Abstract
BACKGROUND
One of the most overspread postural abnormalities is forward head posture (FHP) and it is described as head projection anteriorly in relation to the trunk which appears mainly in sagittal plane. Scapular stabilization exercise (SSE) is capable of restoring each of thoracic cage and head neutral optimum position by neck and shoulder muscles interactions and through controlling scapular position and movement
AIM
This study was conducted to investigate the impact of adding scapular stabilization (SSE) to postural correctional exercises (PCE) on symptomatic FHP.
DESIGN
The pre-post single-masking (assessor) randomized experimental trial.
SETTING
Participants with postural dysfunction in form of FHP admitted to outer clinic of the Faculty of Physical Therapy.
POPULATION
Sixty participants (20 to 35 years) with symptomatic FHP and recruited from outer clinic at faculty of physical therapy.
METHODS
Participants were allocated randomly by opaque sealed envelope to two groups who are referred from an orthopedist: Group “A” received SSE and postural correction exercises, whereas Group “B” received only postural correctional exercises; treatments were performed three times/week for 10 weeks. The craniovertebral angle, pressure pain threshold, cervical flexor and extensor muscles endurance, Arabic neck disability index, upper trapezius and sternocleidomastoid muscle root mean square during rest and activity were used to evaluate the patients’ pretreatment and post-treatment.
RESULTS
within group analysis for sixty participants reported statistical significant difference between baseline and post-treatment as P value <0.05 with more refinement in stabilization exercise group.
CONCLUSIONS
Adding SSEs to PCEs is more effective method than PCEs seldom for the management of FHP patients.
CLINICAL REHABILITATION IMPACT
Both scapular stabilization and postural correction exercise increase craniovertebral angle and pressure pain threshold (PPT) and decrease muscle activity and disability. Scapular stabilization alone increase craniovertebral angle and PPT and decrease muscle activity and disability more than postural correction exercise. In addition of statistical significant difference in all variables but there were clinical change in disability only.
Key words: Exercises, Electromyography, Posture
It was reported in the latest surveys that about 75% of the whole world population takes up most of their time on high technology devices such as smartphones, iPads, laptops, electronic readers, and video-game devices.1 Prolonged inherence of static position due to overuse of such devices, ultimately lead to spasm of neck muscles and assumption of awkward postures2. Prolonged sitting in specific static posture is the main cause of postural abnormalities such as forward head posture (FHP), which is identified by head anteriorly displaced in regard to the line of gravity.3 FHP causes exaggerated extension at the upper cervical spine (C1-C3) and flexion at the lower cervical spine (C4-C7) which is a consequence of changing head position in relation to the line of gravity.4, 5
FHP has been found to be a possible hazard element for shoulder aches,6 abnormal scapular kinematics,7 myofascial pain syndrome7 and apparently producing imbalance of several neck muscles, as the upper cervical spine flexors, scapular retractor muscles, suboccipitals, scalenus anterior, upper trapezius and sternocleidomastoid, levator scapulae, and semispinalis capitis post major8 Besides, assuming such posture results in over activation of the neck extensor and the upper and lower trapezius muscles even during rest9. Similarly, the load on posterior structures of cervical spine as ligaments, joints, and muscles is magnified in response of prolonged forward posture of the head and lead to change of both scapular position and kinematics.10
Furthermore, it was reported that FHP lead to spasm and shortening of cervical extensor muscles, inhibition of cervical flexor muscles, in addition awkward scapular position and movement11. Also, inhibition of mid scapular retractor (i.e., Rhomboids, Middle and Lower fibers of trapezius) and spasm of Pectoralis muscles is reported.3 Some compensatory actions occur in FHP, the upper trapezius muscle over activated to overcome weakened cervical extensor muscles in order to carry the weight of the head,12 and the sternocleidomastoid to overcome inhibited cervical flexors.13 Both of these muscles have shown increment of the electromyographic activity.12
These compensatory actions from UT and SCM muscles executed to prevent damage to the body and decrease pain14 but this action in the same time lead to malalignment in the neck, posture tilting, and muscle imbalance.15 For resolving this difficult; patients with FHP should restore the normal body alignment. This involves strengthening the weak muscles (deep cervical flexor muscles) and lengthening of the shorted muscles (cervical extensor).16 Patients with FHP not only have problems around the neck but also around the neck-shoulder muscles, in addition abnormal postures such as rounded shoulders.17 In order to correct head and neck posture, it is important to improve the thoracic spine.18 Therefore, scapular stabilization exercise (SSE) is used as an effective way to recover the imbalance in posture and muscles19
SSE is effective in the early rehabilitation and the balance of both sides of the trapezius with the movement and couple motion of the scapula20 and also for placing cage of the thorax at the normal central position, restore normal alignment of the neck and correct its awkward posture through correcting position and restoring kinematics of the scapula.21 However, there is lack of randomized studies investigating the influence of adding SSEs to postural correctional (PCE) on correcting FHP in symptomatic patients. Therefore, the aim of our study was to investigate, through a randomized study, the impact of scapula stabilizing exercises on PCE on correcting FHP in symptomatic patients” and answer the following question; was there a difference between scapular stabilization in addition to PCE and PCE alone on craniovetebral angle (CVA), pressure pain threshold (PPT), endurance of flexor and extensor muscles, SCM and UT muscles activity and disability in patients with FHP?
Materials and methods
Study design
This pre-post single-masking (assessor) parallel randomized experimental trial was conducted in acquiescence with the 1964 Helsinki Declaration and its subsequent modifications and the guidelines of Consolidated Standards of Reporting Trials. This trial conducted from July 2021 to the end of September 2021 at out-patient clinic at Faculty of Physical Therapy, Cairo University. The ethical unique number for this trial was P. T. REC/012/0023244 and the date was 15/6/2021 from Research Ethics Committee at Faculty of Physical therapy, Cairo University. Prof/Dr: Amira El Tohamy was the chairperson of research ethics committee. The other unique number from Clinical Trials Registry (Registry ID: NCT 04959942). Before participating in study, the participants signed a written consent form and were given details about the study.
Sample size
The sample-size calculated based on t-test, power 80%, type I error 5% two sided. The effect size (0.82) calculated on the primary outcome (CVA) from pilot study on 10 subjects. The minimum sample size =50 and to account for drop out, the number increased by 10%. The appropriate sample was 60 subjects. G* Power version 3.1.9.2 (Franz Faul, Uni Kiel, Germany) was used for calculation.
Participants and randomization
A computer-generated block randomization was used to sort the subjects randomly into two groups. The size of the block was four to avoid bias and assures balance between groups. To ensure the concealment of the allocation, randomization codes were placed in sealed envelopes with sequential numbers. The first author, who was not involved in data collection, applied randomization, the second author opened the opaque sealed envelope and applied the treatment, the fourth author gathered the data and was blinded to the allocation stage, and the third author analyzed and interpret the data.
The patients included in this study if they have CVA equal or less than 50, and had cervical pain for more than 6 weeks and had visited an orthopedist clinic.22 Patients were excluded, if they had clinical conditions other than MNP, like 1) cervical spine spondylosis; 2) fractures or cervical spinal surgery; 3) Cervical or shoulder neurological movement disorder; 4) temporo-mandibular surgery; 5) pathologic trauma. Eight patients were excluded because they did not meet the inclusion criteria23 (Figure 1, 2).
Figure 1.
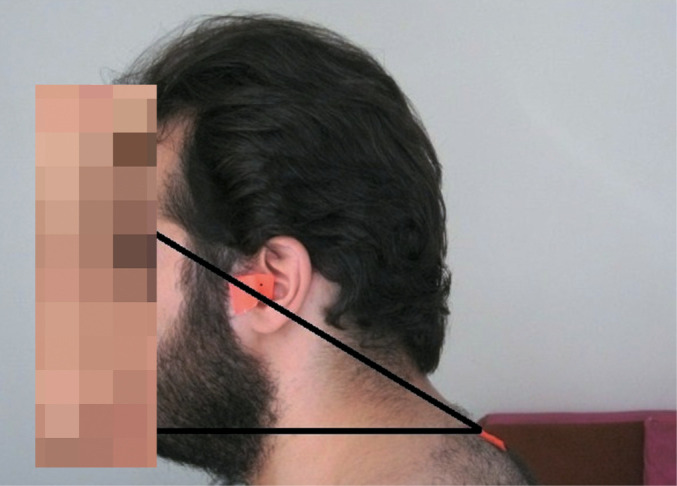
—CVA measurement.
Figure 2.
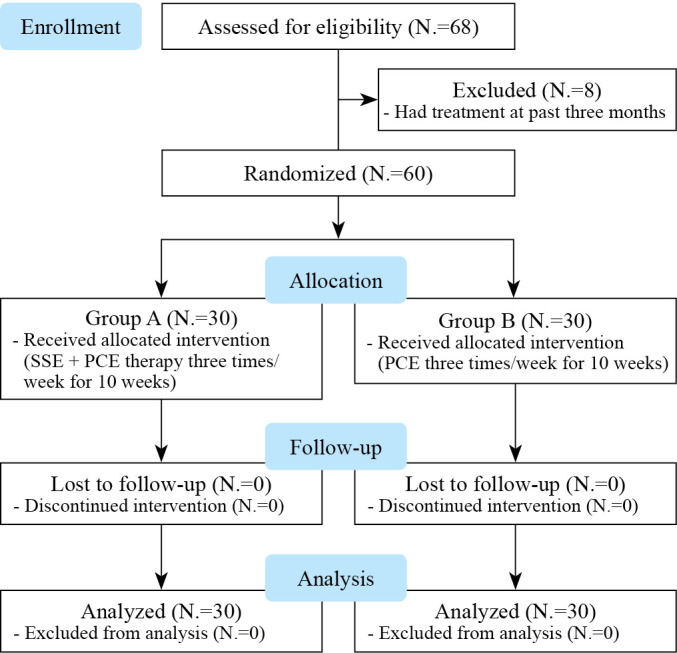
—CONSORT flow chart.
Outcome measures
The outcomes of the study were measured before beginning the treatment program and after 10 weeks of study. Outcome measures were neck alignment assessed by calculating CVA by photographing (Canon power shot A490, 3.3 optical zoom, 10 mega pixels, China), PPT measured by the Commander Algometry (JTECH medical, Midvale, UT, USA), endurance of cervical flexor and extensor muscles assessed by using Stop watch. The Arabic Neck Disability Index (ANDI) was used to measure neck function, ultimately, muscle activity in the form of root mean square (RMS) at rest and activity via EMG.
CVA
Lateral photographing is a valid and reliable instrument to objectively measure FHP.24 CVA is the angle between a horizontal line passing across C7 and a line passing over C7 to the tragus of the ear.25 Adhesive markers were fixed on the tragus of the ear and the spinous process of the C7 vertebra (Figure 1).
PPT
The Commander Algometry (JTECH medical, Midvale, UT, USA) is a valid tool and commonly used for the assessment of the PPT.26 It is a handheld device that applies manual pressure to assess pain sensitivity of deeper structures. Its tip was positioned on the trigger area on UT and pressure was slowly increased by 1 kg/s. When the patients sensed discomfort and verified it verbally, the value of pressure was recorded in kilograms per square centimeters. The process was repeated three times with 60 s intervals in between.27
Endurance of cervical muscles
Neck flexion endurance
NFET is considered a suitable and reliable technique for non-instrumented evaluation of endurance of DNF muscle. It is considered to have good to excellent intra-rater reliability.28 The test was done while the patient was lying in the supine and crook positions with maintaining the chin tucked to the maximum and isometrically maintained, the patient was asked to lift the head and neck till the head was around 2.5 cm off the plinth with keeping the chin tucked to the chest. If the patient lost the retraction of the chin, a verbal command was given such as “ keep your chin in.”28 Normal Value: 34 sec.29
Neck extension endurance
NEET is maybe the most common one, as it is a simple test using by the clinicians without any complex tools. The patients was instructed to lie in a prone position with her head out of the plinth and held on a stool, her arms were at side and a physiotherapy belt was tightened and secured across the level of T6 to support the upper thoracic spine. A perpendicular line was secured beneath the Velcro strap attached around her head, which hung to just short of the floor. Then she was asked to tuck the chin in and hold the head stable in a straight position while the stool was removing. At this moment, the stopwatch was started to record the endurance time in seconds.30 Sixty seconds are the target time for the test, but if any subject could able to hold for longer, they are encouraged to do so, and this was recorded as their holding time.30
Neck function
The neck function was assessed by the ANDI tool which has a moderate value of reliability and validity.31 It includes 10 sets, each including six choices (0-5). Scores of 0-4 indicate no disability; 5-15, mild disability; 5-14, moderate disability; 25-34, severe disability; and >34, complete disability.32 Patients were asked to pick the choice that described their function.
Electro myographic activity of UT and SCM Muscles
First skin of the subject prepared in a standard way before application of electrode to minimalize electrical impedance. After cleaning and abrading the skin, bipolar surface electrodes (Ag/AgCl) were positioned over the UT and SCM muscles consistent with established Surface Electromyography for the Non-Invasive Assessment of Muscles guidelines.33 Placement of electrodes for the UT, 1 electrode was located 2 cm lateral from the midpoint of a line connecting spinous process of C7 and the acromion. A second electrode was located 1 cm laterally on the same line, and the reference electrode was located on the C7 spinous process. For the SCM, electrodes were positioned at the lower third of the line joining the mastoid process and the sternal notch. The reference electrode was positioned over the acromion process.34
For maximum voluntary isometric contraction (MVIC) of the UT, the patient was instructed to do a shoulder shrug against resistance given by the physiotherapist. For MVIC of the SCM, the patient was asked to lie in a supine position and asked to flex the neck against resistance given by the examiner on the forehead.35 These MVIC tests were repeated 3 times for each muscle, and the mean of the 3 tests was recorded for further assessments. After each MVIC effort, a 30 seconds rest period was given.
Electromyographic signals were measured and analyzed by an analog-to-digital convertor (the MyoSystem 1400A Noraxon, Scottsdale, AZ, USA). Data collected at a sampling rate of 1000 Hz were measured with a combined preamplifier gain of 100<&thins P>000 to 10,000 and a bandwidth of 20 to 450 Hz36. The EMG activity of both UT and SCM muscles was measured at rest for 10 seconds when the patient was in a relaxed sitting position. In addition to resting EMG activity, these muscles were assessed during activity, specifically 120° of shoulder abduction for the UT in a standing position and neck flexion in a supine position for the SCM. The mean root-mean-square of 3 contractions was taken for evaluation.37 The root-mean-square of EMG signals was recorded during rest and activity for both muscles were obtained and normalized by their respective MVICs to obtain muscle activity at rest and during activity in terms of %MVIC.
Interventions
Group (A) received SSE and PCE three times a week for 10 weeks, whereas Group (B) received PCE only three times a week for 10 weeks.
SSEs
Consisted of five phases. In supine lying position, the patient was instructed to take a deep breath in order to relax her body. In crook-lying position, she raised her dominant arm to 90° shoulder flexion with full extension of elbow and scapular protraction.35 In quadruped position, she lifted up her arms alternatively with shoulder abduction and 120 ° flexion. In sitting position, with 90° knee flexion on a stool or bed without backrest, she held a pair of dumbbells (2 kg) in each hand and lifted them up laterally while maintaining scapulae’s height below 80°. The patient was instructed to hold each stage for 10 seconds and then return to the starting position and three sets of 10 repetitions with 30-second pause in between were completed. In sitting position, the patient was sitting in front of a mirror. Then, she was asked to check and correct her posture by herself.38
As for the progression of SSE, T to Y the patient was instructed to lie in prone lying position on Swiss ball with arms abducted to 90° (the letter T); then she asked to flex her elbows to 90°, retract her scapulae and externally rotate her arms while keeping her arm in 90° abductions. While maintaining the retraction of scapula, she asked to raise her arms above head and extend the elbow while her arm flexed and abducted to 120° (the letter Y).
As for T to Y to W the patient was instructed to lie in prone lying position on Swiss ball and formed the letter T (as described before) then she changed her position to letter Y with her thumbs up. She depressed and retracted scapulae while raising her arm 10 -15 cm. While maintaining the retraction of scapula; she flexed her elbows and extended her shoulders to form the letter W.
As for scapular protraction, the patient was instructed to lie in prone lying position, with her toes and forearms held the body, and then she pushed up 1-2 cm and protracted her scapulae.
Scapular-clock exercise was the second exercise we used to ease the motions of the scapulae (elevation, depression, protraction, and retraction) in addition to joint kinesthesia (to develop proprioceptive consciousness of positioning, posture and safe movement) and range of motion. The patient was asked to stand beside a wall and put her hand on a ball and press it while moving it to show 3, 6, 9 or 12 o’clock based on an imaginary clock she had on her mind.39
PCEs
The program consisted of four exercises; two of them strengthening (deep cervical flexors and scapular retractors) and the other two stretching: cervical extensors (sub-occipital muscles and pectoral muscles). The program was based on a program by Harman.3
As for strengthening of deep cervical flexor muscles, each patient was instructed to sit with her arms relaxed by her side. The therapist lightly touched the area under the nose and above the lip then, asked the patient to tuck her head in and down.
As for strengthening of the scapular retractor muscles, the patient started this exercise with sitting on a chair without backrest. The patient was asked to squeeze the inferior angle of the scapula together; to retract them; while the therapist resisted this motion gently. The patient was asked to imagine grasping a quarter between the shoulder blades. Then, the patient was asked to stand with her hands holding together across the lower back; to adduct the scapulae.
These exercises were applied for three sets with 12 repetitions per set, with 6 seconds hold.
Stretching exercises
In stretching of sub-occipital muscles, the patient assumed sitting position. Then, after identification the spinous process of the 2nd cervical vertebra, it was stabilized by the therapist’s thumb. After that, the patient was asked to slowly nod, doing just a tipping motion of the head on the upper spine.
In stretching of the pectoralis major muscle, the patient assumed sitting position with her hands behind the head, in order to stretch sternal head, shoulders should be abducted and externally rotated 90° and in order to stretch the costal division, arm should be raised to approximately 135 degrees. Then, the therapist applied passive stretch at the end of range of motion.
The exercise was performed three times with 30 seconds hold in between.
Statistical analysis
The data analysis was carried out by using SPSS software version 23.0 (Armonk, NY, USA). Descriptive statistics were calculated before the beginning of treatment and after ten weeks of intervention. For checking the normality of data, Shapiro-Wilk’s test was used. According to the results of normality distribution, mixed-design multivariate analyses of variance (MANOVA) was used to identify any change between both groups on the combined mean change scores of CVA, PPT, ANDI and RMS. Wilks’ lambda was used to detect the F value. When there is significant difference between both groups multiple pairwise comparisons by Bonferroni were applied. Un-paired t-test was used to identify between groups changes in physical characteristics of subjects. Chi-square (χ2) test was used to clarify the difference between groups at sex and the affected side.
Results
Figure 2 illustrates the flow chart of the study, which demonstrated that sixty eight subjects with symptomatic FHP were recruited from the outpatient clinic at the faculty of physical therapy in Giza governorate. Eight subjects were excluded because they had received treatment within the previous three months. So, sixty people were eligible to participate in the study and were randomly assigned to either the experimental or control groups. For physical characteristics analysis between groups; Un-paired t-test was used and informed no statistical significance difference with regard to age, weight, height, BMI, six and affected side distribution between both groups as P>0.05 (Table I).
Table I. —Demographic data of experimental and control groups.
| Mean±SD | P value | ||
|---|---|---|---|
| Experimental group | Control group | ||
| Age (years) | 24.32±1.25 | 25.47±3.56 | 0.61 b |
| Weight (kg) | 66.8±8.71 | 69.65±9.21 | 0.32 b |
| Height (cm) | 167.8±11.79 | 172.85±8.89 | 0.13 b |
| BMI (kg/m2) | 23.6±0.89 | 23.89±0.23 | 0.48 b |
| Sex | χ2=1.1 0.29 b |
||
| Males | 14 (47%) | 10 (33%) | |
| Females | 16 (53%) | 20 (67%) | |
| Affected side | χ2=0.57 0.44 b |
||
| Right | 25 (83%) | 27 (90%) | |
| Left | 5 (17%) | 3 (10%) | |
bno significance difference; x-par: mean; SD: standard deviation; P value: significance level; BMI: Body Mass Index; χ2: chi square test.
Results of outcome measures; CVA, PPT, CROM, NFE, NEE, ANDI, and RMS:
Generally, MANOVA reported statistically significant difference between both groups as Wilks’ Lambda (λ) value=0.16, f=13.59 and P=0.001. Also, there were statistical significant effect at times as λ=0.005, f=333.74 and P=0.0001. Finally, there were significant interaction between groups and time as λ=0.09, f=16.82 and P=0.0001.
Univariate test revealed statistically significant effect at time (pre and post-treatment) in CVA as f=192.1 and P=0.0001, in PPT at right and left side the f-value= 35.9 and 89.53 respectively and P=0.0001 at both sides.in flexion and extension endurance test the f-value=366.1 and 241.1 respectively and P=0.0001 at both tests. At UT right and left side in resting position; the f=101.17 and 117.41 respectively and P=0.0001 at both sides. During activity the f-value=258.16 and 191.3 respectively and P=0.0001 at both sides. At resting position of SCM at right and left side the f-value=275.2 and 235.25 respectively and in activity f=285.3 and 289 respectively and P=0.0001. Finally, f=293.3 and P=0.001 in ANDI.
In the same line Univariate Test revealed statistical significant effect at treatment in CVA as f=20.41 and P=0.001, in PPT at right and left side the f-value= 16.18 and 5.38 respectively and P=0.0001 at right and 0.02 at left side. In flexion and extension endurance test the f-value=10.2 and 20.8 respectively and P=0.01 at flexion and 0.0001 at extension endurance. At UT right and left side in resting position; the f=5.41 and 11.13 respectively and P=0.02 and 0.002 respectively. During activity the f-value=23.1 and 38.01 respectively and P=0.0001 at both sides. At resting position of SCM at right and left side the f-value=2.36 and 0.64 and P= 0.01 and 0.12 respectively and in activity f=11.73 and 19.47 respectively and P=0.001 and 0.0001 respectively. Finally, f=31.8 and P=0.0001 in ANDI.
Within and between group analysis:
In CVA and PPT at both sides there were statistically significant increase in both groups as P<0.05 with more favor to experimental group. Between groups analysis at post-treatment there were statistically significant difference as P<0.05. Also, there was statistical significant increase in flexion and extension endurance test in both groups with more favor to experimental group. Between groups analysis at post-treatment there were statistical significant difference as P<0.05.
In UT muscle the RMS value during rest and activity decreased significantly as both groups as P<0.05 with more favor to experimental group and also there were statistical significant difference at post-treatment between both groups. In RMS of SCM at rest and activity there were significant decreases at both groups with more favor to experimental groups and also there were statistical significant difference between both groups at post-treatment except for left SCM at resting position. Finally the disability decreased in both groups with more favor to experimental group (Table II).
Table II. —Between and within group analysis of CVA, PPT, NFE, NEE, ANDI, and RMS during rest and activity.
| Outcome measures | Mean±SD | P value between |
F value between |
|
|---|---|---|---|---|
| Experimental group | Control group | |||
| CVA | ||||
| Baseline | 39.58±3.97 | 39.02±2.86 | 0.62 | 0.25 |
| Post-treatment | 52.89±4.18 | 45.66±2.97 | 0.0001 a | 39.6 |
| P value (within) | 0.0001 a | 0.001 a | ||
| Mean difference | -13.31 | -6.64 | ||
| 95% (CI) | -15.3 to-11.2 | -8.7 to-4.58 | ||
| PPT right | ||||
| Baseline | 1.62±0.22 | 1.55±0.38 | 0.45 b | 0.57 |
| Post-treatment | 2.41±0.41 | 1.83±0.45 | 0.0001 a | 16.99 |
| P value (within) | 0.0001 a | 0.03 a | ||
| Mean difference | -0.79 | -0.28 | ||
| 95% (CI) | -1.05 to -0.53 | -0.54 to -0.03 | ||
| PPT left | ||||
| Baseline | 1.15±0.35 | 1.24±0.31 | 0.4 b | 0.71 |
| Post-treatment | 2.21±0.42 | 1.71±0.39 | 0.001 a | 14.18 |
| P value (within) | 0.0001 a | 0.0001 a | ||
| Mean difference | -1.04 | -0.47 | ||
| 95% (CI) | -1.27 to -0.81 | -0.7 to -0.24 | ||
| ANDI | ||||
| Baseline | 27.6±2.32 | 28.4±2.64 | 0.31 b | 1.03 |
| Post-treatment | 12.2±2.44 | 17.1±1.33 | 0.0001 a | 62.06 |
| P value (within) | 0.0001 a | 0.0001 a | ||
| Mean difference | 15.40 | 11.30 | ||
| 95% (CI) | 13.97 to 16.82 | 9.87 to 12.72 | ||
| Flexion endurance | ||||
| Baseline | 21.8±3.99 | 23.1±2.61 | 0.23 b | 1.48 |
| Post-treatment | 37.5±3.03 | 33.65±3.2 | 0.0001 a | 14.99 |
| P value (within) | 0.0001 a | 0.0001 a | ||
| Mean difference | -15.7 | -10.55 | ||
| 95% (CI) | -17.6 to -13.7 | -12.5 to -8.58 | ||
| Extension endurance | ||||
| Baseline | 36.25±3.56 | 37.45±4.36 | 0.6 b | 0.28 |
| Post-treatment | 63.9±5.7 | 48.55±4.7 | 0.0001 a | 84.72 |
| P value (within) | 0.0001 a | 0.001 a | ||
| Mean difference | -27.65 | -11.10 | ||
| 95% (CI) | -31.22 to -24 | -14.67 to -7.52 | ||
| Right UT (rest) | ||||
| Baseline | 2.15±0.49 | 2.28±0.39 | 0.37 b | 0.88 |
| Post-treatment | 1.20±0.37 | 1.59 | 0.006 a | 8.49 |
| P value (within) | 0.0001 a | 0.0001 a | ||
| Mean difference | 0.94 | 0.68 | ||
| 95% (CI) | 0.71 to 1.18 | 0.44 to 0.91 | ||
| Left UT (rest) | ||||
| Baseline | 2.31±0.41 | 2.48±0.51 | 0.24 b | 1.38 |
| Post-treatment | 1.02±0.32 | 1.58±0.21 | 0.001 a | 14.15 |
| P value (within) | 0.0001 a | 0.0001 a | ||
| Mean difference | 1.28 | 0.89 | ||
| 95% (CI) | 0.99 to 1.57 | 0.6 to 1.18 | ||
| Right UT (activity) | ||||
| Baseline | 70.05±3.04 | 69.98±4.02 | 0.95 b | 0.004 |
| Post-treatment | 49.95±2.74 | 60.75±5.93 | 0.0001 a | 54.48 |
| P value (within) | 0.0001 a | 0.001 a | ||
| Mean difference | 20.09 | 9.23 | ||
| 95% (CI) | 18.14 to 22 | 7.28 to 11.17 | ||
| Left UT (activity) | ||||
| Baseline | 71.07±3.64 | 72.11±4.19 | 0.41 b | 0.71 |
| Post-treatment | 51.55±5.79 | 61.11±3.71 | 0.0001 a | 38.47 |
| P value (within) | 0.0001 a | 0.001 a | ||
| Mean difference | 19.52 | 11.01 | ||
| 95% (CI) | 16.36 to 22.6 | 7.85 to 14.17 | ||
| Right SCM (rest) | ||||
| Baseline | 3.2±0.45 | 3.07±0.61 | 0.42 b | 0.67 |
| Post-treatment | 1.75±0.24 | 2.09±0.43 | 0.004 a | 9.50 |
| P value (within) | 0.0001 a | 0.001 a | ||
| Mean difference | 1.46 | 0.97 | ||
| 95% (CI) | 1.25 to 1.67 | 0.76 to 1.18 | ||
| Left SCM (rest) | ||||
| Baseline | 3.38±0.51 | 3.42±0.47 | 0.82 b | 0.05 |
| Post-treatment | 1.98±0.37 | 2.16±0.35 | 0.27 b | 1.23 |
| P value (within) | 0.0001 a | 0.0001 a | ||
| Mean difference | 1.40 | 1.25 | ||
| 95% (CI) | 1.15 to 1.64 | 1 to 1.5 | ||
| Right SCM (activity) | ||||
| Baseline | 79.18±3.76 | 76.6±4.92 | 0.07 b | 3.47 |
| Post-treatment | 54.06±3.5 | 64.2±4.88 | 0.0001 a | 56.93 |
| P value (within) | 0.0001 a | 0.001 a | ||
| Mean difference | 25.12 | 12.40 | ||
| 95% (CI) | 22.81 to 27.4 | 10.09 to 14.71 | ||
| Left SCM (activity) | ||||
| Baseline | 80.21±3.41 | 80.5±3.63 | 0.79 b | 0.06 |
| Post-treatment | 57.65±3.75 | 64.1±3.09 | 0.0001 a | 34.79 |
| P value (within) | 0.0001 a | 0.001 a | ||
| Mean difference | 22.56 | 16.4 | ||
| 95% (CI) | 20.27 to 24.8 | 14.1 to 18.68 | ||
aSignificant difference; bno significance difference; x-par: mean; SD: standard deviation; P value: significance level; PPT: pressure pain threshold; ANDI: Arabic Neck Disability Index; CVA: cranio vertebral angle; CI: confidence interval.
Discussion
This study investigated the effect of SSE on CVA, PPT, NFE, NEE, neck function, and muscle activity of both upper trapezius and sternocleidomastoid (muscle amplitude (RMS) at rest and activity) in patients with FHP. As stated by our statistical analysis and findings, the results showed significant improvement in both groups with more supremacy to experimental group (SSEs).
In order to clarify the role of SSE and PCE on FHP, we have to shed a light on the results of FHP on cervical spine alignment and scapula. FHP aggravates spasm in muscles that interfere and inhibit scapular upward rotation. Consequently, there is an evident increase in UT muscle activity in such cases40 even during rest. Besides, we hypothesized that prolonged FHP induced clear cervical length-tension relationship transformation, that result in increased need of cervical neck muscles stabilization; at the time they are not capable of meeting such need, so they are counter balanced by UT and SCM hyperactivity. Further, Weon et al. assured that when the head is in a neutral position induced reduction in the activity of both upper and lower trapezius muscles. For that reason, it could be presumed that excessive activity of the superficial muscles of cervical spine can be prevented by enhancing alignment of head posture.7
Effects of SSEs
SSE is accounted as effective strategies that enhance and improve abnormal FHP.41 As stated by the results, there was significant increase in CVA which proofs an improvement in FHP. A preceding study showed the influence of applying stretching and muscle strengthening exercise programs on refining and improving FHP through CVA increment.42 Besides, Shiravi et al. declared that cervical muscle strength and function is improved through inhibiting upper trapezius muscle activity in FHP subjects using SSE.43 Kang et al. emphasized the influence of SSE in facilitating cervical muscles, dampening the trapezius and serratus anterior muscles, and correction of FHP, which empowers the results of this study.44
When this awkward FHP is corrected, this result in proper alignment of the cervical spinal, inhibiting the superficial muscles spasm and fatigue such as the upper trapezius and sternocleidomastoid, therefore muscle imbalance is alleviated. So, there is a positive influence of pain reduction on PPT and NDI. McDonnel et al. assumed that there is a significant reduction of NDI after the intervention programs being implemented, involving scapular exercise for three months, in order to relocate the abnormally aligned scapula, which is compatible with the study results.45
Our study supposed that there is a significant decrease in the sternocleidomastoid, upper trapezius muscle activity following the intervention. Kang et al. assured on the enhancement of the activities of the lower trapezius, serratus anterior muscles and the role of scapular stabilization on inducing massive improvement of the neck muscles activity.41 Moreover, increasing of scapular tilt and reduction in the upper rotation angle through scapular alignment as a consequence of lower trapezius muscle activation2 In addition, increasing serratus anterior muscle activity result in inhibition of upper trapezius hyperactivity which has a viable role on raising of the scapula and stretching of the neck.
Accordingly, an opposite rotating movement is supposed to occur as a sign of improvement of such abnormal postures.44 Thus, SSEs can be regarded as a method of producing structural changes of the neck and muscles compensation to produce a massive improvement in subjects suffering FHP while solving neck, back and scapular problems.41
Effects of PCEs
The two primary advantages resulting from performing PCEs on regular basis are; firstly, they have a great effect on reducing adverse mechanical loads caused by cervical and scapular awkward kinetics and position. Secondly, they improve deep spinal postural stabilizing muscles strength. Moreover, performing such exercises on regular basis may produce postural habits changes.46 We postulated that assuming proper posture and increasing awareness of its importance play a viable role in alleviating pain and discomfort. Our findings come in agreement those of Mclean, who assured the impact and effectiveness of PCEs on cervical muscles.47 Abd El-wahab and Sabbahi discovered changes in the amplitude of the H-reflex in response to PCEs and as a result it was proposed for cases suffering of cervical radiculopathy (C7).48
The control group improvement may be correlated to PCEs, instructions on daily activities performance within limit of pain, and keeping away from muscle excess load. Factors as task acquaintance or improved postural awareness could be the main cause of their improvement,24 or caused by the deep cervical flexor muscles direct activation49 which have a fairly high density of muscle spindles50 that improve cervical kinesthetic senses.51
Limitations of the study
Despite potential strengths, the present study shows certain limitations. First, young individuals with FHP were recruited, which limits the generalizability of the results to the same population. Second, CVA was measured by taking digital pictures rather than more robust cephalometric radiographic analysis. And third, we haven’t measured the EMG activity of both lower trapezius and serratus anterior muscle despite it has an integral role in scapular kinetic and kinematics.
Conclusions
Adding SSEs would seem to be more effective in improving the craniovertebral angle, pressure pain threshold, muscle activity and disability than postural correction exercises alone. Further studies are needed with large sample and different age groups such as adolescent, young adult and old to increase the generalizability of trial, in addition using objective methods for assessment to increase strength of trial and also assess serratus anterior and lower trapezius due to its integral role in scapular kinetics and kinematics.
References
- 1.Fishman E, Washington S, Haworth N. Bike share: a synthesis of the literature. Transp Rev 2013;33:148–65. 10.1080/01441647.2013.775612 [DOI] [Google Scholar]
- 2.Vakili L, Halabchi F, Mansournia MA, Khami MR, Irandoost S, Alizadeh Z. Prevalence of common postural disorders among academic dental staff. Asian J Sports Med 2016;7:e29631. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27625751&dopt=Abstract 10.5812/asjsm.29631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harman K, Hubley-Kozey CL, Butler H. Effectiveness of an exercise program to improve forward head posture in normal adults: a randomized, controlled 10-week trial. J Manual Manip Ther 2005;13:163–76. 10.1179/106698105790824888 [DOI] [Google Scholar]
- 4.Gonzalez HE, Manns A. Forward head posture: its structural and functional influence on the stomatognathic system, a conceptual study. Cranio 1996;14:71–80. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=9086879&dopt=Abstract 10.1080/08869634.1996.11745952 [DOI] [PubMed] [Google Scholar]
- 5.Mangone M, Paoloni M, Procopio S, Venditto T, Zucchi B, Santilli V, et al. Sagittal spinal alignment in patients with ankylosing spondylitis by rasterstereographic back shape analysis: an observational retrospective study. Eur J Phys Rehabil Med 2020;56:191–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32043853&dopt=Abstract 10.23736/S1973-9087.20.05993-6 [DOI] [PubMed] [Google Scholar]
- 6.Sohn JH, Choi HC, Lee SM, Jun AY. Differences in cervical musculoskeletal impairment between episodic and chronic tension-type headache. Cephalalgia 2010;30:1514–23. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20974583&dopt=Abstract 10.1177/0333102410375724 [DOI] [PubMed] [Google Scholar]
- 7.Weon JH, Oh JS, Cynn HS, Kim YW, Kwon OY, Yi CH. Influence of forward head posture on scapular upward rotators during isometric shoulder flexion. J Bodyw Mov Ther 2010;14:367–74. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20850044&dopt=Abstract 10.1016/j.jbmt.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 8.Dover G, Powers ME. Reliability of joint position sense and force-reproduction measures during internal and external rotation of the shoulder. J Athl Train 2003;38:304–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=14737211&dopt=Abstract [PMC free article] [PubMed] [Google Scholar]
- 9.Edmondston SJ, Sharp M, Symes A, Alhabib N, Allison GT. Changes in mechanical load and extensor muscle activity in the cervico-thoracic spine induced by sitting posture modification. Ergonomics 2011;54:179–86. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21294015&dopt=Abstract 10.1080/00140139.2010.544765 [DOI] [PubMed] [Google Scholar]
- 10.Yoo WG. Effect of the neck retraction taping (NRT) on forward head posture and the upper trapezius muscle during computer work. J Phys Ther Sci 2013;25:581–2. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24259806&dopt=Abstract 10.1589/jpts.25.581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindstrøm R, Schomacher J, Farina D, Rechter L, Falla D. Association between neck muscle coactivation, pain, and strength in women with neck pain. Man Ther 2011;16:80–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20696610&dopt=Abstract 10.1016/j.math.2010.07.006 [DOI] [PubMed] [Google Scholar]
- 12.Xu L, Hwang B, Kim T. The effect of postural correction and visual feedback on muscle activity and head position change during overhead arm lift test in subjects with forward head posture. J Korean Phys Ther 2019;31:151–6. 10.18857/jkpt.2019.31.3.151 [DOI] [Google Scholar]
- 13.Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther 1992;72:425–31. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=1589462&dopt=Abstract 10.1093/ptj/72.6.425 [DOI] [PubMed] [Google Scholar]
- 14.Kim CH, Sim JH. Comparison of the effects of cervical mobilization technique, neuromuscular release, and cervical traction on cervical alignment and muscle activity in people with forward head posture. Kor J Neuromusc Rehabil 2016;6:9–18. [Google Scholar]
- 15.Kim SD, Hong SH, Kim JH. The effects of neck scapula corrective exercise on Sc tatic posture balance and muscle stiffness. J KSSLS 2017;68:601–10. 10.51979/KSSLS.2017.05.68.601 [DOI] [Google Scholar]
- 16.Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br J Sports Med 2010;44:376–81. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20371564&dopt=Abstract 10.1136/bjsm.2009.066837 [DOI] [PubMed] [Google Scholar]
- 17.Singla D, Veqar Z. Association between forward head, rounded shoulders, and increased thoracic kyphosis: a review of the literature. J Chiropr Med 2017;16:220–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29097952&dopt=Abstract 10.1016/j.jcm.2017.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caneiro JP, O’Sullivan P, Burnett A, Barach A, O’Neil D, Tveit O, et al. The influence of different sitting postures on head/neck posture and muscle activity. Man Ther 2010;15:54–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19643658&dopt=Abstract 10.1016/j.math.2009.06.002 [DOI] [PubMed] [Google Scholar]
- 19.Ha SM, Kwon OY, Cynn HS, Lee WH, Park KN, Kim SH, et al. Comparison of electromyographic activity of the lower trapezius and serratus anterior muscle in different arm-lifting scapular posterior tilt exercises. Phys Ther Sport 2012;13:227–32. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23068897&dopt=Abstract 10.1016/j.ptsp.2011.11.002 [DOI] [PubMed] [Google Scholar]
- 20.De Mey K, Danneels L, Cagnie B, Van den Bosch L, Flier J, Cools AM. Kinetic chain influences on upper and lower trapezius muscle activation during eight variations of a scapular retraction exercise in overhead athletes. J Sci Med Sport 2013;16:65–70. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22658589&dopt=Abstract 10.1016/j.jsams.2012.04.008 [DOI] [PubMed] [Google Scholar]
- 21.Kim EK, Kim SG. The effect of an active vibration stimulus according to different shoulder joint angles on functional reach and stability of the shoulder joint. J Phys Ther Sci 2016;28:747–51. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27134352&dopt=Abstract 10.1589/jpts.28.747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yip CH, Chiu TT, Poon AT. The relationship between head posture and severity and disability of patients with neck pain. Man Ther 2008;13:148–54. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17368075&dopt=Abstract 10.1016/j.math.2006.11.002 [DOI] [PubMed] [Google Scholar]
- 23.El-Hamalawy FA. Forward Head Correction Exercises for Management of Myogenic Tempro-mandibular Joint Dysfunction. J Am Sci 2011;7:71–7. [Google Scholar]
- 24.Falla D, Jull G, Russell T, Vicenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther 2007;87:408–17. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17341512&dopt=Abstract 10.2522/ptj.20060009 [DOI] [PubMed] [Google Scholar]
- 25.Quek J, Pua YH, Clark RA, Bryant AL. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther 2013;18:65–71. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22959228&dopt=Abstract 10.1016/j.math.2012.07.005 [DOI] [PubMed] [Google Scholar]
- 26.Graven-Nielsen T, Vaegter HB, Finocchietti S, Handberg G, Arendt-Nielsen L. Assessment of musculoskeletal pain sensitivity and temporal summation by cuff pressure algometry: a reliability study. Pain 2015;156:2193–202. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26172551&dopt=Abstract 10.1097/j.pain.0000000000000294 [DOI] [PubMed] [Google Scholar]
- 27.Fischer AA. Algometry in Diagnosis of Musculoskeletal Pain and Evaluation of Treatment Outcome: an Update. J Musculoskeletal Pain 1998;6:5–32. 10.1300/J094v06n01_02 [DOI] [Google Scholar]
- 28.Harris KD, Heer DM, Roy TC, Santos DM, Whitman JM, Wainner RS. Reliability of a measurement of neck flexor muscle endurance. Phys Ther 2005;85:1349–55. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16305273&dopt=Abstract 10.1093/ptj/85.12.1349 [DOI] [PubMed] [Google Scholar]
- 29.Domenech MA, Sizer PS, Dedrick GS, McGalliard MK, Brismee JM. The deep neck flexor endurance test: normative data scores in healthy adults. PM R 2011;3:105–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21333948&dopt=Abstract 10.1016/j.pmrj.2010.10.023 [DOI] [PubMed] [Google Scholar]
- 30.Lee H, Nicholson LL, Adams RD. Neck muscle endurance, self-report, and range of motion data from subjects with treated and untreated neck pain. J Manipulative Physiol Ther 2005;28:25–32. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15726032&dopt=Abstract 10.1016/j.jmpt.2004.12.005 [DOI] [PubMed] [Google Scholar]
- 31.Shaheen AM, Omar MT, Vernon H. Cross-cultural Adaptation, Reliability, and Validity of the Arabic Version of Neck Disabilit0079 Index in Patients with Neck Pain. Pain 2013;38:609–15. [DOI] [PubMed] [Google Scholar]
- 32.MacDermid JC, Walton DM, Avery S, Blanchard A, Etruw E, McAlpine C, et al. Measurement properties of the neck disability index: a systematic review. J Orthop Sports Phys Ther 2009;39:400–17. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19521015&dopt=Abstract 10.2519/jospt.2009.2930 [DOI] [PubMed] [Google Scholar]
- 33.Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol 2000;10:361–74. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11018445&dopt=Abstract 10.1016/S1050-6411(00)00027-4 [DOI] [PubMed] [Google Scholar]
- 34.Falla D. Unravelling the complexity of muscle impairment in chronic neck pain. Man Ther 2004;9:125–33. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15245706&dopt=Abstract 10.1016/j.math.2004.05.003 [DOI] [PubMed] [Google Scholar]
- 35.Ekstrom RA, Soderberg GL, Donatelli RA. Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. J Electromyogr Kinesiol 2005;15:418–28. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15811612&dopt=Abstract 10.1016/j.jelekin.2004.09.006 [DOI] [PubMed] [Google Scholar]
- 36.Kim EK, Kang JH, Lee HT. The effect of the shoulder stability exercise using resistant vibration stimulus on forward head posture and muscle activity. J Phys Ther Sci 2016;28:3070–3. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27942122&dopt=Abstract 10.1589/jpts.28.3070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khan A, Khan Z, Bhati P, Hussain ME. influence of forward head posture on cervicocephalic kinesthesia and electromyographic activity of neck musculature in asymptomatic individuals. J Chiropr Med 2020;19:230–40. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33536860&dopt=Abstract 10.1016/j.jcm.2020.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Im B, Kim Y, Chung Y, Hwang S. Effects of scapular stabilization exercise on neck posture and muscle activation in individuals with neck pain and forward head posture. J Phys Ther Sci 2016;28:951–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27134391&dopt=Abstract 10.1589/jpts.28.951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moezy A, Sepehrifar S, Solaymani Dodaran M. The effects of scapular stabilization based exercise therapy on pain, posture, flexibility and shoulder mobility in patients with shoulder impingement syndrome: a controlled randomized clinical trial. Med J Islam Repub Iran 2014;28:87. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25664288&dopt=Abstract [PMC free article] [PubMed] [Google Scholar]
- 40.Rahnama L, Abdollahi I, Karimi N, Akhavan N, Arab-Khazaeli Z, Bagherzadeh M. Cervical position sense in forward head posture versus chronic neck pain: a comparative study. Physiother Res Int 2017;2:39–42. [Google Scholar]
- 41.Kang JI, Choi HH, Jeong DK, Choi H, Moon YJ, Park JS. Effect of scapular stabilization exercise on neck alignment and muscle activity in patients with forward head posture. J Phys Ther Sci 2018;30:804–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29950768&dopt=Abstract 10.1589/jpts.30.804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nemmers TM, Miller JW, Hartman MD. Variability of the forward head posture in healthy community-dwelling older women. J Geriatr Phys Ther 2009;32:10–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19856630&dopt=Abstract 10.1519/00139143-200932010-00003 [DOI] [PubMed] [Google Scholar]
- 43.Shiravi S, Letafatkar A, Bertozzi L, Pillastrini P, Khaleghi Tazji M. Efficacy of abdominal control feedback and scapula stabilization exercises in participants with forward head, round shoulder postures and neck movement impairment. Sports Health 2019;11:272–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31013190&dopt=Abstract 10.1177/1941738119835223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Park HK, Han KJ. Effects of upper trapezius pain and head position on scapular upward rotator activities during shoulder abduction on the scapular plane. Kor J Neuromusc Rehabil 2017;7:14–20. [Google Scholar]
- 45.McDonnell GV, Bell KE, Hawkins SA. A pain in the neck. Postgrad Med J 2000;76:57–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10622791&dopt=Abstract 10.1136/pmj.76.891.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morningstar M. Cervical curve restoration and forward head posture reduction for the treatment of mechanical thoracic pain using the pettibon corrective and rehabilitative procedures. J Chiropr Med 2002;1:113–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19674570&dopt=Abstract 10.1016/S0899-3467(07)60013-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McLean L. The effect of postural correction on muscle activation amplitudes recorded from the cervicobrachial region. J Electromyogr Kinesiol 2005;15:527–35. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16150608&dopt=Abstract 10.1016/j.jelekin.2005.06.003 [DOI] [PubMed] [Google Scholar]
- 48.Abdulwahab SS, Sabbahi M. Neck retractions, cervical root decompression, and radicular pain. J Orthop Sports Phys Ther 2000;30:4–9, discussion 10–2. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10705591&dopt=Abstract 10.2519/jospt.2000.30.1.4 [DOI] [PubMed] [Google Scholar]
- 49.Falla D, Bilenkij G, Jull G. Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine 2004;29:1436–40. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15223935&dopt=Abstract 10.1097/01.BRS.0000128759.02487.BF [DOI] [PubMed] [Google Scholar]
- 50.Boyd-Clark LC, Briggs CA, Galea MP. Muscle spindle distribution, morphology, and density in longus colli and multifidus muscles of the cervical spine. Spine 2002;27:694–701. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11923661&dopt=Abstract 10.1097/00007632-200204010-00005 [DOI] [PubMed] [Google Scholar]
- 51.Jull G, Falla D, Treleaven J. Retraining cervical joint position sense: the effect of two exercise regimes. J Orthop Res 2007;25:402–12. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17143898&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 52.Cimbiz A, Beydemir F, Manisaligil U. Evaluation of trigger points in young subjects. J Musculoskeletal Pain 2006;14:27–35. 10.1300/J094v14n04_04 [DOI] [Google Scholar]


