Abstract
Objective:
Mental health issues increased during the COVID - 19 pandemic, especially among children. Our past research efforts found that surveillance data can address a variety of health concerns; that personal psychological awareness impacted ability to cope, and mental health outcomes were improved when survivors were triaged to mental health countermeasures. To build upon our public health efforts, we wanted to see if increased screen time due to remote learning caused by the pandemic influenced school aged children’s mental health.
Methods:
With the hypothesis that excessive time spent isolated during remote learning increased the amount of mental health events in children, we conducted a public health surveillance project on actual diagnoses rather than just symptoms, controlling for historical mental health and emotional disorders.
Results:
The entire cohort of children aged 6 to 17 years were studied over time before and during the pandemic for their medically diagnosed mental health and emotional outcomes by the amount of pandemic induced social isolation.
Conclusions:
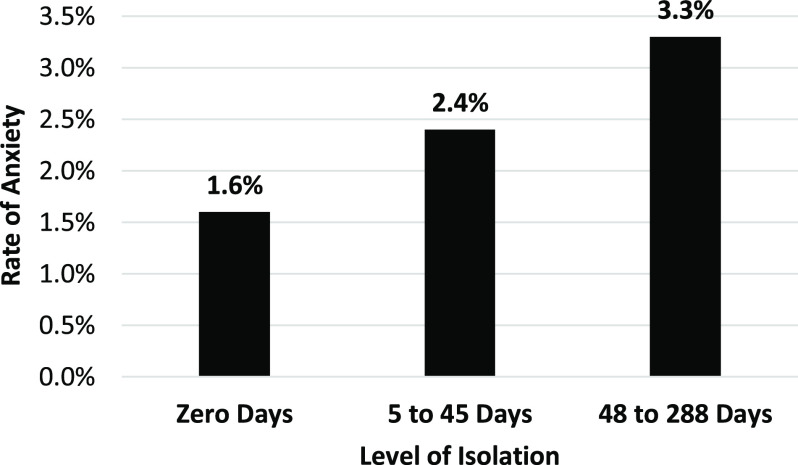
After controlling for historical diagnoses and the rate of COVID - 19, the effect of pandemic - induced social isolation had a linear increase on the amount of anxiety, resulting in a 4-fold increase in pandemic social isolation - induced anxiety.
Keywords: child, adolescent, mental health, pandemic, anxiety, COVID - 19
Introduction
The COVID - 19 pandemic caused fear and anxiety across society. 1 Stress, anxiety, and depressive symptoms were correlated with COVID - 19 prevalence and increased with decreasing age. 2–5 Over 33% of children have reported COVID - 19 related anxiety. 6 The prevalence of obsessive - compulsive disorder (OCD) symptoms increased during the pandemic and OCD increased the likelihood of presenting with elevated stress, anxiety, and depression. 7 The rates of mental health issues increased among children who had an emotion - focused versus a problem - focused coping style. 8 Online learning difficulties and feeling socially disconnected during lockdown were associated with decreased life satisfaction, particularly among girls, and increased depression and anxiety. 9 The psychological impact of the pandemic was worsened by prolonged homestays and increased especially among high school versus primary school students. 10,11 Feelings of social isolation with anxiety being the prevalent symptom among children aged 10 to 17 during the March 2020 pandemic lockdown, followed by depression and stress. 12–14 Disruption of social life and loneliness caused by the pandemic’s necessity to spend a higher number of hours online put children at increased risk of psychiatric disorders. 15,16
In the pre - COVID - 19 pandemic era, persons were more compliant with the recommended protective behavior if they had awareness and could demonstrate knowledge of the public health issue. 18,19 Syndromic surveillance data have been used to address a variety of health concerns. 20 Also, our past research found that persons who were aware of how fear would impact their ability to cope were able to be more compliant regarding recommended protective health behavior. 21 Further, we have found that survivors triaged for mental health countermeasures to mitigate psychological trauma had better long - term outcomes. 22 The Adolescent Behaviors and Experiences Survey (ABES), found poor mental health was less prevalent among those who were socially and virtually connected during the pandemic. 23 The researchers of that finding concluded that improving connections at home, in the community, and at school might improve mental health among youths during and after the pandemic. The authors of the ABES study noted several limitations, including the fact that they did not study diagnosed conditions, that most students were connected, and that the study was not longitudinal. ‘DISCONNECT TO CONNECT’ is a collaborative public awareness and education campaign focused on finding balance in a digital world, to improve the mental health and well - being of our children, youth, and families. This project was in the works before the COVID - 19 pandemic but was re - engaged following the release of the Youth and Mental Health Advisory by the US Surgeon General in December, 2021. 24
During our public health efforts, we wanted to see if increased screen time due to remote learning caused by the pandemic influenced school - aged children’s emotional state or mental health, controlling for the children’s history of past mental health and emotional disorders. With the hypothesis that excessive time spent isolated during remote learning increased the amount of emotional and mental health events in children, we conducted a public health surveillance project to look at actual diagnoses rather than symptoms. The current research herein studied an entire cohort over time before and during the pandemic, including all the cases regardless of their connectedness, and medically diagnosed mental health and emotional disorders.
Methods
Under subpart A of 45 CFR part 46, known as the Common Rule, public health surveillance activities conducted, and supported, as well as requested, ordered, required, or authorized by a public health authority are deemed not to be research. Therefore, no Institutional Review Board review was sought. The data used in this study were from 2 sources: (1) EpiCenter version 3.5.23 (Health Monitoring Systems Inc., Pittsburgh, Pennsylvania, USA). The EpiCenter system analyzes healthcare data to detect increases of health events that may be important to public health, including disease outbreaks. When anomalies are detected, EpiCenter provides automatic notification to appropriate health department personnel, and (2) The Ohio Disease Reporting System (ODRS). ODRS is the Ohio Department of Health’s data system that contributes to the National Notifiable Diseases Surveillance System (NNDSS). These data were provided by the Ohio Department of Health. The Department specifically disclaims responsibility for any analyses, interpretations, or conclusions. The NNDSS is a program of the Centers for Disease Control and Prevention’s Division of Health Informatics and Surveillance, US Department of Health and Human Services. The data was analyzed using SPSS version 28 (IBM Corp., Armonk, New York, USA). The method for presenting the data herein assured protection of any persons’ identity by exceeding compliance with the Ohio Department of Health’s Disclosure Limitation Standard and the Public Health Service Act (42 US C. 242m(d)).
For this report, the word ‘children’ will include ages 6 to 17 years. The study cohort of children, residents of Greene County, Ohio, that visited a provider or hospital, were followed for 2 years before and during the pandemic years of 2021 and 2022. The study area was a mix of urban and rural areas. All acute care visits for the cohort were reviewed for individual diagnoses within the mental health and emotional diagnostic conditions at 4 - time spans. All acute care visits were examined for the complete month of January, with historical visits taken into account, for all child residents for each year from 2019 through 2022. These included mental disorders (as shown in Table 1) due to known physiological conditions (F01 - F09); mental and behavioral disorders due to psychoactive substance use (F10 - F19); schizophrenia, schizotypal, delusional, and other non - mood psychotic disorders (F20 - F29); mood [affective] disorders (F30 - F39); anxiety, dissociative, stress - related, somatoform and other nonpsychotic mental disorders (F40 - F48); behavioral syndromes associated with physiological disturbances and physical factors (F50 - F59); disorders of adult personality and behavior (F60 - F69), intellectual disabilities (F70 - F79); pervasive and specific developmental disorders (F80 - F89); behavioral and emotional disorders with onset usually occurring in childhood and adolescence (F90 - F98); and any emotional disorders (R45). A selection of diagnostic codes was grouped together that included ICD 10 codes for F01 - F09, F20 - F29, F40 - F49, and F50 - F59, as well as F80 - F89 and R45. These were grouped because they were thought to be most likely to be affected by exogenous factors. The rationale for this grouping was to increase the power to find a difference by excluding those conditions that ‘a priori’ were thought to be invariable to the exposure. Table 1 displays the conditions that met the assumption and thus were included versus excluded in the analysis. Disorders of adult personality and behavior (F60 - F69) were excluded since they were not appropriate for this study population. Care and education centers for intellectual disabilities, including those with at - home education and other service providers, did not necessarily follow the remote learning schedule that boards of education instituted. Hence, those persons with intellectual disabilities would not be expected to have the same variability of mental health acute care visits from being isolated as the rest of the population of school - aged children. The diagnostic group was tested for the assumption but the combined categories of F02458 did not include that grouping. Including the grouping of any emotional (R45) or mental health code (using the first ICD 10 code to designate groups F02458) did not preclude each diagnostic code from being processed separately to see if that diagnostic code met the assumptions for the analysis to continue.
Table 1.
Modeling of dependent variable homogeneity of covariate coefficients assumption (if significant, analysis of covariance (ANCOVA) was not conducted on the dependent variable)
| Dependent Variable | Interaction Term Significance | Between Subjects Factor Isolation Levels | Assumption Met |
|---|---|---|---|
| Mental Health or Emotional State Diagnoses | < 0.001 | 3 | No |
| Emotional (R45) or Any MH Dx (F02458) Max | 0.601 | 3 | Yes |
| Mental disorders due to known physiological conditions (F01 - F09) | 0.996 | 3 | Yes |
| Mental and behavioral disorders due to psychoactive substance use (F10 - F19) | 0.998 | 3 | Yes |
| Schizophrenia, schizotypal, delusional, and other non - mood psychotic disorders (F20 - F29) | 0.984 | 3 | Yes |
| Mood [affective] disorders (F30 - F39) | 0.673 | 2 | Yes |
| Anxiety, dissociative, stress - related, somatoform and other nonpsychotic mental disorders (F40 - F48) | 0.177 | 3 | Yes |
| Behavioral syndromes associated with physiological disturbances and physical factors (F50 - F59) | < 0.001 | 3 | No |
| Disorders of adult personality and behavior (F60 - F69) | < 0.001 | 3 | No |
| Intellectual disabilities (F70 - F79) | NA | 3 | No |
| Pervasive and specific developmental disorders (F80 - F89) | 0.998 | 3 | Yes |
| Behavioral and emotional disorders with onset usually occurring in childhood and adolescence (F90 - F98) | < 0.001 | 3 | No |
| Signs and Symptoms of Emotional State (R45) | 0.791 | 3 | Yes |
The method of analysis of covariance was chosen to control for the child’s past mental health and emotional state. The statistical assumption of analysis of covariance is that there is no significant interaction between the covariate and the exposure. The pre - pandemic mental and emotional acute care visits should not have an interaction with the future amount of isolation the children were exposed to. This ‘homogeneity of covariate coefficients’ assumption that the prior diagnoses for emotional or mental health conditions were not associated with the isolation exposure was checked by fitting an interaction term between prior diagnoses and future exposure to isolation. Each of the thirteen dependent variables was examined and if the interaction was significant that analysis was not performed. If the significance value was greater than 0.05 and the proportion of variance explained by the interaction was close to zero, then homogeneity of the coefficients for the covariate can be assumed across the levels of the isolation factor.
The days of remote learning, isolated from in - person school was used as a surrogate for screen time. The exposure level was days isolated in the twelve months prior to the month diagnosed. Exposure groups were assigned by place of residence and the likely education district the child would have attended. An exposure matrix for the predictor factor coded ‘zero isolation days per year’ as zero, ‘greater than zero but less than 48 days’ was coded as one, and ‘greater than or equal to 48 days isolated’ was coded as two. The levels for mood affective disorders (F30 - F39) were collapsed to two levels to meet the assumption of no interaction with the covariate. The results of the interaction term for the covariate and the dependent variables selected for analysis are shown in Table 1. The selection of the dependent variables produced an analysis of covariance (ANCOVA) to assess the effect of isolation due to the pandemic, controlling for past diagnoses, on children’s emotional and mental health diagnoses. The descriptive statistics show the rate of emotional - mental health diagnoses during acute care visits during the pandemic.
The incidence of COVID - 19 would also account for the quarantine isolation the children were subjected to. The admitting diagnosis of COVID - 19 was very low in this age group, but the amount of quarantine was high, so the COVID - 19 rate per 1000 children per residential area was explored if the initial ANCOVA analysis was significant. The homogeneity of variances was evaluated using Levene’s test. If the significance value for the isolation level was less than 0.05, indicating it has a significant effect on the dependent variable of mental health or emotional disorder diagnosis, the parameter estimates were examined to determine the size of that effect.
By specifying an interaction between the covariate and factor, the homogeneity of the covariate parameter estimates across levels of isolation were tested for. If the interaction term was not significant, indicating the covariate parameter estimates were considered homogenous, the analysis of covariance was conducted to determine if isolation affected mental health and/ or emotional disorders.
If the interaction term was significant, the model could be used with the interaction term, with the understanding that assessing the effect of being isolated is complicated by the presence of having a history of mental health disorders. That is, when this interaction term is significant, the difference between isolation levels changes for persons with and without past mental health diagnoses.
Results
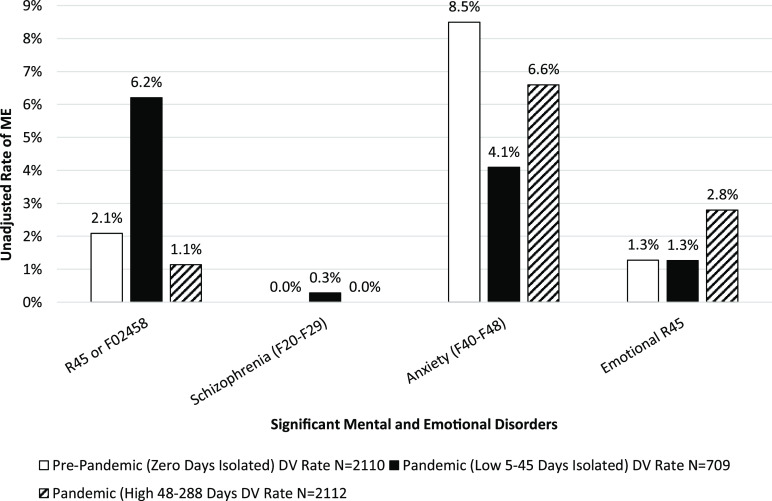
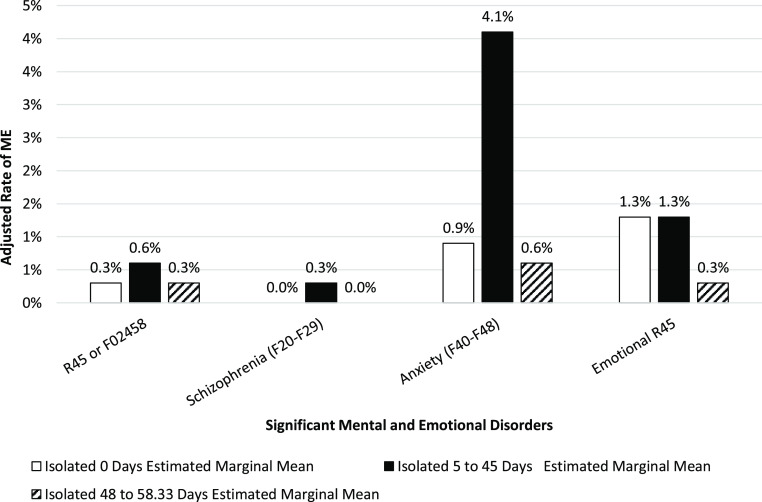
The rates for acute care for anxiety was significantly increased among children after exposure to 5 - 45 days of isolation versus no exposure (4.1% to 0.9%), greater than a 4.5 - fold increase in anxiety diagnoses (Figures 1 and 2).
Figure 1.
Children aged 6 to 17 years residing in Greene County, Ohio, 2018 through January 2022, unadjusted rate of ‘mental and emotional disorders’ (ME) diagnosed during acute care visits 2 years before and during the pandemic (F02458 indicates grouping of mental health disorders by the first digit of the ICD - 10 codes) by stage of pandemic induced social isolation.
Figure 2.
Children aged 6 to 17 years residing in Greene County, Ohio, 2018 through January 2022, adjusted rates of mental and emotional disorders (ME) diagnosed during acute care visits 2 years before and during the pandemic (F02458 indicates grouping of mental health disorders by the first digit of the ICD - 10 codes) by stage of pandemic induced social isolation.
The risk of any child being diagnosed with F0, F2, F4, F5, or F8 mental health disorders after any isolation from the pandemic was 1.571 (95% CI 1.4 - 1.76), Table 2. While the prevalence in the population was low (1.43%), the etiological fraction in the exposed was over 36%, as calculated from the information in contingency Table 2.
Table 2.
Counts of mental health disorders diagnosed by exposure to pandemic induced social isolation among Greene County Children aged 6 to 17 for 2 years before and during the COVID - 19 Pandemic, Risk Ratio 1.571 (95% CI 1.4 - 1.76)
| Isolation Level | Diagnosed with F0, F2, F4, F5 or F8 Mental Health Disorders | No Diagnoses |
|---|---|---|
| Any Isolation | 106 | 56 |
| No Isolation | 2590 | 3630 |
Based on the low rate of admitting diagnosis from COVID - 19 and a high amount of quarantine in this age group, the methodology called for the COVID - 19 rate per 1000 children per residential area to be explored if the initial ANCOVA analysis was significant. Since anxiety, dissociative, stress - related, and somatoform/ other nonpsychotic mental disorders (F40 - F48) were found to be elevated, the random variable for the rate of COVID - 19 per sub - population area was added to the model. By controlling for past diagnoses and assuring there was no interaction between the pre - pandemic mental and emotional acute care visits with future amounts of isolation the analysis provided a more accurate result. This pre - planned post hoc analysis found anxiety to be sequentially greater with increasing isolation when the case rate of COVID - 19 and mental health diagnoses was controlled for (Figure 3).
Figure 3.
Rate of anxiety by amount of pandemic induced social isolation while controlling for historical anxiety diagnoses and the local rate of COVID-19.
Limitations
The providers of the diagnoses for the cohort were not limited to the residential geographic area, but included providers in the state that were part of the public health syndromic surveillance system. If the provider or hospital system used a different patient identification system, the patient would not have been matched to prior visits. The past diagnoses were reviewed not for just 1 year but 2 years prior to the pandemic. This strength of the study design did not prevent a subacute diagnosis being present. The reason for our research into the relationship between pandemic induced social isolation and mental health diagnoses was to promote public health. The Disconnect - to - Connect program planning that focused on reducing the harmful effects of increased screen time began before the pandemic. At a population – level, the ‘known - pandemic - caused - remote - learning’ among children ages 6 to 17 preceded an increase of mental illness when compared to those children without remote learning. This finding assumes that the known pandemic caused remote learning is commensurate with increased exposure to screen time and decreased in - person socialization (Note that the finding was at the population level and controlled for past acute care mental health visits). This finding, that there is a difference between cohorts of pandemic induced socially isolated children (when if, in reality, there was no difference) could be a Type I error. We believe a Type I error was minimized by our design because those most amenable to finding a difference when 1 existed would be those already in therapy, or already isolated due to other chronic conditions, and that the whole population was included in the analysis, providing enough power to find truthful results.
Discussion
Pandemic social isolation significantly impacted the level of anxiety in this population. Using days of remote learning as a surrogate for screen time increases the error term because it does not capture all the screen time at the individual level. Remote learning supplies a definitive amount of screen time because of the intrinsic nature of virtual learning. The risk of only using this measure is that it may lessen the chance of finding a significant effect when 1 exists, a type II error. In this situation, if a significant finding is found, then we can be assured that there is even more of an effect from being isolated for an extended period. The assignment of exposures was by the education district the child likely would have attended. Though some schools allow students outside of their district to enroll, most students go to the school where they live. Even those who did not, such as those in private schools, would still have similar exposures based on their residential address. Many private schools follow the practice of the local boards of health when it comes to policy. In a recent article, experts stress the need for ‘healthy technology behaviors to be mindful of the physical, mental, and social effects of too much screen time. 25 The longer - term mental health effects of pandemic induced social isolation should be studied. The study design controls for evaluating children based on their exposure to social isolation due to remote learning. Social isolation from other causes should otherwise be randomly dispersed among the strata of remote learning. The American Academy of Pediatric states that, ‘worsening crisis in child and adolescent mental health is inextricably tied to stress brought on by COVID 19.’ 26 The Academy also mentions the stress of structural racism as an urgent area of concern regarding children’s mental health; however our study did not address this or other causes of childhood mental health, rather the study design was to find the etiological fraction in the population caused by pandemic social isolation due to remote learning. Note that the distribution of race and ethnicity is comparable in the study area to the United States. However, it is not directly comparable to areas with higher rates of poverty and minority status. Those areas would be expected to have greater social vulnerability to the isolation caused by the pandemic. The results of this study should be considered on the lower spectrum of harmful effects from the pandemic. Since a term was added to the model for children with and without prior mental health conditions, the statistical method allowed for singling out the effect of pandemic isolation to precede an acute healthcare visit where a mental health diagnosis was made. The severity of mental health illness was partially also controlled for not only by looking at individual mental health diagnoses, but also by the number of mental health acute care visits. This certainly reduced the error term for hiding any main effect (a reduction in Type II error). In plain language this would allow for determination of the social isolation effect from the pandemic on mental health regardless of those at more risk for developing worsening mental health issues as well as those without prior mental health concerns.
Future direction
The ‘DISCONNECT TO CONNECT’ project is a movement Greene County community partners implemented to raise awareness about the mental health crisis facing our children and youth. This awareness campaign was not designed to attach any causal relationship between technology use and mental well - being. Instead, it is an effort to raise awareness about how children, youths, and families make use of technology and how to find the balance between productive use and avoiding or minimizing any harmful aspects. There are environmental factors outside of our control (positive and negative life experiences), personality and coping styles, and biological factors (genes and brain chemistry) that impact the mental health and well - being of our children and youth. However, there are external factors that collectively, persons have the power to adjust, such as the quantity and quality of personal digital use. While computers, smartphones, and tablets play an important role in education, and enhance our lives in many ways, excessive or inappropriate use is a cause for concern.
Greene County Public Health officials, along with the Mental Health Recovery Board of Clark, Greene, and Madison Counties, the Greene County Public Library, Greene County Children Services, Greene County Family and Children First Council, and the Greene County Educational Service Center are working collaboratively to raise community awareness of the problem along with providing resources and practical information to help children, youth, educators, parents, families, and community organizations make impactful changes toward improving mental health and wellbeing of children and youth in Greene County.
A 6 - part series of articles that share information, and focuses on practical tips, techniques, and strategies to address the issue were published in a local media outlet that serves multiple communities in the area. Each month, an article targeted different age groups from infants to young adults. The final article focused on parents, teachers, and the community at large. A logo was developed by students at the Greene County Career Center to brand the project. In addition to press releases and printed newspaper articles, printed materials were developed for dissemination, book lists for different age groups were developed to be featured at the county libraries, social media posts with stats and tips were shared, and a poster activity was conducted in the schools for the middle and elementary grades. The collaborative group participated in a sidewalk chalk event during Children’s Mental Health Awareness Week at a community park in May, 2022. The initiative intends to continue with public awareness activities through the next school term. Participation in National Unplug Day is planned countywide and to have an even larger awareness activity through the schools during Mental Health Awareness Month in 2023.
Conclusion
Disease morbidity and mortality associated with COVID - 19 along with pandemic isolation (which is 1 of the major causes of increased screen time) is a plausible hypothesis for increases in diagnoses of mood disorders. Extended grief was recently added to the diagnostic manual. This study did include emotional disorders including dysthymia, but not this new diagnostic code of extended grief. Children have lost parents, grandparents, and siblings to the pandemic. We have found in our past research, during a disaster, survivors with chronic care needs who are offered support, are better able to receive services. 27 In our interconnected world, infectious diseases can spread quickly. 28 Assuring that the effects on the body and the mind are addressed will be increasingly important. After controlling for historical diagnoses and the rate of COVID -19 in the community, the effect of pandemic - induced social isolation had a linear increase in the amount of anxiety, resulting in a 4-fold increase in pandemic social isolation - induced anxiety.
Author contributions
Donald Brannen – Author of first draft and biostatistician; Sheryl Wynn – Original conceptual idea and coordination with local mental health agencies; Jaime Shuster – Update coordination, editing and compliance with local and federal good clinical practices; Melissa Howell – Team authority and project oversight.
Funding statement
Direct financial support was provided by the author’s hosting organizations.
Conflicts of interest
The authors have no financial or ethical conflicts of interest.
Abbreviations
ABES, Adolescent Behaviors and Experiences Survey; ANCOVA, Analysis of Covariance; NNDSS, National Notifiable Diseases Surveillance System; OCD, Obsessive Compulsive Disorder; ODRS, Ohio Disease Reporting System
References
- 1. Franic T, Dodig-Curkovic K. Covid-19, child and adolescent mental health - Croatian (in) experience. Ir J Psychol Med. 2020;7(3):214-217. doi: 10.1017/ipm.2020.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychol Trauma. 2020;12(S1):S17-S21. doi: 10.1037/tra0000924 [DOI] [PubMed] [Google Scholar]
- 3. Czeisler ME, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR. 2020;69(32):1049-1057. doi: 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brown SM, Doom JR, Lechuga-Peña S, Watamura, SE , Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse Negl. 2020;110(Pt 2):104699. doi: 10.1016/j.chiabu.2020.104699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nwachukwu I, Nkire N, Shalaby R, et al. COVID-19 pandemic: age-related differences in measures of stress, anxiety and depression in Canada. Int J Environ Res Public Health. 2020;17(17):6366. doi: 10.3390/ijerph17176366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Abawi O, Welling MS, van den Eynde E, et al. COVID-19 related anxiety in children and adolescents with severe obesity: a mixed-methods study. Clin Obes. 2020;10(6):e12412. doi: 10.1111/cob.12412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abba-Aji A, Li D, Hrabok M, et al. COVID-19 pandemic and mental health: prevalence and correlates of new-onset obsessive-compulsive symptoms in a Canadian province. Int J Environ Res Public Health. 2020;17(19):6986. doi: 10.3390/ijerph17196986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J Affect Disord. 2020;275:112-118. doi: 10.1016/j.jad.2020.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Magson NR, Freeman JYA, Rapee RM, Richardson CE, Oar EL, Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50(1):44-57. doi: 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tee ML, Tee CA, Anlacan JP, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379-391. doi: 10.1016/j.jad.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Qin Z, Shi L, Xue Y, et al. Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the COVID-19 pandemic in China. JAMA Netw Open. 2021;4(1):e2035487. doi: 10.1001/jamanetworkopen.2020.35487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tang S, Xiang M, Cheung T, Xiang YT. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J Affect Disord. 2021;279:353-360. doi: 10.1016/j.jad.2020.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. O’Sullivan K, Clark S, McGrane A, et al. A qualitative study of child and adolescent mental health during the COVID-19 pandemic in Ireland. Int J Environ Res Public Health. 2021;18(3):1062. doi: 10.3390/ijerph18031062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu Y, Yue S, Hu X, et al. Associations between feelings/ behaviors during COVID-19 pandemic lockdown and depression/anxiety after lockdown in a sample of Chinese children and adolescents. J Affect Disord. 2021;284:98-103. doi: 10.1016/j.jad.2021.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Murata S, Rezeppa T, Thoma B, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021;38(2):233-246. doi: 10.1002/da.23120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mohler-Kuo M, Dzemaili S, Foster S, Werlen L, Walitza S. Stress and mental health among children/adolescents, their parents, and young adults during the first COVID-19 lockdown in Switzerland. Int J Environ Res Public Health. 2021;18(9):4668. doi: 10.3390/ijerph18094668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Luijten MAJ, van Muilekom MM, Teela L, et al. The impact of lockdown during the COVID-19 pandemic on mental and social health of children and adolescents. Qual Life Res. 2021;30(10):2795-2804. doi: 10.1007/s11136-021-02861-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brannen DE, Stanley SA. Critical issues in bioterrorism preparedness: before and after September 2001. J Public Health Manag Pract. 2004;10(4):290-8. doi: 10.1097/00124784-200407000-00005 [DOI] [PubMed] [Google Scholar]
- 19. Ludtke JR, Narayan R, Matariyeh A, et al. Willingness to respond for radiologic incidents: a hands-on approach. Am J Disaster Med. 2014;9(4):259-72. doi: 10.5055/ajdm.2014.0178 [DOI] [PubMed] [Google Scholar]
- 20. Brannen DE, Howell M, Steveley A, Webb J, Owsley D. Syndromic surveillance data for accidental fall injury. Online J Public Health Inform. 2021;13(3):e18. doi: 10.5210/ojphi.v13i3.10264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brannen DE, Caudill K, Cottingim S, et al. Medication adherence and fear among the public health system responders to a bioterrorism pandemic. Poster presented at Public Health Preparedness Summit; April 17-20, 2018; Atlanta, GA. doi:10.13140/RG.2.2.13096.06407
- 22. Brannen DE, Barcus R, McDonnell MA, Price A, Alsept C, Caudill K. Mental health triage tools for medically cleared disaster survivors: an evaluation by MRC volunteers and public health workers. Disaster Med Public Health Prep. 2013;7(1):20-8. doi: 10.1001/dmp.2012.49. PMID: [DOI] [PubMed] [Google Scholar]
- 23. Jones SE, Ethier KA, Hertz M, et al. Mental health, suicidality, and connectedness among high school students during the COVID-19 pandemic — Adolescent Behaviors and Experiences Survey, United States, January – June 2021. MMWR Suppl. 2022;71(Suppl-3):16-21. doi: 10.15585/mmwr.su7103a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Murthy VH. Protecting youth mental health. Published 2021. https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf
- 25. Sparks SD. Students are behaving badly in class. Excessive screen time might be to blame. Student Well-Being, Education Week Research Center, Education Week, April 12, 2022. Accessed May 11, 2022. https://www.edweek.org/leadership/students-are-behaving-badly-in-class-excessive-screen-time-might-be-to-blame/2022/04. Accessed May 12, 2022
- 26. American Academy of Pediatrics. Declaration of a National Emergency in Child and Adolescent Mental Health. Published October 19, 2021. https://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health
- 27. Fannin A, Brannen DE, Howell M, Martin S. Using functional needs and personal care assistance rather than disability status during chronic care triage in community mass care. Disaster Med Public Health Prep. 2015;9(3):265-74. doi: 10.1017/dmp.2015.21 [DOI] [PubMed] [Google Scholar]
- 28. Brannen DE, Alhammad A, Branum M, Schmitt A. International air travel to Ohio, USA, and the impact on malaria, influenza, and hepatitis A. Scientifica. 2016;2016:8258946. doi: 10.1155/2016/8258946 [DOI] [PMC free article] [PubMed] [Google Scholar]