Abstract
Introduction and importance
Morgagni–Larrey hernias (MLHs) are rare diaphragmatic hernias that can cause incarceration or strangulation of the hernia contents in some cases. Here we report a case of incarcerated Larrey hernia with small bowel obstruction, which was successfully treated with emergent laparoscopic surgery.
Case presentation
An 87-year-old woman presented to our hospital with abdominal pain and nausea. Computed tomography scan revealed an MLH comprising an obstructed intestinal loop. The patient underwent emergency laparoscopic surgery. Surgical findings showed incarceration of the small bowel on the left side of the falciform ligament. The small bowel was laparoscopically reduced and does not show signs of intestinal ischemia or perforation. The hernia orifice, which was approximately 15 mm in diameter, was closed with a surgical suture without the need for sac excision. The patient was discharged on postoperative day 7 without postoperative complications.
Clinical discussion
There are no established surgical techniques for the treatment of MLH due to its rarity. Our experience in the present case suggests that the laparoscopic approach might be considered as a feasible method even for incarcerated MLH.
Conclusion
Surgical techniques for MLH should be selected on a case-by-case basis.
Keywords: Morgagni–Larrey hernia, small bowel obstruction, laparoscopic surgery; Case report
Highlights
-
•
Morgagni–Larrey hernias (MLHs) are rare diaphragmatic hernias.
-
•
MLHs can lead to the incarceration or strangulation of hernia contents.
-
•
Surgical techniques for MLHs are selected on a case-by-case basis.
-
•
Laparoscopic approach might be useful for incarcerated or strangulated MLHs.
1. Introduction
Morgagni–Larrey hernias (MLHs) are rare and account for only 2 %–4 % of all congenital diaphragmatic hernias [1]. MLH occurs owing to the defective fusion of the septum transversum with costal arches. In the current literature, the frequency of right-sided (Morgagni) hernias is the highest with 90 %, followed by bilateral MLH (8 %) and left-sided (Larrey) hernias (2 %) [2]. Some cases are asymptomatic and are noted incidentally during imaging studies; most of the patients present with nonspecific respiratory and gastrointestinal symptoms. Colon, small bowel, or stomach herniation is associated with a higher risk of strangulation and possible ischemia and perforation. There is no established technique for treating MLH in adults [3]. Here, we report a case of incarcerated Larrey hernia with small bowel obstruction successfully treated with emergency laparoscopic surgery. This work has been reported following the Surgical Case Report guidelines [4].
2. Presentation of case
An 87-year-old woman with a history of moderate aortic valve stenosis, atrial fibrillation, and hypertension presented with abdominal pain and nausea. The patient was being treated with rivaroxaban for atrial fibrillation. Her body weight, height, and body mass index were 35 kg, 140 cm, and 17.9 kg/m2, respectively. Abdominal examination revealed distended abdomen with mild epigastric tenderness and hypoactive bowel sounds.
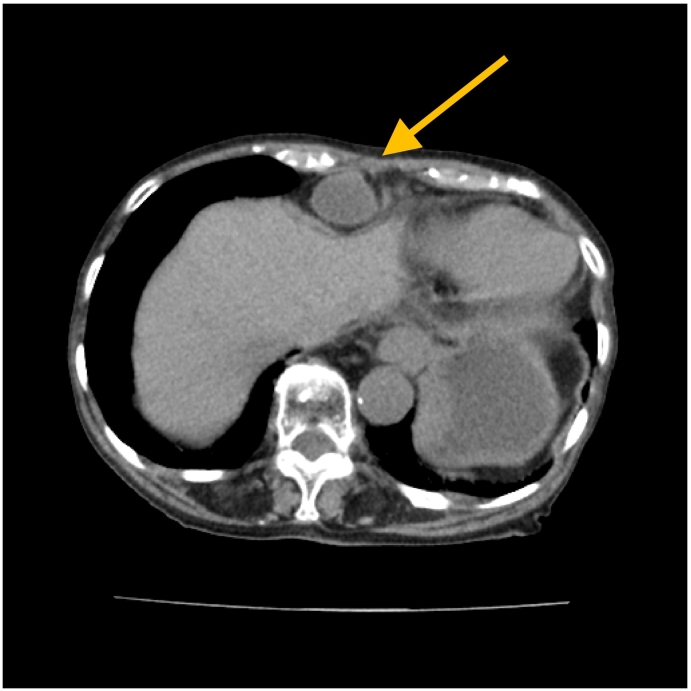
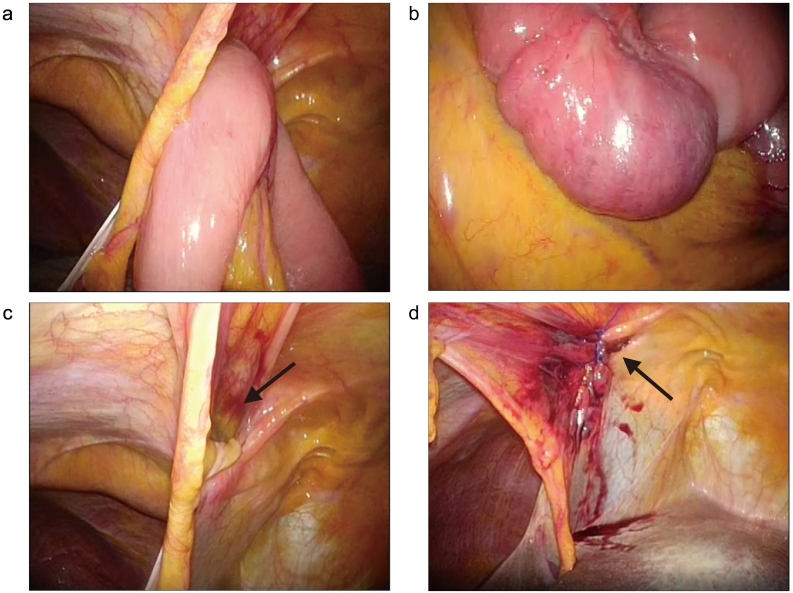
Computed tomography revealed an anterior diaphragmatic hernia including an obstructed intestinal loop (Fig. 1). The preoperative diagnosis was incarcerated Morgagni or Larrey hernia with small bowel obstruction, and the patient underwent emergency laparoscopic surgery under general anesthesia. Three trocars were used: one 12-mm umbilical trocar for the scope placed using the Hasson technique and two 5-mm trocars placed on each side of the umbilical region as working ports. Abdominal air pressure was set at 10 mmHg, and a flexible scope was introduced into the peritoneal cavity. Based on the intraoperative finding of small bowel incarceration on the left side of the falciform ligament (Fig. 2a), the diagnosis was incarcerated Larrey hernia with small bowel obstruction. The small bowel was laparoscopically reduced by traction of the mesentery using forceps. No signs of small intestinal necrosis, perforation, or cicatricial stenosis were observed (Fig. 2b). The hernia orifice was approximately 15 mm (Fig. 2c), which was laparoscopically closed using a nonabsorbable surgical suture without sac excision (Fig. 2d). The total operating time was 49 min, and the blood loss volume was 1 mL. The patient was initiated on a liquid diet on postoperative day 3 and discharged without postoperative complications on postoperative day 7. The patient exhibited no signs of hernia recurrence at the 6-month follow-up evaluation.
Fig. 1.
Computed tomography showing a Morgagni–Larrey hernia comprising an obstructed intestinal loop (arrow).
Fig. 2.
Intraoperative findings. (a) Small intestine is incarcerated into the left side of the falciform ligament. (b) No signs of small intestinal necrosis or perforation are observed. (c) Hernia orifice (arrow) is approximately 15 mm in diameter. (d) Hernia orifice is closed with a nonabsorbable surgical suture (arrow).
3. Discussion
There are no established surgical techniques for the treatment of MLH due to its rarity [3]. Surgical techniques used for MLH treatment have been discussed in terms of the following two points: surgical approach and hernia repair.
Abdominal and thoracic surgical approaches are employed for MLH treatment. The abdominal approach allows for easier reduction of hernia contents, better evaluation of contralateral diaphragmatic defects, and better evaluation and repair of intraabdominal lesions. However, this approach is not advantageous in patients with obesity or those with a history of abdominal surgery. The thoracic approach allows for an easier separation of the hernia sac from the mediastinal and pleural structures [5]. However, the thoracic approach requires single-lung ventilation, does not allow for the inspection of both sides of the diaphragm, and limits the ability to evaluate hernia contents. There is no consensus on the specific approach with better outcomes; however, the abdominal approach provides a clear advantage in patients with suspicious strangulation or perforation. The recent increase in the popularity of laparoscopic and thoracoscopic approaches as minimally invasive procedures has been reported to be associated with reduced surgical trauma, less postoperative pain, shorter hospital stays, and earlier return to activity than conventional open approaches in MLH [3], [6], [7], [8].
Surgical hernia repair methods include primary closure, mesh interposition, and mesh reinforcement with primary closure [9]. The cause of differences in the recurrence rate among these repair methods is unclear. Some studies recommend mesh use to avoid tension in cases with a large hernia portal [7]. Radical excision and resection of the hernia sac for MLH cases are controversial [2], [6]. Sac excision in patients with paraesophageal hernias has been reported to decrease recurrence [10]. In paraesophageal hernias, esophagus is a part of the sac. However, in MLH, the sac wall includes the falciform ligament and ligamentum teres; as such, sac excision may not be necessary [11]. Furthermore, sac excision for MLH is associated with the risk of violating the neighboring viscera, including the phrenic nerve, pericardium, pleura, and lung.
In the present case, emergency surgery was performed for incarcerated Larrey hernia with small bowel obstruction in an older, low-weight adult patient with cardiac disease who was treated with an anticoagulant. Open abdominal approach was often chosen in previously reported cases of incarcerated MLH with small bowel obstruction [12], [13], [14], [15]. The laparoscopic approach allowed the reduction of the incarcerated small bowel and its evaluation for the presence of stenosis or ischemia. Small bowel resection with slight extension of the umbilical wound would have been possible in the presence of necrosis affecting the incarcerated small bowel. Laparoscopic primary closure of the hernia orifice without sac excision resulted in a shorter operative time and minimal blood loss, and the patient did not develop complications. The laparoscopic method was successful because of the small hernia orifice in the present case. However, in incarcerated MLH with a large hernia orifice, initial surgery should be limited to improve bowel obstruction and delayed hernia repair should be considered. The evidence level for MLH repair in adults is low due to the limited number of cases and lack of long-term follow-up of patients, and long-term outcomes in larger cohorts should be evaluated.
4. Conclusion
Surgical techniques for MLH should be selected on a case-by-case basis due to its rarity. The present case suggests that the laparoscopic approach with simple closure repair of the MLH might be considered as a safe and effective approach in older patients with comorbidities such as those using anticoagulants.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
Not applicable.
Ethics approval
Ethic approval has been exempted by Clinical Research Ethics Committee of Iwate Prefectural Ninohe Hospital.
Author contribution
NS conceived the case presentation and drafted the manuscript.
SM, YM, and YI took care of the management of the patient.
AS read and approved the final manuscript.
Guarantor
Noriyuki Sasaki.
Registration of research studies
This case report does not require registration as a research study.
Declaration of competing interest
None.
Acknowledgements
None.
References
- 1.Katsaros I., Katelani S., Giannopoulos S., Machairas N., Kykalos S., Koliakos N., et al. Management of Morgagni’s hernia in the adult population: a systematic review of the literature. World J. Surg. 2021;45:3065–3072. doi: 10.1007/s00268-021-06203-3. [DOI] [PubMed] [Google Scholar]
- 2.Dapri G., Himpens J., Hainaux B., Roman A., Stevens E., Capelluto E., et al. Surgical technique and complications during laparoscopic repair of diaphragmatic hernias. Hernia. 2007;11:179–183. doi: 10.1007/s10029-006-0161-8. [DOI] [PubMed] [Google Scholar]
- 3.Horton J.D., Hofmann L.J., Hetz S.P. Presentation and management of morgagni hernias in adults: a review of 298 cases. Surg. Endosc. 2008;22:1413–1420. doi: 10.1007/s00464-008-9754-x. [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Sirmali M., Türüt H., Gezer S., Findik G., Kaya S., Tastepe Y., et al. Clinical and radiologic evaluation of foramen of morgagni hernias and the transthoracic approach. World J. Surg. 2005;29:1520–1524. doi: 10.1007/s00268-005-0055-4. [DOI] [PubMed] [Google Scholar]
- 6.Rau H.G., Schardey H.M., Lange V. Laparoscopic repair of a morgagni hernia. Surg. Endosc. 1994;8:1439–1442. doi: 10.1007/BF00187355. [DOI] [PubMed] [Google Scholar]
- 7.Thoman D.S., Hui T., Phillips E.H. Laparoscopic diaphragmatic hernia repair. Surg. Endosc. Other Interv. Tech. 2002;16:1345–1349. doi: 10.1007/s00464-001-8162-2. [DOI] [PubMed] [Google Scholar]
- 8.Hussong R.L., Jr., Landreneau R.J., Cole F.H., Jr. Diagnosis and repair of a morgagni hernia with video-assisted thoracic surgery. Ann. Thorac. Surg. 1997;63:1474–1475. doi: 10.1016/s0003-4975(97)00216-6. [DOI] [PubMed] [Google Scholar]
- 9.Ryan J.M., Rogers A.C., Hannan E.J., Mastrosimone A., Arumugasamy M. Technical description of laparoscopic morgagni hernia repair with primary closure and onlay composite mesh placement. Hernia. 2018;22:697–705. doi: 10.1007/s10029-018-1760-x. [DOI] [PubMed] [Google Scholar]
- 10.Edye M., Salky B., Posner A., Fierer A. Sac excision is essential to adequate laparoscopic repair of paraesophageal hernia. Surg. Endosc. 1998;12:1259–1263. doi: 10.1007/s004649900832. [DOI] [PubMed] [Google Scholar]
- 11.Kelly M.D. Laparoscopic repair of strangulated Morgagni hernia. World J. Emerg. Surg. 2007;2:27. doi: 10.1186/1749-7922-2-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saqib S.U., Hamid K., Chawla T.U. Congenital morgagni hernia presenting as complete small bowel obstruction in the adult - a case report. Int. J. Surg. Case Rep. 2020;76:390–393. doi: 10.1016/j.ijscr.2020.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muhumuza J., Bitamazire D., Atumanyire J., Akello V., Sikakulya F.K., Kagenderezo B. A rare presentation of morgagni hernia in an adult with strangulated ileum: a case report. Int. J. Surg. Case Rep. 2022;99 doi: 10.1016/j.ijscr.2022.107675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ohn M.H., Ng J.R., Mehan T.N., Luen N.P. Strangulated morgagni hernia masquerading as an acute coronary syndrome. BMJ Case Rep. 2021;14(7) doi: 10.1136/bcr-2021-244045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Modi M., Dey A.K., Mate A., Rege S. Strangulated Morgagni's hernia: a rare diagnosis and management. Case Rep. Surg. 2016;2016 doi: 10.1155/2016/2621383. [DOI] [PMC free article] [PubMed] [Google Scholar]