Dear Editor,
Long-term sequelae of COVID-19 pneumonia are still unknown. Han et al. [1] were the first to describe chest CT findings with pulmonary fibrosis-like changes (FLC) in about one third of patients at six-months follow-up; in this study FLC were defined by the presence of traction bronchiectasis, parenchymal bands and/or honeycombing. Similar results were observed by our group at six months in a cohort of patients hospitalized for severe Covid-19 pneumonia [2]. However, whether these lesions represent a marker of ongoing fibrosis and their clinical meaning remain uncertain.
The aim of this study is to evaluate the radiologic findings at two-years follow-up chest CT-scans in patients who presented FLC on chest-CT performed 6 months after severe COVID-19 pneumonia.
This study obtained ethical approval by the Ethics Committee of our Hospital. We retrospectively evaluated two-years CT scans of patients who had evidence of FLC at 6-months follow-up after severe COVID 19 pneumonia.
All CT images were evaluated by a radiologist with 20-years experience in thoracic radiology, who was blinded to patients’ clinical data. CT lesions were defined according to Fleishner Society classification system. We assessed the extent of pulmonary abnormalities by a semi-quantitative score (CT-score) and calculated the Warrick score, as previously described [2].
Recorded clinical data and pulmonary function tests data were also evaluated. Statistical analysis: categorical variables were reported as counts (percentages) whereas continuous variables were reported as mean (standard deviation, SD) or median (interquartile range, IQR), as appropriate.
Eighteen patients (15 men; 3 women; median age 70—IQR 64.75–77.75)-out of 24 in which FLC had been found at six months [2]—underwent a two years CT scan and follow-up clinical evaluation at our hospital.
The worst, median P/F during hospitalization for Covid-19 pneumonia was 171 (IQR 97.25–259); 10 patients underwent non-invasive and 1 invasive mechanical ventilation.
As compared to 6-months’ findings, 2-years CT scans showed a marked reduction in ground glass opacities (GGO) while reticular lesions remained the predominant pattern. Of notice, none of the patients showed honeycombing and/or traction bronchiectasis as new findings at 2-years follow-up. Persistence of FLC was confirmed in 18/18 patients, although a reduction in density and number of lesions was observed in most of the patients (Fig. 1). At two years, CT and Warrick scores improved respectively in 6 and 5 patients, leading to a trend toward reduction in mean scores values (Table 1).
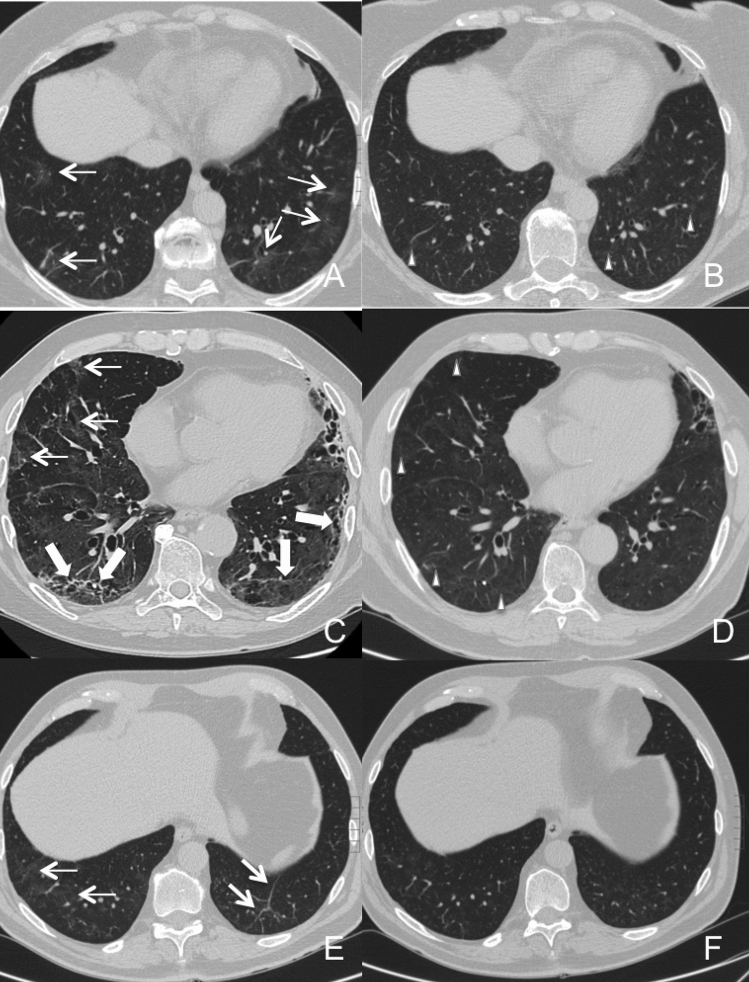
Fig. 1.
Serial non-contrast axial chest CTs of three studied patients with prior severe COVID-19 pneumonia. Upper line: chest CT of a 61-year-old woman showed ground-glass opacities, reticular alterations and parenchymal bands (Warrick Score: 8; CT score: 5) in both lower lobes at the 6-month CT follow-up (Panel A). At the 2-years follow-up (Panel B) complete resolution of GGO with persistency of reticulations and bands was noticed (Warrick score: 5; CT score: 3). Middle line: panel C shows six-month follow-up chest CT of a 65-year-old woman demonstrating ground-glass opacities, reticular alterations, parenchymal bands and traction bronchiectasis in middle lobe, lingula and in both lower lobes (Warrick score: 20; CT score: 9). At the 2-years follow-up (Panel D) almost complete resolution of traction bronchiectasis, bands and GGO with persistency of reticulations was noted (Warrick score: 13; CT score: 6). Bottom line: panel E shows chest CT of a 57-year-old woman with reticular alterations and parenchymal bands in the lung lower lobes at the 6-month follow-up (Warrick score: 8; CT score: 8). At 2-years follow-up (Panel F) complete resolution of GGO and parenchymal bands with persistency of tiny residual reticulations are observed (Warrick score: 5; CT score: 5).
Table 1.
The table describes CT findings with a comparison between 6-months and 2-years follow-up CT examinations
| 6 months | 2 years | |
| CT findings | ||
| CT score—median (IQR) | 5 (3.75–6.25) | 4 (3–6) |
| Warrick score—median (IQR) | 8 (7–9) | 7 (5–9) |
| Presence of fibrotic like changes—no. (%) | 18 | 18 |
| Predominant abnormal CT pattern | N° lesions (%)* | N° lesions (%)** |
| Ground-glass opacities | 9 (50) | 1 (5.5) |
| Reticular abnormalities | 12 (66.7) | 15 (83.3) |
| Parenchymal bands | 7 (38.9) | 7 (38.9) |
| CT lesions ° | N° lesions (%) | N° lesions (%) |
| Ground-glass opacities | 13 (72.2) | 7 (38.9) |
| Consolidation or nodules | 0 | 0 |
| Reticular abnormalities | 18 | 18 |
| Parenchymal bands | 18 | 18 |
| Traction bronchiectasis | 6 (33.3) | 3 (16.7) |
| Honeycombing | 2 (11.1) | 2 (11.1) |
| Pleural abnormalities (irregular pleura) | 2 (11.1) | 2 (11.1) |
*9 patients presented more than one prevalent abnormal CT pattern
**5 patients presented more than one prevalent abnormal CT pattern
°All patients, both at 6 and 24 months, presented more than one alteration
In more than half (72%) of the patients we observed persistency of symptoms; in particular, 39% reported fatigue and/or dyspnea. In 83% of patients a reduction in DLCO (< 80%) was detected; two patients showed a DLCO < 60%.
To the best of our knowledge, this is the first report to investigate the evolution of lung CT abnormalities after two years from severe COVID-19 pneumonia.
In most patients we observed a progressive reabsorption of GGO with persistency of reticulations and parenchymal bands, thus confirming findings reported in studies with shorter follow-up.
Furthermore, we noticed a persistency of FLC in all the patients with a slight reduction in their extent over time, similarly to what reported at one-year evaluation [3, 4].
A careful longitudinal analysis of CT findings suggests that these lung abnormalities may not be clues of a developing fibrosis. In fact, thin reticulations and parenchymal bands were the most common findings, while none of the patients had a new diagnosis of traction bronchiectasis and/or honeycombing which are considered true markers of fibrotic evolution.
These observations are supported by a trend toward a reduction in quantitative scores together with fading of lesions in most of the patients.
In conclusion, we suppose that the CT alterations reported may represent residual radiological scars-as suggested by Wells et al. [5]—rather than markers of ongoing fibrosis. Future studies on larger populations and longer follow-up period are needed to verify this hypothesis, which could impact on follow-up management of patients with COVID-19 pneumonia.
Data availability statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
All procedures performed in our study were in accordance with the ethical standard of institutional research committee and with the 1964 Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nicola Flor, Email: nicola.flor@unimi.it.
Federica Leidi, Email: federica.leidi@asst-fbf-sacco.it.
Francesco Casella, Email: francesco.casella@asst-fbf-sacco.it.
Leonardo Mariani, Email: leonardo.mariani@unimi.it.
Mattia Piazza, Email: mattia.piazza@unimi.it.
Marta Del Medico, Email: marta.delmedico@asst-fbf-sacco.it.
Chiara Beatrice Cogliati, Email: chiara.cogliati@asst-fbf-sacco.it.
References
- 1.Han X, Fan Y, Alwalid O, Na L, Xi J, Mei Y, Yumin L, Yucun C, Jin J, Hanping W, Heshui S. Six-month follow-up chest CT findings after severe COVID-19 pneumonia. Radiology. 2021;299:E177–E186. doi: 10.1148/RADIOL.2021203153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Russo G, Flor N, Casella F, Ippolito S, Leidi F, Casazza G, Radovanovic D, Vezzulli F, Santus P, Cogliati C. Lung ultrasound in the follow-up of severe COVID-19 pneumonia: six months evaluation and comparison with CT. Intern Emer Med. 2022 doi: 10.1007/s11739-022-03084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Han X, Fan Y, Alwalid O, Zhang X, Jia X, Zheng Y, Shi H. Fibrotic interstitial lung abnormalities at 1-year follow-up CT after severe COVID-19. Radiology. 2021;301:E438–440. doi: 10.1148/radiol.2021210972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faverio P, Luppi F, Rebora P, D’Andrea G, Stainer A, Busnelli S, et al. One-year pulmonary impairment after severe COVID-19: a prospective, multicenter follow-up study. Respir Res. 2022;23:65. doi: 10.1186/s12931-022-01994-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wells AU, Devaraj A. Residual lung disease at six-month follow-up CT after COVID-19: clinical significance is a key issue. Radiology. 2021;301(2):E406–408. doi: 10.1148/radiol.2021211284. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.