Abstract
Polygenic risk scores (PRS) have led to enthusiasm for precision medicine. However, it is well documented that PRS do not generalize across groups differing in ancestry or sample characteristics e.g., age. Quantifying performance of PRS across different groups of study participants, using genome-wide association study (GWAS) summary statistics from multiple ancestry groups and sample sizes, and using different linkage disequilibrium (LD) reference panels may clarify which factors are limiting PRS transferability. To evaluate these factors in the PRS generation process, we generated body mass index (BMI) PRS (PRSBMI) in the Electronic Medical Records and Genomics (eMERGE) network (N=75,661). Analyses were conducted in two ancestry groups (European and African) and three age ranges (adult, teenagers, and children). For PRSBMI calculations, we evaluated five LD reference panels and three sets of GWAS summary statistics of varying sample size and ancestry. PRSBMI performance increased for both African and European ancestry individuals using cross-ancestry GWAS summary statistics compared to European-only summary statistics (6.3% and 3.7% relative R2 increase, respectively, pAfrican=0.038, pEuropean=6.26×10−4). The effects of LD reference panels were more pronounced in African ancestry study datasets. PRSBMI performance degraded in children; R2 was less than half of teenagers or adults. The effect of GWAS summary statistics sample size was small when modeled with the other factors. Additionally, the potential of using a PRS generated for one trait to predict risk for comorbid diseases is not well understood especially in the context of cross-ancestry analyses – we explored clinical comorbidities from the electronic health record associated with PRSBMI and identified significant associations with type 2 diabetes and coronary atherosclerosis. In summary, this study quantifies the effects that ancestry, GWAS summary statistic sample size, and LD reference panel have on PRS performance, especially in cross-ancestry and age-specific analyses.
Keywords: polygenic risk scores (PRS), risk prediction, transferability, diversity
Introduction
Polygenic risk scores (PRS) provide individualized genetic estimates of a phenotype by aggregating genetic effects across hundreds or thousands of loci, typically from genome-wide association studies (GWAS). PRS are potentially a powerful source of increased prediction performance, even when combined with family history (1,2). However, in recent years it has become increasingly apparent that performance of PRS is substantially reduced when the ancestry of the individuals in whom prediction is being done differs from the ancestry of the individuals from the GWAS used to generate SNP weights used for PRS construction. For instance, when using GWAS from European ancestry individuals, the prediction accuracy of polygenic scores in individuals of African or Hispanic/Latino ancestry have a relative performance of 25% and 65% compared to performance in European ancestry individuals (3). Additionally, evidence exists suggesting that for some traits, such as adiposity traits, this disparity may be further exacerbated by environmental, demographic, or social risk factors (including age, physical activity, smoking status, and alcohol use (4–7)). For example, differences in the genetic architecture of body mass index (BMI) have been shown to differ between age groups (8–11). Thus, the performance of PRS for BMI is also affected by the age of the individuals used in the GWAS and the study data where the PRS is evaluated (12). Broad-sense heritability estimates for BMI in adults ranges from 40%−90% when estimated in adults of different cohorts even of homogeneous ancestry (13); even if heritability estimates are similar across populations, genetic architecture and enrichment for variants in different functional categories may still differ (14,15).
Several outstanding questions surrounding PRS, especially within the context of adiposity traits and BMI, warrant further investigation. For instance, when cross-ancestry summary statistics (i.e., those including individuals of multiple ancestry groups in the GWAS) are available, can they be used to improve prediction performance in individuals from one or more different ancestry groups? We need a more thorough evaluation of the potential prediction performance gain (or loss) in African ancestry individuals when cross-ancestry GWAS summary statistics are used to estimate the SNP weights. In addition, we need to improve our understanding of the impact of the composition of the linkage disequilibrium (LD) reference panel in combination with cross-ancestry GWAS summary statistics on PRS prediction performance. For prediction of BMI specifically, how does prediction performance differ for individuals in different age groups, especially those who are not adults (i.e., less than age 18)? Additionally, how much these different variables impact the PRS performance when considered together is important to explore. Developing a deeper understanding of which features (ancestry of individuals in the GWAS, ancestry of the individuals generating the LD references panel, ancestry of the study data, age of the study data) have the greatest impact of PRS performance will help the field develop future studies and strategies around clinical risk prediction with PRS. The degree to which increased GWAS sample size increases prediction performance regardless of these other factors is also important to determine. Finally, there is potential for using a PRS generated for one trait to predict risk for comorbid traits. Understanding how much the different elements of PRS generation affects associations with clinical comorbidities of obesity is of great importance for precision medicine.
We comprehensively investigated the influence of these factors on the performance of PRS using the Electronic Medical Records and Genomics (eMERGE) Network dataset. eMERGE is an NIH funded consortium that combines participants from multiple electronic health record (EHR) linked biobanks (16). In the present study, we included 75,661 individuals of diverse ancestry and age (14% African ancestry, 55% female, and 12% children age < 13). These individuals were from the eMERGE III imputed array dataset (N=83,717) (dbGaP Study: phs001584.v2.p2), estimated European or African ancestry, and had BMI measurements available. For these analyses, we used published BMI GWAS summary statistics from the GIANT (Genetic Investigation of ANthropometric Traits) consortium, an international consortium that primarily studies anthropometric traits, which included participants (max N=339,224, mean N per variant=226,960) from European, African, and Asian ancestry groups (17). We also used summary statistics from a European ancestry BMI GWAS (18) in UK Biobank (UKBB) individuals (N=339,721), which was conducted using both the full sample size of the European ancestry UKBB, as well as after down-sampling to the same number of individuals in the GIANT GWAS. This comparison allowed us to better evaluate whether it was the ancestry composition or the sample size of the dataset where the GWAS summary statistics were derived that affected the results of the PRS performance. We calculated PRS for BMI (PRSBMI) across 90 different combinations of analyses (described more in Methods) – six different groupings based on ancestry and age, five different LD reference panels (of varying ancestry and from three different cohorts), and the three mentioned sets of GWAS summary statistics. We then statistically compared the different sets of analyses to see what factors most influence PRSBMI performance across various groupings of individuals based on ancestry and age. Lastly, we also tested the association of the best performing PRSBMI with common comorbidities across ancestry groups to identify the clinical relevance of the PRSBMI in phenotypes derived from an Electronic Health Record (EHR). Investigation of these variables elucidates our understanding of the factors that affect PRS performance and transferability across ancestries and populations, especially within the context of BMI, as well as the potential of using PRSBMI to predict risk for comorbid disease.
Methods
Overall study design
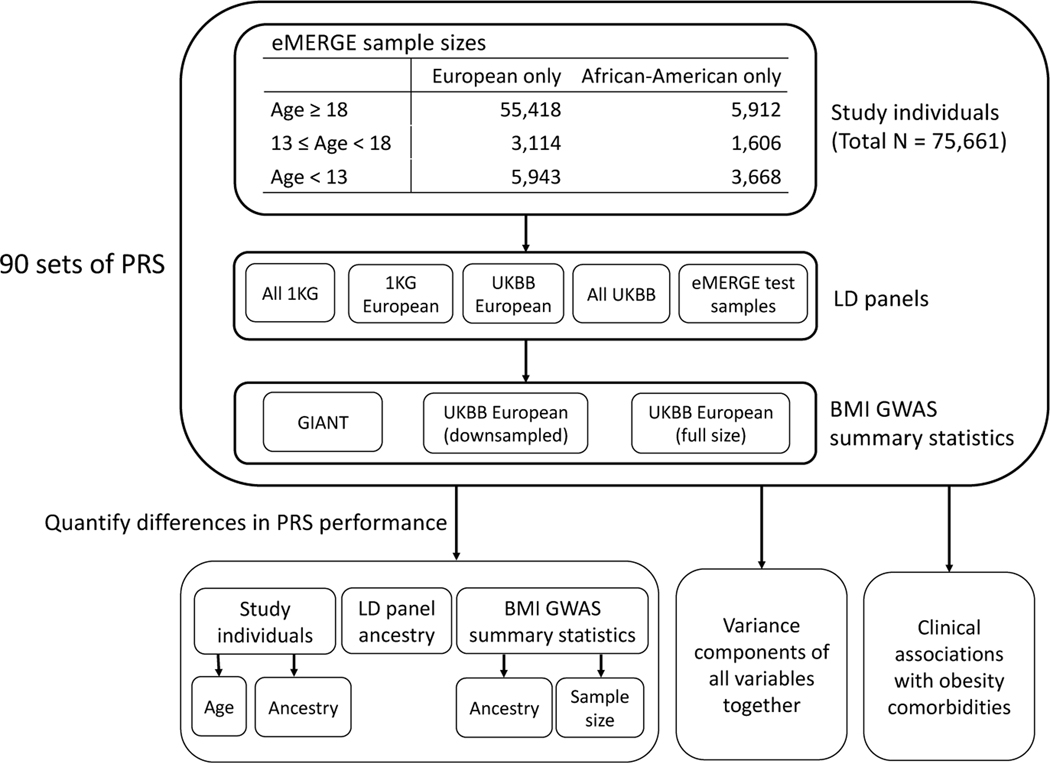
The electronic Medical Records and Genomics (eMERGE) network dataset is an NIH funded consortium that combines participants from multiple electronic health record (EHR) linked biobanks. In this study, we included 75,661 individuals with available genetic and phenotypic data. The individuals in the eMERGE dataset include multiple ancestry groups – genetically inferred ancestry was assigned by the eMERGE consortium (16) – and a large age distribution (14% African ancestry, 19% less than age 18, Figure 1). Briefly, we calculated PRSBMI for all individuals within each combination where the following elements of the model varied: 1) LD panels that differed in ancestry, 2) GWAS summary statistics with variable ancestry composition, and 3) GWAS summary statistics for two different sample sizes. The details for each of these are provided more below. The data was also split by ancestry and age group, and we statistically compared PRSBMI performance between all the different groups – in total, 90 sets of PRSBMI were calculated separately and then compared. We first estimated the effect and significance of each variable (i.e., ancestry of GWAS summary statistics and test data, LD panel ancestry, size of GWAS summary statistics, and age of test individuals) on PRS performance. Next, we estimated how much each variable affects PRSBMI performance when all are modeled together, and finally we analyzed the potential clinical associations by testing the PRSBMI for association with common comorbid conditions from the EHR. For the primary results related to LD panel or ancestry of summary statistics and test data, we restricted analyses to adults as the other age groups were limited in sample size. In the following sections, we describe all these elements in more detail.
Figure 1.
Flowchart of project. Max size of LD panel was 5,000 individuals. UK Biobank (UKBB) European GWAS summary statistics were down-sampled to the mean sample size per variant of GIANT (N=226,960), full size of UKBB European was N=377,921. 1000 Genomes is abbreviated as 1KG.
Summary statistics to generate PRSBMI
We obtained published GWAS summary statistics from the GIANT consortium (17) to use as one set of BMI GWAS summary statistics. Up to 322,154 adults of European ancestry, as well as an additional 17,072 adults of non-European ancestry (adults of African, East Asian, and South Asian ancestry), were included in the GIANT GWAS analysis.
For the second set of summary statistics, we performed a GWAS in the individuals of European ancestry from the UK Biobank (UKBB). Individuals were first filtered by low quality samples (sex mismatch between genetically inferred and self-reported, variant missingness > 5%), relatedness (no 2nd degree relatives or higher), and within the White British ancestry subset (with these individuals being defined by UKBB and selected based on self-reports and genetically determined ancestry) (18); a total of 377,921 individuals initially remained. Variants were filtered on imputation quality score (using the INFO metric (19)) > 0.30, and minor allele frequency > 1% within this subset of individuals. In addition, we generated a second set of GWAS summary statistics from the UKBB, where we randomly down-sampled individuals to the sample size in the GIANT GWAS dataset (N=226,960). In each UKBB GWAS, data processing and modeling were performed similarly as in the GIANT GWAS – summary statistics were calculated using linear regression, with age, age2, sex, and the first 5 genetic principal components (PCs) included as covariates. BMI, defined as weight in kilograms divided by squared height in meters, was first inverse-rank normal transformed.
After calculation of BMI GWAS summary statistics in each of the two datasets of UKBB individuals of European ancestry, we harmonized variants across all datasets used (UKBB, eMERGE, GIANT, and 1000 Genomes Phase 3). For the remainder of downstream analyses, we kept only those variants that were present in all datasets, and additionally excluded any strand-ambiguous SNPs (alleles A/T or C/G), and retained only biallelic variants; in total, 2,014,457 variants were retained for analyses.
LD reference panels
Five different LD reference panels were used for each set of PRSBMI calculations: 1) all of 1000 Genomes (1KGAll) (N=2,504), 2) 1000 Genomes European ancestry (1KGEUR) (N=503), 3) 5,000 randomly selected European ancestry individuals from the UK Biobank (UKBBEUR), 4) 5,000 randomly selected individuals from all of UK Biobank (UKBBAll), and 5) up to 5,000 randomly selected individuals from the dataset for which PRSBMI were being calculated for in the eMERGE dataset (referred to as test data henceforward). These panels were chosen to test for differences in ancestry distribution and sample size on PRS performance.
Statistical methods
PRS software
For each comparison set, PRSBMI were calculated using pruning and thresholding method via PRSice v2.1.9 (20). We chose to use PRSice due to the flexibility it provides in choosing external LD panels and allowed us to easily include multi-ancestry LD panels in our analyses. Default parameters were used in all analyses (clumping performed in 250 kb windows using an R2 of 0.1, p-value step size of 0.00005 between p-values of .0001 up to .10 and step size of .0001 between p-values of .10 up to .50).
Statistical comparisons
Incremental R2 for PRSBMI was calculated by subtracting the R2 using a model with only the covariates from the R2 of the model using the covariates and the PRSBMI (the default option in PRSice). Statistical differences between model performances from different iterations were determined using the Wilcoxon rank-sum test to compare the distributions of the squared residuals generated from the model for all individuals in the iteration; for comparisons between the same set of individuals, the paired Wilcoxon rank-sum test was used. When testing which of the five LD panels performed the best, we used a Bonferroni-corrected threshold of 0.05/10 = 0.005 (ten comparisons between five LD panels). When comparing the best performing PRSBMI across ancestries and summary statistics using their best LD panel, we used a Bonferroni threshold of 0.05/25 = 0.002 (25 comparisons between the five LD panels used).
Proportion of variance explained by each individual variable
We modeled all evaluated features together in the following linear regression model:
Where the Sumstat subscript is defined as a set of GWAS summary statistics, and the Test subscript is defined as a set of test individuals that PRS prediction is being assessed in. We quantified the variance in R2 that could be explained by each of these different variables using type II sum of squares from ANOVA. The sum of squares of variables involving ancestry were summed together; an interaction term between summary statistics ancestry and test data ancestry was included to identify whether the ancestry of summary statistics and test data matched.
Association of PRSBMI with comorbidities
We selected the ten most frequent Phecodes (21) from the EHR data in the eMERGE dataset (which includes obesity as a positive control) to test their association with the PRSBMI. For each Phecode, individuals were classified as a case for the condition if there was at least one occurrence of the respective Phecode in their EHR record; individuals were classified as a control for that condition if there was no occurrence of the Phecode. This classification is a rule-of-one instance of a Phecode to define case status. For each eMERGE ancestry subgroup, we selected the best performing PRSBMI i.e., the PRSBMI with the highest R2, and tested the association of the PRSBMI with these ten clinical conditions using a logistic regression model. PRSBMI was first mean-centered and standard deviation was set to 1. Sex, age, age2, and the first five genetic PCs were included as covariates.
Data visualization
The ‘ggplot2’ R package was used for plotting, with the ‘geom_signif’ package used to include significance bars. The association results were plotted using PheWAS-View (22).
Results
Effect of LD panel
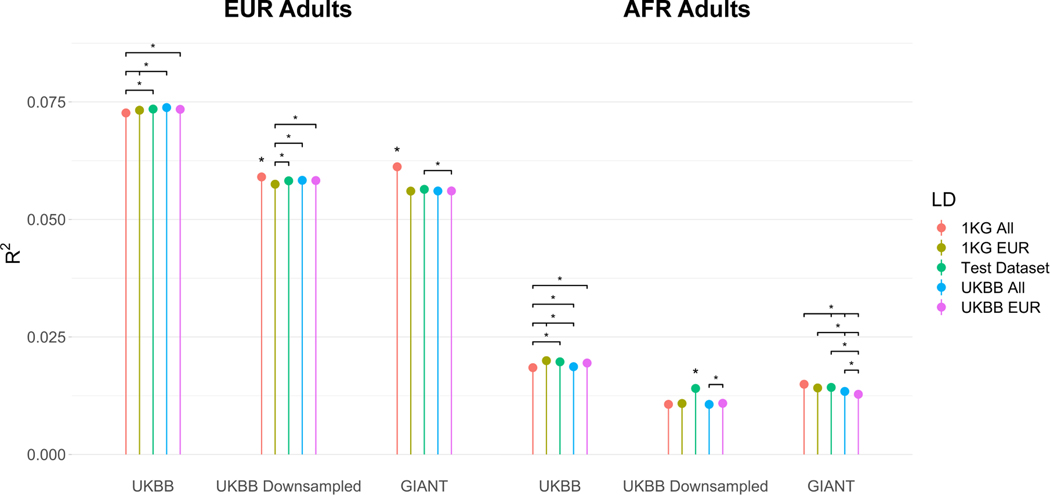
For adults of African ancestry, when using the down-sampled UKBB GWAS summary statistics, using either cross-ancestry or African ancestry test data LD panels significantly improved PRSBMI performance compared to European ancestry LD panels (Figure 2). When using the UKBB summary statistics, the top PRSBMI R2 was 0.0140 using the test data as LD panel, while the second-best performing LD panel (UKBB European) had an R2 of 0.0109 (p = 4.94×10−20). When using the GIANT summary statistics, the top PRSBMI R2 was 0.0149 using 1KGAll as the reference panel. The PRSBMI calculated using the best European ancestry panel (1KGEUR) resulted in a R2 of 0.0141, but this difference between these two reference panels was not Bonferroni significant (p = 0.037). However, the 1KGall LD panel performed significantly better than the two UKBB LD panels (UKBBAll: R2 = 0.0134, p = 3.65×10−5; UKBB European: R2 = 0.0128, p = 3.65×10−9). The test data LD panel performed the second-best with an R2 of 0.0142, and significantly outperformed the UKBB European LD panel (p = 4.78×10−5). For adults of European ancestry, we observed more significant differences in performance when using the GIANT summary statistics compared to the down-sampled UKBB summary statistics. The 1KGAll LD panel performed the best with a R2 of 0.0612. It also significantly outperformed all other LD panels (1KGEUR: R2 = 0.0560, p = 5.54×10−104; Test data: R2 = 0.0564, p = 6.50×10−67; UKBBAll: R2 = 0.0561, 8.09×10−107; UKBBEUR: R2 = 0.0561, p = 3.02×10−77). We note that this increase was larger when using the GIANT summary statistics but was still present when using the UKBB summary statistics. When using the UKBB summary statistics, the choice of LD panel had a much smaller impact on prediction performance. While the 1KGAll LD panel performed the best, the difference in performance was much less significant between the next best performing LD panel (R21KGAll = 0.0590, R2UKBBAll = 0.0583, p = 3.48×10−4). The difference between the best and worst performing scores – LD panel using 1KG all versus 1KG European – was also much less significant (p= 1.15×10−12). These results suggest that the choice of LD panel particularly matters when calculating PRSBMI using cross-ancestry GWAS, or for African ancestry individuals when the GWAS summary statistics are derived from European ancestry individuals.
Figure 2.
PRS R2 values across all runs in adults. Asterisks without bars indicate significantly different R2 values between the other 4 LD panels used. Bars are present for significant differences between specific R2 values.
However, we did observe a slight decrease in the impact of the choice of LD panel when using the full UKBB summary statistics for adults; again, the largest differences were observed in adults of African ancestry, but differences in performance across LD panels were not as significant. The test LD panel performed second best with the 1KGEUR LD panel performing best (R2Test = 0.0197, R21KGEUR = 0.0200, p = 0.18). The 1KGAll LD panel was the worst performing LD panel with an R2 of 0.0185, and this difference between the 1KGEUR LD panel was significant after multiple hypothesis correction (p = 5.08×10−7).
Effect of summary statistics and ancestry of test data
As expected, the R2 values of the PRSBMI were significantly higher when calculated for European ancestry adults than adults of African ancestry, even when using the cross-ancestry GIANT summary statistics (Figure 2). When using the GIANT summary statistics, the best performing PRSBMI in adults of European ancestry had an R2 of 0.0612, which was significantly higher than the R2 from the best performing PRSBMI in African ancestry adults (R2 = 0.0149, p < 4.9×10−324).
In African ancestry adults, the R2 when using the GIANT summary statistics was higher than the R2 when using the down-sampled UKBB summary statistics with their respective best LD panel (GIANT (1KGAll LD panel): R2 = 0.0149, UKBB (test data LD panel): R2 = 0.0140; p = 0.038). This difference was not statistically significant after multiple hypothesis correction. However, the GIANT summary statistics with the 1KGAll LD panel did significantly outperform the UKBB summary statistics with all other LD panels. When keeping the LD panel constant, the PRSBMI calculated using the GIANT summary statistics resulted in higher R2 than using the UKBB summary statistics for all LD panels except for the test data LD panel, and this difference was statistically significant for the 1KGAll (p = 1.55×10−33), 1KGEUR (p = 6.78×10−18), and UKBBAll (p = 1.28×10−15) LD panels. Somewhat surprisingly, we observed higher R2 values for European ancestry adults when using the cross-ancestry GIANT summary statistics versus the down-sampled European UKBB summary statistics (R2GIANT = 0.0612 versus R2UKBB = 0.0590), with this difference being statistically significant (p = 6.26×10−4); the best performing LD panel for both set of summary statistics was 1KGAll.
We also compared prediction performance in all individuals using the full (N=377,921) European UKBB GWAS versus the European UKBB GWAS down-sampled to GIANT’s sample size (N=226,960) (Figure 2, Supplemental Table 1). For consistency, UKBB European individuals were used for the European test ancestry comparisons, and for the African ancestry comparisons the test sets (i.e., African ancestry LD panels) were used as LD panels. Uniformly across test ancestry and age groups, we observed higher and statistically significant increases in R2.
Prediction performance across different age groups
Across different ancestries and summary statistics, we broadly observed similar R2 values for adults and teenagers, with substantially reduced performance in children (Supplemental Figure 1). R2 values in children were consistently less than half of that in adults and teenagers, with differences in R2 values for adults and teenagers being minimal (except in the case of African ancestry individuals using the GIANT summary statistics, with teenagers having more than double the R2 of adults). Somewhat surprisingly, teenagers consistently had higher R2 than adults across all analyses, although these differences were much less significant than those compared with children.
Proportion of variance explained by each assessed factor
While we observed significant differences due to ancestry, age, and number of individuals used to calculate summary statistics, we aimed to quantify the effect of these different variables on PRSBMI performance when considered together (Table 1). We observed that 89.5% of the variance in PRSBMI R2 could be explained using these variables, indicating that the majority of the effects of LD panel, ancestry, age, and sample size could be explained through linear relationships with PRSBMI R2. In the context of these comparisons, the ancestry of the summary statistics or test data accounts for 55.1% of the variance explained in PRSBMI R2. Choice of LD panel and age of test individuals accounted for similar amounts of variance explained in PRSBMI R2 (16.5% and 15.9%, respectively), while the number of individuals used to calculate the GWAS summary statistics only accounted for 1.9% of variance explained in PRSBMI R2. Per previous sections, while number of individuals used for summary statistics resulted in significant differences in PRSBMI performance, its overall impact when modeled jointly with all the other factors in the context of these analyses seemed to be small.
Table 1.
Proportion of variance in R2 that can be explained by different variables using type II sum of squares from ANOVA.
| Variable | Proportion of explained variance |
|---|---|
| Ancestry of summary statistics or test data | 0.5510 |
| Choice of LD reference panel | 0.1650 |
| Age of test individuals | 0.1590 |
| N individuals used to calculate summary statistics | 0.0195 |
| Residuals (unexplained variance) | 0.1050 |
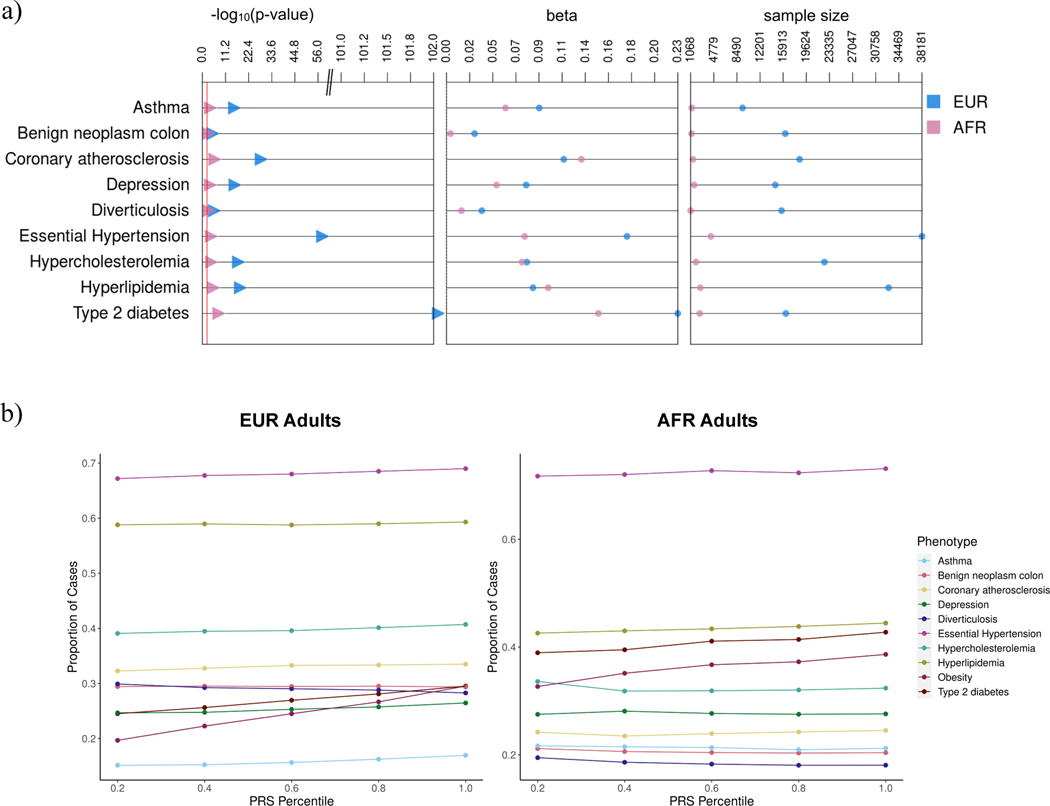
PRSBMI association with comorbid traits
To determine whether the PRSBMI was associated with clinical comorbidities, we performed a Phenome-Wide Association Study for ten clinical conditions (Supplemental Table 2, described more in Methods). Here, the PRSBMI was tested for association with diagnosis codes (Phecodes) to evaluate whether the polygenic background for BMI associates with these clinical diagnoses. The PRSBMI was significantly associated with several of the most frequent Phecodes in eMERGE, particularly in European adults (Figure 3a). As expected, obesity had the strongest association with PRSBMI in all ancestry groups (pEUR < 4.9×10−324; pAFR = 5.17×10−8); this was a positive control. In European ancestry individuals, the best performing PRSBMI was also significantly positively associated with type 2 diabetes (pEUR = 1.04×10−102), essential hypertension (pEUR = 7.12×10−56), coronary atherosclerosis (pEUR = 3.61×10−26), hyperlipidemia (pEUR = 4.38×10−16), depression (pEUR = 1.95×10−13), hypercholesteremia (pEUR = 3.64×10−15), asthma (pEUR = 3.13×10−13), and diverticulosis (pEUR = 0.0017). These associations were less statistically significant in African ancestry individuals, which had much lower sample size, and many associations were no longer significant after Bonferroni correction. Only type 2 diabetes (pAFR = 1.2×10−5) and coronary atherosclerosis (pAFR = 0.001) were significantly associated with the PRSBMI in African ancestry adults. We also looked at the prevalence of each condition per PRS quintile for the most significantly associated conditions (Figure 3b). The case prevalence generally increased in higher PRSBMI quintile groups for conditions significantly associated with the PRSBMI, a trend matching the results we obtained from the association analysis. Phenotypes with downward trends were not significantly associated with PRSBMI, and low sample sizes in earlier quintile groups may have contributed to this seemingly decreasing prevalence. We performed similar analyses in teens and children but identified no statistically significant associations (results not shown). The much smaller sample sizes of the Phecodes in these age groups may have also contributed to the lack of statistically significant results – most of these diagnoses are adult-onset conditions.
Figure 3.
a) Best PRSBMI associations with top 9 most prevalent conditions overall in eMERGE adults.
Note the association with obesity is not included in the plot because the p-value in European ancestry individuals was pEUR < 4.9×10−324 which was off the scale of the plot. b) Prevalence plots of significantly associated conditions in eMERGE adults by best performing PRS quintile
Discussion
Somewhat unintuitively, African ancestry LD panels performed best for African ancestry individuals, regardless of whether European ancestry or cross-ancestry GWAS summary statistics were used. We observed minimal impact of the choice of LD panel when both test data and summary statistics were of European ancestry. These results suggest that as long as either the test data or GWAS summary statistics are of similar ancestry, or the test data and LD panel are of similar ancestry, the difference in PRS performance may be minimal as compared to if all the GWAS summary statistics, test data, and LD panel are all of the same ancestry. We also observed significantly decreased PRS performance in children compared to adults and teens, with the GWAS used in this study being conducted on adult populations.
While the findings in this study highlight many important strategies for performing PRS in different ancestry and age groups, there are limitations that should be addressed in future studies.
First, inclusion of analyses that evaluate how different proportions of non-European ancestry individuals affect the prediction performance of PRS would be useful. The GIANT summary statistics we used in this study are only about 6% non-European ancestry. It may be useful to see how the PRS prediction performance changes in both non-European and European ancestry datasets as a function of the proportion of non-European ancestry samples included in the GWAS. Such analyses may be possible by combining African ancestry individuals from these different datasets. These analyses will be possible once larger datasets that include non-European ancestry cohorts are publicly available or could be tested by analyzing other traits with larger African ancestry GWAS. Future analyses could also include sex-stratified GWAS and comparison sets to evaluate the influence of sex on PRSBMI performance. Finally, repeating these types of analyses with different PRS methods would be useful as novel PRS methods are being developed on a regular basis, many of which incorporate ancestry in different ways.
Overall, this study demonstrates the importance of expanding non-European ancestry data resources for PRS, specifically in the generation of GWAS summary statistics and LD reference panels. Failure to do so reduces the impact of PRS in diverse populations and increases the potential for continued health disparities, especially in precision medicine where genetics is being integrated into clinical care.
Supplementary Material
Acknowledgements
eMERGE Network (Phase III): This phase of the eMERGE Network was initiated and funded by the NHGRI through the following grants: U01HG8657 (Group Health Cooperative/University of Washington); U01HG8685 (Brigham and Women’s Hospital); U01HG8672 (Vanderbilt University Medical Center); U01HG8666 (Cincinnati Children’s Hospital Medical Center); U01HG6379 (Mayo Clinic); U01HG8679 (Geisinger Clinic); U01HG8680 (Columbia University Health Sciences); U01HG8684 (Children’s Hospital of Philadelphia); U01HG8673 (Northwestern University); U01HG8701 (Vanderbilt University Medical Center serving as the Coordinating Center); U01HG8676 (Partners Healthcare/Broad Institute); and U01HG8664 (Baylor College of Medicine). UK Biobank: All data for this cohort pertained to project 32133 – “Integration of multi-organ imaging phenotypes, clinical phenotypes, and genomic data”. MDR would also like to acknowledge NIH AI077505.
Footnotes
Description of supplemental data
Supplemental data include one figure and two tables (https://upenn.box.com/s/7cec571ltjkcyv409vwi7w9t0stkvo12).
Declaration of author competing interests
Authors have no competing interests to declare.
Data and code availability
Code supporting the current study are available from the corresponding author on request.
References
- 1.Truong B, Zhou X, Shin J, Li J, van der Werf JHJ, Le TD, et al. Efficient polygenic risk scores for biobank scale data by exploiting phenotypes from inferred relatives. Nat Commun. 2020. Jun 17;11(1):3074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Margaux LA Hujoel Po-Ru Loh, Benjamin M. Neale, Alkes L.Price. Incorporating family history of disease improves polygenic risk scores in diverse populations. Available from: https://www.biorxiv.org/content/10.1101/2021.04.15.439975v1 [DOI] [PMC free article] [PubMed]
- 3.Martin AR, Kanai M, Kamatani Y, Okada Y, Neale BM, Daly MJ. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat Genet. 2019. Apr;51(4):584–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rask-Andersen M, Karlsson T, Ek WE, Johansson Å. Gene-environment interaction study for BMI reveals interactions between genetic factors and physical activity, alcohol consumption and socioeconomic status. PLoS Genet. 2017. Sep;13(9):e1006977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robinson MR, English G, Moser G, Lloyd-Jones LR, Triplett MA, Zhu Z, et al. Genotype-covariate interaction effects and the heritability of adult body mass index. Nat Genet. 2017. Aug;49(8):1174–81. [DOI] [PubMed] [Google Scholar]
- 6.Sulc J, Mounier N, Günther F, Winkler T, Wood AR, Frayling TM, et al. Quantification of the overall contribution of gene-environment interaction for obesity-related traits. Nat Commun. 2020. Mar 13;11(1):1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Justice AE, Winkler TW, Feitosa MF, Graff M, Fisher VA, Young K, et al. Genome-wide meta-analysis of 241,258 adults accounting for smoking behaviour identifies novel loci for obesity traits. Nat Commun. 2017. Apr 26;8:14977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Helgeland Ø, Vaudel M, Juliusson PB, Lingaas Holmen O, Juodakis J, Bacelis J, et al. Genome-wide association study reveals dynamic role of genetic variation in infant and early childhood growth. Nat Commun. 2019. Oct 1;10(1):4448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vogelezang S, Bradfield JP, Ahluwalia TS, Curtin JA, Lakka TA, Grarup N, et al. Novel loci for childhood body mass index and shared heritability with adult cardiometabolic traits. PLoS Genet. 2020. Oct;16(10):e1008718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Couto Alves A, De Silva NMG, Karhunen V, Sovio U, Das S, Taal HR, et al. GWAS on longitudinal growth traits reveals different genetic factors influencing infant, child, and adult BMI. Sci Adv. 2019. Sep;5(9):eaaw3095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choh AC, Lee M, Kent JW, Diego VP, Johnson W, Curran JE, et al. Gene-by-age effects on BMI from birth to adulthood: the Fels Longitudinal Study. Obes Silver Spring Md. 2014. Mar;22(3):875–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mostafavi H, Harpak A, Agarwal I, Conley D, Pritchard JK, Przeworski M. Variable prediction accuracy of polygenic scores within an ancestry group. eLife. 2020. Jan 30;9:e48376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elks CE, den Hoed M, Zhao JH, Sharp SJ, Wareham NJ, Loos RJF, et al. Variability in the heritability of body mass index: a systematic review and meta-regression. Front Endocrinol. 2012;3:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galinsky KJ, Reshef YA, Finucane HK, Loh PR, Zaitlen N, Patterson NJ, et al. Estimating cross-population genetic correlations of causal effect sizes. Genet Epidemiol. 2019. Mar;43(2):180–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shi H, Gazal S, Kanai M, Koch EM, Schoech AP, Siewert KM, et al. Population-specific causal disease effect sizes in functionally important regions impacted by selection. Nat Commun. 2021. Feb 17;12(1):1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stanaway IB, Hall TO, Rosenthal EA, Palmer M, Naranbhai V, Knevel R, et al. The eMERGE genotype set of 83,717 subjects imputed to ~40 million variants genome wide and association with the herpes zoster medical record phenotype. Genet Epidemiol. 2019. Feb;43(1):63–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015. Feb 12;518(7538):197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018. Oct;562(7726):203–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howie BN, Donnelly P, Marchini J. A flexible and accurate genotype imputation method for the next generation of genome-wide association studies. PLoS Genet. 2009. Jun;5(6):e1000529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Euesden J, Lewis CM, O’Reilly PF. PRSice: Polygenic Risk Score software. Bioinforma Oxf Engl. 2015. May 1;31(9):1466–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu P, Gifford A, Meng X, Li X, Campbell H, Varley T, et al. Mapping ICD-10 and ICD-10-CM Codes to Phecodes: Workflow Development and Initial Evaluation. JMIR Med Inform. 2019. Nov 29;7(4):e14325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pendergrass SA, Dudek SM, Crawford DC, Ritchie MD. Visually integrating and exploring high throughput Phenome-Wide Association Study (PheWAS) results using PheWAS-View. BioData Min. 2012. Jun 8;5(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Code supporting the current study are available from the corresponding author on request.