This time-series analysis assesses the association of implementation of postoverdose outreach programs with opioid fatality rates in Massachusetts municipalities with high numbers of opioid-related medical emergency services responses.
Key Points
Question
Among Massachusetts municipalities with high numbers of opioid-related medical emergency services responses, was implementation of postoverdose outreach programs associated with reductions in fatal opioid overdoses?
Findings
In this multisite interrupted time-series analysis of 93 Massachusetts municipalities, implementation of postoverdose outreach programs was significantly associated with lower opioid fatality rates over time compared with municipalities that did not implement such programs.
Meaning
In this study, among Massachusetts municipalities with high numbers of opioid-related emergency services responses, implementation of postoverdose outreach programs was significantly associated with lower opioid fatality rates over time.
Abstract
Importance
Nonfatal opioid overdose is the leading risk factor for subsequent fatal overdose and represents a critical opportunity to reduce future overdose and mortality. Postoverdose outreach programs emerged in Massachusetts beginning in 2013 with the main purpose of linking opioid overdose survivors to addiction treatment and harm reduction services.
Objective
To evaluate whether the implementation of postoverdose outreach programs among Massachusetts municipalities was associated with lower opioid fatality rates compared with municipalities without postoverdose outreach programs.
Design, Setting, and Participants
This retrospective interrupted time-series analysis was performed over 26 quarters (from January 1, 2013, through June 30, 2019) across 93 municipalities in Massachusetts. These 93 municipalities were selected based on a threshold of 30 or more opioid-related emergency medical services (EMS) responses in 2015. Data were analyzed from November 2021 to August 2022.
Exposures
The main exposure was municipality postoverdose outreach programs. Municipalities had various program inceptions during the study period.
Main Outcomes and Measures
The primary outcome was quarterly municipal opioid fatality rate per 100 000 population. The secondary outcome was quarterly municipal opioid-related EMS response (ambulance trips) rates per 100 000 population.
Results
The mean (SD) population size across 93 municipalities was 47 622 (70 307), the mean (SD) proportion of female individuals was 51.5% (1.5%) and male individuals was 48.5% (1.5%), and the mean (SD) age proportions were 29.7% (4.0%) younger than 25 years, 26.0% (4.8%) aged 25 to 44 years, 14.8% (2.1%) aged 45 to 54 years, 13.4% (2.1%) aged 55 to 64 years, and 16.1% (4.4%) aged 65 years or older. Postoverdose programs were implemented in 58 municipalities (62%). Following implementation, there were no significant level changes in opioid fatality rate (adjusted rate ratio [aRR], 1.07; 95% CI, 0.96-1.19; P = .20). However, there was a significant slope decrease in opioid fatality rate (annualized aRR, 0.94; 95% CI, 0.90-0.98; P = .003) compared with the municipalities without the outreach programs. Similarly, there was a significant slope decrease in opioid-related EMS response rates (annualized aRR, 0.93; 95% CI, 0.89-0.98; P = .007). Several sensitivity analyses yielded similar findings.
Conclusions and Relevance
In this study, among Massachusetts municipalities with high numbers of opioid-related EMS responses, implementation of postoverdose outreach programs was significantly associated with lower opioid fatality rates over time compared with municipalities that did not implement such programs. Program components, including cross-sectoral partnerships, operational best practices, involvement of law enforcement, and related program costs, warrant further evaluation to enhance effectiveness.
Introduction
Deaths from opioid overdose exceeded 500 000 in the US from 1999 to 2018.1 In the 12 months ending in April 2021, there were 75 673 opioid deaths, mostly associated with fentanyl’s presence in the illicit drug supply.2 The burden of opioid use disorder (OUD) had increasingly disproportionate effects on racially and economically marginalized groups.3
Efforts to address opioid overdose included expanded access to naloxone, such as community, pharmacy, and coprescribing overdose education and naloxone distribution (OEND) programs4,5,6,7; expansion of prescription drug monitoring programs8; expansion of access to medications for OUD9; passing 911 Good Samaritan laws10; and for several states, declaring public health emergencies.11 A cohort study using data from the 2014 Massachusetts All-Payer Claims Database showed that nonfatal opioid overdose was associated with subsequent fatal overdose,12 which highlighted the importance of engaging overdose survivors to seek OEND or medications for OUD.
Postoverdose outreach programs emerged as an approach for engaging recent opioid overdose survivors. Outreach programs, typically organized among municipalities, deployed teams composed of public health and public safety staff.13 These teams used contact information from emergency responses to outreach to survivors and/or their social networks. Programs focused on linkage to treatment for OUD and offered harm reduction services to survivors and their network.14
In Massachusetts, municipalities began implementing postoverdose outreach programs in 2013.15 Despite their proliferation, postoverdose programs have not been rigorously evaluated. Because it would take time to initiate these programs and conduct outreach activities, we hypothesized that the implementation of these programs would not be associated with an immediate change in overdose rates but that outreach programs would be associated with a gradual decline in overdose rates over time.
Methods
Study Design and Setting
The study was reviewed and designated as not human participant research by the institutional review board of the Boston University Medical Center and the Massachusetts Department of Public Health, and informed consent was waived for this reason. We conducted a multisite interrupted time-series analysis of quarterly municipal opioid-related fatality rates and emergency response rates from January 1, 2013, through June 30, 2019. This study followed the Transparent Reporting of Evaluations With Nonrandomized Designs (TREND) reporting guideline.
Data Collection
Outreach program establishment data were collected from a 2-phase survey conducted between February and November 2019 in all 351 municipalities in Massachusetts.15 Survey methods and characteristics of these programs were described in previous publications.15,16
Exposure
Of the 93 municipalities with at least 30 opioid emergency responses in 2015, the phase 1 screener survey identified 65 municipalities with overdose outreach programs. The inceptions of outreach programs were determined based on the question, “When did your organization’s postoverdose outreach program begin? [Enter date as mm/dd/yyyy.]” Because 7 municipalities did not provide information on program inception, we coded these 7 municipalities as not having an outreach program. We conducted a sensitivity analysis by removing these municipalities from the analysis.
Outcomes
The primary outcome was the quarterly fatal opioid overdose rate. We calculated municipal-specific rates per 100 000 residents of opioid-related drug poisoning deaths (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10] codes X40-X44, Y10-Y14) and an opioid specific T40.0 to T40.4 and/or narcotic T40.6 in any of the multiple cause-of-death fields.4
The secondary outcome was the quarterly municipal-specific opioid emergency medical service (EMS) response rate. We used the Massachusetts Ambulance Trip Record Information System17 to calculate the opioid emergency response rate per 100 000 residents. Full-year data by quarters were available beginning in 2014. Opioid EMS responses were based on trips with notation for poisoning, administration of naloxone, or patient self-reported opioid use.17
Covariates
We obtained demographic data from the American Community Survey,18 including population size, age group proportions (<25, 25-44, 45-54, 55-64, and ≥65 years), sex, race and ethnicity (African American/Black, American Indian/Alaska Native, Asian, Hispanic/Latinx, Pacific Islander, White, and other, which included multiracial and other groups), high school education or less, and housing vacancy rates. Because the prevalence of OUD varied across racial and ethnic groups, we followed a prior approach and used racial and ethnic proportions data with fixed categories defined by the American Community Survey for the adjusted analyses.4 Vacancy rate was measured by vacant housing units per 1000 population, which was a marker of neighborhood distress.19 We obtained from Massachusetts Department of Public Health the number of naloxone kits distributed to the communities by state-funded OEND programs. To describe and adjust for the level of addiction treatment, we obtained quarterly methadone treatment admission rates and residential treatment admission rates from the Massachusetts Bureau of Substance Addiction Services.4 The Massachusetts Prescription Monitoring Program provided patient rates of buprenorphine prescriptions indicative of OUD treatment. These covariates were assessed in prior studies on opioid use.4,20,21 Given the public safety involvement, we obtained municipal-level indicators of whether public safety personnel were equipped with naloxone and whether there was a municipal drug court or jail diversion program. To account for drug-related law enforcement, we obtained community release rates from the Massachusetts Department of Correction and community drug arrest rates (eg, code Drug/Narcotic Violations-35A).22 We used an indicator variable to account for the community-level presence of Massachusetts Opioid Abuse Prevention Collaborative coalitions. In addition, because fentanyl in the illicit drug supply was associated with surging overdose deaths, we used the community-specific proportion of fentanyl-involved deaths among all opioid deaths as a proxy measure to control for fentanyl-related burden among these municipalities.23
Sample Size Calculation and Precision
Massachusetts consists of 351 distinct municipalities. For sample size calculation and related precision for estimates, we compared the annual rate change of opioid emergency responses between 2015 and 2016 and used the rate difference between municipalities with outreach programs and those without programs, accounting for the baseline rate in 2015. To have at least 80% statistical power, we included the 93 municipalities with at least 30 opioid emergency responses in 2015.
Statistical Analysis
Data were analyzed from November 2021 to August 2022. Similar to prior research,4 we used Poisson regression models with overdispersion adjustment through a scale parameter to model rates at municipality (i) in quarter (t) with a log-linear model as the primary approach. We used the segmented regression analysis approach24 and included multiple time series with a generalized estimation equations approach25 to examine the target parameters of interest, level change (β2) and slope change (β3), assuming the preimplementation trend remained unchanged. Level changes were immediate changes in the outcome after program implementation, and slope changes were changes in the trend of outcome after program implementation.
| log (Yit) = β0 + β1 Time + β2 Programit + β3 Time After Programit + BXit + eit |
We included the nonimplementing municipalities as additional control series to account for potential confounding due to statewide concurrent events including secular trend and potential regression to the mean effect due to sample selection. We assessed the assumptions of baseline equivalence of the levels and slopes between the nonimplementing control series and the preimplementation series among the implementing municipalities. We used quasi-likelihood information criteria to assess goodness of fit and determine the covariance structure of the repeated measures.26 We exponentiated the annualized β3 to obtain rate ratios (RRs) to represent the relative slope change per year for the postimplementation period. In addition, as a secondary modeling approach, we used an identity link function with normal distribution to estimate baseline rates and absolute rate differences to facilitate interpretation of the magnitude of the association in additive scale. For modeling sequence, we followed 3 related modeling steps: (1) the base (unadjusted) model, which evaluated the changes without accounting for covariates; (2) adjusted model 1, which served as the main model and evaluated the changes accounting for a variety of municipality-level characteristics; and (3) adjusted model 2, which served as an a priori sensitivity analysis and further accounted for municipalities as fixed effects. Because quarterly aggregates of municipality-level data were used, there were no missing data.
We conducted 2 a priori sensitivity analyses. First, to ascertain whether the findings were confounded by unmeasured health system effects, we refit the adjusted Poisson fatal overdose models, replacing fatal death rates with opioid death–to–cancer death RRs for each community-quarter.4 We used codes representing malignant neoplasms (ICD-10 codes C000-C979) to define cancer deaths. Cancer death rate served as a positive control of the underlying health system change over the study period; therefore, a significant association with the opioid-to-cancer death RR outcome would suggest that opioid deaths were associated with the outreach programs after accounting for the underlying health system changes. Second, we added community-level fixed effects (as dummy variables) to control for unmeasured community-level confounders.27,28 Third, we conducted a post hoc sensitivity analysis removing OEND and addiction treatment variables (eg, naloxone kit rate by OEND program, methadone admission rate, residential admission rate, and patient rate of buprenorphine prescription for OUD) that were potential mediators. Fourth, we performed another post hoc sensitivity analysis using an indicator to code the last quarter of 2018 and after to further account for the statewide pharmacy naloxone standing order mandate effective in October 2018.29 In addition, we conducted a post hoc analysis removing the 7 municipalities lacking program inception information. All tests used a 2-sided significance level of 0.05. All analyses were conducted using SAS, version 9.4 (SAS Institute Inc).
Results
The 93 Massachusetts communities accounted for 66% of the state’s population and contributed 78% (8673 of 11 111) of the fatal opioid overdoses over the study period. Outreach programs were implemented in 58 municipalities (62%) by the second quarter of 2019. The implementation of outreach programs over the study period was mapped with the opioid fatality rates and the EMS response rates (eFigures 1 and 2 in Supplement 1) across these 93 municipalities. Twenty-eight municipalities did not implement outreach programs, and 7 lacked information on program inception. The mean (SD) population size across 93 municipalities was 47 622 (70 307), the mean (SD) proportion of female individuals was 51.5% (1.5%) and male individuals was 48.5% (1.5%), and the mean (SD) age proportions were 29.7% (4.0%) younger than 25 years, 26.0% (4.8%) aged 25 to 44 years, 14.8% (2.1%) aged 45 to 54 years, 13.4% (2.1%) aged 55 to 64 years, and 16.1% (4.4%) aged 65 years or older. The mean (SD) proportion for each race and ethnicity group was 5.3% (7.0%) African American/Black, 0.2% (0.4%) American Indian/Alaska Native, 4.7% (5.1%) Asian, 10.1% (12.9%) Hispanic/Latinx, 0.02% (0.1%) Pacific Islander, 83.0% (13.3%) White, and 6.8% (7.2%) other race and ethnicity. There were no significant differences among all characteristics and outcomes at baseline between municipalities that eventually established a program and those that did not (Table 1) except for the methadone admission rate being higher among municipalities without an outreach program compared with municipalities with an outreach program (mean [SD], 0.51 [0.42] vs 0.34 [0.27] per 1000 population; P = .02). In the second quarter of 2019, opioid EMS response rates were significantly lower in municipalities with outreach programs compared with those without outreach programs (mean [SD], 79.9 [59.6] vs 109.7 [62.2] per 100 000 population; P = .02) (Table 1). Over the study period, the mean (SD) quarterly opioid EMS response rate was 87.1 (61.5) episodes per 100 000 population.
Table 1. Comparison of Characteristics of 93 Municipalities in Massachusetts in the First Quarter of 2013 and the Second Quarter of 2019a.
| Characteristic | First quarter of 2013b | Second quarter of 2019 | ||||
|---|---|---|---|---|---|---|
| Mean (SD) | P value | Mean (SD) | P value | |||
| Municipalities that eventually developed program (n = 58) | Municipalities that did not develop program (n = 35) | Municipalities that developed program (n = 58) | Municipalities that did not develop program (n = 35) | |||
| Quarterly opioid fatality rate, per 100 000 population | 4.6 (4.8) | 3.7 (3.4) | .36 | 7.4 (6.0) | 7.9 (5.0) | .70 |
| Quarterly opioid EMS response rate, per 100 000 populationc | 45.0 (34.8) | 56.5 (52.8) | .21 | 79.9 (59.6) | 109.7 (62.2) | .02 |
| Age, % | ||||||
| <25 y | 30.1 (4.2) | 30.7 (3.6) | .46 | 28.8 (4.2) | 29.2 (3.3) | .58 |
| 25-44 y | 26.1 (5.2) | 26.6 (3.0) | .58 | 25.2 (5.5) | 25.9 (3.2) | .48 |
| 45-54 y | 15.4 (2.4) | 15.7 (1.8) | .66 | 13.5 (2.2) | 13.7(1.5) | .60 |
| 55-64 y | 12.8 (2.2) | 12.7 (1.8) | .80 | 13.9 (2.3) | 13.8 (1.6) | .90 |
| ≥65 y | 15.6 (4.7) | 14.4 (2.3) | .14 | 18.7 (5.0) | 17.3 (2.5) | .14 |
| Sex, % | ||||||
| Female | 51.8 (1.5) | 51.3 (1.4) | .12 | 51.6 (1.5) | 51.3 (1.1) | .27 |
| Male | 48.2 (1.5) | 48.7 (1.4) | .12 | 48.4 (1.5) | 48.7 (1.1) | .27 |
| Race and ethnicity, % | ||||||
| African American/Black | 4.7 (6.7) | 5.4 (7.6) | .64 | 5.4 (6.9) | 5.9 (7.2) | .75 |
| American Indian/Alaska Native | 0.21 (0.3) | 0.21 (0.2) | .94 | 0.20 (0.5) | 0.19 (0.2) | .91 |
| Asian | 4.4 (4.9) | 4.2 (4.8) | .84 | 5.2 (5.4) | 4.8 (4.8) | .69 |
| Hispanic/Latinx | 7.8 (10.9) | 11.3 (14.6) | .19 | 9.2 (11.4) | 13.0 (15.1) | .17 |
| Pacific Islander | 0.02 (0.05) | 0.01 (0.04) | .50 | 0.04 (0.04) | 0.04 (0.04) | .73 |
| White | 84.8 (13.3) | 83.0 (14.1) | .54 | 82.5 (13.5) | 81.2 (13.0) | .66 |
| Otherd | 5.9 (6.8) | 7.2 (8.8) | .43 | 6.7 (6.9) | 7.9 (7.6) | .42 |
| Educational level, % | ||||||
| High school education or less | 38.5 (12.6) | 42.6 (8.7) | .10 | 35.6 (12.5) | 39.5 (8.7) | .12 |
| College or more | 61.5 (12.6) | 57.4 (8.7) | .10 | 64.4 (12.5) | 60.5 (8.7) | .12 |
| Vacancy units, per 1000 population | 53.8 (95.6) | 37.2 (30.5) | .32 | 52.5 (100) | 34.7 (30.2) | .31 |
| Naloxone kits distributed by OEND program, per 1000 population | 0.28 (0.21) | 0.28 (0.27) | .94 | 1.19 (1.18) | 1.62 (1.79) | .17 |
| Municipality programs, No. (%) | ||||||
| Public safety equipped with naloxone | 20 (34.5) | 11 (31.4) | .77 | 20 (34.5) | 11 (31.4) | .77 |
| Drug court or a jail diversion program | 29 (50.0) | 15 (42.9) | .51 | 29 (50.0) | 15 (42.9) | .51 |
| MOAPC program established | 0 | 0 | NA | 36 (62.1) | 23 (65.7) | .83 |
| Drug arrests, per 1000 population | 0.32 (0.30) | 0.41 (0.50) | .27 | 0.23 (0.34) | 0.25 (0.33) | .77 |
| Releases from incarceration, per 1000 population | 0.14 (0.12) | 0.13 (0.10) | .54 | 0.11 (0.10) | 0.11 (0.10) | .92 |
| BSAS methadone admissions, per 1000 population | 0.34 (0.27) | 0.51 (0.42) | .02 | 0.03 (0.05) | 0.11 (0.17) | <.001 |
| BSAS residential admissions, per 1000 population | 2.17 (1.17) | 2.09 (1.09) | .73 | 2.11 (1.37) | 2.40 (1.29) | .31 |
| Fentanyl-related deaths among opioid-related deaths, % | 6.0 (20.1) | 15.0 (33.3) | .11 | 78.6 (37.4) | 82.4 (35.7) | .63 |
| Buprenorphine prescription for OUD, per 1000 population | 7.8 (3.1) | 8.4 (4.3) | .45 | 11.1 (4.9) | 13.6 (6.9) | .04 |
| Cancer-related death rate, per 100 000 population | 47.1 (19.5) | 41.3 (15.6) | .14 | 40.4 (12.2) | 37.8 (12.3) | .33 |
| Municipal population, No. | ||||||
| Mean | 52 769 | 36 842 | .28 | 54 230 | 37 762 | .28 |
| Median | 30 510 | 32 352 | 31 278 | 33 854 | ||
Abbreviations: BSAS, Massachusetts Bureau of Substance Addiction Services; EMS, emergency medical service; MOAPC, Massachusetts Opioid Abuse Prevention Collaborative; NA, not applicable; OEND, opioid education and naloxone distribution; OUD, opioid use disorder.
Ninety-three municipalities were eligible based on a threshold of 30 overdose-related emergency encounters in 2015. The first quarter was from January to March 2013, and the second from April to June 2019.
Comparison was based on the municipal-level factors in the first quarter of 2013 and by whether the municipality eventually established a postoverdose outreach program during the study period. The cumulative number of towns with outreach programs was 1 by 2013, 7 by 2014, 19 by 2015, 33 by 2016, 42 by 2017, 54 by 2018, and 58 by June 2019.
Data were available from 2014 to 2019 from the Massachusetts Ambulance Trip Record Information System. Baseline comparison was based on data in the first quarter of 2014.
Included multiracial and other.
Baseline Difference in Opioid Fatality Rate Level and Slope
The comparison of the opioid fatality rate between the nonimplementing municipalities series and the preimplementing series of the implementing municipalities found no statistically significant baseline difference in level (rate difference, 0.15; 95% CI, −0.69 to 1.15) or slope (rate difference, 0.02; 95% CI, −0.04 to 0.07) without adjusting for municipal-level covariates (eTable 1 in Supplement 1). In models adjusting for covariates, there were also no significant baseline differences in opioid fatality rates in terms of the level and slope by municipalities’ program status. Given the lack of significant difference in both baseline levels and baseline slopes, all subsequent analyses were conducted among all 93 municipalities without explicitly modeling the terms on municipalities’ program status and its interaction with baseline slope.
Fatal Opioid Overdose Rates
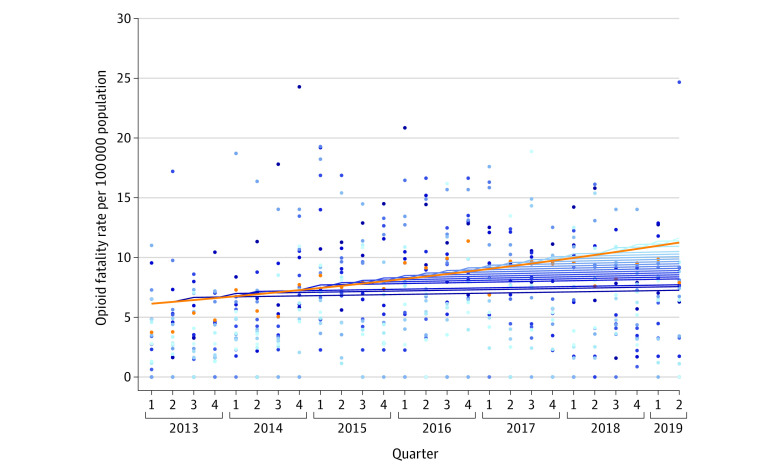
Table 2 summarizes the changes in fatal overdose rates after program implementation. As hypothesized, the main model (adjusted model 1) did not detect a statistically significant level change (adjusted RR [aRR], 1.07; 95% CI, 0.96-1.19; P = .20), but there was a significant slope change (annualized aRR, 0.94; 95% CI, 0.90-0.98; P = .003). This slope decrease corresponded to an annualized change in opioid fatality rate of −0.43 per 100 000 population (95% CI, −0.79 to −0.07 per 100 000 population; P = .02). The Figure shows the fitted quarterly opioid fatality rates of municipalities without and with programs grouped by their implementing quarters. eFigure 3 in Supplement 1 shows that the aggregate trends by outreach program status started from similar baseline levels, yet the slope of the trend of the implementing municipalities was reduced compared with the slope of the nonimplementing municipalities. In the main model (Table 3), greater proportions of people with only high school education or less, greater rates of vacancy units, inpatient residential admissions, more patients with buprenorphine prescriptions per population, and a greater proportion of fentanyl-involved opioid fatalities were significantly associated with increased opioid fatality rate.
Table 2. Changes in Level and Slope of Opioid Overdose Rates After Implementation of Postoverdose Programs Among 93 Municipalities in Massachusetts From January 2013 to June 2019.
| Outcome | Baseline | Change | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rate (95% CI)a | P value | Base modelsb | Main modelsc | Sensitivity modelsd | ||||||||||
| RR (95% CI)e | P value | RD (95% CI)f | P value | RR (95% CI)e | P value | RD (95% CI)f | P value | RR (95% CI)e | P value | RD (95% CI)f | P value | |||
| Opioid fatality rate | ||||||||||||||
| Level | 4.94 (4.38 to 5.49) | <.001 | 1.08 (0.95 to 1.23) | .24 | 0.53 (−0.52 to 1.58) | .32 | 1.07 (0.96 to 1.19) | .20 | 0.60 (−0.26 to 1.47) | .17 | 1.07 (0.96 to 1.20) | .21 | 0.58 (−0.33 to 1.49) | .21 |
| Slopeg | 0.78 (0.59 to 0.97) | <.001 | 0.92 (0.86 to 0.98) | .01 | −0.64 (−1.17 to −0.12) | .02 | 0.94 (0.90 to 0.98) | .003 | −0.43 (−0.79 to −0.07) | .02 | 0.93 (0.89 to 0.97) | .002 | −0.54 (−0.93 to −0.16) | .006 |
| Opioid emergency responses rateh | ||||||||||||||
| Level | 55.88 (47.37 to 64.40) | <.001 | 1.05 (0.94 to 1.17) | .38 | 2.94 (−7.25 to 13.12) | .57 | 1.10 (0.99 to 1.21) | .06 | 6.93 (−2.35 to 16.22) | .14 | 1.09 (0.98 to 1.21) | .12 | 7.43 (−1.76 to 16.62) | .11 |
| Slopeg | 8.77 (6.70 to 10.84) | <.001 | 0.94 (0.88 to 1.00) | .07 | −5.70 (−12.01 to 0.62) | .08 | 0.93 (0.89 to 0.98) | .007 | −5.14 (−9.96 to −0.32) | .04 | 0.93 (0.88 to 0.98) | .004 | −5.87 (−10.61 to −1.14) | .02 |
Abbreviations: RD, rate difference; RR, rate ratio.
Estimated based on identity link function with normal distribution.
Base model was a generalized estimating equations–based model with municipality-quarters as the unit of analysis assessing the pre-post level change in the outcome and the slope change after program implementation while accounting for the trend of preintervention period. Robust SEs were used to account for the clustering of repeated quarterly measures at the community level.
In addition to the base model, main models (adjusted model 1) further accounted for municipal-level factors of age groups (<25, 25-44, 45-54, 55-64, and ≥65 years), male sex, race and ethnicity (African American/Black, American Indian/Alaska Native, Asian, Hispanic/Latinx, Pacific Islander, White, and other), high school education or less, vacancy units, naloxone kits distributed by Massachusetts’ opioid education and naloxone distribution program, public safety equipped with naloxone, presence of a drug court or jail diversion program, drug arrests, releases from incarceration, Massachusetts Bureau of Substance Addiction Services methadone treatment admissions and residential admissions, Massachusetts Prescription Monitoring Program patient rate of buprenorphine prescriptions indicated for opioid use disorder, presence of Massachusetts Opioid Abuse Prevention Collaborative, and proportion of fentanyl-related deaths.
In addition to adjusted model 1, the sensitivity models (adjusted model 2) further accounted for municipal-level fixed effects using dummy variables.
Rate ratio was estimated based on a Poisson model with log-linear function.
Rate difference was estimated based on identity link function with normal distribution.
To aid interpretation, annualized slope change based on RR per year instead of per quarter after program implementation is reported.
Data of opioid emergency response rate per 100 000 population were available from 2014 to 2019 according to the Massachusetts Ambulance Trip Record Information System.
Figure. Quarterly Opioid Fatality Rate Grouped by Implementing Quarters of the Postoverdose Outreach Programs Among 93 Municipalities in Massachusetts From January 2013 Through June 2019.
Ninety-three communities were eligible based on a threshold of 30 overdose-related emergency encounters in 2015. During the study period, 58 municipalities implemented postoverdose outreach programs with varying inception quarters. Municipalities with the same implementing quarters were grouped, and their mean opioid fatality rates over time were plotted using the same shade of blue, with fitted lines indicating preimplementation slope and postimplementation slope. Among the remaining 35 municipalities that did not implement outreach programs or did not provide specific inception information, the mean opioid fatality rates over time were plotted with orange dots with a fitted line.
Table 3. Interrupted Time-Series Poisson Regression Models of the Associations of Postoverdose Programs With the Outcomes of Opioid Fatality Rate and Opioid Emergency Response Rate in Massachusetts From January 2013 to June 2019a.
| Exposure variables | Adjusted model 1b | |||
|---|---|---|---|---|
| Opioid fatality rate | Opioid overdose emergency response rate | |||
| β | P value | β | P value | |
| Intercept | −0.097 | .94 | 1.468 | .36 |
| Change in the outcome level after program | 0.069 | .20 | 0.095 | .06 |
| Change in trend per quarter after program | −0.016 | .003 | −0.017 | .007 |
| Trend per quarter before program | −0.006 | .18 | 0.020 | <.001 |
| Age, % | ||||
| 25-44 y | 0.009 | .33 | 0.009 | .51 |
| 45-54 y | 0.039 | .04 | 0.044 | .05 |
| 55-64 y | 0.012 | .45 | 0.010 | .64 |
| ≥65 y | −0.012 | .25 | −0.020 | .29 |
| Male sex, % | 0.010 | .60 | 0.007 | .78 |
| Race and ethnicity, % | ||||
| African American/Black | −0.009 | .19 | 0.0004 | .97 |
| American Indian/Alaska Native | 0.016 | .73 | 0.068 | .23 |
| Asian | −0.010 | .19 | 0.005 | .66 |
| Hispanic/Latinx | −0.005 | .19 | 0.003 | .51 |
| Pacific Islander | 0.090 | .80 | −0.269 | .43 |
| White | −0.007 | .24 | 0.002 | .78 |
| High school education or less, % | 0.014 | <.001 | 0.019 | <.001 |
| Vacancy units, per 1000 population | 0.002 | <.001 | 0.002 | .03 |
| Naloxone kits distributed by OEND program, per 1000 population | −0.016 | .46 | 0.068 | <.001 |
| Municipality programs | ||||
| Public safety equipped with naloxone | 0.051 | .39 | 0.140 | .10 |
| Drug court or a jail diversion program | −0.108 | .08 | −0.015 | .87 |
| MOAPC program established | 0.017 | .71 | 0.161 | .007 |
| Drug arrests, per 1000 population | 0.019 | .70 | 0.098 | <.001 |
| Releases from incarceration, per 1000 population | −0.213 | .26 | 0.230 | .09 |
| BSAS methadone admissions, per 1000 population | −0.099 | .07 | 0.008 | .79 |
| BSAS residential admissions, per 1000 population | 0.110 | <.001 | 0.054 | .008 |
| Fentanyl-related deaths among opioid-related deaths, % | 0.014 | <.001 | 0.002 | <.001 |
| Patients with buprenorphine prescription for OUD, per 1000 population | 0.022 | .007 | 0.010 | .26 |
Abbreviations: BSAS, Massachusetts Bureau of Substance Addiction Services; MOAPC, Massachusetts Opioid Abuse Prevention Collaborative; OEND, opioid education and naloxone distribution; OUD, opioid use disorder.
Municipality quarterly data of opioid fatality rate per 100 000 population were available from the first quarter of 2013 to the second quarter of 2019. Data on opioid emergency response rate per 100 000 population were available from the first quarter of 2014 to the second quarter of 2019 according to the Massachusetts Ambulance Trip Record Information System.
Adjusted model 1 was a generalized estimating equations Poisson model with municipality-quarters as unit of analysis assessing the pre-post level change in the outcome and the slope change after program implementation while accounting for the trend of preintervention period and a variety of municipal-level covariates, including age group (<25, 25-44, 45-54, 55-64, and ≥65 years), male sex, race and ethnicity (African American/Black, American Indian/Alaska Native, Asian, Hispanic/Latinx, Pacific Islander, White, and other), high school education or less, vacancy units, naloxone kits distributed by Massachusetts OEND program, public safety equipped with naloxone, presence of a drug court or jail diversion program, drug arrests, releases from incarceration, BSAS methadone treatment admissions and residential admissions, Massachusetts Prescription Monitoring Program patient rate of buprenorphine prescriptions indicated for OUD, presence of Massachusetts Opioid Abuse Prevention Collaborative, and proportion of fentanyl-related deaths, without accounting for municipal-level fixed effects. Robust SEs were used to account for the clustering of repeated quarterly measures at municipal level.
Opioid Emergency Response Rates
The main model (adjusted model 1) on the opioid EMS response rate outcome also showed a statistically significant slope change (annualized aRR, 0.93; 95% CI; 0.89-0.98; P = .007), which corresponded to an annual opioid EMS response rate change of −5.14 per 100 000 population (95% CI, −9.96 to −0.32 per 100 000 population; P = .04) (Table 2). We detected no statistically significant level changes of the opioid EMS response rate either based on RR or rate difference (Table 2). Greater proportions of people with only high school education or less, greater rates of vacancy units, community naloxone distribution, inpatient residential admissions, more drug arrests per population, having an opioid abuse prevention collaborative coalition, and a greater proportion of fentanyl-involved opioid fatalities were significantly associated with increased opioid EMS response rates (Table 3).
Sensitivity Analyses
Sensitivity analysis models in which the opioid-related overdose fatality outcomes were substituted for the ratio of opioid fatality rates among cancer-related fatality rates showed no statistically significant level change (aRR, 0.99; 95% CI, 0.87-1.12; P = .87) but a significant slope change (aRR, 0.94; 95% CI, 0.90-0.99; P = .04). In the adjusted model 2, controlling for municipalities as fixed effects (Table 2), the implementation of outreach programs was not significantly associated with level changes in either opioid fatality rate (aRR, 1.07; 95% CI, 0.96-1.20; P = .21) or opioid EMS response rate (aRR, 1.09; 95% CI, 0.98-1.21; P = .12) but were significantly associated with slope changes in opioid fatality rate (aRR, 0.93; 95% CI, 0.89-0.97; P = .002) and opioid EMS response rate (aRR, 0.93; 95% CI, 0.88-0.98; P = .004). The sensitivity analysis using the ratio of opioid fatality rates over cancer-related fatality rates and further controlling for municipalities as fixed effects also showed a significant slope change (aRR, 0.92; 95% CI, 0.88-0.99; P = .01). Statistically significant slope changes were also detected in additional post hoc sensitivity analyses when (1) removing municipal addiction utilization and naloxone distribution through OEND programs (aRR, 0.94; 95% CI, 0.90-0.98; P = .005 in adjusted analysis 3), (2) controlling for statewide pharmacies standing order mandate effective starting in October 2018 (aRR, 0.94; 95% CI, 0.90-0.98; P = .008 in adjusted analysis 4), and (3) excluding the 7 communities that did not provide the program inception information (aRR, 0.94; 95% CI, 0.90-0.98; P = .007 in adjusted analysis 5) (eTable 2 in Supplement 1).
Discussion
In this study, among Massachusetts municipalities with high numbers of opioid-related emergency responses, implementation of postoverdose outreach programs was significantly associated with lower opioid fatality rates over time compared with municipalities without such programs. Several sensitivity analyses confirmed the results.
Implementation of these outreach programs was also associated with a significant and gradual reduction in opioid emergency response rates. A true decrease in the number of total overdoses would mark a success from these programs; decreased help-seeking could be consistent with lower potential harm in the community but may also suggest an unintended negative consequence. Survivors may be concerned that details of their overdose or substance use may be shared with law enforcement and other stakeholders without their permission and may fear that they are more likely to be arrested due to existing warrants or that they may be subject to involuntary civil commitment.15,16 This can result in the arrest of overdose survivors or social network members.16,30 Loss of privacy, eviction, concerns about child protective services,31 and other legal issues may also affect how outreach efforts are perceived and experienced and thus may reduce help-seeking behaviors.
The study found no statistically significant association between racial and ethnic composition in municipalities with the opioid overdose outcomes. However, many African American/Black, American Indian/Alaska Native, and Hispanic/Latinx people, who have been historically and currently overpoliced and excluded from health care and other supportive services,32 may not readily benefit from outreach, especially if outreach involves law enforcement. Thus, postoverdose outreach programs should be designed with the awareness of racial and ethnic disparities in opioid overdose. The form and components of programs designed to address these inequalities deserve further study.
Communities with greater housing vacancy rates or larger proportions of residents with lower education had higher rates of opioid overdose. This finding highlights the potential role of sociocontextual determinants of health in driving the opioid crisis. Housing vacancy is often linked to neighborhood distress, unemployment, and foreclosure, which are associated with increased rates of opioid misuse.33 Those with only high school educational attainment are more likely to die of opioid overdose compared with those with a graduate degree.21 Postoverdose programs should pay attention to a broad range of components of social capital,34 including housing, education, and job training, that may support and sustain individuals’ well-being after overdose.35
Limitations
The study has several limitations. First, despite the inclusion of a rich set of community-level covariates, the detected associations were subject to residual confounding. Second, findings may not be generalizable to other communities where there are fewer opioid overdoses and, to the degree that overdose burden may be a proxy for population, may not be generalizable to more sparsely populated or rural regions. Third, the true population sizes of people who use opioids and overdose survivors in each community were not fully known as these could be stigmatized conditions and underreported. Fourth, the amount of naloxone in a given municipality was unknown. Fifth, although the many outreach programming activities were similar across communities, actual implementation varied in outreach intensity and other implementation characteristics.19 Sixth, we used incidence RR and incidence rate difference regression analyses to assess the association between program implementation and overdose outcomes. While the precise magnitude of the association cannot be reconciled between the 2 modeling strategies,36 together they offered a range and provided consistent direction of the associations.
Conclusions
In this study, among Massachusetts municipalities with high numbers of opioid-related emergency responses, implementation of postoverdose outreach programs was significantly associated with lower opioid fatality rates over time compared with municipalities that did not implement such programs. Given heterogeneity in program components and implementation as well as other contemporaneous programs that may have been in effect within municipalities, further research is needed to understand possible contributions of these various components and related program costs to the findings.
eTable 1. Baseline Difference in Opioid Fatality Rate Level and Slope between the Series of Non-implementing Municipalities and the Pre-implementation Series of the Implementing Municipalities
eTable 2. Post hoc Sensitivity Analyses of the Associations of Post-overdose Programs With the Outcomes of Opioid Fatality Rate, and Opioid Emergency Response Rate, in Massachusetts, From January 2013 to June 2019
eFigure 1. Change of Opioid Overdose Fatality Rate and Uptake of Post-overdose Outreach Programs among 93 Municipalities in Massachusetts
eFigure 2. Change of Opioid Emergency Response Rate and Uptake of Post-overdose Outreach Programs among 93 Municipalities in Massachusetts
eFigure 3. Predicted Quarterly Opioid Fatality Rate among 93 Municipalities and Aggregated by Outreach Program Status
Data Sharing Statement
References
- 1.Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999-2018. NCHS data brief, No. 356. National Center for Health Statistics; 2020. Accessed June 1, 2022. https://www.cdc.gov/nchs/products/databriefs/db356.htm
- 2.Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. 2022. Accessed June 1, 2022. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- 3.Friedman J, Mann NC, Hansen H, et al. Racial/ethnic, social, and geographic trends in overdose-associated cardiac arrests observed by US emergency medical services during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(8):886-895. doi: 10.1001/jamapsychiatry.2021.0967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. doi: 10.1136/bmj.f174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pollini RA, Joyce R, Ozga-Hess JE, Xuan Z, Green TC, Walley AY. Assessing pharmacy-based naloxone access using an innovative purchase trial methodology. J Am Pharm Assoc (2003). 2020;60(6):853-860. doi: 10.1016/j.japh.2020.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Razaghizad A, Windle SB, Filion KB, et al. The effect of overdose education and naloxone distribution: an umbrella review of systematic reviews. Am J Public Health. 2021;111(8):e1-e12. doi: 10.2105/AJPH.2021.306306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coffin PO, Behar E, Rowe C, et al. Nonrandomized intervention study of naloxone coprescription for primary care patients receiving long-term opioid therapy for pain. Ann Intern Med. 2016;165(4):245-252. doi: 10.7326/M15-2771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pardo B. Do more robust prescription drug monitoring programs reduce prescription opioid overdose? Addiction. 2017;112(10):1773-1783. doi: 10.1111/add.13741 [DOI] [PubMed] [Google Scholar]
- 9.Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality. Ann Intern Med. 2018;169(3):137-145. doi: 10.7326/M17-3107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McClellan C, Lambdin BH, Ali MM, et al. Opioid-overdose laws association with opioid use and overdose mortality. Addict Behav. 2018;86:90-95. doi: 10.1016/j.addbeh.2018.03.014 [DOI] [PubMed] [Google Scholar]
- 11.Rutkow L, Vernick JS. Emergency legal authority and the opioid crisis. N Engl J Med. 2017;377(26):2512-2514. doi: 10.1056/NEJMp1710862 [DOI] [PubMed] [Google Scholar]
- 12.Larochelle MR, Bernstein R, Bernson D, et al. Touchpoints—opportunities to predict and prevent opioid overdose: a cohort study. Drug Alcohol Depend. 2019;204:107537. doi: 10.1016/j.drugalcdep.2019.06.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bagley SM, Schoenberger SF, Waye KM, Walley AY. A scoping review of post opioid-overdose interventions. Prev Med. 2019;128:105813. doi: 10.1016/j.ypmed.2019.105813 [DOI] [PubMed] [Google Scholar]
- 14.Formica SW, Apsler R, Wilkins L, Ruiz S, Reilly B, Walley AY. Post opioid overdose outreach by public health and public safety agencies: exploration of emerging programs in Massachusetts. Int J Drug Policy. 2018;54:43-50. doi: 10.1016/j.drugpo.2018.01.001 [DOI] [PubMed] [Google Scholar]
- 15.Formica SW, Waye KM, Benintendi AO, et al. Characteristics of post-overdose public health-public safety outreach in Massachusetts. Drug Alcohol Depend. 2021;219:108499. doi: 10.1016/j.drugalcdep.2020.108499 [DOI] [PubMed] [Google Scholar]
- 16.Tori ME, Cummins E, Beletsky L, et al. Warrant checking practices by post-overdose outreach programs in Massachusetts: a mixed-methods study. Int J Drug Policy. 2022;100:103483. doi: 10.1016/j.drugpo.2021.103483 [DOI] [PubMed] [Google Scholar]
- 17.Mass.gov. Emergency medical services data—May 2021. Accessed June 1, 2022. https://www.mass.gov/doc/emergency-medical-services-data-may-2021
- 18.US Census Bureau. American Community Survey 5-Year Data (2009-2021). Accessed November 1, 2021. https://www.census.gov/data/developers/data-sets/acs-5year.html
- 19.Li Y, Hyder A, Southerland LT, Hammond G, Porr A, Miller HJ. 311 Service requests as indicators of neighborhood distress and opioid use disorder. Sci Rep. 2020;10(1):19579. doi: 10.1038/s41598-020-76685-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yamamoto A, Needleman J, Gelberg L, Kominski G, Shoptaw S, Tsugawa Y. Association between homelessness and opioid overdose and opioid-related hospital admissions/emergency department visits. Soc Sci Med. 2019;242:112585. doi: 10.1016/j.socscimed.2019.112585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Altekruse SF, Cosgrove CM, Altekruse WC, Jenkins RA, Blanco C. Socioeconomic risk factors for fatal opioid overdoses in the United States: findings from the Mortality Disparities in American Communities Study (MDAC). PLoS One. 2020;15(1):e0227966. doi: 10.1371/journal.pone.0227966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Massachusetts Crime Statistics. Accessed February 12, 2023. https://ma.beyond2020.com/ma_tops/report/drugs-dui/massachusetts/2019
- 23.Gladden RM, O’Donnell J, Mattson CL, Seth P. Changes in opioid-involved overdose deaths by opioid type and presence of benzodiazepines, cocaine, and methamphetamine—25 states, July-December 2017 to January-June 2018. MMWR Morb Mortal Wkly Rep. 2019;68(34):737-744. doi: 10.15585/mmwr.mm6834a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Soumerai SB, Ross-Degnan D, Gortmaker S, Avorn J. Withdrawing payment for nonscientific drug therapy. Intended and unexpected effects of a large-scale natural experiment. JAMA. 1990;263(6):831-839. doi: 10.1001/jama.1990.03440060077036 [DOI] [PubMed] [Google Scholar]
- 25.Kuhn L, Davidson LL, Durkin MS. Use of Poisson regression and time series analysis for detecting changes over time in rates of child injury following a prevention program. Am J Epidemiol. 1994;140(10):943-955. doi: 10.1093/oxfordjournals.aje.a117183 [DOI] [PubMed] [Google Scholar]
- 26.Pan W. Akaike’s information criterion in generalized estimating equations. Biometrics. 2001;57(1):120-125. doi: 10.1111/j.0006-341X.2001.00120.x [DOI] [PubMed] [Google Scholar]
- 27.Abouk R, Pacula RL, Powell D. Association between state laws facilitating pharmacy distribution of naloxone and risk of fatal overdose. JAMA Intern Med. 2019;179(6):805-811. doi: 10.1001/jamainternmed.2019.0272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Toce MS, Michelson K, Hudgins J, Burns MM, Monuteaux MC, Bourgeois FT. Association of state-level opioid-reduction policies with pediatric opioid poisoning. JAMA Pediatr. 2020;174(10):961-968. doi: 10.1001/jamapediatrics.2020.1980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pollini RA, Slocum S, Ozga J, et al. Pharmacists’ experiences with a statewide naloxone standing order program in Massachusetts: a mixed methods study. J Am Pharm Assoc (2003). 2022;62(1):157-166. doi: 10.1016/j.japh.2021.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wagner KD, Harding RW, Kelley R, et al. Post-overdose interventions triggered by calling 911: centering the perspectives of people who use drugs (PWUDs). PLoS One. 2019;14(10):e0223823. doi: 10.1371/journal.pone.0223823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carroll JJ, El-Sabawi T, Ostrach B. The harms of punishing substance use during pregnancy. Int J Drug Policy. 2021;98:103433. doi: 10.1016/j.drugpo.2021.103433 [DOI] [PubMed] [Google Scholar]
- 32.Substance Abuse and Mental Health Services Administration . The opioid crisis and the Black/African American Population: an urgent issue. Publication No. PEP20-05-02-001. Office of Behavioral Health Substance Abuse and Mental Health Services Administration, 2020. Accessed February 12, 2023. https://store.samhsa.gov/product/The-Opioid-Crisis-and-the-Black-African-American-Population-An-Urgent-Issue/PEP20-05-02-001
- 33.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078-15083. doi: 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.White W, Cloud W. Recovery capital: a primer for addictions professionals. Counselor (Deerfield Beach). 2008;9:22-27. [Google Scholar]
- 35.Xuan Z, Choi J, Lobrutto L, et al. Support services for young adults with substance use disorders. Pediatrics. 2021;147(suppl 2):S220-S228. doi: 10.1542/peds.2020-023523E [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Aalst R, Thommes E, Postma M, Chit A, Dahabreh IJ. On the causal interpretation of rate-change methods: the prior event rate ratio and rate difference. Am J Epidemiol. 2021;190(1):142-149. doi: 10.1093/aje/kwaa122 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Baseline Difference in Opioid Fatality Rate Level and Slope between the Series of Non-implementing Municipalities and the Pre-implementation Series of the Implementing Municipalities
eTable 2. Post hoc Sensitivity Analyses of the Associations of Post-overdose Programs With the Outcomes of Opioid Fatality Rate, and Opioid Emergency Response Rate, in Massachusetts, From January 2013 to June 2019
eFigure 1. Change of Opioid Overdose Fatality Rate and Uptake of Post-overdose Outreach Programs among 93 Municipalities in Massachusetts
eFigure 2. Change of Opioid Emergency Response Rate and Uptake of Post-overdose Outreach Programs among 93 Municipalities in Massachusetts
eFigure 3. Predicted Quarterly Opioid Fatality Rate among 93 Municipalities and Aggregated by Outreach Program Status
Data Sharing Statement