Abstract
Background
The current COVID-19 pandemic has led to many studies examining its arrhythmogenic effects. However, there are many other viruses that are capable of inducing arrhythmias that have not received as much attention. The objective of this study was to review common viruses and identify studies highlighting their arrhythmogenic effects.
Methods and results
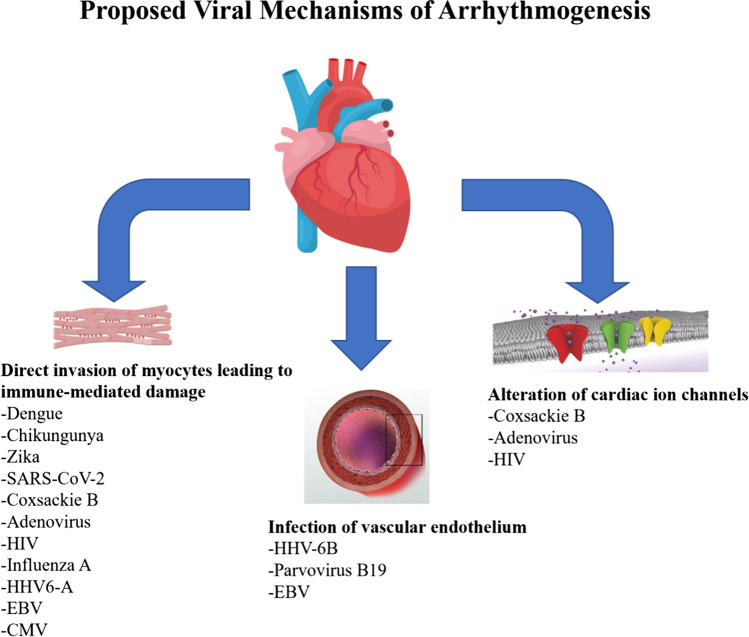
In this review, we examined 15 viruses and the literature regarding their arrhythmogenic effects. The common mechanisms of action appear to be direct invasion of myocytes leading to immune mediated damage, infection of vascular endothelium, and alteration of cardiac ion channels.
Conclusions
This review highlights the growing evidence that supports the involvement of other viral infections in the development of arrhythmia. Physicians should be aware of these potentially life-threatening effects when caring for patients with these viruses, some of which are very common. Additional studies are required to better understand the complex mechanism and risk factors of cardiac arrhythmias in patients suffered from viral infections to determine whether the processes can be reversed or even prevented.
Keywords: Viral arrhythmia, Myocarditis, Ventricular arrhythmia, Supraventricular arrhythmia
Introduction
The current COVID-19 pandemic has led to a plethora of studies examining its cardiac complications, including its arrhythmogenic effects [1]. However, many other viruses are known to be capable of inducing arrhythmias. To our knowledge, there is no review of the arrhythmogenic effects of other viruses; therefore, the goal of this paper is to review the literature regarding the arrhythmias induced by multiple viruses, including COVID-19 (Tables 1, 2, and 3; Fig. 1; central illustration). Being aware of the arrhythmogenic effects of viruses can improve outcomes in patients hospitalized with these diseases.
Table 1.
Cardiac arrhythmias in RNA viruses
| Virus | Author, year, country | Study design | Sample size (n) | Notable arrhythmias | Reported myocarditis (%) |
|---|---|---|---|---|---|
| Dengue | Poornima 2019, India | Retrospective observational | 341 |
Sinus bradycardia (8.79%) T wave inversion (4.1%) AF (2.93%) AV block (2.34%) ST depression (2.3%) |
N/A |
| Shah 2020, India | Prospective observational | 320 |
Sinus bradycardia (19.7%) Sinus tachycardia (6.9%) AF (3.75%) VT (0.60%) |
17.5 (no CMRI nor biopsy done) | |
| CHIKV | Carta 2018, Venezuela | Prospective observational | 287 |
Bradyarrhythmia (33%) AF (6.6%) |
N/A |
| Villamil-Gómez 2016, Colombia | Case series | 42 |
1st degree AV block (19%) Left anterior hemiblock (9.5%) Bradyarrhythmia (7.1%) AF (2.4%) Tachyarrhythmias (4.8%) |
“Suspected in all” | |
| Dengue/CHIKV | Obeyeskere 1973, Sri Lanka | Case series | 35 |
Frequent ventricular ectopy (31.4%) Sinus tachycardia (17.1%) AF (2.8%) Transient complete AV dissociation (2.8%) VT (2.8%) |
100 a |
| Zika | Mendoza 2018, unknown location | Prospective observational | 16 |
Complex ventricular arrhythmias (62.5%) Non-sustained atrial tachycardia (62.5%) AF (43.8%) VT (31.3%) |
100 |
| Villamil-Gómez 2018, Colombia | Case series | 2 |
Sinus tachycardia with prolonged Qtc (50%) Left anterior hemiblock (50%) |
N/A | |
| SARS-CoV-2 | Rosenblatt 2022, USA | Retrospective database | 30,999 | AF (5.4%) | N/A |
| Li 2021, N/A | Meta-analysis of 19 studies | 21,653 | AF (11%) | N/A | |
| Bhatla 2020, USA | Retrospective observational | 700 |
AF (3.6%) Non-sustained VT (1.4%) Clinically significant bradyarrhythmia (1.3%) |
N/A | |
| Cho 2020, united states | Prospective observational | 143 |
Sinus tachycardia (39.9%) Non-sustained VT (15.4%) Sustained VT (1.4%) VF (0.7%) |
N/A | |
| Coxsackie B Virus | Multiple | Case reports | Ventricular arrhythmias | N/A | |
| Influenza A | Madjid 2019, USA | Retrospective observational | 163,831 | Ventricular arrhythmias requiring shock or antitachycardia pacing increased during periods of high and moderate influenza activity | N/A |
| Chang 2016, Taiwan | Retrospective case–control | 56,870 | AF (18% increase in risk) compared to control group | N/A | |
| Ukimura 2010, Japan | Case series | 15 |
VF (26.7%) Complete AV block (26.7%) SVT (13.3%) AF (13.3%) |
100 | |
| Rubella | Multiple | Case reports | AV block | N/A | |
| HIV | Abudan 2020, USA | Retrospective database | 2,370,751 |
AF (2110†) VT (560†) Atrial flutter (420†) SVT (170†) VF (130†) |
N/A |
| Park 2022, USA | Meta-analysis of 7 studies | 94,928 | Atrial arrhythmia (6.4 cases per 1000 person years); 35% greater than those without HIV | N/A |
aDiagnostic criteria used: (1) clinical evidence of myocarditis; (2) presence of electrocardiographic evidence of myocarditis, ST segment and T wave changes, and disturbances in conduction and rhythm; (3) recent history of “dengue-like” fever; (4) serological evidence of past dengue or chikungunya infection as revealed by the presence of antibody in high titers
†Per 100,000 hospitalizations
Table 2.
Cardiac arrhythmias in DNA viruses
| Virus | Author, year, country | Study design | Sample size (n) | Notable arrhythmias | Reported myocarditis (%) |
|---|---|---|---|---|---|
| Adenovirus | Multiple | Case reports | Ventricular arrhythmias | N/A | |
| HHV-6 | Amin 2021, Iran | Case series | 3 |
Mobitz type II AV block (33.3%) VT (33.3%) |
100 |
| Parvovirus B19 | Multiple | Case reports | Ventricular arrhythmias | N/A | |
| HSV | Chiang 2011, Taiwan | Retrospective case–control | 88,377 | AF (1.6% of study vs 1.1% in control) | N/A |
| CMV | Multiple | Case reports | AV block | N/A | |
| EBV | Mavrogeni 2011, Greece | Case series | 6 | VT (100%) | 100 |
| VZV | Cha 2018, South Korea | Retrospective case control | 153,425 | AF (6.4 per 1,000 patient-years) in severe VZV vs (2.6 per 1000 patient-years) in non-VZV group | N/A |
| Park 2022, USA | Meta-analysis of 7 studies | 94,928 | Atrial arrhythmia (6.4 cases per 1000 person years); 35% greater than those without HIV |
Table 3.
Proposed mechanism of arrhythmias in viral infections
| Virus | Arrhythmias reported | Proposed mechanism of action |
|---|---|---|
| Dengue virus |
Sinus bradycardia AV block AF |
Direct invasion, immune mediated cardiomyocyte damage direct involvement of conduction system Prodromal phase in acute myocarditis leading to arrhythmia |
| Chikungunya | AF, brady-arrhythmias, AV block | Penetrates myocytes and directly damaging muscle fibers; prodromal phase in acute myocarditis leading to arrhythmia |
| Zika | AF, atrial tachycardia, ventricular arrhythmias | Invasion of cardiac cells, leading to autoimmune induced apoptosis |
| SARS-CoV-2 | AF, VT | Binds to ACE2 of myocardial cells, leading to myocarditis via direct toxicity, induced inflammatory response |
| Coxsackie B | Ventricular arrhythmias | Binds to CAR and DAF of cardiac myocytes, cleavage of dystrophin leading to DCM; alteration of cardiac ion channels |
| Adenovirus | Ventricular arrhythmias | Binds to CAR and integrins αvβ3 and αvβ5 of cardiac myocytes; alteration of cardiac ion channels |
| Rubella | AV block | Unclear, likely from myocardial inflammation and scarring |
| HIV | AF, atrial arrhythmias | Release of Nef, leading to dysregulation of autophagy causing cardiomyocyte death; HIV tat protein causing inactivation of hERG K+ channels |
| Influenza A | AF, AV block, ventricular arrhythmias | Infection of cardiomyocytes, Purkinje cells, and endothelial cells |
| HHV-6 | AV block, ventricular arrhythmias | Direct infection of cardiomyocytes (HHV-6A), infection of vascular endothelium leading to endothelial/diastolic dysfunction (HHV-6B) |
| Parvovirus B19 | Ventricular arrhythmias | Infection of endothelial cells of small cardiac vessels leading to diastolic dysfunction |
| HSV | AF, sinus node dysfunction | Inflammation (AF); CNS dysfunction from HSV encephalitis |
| CMV | AV block | Invasion of cardiomyocytes; inflammation and edema of conduction system from myocarditis |
| EBV | Ventricular arrhythmias, AV block | Invasion of cardiomyocytes and vascular endothelium |
| VZV |
Ventricular arrhythmias AF, AV block |
Inflammation (AF); resultant fibrosis and scarring leading to conduction blocks and reentry circuits |
Fig. 1.
Proposed viral mechanisms of arrhythmogenesis. Illustration representing the three most common proposed viral mechanisms of arrhythmogenesis
Dengue virus
Dengue virus is a positive-sense single-stranded RNA virus with a lipid envelope. It is part of the Flavivirus family [2]. It is transmitted by the Aedes mosquito and is the leading cause of arthropod-borne viral disease in the world, with about 400 million infections occurring per year with a mortality rate of greater than 5–20% in some endemic areas [3]. It is known for causing dengue fever, characterized by a biphasic, high-grade fever, retrobulbar headache, and myalgias/joint pain, hence its nickname “breakbone fever” [2].
It is unclear how dengue infection causes cardiac disease. It is thought that direct invasion, immune-mediated cardiomyocyte damage, and direct involvement of the conduction system contribute to its cardiac effects, which can range from transient arrhythmia to myocarditis [4]. There are several studies examining the arrhythmogenic effects of dengue virus. The largest study is a retrospective observation study of 341 dengue patients admitted to a rural tertiary care center. Sinus bradycardia was the most common ECG abnormality (8.79%), followed by T inversions (4.1%) and ST depression (2.3%). Atrioventricular (AV) block was seen in 2.34%, and transient atrial fibrillation (AF) was seen in 2.93% of patients [5]. There also is a prospective study of 320 patients without pre-existing heart disease who were hospitalized with dengue. Sinus bradycardia was the most common ECG finding seen (19.7%), followed by sinus tachycardia (6.90%) [6]. It appears the most prominent ECG findings induced by dengue are sinus bradycardia, AV block, and AF that tends to resolve spontaneously.
Chikungunya
Chikungunya is a positive-sense single-stranded RNA virus with a small spherical envelope. It is from the Togaviridae family. It is spread by the Aedes mosquito. Chikungunya (CHIKV) is considered endemic in parts of West Africa, but has spread globally due to human and vector travel [7]. Acute infection is similar to dengue fever, with rapid onset fever, polyarthralgia/arthritis, myalgias, and headache [8]. CHIKV exerts its cardiogenic effects by penetrating the myocytes and directly damaging the muscle fibers, a concomitant inflammatory response resulting in further damage. Clinical effects range from full recovery to heart failure from congestive cardiomyopathy. There is thought to be a “prodromal” phase in the course of acute myocarditis that can lead to the development of arrhythmias and proposed to be the mechanism behind other arbovirus heart disease [9].
Few studies have examined the arrhythmogenic effects of CHIKV. To our knowledge, the largest study focusing on this is a prospective multicenter observation study of 287 patients during a Venezuelan outbreak. Arrhythmias were noted in 45% of cases; the most common arrhythmia seen were bradyarrhythmia (33%). AF was seen in 19 cases. The study notes ectopic atrial tachycardia, non-sustained ventricular tachycardia (VT), conduction disturbances, and ventricular ectopic beats and tachyarrhythmias [10]. A case series of 35 patients with arbovirus heart disease including both dengue and CHIKV patients reports 25 patients with arrhythmia. Sinus tachycardia was seen in 6, bradycardia in 1, frequent ventricular ectopy in 11, AF in 2, transient complete AV dissociation in 1, and 1 patient with ventricular ectopy that developed VT leading to death. However, the study did not differentiate between dengue and CHIKV when describing these cardiovascular effects [9]. A case series of 42 patients in Colombia with chikungunya fever examined the ECG changes in infection; repolarization disturbances were in 21.4%. First degree AV block was seen in 19%, and left anterior hemiblock was seen in 9.5%. Bradyarrhythmia was seen in 7.1% [11]. Based on the available data, it appears that bradyarrhythmia, AV block, and AF are arrhythmias to be mindful of in CHIKV infection.
Zika virus
Zika virus is a single-stranded, positive-sense RNA virus which is enveloped. It is a part of the Flavivirus family [12]. Also, as a tropical virus, it is transmitted by the Aedes aegypti and albopictus mosquitos. However, it can be transmitted sexually, via blood, and perinatally [13]. In adults, most acute infections are asymptomatic or present with mild symptoms which can consist of a maculopapular rash, conjunctivitis, fever, headache, and arthralgias/myalgias [12]. However, Zika infections during pregnancy can lead to congenital defects, most notably microcephaly [12]. In 2015, an increase in congenital microcephaly was noted in Brazil that was associated with Zika infection during pregnancy, leading to Zika being deemed by the World Health Organization to be a public health emergency in 2016 [14].
It is thought that Zika enters the cardiac cells via the intercellular adhesion molecule-3 (ICAM3) and tyrosine protein kinase 3 receptors, eventually leading to autoimmune induced apoptosis [15]. One study showed Zika induces a myocardial immune response in mice with induced inactivation of interferon (IFN) α and β receptors but not in the wild-type mice, suggesting that this can generate a severe myocarditis in the immunocompromised [16].
There are a paucity of studies examining the arrhythmogenic effects of Zika in humans. To our knowledge, the largest is a prospective observation study of 16 patients with acute Zika myocarditis; acute AF developed in 7 patients, non-sustained atrial tachycardia in 10, VT in 5 patients, and complex ventricular arrhythmias in 10 cases [17]. There is a case series of 2 pregnant women with confirmed Zika infection: one with sinus tachycardia with a prolonged QTc with a pericardial effusion and the other with a left anterior hemiblock, also with pericardial effusion [18]. There is a case report of acute Zika infection leading to acute AF without any other changes seen on echocardiogram nor coronary angiography [19]. Based on the limited data available, it appears that both atrial tachycardia and ventricular arrhythmias are seen most likely in the context of myocarditis.
Severe acute respiratory syndrome coronavirus 2
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a positive-stranded RNA virus of the Coronaviridae family. It has a crown-like appearance due to its spike glycoproteins on its envelope. It is responsible for the recent COVID-19 pandemic leading to the deaths of over 6 million [20]. It is primarily transmitted via infectious respiratory droplets. The virus uses its spike protein to bind to the human angiotensin-converting enzyme 2 (ACE2) receptors that are present in the respiratory epithelium [21]. It is thought that SARS-CoV-2 binds to the ACE2 receptors expressed by myocardial cells, leading to myocarditis via direct cytotoxicity. An induced inflammatory response is thought to lead to cardiac arrhythmias [22].
There are a plethora of studies examining the arrhythmogenic effects of SARS-CoV-2 and its effects on mortality, especially in AF. In an analysis of 30,999 patients from the American Heart Association COVID-19 Cardiovascular Disease Registry, 5.4% developed new-onset AF during their hospitalization. When adjusted for demographics, comorbidities, and severity of disease, patients with new-onset AF did not have a significantly increased rate of death when compared to those with COVID-19 without AF, but had a significantly higher rate of major adverse cardiovascular events, with the authors suggesting that AF in COVID-19 is a marker of disease severity [23]. In contrast, a cohort study (n = 9564) did find new-onset AF to be significantly associated with mortality in COVID-19 patients [24]. A meta-analysis of 19 observational studies with 21,653 hospitalized patients with COVID-19 found the pooled prevalence of AF to be 11%, significantly associated with an increased risk of all-cause mortality [25]. A retrospective cohort study found atrial arrhythmias to be associated with mortality in COVID-19 [26].
Other arrhythmias manifest in COVID-19, including ventricular arrhythmias, which are less common. An analysis of 4526 patients worldwide found 18.3% to have an arrhythmia, with VT/non-sustained VT/VF consisting of a much smaller fraction compared to atrial arrhythmias (236 versus 675) [27]. An analysis of 700 patients admitted with COVID-19 discovered 53 arrhythmia related events which included 9 cardiac arrests, 25 AF events, 9 clinically significant bradyarrhythmia, and 10 non-sustained VT [28]. In an observational prospective study of 143 hospitalized patients with COVID-19, non-sustained VT occurred in 15.4% of patients. Sustained VT was seen in 1.4% and VF was seen in 0.7% [29]. A retrospective cohort study of 1053 patients with COVID-19 found VT or VF (ventricular fibrillation) in 2.6% of patients; VT/VF was associated with in-hospital mortality [26]. It appears AF is a common occurrence in COVID-19. Ventricular arrhythmias are less common. However, it is up for debate as to whether AF is the result of the direct arrhythmogenic effects of the virus, as AF is known to be a complication of critical illness.
Coxsackie B virus
Coxsackie B virus is part of the Picornavirus family and is a positive-sensed, single-stranded RNA virus that does not have an envelope [30]. Infections occur worldwide and generally during the summer months. It binds to the coxsackievirus-adenovirus receptor (CAR), which can be found in intercalated discs. Manifestations include aseptic encephalitis, aseptic meningitis, pancreatitis, pleurodynia (also known as Bornholm disease), and myopericarditis [30].
Coxsackie B virus, specifically B3, is considered the most common cause of viral myocarditis and can lead to dilated cardiomyopathy (DCM) [31]. It has a tropism for the heart due to the relatively higher levels of CAR on the cardiac myocyte, which it uses to enter the myocyte, after which it releases proteases that promote viral replication and cleaves dystrophin [32]. This may be important in mediating DCM, as dystrophin gene mutations have been noted to be the cause of genetic DCM, such as Duchenne/Becker’s [33]. Interestingly, one study showed that knockout mice without the expression of CAR blocks coxsackievirus B3 entry and its harmful effects, further establishing the important role of CAR in coxsackievirus pathology [34].
Ventricular arrhythmias and sudden death are well-known complications of coxsackie B myocarditis [35–38] with many case reports documenting this phenomenon. One study showed that coxsackie B3 altered the abundance of cardiac ion channels KCNQ1, hERG1, and Cav1.2 in infected murine hearts, providing a possible explanation for the development of these ventricular arrhythmias [36]. Other implicated arrhythmias documented in case reports include AV blocks [39] and Torsades de Pointes [40 41].
Adenovirus
There are over 100 different types of adenovirus, a non-enveloped, double-stranded DNA virus of the family Adenoviridae. It has several routes of transmission which include fecal–oral, blood, and aerosolized droplets. Generally, infections are asymptomatic and self-limited in immunocompetent people [42]. Adenoviruses are known to spread in crowded areas such as public swimming pools and military barracks, causing epidemics that can spread rapidly [43]. Symptoms, when they do occur, include keratoconjunctivitis, acute hemorrhagic cystitis, and gastroenteritis. Pneumonia can also be seen [42]. Upon exposure, adenovirus can either undergo the lytic replication cycle when entering epithelial cells, or latent infection of lymphoid tissue [44].
Adenovirus is implicated in myocarditis and DCM. One study analyzing myocardial samples of 773 patients with myocarditis and DCM found adenovirus to be the most commonly found virus, even over enteroviruses [45]. Like coxsackievirus, it is thought that adenovirus also binds CAR seen in myocytes but with integrins αvβ3 and αvβ5 as its coreceptors, leading to its internalization [46]. Recent research demonstrated the cardiotropism of adenovirus in mice studies. RR interval widening was noted in infected mice with reductions in cardiac ion channel and gap junction mRNA transcripts, along with altered conduction velocity and electrical impairment manifesting as AV dissociation [47]. Like coxsackievirus, it is well documented that adenovirus myocarditis/DCM can lead to ventricular arrythmias leading to sudden cardiac death [48–52].
Rubella
Rubella, also known as German measles, is an enveloped, single-stranded positive-sense RNA virus of the Matonaviridae family [53]. Before its vaccine was developed, rubella was the source of major outbreaks, with the last epidemic in the USA taking place in 1964–1965 where 12.5 million people got rubella, leading to 11,000 miscarriages and 20,000 babies born with congenital rubella syndrome [54]. Rubella is well known for its ability to cause congenital heart defects. These include branch pulmonary artery stenosis and patent ductus arteriosus [55]. However, its ability to cause arrhythmia is not well-established with limited studies evaluating this. One reports 2 cases of postnatal rubella myocarditis leading to complete AV block in one of the patients, who was 6 years old [56]. In one case report, rubella myocarditis led to transient complete AV block [57], and in another case report, permanent AV block occurred 3 weeks after rubella infection [58]. Both of these cases occurred in young adult males [57 58]. Another case report showed rubella causing a bifascicular block in a 29-year-old male [59]. Wolff-Parkinson-White syndrome in congenital rubella [60] and SVT in acquired rubella [61] have been documented as well.
Human immunodeficiency virus
HIV is a retrovirus containing 2 copies of single-stranded RNA. It is enveloped and of the family Retroviridae. HIV attaches to CD4 and CCR5 receptors that are present in helper T cells, where it uses reverse transcriptase to incorporate its genome into the host DNA. Eventually, HIV viruses are assembled in the host cell and released via lysis [62]. It is estimated at 38.4 million adults and 1.7 million children worldwide live with HIV [63]. HIV has increasingly been implicated in cardiac disease. HIV displays cardiac tropism by releasing a viral protein called Nef, leading to dysregulation of autophagy causing cardiomyocyte death [64]. Those with HIV have an increased risk of cardiovascular disease, including increased risk of myocardial infarction and coronary artery disease [65]. HIV patients may also be more prone to sudden cardiac death, with possible mechanisms including QTc prolongation, ischemic heart disease, and AF [66].
AF appears to be the most prominent arrhythmia seen in HIV. In one study examining over 2 million HIV hospitalizations, AF was the most common arrhythmia (2110 per 100,000) [67]. A meta-analysis consisting of 94,928 pts also demonstrated an increased risk of atrial arrhythmia, including AF, in HIV [68]. This is further supported by another study that showed that a lower CD4 counts and higher viral loads were associated with an increased incidence of AF [69]. It has been proposed that chronic inflammation may be the trigger for AF in HIV [68].
QTc prolongation has been shown to be more prevalent in HIV, even after adjusting for QT- prolonging medications, which may predispose to life-threatening arrhythmias such as Torsades de Pointes [70]. One proposed mechanism for this in HIV infection is the HIV trans-activator protein called HIV tat protein causing inactivation of the hERG K+ channels, leading to inhibition of IKr currents and therefore QTc prolongation [71]. Other possible causes includes medications used in HIV such as fluconazole and protease inhibitors [70].
Influenza
Influenza is a negative-sensed single-stranded RNA virus of the family Orthomyxoviridae. Its genome consists of segments and also contains an envelope. Influenza A is responsible for causing frequent seasonal epidemics owing to its ability to evolve rapidly [72]. Although not as well-known a cause of myocarditis, influenza infection involves the myocardium in an estimated 10% of cases [73]. A recent study demonstrated the ability of influenza A to infect cardiomyocytes, Purkinje cells, and endothelial cells [74]. Several studies report the arrhythmogenic effects of influenza in the setting of myocarditis. In a case series of 15 patients with influenza A myocarditis during the 2009 H1N1 pandemic in Japan, ECG findings included VF in 4, complete AV block in 4, SVT in 2, and AF in 2 [75]. One case report details fatal influenza A myocarditis, where the patients developed VF and later incessant VT [76]. Another case report documented non-sustained VT in a 54-year-old man, with endomyocardial biopsy revealing influenza A myocarditis and the resolution of arrhythmia after therapy with oseltamivir [77]. An 18-year-old suffered sudden cardiac death after developing VF and later electromechanical dissociation from influenza A myocarditis [78]. A case series of 2 patients demonstrated high-grade AV block associated with influenza A virus in the absence of myocarditis seen on imaging [79]. Other case reports also report AV block in acute influenza infection [80–82].
There was a recent study of 11,374 patients with newly diagnosed AF from the Taiwan National Health Insurance Research Database. Patients with influenza infection without vaccination (n = 1369) had a higher risk of AF after adjustment for baseline differences. Those who received vaccination and also were infected with influenza had a lower risk of AF compared to the non-vaccinated group [83]. In a large retrospective study of 163,831 patients with implantable cardiac defibrillator or cardiac resynchronization therapy, Madjid et al. found a significant association between influenza activity and the incidence of ventricular arrhythmias requiring shock or anti-tachycardia pacing treatment [84]. It appears based on these studies that ventricular arrhythmias, AV block, and AF are arrhythmias to be on the lookout for in acute influenza infection.
Herpes virus type 6
Herpes virus type 6 (HHV-6) is a double-stranded DNA virus of the Herpesviridae family. It is thought that its primary route of transmission is via saliva from mother to infant. The two main subtypes are HHV-6A and HHV-6B. HHV-6A infects CD4 + T lymphocytes via binding to the CD46 receptor and enters via receptor-medicated endocytosis during primary infection [85]. In contrary, HHV-6B uses CD134 to bind to T cells [86]. HHV is ubiquitous in the adult population, with greater than 95% of adults being seropositive [85].
HHV-6 is also another cause of myocarditis and DCM. It is thought that HHV-6A may directly infect cardiomyocytes, while HHV-6B infects the vascular endothelium leading to endothelial and diastolic dysfunction [87]. A study with 172 patients with clinical history of myocarditis/DCM whose endomyocardial biopsies were analyzed showed HHV-6 DNA in 10.5%, which was the third highest after enterovirus and parvovirus. Persistent of the viral genomes in the myocardium was associated with a progressive impairment of left ventricular ejection fraction [88].
There exist several case reports examining arrhythmias in acute HHV-6 infection. A case series of 3 patients with HHV 6-myocarditis; one patient had Mobitz type II AV block and later refractory VT. No arrhythmias were documented for the other 2 patients. One of these two patients was admitted with aborted sudden cardiac death [89]. Another case report discusses a 5-month-old child who had VT, during HHV-6 myocarditis [90]. Another discusses a 5-year-old girl who developed complete AV block in HHV-6 myocarditis [91]. There is a case report of fulminant myocarditis in an immunocompetent 59-year-old who died from ventricular arrhythmia (but does specify which type) [92]. There is an interesting case report of a 19-year-old bone marrow transplant recipient who developed HHV6 encephalomyelitis but developed prolonged sinus tachycardia that persisted despite the disappearance from HHV-6 from cerebrospinal fluid, with the authors suggesting it being from both an inflammatory response and post-inflammatory degeneration of nerve cells [93]. Based on the evidence above, it appears most arrhythmias result from myocarditis in HHV-6.
Parvovirus B19
Parvovirus B19 is a single-stranded DNA virus of the family Parvoviridae. It does not contain an envelope. It is transmitted via respiratory secretions and blood products; however, it can also be transmitted vertically. It binds to host cells in the respiratory tract and enters the cells. After replicating its genome and assembling virions, it causes cell lysis, releasing the newly made virions. Parvovirus B19 is quite common, reaching 40–60% prevalence in adults. Parvovirus B19 is responsible for erythema infectiosum, characterized by a prodrome of myalgias, fever, and headache followed by an erythema of the cheeks, also known as “slapped cheek” [94].
Parvovirus is known as one of the viral triggers for myocarditis. In a study examining 172 endomyocardial biopsies of patients with a clinical history of myocarditis/DCM, parvovirus B19 was isolated in 36.6%, which was the most in the analysis, even over enteroviruses. Interestingly, 12.2% of the tissue samples showed both parvovirus 19 and HHV6 DNA [88]. Parvovirus’s role in cardiomyopathy is further supported by a study that found parvovirus B19 genome to be the most common viral genome in the myocardium of patients with isolated diastolic dysfunction of unknown etiology and also found the presence of parvovirus to be strongly associated with endothelial dysfunction [87]. A recent study (2021) examined whether a wearable cardioverter defibrillator would prevent sudden cardiac death after myocarditis. Parvovirus was found to be the most common etiology of myocarditis in this study (71%). Two of the patients had episodes of VT when wearing the wearable cardioverter defibrillator, with endomyocardial biopsies showing parvovirus B19 DNA; however, the authors question the significance of this finding as they note that parvovirus B19 DNA can be found in healthy individuals as well [95].
There are many case reports of pediatric myocarditis from parvovirus B19, but without any presenting arrhythmia [96–98]. In a case series of 3 patients with parvovirus B19 myocarditis, one patient presented with VT 2 weeks after suspected erythema infectiosum [99]. There is another case report of a child with fulminant myocarditis, with the course complicated by regular SVT with ST segment elevation [100]. Interestingly, there are several case reports of parvovirus B19 myocarditis leading to sudden cardiac death in young males with Brugada syndrome. One of them reports a case of a 34-year-old patient who was found to be in VF, with later ECGs showing patterns of intermittent ST segment elevation with incomplete RBBB induced by ajmaline [101]. Another case report documents a 22-year-old male found dead; however, he recently had been worked up for a syncopal episode in the setting of flu-like symptoms with ECG during that workup showing findings consistent with Brugada syndrome [102]. Another case report documents myopericarditis in a 43-year-old female presenting with supraventricular arrhythmia [103].
Herpes simplex virus
HSV is a linear double-stranded DNA virus of the Herpesviridae family. The two main subtypes are HSV-1 and HSV-2. HSV-1 is generally spread via direct contact with contaminated bodily fluids, while HSV-2 is spread by sexual contact. Both HSV-1 and HSV-2 replicate in the mucocutaneous tissue and travel retrogradely down the axon to the dorsal root ganglia, where it can remain latent until reactivation [104 105]. HSV-1 is thought to have caused symptomatic infection in about one third of the global population [106]. Approximately 16% of the population form the ages 14–49 were seropositive for HSV-2 from 2005 to 2010 [107].
HSV can also cause myocarditis, leading to ventricular arrhythmias, although not as commonly as the other viruses reported earlier, such as parvovirus B19. Evidence appears limited to case reports. One reports fulminant HSV-2 myocarditis in a healthy 41-year-old female, with presenting ECG showing ST depression and later VF [108]. Another case report describes a 3-year-old with HSV myocarditis whose ECG on admission showed sinus bradycardia [109].
There are several interesting case reports of sinus node dysfunction seen in HSV encephalitis. One such report discusses a 59-year-old female with HSV encephalitis, who had recurrent syncopal episodes due to sinus node arrest [110]. Another reports a 54-year-old male with HSV encephalitis who was put on Holter monitoring after a syncopal episode, which captured several episodes of sinus arrest, which resolved after antiviral treatment and resolution of the encephalitis [111]. Another reports a 48-year-old female with HSV encephalitis with several spontaneous pauses of 4 to 8 s during her sleep, with Holter monitoring after resolution of the encephalitis showing no further episodes [112]. Another case report also reports sinus node dysfunction in HSV encephalitis, manifesting as sinus pauses [113]. Lastly, another case report in 1986 documented HSV encephalitis with presented with sick sinus syndrome [114]. It is not clear why HSV encephalitis causes sinus node dysfunction, but is suggested by one of the authors of one of the case reports to be from central nervous system dysfunction rather than a primary cardiac disease [111].
To our knowledge, the largest study examining HSV and arrhythmia is a nationwide study in Taiwan, examining 15,180 patients with the diagnosis of HSV infection, and found those with HSV to have a significantly increased incidence of AF development compared to the control group. The authors propose that the inflammation caused by HSV may be the reason why [115].
Cytomegalovirus
Cytomegalovirus (CMV), also known as human herpesvirus 5, is a double-stranded DNA virus of the Herpesviridae family. CMV is spread via blood products, breastmilk, sexual contact, perinatally, and in close-contact settings. Generally, primary infection is asymptomatic in the immunocompetent but can cause mononucleosis. After primary infection, the virus remains dormant in the myeloid cells, but can be reactivated during immunosuppression, leading to the release of virions into the bodily fluids and blood [116]. CMV in the immunocompromised can lead to a host of serious conditions, such as hepatitis, retinitis, esophagitis, colitis, and pneumonitis [116–118]. CMV is extremely prevalent, estimated to be about 100% in Asia and Africa and 80% in North America and Europe [119].
In an analysis of myocardial samples from 40 patients who died from myocarditis, CMV was the most common viral nucleic acid found located in interstitial cells and cardiomyocytes [120]. Many case reports document CMV myocarditis in the immunocompetent, despite it generally being asymptomatic in that population [121–125]. One reports an immunocompetent patient with a reported absence of cardiac abnormalities in the past whose ECG showed sinus tachycardia with left bundle branch block (LBBB) [126]. One case report documents AF with rapid ventricular response in a case of severe CMV myocarditis, pneumonitis, and hepatitis who recovered after treatment with IV ganciclovir [127].
There are several case reports documenting heart block in CMV infection. One is of a previously healthy 34-year-old woman with transient high-degree AV block and cardiac magnetic resonance imaging (CMRI) findings suggestive of myocarditis and serology positive for CMV infection. After resolution of acute infection, the patient had recurrent syncopal episodes associated with intermittent high degree AV block, for which a permanent dual-chamber pacemaker was placed; the authors proposed that inflammation and edema of the conduction system causing AV block [128]. Another documents a newborn with congenital complete AV block in addition to other congenital abnormalities, suspected to be from CMV infection during early gestation [129]. Other case reports document fetal heart block with congenital CMV infection as well [130 131]. Unlike influenza, HIV, COVID, and HSV, CMV is not associated with an increased incidence of AF per a recent cohort study utilizing the National Health Insurance Database in South Korea [132].
Epstein-Barr virus
Epstein-Barr virus (EBV) is a double-stranded DNA virus of the Herpesviridae family. It is spread via salivary secretions, stem cell/organ transplantation, and blood transfusion. It uses glycoproteins which it uses to bind and enter B cells and epithelial cells. In B cells, EBV causes it to differentiate into memory B cells that spread hematogenously or where it can become latent until reactivation. It is extremely ubiquitous and estimated that nearly all people are seropositive. Primary infection can be asymptomatic but can have splenomegaly, lymphadenopathy, headache, malaise, fever, and sore throat [133]. In the immunocompromised, EBV infection can cause fulminant mononucleosis, invasive polyclonal B cell hyperplasia, and monoclonal B cell malignancies [134].
EBV also is an etiology of myocarditis as well. Sasko et al. conducted a study analyzing patients with ICDs implanted after life-threatening arrhythmias in confirmed acute viral myocarditis. The most frequently isolated virus was EBV, followed by adenovirus and coxsackie virus. Recurring arrhythmias, such VT and VF, was documented in 31 of the total 51 patients, but there was no correlation found between recurrent arrhythmia and virus type [135]. Most of the literature on arrhythmias are in the setting of myocarditis. Several case reports document ventricular arrhythmia in EBV myocarditis, including a case series of 6 patients with EBV myocarditis, all of whom had VT identified on ECG [136]. Another case report documents VT and eventually cardiac arrest in acute EBV myocarditis in an immunocompetent patient [137]. A case report documents AF with rapid ventricular response in a 19-year-old male with infectious mononucleosis complicated by a small pericardial effusion [138]. Another report documents chronic active EBV infection found to have myocarditis with the presenting ECG showing AF with premature ventricular contractions [139]. One case report documents complete heart block in EBV myocarditis in a child [140]. Another documents complete heart block and ventricular asystole leading to syncope in an immunocompetent 20-year-old female with EBV myocarditis [141].
Varicella-zoster virus
Varicella zoster virus (VZV), also known as human herpesvirus 3, is a double-stranded DNA virus of the Herpesviridae family. It is well known as the etiology of chickenpox and shingles. After initially infecting the mucosa of the upper respiratory tract, VZV enters the bloodstream, leading to viremia and later the formation of vesicles on the skin, known as chicken pox. After the resolution of the primary infection, it remains latent in the dorsal root ganglia, from which it can reactivate to cause several pathologies, such as postherpetic neuralgia and shingles [142]. Like the other herpesviruses, VZV causes myocarditis, for which most of the literature regarding arrhythmia is centered upon. It is thought that VZV has a direct cytotoxic effect on cardiac myocytes; after the acute inflammatory response, fibrosis and scarring lead to conduction abnormalities [143]. One such report is of a healthy 10-year-old boy with VZV infection who presented with syncopal episodes with ECG showing sinus bradycardia with frequent multiform ventricular ectopic beats accompanied by bursts of VT. Later monitoring showed self-terminating runs of VF and Torsades de Pointes. Echocardiogram showed decreased contractility in both ventricles; no endomyocardial biopsy was done [144]. One interesting case report discusses a 46-year-old man who presented with collapse secondary to VF for which he was cardioverted in the field. His history was only remarkable for sick contacts with chickenpox, and his physical exam was notable for vesicular lesions. He recovered and was discharged, but 8 years later presented with another syncopal episode, with CMRI showing findings consistent with myocarditis and ICD placed. Two years later, he developed VF for which he received shocks from the ICD, with a normal echocardiogram [143]. Another case report discusses VZV myocarditis induced VF in a 34-year-old man [145].
Of note, other case reports document complete AV block in VZV infection in children [146–149]. One report documents a case of VZV induced complete heart block which improved upon administration of a single dose of intravenous immune globulin [150]. One large database study from the Korean National Health Insurance Service showed that severe VZV infection requiring hospitalization was associated with a significantly increased risk of incident AF compared to the control group; this was not seen in the mild VZV group [151].
The current COVID-19 pandemic has generated a lot of interest in the arrythmias caused by SARS-CoV-2. This review highlights the growing evidence that supports the involvement of other viral infections in the development of arrhythmia. Physicians should be aware of these potentially life-threatening effects when caring for patients with these viruses, some of which are very common. Additional studies are required to better understand the complex mechanism and risk factors of cardiac arrhythmias in patients who suffered from viral infections to determine whether the processes can be reversed or even prevented.
Declarations
Compliance with ethical standards
Not applicable — since it is a review paper.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Babapoor-Farrokhran S, Rasekhi RT, Gill D, Babapoor S, Amanullah A. Arrhythmia in COVID-19. SN Compr Clin Med. 2020;2(9):1430–1435. doi: 10.1007/s42399-020-00454-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schaefer TJ, Panda PK, Wolford RW. Dengue fever. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK430732/ [PubMed]
- 3.Linares EM, Pannuti CS, Kubota LT, Thalhammer S. Immunospot assay based on fluorescent nanoparticles for dengue fever detection. Biosens Bioelectron. 2013;41:180–5. doi: 10.1016/j.bios.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Parchani A, Krishnan Vs G, Kumar VKS. Electrocardiographic changes in dengue fever: a review of literature. Int J Gen Med. 2021;14:5607–14. doi: 10.2147/IJGM.S328755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poornima H, John J. Cardiac manifestations in dengue patients in a rural tertiary care centre in Coastal Kerala. Int J Innov Res Med Sci. 2019;4(04):302 to 03. doi: 10.23958/ijirms/vol04-i04/628. [DOI] [Google Scholar]
- 6.Shah C, Vijayaraghavan G, Kartha CC. Spectrum of cardiac involvement in patients with dengue fever. Int J Cardiol. 2021;324:180–85. doi: 10.1016/j.ijcard.2020.09.034. [DOI] [PubMed] [Google Scholar]
- 7.Pialoux G, Gauzere BA, Jaureguiberry S, Strobel M. Chikungunya, an epidemic arbovirosis. Lancet Infect Dis. 2007;7(5):319–327. doi: 10.1016/S1473-3099(07)70107-X. [DOI] [PubMed] [Google Scholar]
- 8.Ojeda Rodriguez JA, Haftel A, Walker IJ. Chikungunya fever. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK534224/ [PubMed]
- 9.Obeyesekere I, Hermon Y. Arbovirus heart disease: myocarditis and cardiomyopathy following dengue and chikungunya fever–a follow-up study. Am Heart J. 1973;85(2):186–194. doi: 10.1016/0002-8703(73)90459-6. [DOI] [PubMed] [Google Scholar]
- 10.Carta KAG, Mendoza-Britto IJ, Finizola V, et al. Abstract 13292: Bradycardia as a manifestation of chikungunya myocarditis. A new threat to America. Circulation. 2016;134(suppl_1):A13292–A92. doi: 10.1161/circ.134.suppl_1.13292. [DOI] [Google Scholar]
- 11.Villamil-Gómez WE, Ramirez-Vallejo E, Cardona-Ospina JA, Silvera LA, Rodríguez-Morales AJ. Electrocardiographic alterations in patients with chikungunya fever from Sucre, Colombia: a 42-case series. Travel Med Infect Dis. 2016;14(5):510–512. doi: 10.1016/j.tmaid.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 12.Wolford RW, Schaefer TJ. Zika virus. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK430981/
- 13.Zambrana JV, Bustos Carrillo F, Burger-Calderon R, et al. Seroprevalence, risk factor, and spatial analyses of Zika virus infection after the 2016 epidemic in Managua, Nicaragua. Proc Natl Acad Sci U S A. 2018;115(37):9294–9299. doi: 10.1073/pnas.1804672115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hills SL, Fischer M, Petersen LR. Epidemiology of Zika virus infection. J Infect Dis. 2017;216(suppl_10):868–74. doi: 10.1093/infdis/jix434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scatularo CE, Ballesteros OA, Saldarriaga C, et al. Zika & heart: a systematic review. Trends Cardiovasc Med. 2022;32(1):52–58. doi: 10.1016/j.tcm.2020.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Bai C, Li S, Song S, et al. Zika virus induces myocardial immune response and myocarditis in mice. J Mol Cell Cardiol. 2020;148:103–05. doi: 10.1016/j.yjmcc.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mendoza I, Gonzalez K, Morr I, et al. Abstract 13257: A rash from the heart. Zika myocarditis manifesting with coexisting acute atrial and ventricular arrhythmias and itchy rash. Circulation. 2018;138(Suppl_1):A13257–A57. doi: 10.1161/circ.138.suppl_1.13257. [DOI] [Google Scholar]
- 18.Villamil-Gómez WE, Ramirez-Vallejo E, Rodriguez-Morales AJ. Cardiac compromise in Zika virus infection. Mayo Clin Proc. 2018;93(3):393–394. doi: 10.1016/j.mayocp.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Abdalla LF, Santos JHA, Barreto RTJ, et al. Atrial fibrillation in a patient with Zika virus infection. Virol J. 2018;15(1):23. doi: 10.1186/s12985-018-0938-2[publishedOnlineFirst:20180125]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cascella M, Rajnik M, Aleem A, Dulebohn SC, Di Napoli R. Features, evaluation, and treatment of coronavirus (COVID-19). StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK554776/ [PubMed]
- 21.Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenblatt AG, Ayers CR, Rao A, et al. New-onset atrial fibrillation in patients hospitalized with COVID-19: results from the American Heart Association COVID-19 Cardiovascular Registry. Circ Arrhythm Electrophysiol. 2022;15(5):e010666. doi: 10.1161/CIRCEP.121.010666. [DOI] [PubMed] [Google Scholar]
- 24.Mountantonakis SE, Saleh M, Fishbein J, et al. Atrial fibrillation is an independent predictor for in-hospital mortality in patients admitted with SARS-CoV-2 infection. Heart Rhythm. 2021;18(4):501–507. doi: 10.1016/j.hrthm.2021.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Z, Shao W, Zhang J, et al. Prevalence of atrial fibrillation and associated mortality among hospitalized patients with COVID-19: a systematic review and meta-analysis. Front Cardiovasc Med. 2021;8:720129. doi: 10.3389/fcvm.2021.720129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peltzer B, Manocha KK, Ying X, et al. Arrhythmic complications of patients hospitalized with COVID-19: incidence, risk factors, and outcomes. Circ Arrhythm Electrophysiol. 2020;13(10):e009121. doi: 10.1161/CIRCEP.120.009121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coromilas EJ, Kochav S, Goldenthal I, et al. Worldwide survey of COVID-19-associated arrhythmias. Circ Arrhythm Electrophysiol. 2021;14(3):e009458. doi: 10.1161/CIRCEP.120.009458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhatla A, Mayer MM, Adusumalli S, et al. COVID-19 and cardiac arrhythmias. Heart Rhythm. 2020;17(9):1439–1444. doi: 10.1016/j.hrthm.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cho JH, Namazi A, Shelton R, et al. Cardiac arrhythmias in hospitalized patients with COVID-19: a prospective observational study in the western United States. PLoS One. 2020;15(12):e0244533. doi: 10.1371/journal.pone.0244533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tariq N, Kyriakopoulos C. Group B coxsackie virus. StatPearls. Treasure Island (FL), 2022. https://pubmed.ncbi.nlm.nih.gov/32809618/ [PubMed]
- 31.Esfandiarei M, McManus BM. Molecular biology and pathogenesis of viral myocarditis. Annu Rev Pathol. 2008;3:127–55. doi: 10.1146/annurev.pathmechdis.3.121806.151534. [DOI] [PubMed] [Google Scholar]
- 32.Knowlton KU. CVB infection and mechanisms of viral cardiomyopathy. Curr Top Microbiol Immunol. 2008;323:315–35. doi: 10.1007/978-3-540-75546-3_15. [DOI] [PubMed] [Google Scholar]
- 33.Oldfors A, Eriksson BO, Kyllerman M, Martinsson T, Wahlstrom J. Dilated cardiomyopathy and the dystrophin gene: an illustrated review. Br Heart J. 1994;72(4):344–348. doi: 10.1136/hrt.72.4.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shi Y, Chen C, Lisewski U, et al. Cardiac deletion of the coxsackievirus-adenovirus receptor abolishes coxsackievirus B3 infection and prevents myocarditis in vivo. J Am Coll Cardiol. 2009;53(14):1219–1226. doi: 10.1016/j.jacc.2008.10.064. [DOI] [PubMed] [Google Scholar]
- 35.Terasaki F, Kitaura Y, Hayashi T, Nakayama Y, Deguchi H, Kawamura K. Arrhythmias in coxsackie B3 virus myocarditis. Continuous electrocardiography in conscious mice and histopathology of the heart with special reference to the conduction system. Heart Vessels Suppl. 1990;5:45–50. [PubMed] [Google Scholar]
- 36.Steinke K, Sachse F, Ettischer N, et al. Coxsackievirus B3 modulates cardiac ion channels. FASEB J. 2013;27(10):4108–4121. doi: 10.1096/fj.13-230193. [DOI] [PubMed] [Google Scholar]
- 37.Cunningham R, Silbergleit R. Viral myocarditis presenting with seizure and electrocardiographic findings of acute myocardial infarction in a 14-month-old child. Ann Emerg Med. 2000;35(6):618–622. doi: 10.1016/S0196-0644(00)70037-0. [DOI] [PubMed] [Google Scholar]
- 38.Tai YT, Lau CP, Fong PC, Li JP, Lee KL. Incessant automatic ventricular tachycardia complicating acute coxsackie B myocarditis. Cardiology. 1992;80(5–6):339–344. doi: 10.1159/000175023. [DOI] [PubMed] [Google Scholar]
- 39.Sato Y, Osaku A, Koyama S, et al. Complete atrioventricular block associated with regional myocardial scarring in a patient with coxsackie B2 myocarditis. Jpn Heart J. 1989;30(6):935–941. doi: 10.1536/ihj.30.935. [DOI] [PubMed] [Google Scholar]
- 40.Sareli P, Schamroth CL, Passias J, Schamroth L. Torsade de pointes due to coxsackie B3 myocarditis. Clin Cardiol. 1987;10(5):361–362. doi: 10.1002/clc.4960100514. [DOI] [PubMed] [Google Scholar]
- 41.Badorff C, Zeiher AM, Hohnloser SH. Torsade de pointes tachycardia as a rare manifestation of acute enteroviral myocarditis. Heart. 2001;86(5):489–490. doi: 10.1136/heart.86.5.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Usman N, Suarez M. Adenoviruses. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK559072/
- 43.Lynch JP, 3rd, Kajon AE. Adenovirus: epidemiology, global spread of novel serotypes, and advances in treatment and prevention. Semin Respir Crit Care Med. 2016;37(4):586–602. doi: 10.1055/s-0036-1584923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ghebremedhin B. Human adenovirus: viral pathogen with increasing importance. Eur J Microbiol Immunol (Bp) 2014;4(1):26–33. doi: 10.1556/EuJMI.4.2014.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bowles NE, Ni J, Kearney DL, et al. Detection of viruses in myocardial tissues by polymerase chain reaction. Evidence of adenovirus as a common cause of myocarditis in children and adults. J Am Coll Cardiol. 2003;42(3):466–72. doi: 10.1016/s0735-1097(03)00648-x. [DOI] [PubMed] [Google Scholar]
- 46.Bergelson JM, Cunningham JA, Droguett G, et al. Isolation of a common receptor for coxsackie B viruses and adenoviruses 2 and 5. Science. 1997;275(5304):1320–1323. doi: 10.1126/science.275.5304.1320. [DOI] [PubMed] [Google Scholar]
- 47.Padget RL, King DR, North MD, et al. Abstract MP114: Cardiotropic adenovirus increases arrhythmia susceptibility during acute infection. Circ Res. 2020;127(Suppl_1):AMP114–AMP14. doi: 10.1161/res.127.suppl_1.MP114. [DOI] [Google Scholar]
- 48.Savon C, Acosta B, Valdes O, et al. A myocarditis outbreak with fatal cases associated with adenovirus subgenera C among children from Havana City in 2005. J Clin Virol. 2008;43(2):152–157. doi: 10.1016/j.jcv.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 49.Valdés O, Acosta B, Piñón A, et al. First report on fatal myocarditis associated with adenovirus infection in Cuba. J Med Virol. 2008;80(10):1756–1761. doi: 10.1002/jmv.21274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Treacy A, Carr MJ, Dunford L, et al. First report of sudden death due to myocarditis caused by adenovirus serotype 3. J Clin Microbiol. 2010;48(2):642–645. doi: 10.1128/JCM.00815-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Splaingard ML, Frazier OH, Jefferson LS, Stein F, Harrison GM. Extracorporeal membrane oxygenation: its role in the survival of a child with adenoviral pneumonia and myocarditis. South Med J. 1983;76(9):1171–1173. doi: 10.1097/00007611-198309000-00030. [DOI] [PubMed] [Google Scholar]
- 52.Henson D, Mufson MA. Myocarditis and pneumonitis with type 21 adenovirus infection. Association with fatal myocarditis and pneumonitis. Am J Dis Child. 1971;121(4):334–6. doi: 10.1001/archpedi.1971.02100150108015. [DOI] [PubMed] [Google Scholar]
- 53.Camejo Leonor M, Mendez MD. Rubella. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK559040/ [PubMed]
- 54.Rubella surveillance no. 1, June 1969. In: National Communicable Disease C, ed. Atlanta, GA, 1969. https://www.cdc.gov/vaccines/pubs/surv-manual/chpt14-rubella.html
- 55.Oster ME, Riehle-Colarusso T, Correa A. An update on cardiovascular malformations in congenital rubella syndrome. Birth Defects Res A Clin Mol Teratol. 2010;88(1):1–8. doi: 10.1002/bdra.20621. [DOI] [PubMed] [Google Scholar]
- 56.Thanopoulos BD, Rokas S, Frimas CA, Mantagos SP, Beratis NG. Cardiac involvement in postnatal rubella. Acta Paediatr Scand. 1989;78(1):141–144. doi: 10.1111/j.1651-2227.1989.tb10905.x. [DOI] [PubMed] [Google Scholar]
- 57.Logue R, Hanson JF. Complete heart block in German measles. Am Heart J. 1945;30:205. doi: 10.1016/0002-8703(45)90011-1. [DOI] [Google Scholar]
- 58.Goldfinger D, Schreiber W, Wosika PH. Permanent heart block following German measles. Am J Med. 1947;2(3):320–323. doi: 10.1016/0002-9343(47)90237-4. [DOI] [PubMed] [Google Scholar]
- 59.Uemura A, Morimoto S, Hiramitsu S, et al. A case of brain stem encephalitis complicated with bifascicular block caused by rubella virus. Kokyu To Junkan. 1992;40(5):499–503. [PubMed] [Google Scholar]
- 60.Kasturi N, Matalia J, Tejwani S, Shetty BK. Wolff-Parkinson-White syndrome in congenital rubella syndrome. Indian J Pediatr. 2014;81(12):1392–1393. doi: 10.1007/s12098-014-1349-z. [DOI] [PubMed] [Google Scholar]
- 61.Fukushige J, Kuroiwa T, Ueda K, Miyazaki C, Takagi S. Supraventricular tachycardia in acquired rubella infection: a case report. Acta Paediatr Jpn. 1990;32(1):94–97. doi: 10.1111/j.1442-200x.1990.tb00790.x. [DOI] [PubMed] [Google Scholar]
- 62.Justiz Vaillant AA, Gulick PG. HIV disease current practice. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK534860/
- 63.HIV/AIDS JUNPo. Fact sheet. Global HIV & AIDS statistics 2022. https://www.unaids.org/en/resources/fact-sheet
- 64.Gupta MK, Kaminski R, Mullen B, et al. HIV-1 Nef-induced cardiotoxicity through dysregulation of autophagy. Sci Rep. 2017;7(1):8572. doi: 10.1038/s41598-017-08736-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Currier JS, Taylor A, Boyd F, et al. Coronary heart disease in HIV-infected individuals. J Acquir Immune Defic Syndr. 2003;33(4):506–512. doi: 10.1097/00126334-200308010-00012. [DOI] [PubMed] [Google Scholar]
- 66.Tseng ZH, Secemsky EA, Dowdy D, et al. Sudden cardiac death in patients with human immunodeficiency virus infection. J Am Coll Cardiol. 2012;59(21):1891–1896. doi: 10.1016/j.jacc.2012.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Abudan AA, Vaidya VR, Tripathi B, et al. Burden of arrhythmia in hospitalized HIV patients. Clin Cardiol. 2021;44(1):66–77. doi: 10.1002/clc.23506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Park DY, An S, Romero ME, et al. Incidence and risk factors of atrial fibrillation and atrial arrhythmias in people living with HIV: a systematic review and meta-analysis. J Interv Card Electrophysiol. 2022;65(1):183–191. doi: 10.1007/s10840-022-01233-w. [DOI] [PubMed] [Google Scholar]
- 69.Hsu JC, Li Y, Marcus GM, et al. Atrial fibrillation and atrial flutter in human immunodeficiency virus-infected persons: incidence, risk factors, and association with markers of HIV disease severity. J Am Coll Cardiol. 2013;61(22):2288–2295. doi: 10.1016/j.jacc.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 70.Myerson M, Kaplan-Lewis E, Poltavskiy E, Ferris D, Bang H. Prolonged QTc in HIV-infected patients: a need for routine ECG screening. J Int Assoc Provid AIDS Care. 2019;18:2325958219833926. doi: 10.1177/2325958219833926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bai YL, Liu HB, Sun B, et al. HIV Tat protein inhibits hERG K+ channels: a potential mechanism of HIV infection induced LQTs. J Mol Cell Cardiol. 2011;51(5):876–880. doi: 10.1016/j.yjmcc.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 72.Boktor SW, Hafner JW. Influenza. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK459363/
- 73.Nicholson KG. Human influenza. Textbook of Influenza 1998. https://www.cabdirect.org/cabdirect/abstract/19982013846
- 74.Filgueiras-Rama D, Vasilijevic J, Jalife J, et al. Human influenza A virus causes myocardial and cardiac-specific conduction system infections associated with early inflammation and premature death. Cardiovasc Res. 2021;117(3):876–889. doi: 10.1093/cvr/cvaa117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ukimura A, Izumi T, Matsumori A, Clinical Research Committee on Myocarditis Associated with Influenza APiJobJCS A national survey on myocarditis associated with the 2009 influenza A (H1N1) pandemic in Japan. Circ J. 2010;74(10):2193–9. doi: 10.1253/circj.cj-10-0452. [DOI] [PubMed] [Google Scholar]
- 76.Saraiya N, Singh S, Corpuz M. Fatal influenza myocarditis with incessant ventricular tachycardia. BMJ Case Rep. 2019;12(7). 10.1136/bcr-2018-228201. [DOI] [PMC free article] [PubMed]
- 77.Frustaci A, Petrosillo N, Ippolito G, Chimenti C. Transitory ventricular tachycardia associated with influenza A infection of cardiac conduction tissue. Infection. 2016;44(3):353–356. doi: 10.1007/s15010-016-0892-0. [DOI] [PubMed] [Google Scholar]
- 78.Gdynia G, Schnitzler P, Brunner E, et al. Sudden death of an immunocompetent young adult caused by novel (swine origin) influenza A/H1N1-associated myocarditis. Virchows Arch. 2011;458(3):371–376. doi: 10.1007/s00428-010-1035-0. [DOI] [PubMed] [Google Scholar]
- 79.Ergle K, Gooden JY, Ahmed MM. High-grade atrioventricular block associated with acute influenza. Tex Heart Inst J. 2020;47(3):220–23. doi: 10.14503/THIJ-18-6658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rivera-Guzman N, Del Olmo-Arroyo F, Robles-Arias CM, Rodriguez-Cintron W. Transient AV block as a hemodynamic complication of the influenza A virus: a case report. P R Health Sci J. 2016;35(3):173–175. [PubMed] [Google Scholar]
- 81.Engblom E, Ekfors TO, Meurman OH, Toivanen A, Nikoskelainen J. Fatal influenza A myocarditis with isolation of virus from the myocardium. Acta Med Scand. 1983;213(1):75–78. doi: 10.1111/j.0954-6820.1983.tb03693.x. [DOI] [PubMed] [Google Scholar]
- 82.Gokhroo RK, Barjaty HD, Bhawna K. Cardiac conduction system affection in a case of swine flu. J Assoc Physicians India. 2011;59:51–52. [PubMed] [Google Scholar]
- 83.Chang TY, Chao TF, Liu CJ, et al. The association between influenza infection, vaccination, and atrial fibrillation: a nationwide case-control study. Heart Rhythm. 2016;13(6):1189–1194. doi: 10.1016/j.hrthm.2016.01.026. [DOI] [PubMed] [Google Scholar]
- 84.Madjid M, Connolly AT, Nabutovsky Y, Safavi-Naeini P, Razavi M, Miller CC. Effect of high influenza activity on risk of ventricular arrhythmias requiring therapy in patients with implantable cardiac defibrillators and cardiac resynchronization therapy defibrillators. Am J Cardiol. 2019;124(1):44–50. doi: 10.1016/j.amjcard.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 85.Braun DK, Dominguez G, Pellett PE. Human herpesvirus 6. Clin Microbiol Rev. 1997;10(3):521–567. doi: 10.1128/CMR.10.3.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pantry SN, Medveczky PG. Latency, integration, and reactivation of human herpesvirus-6. Viruses 2017;9(7) 10.3390/v9070194 [published Online First: 20170724]. [DOI] [PMC free article] [PubMed]
- 87.Tschope C, Bock CT, Kasner M, et al. High prevalence of cardiac parvovirus B19 infection in patients with isolated left ventricular diastolic dysfunction. Circulation. 2005;111(7):879–886. doi: 10.1161/01.CIR.0000155615.68924.B3. [DOI] [PubMed] [Google Scholar]
- 88.Kuhl U, Pauschinger M, Seeberg B, et al. Viral persistence in the myocardium is associated with progressive cardiac dysfunction. Circulation. 2005;112(13):1965–1970. doi: 10.1161/CIRCULATIONAHA.105.548156. [DOI] [PubMed] [Google Scholar]
- 89.Amin A, Taghavi S, Chenaghlou M, Zare E, Kamali M, Naderi N. Targeted treatment in viral-associated inflammatory cardiomyopathy. Clin Case Rep. 2021;9(7):e04518. doi: 10.1002/ccr3.4518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yoshikawa T, Ihira M, Suzuki K, et al. Fatal acute myocarditis in an infant with human herpesvirus 6 infection. J Clin Pathol. 2001;54(10):792–795. doi: 10.1136/jcp.54.10.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Baranowski A, Buczynski M, Pajak J, et al. Fulminant herpes virus 6 myocarditis with complete atrioventricular block successfully treated with extracorporeal life support and ganciclovir. Kardiol Pol. 2020;78(12):1286–88. doi: 10.33963/KP.15587. [DOI] [PubMed] [Google Scholar]
- 92.Chang YL, Parker ME, Nuovo G, Miller JB. Human herpesvirus 6-related fulminant myocarditis and hepatitis in an immunocompetent adult with fatal outcome. Hum Pathol. 2009;40(5):740–745. doi: 10.1016/j.humpath.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 93.Nishimoto M, Nakamae H, Hayashi Y, et al. Prolonged sinus tachycardia caused by human herpesvirus 6 (HHV6) encephalomyelitis after allogeneic bone marrow transplantation. Intern Med. 2012;51(10):1265–1267. doi: 10.2169/internalmedicine.51.6640. [DOI] [PubMed] [Google Scholar]
- 94.Macri A, Crane JS. Parvoviruses. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK482245/
- 95.Tscholl V, Wielander D, Kelch F, et al. Benefit of a wearable cardioverter defibrillator for detection and therapy of arrhythmias in patients with myocarditis. ESC Heart Fail. 2021;8(4):2428–2437. doi: 10.1002/ehf2.13353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Adda J, Machado S, Eberst E, Roubille C, Macia JC, Roubille F. Parvovirus B19 infection and acute myocarditis. Intern Med. 2010;49(1):79. doi: 10.2169/internalmedicine.49.2606. [DOI] [PubMed] [Google Scholar]
- 97.Pesce R, Taffarello P, Rizzo S, et al. Fulminant myocarditis parvovirus B19 related in a young woman. J Artif Organs. 2021;24(4):498–502. doi: 10.1007/s10047-021-01247-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Koehl B, Oualha M, Lesage F, et al. Fatal parvovirus B19 myocarditis in children and possible dysimmune mechanism. Pediatr Infect Dis J. 2012;31(4):418–421. doi: 10.1097/INF.0b013e3182425786. [DOI] [PubMed] [Google Scholar]
- 99.Munro K, Croxson MC, Thomas S, Wilson NJ. Three cases of myocarditis in childhood associated with human parvovirus (B19 virus) Pediatr Cardiol. 2003;24(5):473–475. doi: 10.1007/s00246-002-0173-9. [DOI] [PubMed] [Google Scholar]
- 100.Dina J, Vabret A, Rambaud C, et al. Fulminant myocarditis associated with parvovirus B19 infection in a child. J Clin Virol. 2008;42(1):70–71. doi: 10.1016/j.jcv.2007.12.018. [DOI] [PubMed] [Google Scholar]
- 101.Buob A, Siaplaouras S, Janzen I, et al. Focal parvovirus B19 myocarditis in a patient with Brugada syndrome. Cardiol Rev. 2003;11(1):45–49. doi: 10.1097/00045415-200301000-00009. [DOI] [PubMed] [Google Scholar]
- 102.Juhasz Z, Tiszlavicz L, Kele B, et al. Sudden cardiac death from parvovirus B19 myocarditis in a young man with Brugada syndrome. J Forensic Leg Med. 2014;25:8–13. doi: 10.1016/j.jflm.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 103.Chia JK, Jackson B. Myopericarditis due to parvovirus B19 in an adult. Clin Infect Dis. 1996;23(1):200–201. doi: 10.1093/clinids/23.1.200. [DOI] [PubMed] [Google Scholar]
- 104.Mathew Jr J, Sapra A. Herpes simplex type 2. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK554427/
- 105.Saleh D, Yarrarapu SNS, Sharma S. Herpes simplex type 1. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK482197/
- 106.Chaabane S, Harfouche M, Chemaitelly H, Schwarzer G, Abu-Raddad LJ. Herpes simplex virus type 1 epidemiology in the Middle East and North Africa: systematic review, meta-analyses, and meta-regressions. Sci Rep. 2019;9(1):1136. doi: 10.1038/s41598-018-37833-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bradley H, Markowitz LE, Gibson T, McQuillan GM. Seroprevalence of herpes simplex virus types 1 and 2–United States, 1999–2010. J Infect Dis. 2014;209(3):325–333. doi: 10.1093/infdis/jit458. [DOI] [PubMed] [Google Scholar]
- 108.Colombo D, Albore M, Nonno FD, et al. Fatal fulminant HSV-2 myocarditis: a complicated presentation. Int J Infect Dis. 2022;114:124–27. doi: 10.1016/j.ijid.2021.10.046. [DOI] [PubMed] [Google Scholar]
- 109.Koga M, Fujiwara M, Ariga S, et al. CD8+ T-lymphocytes infiltrate the myocardium in fulminant herpes virus myocarditis. Pediatr Pathol Mol Med. 2001;20(3):189–195. doi: 10.1080/15513810109168611. [DOI] [PubMed] [Google Scholar]
- 110.Smith BK, Cook MJ, Prior DL. Sinus node arrest secondary to HSV encephalitis. J Clin Neurosci. 2008;15(9):1053–1056. doi: 10.1016/j.jocn.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 111.Braiman D, Konstantino Y, Westreich R. When the brain slows the heart-herpes encephalitis and sinus arrest: a case report. Eur Heart J Case Rep. 2021;5(8):ytab254. doi: 10.1093/ehjcr/ytab254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Alsolaiman MM, Alsolaiman F, Bassas S, Amin DK. Viral encephalitis associated with reversible asystole due to sinoatrial arrest. South Med J. 2001;94(5):540–541. doi: 10.1097/00007611-200105000-00023. [DOI] [PubMed] [Google Scholar]
- 113.Nicol PP TJ, Joseph T. Herpes simplex encephalitis, an unusual cause of sinus node dysfunction: case report and literature review. Int J Clin Cardiol 2015;2(4) 10.23937/2378-2951/1410042.
- 114.Pollock S, Reid H, Klapper P, Metcalfe RA, Ahmed N. Herpes simplex encephalitis presenting as the sick sinus syndrome. J Neurol Neurosurg Psychiatry. 1986;49(3):331–332. doi: 10.1136/jnnp.49.3.331-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chiang CH, Huang CC, Chan WL, et al. Herpes simplex virus infection and risk of atrial fibrillation: a nationwide study. Int J Cardiol. 2013;164(2):201–204. doi: 10.1016/j.ijcard.2011.06.126. [DOI] [PubMed] [Google Scholar]
- 116.Gupta M, Shorman M. Cytomegalovirus. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK459185/
- 117.Zheng QY, Huynh KT, van Zuylen WJ, Craig ME, Rawlinson WD. Cytomegalovirus infection in day care centres: a systematic review and meta-analysis of prevalence of infection in children. Rev Med Virol. 2019;29(1):e2011. doi: 10.1002/rmv.2011. [DOI] [PubMed] [Google Scholar]
- 118.Nosotti M, Tarsia P, Morlacchi LC. Infections after lung transplantation. J Thorac Dis. 2018;10(6):3849–68. doi: 10.21037/jtd.2018.05.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cannon MJ, Schmid DS, Hyde TB. Review of cytomegalovirus seroprevalence and demographic characteristics associated with infection. Rev Med Virol. 2010;20(4):202–213. doi: 10.1002/rmv.655. [DOI] [PubMed] [Google Scholar]
- 120.Kyto V, Vuorinen T, Saukko P, et al. Cytomegalovirus infection of the heart is common in patients with fatal myocarditis. Clin Infect Dis. 2005;40(5):683–688. doi: 10.1086/427804. [DOI] [PubMed] [Google Scholar]
- 121.Roubille C, Brunel AS, Gahide G, Vernhet Kovacsik H, Le Quellec A. Cytomegalovirus (CMV) and acute myocarditis in an immunocompetent patient. Intern Med. 2010;49(2):131–133. doi: 10.2169/internalmedicine.49.2313. [DOI] [PubMed] [Google Scholar]
- 122.Vanstechelman F, Vandekerckhove H. Cytomegalovirus myocarditis in an immunocompetent patient. Acta Cardiol. 2012;67(2):257–260. doi: 10.1080/ac.67.2.2154221. [DOI] [PubMed] [Google Scholar]
- 123.Padala SK, Kumar A, Padala S. Fulminant cytomegalovirus myocarditis in an immunocompetent host: resolution with oral valganciclovir. Tex Heart Inst J. 2014;41(5):523–9. doi: 10.14503/THIJ-13-3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Waris E, Rasanen O, Kreus KE, Kreus R. Fatal cytomegalovirus disease in a previously healthy adult. Scand J Infect Dis. 1972;4(1):61–67. doi: 10.3109/inf.1972.4.issue-1.13. [DOI] [PubMed] [Google Scholar]
- 125.Dietz AJ., Jr Cytomegalovirus infection with carditis, hepatitis, and anemia. Postgrad Med. 1981;70(3):203–8. doi: 10.1080/00325481.1981.11715865. [DOI] [PubMed] [Google Scholar]
- 126.Wilson RS, Morris TH, Rees JR. Cytomegalovirus myocarditis. Br Heart J. 1972;34(8):865–868. doi: 10.1136/hrt.34.8.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.McCormack JG, Bowler SD, Donnelly JE, Steadman C. Successful treatment of severe cytomegalovirus infection with ganciclovir in an immunocompetent host. Clin Infect Dis. 1998;26(4):1007–1008. doi: 10.1086/517635. [DOI] [PubMed] [Google Scholar]
- 128.Dilaveris P, Dimitriadis K, Lazaros G, Gatzoulis K, Stefanadis C. Cytomegalovirus infection: a potential threat to atrioventricular conduction? Am J Med. 2010;123(8):e3–4. doi: 10.1016/j.amjmed.2009.12.036. [DOI] [PubMed] [Google Scholar]
- 129.Mulder TJ, Niyazov DM, Kattash MM, Longo SA, Robichaux Iii AG, Snyder CS. A newborn with congenital complete atrioventricular block, lissencephaly, and skeletal abnormalities: a case of suspected cytomegalovirus infection. Congenit Heart Dis. 2010;5(5):486–490. doi: 10.1111/j.1747-0803.2010.00390.x. [DOI] [PubMed] [Google Scholar]
- 130.Lewis PE, 2nd, Cefalo RC, Zaritsky AL. Fetal heart block caused by cytomegalovirus. Am J Obstet Gynecol. 1980;136(7):967–968. doi: 10.1016/0002-9378(80)91064-9. [DOI] [PubMed] [Google Scholar]
- 131.Karn K, Julian TM, Ogburn PL., Jr Fetal heart block associated with congenital cytomegalovirus infection A case report. J Reprod Med. 1984;29(4):278–280. [PubMed] [Google Scholar]
- 132.Lee KH, Yoo SG, Han KD, La Y, Kwon DE, Han SH. Association of cytomegalovirus diseases with newly developed myocardial infarction and congestive heart failure: data from a national population-based cohort. Arch Med Sci. 2022;18(5):1188–1198. doi: 10.5114/aoms/105157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hoover K, Higginbotham K. Epstein Barr virus. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK559285/ [PubMed]
- 134.List AF, Greco FA, Vogler LB. Lymphoproliferative diseases in immunocompromised hosts: the role of Epstein-Barr virus. J Clin Oncol. 1987;5(10):1673–1689. doi: 10.1200/JCO.1987.5.10.1673. [DOI] [PubMed] [Google Scholar]
- 135.Sasko B, Patschan D, Nordbeck P, et al. Secondary prevention of potentially life-threatening arrhythmia using implantable cardioverter defibrillators in patients with biopsy-proven viral myocarditis and preserved ejection fraction. Cardiology. 2021;146(2):213–221. doi: 10.1159/000511120. [DOI] [PubMed] [Google Scholar]
- 136.Mavrogeni S, Spargias K, Bratis C, Kolovou G, Papadopoulou E, Pavlides G. EBV infection as a cause of VT: evaluation by CMR. JACC Cardiovasc Imaging. 2011;4(5):561–562. doi: 10.1016/j.jcmg.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 137.Watanabe M, Panetta GL, Piccirillo F, et al. Acute Epstein-Barr related myocarditis: an unusual but life-threatening disease in an immunocompetent patient. J Cardiol Cases. 2020;21(4):137–140. doi: 10.1016/j.jccase.2019.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Aghenta A, Osowo A, Thomas J. Symptomatic atrial fibrillation with infectious mononucleosis. Can Fam Physician. 2008;54(5):695–696. [PMC free article] [PubMed] [Google Scholar]
- 139.Takano H, Nakagawa K, Ishio N, et al. Active myocarditis in a patient with chronic active Epstein-Barr virus infection. Int J Cardiol. 2008;130(1):e11–e13. doi: 10.1016/j.ijcard.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 140.Reitman MJ, Zirin HJ, DeAngelis CJ. Complete heart block in Epstein-Barr myocarditis. Pediatrics. 1978;62(5):847–849. doi: 10.1542/peds.62.5.847. [DOI] [PubMed] [Google Scholar]
- 141.Leis P, Correa A, Setareh-Shenas S, Paka P, Mehta D. A heart-stopping encounter: a case of complete heart block from Epstein-Barr virus-associated myocarditis. J Am Coll Cardiol. 2020;75(11):2841–2941. doi: 10.1016/S0735-1097(20)33468-9. [DOI] [Google Scholar]
- 142.Ayoade F, Kumar S. Varicella Zoster. StatPearls. Treasure Island (FL), 2022. https://www.ncbi.nlm.nih.gov/books/NBK448191/
- 143.Ioannou A, Tsappa I, Metaxa S, Missouris CG. Ventricular fibrillation following varicella zoster myocarditis. Case Rep Cardiol. 2017;2017:1017686. doi: 10.1155/2017/1017686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Fiddler GI, Campbell RW, Pottage A, Godman MJ. Varicella myocarditis presenting with unusual ventricular arrhythmias. Br Heart J. 1977;39(10):1150–1153. doi: 10.1136/hrt.39.10.1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Dennison P, Zaremba E. Varicella zoster induced cardiac dysfunction: a case report. Emerg Med J. 2007;24(9):682–683. doi: 10.1136/emj.2006.034280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Nurnberg JH, Senft G, Sperling P, Lange PE. A delayed life-threatening complication after uneventful varicella infection: transient complete heart block. Klin Padiatr. 2002;214(3):113–116. doi: 10.1055/s-2002-30145. [DOI] [PubMed] [Google Scholar]
- 147.Rich R, McErlean M. Complete heart block in a child with varicella. Am J Emerg Med. 1993;11(6):602–605. doi: 10.1016/0735-6757(93)90011-y. [DOI] [PubMed] [Google Scholar]
- 148.Ettedgui JA, Ladusans E, Bamford M. Complete heart block as a complication of varicella. Int J Cardiol. 1987;14(3):362–365. doi: 10.1016/0167-5273(87)90208-7. [DOI] [PubMed] [Google Scholar]
- 149.Katsuta T, Kato H, Kaneko Y, et al. Complete atrioventricular block as a complication of varicella in children. Pediatr Infect Dis J. 2011;30(5):445–446. doi: 10.1097/INF.0b013e3182011286. [DOI] [PubMed] [Google Scholar]
- 150.Uysal F, Bostan OM, Cetin B, Uysal B, Guney B, Cil E. Complete atrioventricular block as a complication of varicella infection in a child: recovery with a single dose of intravenous immunoglobulin therapy. Clin Pediatr (Phila) 2016;55(7):677–679. doi: 10.1177/0009922816629617. [DOI] [PubMed] [Google Scholar]
- 151.Cha M-J, Seo H-M, Choi E-K, et al. Increased risk of atrial fibrillation in the early period after herpes zoster infection: a nationwide population-based case-control study. Jkms. 2018;33(22):0–0. doi: 10.3346/jkms.2018.33.e160. [DOI] [PMC free article] [PubMed] [Google Scholar]