Background:
Losing postural control ability and related injuries are of particular concern for elders living in the nursing home (NH). The Otago Exercise Program (OEP) is a multimodal exercise training program initially designed as an individually tailored home exercise for community-dwelling elders, but whether its movement characteristics and exercise intensity meet NH elders’ needs still needs to be clarified. This study aimed to determine the effects of the OEP in enhancing postural control ability among elders in the NH.
Methods:
A systematic literature search of English language databases (Cochrane Library, PubMed, EMBASE, CINAHL, and Web of Science) and Chinese language databases (China National Knowledge Infrastructure, Wanfang, and Chongqing VIP) until 15 April 2022 were performed by 2 reviewers on searching randomized controlled trial (RCT) and non-RCT. A meta-analysis was performed using Review Manager 5.3 software. Continuous data were expressed as mean difference (MD) with 95% confidence intervals (95% CI). Dichotomous data were presented as risk ratios (RRs) with 95% CI. Study methodological quality was assessed according to the Cochrane Handbook for Systematic Reviews of Interventions for RCTs and Risk Of Bias In Non-randomized Studies-of Interventions for non-RCTs by 3 reviewers.
Results:
Nine studies with 546 participants were included in this review. Two hundred and sixty-nine participants received OEP, and 277 only had conventional exercise training. Compared to the conventional exercise training group, the NH elders in the OEP group have considerably decreased in fall risk (MD = −0.84; 95% CI = −1.17, −0.51; P < .00001) and positively increased in postural balance (MD = 5.55; 95% CI = 3.60, 7.50; P < .00001), functional mobility in short-distance (MD = −6.39; 95% CI = −8.07, −4.70; P < .00001), lower-limb muscle strength (MD = 4.32; 95% CI = 3.71, 4.93; P < .00001), and health status (risk ratio = 0.35; 95% CI = 0.18, 0.66; P = .001).
Conclusions:
Current evidence suggests that OEP is practical and feasible in NH. The nursing personnel can receive sufficient support for maintaining and enhancing these elders’ postural control ability, especially during the COVID-19 pandemic.
Keywords: elders, fall risk, meta-analysis, NH, OEP, postural control ability
1. Introduction
The trend of aging is becoming increasingly severe, and a proportional increase in elders has been observed in virtually all nations and regions globally.[1] Deficiencies in balance and muscle strength are a common manifestation of a reduction in postural control ability, and 28% to 35% of elders experience falls each year, contributing to health deterioration and an increase in hospitalization probability.[2,3] Nursing home (NH) has relatively closed spaces, limiting daily activity intensity for the elderly, who may spend almost 79% of their day sedentary, with only 1% moderate-to-vigorous physical activity, causing negative influences on mobility and aerobic endurance.[4,5] Loss of postural control ability and related injuries are of particular concern for elders living in NHs. A previous study verified that agility and balance were lower in elders living in NHs than in those dwelling within the community.[6] The reduced postural control ability could induce increased fall rates making elders more susceptible to cause injuries and long-term disabilities.[3] Additionally, the COVID-19 pandemic further exacerbated the social isolation of the elderly, decreasing their likelihood of engaging in physical activity and maintaining motor function,[7] which is especially serious for those living in NHs.
Many studies have demonstrated that exercise is the most effective and convenient method to minimize adverse body changes.[8,9] However, those living in NHs have a greater need for reliable and scientific exercise training programs due to their poor health,[3] and there is still a need for an efficient and systematic exercise program for this population.
The Otago Exercise Program (OEP) is a multimodal exercise training program initially designed as an individually tailored home exercise program for community-dwelling elders and has been proven to be an effective evidence-based exercise program to enhance postural control and minimize risk of falls through improved muscle strength, balance, and endurance.[10,11] Some scholars consider the OEP likely to be accepted by elders in NHs and that the program is readily conducive to popularization.[12] However, only the effect of the OEP was analyzed for community-dwelling elders from an evidence-based level; whether the movement characteristics and exercise intensity meet the needs of NH elders still needs to be clarified and investigated through a thorough review and meta-analysis.[13] We aimed to conduct a systematic review and meta-analysis to determine whether the OEP can effectively enhance the postural control ability of the elderly living in NHs by comparing the changes in relevant indices between baseline and after the intervention, identify the feasibility of conducting the OEP in NHs, and provide theoretical references to nursing personnel.
2. Materials and methods
2.1. Literature search
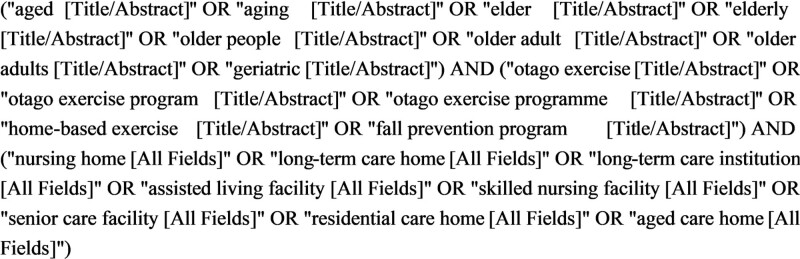
This review and meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Two reviewers (L.K. and X.Z.) independently searched for studies published in 5 English language databases (Cochrane Library, PubMed, EMBASE, CINAHL, and Web of Science) and 3 Chinese language databases (China National Knowledge Infrastructure, Wanfang, and Chongqing VIP) from establishment to April 15, 2022. Search terms included combinations of variants for the keyword “elders” and different terms for the Otago exercise and NHs. The search strategy for PubMed is shown in Figure 1.
Figure 1.
Search strategy of PubMed.
2.2. Eligibility criteria and study selection
The selection criteria were as follows: participants aged ≥ 65 years; the study was conducted in a NH or a similar institution; the exercise training program was the OEP; and the full text could be accessed. We excluded studies conducted in communities; those presented in reviews, case reports, case series studies; and those with inadequate information.
2.3. Data extraction and outcome measures
All search results were exported to EndNote X9 and a duplication check was conducted. Two reviewers (L.K. and X.Z.) then independently evaluated studies to ensure that each met the selection criteria. Titles and abstracts were scanned, and the inclusion criteria were confirmed through a full-text review. The data on posture control ability and relevant changes in the 2 groups after undergoing the OEP or conventional exercise intervention were then extracted by the reviewers. The data of the included studies shown by median (interquartile range) were processed and transferred to mean ± standard deviation for the follow-up meta-analysis.[14]
2.4. Assessment for risk of bias
The methodological quality of the included studies was evaluated by 2 reviewers (L.K. and X.Z.) following the criteria described in the Cochrane Handbook for Systematic Reviews of Interventions for randomized controlled trials (RCT), and Risk Of Bias in Non-Randomized Studies of Interventions was used for non-RCTs.[15,16] Disagreement between the 2 reviewers was resolved by a third reviewer (X.Z.) and a consensus was reached.
2.5. Synthesis methods
The extracted data were statistically analyzed using Review Management Software 5.3. A heterogeneity test was performed using the I2 statistic for each analysis. When the I2 value was <50%, the pooled data were considered homogeneous and a fixed-effects model was used. If the I2 value was ≥50%, the pooled data were considered to have substantial heterogeneity and the random-effects model was used. Weighted mean differences with a 95% confidence interval (CI) were used for continuous outcomes with the same or different measurement units. The risk ratio with 95% CI was used for qualitative data to evaluate the total effective rate. P value <.05 was considered to indicate statistical significance. The meta-analysis was performed only when two or more studies were compared for each survey item. Publication bias was assessed visually using a funnel plot showing the relationship between the sample size and effect size. Egger’s test was performed using R software 4.2.0, and an alpha of 0.05 was used as the cutoff for significant publication bias.
2.6. Ethics and dissemination
This study was a systematic review and meta-analysis, included secondary data processing of previously published studies, and there was no requirement for ethical approval on account of the data being extracted from published literature, which does not involve patient and animal privacy.
3. Results
3.1. Study selection and characteristics
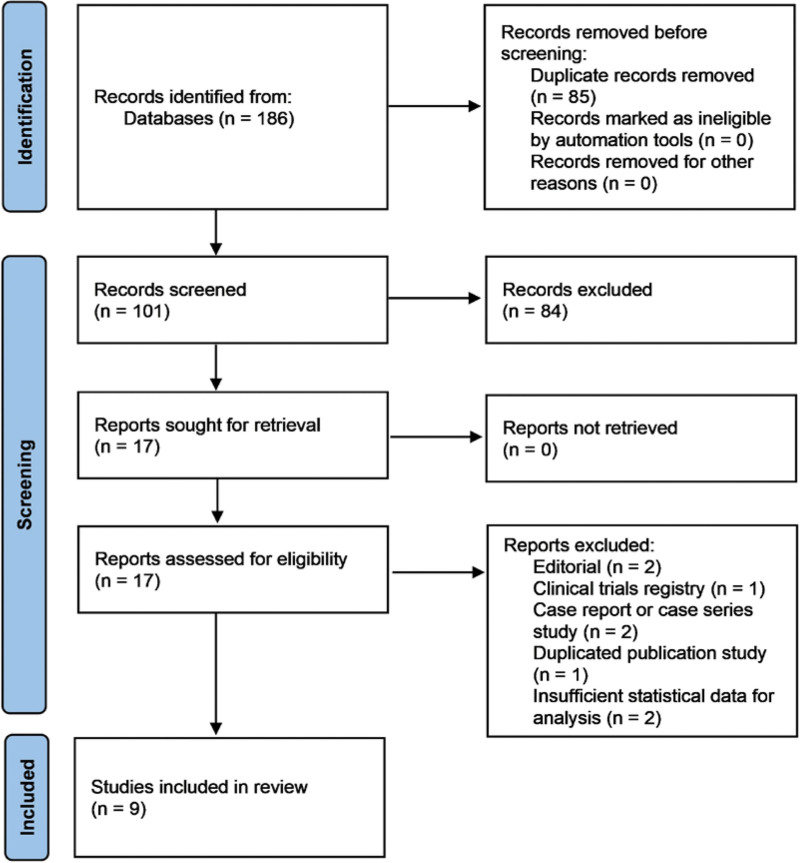
A total of 184 studies were searched using the search strategy, and nine were finally selected. Our Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram is shown in Figure 2.
Figure 2.
Process of studies selection flow chart.
3.2. Study characteristics
We included 9 studies, with a total of 546 participants, including 269 participants allocated to the OEP group and 277 participants allocated to the control group, and only had conventional exercise training.[17–25] The characteristics of the included studies are presented in Table 1.
Table 1.
Characteristics of included studies.
| Study (year) | Written language | Type of study | Participants description (M ± SD) | Intervention form and intensity of the OEP | Duration | Measurement methods | |
|---|---|---|---|---|---|---|---|
| EG (N = 269) | CG (N = 277) | ||||||
| Kocic et al (2018)[17] | English | RCT | N = 27 Age = 77.5 ± 6.9 | N = 33 Age = 78.7 ± 7.3 | Part one: ≥40 min/3 d/wk, Part two: 30 min/≥2 d/wk | 3 mo | BBS TUG |
| Wang et al (2019)[18] | Chinese | Non-RCT | N = 35 Age = 85.0 ± 3.0 |
N = 41 Age = 84.6 ± 6.0 |
Part one: 40–60 min/≥2 d/wk Part two: 30 min/≥2 d/wk |
3 mo | TUG 30s-CST Number of frail elders |
| Cheng et al (2020)[19] | Chinese | Non-RCT | N = 10 Age = 84.7 ± 4.7 |
N = 10 Age = 81.4 ± 4.3 |
Part one + two: 45 min/3 d/wk | 6 mo | 30s-CST |
| Jahanpeyma et al (2020)[20] | English | RCT | N = 35 Age = 74.6 ± 5.9 |
N = 36 Age = 75.8 ± 4.5 |
Part one: 45 min/3 d/wk Part two: 30 min/3 d/wk |
3 mo | BBS 6MWT 30s-CST Number of falls |
| Chen et al (2021)[21] | English | RCT | N = 29 Age = 84.6 ± 4.2 |
N = 30 Age = 84.8 ± 5.4 |
Part one: 30 min/3 d/wk | 3 mo | BBS TUG |
| Knott et al (2021)[22] | English | Non-RCT | N = 30 Age = 87.3 ± 7.0 |
N = 29 Age = 87.6 ± 5.2 |
Part one + two: 30–45 min/2–3 d/wk | 1 y | Number of falls |
| García-Gollarte et al (2021) [23] | English | RCT | N = 39 Age = 86.0 ± 5.9 |
N = 34 Age = 87.3 ± 5.3 |
Part one + two: 45–60 min/3 d/wk | 6 mo | BBS TUG 6MWT |
| Zou et al (2022)[24] | English | Non-RCT | N = 29 Age = 85.2 ± 3.1 |
N = 28 Age = 85.8 ± 5.1 |
Part one: 40–60 min/≥2 d/wk Part two: 30 min/≥2 d/wk |
3 mo | TUG 30s-CST |
| Sahin et al (2022)[25] | English | RCT | N = 35 Age = 74.6 ± 5.9 |
N = 36 Age = 75.8 ± 4.5 |
Part one: 45 min/3 d/wk Part two: 30 min/3 d/wk |
3 mo | Number of frail elders |
30s-CST = 30-second Chair Stand Test, 6MWT = 6-minute walking test, BBS = Berg Balance Scale, CG = control group, EG = experimental group, M = mean, N = number of participants, RCT = randomized controlled trial, SD = standard deviation, TUG = Timed Up and Go test.
The OEP consists of 2 training parts. Part one consists of 22 exercises (5 warm-up movements, 5 strength training movements, and twelve balance training movements) and involves strengthening functions. Strength and balance training has 4 levels (A, B, C, and D) tailored to the elderly, which promote physical activity and inhibit functional decline from easy to difficult to accomplish.[24,25] The participants were allowed to start from their most suitable levels. Part two emphasizes walking training for a certain period, which is responsible to maintain daily activity. In the intervention form and intensity of the OEP, in 3 studies, the 2 parts were carried out sequentially on the same day, and the average training time was 45 minutes, 2 to 3 times per week.[19,22,23] In 5 studies, the elders completed part two at other times in 1 week after undergoing part one, and the training time ranged from 40 to 60 minutes, at least twice a week; the second part was 30 minutes, no less than twice a week.[17,18,20,24,25] One study only employed part one for a 30-minute intervention on 3 fixed days in 1 week.[21] Regarding the intervention duration, 6 studies were 3 months,[17,18,20,21,24,25] 2 studies were 6 months,[19,23] and one was 1 year.[22]
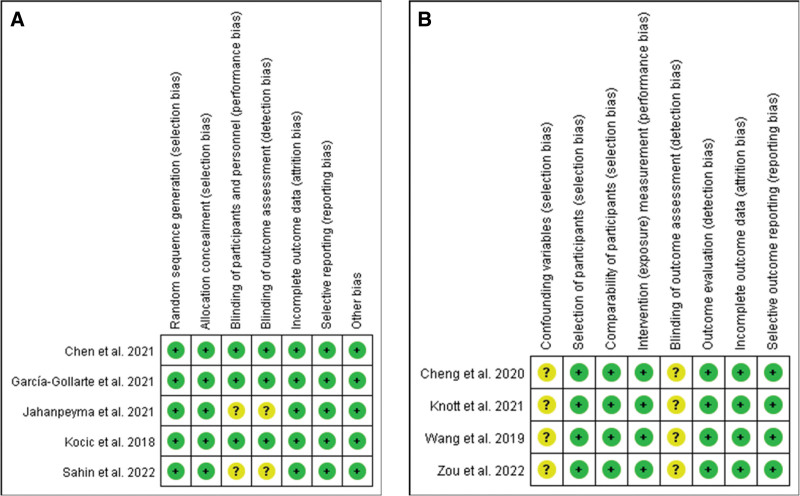
3.3. Risk of bias and level of evidence
All RCTs had a low risk of bias in random sequence generation and allocation concealment. Concerning blinding of participants and personnel, and blinding of outcome assessment, 3 studies had a low risk of bias, but Jahanpeyma et al[20] and Sahin et al[25] had an unclear risk of bias. Concerning incomplete outcome data, selective reporting data, and other bias categories, all studies had a low risk of bias (Fig. 3A). All non-RCTs had an unclear risk of bias in confounding variables and blinding of outcome assessment. In the selection and comparability of participants, intervention (exposure) measurement, outcome evaluation, incomplete outcome data, and selective outcome reporting have a low risk of bias (Fig. 3B).
Figure 3.
Results of quality assessment of (A) the selected randomized controlled trial studies and (B) non-randomized controlled trial studies. Based on the Cochrane risk of bias tool, the summary: “−,” “+,” and “?” indicate high, low, and unclear risk of bias, respectively.
3.4. Synthesis of results
The postural balance, functional mobility in short-distance and long-distance, lower-limb strength, and fall risk were evaluated to assess postural control ability. Meanwhile, health status was also evaluated.
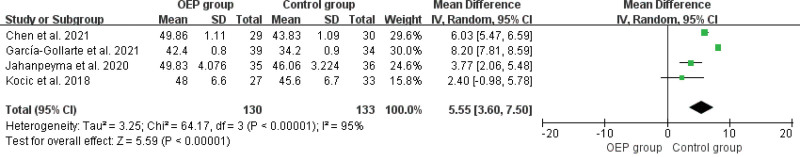
3.4.1. Postural balance.
The postural balance was tested by Berg Balance Scale (BBS) in 4 studies with 263 participants, including 130 in the OEP group and 133 in the control group.[17,20,21,23] The meta-analysis confirmed that BBS scores increased significantly in the OEP group compared to the control group (mean difference [MD] = 5.55; 95% CI = 3.60, 7.50; I2 = 95%; P < .00001; Fig. 4).
Figure 4.
Results of the meta-analysis of postural balance.
3.4.2. Fall risk.
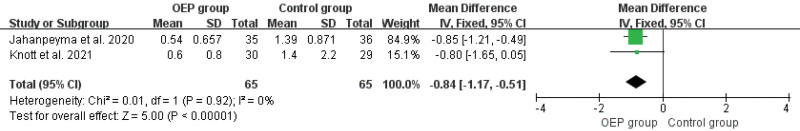
The fall risk was evaluated by the number of falls in 2 studies that included 130 participants, 65 in the OEP group and 65 in the control group.[20,22] The meta-analysis confirmed that the number of falls decreased significantly in the OEP group compared to the control group (MD = −0.84; 95% CI = −1.17, −0.51; I2 = 0%; P < 0.00001; Fig. 5).
Figure 5.
Results of the meta-analysis of fall risk.
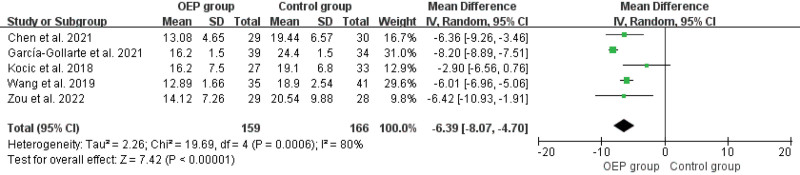
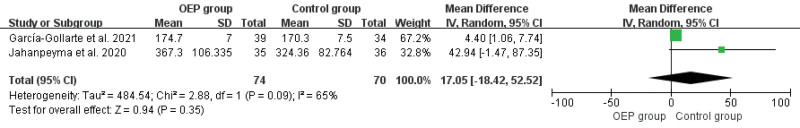
3.4.3. Functional mobility.
Functional mobility in short-distance was tested by the Timed Up and Go test (TUG) in 5 studies with 325 participants, including 159 in the OEP group and 166 in the control group.[17,18,21,23,24] The meta-analysis confirmed that the consuming time of TUG reduced significantly in the OEP group compared to the control group (MD = −6.39; 95% CI = −8.07, −4.70; I2 = 80%; P < .00001; Fig. 6). Functional mobility in long-distance was tested by the 6-minute walking test (6MWT) in 2 studies with 144 participants, including 74 in the OEP group and 70 in the control group.[20,23] The meta-analysis confirmed that the walking distance of 6MWT did not significantly change in the OEP group compared to the control group (MD = 17.05; 95% CI = −18.42, 52.52; I2 = 65%; P = .35; Fig. 7).
Figure 6.
Results of the meta-analysis of functional mobility in short-distance.
Figure 7.
Results of the meta-analysis of functional mobility in long-distance.
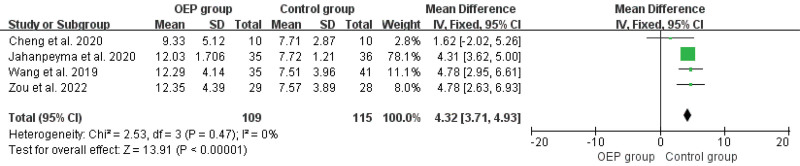
3.4.4. Lower-limb strength.
The lower-limb strength was tested by a 30-second Chair Stand Test (30s-CST) in 4 studies with 224 participants, including 109 in the OEP group and 115 in the control group.[18–20,24] The meta-analysis confirmed that the completed number in 30s-CST increased significantly in OEP group compared to control group (MD = 4.32; 95% CI = 3.71, 4.93; I2 = 0%; P < .00001; Fig. 8).
Figure 8.
Results of the meta-analysis of lower-limb strength.
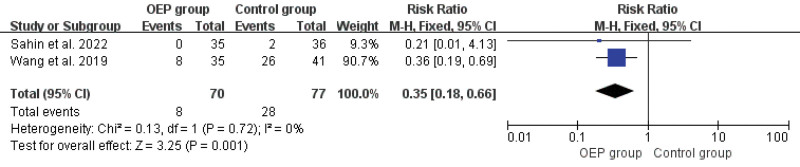
3.4.5. Health status.
The health status was tested by the number of frail elders in 2 studies with 147 participants, including 70 in the OEP group and 77 in the control group.[18,25] The meta-analysis confirmed that the number of frail elders reduced significantly in the OEP group compared to the control group (risk ratio = 0.35; 95% CI = 0.18, 0.66; I2 = 0%; P = .001; Fig. 9).
Figure 9.
Results of the meta-analysis of health status.
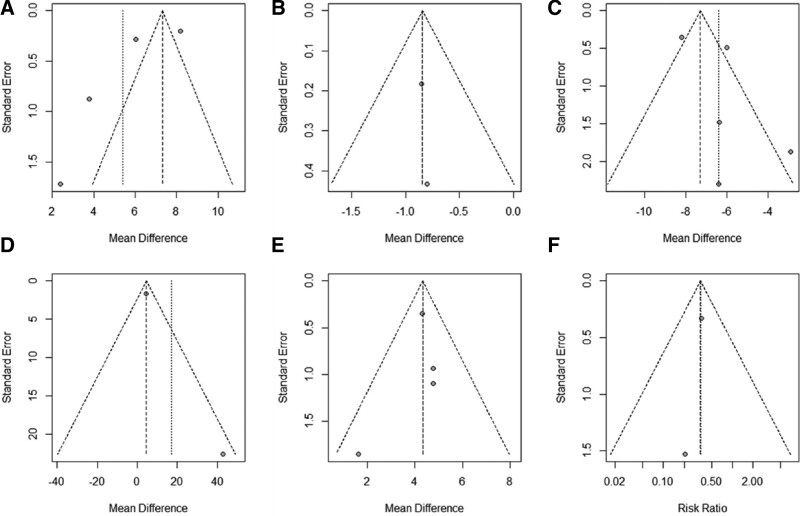
3.5. Publication bias
A funnel plot analysis was performed. The graphic funnel plots of the comparison in TUG, 30s-CST, 6MWT, number of falls and number of frail elders between the OEP group and control group were symmetrical except for BBS (Fig. 10). The Egger’s test was performed in BBS (t = −1.67, P = .2374), TUG (t = 1.25, P = .3008), and 30s-CST (t = −0.51, P = .6618), and was not performed for the number of studies being too small in terms of functional mobility in long-distance, fall risk, and health status.
Figure 10.
Graphic funnel plots of (A) postural balance, (B) fall risk, (C) functional mobility in short-distance, (D) functional mobility in long-distance, (E) lower-limb strength, and (F) health status.
4. Discussion
4.1. Summary of results
Compared with conventional exercise training, elders living in a NH following the OEP intervention had fewer falls, increased BBS scores, completed the number of 30s-CST, had faster TUG, and were less frail. No significant change in walking distance in the 6MWT was observed.
4.2. Postural control ability in elders living in the NH
Aging is closely associated with postural control deterioration, and approximately 18% of elderly individuals aged > 60 years have impaired postural control ability, rising to 24% for those >80 years.[26,27] Only 3 studies included in this review had mean ages under 80 years, indicating a strong likelihood that these detrimental alterations would manifest in elders living in the NH.[17,20,25] Elders living in NHs may consciously or unconsciously reduce the proportion of exercise in their daily activities, further reducing physical activity and leading to poor postural control, thereby forming a vicious circle.[28]
Falls are more likely to occur when postural control ability is compromised, particularly in individuals with balance impairment. The risk of falling is nearly 3 times higher in elders living in NHs than in the community, and walking instability increases by 39%.[29,30] Knee bending, walking backward, walking and turning around, walking sideways, tandem stance, tandem walk, 1-leg stand, heel walking, toe walking, heel-toe walking backward, sit-to-stand, and stair walking are some of the balance training exercises used in the OEP.[25] These actions can strengthen the body’s static and dynamic balance by simulating the movements frequently utilized in the daily activities of elders and reduce their fall risk. In this study, compared to conventional exercise training, the OEP had a more positive effect on enhancing postural balance and reducing fall risk in NH elders. Additionally, a previous meta-analysis found that the benefits of the OEP on balance were unrelated to the entire training duration, but related to training intensity within a week.[10] According to Kocic et al[17] and Wang et al,[18] when carrying out the OEP in the NH, doing part one for 40 minutes a day at least twice a week and part two for 30 minutes a day at least twice a week, with the 2 parts not carried out on the same day, will improve the elderly’s capacity to maintain their postural balance effectively.
Mobility limitations are more common among the elderly population, and are an important sign of a decline in posture control ability. This has adverse effects on the physical, psychological, and social aspects of the elderly.[31] Compared to community-dwelling elders, the mobility of elders living in NHs will significantly decline in short- and long-distance mobility. For example, gait speed in NH elders is 0.2 m/s slower than that of community-dwelling elders, and the time required for the postural transition to stability is doubled.[30,32] According to our results, the functional mobility of elders within NHs, at short distances, was more effectively improved after the OEP intervention, and the mean consumption time was reduced by 29.2% compared to conventional exercise training. Long-distance functional mobility is closely related to cardiopulmonary function, such as maximum oxygen uptake. However, part one of the OEP is carried out in situ or within the range of 10 steps; part two only emphasizes walking time, but does not emphasize the distance to be completed per unit of time.[17] Because of these characteristics of the OEP, the training intensity does not meet the minimum requirements to enhance cardiopulmonary function, which may be the main reason that long-distance mobility did not significantly improve in these elders.
Muscle strength decreases with age, which affects movement, reduces physical function, and causes related diseases. For instance, the incidence rate of sarcopenia is 6.54% to 40.4% in elderly individuals compared to 35.4% to 47.4% in those in NHs.[33–35] Improving the composition and size of the muscles could reduce frailty and fall risk in elderly individuals. Resistance training can improve physical activity and muscle strength by increasing the cross-sectional area of the muscles and muscle bundles. The OEP prioritizes strengthening the muscles used in knee flexion and extension, hip abduction, and ankle dorsiflexion and plantarflexion.[25] As seen by the mean improvement of 67% in the lower limb muscle strength of those living in NHs in our results, thus, this training approach fits the demands of these elders to enhance and maintain normal muscle strength.
Frailty is characterized by reduced declined physiological capacity across several organ systems, and the critical phenotype is diminished motor resilience that eventually leads to loss of activities of daily living.[36] Sufficient exercise training is particularly beneficial, and can reduce physical atrophy caused by inactivity, maintain body function, and reverse frailty.[28,37] Our results suggest the health status of elders living in NHs was significantly improved by the OEP, and the proportion of frail elders was only 11.4% in the OEP group compared to 36.4% in the conventional exercise group after intervention. Therefore, after undergoing the OEP, elders living in NHs will have improved motor resilience and postural control ability to perform their daily activities and better health status to enjoy their lives.
4.3. Limitations
Although this review is comprehensive, there are some limitations to our study. The included studies regarding fall risk, functional mobility in long-distance, and health status were relatively small and might not render sufficient statistical power to support the results, and more high level of evidence and studies should be further conducted.
4.4. Implications for clinical practice
The OEP is feasible to be used in elders living in the NH to reduce elders’ fall risk and enhance their postural control ability. Based on the current evidence, we recommend separating the 2 parts of the OEP for training in 1 week, which will be more suitable for these elders; the OEP is capable of reducing their risk factors for falls if delivered in supervised sessions for 3 to 6 months.
5. Conclusion
Current evidence suggests that the OEP, used for more than 3 months, reduces the fall risk and positively affects the postural control ability of elders living in the NH. Nursing personnel can popularize and carry out this exercise program in NHs to maintain or improve the daily activity function of elderly individuals.
Author contributions
Conceptualization: Lingyu Kong, Xinwen Zhang.
Data curation: Lingyu Kong, Xinwen Zhang.
Formal analysis: Lingyu Kong, Xinwen Zhang.
Funding acquisition: Lingyue Meng.
Methodology: Lingyu Kong, Xinrui Zhu.
Project administration: Xinrui Zhu.
Resources: Xinrui Zhu.
Software: Lingyu Kong, Xinrui Zhu.
Supervision: Lingyue Meng, Qiuxia Zhang.
Validation: Lingyue Meng.
Visualization: Lingyue Meng.
Abbreviations:
- 30s-CST
- 30-second Chair Stand Test
- 6MWT
- 6-minute walking test
- BBS
- Berg Balance Scale
- CI
- confidence interval
- MD
- mean difference
- NH
- nursing home
- OEP
- Otago Exercise Program
- RCT
- randomized controlled trial
- TUG
- Timed Up and Go test
This study was supported by Soochow University (AS10600821, AS10600221, and 5731502622).
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
How to cite this article: Kong L, Zhang X, Zhu X, Meng L, Zhang Q. Effects of Otago Exercise Program on postural control ability in elders living in the nursing home: A systematic review and meta-analysis. Medicine 2023;102:11(e33300).
Contributor Information
Lingyu Kong, Email: kly9710@163.com.
Xinwen Zhang, Email: qxzhang@suda.edu.cn.
Xinrui Zhu, Email: 13046480719@163.com.
Lingyue Meng, Email: mly15550464798@163.com.
References
- [1].Schweighart R, O’Sullivan JL, Klemmt M, et al. Wishes and needs of nursing home residents: a scoping review. Healthcare (Basel). 2022;10:854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Viveiro LAP, Gomes GCV, Bacha JMR, et al. Reliability, validity, and ability to identity fall status of the berg balance scale, balance evaluation systems test (BESTest), Mini-BESTest, and Brief-BESTest in older adults who live in nursing Homes. J Geriatr Phys Ther. 2019;42:E45–54. [DOI] [PubMed] [Google Scholar]
- [3].Severance JJ, Rivera S, Cho J, et al. A collaborative implementation strategy to increase falls prevention training using the age-friendly health systems approach. Int J Environ Res Public Health. 2022;19:5903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Barber SE, Forster A, Birch KM. Levels and patterns of daily physical activity and sedentary behavior measured objectively in older care home residents in the United Kingdom. J Aging Phys Act. 2015;23:133–43. [DOI] [PubMed] [Google Scholar]
- [5].Kazoglu M, Yuruk ZO. Comparison of the physical fitness levels in nursing home residents and community-dwelling older adults. Arch Gerontol Geriatr. 2020;89:104106. [DOI] [PubMed] [Google Scholar]
- [6].Kang KH, White KN, Hayes WC, et al. Agility and balance differ between older community and retirement facility residents. J Appl Gerontol. 2004;23:457–68. [Google Scholar]
- [7].Lytras D, Sykaras E, Iakovidis P, et al. Effects of a modified Otago exercise program delivered through outpatient physical therapy to community-dwelling older adult fallers in Greece during the COVID-19 pandemic: a controlled, randomized, multicenter trial. Eur Geriatr Med. 2022;13:893–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Brett L, Stapley P, Meedya S, et al. Effect of physical exercise on physical performance and fall incidents of individuals living with dementia in nursing homes: a randomized controlled trial. Physiother Theory Pract. 2021;37:38–51. [DOI] [PubMed] [Google Scholar]
- [9].Cao PY, Zhao QH, Xiao MZ, et al. The effectiveness of exercise for fall prevention in nursing home residents: a systematic review meta-analysis. J Adv Nurs. 2018;74:2511–22. [DOI] [PubMed] [Google Scholar]
- [10].Chiu HL, Yeh TT, Lo YT, et al. The effects of the Otago Exercise Programme on actual and perceived balance in older adults: a meta-analysis. PLoS One. 2021;16:e0255780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ries JD, Carroll M. Feasibility of a small group Otago exercise program for older adults living with dementia. Geriatrics (Basel). 2022;7:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ecsedy AE, Depner C, Hudlikar AN. Application of the OTAGO exercise/fall prevention program in the long-term care setting. GeriNotes. 2021;28:12–5. [Google Scholar]
- [13].Thomas S, Mackintosh S, Halbert J. Does the “Otago exercise programme” reduce mortality and falls in older adults?: a systematic review and meta-analysis. Age Ageing. 2010;39:681–7. [DOI] [PubMed] [Google Scholar]
- [14].Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kocic M, Stojanovic Z, Nikolic D, et al. The effectiveness of group Otago exercise program on physical function in nursing home residents older than 65years: a randomized controlled trial. Arch Gerontol Geriatr. 2018;75:112–8. [DOI] [PubMed] [Google Scholar]
- [18].Wang L, Zhang T, Zhang Q, et al. Effectiveness of the Otago exercise on frailty in institutionalized residents. J Nur Sci. 2019;34:12–5. [Google Scholar]
- [19].Cheng Y, Liao Y, Hsieh L. Effects of the Otago exercise program on lower extremity strength in residents of a long-term care institution. J Nurs. 2020;67:48–55. [DOI] [PubMed] [Google Scholar]
- [20].Jahanpeyma P, Kayhan Koçak FO, Yildirim Y, et al. Effects of the Otago exercise program on falls, balance, and physical performance in older nursing home residents with high fall risk: a randomized controlled trial. Eur Geriatr Med. 2021;12:107–15. [DOI] [PubMed] [Google Scholar]
- [21].Chen X, Zhao L, Liu Y, et al. Otago exercise programme for physical function and mental health among older adults with cognitive frailty during COVID-19: a randomised controlled trial. J Clin Nurs. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Knott S, Hollis A, Jimenez D, et al. Efficacy of traditional physical therapy versus Otago-based exercise in fall prevention for ALF-residing older adults. J Geriatr Phys Ther. 2021;44:210–8. [DOI] [PubMed] [Google Scholar]
- [23].García-Gollarte F, Mora-Concepción A, Pinazo-Hernandis S, et al. Effectiveness of a supervised group-based Otago exercise program on functional performance in frail institutionalized older adults: a multicenter randomized controlled trial. J Geriatr Phys Ther. 2021. [DOI] [PubMed] [Google Scholar]
- [24].Zou Z, Chen Z, Ni Z, et al. The effect of group-based Otago exercise program on fear of falling and physical function among older adults living in nursing homes: a pilot trial. Geriatr Nurs. 2022;43:288–92. [DOI] [PubMed] [Google Scholar]
- [25].Sahin S, Şenuzun Aykar F, Yildirim Y, et al. The impact of the Otago exercise program on frailty and empowerment in older nursing home residents: a randomized controlled trial. Ann Geriatr Med Res. 2022;26:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Da Silva JL, Agbangla NF, Le Page C, et al. Effects of chronic physical exercise or multicomponent exercise programs on the mental health and cognition of older adults living in a nursing home: a systematic review of studies from the past 10 years. Front Psychol. 2022;13:888851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Smit D, Willemse B, de Lange J, et al. Wellbeing-enhancing occupation and organizational and environmental contributors in long-term dementia care facilities: an explorative study. Int Psychogeriatr. 2014;26:69–80. [DOI] [PubMed] [Google Scholar]
- [28].Chou CH, Hwang CL, Wu YT. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: a meta-analysis. Arch Phys Med Rehabil. 2012;93:237–44. [DOI] [PubMed] [Google Scholar]
- [29].Cameron ID, Dyer SM, Panagoda CE, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2018;9:CD005465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Rabuffetti M, Zemp DD, Tettamanti M, et al. Stabilization after postural transitions in the elderly: experimental study on community-dwelling subjects and nursing home residents. Gait Posture. 2022;91:105–10. [DOI] [PubMed] [Google Scholar]
- [31].Brown CJ, Flood KL. Mobility limitation in the older patient: a clinical review. JAMA. 2013;310:1168–77. [DOI] [PubMed] [Google Scholar]
- [32].Tansuğ M, Kahraman T, Genç A. Differences in pain characteristics and functional associations between nursing home residents and community-dwelling older adults: a cross-sectional study. Ann Geriatr Med Res. 2021;25:187–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Cruz-Jentoft AJ, Bahat G, Bauer J, et al.; Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Martín Del Campo Cervantes J, Habacuc Macías Cervantes M, Monroy Torres R. Effect of a resistance training program on sarcopenia and functionality of the older adults living in a nursing home. J Nutr Health Aging. 2019;23:829–36. [DOI] [PubMed] [Google Scholar]
- [35].Marzetti E, Calvani R, Tosato M, et al.; SPRINTT Consortium. Sarcopenia: an overview. Aging Clin Exp Res. 2017;29:11–7. [DOI] [PubMed] [Google Scholar]
- [36].Kong L, Wang W, Zhu X, et al. Effect of frailty on kinematic characteristics of walking in community-dwelling elders. Z Gerontol Geriatr. 2022;55:689–95. [DOI] [PubMed] [Google Scholar]
- [37].Courel-Ibáñez J, Buendía-Romero A, Pallarés JG, et al. Impact of tailored multicomponent exercise for preventing weakness and falls on nursing home residents’ functional capacity. J Am Med Dir Assoc. 2022;23:98–104.e3. [DOI] [PubMed] [Google Scholar]