident treatment plan (P =.02).9 In another study conducted among residents (n = 9) at the University of Pennsylvania, the resident-investigator concordance rate was 53% for diagnosis and 65% for management plans. However, diagnosis and management plans were concordant for 92% and 89% of cases, respectively, between investigators.10 Another study assessing concordance involved trainees at an urgent care clinic in NYC taking consults and reviewing cases with offsite attending physicians through teledermatology. The number of residents was unspecified; however, overall concordance was found to be high at 96%.11
This particular study, and several others, also indicated self-reported satisfaction levels of residents after participation in teledermatology. Residents reported low satisfaction levels (4/10) despite indicating ease of use (4/10, with 10 being very difficult to use).12 Notably, the attending satisfaction rates were high. Another teledermatology consultation service involving 44 trainees (31 residents and 13 medical students) covered 50 consultations. Although survey data did not distinguish between residents and medical students, trainees overall reported significant improvement (22%, P < 0.002) in competency and high levels of satisfaction [86%-88% of trainees were very satisfied and expressed intent to apply teledermatology in future practice (≥5 on a 7-point scale)].13 Another study that evaluated both resident and medical student perceptions of teledermatology after a similar implementation grouped results by resident vs. medical student. Both groups reported high satisfaction levels, with 79% of residents (n = 14), strongly agreeing or agreeing.
Some studies used various metrics to assess improvement in diagnostic accuracy with teledermatology. When residents (n = 31) were randomized to receiving teledermatology cases with still images only vs still images + video (mixed), residents in the mixed group scored significantly higher on management accuracy (87.6 ± 12.9 vs 71.7 ± 14.2; P =.003).14 These findings are consistent with that of another uncontrolled study, where 91% of residents (n = 11) reported that eConsult-based training enhanced their education and should be a permanent fixture in the curriculum.15
The most recent study reported on the incorporation of teledermatology in the residency program at the University of California, San Francisco School of Medicine. Residents (n = 15) shared narrative feedback through post-participation surveys. As such, 9 out of 15 narratives indicated that teledermatology enabled residents to evaluate more patient cases vs in-person clinics. Similarly, 8 of 15 narratives mentioned teledermatology provided a low-stress learning environment.16
Teledermatology in medical student education
For interventions targeting medical student education, outcomes ranged broadly, including self-reported satisfaction rates, self-improvement rates, and the ability for clinics to provide greater access to skin care for underrepresented populations.
In the aforementioned article by Shaikh et al10 assessing a teledermatology consultation service involving 44 trainees (31 residents and 13 medical students), trainees reported high levels of improvement (88%) and satisfaction (86%), although this outcome did not differentiate medical students from residents. The study by Boyer et al13 referenced above in the context of resident education reported on a similar intervention and assessed medical student perceptions independently. Both groups reported high levels of satisfaction, with 88% of medical students strongly agreeing or agreeing.
The COVID-19 pandemic allowed medical students to engage with teledermatology in new ways, as demonstrated by a virtual pediatric dermatology student-run clinic in Boston, Massachusetts. Medical students (n = 5) were involved with scheduling patients for virtual appointments and taking patient histories, while residents and attendings formulated assessments and plans for patient care during virtual visits. Patient no-show rates at the virtual student-run clinic (37 patients), predominantly those with skin of color, were 9.8% compared with 30% at the internal dermatology department.17 With the advent of virtual reality (VR) in dermatology education, 14 individuals were invited to engage in a VR memory palace for dermatology education. Participants included medical students (n = 5) and dermatology residents and fellows. Self-reported satisfaction (86%) and ease of access (79%) and use (93%) were generally high, although these data included medical students (n = 5) as part of the overall population (n = 14).18
Teledermatology in global dermatology education
Due to the heterogeneity and relative paucity of data on the use of teledermatology for global health education, developing a generalized list of outcomes is highly challenging and ultimately impractical. However, each study that presented outcomes was assessed independently.
A total of 1229 teleconsultations were reviewed from points of origin in 13 Sub-Saharan African nations by United States dermatology institutions spearheading the African Teledermatology Project. Clinicians submitting from Africa presented diagnoses in 63% of cases and a list of differential diagnoses in 30% of cases. Clinicians reviewing cases in the United States agreed with the diagnoses in 60% of cases.19
A virtual grand rounds pilot curriculum was created by the Emory Department of Dermatology based on teledermatology cases from Kabul, Afghanistan, which were also supervised by Emory faculty. A postprogram survey was administered to dermatology faculty, residents, and medical students in attendance to assess the curriculum’s effectiveness. Responses (n = 85) indicated that the curriculum was a valuable educational tool for learning more about the diagnosis and treatment of skin diseases in the international setting.20
Emory Dermatology faculty also developed a free, online dermatology course completed by 104 trainees from the University of Gondar, Ethiopia. Compared to historical controls (n = 236), the cohort (n = 104) averaged > 4 points higher on a standardized board examination (P <.0001). Most participants were satisfied with all aspects of the course and desired components of virtual learning in future training.21 In a follow-up qualitative analysis study, common themes underlying positive feedback included: “adequate coverage of core dermatological concepts” (41, 18%), “convenience of self-pacing,” (30, 13%), and “greater accessibility due to virtual format” (19, 8%); and most common negative feedback stemmed from “lack of adequate clinical images” (29, 13%), “lack of compatibility with local network connectivity” (23, 10%), “minimally interactive course” (15, 7%), and “difficulties navigating the registration process” (15, 7%).22
Most recently, the Global Dermatology Talks series was launched to address the needs in dermatology education through supplementing in-person academic and research training. The survey was distributed using Qualtrics to viewers from the United States, India, Japan, Mexico, United Kingdom, Nigeria, Vietnam, Saudi Arabia, Israel, and Taiwan, and responses (n = 39) reported on the following: 80% of participants strongly agreed that the subject matter was interesting and appropriate. Additionally, 85% strongly agreed that it was more cost-effective than live, in-person programming. Limitations to this analysis include the absence of non-responder rates, as countries with less access to social media may be less likely to respond. Furthermore, it was not possible to determine the percentage of viewers representing learners as opposed to practitioners.23
Discussion
Given the growing interest of residency programs to implement teledermatology in the clinical setting, the outcomes we found indicate generally high levels of satisfaction and usefulness among residents.24 Additionally, we found that resident-investigator concordance rates tend to vary. This discrepancy could be interpreted in several ways. Studies that indicate high concordance rates provide evidence for the validity of teledermatology as comparable to standard in-person patient visits.7, 8, 9 Studies that present low rates of concordance indicate the need for more resident exposure to teledermatology. Future studies should also assess resident productivity in teledermatology clinics as compared to in-person clinics to validate the findings presented by Zakaria et al.16
While data on outcomes for teledermatology interventions are relatively limited in medical student education, early data appear to be promising. Given that the target audience may be more technologically inclined and receptive to the implementation of new technologies, the opportunity exists to expand effective virtual dermatological teaching instruments, such as through VR.
Perhaps the area of greatest potential for teledermatology education is the global setting. Scalable teledermatological interventions, such as those designed by Yeung et al20 and Revankar et al21,22, may help to address the growing burden of skin disease in areas where research efforts and funding are severely lacking.
Conclusion
Our study is limited, primarily due to the heterogeneity of study design and outcomes reported. Therefore, we were not able to conduct a meta-analysis. However, this review is unique because it systematically analyzes the outcomes of teledermatological interventions in the education of medical students, residents, and other dermatology trainees globally.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Loh T.Y., Hsiao J.L., Shi V.Y. COVID-19 and its effect on medical student education in dermatology. J Am Acad Dermatol. 2020;83(2):e163–e164. doi: 10.1016/j.jaad.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nguyen Q.D., Starling C.T., Baig I.T., Koshelev M.V., Nelson K.C. Online dermatology curriculum experiences among US dermatology residents and faculty. Clin Dermatol. 2022;40(6):788–791. doi: 10.1016/j.clindermatol.2022.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oldenburg R., Marsch A. Optimizing teledermatology visits for dermatology resident education during the COVID-19 pandemic. J Am Acad Dermatol. 2020;82(6):e229. doi: 10.1016/j.jaad.2020.03.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lam M., Doiron P.R. The use of teledermatology in medical education. Med Sci Educ. 2021;32(1):243–246. doi: 10.1007/s40670-021-01465-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wanat K.A., Newman S., Finney K.M., Kovarik C.L., Lee I. Teledermatology education: Current use of teledermatology in US residency programs. J Grad Med Educ. 2016;8(2):286–287. doi: 10.4300/JGME-D-16-00041.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clarke E.L., Boothe W.D., Jambusaria-Pahlajani A., Sebastian K., Diaz L.Z., Ahmed A.M. Assessment of teledermatology education during residency training: a nationwide survey of residents and program directors. Dermatol Online J. 2021;27(4) 13030/qt3vx945t9. [PubMed] [Google Scholar]
- 7.Seth D., Cheldize K., Brown D., Freeman E.F. Global burden of skin disease: Inequities and innovations. Curr Dermatol Rep. 2017;6(3):204–210. doi: 10.1007/s13671-017-0192-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kantor J. Scalable global dermatology education. JAAD Int. 2022;6:143. doi: 10.1016/j.jdin.2022.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scheinfeld N. The use of teledermatology to supervise dermatology residents. J Am Acad Dermatol. 2005;52(2):378–380. doi: 10.1016/j.jaad.2004.07.050. [DOI] [PubMed] [Google Scholar]
- 10.Shaikh N., Lehmann C.U., Kaleida P.H., Cohen B.A. Efficacy and feasibility of teledermatology for paediatric medical education. J Telemed Telecare. 2008;14(4):204–207. doi: 10.1258/jtt.2008.071108. [DOI] [PubMed] [Google Scholar]
- 11.Camacho I., Perez O., Berman B., Burdick A. Jackson memorial hospital resident teledermatology training. J Am Acad Dermatol. 2008;58:AB76. [Google Scholar]
- 12.Nelson C., Wanat K., Roth R., James W., Kovarik C., Takeshita J. Teledermatology as pedagogy: diagnostic and management concordance between resident and attending dermatologists. J Am Acad Dermatol. 2015;72:555–557. doi: 10.1016/j.jaad.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boyers L.N., Schultz A., Baceviciene R., et al. Teledermatology as an educational tool for teaching dermatology to residents and medical students. Telemed J E Health. 2015;21(4):312–314. doi: 10.1089/tmj.2014.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feigenbaum D.F., Boscardin C.K., Frieden I.J., Mathes E.F.D. Can you see me now? video supplementation for pediatric teledermatology cases. Pediatr Dermatol. 2017;34(5):566–571. doi: 10.1111/pde.13210. [DOI] [PubMed] [Google Scholar]
- 15.Mahmood F., Cyr J., Keely E., et al. Teledermatology utilization and integration in residency training over the COVID-19 pandemic. J Cutan Med Surg. 2022;26(2):135–142. doi: 10.1177/12034754211045393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zakaria A., Maurer T., Amerson E. Impact of teledermatology program on dermatology resident experience and education. Telemed J E Health. 2021;27(9):1062–1067. doi: 10.1089/tmj.2020.0350. [DOI] [PubMed] [Google Scholar]
- 17.Linggonegoro D., Rrapi R., Ashrafzadeh S., et al. Continuing patient care to underserved communities and medical education during the COVID-19 pandemic through a teledermatology student-run clinic. Pediatr Dermatol. 2021;38(4):977–979. doi: 10.1111/pde.14653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ranpariya V.K., Huang W.W., Feldman S.R. Virtual reality memory palace: An innovative dermatology education modality. J Am Acad Dermatol. 2022;86(6):1435–1437. doi: 10.1016/j.jaad.2021.06.859. [DOI] [PubMed] [Google Scholar]
- 19.Lipoff J.B., Cobos G., Kaddu S., Kovarik C.L. The Africa Teledermatology Project: A retrospective case review of 1229 consultations from sub-Saharan Africa. J Am Acad Dermatol. 2015;72(6):1084–1085. doi: 10.1016/j.jaad.2015.02.1119. [DOI] [PubMed] [Google Scholar]
- 20.Yeung H., Sargen M.R., Luk K.M., et al. Teledermatology and teledermatopathology as educational tools for international dermatology: a virtual grand rounds pilot curriculum. Int J Dermatol. 2018;57(11):1358–1362. doi: 10.1111/ijd.14014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Revankar R., Bilcha K., Befekadu A., Yeung H., Stoff B. Free online dermatology course for medical trainees in Ethiopia: A pilot study. JAAD Int. 2021;6:20–26. doi: 10.1016/j.jdin.2021.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Revankar R., Sood A., Patel H., et al. Developing a virtual global dermatology curriculum: Qualitative analysis based on a pilot study in Ethiopia. JAAD Int. 2022;10:41–43. doi: 10.1016/j.jdin.2022.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ederaine S.A., Kimball K.M., Enwereji N., et al. Global dermatology talks is a virtual lecture series for equitable dissemination of dermatologic information. JAAD Int. 2022;9:116–118. doi: 10.1016/j.jdin.2022.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song E., Amerson E., Twigg A.R. Teledermatology in medical and continuing education. Curr Derm Rep. 2020;9:136–140. [Google Scholar]