Abstract
The homeless population in the United States is rapidly aging, with a parallel increase in Alzheimer’s disease and related dementia (ADRD). During an evolving pandemic that jeopardizes employment and housing, assessing the relationship between ADRD and homelessness is critical since the latter is potentially intervenable. The objective of this study is to review the literature and determine whether there is an association between homelessness and dementia risk. A systematic review of existing studies was conducted through PubMED, SCOPUS, and EMBASE among others. Of the 228 results found, nine met inclusion criteria. Homeless studies mainly centered on veteran populations (n = 6/9). There is a complex relationship suggesting homelessness as a risk for and consequence of ADRD but also co-occurrence with psychiatric disorders, substance abuse, and traumatic injuries. Future studies should employ enumeration surveys with modular longitudinal tracking and measure social determinants of health, discrimination, chronic stress, and mood disorders.
Keywords: homeless, Alzheimer disease, dementia, older adults, housing, risk factor
Introduction
The United States (US) population is aging rapidly, with over 10,000 adults turning 65 years of age daily (AARP International, 2021). By 2030, 21% of Americans will be 65 years or older. The population will also become more diverse with projected increases among Black (13.3%–15%), Hispanics/Latinx (17.8%–27.5%), and Asian (5.7–9.1%) people by 2060 (Vespa et al., 2018). Conversely, there will also be a decrease in non-Hispanic white people (76.9%–68.0%). Age-related changes in cognitive functioning, motor, and sensory systems may lead to a greater risk for chronic diseases. After age 45, the risk of arthritis, asthma, cancer, coronary heart disease, diabetes, kidney disease, and stroke steadily increase over time (Raghupathi & Raghupathi, 2018). Due to structural and social determinants, racialized and ethnic groups are more susceptible to chronic illnesses (Bailey et al., 2017; Glymour & Manly, 2008), which is a growing concern when considering the increasing diversity of the older adult population. However, these chronic illnesses are far more prevalent and understudied in the homeless population.
Homelessness is a chronic, systemic, and societal issue that affects over half a million adults and children on any given night in the US. The Department of Housing and Urban Development (HUD) defines homelessness as a complex situation where persons are living in places unfit for human shelter, people who are unstably housed or in transitional housing (including children and families), and people fleeing domestic violence (Anonymous, n.d) (42 U.S.C. § 11302). It is an understudied topic that warrants more attention, especially when considering the changing dynamics of the homeless population.
Homelessness has steadily increased in prevalence in the US over the past few decades. The Point-in-Time count (PIT) is an annual event required by HUD conducted at the end of January by Continuum-of-Care agencies (non-profits and state/local governments who receive federal funds from the McKinney-Vento Homeless Assistance grants). Outreach workers canvas areas of their communities to estimate the total number of those affected by homelessness in their neighborhoods and the resulting compiled data is the PIT count. The 2020 PIT count provided by the HUD reflected an increase of 2.2% in homelessness from 2019 to date with approximately 580,000 experiencing homelessness at that given time (United States Interagency Council on Homelessness, 2021). Approximately 18 per 10,000 individuals in the US at any given moment are experiencing homelessness.
On average, persons who experience homelessness have a life expectancy of 50 years, which is 20 years less than the life expectancy of housed individuals (Romaszko et al., 2017). The 2020 Annual Homeless Assessment Report to Congress indicated that a disproportionate percentage of the homeless population are from racialized and minoritized groups, with 40% self-identifying as Black and another 25% identifying as Hispanic/Latinx (Henry et al., 2021). Such groups are already disproportionately impacted by the COVID-19 pandemic (Webb Hooper et al., 2020). The pandemic-induced recession led to escalating unemployment and housing insecurity in many of these racialized and minoritized groups. With intersecting structural and social determinants at play, chronic homelessness is projected to increase by 49% over the next four years (Flaming et al., 2021).
Homeless persons are also more likely to lack health insurance, which may result in increased utilization of the emergency department (Garrett, 2012). The homeless population often falls under the categories of “frequent users” (more than four visits per year) and “superusers” (more than 20 visits per year) (Ku et al., 2014). While further research needs to be conducted on the unique experience of homelessness, it is evident that more public policy needs to be implemented to provide access to care for unhoused persons.
The number of homeless older adults, primarily male, has grown from 22.9% in 2007 to 33.8% in 2017 (Joint Center for Housing Studies, 2019). The growing number of older individuals from racialized and minoritized groups combined with their overrepresentation in the homeless demographic is a critical public health issue given the complexities associated with health disparities, life expectancy, and access to essential care services. Older homeless adults are also more likely to be admitted to the hospital with acute conditions, receive a delayed diagnosis due to infrequent access, and experience greater severity of symptoms from chronic illnesses such as cognitive impairment (People I. of M (US) C on HC for H, 1988). A recent scoping review examined the relationship between homelessness and cognitive impairment in several countries and found that risk factors for homelessness were greater with the presence of cognitive impairment (Stone et al., 2019).
Alzheimer’s disease and related dementia (ADRD) is an umbrella that encompasses a number of the most common neurodegenerative diseases in the brain that present with impaired memory, thought processes, and functioning. Alzheimer’s disease alone is projected to grow in the US to 12.7 million affected by 2050, compared to 6.2 million in 2021 (Alzheimer’s Association, 2021). Many factors from every stage of life increase the chance of developing dementia later in life. A prominent risk factor in early life (<45 years) relates to a lack of education or attending a segregated school; in midlife, the highest risk factors are hearing loss and residential segregation, and in late life, the highest risk factor is depression (Livingston et al., 2020; Caunca et al., 2020; Peterson et al., 2021). Understanding ADRD prevalence in homeless populations is incredibly challenging due to diagnostics inaccessibility and limited or no access to specialties like neurology and/or neuropsychology (White & Newman, 2015). Additionally, a lack of follow-up due to transient characteristics of the population and a higher prevalence of comorbid mental health disorders (e.g., depression, anxiety, PTSD) and substance abuse may further complicate a timely diagnosis (Gicas et al., 2020).
The purpose of this systematic review is to examine the extant literature surrounding homelessness and ADRD and review the evidence of dementia prevalence among those who are currently or have been homeless within the US.
Methods
Literature Search Strategy
This study utilized the PICO (Population, Intervention, Comparison, Outcome) framework to structure the systematic review. The primary interest centered on homelessness within the US context due to the unique social and healthcare systems that differ from other countries. This population focused on older adults due to their increasing representation in the homeless people over the last few decades. The primary focus of this study sought to investigate relationships and associations between ADRD and homelessness rather than the effect of an intervention. Articles that focused on ADRD were included in a broader exploration of comorbidities. While mild cognitive impairment (MCI) may progress to dementia since it may arise from multiple conditions (i.e., injury, illness), it is not a dementia diagnosis, so the review focused on ADRD. Published abstracts were not included in the review.
The published literature was searched using strategies created by a medical librarian in consultation with the authors for the concepts of homeless persons, dementia, and Alzheimer’s disease. These strategies were established using a combination of standardized terms and keywords. They were implemented in PubMed/MEDLINE (1946-), EMBASE (1947-), SCOPUS (1823-), The Web of Science Core Collection (WOS, 1900-), The Cochrane Library, and Clinicaltrials.gov from the inception of each database through October 8, 2021. Results were limited to the English language with database-supplied filters. An additional snowball/hand search was conducted via Google Scholar for any additional publications that may have been missed due to recency and/or availability. All searches were completed in October 2021 (see supplemental material for search strategy).
Inclusion and Exclusion Criteria
Study titles and abstracts were screened for specific criteria. They were excluded if (1) there was no reference to Alzheimer’s disease or related dementia in the study, (2) the focus of the article was outside of the US, (3) a published abstract, a white paper, a book chapter, a clinical trial, a commentary, editorial, or a position paper, (4) did not focus homelessness in the US (5) the study was published before 1991 (including MCI), (6) was a duplicate, or (7) focused on groups younger than 18 years of age.
Data Extraction and Synthesis
Duplicate citations were removed before extraction from the various databases and indices. The results were exported to the Endnote X9 reference manager and an Excel file. The studies were analyzed and filtered independently by two reviewers using the inclusion and exclusion criteria provided in section 2.2. A screen was conducted to separate the studies into four separate thematic groups: (1) both homelessness and ADRD were not identified in the abstract, (2) homelessness was identified with no mention of ADRD, (3) studies that focused on homelessness with general comorbidities, typically with dementia as a covariate, (4) a study on homelessness with ADRD being the primary focus of the study. Two reviewers completed the screenings independently. Any differences in the screening were discussed and reconciled by a third reviewer. The remaining references were read and examined for further relevancy to the study’s purpose and included in the review.
Results
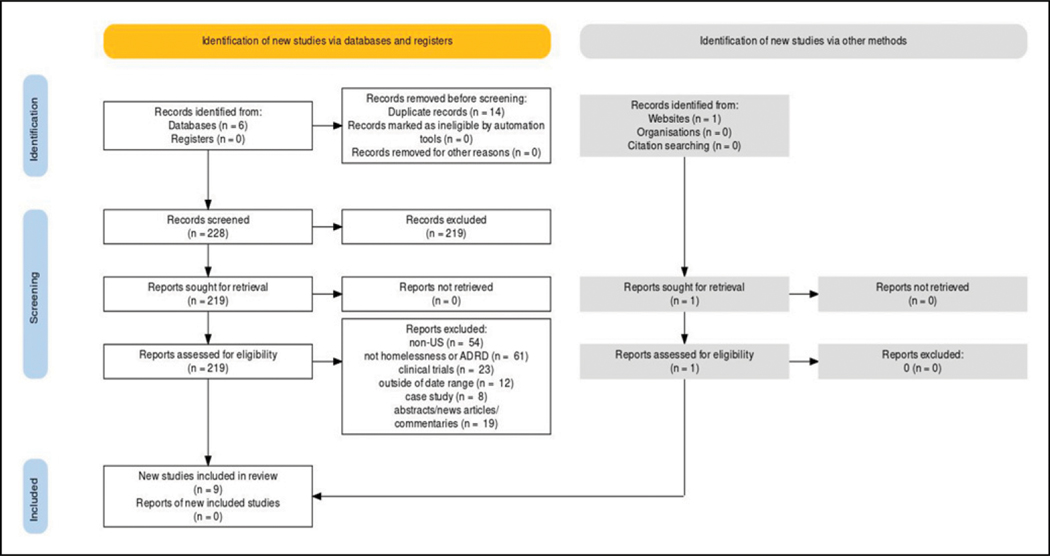
Across the databases queried, the search yielded 228 results. Following the implementation of the inclusion/exclusion criteria to filter the studies returned, nine unique studies remained for inclusion post-screening. Of the excluded citations (219), 54 included studies that were non US-based populations, 61 included older adults without focusing on homelessness or ADRD, 23 were clinical trials, 12 were outside of the specified date range, 8 were case studies, 14 were duplicates, and 19 were published abstracts (e.g. conference), news articles, or commentaries (Figure 1).
Figure 1.
PRISMA flow diagram of studies included in the review.
Of the nine studies retrieved and screened, all focused on homelessness in the US and ADRD, with dementia being screened as a part of a comprehensive catalog of comorbidities and socioeconomic status (Table 1). Most of the included studies (n = 6) focused on homeless veterans; these studies often provided longitudinal data with a more modest sample size relative to non-veteran studies by comparing homeless veterans to non-homeless veterans and the subsequent associations to neurologic deficits.
Table 1.
Publications Included in Systematic Review.
| First Author (Year) | Purpose/Aim | Outcome/Assessment | N/ Age | Notable Findings |
|---|---|---|---|---|
| Keigher and Green blatt (1992) | To examine factors that lead to homelessness and shelter placement of seniors | Dementia/SPMSQ (Short Portable Mental Status Questionnaire) | 1 15/NA | Statistically significant difference found in mean dementia score between “Ever homeless” and “never homeless” groups. Black elderly are overrepresented in housing emergencies |
| Uryu et al. (2010) | To describe the neuropathology of subjects that often include homeless patients | AD/FTLD tauopathies/post-mortem brain dissection | 100/50.5 | Significant burden of AD pathology in cohort examined by medical examiner in the >65 yo group, consistent with diagnoses of AD or FTLD |
| Sajatovic et al. (2006) | To examine the prevalence of comorbidities such as PTSD, SUD, and dementia in a Veterans Health Administration database | Dementia, PTSD, SUD/diagnosis found in VA database | 16330/70.0 | Homelessness was more common in individuals with comorbid BPD and substance abuse (13.2% vs. 2%). No relationship seen between comorbid BPD and dementia with homelessness |
| Piña-Escudero et al. (2020) | Examining the relationship between homelessness and neurodegenerative diseases of the brain | Neurodegenerative diseases of the brain (AD, FTLD, etc.)/prior diagnosis in VA records | 13/59 (median) | Risk of homelessness is elevated in areas with poor social support when combined with early neurodegenerative diseases that lead to dementia. New propensity towards being homeless after a NDDB diagnosis |
| Bennett et al. (2009) | Determining characteristics of HIV-positive patients treated at a psychiatric emergency department | Dementia/diagnosed in claims data | (HIV+) 1 178/38.97 (HIV-) 57,123/38.78 | HIV-positive patients treated at psych ED were more likely to have dementia (2% vs. 1.1%) and more likely to be homeless (OR = 1.33, Cl= 1.08–1.64) and have SUD (OR = 1.4). HIV-positive odds risk of dementia was 3.0 (95% Cl = 1.8–5.1), most robust statistical finding in the study with high study n of 28,817 individual patients or 58,301 visits |
| Gonzalez et al. (2001) | Determining neuropsychological functioning of homeless patients via multiple screenings methods | Neuropsychological impairment/MMSE and Abbreviated Halston-Reitan Test Battery | 60/39.8 | Average Impairment Index (All) was above the impairment threshold of 1.55 at 2.0 across the entire group from ages 19–61 −80% of the cohort was considered neurologically impaired. Impairment was extremely common and not attributed to a specific medical history. |
| Jutkowitz et al. (2019) | To understand the use of nursing homes among veterans with comorbidities and at-risk for homelessness | Dementia/diagnosis in VA records | Homeless 3355/62.5 At-Risk 16264/75.8 Housed 64884/75.3 | Cross Cross sectional study. Homeless veterans were younger upon admission and were more likely to be diagnosed with dementia (ARR 1.14; 95% Cl = 1.04–1.25) as well as alcohol use disorder (ARR 2.18; 95% Cl = 2.05–2.31). Homeless veterans were more likely to be African American |
| Jutkowitz et al. (2021a) | Determining incidence of homelessness amongst American Veterans diagnosed with ADRDs | ADRD/diagnosis in VA records | 383,478/78.55 | Homeless veterans with an ADRD diagnosis were significantly younger (63.70 vs. 78.67, p < .001), more likely to be Black (Hazard rate = 1.67, Cl = 1.52–1.82 vs. White counterparts), and more likely to be single. They were also more likely to be comorbid with SUD, depression, hypertension, and other comorbidities than stably housed veterans |
| Jutkowitz et al. (2021b) | To determine ADRD prevalence in aging veterans with housing insecurity (homelessness or at-risk) | ADRD/diagnosis in VA records | 6,580,126 Homeless ADRD: 7363/64.05 At-risk ADRD: 13,667/76.96 Stably housed ADRD: 190,733/76.73 | Retrospective chart review using claims data from VA-treated homeless, at-risk, and stably housed veterans. Homeless prevalence of ADRDs was 3.66%, at-risk prevalence was 13.48%, and stably housed prevalence was 3.06%. ARR, respectively, was 1.58 (95% Cl 1.51–1.66), and 2.98 (95% Cl 2.81–3.16). Homeless and at-risk veterans with ADRD diagnoses were less likely to be White, more likely to be unmarried, and less likely to be in a rural area than their stably housed counterparts |
Characteristics of Homeless Participants
Homelessness was defined differently across the cadre of studies in this systematic review. Studies that used claims data defined it as a participant assigned using the International Classification of Diseases (ICD) record for homelessness in their database. The studies that used non-claims data (e.g., surveys, descriptive, n = 3) adopted the definition of homelessness akin to that provided by HUD. The HUD definition includes traditionally acknowledged homelessness and individuals residing in transitional housing. The studies provided valuable data on the demographics of the homeless population seen. Jutkowitz et al. (2021a) demonstrated that homeless veterans receiving an ADRD diagnosis were significantly likely to be younger than their stably housed counterparts. Keigher and colleagues (1992) also established that homeless patients were significantly more likely to be Black relative to the larger population. This finding was reiterated by Jutkowitz et al. (2019, 2021a, 2021b) in homeless veteran populations. They also found that homeless veterans upon admission to a nursing home were younger (62.5 years vs. 75.3 years) and more likely to present with an alcohol abuse disorder (ARR = 2.18; 95% CI = 2.05–2.31) or drug use disorder (ARR = 3.03; 95% CI = 2.74–3.33), along with a non-specified mental health disorder diagnosis (ARR = 1.49; 95% CI = 1.45–1.54)
Dementia in Homeless Participants
Piña-Escudero et al. (2020) noted that there was a high risk for patients to become homeless after receiving a neurodegenerative disease diagnosis (primarily Alzheimer’s disease as well as various forms of frontotemporal lobar dementia [FTLD]). Sajatovic and colleagues (2006) noted that geriatric veterans with borderline personality disorder and comorbid substance abuse were more likely to be homeless (13.2%) but noted no relationship between borderline personality disorder and comorbid dementia with homelessness. Uryu and colleagues (2010) noted that 91% of the cases over the age of 65 years old presented with neurodegenerative disease pathology (typically Alzheimer’s disease or FTLD-indicative biomarkers, though no formal diagnosis was offered due to a lack of clinical data), and 13% of the cohort presented with tau pathology. They identified 13 patients with significant neurodegenerative findings—one was considered traditionally homeless, and nine others were found to be living in squalid surroundings or suffered from malnutrition.
Assessment of Dementia and Findings
Dementia was primarily assessed through prior diagnosis by a physician (non-specified), which was established by an ICD-10 code (n = 6 studies). Studies with a physician diagnosis primarily used claims data from the national Veterans Administration (VA) database, containing information on healthcare visits, diagnosis, and treatment made by those who utilized the VA services. Jutkowitz et al. (2019) established that homeless veterans were younger upon admission to skilled nursing facilities and were more likely to have dementia than their stably housed counterparts (adjusted risk ratio (ARR) = 1.14, 95% CI = 1.04–1.25). In another study (Jutkowitz et al., 2021b), it was established that the risk for dementia in all homeless veterans treated at VA facilities was 1.58 (CI = 1.51–1.66), while the ARR in at-risk veterans was 2.98 (95% CI = 2.81–3.16), compared to stably housed counterparts. Bennett and colleagues (2009) did not use a VA database to establish dementia. Rather, they used claims data from a public hospital (Harborview Medical Center), where clinicians assigned a diagnosis of dementia (and other psychiatric disorders) to patients using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). This study found that human immunodeficiency virus (HIV)-positive patients were more likely to be homeless (odds risk (OR) = 1.33, 95% CI = 1.08–1.64) and far more likely to have dementia (OR = 3.0, 95% CI = 1.8–5.1).
An article by Uryu and colleagues (2010) presented a unique method of establishing AD characteristics by providing data found in post-mortem brain dissections. Uryu and colleagues (2010) used biomarkers traditionally associated with ADRDs, including tau pathology, alpha-synuclein pathology, and TDP-43 pathology, when examining the subjects post-mortem. They found that 13% of their cohort presented with significant tau pathology, consistent with progressive neurodegenerative disease.
Studies that were unable to secure a physician diagnosis in homeless populations did not offer a formal diagnosis and instead drew conclusions based on dementia/neuropsychological impairment “scores” based on cut-offs (n = 2 studies). Two studies used mental status screening questionnaires, including the Short Portable Mental Status Questionnaire (SPMSQ), Mini-Mental State Exam (MMSE), and the Abbreviated Halston-Reitan Battery (AHRB). Gonzalez et al. (2001) used the MMSE and the AHRB to determine neuropsychological impairment. An average impairment rating was used based on the AHRB; the mean impairment rating was 2.0 (standard deviation (SD) = 0.6), while impairment begins over a score of 1.55; this classified 80% of the cohort to be impaired, while the MMSE average of 26.4 (SD = 2.9) was only able to type 35% of participants as impaired. Keigher and Greenblatt (1992) used the SPSMQ to create a dementia “score,” which indicated that those who were in the “Ever Homeless” group who were tested (n = 30) had a higher mean dementia score than those who were in the “Never Homeless” group (n = 13, p < .01).
Discussion
This systematic review sought to characterize the extant literature encompassing homelessness and ADRD. Nine studies met inclusion criteria, either exploring this relationship directly or through relationships with other diseases. Dementia was the most common disease investigated and was most often conducted in samples of veteran populations. Despite slight variances, the consensus surrounding these studies indicates a complex relationship where homelessness can be a risk factor for dementia, a consequence of dementia, and also co-vary with other chronic comorbidities. Some evidence suggests that earlier in life, homelessness can lead to neurodegeneration and increase dementia scores in some homeless adults. Other evidence suggests that a new onset of ADRD is likely to the risk of homelessness in older adults. Both homelessness and dementia have also been associated with traumatic brain injury, economic and socioeconomic deprivation, malnutrition, and mood disorders. These relationships indicate that critical exposure to homelessness is a risk for ADRD, and potentially future homelessness if diagnosed with ADRD. Such findings inspire further exploration of the role of structural and social determinants on risk factors for ADRD such as homelessness (Glymour & Manly, 2008).
The associations found in this systematic review draw important parallels to the pernicious effects of health disparities, including the role of structural and social determinants of health that racialized and minoritized populations encounter. The Alzheimer’s Association published a 2021 Special Report on AD inequities, noting that Black and Hispanic/Latinx Americans are disproportionately affected by AD relative to their population representation. These groups face higher perceived barriers to effective care and discrimination when seen by providers. As a result, it may be more challenging to establish a timely diagnosis of ADRD. Since these groups are also more likely to be homeless relative to their representation, this can lead to considerable delays in diagnosis and treatment, as well as a skewed prevalence of minoritized houseless individuals with neurodegenerative disease.
Additionally, Black Americans were consistently seen in these studies in disproportionately higher amounts in veteran and non-veteran homeless persons than their non-Hispanic white counterparts. Black adults are at risk for cardiovascular events and more likely to be at a greater risk of dementia (Carnethon et al., 2017). Furthermore, Piña-Escudero et al. (2020) found that the risk of homelessness induced by a neurodegenerative disease was elevated in areas with limited family support. This is increasingly more common in major urban areas, which face increased gentrification and unaffordable living costs that may split up families who seek more affordable places to live (Torres, 2020). Thus, earlier interventions to structural and social determinants—like healthcare access and homelessness—need to be implemented to reduce the risk of dementia in later life.
There were several limitations in the studies that were retrieved. The most common limitation replete in the non-veteran studies centered on limited longitudinal data due to patients being lost to follow-up. Given the transient nature of the homeless population, the lack of a stable domicile structure is an immutable issue that inevitably impacts longitudinal studies. As a result, we did not conduct a quality appraisal of the studies included in this review since most of the samples were from the homogenous VA system. Numerous external variables can and do rapidly change the housing situation of homeless people, requiring them to move. The veteran populations had a significant advantage in having access to physician health care and diagnostic resources, which allowed them to stay in the VA health database for follow-up. Given the nosological challenges with dementia subtypes, assessment via physician diagnosis may be the most robust method of establishing dementia as commonly used in VA-treated population studies (Kansagara & Freeman, 2010; Morris, 2000). Given the benefits of this infrastructure, this may explain why studies of homeless veterans were more common in this systematic review. Since the infrastructure of services provided by the VA is inaccessible to non-veterans, the extent of dementia impairment and mental disease cannot be systematically interrogated without concerted outreach and research on non-veteran homeless patients. Two studies on non-veteran homeless populations were diagnosed through questionnaires and self-reporting of symptoms, which is problematic in a population traditionally associated with altered mental states. Gonzalez et al. (2001) suggested that the MMSE was a poor marker of neuropsychological impairment, especially in homeless populations, and suggested using the Abbreviated Halston-Reitan Battery test instead, which detected neuropsychological impairment at a greater rate than the MMSE (80% vs. 35%). Another benefit is shorter than the Halston-Reitan Battery Test (1 hr vs. up to 3 hrs) and has approximately a 93% detection rate relative to the whole test (Golden, 1976). This is especially useful in houseless samples that often are unwilling to subject themselves to burdensome and extensive neuropsychological batteries. While the MMSE can be performed quickly, the screen may not capture the full extent of neuropsychological impairment. This can underestimate the true extent of disease and alter treatment plans. Another related limitation in the non-veteran populations was size; cohorts were under 150 people in all non-claims data studies. The self-reported data obtained on life circumstances in Keigher and Greenblatt (1992) provides valuable insight into the subjective reality. Very few mixed methodological studies have examined objective and subjective data on ADRD risk and outcomes.
The annual Point-in-Time Count has been the standard for identifying unsheltered homelessness. However, it is inherently unable to capture the full extent of unsheltered homelessness due to there being unhoused folks in areas that may be inaccessible or dangerous to reach for canvas workers. The COVID-19 pandemic has further compounded this issue since more homeless persons will go uncounted, as many counties have halted their counts due to the risk of disease transmission. Unfortunately, this will prevent a comprehensive understanding of the pandemic’s impact on homelessness across the country until a complete count can be conducted (Fessler, 2021). The US Census is predicated on surveying persons who have a physical address; as a result, our primary source of information on homelessness is from the Point-in-Time count. Optimistically, counties were preparing to resume the Point-in-Time Count in late January 2022, which will provide much-needed information on the impact the pandemic has had on our homeless population.
Since cognitive impairment, mental illness, and addiction are salient, proximal constructs that interact with homelessness, police officers are first responders in the front in dealing with complex situations. A low cost method could target education workshop or supplement simulation training for police officers to help them deal with mental health situations to improve trust, violence de-escalation, and rapid triaging of health crisis to the appropriate health professionals. Given the challenges in accessing this underserved population using traditional assessments, implementing an alternative healthcare model could be a solution to increase access to healthcare in houseless people. Street medicine organizations deliver essential primary care services and housing resources to houseless patients in urban areas. This work is often conducted by volunteer clinicians and medically certified individuals and is often funded by donations and partnerships with non-profits and local/state governments. An example of such a program is Doctors Without Walls, a volunteer-run Santa Barbara-based organization that delivers healthcare to hundreds of homeless patients in the area. Often, homeless patients may seek an emergency room for essential primary care services. A tangible benefit of the broader implementation of similar programs includes reduced emergency care visits by homeless patients and increased success in gaining access to transitional/low-income housing. A retrospective study on dedicated homeless clinics found that they could successfully reduce emergency department (ED) utilization (Holmes et al., 2020). Continued research in this area would be beneficial for policymakers to understand the benefits provided by such organizations and make policies to support these organizations accordingly.
Future studies need to include homeless outreach to non-veteran populations and early prevention of ADRD. Many homeless individuals with altered mental status are treated akin to those with substance use disorders, which leads to underdiagnoses and delays in treatment for homeless patients with a risk of developing ADRD.
Supplementary Material
What This Paper Adds
This manuscript is the first systematic review that explicitly investigates the relationship between homelessness and Alzheimer’s disease and related dementia (ADRD) within the United States.
The results support a complex relationship between homelessness and ADRD where homelessness seems to be a risk factor for ADRD and accelerates decline but this relationship is modified by social forces.
There is a dearth of studies on non-veteran homeless populations regarding ADRD, highlighting the need for a more inclusive and concerted approach to the recruitment, enrollment, and retention of homeless adults.
Applications of Study Findings
In this review, we offer unique recommendations that can be applied to gerontological research and practice in older homeless populations. One example of this supports committing more funding and research towards Federally Qualified Health Centers and street medicine programs that primarily serve this population.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr. Babulal receives research support/grants from the National Institute of Health (NIH) and National Institute on Aging (NIA): R01AG056466, R01AG068183, R01AG067428, R01AG074302 and the BrightFocus Foundation: A2021142S. Dr. Adkins-Jackson receives research support from NIA: DP1AG069874.
Footnotes
Supplemental Material
Supplemental Material for this article is available online.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- AARP International (2021). The aging readiness and competitiveness report - third edition: Driving innovation in healthcare and wellness. 10.26419/int.00049.001 [DOI]
- Alzheimer’s Association (2021). Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 17(3), 327–406. 10.1002/alz.12328 [DOI] [PubMed] [Google Scholar]
- Anonymous. (n.d.). 42 U.S. Code § 11302—general definition of homeless individual. LII/Legal Information Institute. https://www.law.cornell.edu/uscode/text/42/11302 [Google Scholar]
- Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, & Bassett MT (2017). Structural racism and health inequities in the USA: Evidence and interventions. Lancet, 389(10077), 1453–1463. 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- Bennett WM, Joesch JM, Mazur M, & Roy-Byrne P. (2009). Characteristics of HIV-positive patients treated in a psychiatric emergency department. Psychiatric Services, 60(3), 398–401. 10.1176/ps.2009.60.3.398 [DOI] [PubMed] [Google Scholar]
- Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA, Willis M, & Yancy CW, American Heart Association Council on Epidemiology and Prevention, Council on Cardiovascular Disease in the Young, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, Council on Functional Genomics and Translational Biology, Stroke Council (2017). Cardiovascular health in African Americans: A scientific statement from the American Heart Association. Circulation, 136(21), e393–e423. 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- Caunca MR, Odden MC, Glymour MM, Elfassy T, Kershaw KN, Sidney S, Yaffe K, Launer L, & Zeki Al Hazzouri A. (2020). Association of racial residential segregation throughout young adulthood and cognitive performance in middle-aged participants in the cardia study. JAMA Neurology, 77(8), 1000. 10.1001/jamaneurol.2020.0860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fessler P. (2021, January 18). For many areas, count of homeless population is canceled, or delayed. NPR. https://www.npr.org/2021/01/18/957379320/for-many-areas-count-of-homeless-population-is-canceled-or-delayed
- Flaming D, Orlando A, Burns P, & Pickens S. (2021, January 21). Economic roundtable | Locked out. Economic Roundtable. https://economicrt.org/publication/locked-out/
- Garrett DG (2012). The business case for ending homelessness: Having a home improves health, reduces healthcare utilization and costs. Am Health Drug Benefits, 5(1), 17–19. [PMC free article] [PubMed] [Google Scholar]
- Gicas KM, Jones AA, Thornton AE, Petersson A, Livingston E, Waclawik K, Panenka WJ, Barr AM, Lang DJ, Vila-Rodriguez F, Leonova O, Procyshyn RM, Buchanan T, MacEwan GW, & Honer WG (2020). Cognitive decline and mortality in a community-based sample of homeless and precariously housed adults: 9-year prospective study. BJPsych Open, 6(2), e21. 10.1192/bjo.2020.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glymour MM, & Manly JJ (2008). Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychology Review, 18(3), 223–254. 10.1007/s11065-008-9064-z [DOI] [PubMed] [Google Scholar]
- Golden CJ (1976). The identification of brain damage by an abbreviated form of the Halstead-Reitan neuropsychological battery. Journal of Clinical Psychology, 32(4), 821–826. [DOI] [PubMed] [Google Scholar]
- Gonzalez EA, Dieter JN, Natale RA, & Tanner SL (2001). Neuropsychological evaluation of higher functioning homeless persons: A comparison of an abbreviated test battery to the mini-mental state exam. The Journal of Nervous and Mental Disease, 189(3), 176–181. 10.1097/00005053-200103000-00006 [DOI] [PubMed] [Google Scholar]
- Henry M, de Souza T, Roddey C, Gayen S, & Bednar T. (2021). 2020 Annual Homeless Assessment Report (AHAR) to Congress, Part 1. The U.S. Department of Housing and Urban Development. [Google Scholar]
- Holmes CT, Holmes KA, MacDonald A, Lonergan FR, Hunt JJ, Shaikh S, Cheeti R, D’Etienne JP, Zenarosa NR, & Wang H. (2020). Dedicated homeless clinics reduce inappropriate emergency department utilization. Journal of the American College of Emergency Physicians Open, 1(5), 829–836. 10.1002/emp2.12054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint Center for Housing Studies (2019). Housing America’s older adults 2019. Joint Center for Housing Studies of Harvard University. https://www.jchs.harvard.edu/sites/default/files/reports/files/Harvard_JCHS_Housing_Americas_Older_Adults_2019.pdf [Google Scholar]
- Jutkowitz E, DeVone F, Halladay C, Hooshyar D, Tsai J, & Rudolph JL (2021a). Incidence of Homelessness among veterans newly diagnosed with Alzheimer’s disease and related dementias. Rhode Island Medical Journal, 104(4), 20–25. [PMC free article] [PubMed] [Google Scholar]
- Jutkowitz E, Halladay C, McGeary J, O’Toole T, & Rudolph JL (2019). Homeless veterans in nursing homes: Care for complex medical, substance use, and social needs. Journal of the American Geriatrics Society, 67(8), 1707–1712. 10.1111/jgs.15993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jutkowitz E, Halladay C, Tsai J, Hooshyar D, Quach L, O’Toole T, & Rudolph JL (2021b). Prevalence of Alzheimer’s disease and related dementias among veterans experiencing housing insecurity. Alzheimer’s & Dementia. 10.1002/alz.12476 [DOI] [PMC free article] [PubMed]
- Kansagara D, & Freeman M. (2010). A systematic evidence review of the signs and symptoms of dementia and brief cognitive tests available in VA. Department of Veterans Affairs (US). [PubMed] [Google Scholar]
- Keigher SM, & Greenblatt S. (1992). Housing emergencies and the etiology of homelessness among the urban elderly. The Gerontologist, 32(4), 457–465. 10.1093/geront/32.4.457 [DOI] [PubMed] [Google Scholar]
- Ku BS, Fields JM, Santana A, Wasserman D, Borman L, & Scott KC (2014). The urban homeless: Super-users of the emergency department. Population Health Management, 17(6), 366–371. 10.1089/pop.2013.0118 [DOI] [PubMed] [Google Scholar]
- Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C, Costafreda SG, Dias A, Fox N, Gitlin LN, Howard R, Kales HC, Kivimäki M, Larson EB, Ogunniyi A, & Mukadam N. (2020). Dementia prevention, intervention, and care: 2020 Report of the Lancet Commission. Lancet, 396(10248), 413–446. 10.1016/S0140-6736(20)30367-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JC (2000). The nosology of dementia. Neurologic Clinics, 18(4), 773–788. 10.1016/s0733-8619(05)70225-5 [DOI] [PubMed] [Google Scholar]
- People I. of M (US) C on HC for H (1988). Health problems of homeless people. National Academies Press. [Google Scholar]
- Peterson RL, George KM, Barnes LL, Gilsanz P, Mayeda ER, Glymour MM, Mungas D, & Whitmer RA (2021). Association of timing of school desegregation in the United States with late-life cognition in the study of healthy aging among Black individuals in the STAR cohort. JAMA Netw Open, 4(10), Article e2129052. 10.1001/jamanetworkopen.2021.29052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piña-Escudero SD, López L, Sriram S, Longoria Ibarrola EM, Miller B, & Lanata S. (2020). Neurodegenerative disease and the experience of homelessness. Frontiers in Neurology, 11(1876), 562218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghupathi W, & Raghupathi V. (2018). An empirical study of chronic diseases in the United States: A visual analytics approach to public health. International Journal of Environmental Research and Public Health, 15(3), 431. 10.3390/2Fijerph15030431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romaszko J, Cymes I, Dragańska E, Kuchta R, & Glińska-Lewczuk K. (2017). Mortality among the homeless: Causes and meteorological relationships. Plos One, 12(12), Article e0189938. 10.1371/journal.pone.0189938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajatovic M, Blow FC, & Ignacio RV (2006). Psychiatric comorbidity in older adults with bipolar disorder. International Journal of Geriatric Psychiatry: A Journal of the Psychiatry of Late Life and Allied Sciences, 21(6), 582–587. 10.1002/gps.1527 [DOI] [PubMed] [Google Scholar]
- Stone B, Dowling S, & Cameron A. (2019). Cognitive impairment and homelessness: A scoping review. Health & Social Care in the Community, 27(4), e125–e142. 10.1111/2Fhsc.12682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres S. (2020). “For a younger crowd”: Place, belonging, and exclusion among older adults facing neighborhood change. Qualitative Sociology, 43(1), 1–20. 10.1007/s11133-019-09441-z [DOI] [Google Scholar]
- United States Interagency Council on Homelessness. (2021, July 18). Key findings of 2020 point-in-time count. https://www.usich.gov/tools-for-action/2020-point-in-time-count/
- Uryu K, Haddix T, Robinson J, Nakashima-Yasuda H, Lee VMY, & Trojanowski JQ (2010). Burden of neurodegenerative diseases in a cohort of medical examiner subjects. Journal of Forensic Sciences, 55(3), 642–645. 10.1111/j.1556-4029.2010.01347.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vespa J, Medina L, & Armstrong D. (2018) Demographic turning points for the United States: Population projections for 2020 to 2060. U.S. Census Bureau. [Google Scholar]
- Webb Hooper M, Nápoles AM, & Pérez-Stable EJ (2020). COVID-19 and racial/ethnic disparities. JAMA, 323(24), 2466–2467. http://jamanetwork.com/article.aspx?doi=10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White BM, & Newman SD (2015). Access to primary care services among the homeless: A synthesis of the literature using the equity of access to medical care framework. Journal of Primary Care & Community Health, 6(2), 77–87. 10.1177/2150131914556122 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.