Abstract
Background
Early identification of childhood malnutrition is imperative to improve overall health outcomes, and more importantly, to start early intervention to decrease the risk of future complications. This study aimed to evaluate new malnutrition Z-score growth indicators for detecting pediatric malnutrition and degrees of severity and compare their accuracy with that of growth chart centiles.
Patients and Methods
This retrospective study included 475 pediatric patients from several pediatric nutrition clinics for six months. The participant's weight, height, age, and growth parameters were recorded using both traditional growth charts (centiles) and updated malnutrition indicators (z-scores). The percentage and degree of malnutrition using centiles and Z-scores were compared.
Results
In children aged <2 years, the percentage of malnutrition was 4.7% higher when measured using new malnutrition indicators (weight-for-length Z-score) compared with (weight-for-length centiles). Our results also showed 9.6% higher number of malnourished children >2 years of age when BMI-for-age Z-score was used compared to weight-for-height centiles while there were 15.8% higher malnourished children when BMI-for-age Z-score was compared to BMI-for-age centiles for the same group. We found a significant difference (X2 = 202.548, P=<.0001) between the degree of malnutrition in children aged >2 years using BMI-for-age Z-score (normal vs. malnourished) and the degree of malnutrition using BMI centiles (normal vs. malnourished). Approximately 34% of the children classified as normal using centiles were classified as malnourished using Z-scores. Comparing the degrees of Malnutrition, approximately 23% (45 of 196) of children classified as normal based on centiles were classified as having mild malnutrition when Z-scores were used, and 42% (80 of 192) of children who were classified as having mild malnutrition based on centiles were classified as having moderate malnutrition when Z-scores were used.
Conclusions
In our study, a higher percentage of children showed malnutrition when assessed using the Z-score (BMI-for-age for children >2 years/weight-for-length for children <2 years of age) than the centiles growth chart.
Keywords: Pediatric malnutrition, Undernutrition, Nutritional assessment, Malnutrition, Z-score, Growth charts, Centiles
List of abbreviations
- BMI
Body Mass Index
- WHO
World Health Organization
- CDC
Centers for Disease Control and Prevention
- NCHS
National Center for Health Statistics
- UNICEF
United Nations Children's Fund
1. Introduction
Early identification of childhood malnutrition is crucial to improve overall health outcomes, decrease future financial costs [1], facilitate earlier intervention, and decrease the future risk of associated complications [2]. Approximately 45% of the mortality among children aged <5 years is due to malnutrition [3]. The Global Nutrition Report 2018 indicated that 15.95 million children aged <5 years have stunted or wasted growth [4]. Moreover, malnutrition can persist in adolescence, putting individuals at a higher risk for diseases and premature death [5]. The prevelance of Malnutrition in the form of thinness, BMI (Body-Mass-Index) <2 Z-score in school-aged children was reported to be 35% in Africa and Southeast Asia and less than 15% in Latin America, Eastern Mediterranean and Western Pacific [6].
The prevelance of malnutrition in Saudi Arabia has been reported as follows: for children less than 5 years of age, moderate and severe malnutrition (underweight) was 6.9% and 1.3% respectively, moderate and severe malnutrition(wasting) was 9.8% and 2.9%, moderate and severe malnutrition (stunting) was 10.9% and 2.8% [7]. In another study that assessed malnutrition in school-aged children in Saudi Arabia, the prevelance of underweight was 14.2%, stunting was 12.2% and wasting was 13.8% [8].
Pediatric malnutrition has many devastating implications, including increased hospital stay, decreased quality of life [9], and increased hospital costs [10] and also closely linked with brain development and function [11] and alterations in functional outcomes [12]. Children with malnutrition are at an increased risk of developing diarrhea and pneumonia [13]. The consequences of childhood stunting include decreased cognitive development, increased associated comorbidities, and decreased school performance [14].
Nutritional status is assessed via plotting anthropometric measurements on centile charts and allows to compare the growth of a child to a reference population [15,16] A percentile represents the value which a given percentage of the data falls under or above. Therefore, it facilitates interpretation of a child's growth patterns in comparison to other peers of his or her similar age group. Consequently, plotted values over time can help in detecting when growth does not follow a normal pattern [17,18]. The limitation however lies in the centiles themselves due to their bell-shaped curve, they can only compare a value to the norm, they cannot detect how far away from the norm these values are [16,18].
In order to determine the actual deviation from the fiftieth centile or population norm, Z-score charts should be used [18]. Z-score describe the number of standard deviations away from the mean or median where the value is [15]. Z-score charts will always give a numerical value, positive, or negative [15]. Positive Z-score value reflects how many standard deviations above the mean the value is, while negative values reflects how many standard deviations below from the mean the value is [19]. Children with normal growth would fall between -1 and +1 Z-score [18].
Crossing Z-score lines alerts a clinicain as well for a possible nutritional risk [18]. In addition, to being able to identify extreme values, this is another reason why Z-score growth standards are superior to centile charts, as they facilitates monitoring trends over time and assess longitudinal changes [15]. This means that growth patterns can be followed and improvement can be detected, even in those children whose growth is way below the third centile [15]. Morever, unlike centile charts, Z-score charts provide a numerical value, either positive or negative [12]. For example, a percentile chart would define a child's growth as below the 3rd centile, whereas a Z-score chart would describe it with a Z-score of -2.7[15,16]
In addition, to identify extreme values below the third percentile or above the 97th percentile, Z-score growth standards are superior to centile charts, as they facilitate the monitoring of trends over time and the assessment of longitudinal changes [15]. As growth patterns can be monitored, improvements can be detected, even in children whose growth is below the third centile [16].
A new consensus statement defining the standardized indicators to identify stages of pediatric malnutrition was released in 2014 by the Academy of Nutrition and Dietetics and the American Society of Parenteral and Enteral Nutrition [18]. The consensus recommends using World Health Organization (WHO) growth charts for children aged <2 years and those of the Centers for Disease Control and Prevention (CDC) for children aged >2 years. The primary indicators are as follows: weight-for-length in children aged <2 years, BMI-for-age in children aged >2 years, length/height-for-age, and mid-arm circumference. The latter two indicators (length/height-for-age, and mid-arm circumference) are applicable for both age groups. Any of these indicators is sufficient to diagnose pediatric malnutrition. At least two of the following four indicators are required to diagnose malnutrition: weight gain velocity (for children aged <2 years), weight loss (for those aged >2 years), deceleration in weight-for-length/BMI-for-age Z-score, and inadequate nutrient intake [18].
Numerous studies have assessed the growth of the pediatric population; however, no unified or standard criteria have been used to describe pediatric malnutrition. Malnutrition is described as mild, moderate, or severe, as well as, acute or chronic, based on some or a combination of the following parameters: BMI, weight for age, height for age, weight for height, percentile of ideal body weight centiles, or Z-score. Moreover, this would vary depending on the growth chart that has been used for the assessment. There is limited data regarding which indicator is more accurate and if there are potential differences in the percentage of malnutrition if different indicators were used [1,20,21].
The objective of the present study is to assess whether Z-score growth indicators will detect a higher percentage of pediatric malnutrition and also to assess the degree of malnutrition in comparison with growth chart centiles in the same population. We hypothesized that the distribution of degrees of malnutrition using the Z-score is not equal to the degree of malnutrition using the centile chart.
2. Material and methods
2.1. Ethical approval and patient consent
The study protocol was reviewed and approved by the research ethics committee. Waiver for informed patient consent was requested and approved since the nutrition assessment did not differ from routine clinical practice. Pertinent information regarding nutritional status was discussed with the patient/caregiver as per usual practice. The confidentiality of patients was maintained throughout the study. Data was stored in excel sheets; only one copy included medical record numbers, which were encrypted and saved privately with the primary investigator. All other versions of the excel sheets (working files) were without the medical record numbers to maintain confidentiality. The study was approved by Research Advisory Council (RAC), King Faisal Specialist Hospital and Research Centre - Riyadh with IRB Number 2201195.
2.2. Study design and participants
This retrospective study reviewed patient medical charts. Data collection was initiated following the implementation of the new malnutrition indicators at our institute, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia. Growth was assessed using traditional growth parameters, i.e., centile values, and also the updated malnutrition indicators, i.e., Z-score values and academy definitions [18]. Patients were selected from multiple pediatric nutrition clinics. Four dietitians working in the respective clinics collected data for six months. The dietitians were not blinded as data was collected during the routine clinic visit and was outside the context of the study. All patients who attended the clinics during the study period were initially included, a total of 516, however further analysis excluded some patients. The inclusion and exclusion criteria of the study participants are presented in Fig. 1.
Fig. 1.
Inclusion and exclusion criteria of the study participants.
2.3. Data collection
The following data were obtained from patient charts and dietitian notes: weight-for-height/length percentile (plotted on a sex-specific National Center for Health Statistics (NCHS) growth chart) [22], ideal body weight, weight-for-height/length percent median [(actual weight/ideal weight) x 100%], and degree of malnutrition (interpreted according to reference standards) as described in 2.4.
Additional data included BMI-for-age percentile for children aged >2 years, which had been plotted on sex-specific data tables, using “Data Table of BMI-for-age Charts” from the CDC's NCHS.
Finally, upon implementing the new practice endorsed by the Academy of Nutrition and Dietetics and the American Society of Parenteral and Enteral Nutrition [18], growth parameters were assessed using the updated pediatric malnutrition indicators. One single data point (Z-score) value was obtained for each patient: for children aged <2 years, the weight-for-length Z-score was plotted using WHO growth parameters for children aged >2 years, BMI-for-age Z-score value was plotted using CDC growth parameters, and plotting was conducted on www.Peditools.org. The Z-score value was recorded, and the degree of malnutrition was interpreted according to reference standards (more details in the 2.4 section). Data were collected and tabulated as shown in Table 1 and Table 2.
Table 1.
Data collected and documented of children <2 years of age.
| For children below two years of age: | |||||
|---|---|---|---|---|---|
| Sex | Weight-for-length centile | Weight-for-length percent median | Interpretation of percentiles weight-for-length | Weight-for-length Z-score value | Interpretation weight-for-length Z-score |
| Female | Less than, on or above 3rd, 5th, 10th, 20th, 30th, 40th, 50th, 60th, 70th, 80th, 90th, 95th, 97thcentile. | Divide actual weight by ideal weight, then multiply by 100. Number expressed as a percentage. | Normal, Mild, Moderate, Severe | Expressed as an exact number. Negative or positive | Normal Mild malnutrition |
| Male | Moderate malnutrition, Severe malnutrition, Possible risk of overweight, Overweight, Obese | ||||
Table 2.
Data collected and documented of children >2 years of age.
| For children above two years of age | ||||||||
|---|---|---|---|---|---|---|---|---|
| Gender | Weight- for-height centile | Weight-for-height percent median | Interpretation of percentiles weight-for-height | BMI-for-age value | BMI-for-age centile | BMI-for-age centile interpretation | BMI-for-age Z-score value | Interpretation of BMI-for-age Z-score (>2) |
| Female, Male | Centile 20th, 30th, 40th, 50th, 60th, 70th, 80th, 90th, 95th, 97th | Divide actual weight by ideal weight, then multiply by 100. Number expressed as a percentage. | Normal, Mild, Moderate, Severe | Weight divided by height square | Less than, on or 3rd, 5th, 10th, 25th, 50th, 75th, 85th, 95th, 97th centile and above 97th percentile | Normal | Expressed as an exact number. Negative or positive | Normal, Mild, Moderate, Severe Overweight, Obese |
| Underweight | ||||||||
| Overweight | ||||||||
| Obese | ||||||||
2.4. Outcome definitions
Acute malnutrition or wasting can be categorized based on the percentage of ideal body weight, which is calculated by dividing the actual weight by the ideal “weight-for-height/length” and multiplying by 100%, using the clinical growth charts. The percentage of ideal body weight was categorized following the Waterlow method [19]: >90% as normal, 80–90% as mild wasting, 70–79% as moderate wasting, and <70% as severe wasting [23,24].
Stunting is an indication of chronic malnutrition where height-for-age is plotted in the appropriate growth chart. The classification of stunting also utilizes Waterlow Criteria, where: >95% as normal, 90–94th percentile is classified as mild, 85–90th as moderate, and <85th as severe stunting [23,24]. BMI-for-age was also plotted for children aged >2 years on the CDC growth centiles, as these charts included age, weight, and height [25]. The cutoffs for BMI were revised in 2004 by an expert committee [26], The cutoff for underweight is below the 5th percentile, whereas the 5th–85th percentile is considered normal, 85th to < 95th percentile is considered overweight and ≥95th percentile is considered obese [27].
The following criteria are used for the updated pediatric malnutrition indicators based on the consensus statement of the Academy of Nutrition and Dietetics and the American Society of Parenteral and Enteral Nutrition [18].
For the indicators that require only one data point, critera for mild malnutrition were as follows:
-
•
Weight-for-length Z-score ranged between −1 and −1.9 in children aged <2 years
-
•
Or BMI-for-age Z-score between −1 and −1.9 in children aged >2 years,
-
•
Mid-upper arm circumference Z-score between −1 and −1.9.
For the indicators that require at least two data points, the criteria for mild malnutrition were as follows:
-
•
Weight gain velocity <75% of the ideal for children aged <2 years
-
•
Or 5% weight loss from usual body weight for children aged >2 years
-
•
Decline in weight-for-length/BMI-for-age Z-score of 1
-
•
Estimated nutrient intake 51–75% of energy and protein requirements [14].
For the indicators that require only one data point, critera for moderate malnutrition were as follows:
-
•
Weight-for-length ranged between −2 to −2.9 Z-score for children aged <2 years
-
•
Or BMI-for-age was −2 to −2.9 Z-score for children aged >2 years,
-
•
Mid-upper arm circumference between −2 to −2.9 Z-score.
For the indicators that require at least two data points, the criteria for moderate malnutrition were as follows:
-
•
Weight gain velocity <50% of the ideal for children aged <2 years
-
•
Or 7.5% weight loss from usual body weight for children >2 years,
-
•
Decline in weight-for-length/BMI-for-age Z-score of 2
-
•
Estimated nutrient intake 26–50% of energy and protein requirements [14].
For the indicators that require only one data point, criteria for moderate malnutrition were as follows:
-
•
Weight-for-length score was equal to or greater than −3 Z-score score for children aged <2 years
-
•
Or BMI-for-age equal to or greater than −3 Z-score for children aged >2 years,
-
•
Mid-upper arm circumference equal to or greater than −3 Z-score
-
•
Height/length-for-age is −3 Z-score [28].
For the indicators that required at least two data points, the criteria for severe malnutrition were as follows:
-
•
Weight gain velocity <25% of the ideal for children aged <2 years
-
•
Or 10% weight loss from usual body weight for children aged >2 years,
-
•
Decline in weight-for-length/BMI-for-age Z-score of 3
-
•
Estimated nutrient intake ≤25 of energy and protein requirements [14].
2.5. Data analysis
The prevalence of malnutrition in all age groups was compared using centiles and Z-scores. Then, the participants were categorized based on their age into: <2 years and >2 years. For children aged <2 years, the “interpretation of percentile weight-for-length’’ and “interpretation for weight-for-length Z-score" (normal, mild malnutrition, moderate malnutrition, severe malnutrition, possible risk of overweight, overweight, or obese) were compared. For children aged >2 years, the following comparisons were performed: “interpretation of percentile BMI-for-age centiles’’ (normal, underweight, overweight, or obese) vs. “interpretation for BMI-for-age Z-score’’ (normal, mild malnutrition, moderate malnutrition, severe malnutrition, possible risk of overweight, overweight, or obese) and “interpretation of weight-for-height centiles (normal, mild malnutrition, moderate malnutrition, or severe malnutrition)” vs. “interpretation for BMI-for-age Z-score’’ (normal, mild malnutrition, moderate malnutrition, severe malnutrition, possible risk of overweight, overweight, or obese). The prevalence of each degree of malnutrition in both age groups was calculated using the centiles and the Z-score methods.
2.6. Statistical analysis
Data were analyzed using JMP statistical software (SAS Institute, Cary, North Carolina, USA). Contingency tables were constructed to assess the relationships between the variables. For children aged >2 years, a contingency table analysis was conducted to assess the relationship between the degree of malnutrition using BMI-for-age Z-scores and that using weight-for-height values. Using centiles, kappa coefficient values of 0.30 can be taken to represent poor agreement beyond chance between the degree of malnutrition obtained by Z-scores and the degree of malnutrition by centiles.
3. Results
3.1. Study population
A total of 516 children were identified. Of these, 41 participants were excluded as they were overweight or obese (n = 27), aged >18 years (n = 1), “weight-for-height/length” could not be plotted (value not found, n = 4), demi-span was used to estimate height (n = 1), diagnosed with Down Syndrome (n = 4) or cerebral palsy (n = 2), or Sanjad–Sakati Syndrome (n = 2). Finally, 475 patients were included in the analysis.
3.2. Patient characteristics
Among the participants, 197 (41.4%) were females and 278 (58.6%) were males; 406 (85%) were in the age group 2–18 years and 69 (15%) were 0–2 years. Of the participants, 114 (24%) patients were from the nephrology clinic, 110 (23%) from the cardiology clinic, 129 (27%) from the cystic fibrosis clinic, and 122 (25%) from the gastroenterology nutrition clinic, as shown in Table 3.
Table 3.
Characteristics of patients included in the analysis.
| Characteristic | Number | Percent (%) |
|---|---|---|
| Sex | ||
| Female | 197 | 41.1 |
| Male | 278 | 58.6 |
| Age | ||
| 0–2 years | 69 | 15 |
| 2–18 years | 406 | 58 |
| Clinic specialty | ||
| Nephrology | 114 | 24 |
| Cardiology | 110 | 23 |
| Cystic fibrosis | 129 | 27 |
| Gastroenterology | 122 | 25 |
3.3. Prevalence of malnutrition
Our results showed an increase in the number of children classified as having malnutrition when the new malnutrition indicators (Z-scores) were used than when literature standards (centiles) were used. Overall, the percentage of malnutrition was 8.75% higher when Z-scores were used, as shown in Table 4.
Table 4.
Nutritional status of all the participants assessed using centiles vs. z-score.
| Growth parameters | Normal nutritionalstatus n (%) | Malnutrition status n (%) | Total number of children |
|---|---|---|---|
| Weight-for-height/length centiles | 196 (41) | 279 (58.7) | 475 |
| BMI-for-age/weight-for-height/length Z-score | 155 (32) | 320 (67.45) | |
| Percentage difference | 8.75% | ||
For children aged <2 years, the percentage of malnutrition was 4.7% higher using new malnutrition indicators (weight-for-length Z-score) compared with weight-for-length centiles, as shown in Table 5.
Table 5.
Nutritional status of children <2 years based on weight-for-length centiles and z-scores.
| Growth parameters | Normal nutritional status n (%) | Malnutrition status n (%) | Total number of children assessed using weight-for-length |
|---|---|---|---|
| Weight-for-length centiles | 28 (40.5) | 41 (59.4) | 69 |
| Weight-for-length Z-score | 26 (37.6) | 43 (62.3) | |
| Percentage difference | 4.7% | ||
For children aged >2 years, the percentage of malnutrition was 9.6% higher when BMI-for-age Z-score was used compared to weight-for-height centiles while there were 15.8% higher malnourished children when BMI-for-age Z-score used compared to BMI-for-age centiles for the same group, as shown in Table 6, Table 7.
Table 6.
Nutritional status of children >2 years based on weight-for-height centiles and BMI-for-age z-score.
| Growth parameters | Normal nutritional status n (%) | Malnutrition status n (%) | Total number of children assessed using BMI-for-age centiles |
|---|---|---|---|
| Weight-for-height centiles | 168 (41) | 238 (58.6) | 406 |
| BMI-for-age z-score | 129 (31.7) | 277 (68.2) | |
| Percentage difference | 9.6% | ||
Table 7.
Nutritional status of children >2 years based on BMI-for-age centiles and z-scores.
| Growth parameters | Normal nutritional status n (%) | Malnutrition status n (%) | Total number of children assessed using BMI-for-age centiles |
|---|---|---|---|
| BMI-for-age centiles | 193 (47.6) | 213 (52.4) | 406 |
| BMI-for-age Z-score | 129 (31.7) | 277 (68.25) | |
| Percentage difference | 15.8% | ||
3.4. Comparison of the severity of malnutrition
The biggest difference between centiles and Z-score was in severe malnutrition, with 15 vs. 102 patients classified as having severe malnutrition using weight-for-height/length centiles and BMI-for-age/weight-for-height/length Z-scores, respectively. This indicates a 580% increase in the detection of severe malnutrition. There were 72 patients with moderate malnutrition based on weight-for-height/length centiles and 97 with moderate malnutrition based on BMI-for-age/weight-for-height/length Z-scores (34.7% increase in detection of moderate malnutrition). There were 192 patients with mild malnutrition based on weight-for-height/length centiles and 121 with mild malnutrition based on BMI-for-age/weight-for-height/length z-scores. Finally, 196 patients were classified as normal/no malnutrition based on weight-for-height/length centiles, and 155 were classified as normal/no malnutrition based on BMI-for-age/weight-for-height//length Z-scores as illustared in Table 8.
Table 8.
Mosaic plot. Interpretation of malnutrition using centiles (weight-for-height/length for all age groups) versus Z-scores (weight-for-length Z-score for those aged <2 years and BMI-for-age Z-scores for those aged >2 years).
| Normal | Mild | Moderate | Severe | Total | |
|---|---|---|---|---|---|
| Normal count | 149 | 45 | 2 | 0 | 196 |
| Total % | 31.37 | 9.47 | 0.42 | 0.00 | 41.26 |
| Col % | 96.13 | 37.19 | 2.06 | 0.00 | |
| Row % | 76.02 | 22.96 | 1.02 | 0.00 | |
| Mild count | 6 | 75 | 80 | 31 | 192 |
| Total % | 1.26 | 15.79 | 16.84 | 6.53 | 40.42 |
| Col % | 3.87 | 61.98 | 82.47 | 30.39 | |
| Row % | 3.13 | 39.06 | 41.67 | 16.15 | |
| Moderate count | 0 | 1 | 14 | 57 | 72 |
| Total % | 0.00 | 0.21 | 2.95 | 12.00 | 15.16 |
| Col % | 0.00 | 0.83 | 14.43 | 55.88 | |
| Row % | 0.00 | 1.39 | 19.44 | 79.17 | |
| Severe count | 0 | 0 | 1 | 14 | 15 |
| Total % | 0.00 | 0.00 | 0.21 | 2.95 | 3.16 |
| Col % | 0.00 | 0.00 | 1.03 | 13.73 | |
| Row % | 0.00 | 0.00 | 6.67 | 93.33 | |
| Total | 155 | 121 | 97 | 102 | 475 |
| 32.63 | 25.47 | 20.42 | 21.47 |
| Tests | Value | Probability | df |
|---|---|---|---|
| Pearson chi-square | 499.601 | <.0001 | 9 |
| Likelihood ratio | 543.536 | <.0001 | |
| Bowker's test | 193.9419 | <.0001 | |
| Kappa coefficient | 0.352137 | <.0001 | |
| N | 475 |
On the other hand, six patients were classified as normal using BMI-for-age/weight-for-length Z-scores and as mild malnutrition using weight-for-height/length centiles. One patient was classified as having moderate malnutrition using weight-for-height/length centiles and as having mild malnutrition using BMI-for-age or weight-for-height/length Z-scores. Finally, another patient classified as having severe malnutrition using weight-for-height/length centiles was classified as having moderate malnutrition using BMI-for-age or weight-for-height/length Z-scores, as illustared in Table 8.
Among children aged <2 years, three patients were classified as having severe malnutrition using weight-for-length centiles and 11 patients were classified as having severe malnutrition using weight-for-length Z-scores representing a 266% increase in the detection of severe malnutrition. There were 12 patients with moderate malnutrition based on weight-for-length centiles and 13 with malnutrition based on weight-for-length Z-scores (8% increase in detection of moderate malnutrition). Moreover, 25 patients with mild malnutrition were identified using weight-for-length centiles, and 20 with malnutrition using weight-for-length Z-scores. Finally, 28 patients were classified as normal/no malnutrition using weight-for-length centiles, and 26 as normal/no malnutrition using weight-for-length Z-scores as shown in Table 9.
Table 9.
Comparison of degrees of malnutrition using centiles versus Z-score in children <2 years old.
| Interpretation/parameter | Normal | Mild malnutrition | Moderate malnutrition | Severe malnutrition | Total number of children <2 years old |
|---|---|---|---|---|---|
| Weight-for-length centiles | 28 | 25 | 12 | 3 | 69 |
| Weight-for-length Z-score | 26 | 20 | 13 | 11 | 69 |
| Percent increase in detection of malnutrition (%) | – | 8.3 | 266 |
Among children aged >2 years, 12 patients were classified as having severe malnutrition based on weight-for-height centiles, whereas 91 patients were classified as having severe malnutrition based on BMI-for-age Z-score, reflecting an increase of 658.% in detecting severe malnutrition. Regarding moderate malnutrition, 59 patients were identified based on weight-for-height centiles and 85 based on BMI-for-age z-scores, indicating a 44% increase in detection. A total of 167 patients were detected to have mild malnutrition based on weight-for-height centiles and 101 patients based on BMI-for-age Z-scores. Finally, 168 and 129 patients were classified as normal/no malnutrition based on weight-for-height centiles and BMI-for-age Z-scores, respectively as shown in Table 10.
Table 10.
Comparison of degrees of malnutrition using centiles versus Z-score in children >2 years old.
| Interpretation/parameter | Normal | Mild malnutrition | Moderate malnutrition | Severe malnutrition | Total number of children >2 years old |
|---|---|---|---|---|---|
| Weight-for-length centiles | 168 | 167 | 59 | 12 | 406 |
| BMI for age Z-score | 129 | 101 | 85 | 91 | |
| Percent increase in detection of malnutrition (%) | – | – | 44 | 658.3 |
A comparison between BMI-for-age centiles and Z-scores in children aged >2 years was conducted. We found 213 underweight patients based on BMI-for-age centiles and 277 malnourished patients (all degrees of malnutrition: mild, moderate, and severe), which reflects a 30% increase in the detection of malnutrition when BMI-for-age as shown in Table 11.
Table 11.
Mosaic plot. Interpretation of malnutrition for children aged >2 years using BMI-for-age Z-score versus BMI-for-age centile.
| Count, Total% Col%, Row % | Normal | Malnourish | Total | Tests | Value | Probability | df |
|---|---|---|---|---|---|---|---|
| Normal (Count) | 128 | 65 | 193 | Pearson chi-square | 202.548 | <.0001 | 1 |
| Total% | 31.53 | 16.01 | 47.54 | ||||
| Col% | 99.22 | 23.47 | |||||
| Row% | 66.32 | 33.68 | |||||
| Underweight (Count) | 1 | 212 | 213 | Likelihood ratio | 248.295 | <.0001 | 1 |
| Total% | 0.25 | 52.22 | 52.46 | ||||
| Col% | 0.78 | 76.53 | |||||
| Row% | 0.47 | 99.53 | |||||
| Total | 129 | 277 | 406 | n | 406 | ||
| 31.77 | 68.23 |
3.5. Degree of malnutrition
The distribution of the degree of malnutrition using Z-scores was significantly different from that using centiles (X2 (9, N = 475) = 499, P=<.0001) as shown in Table 8. Approximately 23% (45 of 196) of children classified as normal based on centiles were classified as having mild malnutrition when Z-scores were used, and 42% (80 of 192) of children who were classified as having mild malnutrition based on centiles were classified as having moderate malnutrition when Z-scores were used as shown in Table 8.
Regarding the relationship between the degree of malnutrition using Z-scores (weight-for-length Z-score for those aged <2 years and BMI-for-age Z-score for those aged >2 years) and centiles (weight-for-length for all age groups) normal vs. malnourished, a significant difference in distribution was observed (X2 (1, N = 475) = 499, P=<.0001). Approximately 24% (47 of 196) of children classified as normal using weight-for-height/length centiles were classified as malnourished using Z-scores, as shown in Table 12.
Table 12.
Mosaic plot contingency analysis. Interpretation of degree of malnutrition using Z-scores (weight-for-length Z-score for those aged <2 years and BMI-for-age Z-score for those aged >2 years) versus using centiles (weight-for-height/length for all ages).
| Count, Total%, Col%, Row% | Normal | Malnourish | Total |
|---|---|---|---|
| Normal(count) | 149 | 47 | 196 |
| Total% | 31.37 | 9.89 | 41.26 |
| Col% | 96.13 | 14.69 | |
| Row% | 76.02 | 23.98 | |
| Malnourished(count) | 6 | 273 | 279 |
| Total% | 1.26 | 57.47 | 58.74 |
| Col% | 3.87 | 85.31 | |
| Row% | 2.15 | 97.85 | |
| Total | 155 | 320 | 475 |
| 32.63 | 67.37 | ||
| Tests | Value | Probability | df |
| Pearson chi-square | 285.764 | <.0001 | 1 |
| Likelihood ratio | 326.087 | <.0001 | 1 |
| Bowker's test | 31.71698 | <.0001 | |
| Kappa coefficient | 0 0.76 | <.0001 | |
| n | 475 |
A contingency table analysis was conducted to assess the relationship between the degree of malnutrition of children aged >2 years using BMI-for-age Z-score (normal vs. malnourished) and the degree of malnutrition using BMI centiles (normal vs. malnourished). We found a significant difference (X2 (4, N = 406) = 202.548, P=<.0001). Approximately 34% (65 of 193) of children classified as normal using centiles were classified as having malnutrition using Z-scores, as shown in Table 11.
4. Discussion
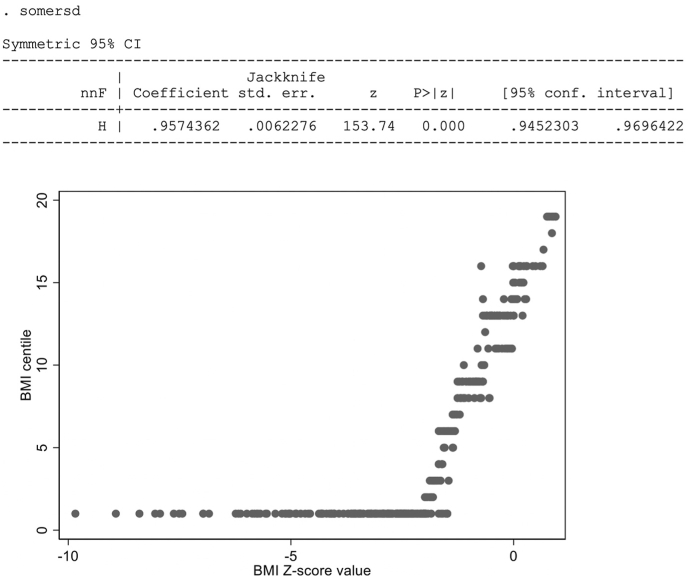
The aim of the present study was to assess whether Z-score growth indicators will detect a higher percentage of pediatric malnutrition and also to assess the degree of malnutrition in comparison with growth chart centiles in the same population. Of the 475 participants whose percentile nutritional status and Z-score nutritional status were assessed. Fig. 2 illustrates the simultaneous distribution of the pairs of measurement for all study participants. There were more gradations for the Z-score scale than for the percentile score, reflecting a natural grouping that is done in practice among nutritionists. The natural trend noted from this figure indicates that as Z-scores increase, the percentile value increases. The degree to which this concordance happens is reflected by Somer's D coefficient, which was equivalent to 0.9574362 (95% confidence interval: 0.9452303–0.9696422). This figure was obtained by considering all possible pairs of subjects (i.e., 475!/(2!)(473!) = 112,575). Among these pairs, 95% were in concordance (i.e., increasing Z-scores between two subjects also showed increasing percentiles). This balance (approximately 5%) reflects situations where the two nutritional indices differed and suggests that perhaps the Z-score is a better index.
Fig. 2.
Somer’s D coefficient, concordance between BMI-for-age Z-score and BMI-for-age centiles.
The prevalence of pediatric malnutrition differs depending on the criteria used for the definition. Indeed, pediatric malnutrition is well documented and has been extensively studied; however, there hasn't been universally consistent to identify malnutrition using the same parameters [20].
The prevalence of acute and chronic pediatric malnutrition in a Canadian tertiary-care pediatric hospital was 6.9–13.4%, respectively, using weight-for-height/length with a cutoff ≤2 standard deviations as an indicator of acute malnutrition and height-for-age with a cutoff ≤2 standard deviations as an indicator of chronic malnutrition [29]. In our study the prevelance of moderate malnutrition was 15% using weight-for-height/length centile and the prevelance was 20% using weight-for-length/BMI-for-age Z-scores.
In a European multi-centric study, the prevalence of moderate to severe malnutrition was 7–10%, respectively, using BMI-for-age. The cutoff “between −2 and ≥ −3 standard deviations” was used as an indicator of moderate malnutrition, and BMI-for-age “>−3 standard deviations” as an indicator of severe malnutrition [9]. In our study the prevelance of moderate to severe Malnutrition for children >2 years of age using the same cutoff points was 20–22% respectively as shown in table 10.
The prevalence of malnutrition in Saudi Arabia was reported to be 9.8% and 2.9% for moderate to severe wasting, respectively, which was defined as weight-for-height below −2 and −3 staundard deviations, respectively [7]. In our study the prevelance of moderate to severe malnutrition for children >2 years using BMI for age −2 and −3 Z-score as cut off points was 20–22% respectively and for children <2 years, prevelance of moderate to severe Malnutrition using Weight for height −2 and −3 Z-score as cut off points was 19–16% respectively as shown in table 9.
In 2009, the WHO, in collaboration with the United Nations Children's Fund (UNICEF), documented diagnostic identification for severe acute malnutrition in children from 6 to 60 months of age, and the cutoff for weight-for-height/length and mid-arm muscle circumference were less than −3 standard deviation and less than 115 cm, respectively [30].
In our study, it is clear that the percentage of malnutrition is higher when using the Z-score (BMI-for-age for children above 2 years/weight-for-length for children below 2 years of age) rather than centiles. This is particularly useful in a clinical setting, as malnutrition is detected sooner, and nutrition intervention can be started earlier.
In this study, we only used one data point, BMI-for-age/weight-for-length, from the new consensus statement defining standardized indicators needed to identify stages of pediatric malnutrition [18]. Height-for-age was assessed for all patients, and although in the clinical setting, height-for-age is a part of the malnutrition assessment, we did not include it in our analysis owing to the many factors involved in stunting (limited data for −1 to −2.9 Z-score, non-nutritional stunting, retarded growth following protein-calorie malnutrition, and genetic factors) [10,12]. Although some patients included in this study were follow-up patients, many were new. Therefore, we could not obtain complete data on weight gain velocity, weight loss, deceleration in BMI-for-age, and weight-for-length Z-score, so those parameters were not used in this study. Additionally, the assessment of mid-upper arm circumference is not a routine practice for all patients in nutrition clinics; thus, it was not used in this study.
Ideally, the Saudi growth charts should have been used since the study population was all Saudi, and the Saudi growth charts are available [31]. El-Mouzan et al. published the Saudi growth chart based on percentiles in 2007 and strongly encouraged clinics in the Kingdom to use them. El-Mouzan et al. also published an article comparing CDC growth charts, 2000, with Saudi growth charts, 2005 [32]. One of the most pertinent findings when comparing BMI curves between both charts was the upward shift of the 95th percentile in the Saudi chart compared to CDC charts; we attribute this to the increase in the prevalence of obesity in our study population. The comparison charts also showed a downward trend of the 50th percentile in Saudi charts for boys aged 2–19 years, possibly indicating that the ideal BMI using Saudi Z-scores would be less than the ideal body weight using CDC growth charts for boys aged 2–19 years. However, the opposite trend was noted for girls aged 2–19 years, as the 50th percentile in Saudi charts reflected an upward trend, indicating that the ideal BMI in the Saudi growth charts for girls could potentially be higher [32].
Our study had a few limitations. First, we focused on only one indicator, i.e., BMI-for-age or weight-for-length, whereas pediatric malnutrition indicators comprise six indicators for each age group [18]. Second, we used the CDC and WHO growth charts as recommended in the new consensus statement [18] instead of the Saudi Z-score growth reference. This was done because despite the availability of the Saudi Z-score growth reference [33,34]. Different cutoff points were used in both of these studies to define malnutrition, stunting, and obesity. Notably, thinness was defined in the Saudi Z-score growth references studies as BMI less than −2 Z-score. The standardized indicators needed to identify the stages of pediatric malnutrition based on the Academy of Nutrition and Dietetics and American Society of Parenteral and Enteral Nutrition [18] statement defined mild malnutrition with a BMI −1 Z-score, moderate malnutrition with a −2 Z-score, and severe malnutrition as −3 Z-score. Owing to the difference in malnutrition cutoff points and the fact that the new indicators of pediatric malnutrition [7] were not validated using Saudi Z-score growth references, we decided to use the CDC and WHO growth charts in this study.
5Future research and conclusion
For future studies, it would be noteworthy to validate the new pediatric malnutrition indicators using the Saudi Z-score growth references for improved accuracy. An online calculator similar to “Peditools.org” would be particularly beneficial in clinical settings, as it is much quicker than plotting each patient on a graph. It may be the case that a modified pediatric malnutrition indicator would need to be developed, taking into account the growth patterns of the Saudi population. It would also be useful to study the percentage of malnutrition using all six indicators for each age group further.
In conclusion, our study found a higher percentage of pediatric malnutrition when growth parameters was assessed using the Z-score (BMI-for-age for children >2 years/weight-for-length for children <2 years of age) than the centiles growth chart. This indicates that updated malnutrition indicators (Z-score) is a more sensitive parameter to the severity of pediatric malnutrition than traditional centiles. Further studies are needed to assess the new pediatric malnutrition indicators using the Saudi Z-score growth references and establishing appropriate cut-off points.
Ethical approval
The study protocol was reviewed and approved by the KFSH research ethics committee.
Waiver of informed consent was requested and approved as the nutrition assessment did not differ from routine clinical practice.
Funding sources
None.
Declaration of competing interest
None.
Acknowledgments
We would like to thank Nourah Alqahtani from Biostatistics, Epidemiology, and Scientific Computing Department (BESC) for her valuable help.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
Contributor Information
Mai Adnan Ezzat, Email: mezzat@kfshrc.edu.sa.
Ebtsam Mohmmed Albassam, Email: ealbassam@kfshrc.edu.sa.
Eman Abdullah Aldajani, Email: ealdajani@kfshrc.edu.sa.
Raneem Abdulaziz Alaskar, Email: ralaskar@kfshrc.edu.sa.
Edward Bentz Devol, Email: edevol@kfshrc.edu.sa.
References
- 1.Klanjsek P., Pajnkihar M., Marcun Varda N., Povalej Brzan P. Screening and assessment tools for early detection of malnutrition in hospitalised children: a systematic review of validation studies. BMJ Open. 2019;9(5) doi: 10.1136/bmjopen-2018-025444. e025444-e025444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Identification of severe acute malnutrition in children 6–59 months of age. 2020. https://www.who.int/elena/titles/sam_identification/en/ Updated 11 February 2019. [Google Scholar]
- 3.World Health Organization . World Health Organization; April 21, 2020. Fact Sheet/Children: reducing mortality.https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality Updated 19 September 2019. [Google Scholar]
- 4.2018 Global Nutrition Report The burden of malnutrition. 21 April, 2020. https://globalnutritionreport.org/reports/global-nutrition-report-2018/burden-malnutrition/c [Chapter 02]
- 5.World Health Organization . 21 April 2020. Fact sheets/Detail/Adolescents: health risks and solutions.https://www.who.int/en/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions Updated 13 December 2018. [Google Scholar]
- 6.Best C., Neufingerl N., van Geel L., van den Briel T., Osendarp S. The nutritional status of school-aged children: why should we care? Food Nutr Bull. 2010/09/01 2010;31(3):400–417. doi: 10.1177/156482651003100303. [DOI] [PubMed] [Google Scholar]
- 7.El Mouzan M.I., Foster P.J., Al Herbish A.S., Al Salloum A.A., Al Omar A.A., Qurachi M.M. Prevalence of malnutrition in Saudi children: a community-based study. Ann Saudi Med. Sep-Oct 2010;30(5):381–385. doi: 10.4103/0256-4947.67076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abou-Zeid A.H., Abdel-Fattah M.M., Al-Shehri A.S., Hifnawy T.M., Al-Hassan S.A. Anemia and nutritional status of schoolchildren living at Saudi high altitude area. Saudi Med J. Jun 2006;27(6):862–869. [PubMed] [Google Scholar]
- 9.Hecht C., Weber M., Grote V., et al. Disease associated malnutrition correlates with length of hospital stay in children. Clin Nutr. Feb 2015;34(1):53–59. doi: 10.1016/j.clnu.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Corkins M.R., Guenter P., DiMaria-Ghalili R.A., et al. Malnutrition diagnoses in hospitalized patients: United States, 2010. JPEN - J Parenter Enter Nutr. Feb 2014;38(2):186–195. doi: 10.1177/0148607113512154. [DOI] [PubMed] [Google Scholar]
- 11.Cusick S.E., Georgieff M.K. The role of nutrition in brain development: the golden opportunity of the "first 1000 days. J Pediatr. 2016;175:16–21. doi: 10.1016/j.jpeds.2016.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beer S.S., Juarez M.D., Vega M.W., Canada N.L. Pediatric malnutrition: putting the new definition and standards into practice. Nutr Clin Pract. Oct 2015;30(5):609–624. doi: 10.1177/0884533615600423. [DOI] [PubMed] [Google Scholar]
- 13.Walson J.L., Berkley J.A. The impact of malnutrition on childhood infections. Curr Opin Infect Dis. 2018;31(3):231–236. doi: 10.1097/qco.0000000000000448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Childhood stunting: context, causes and consequences, WHO conceptual framework. World Health Organization; 26 March 2020. https://www.who.int/nutrition/events/2013_ChildhoodStunting_colloquium_14Oct_ConceptualFramework_colour.pdf [Google Scholar]
- 15.Bouma S. Diagnosing pediatric malnutrition: paradigm shifts of etiology-related definitions and appraisal of the indicators. Nutr Clin Pract. 2017;32(1):52–67. doi: 10.1177/0884533616671861. [DOI] [PubMed] [Google Scholar]
- 16.Fenton T., Sauve R. Using the LMS method to calculate Z-scores for the Fenton preterm growth chart. Eur J Clin Nutr. 2008;61:1380–1385. doi: 10.1038/sj.ejcn.1602667. [DOI] [PubMed] [Google Scholar]
- 17.National Center for Chronic Disease Prevention and Health Promotion . 21 April, 2020. Use and interpretation of the WHO and CDC growth charts for children from birth to 20 Years in the United States.https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/growthchart.pdf Updated May 2013. [Google Scholar]
- 18.Becker P., Carney L.N., Corkins M.R., et al. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition) Nutr Clin Pract. 2015;30(1):147–161. doi: 10.1177/0884533614557642. [DOI] [PubMed] [Google Scholar]
- 19.Driscoll P., Lecky F., Crosby M. Article 4. An introduction to estimation—1. Starting from Z. J Accident Emerg Med. 2000;17(6):409. doi: 10.1136/emj.17.6.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCarthy A., Delvin E., Marcil V., et al. Prevalence of malnutrition in pediatric hospitals in developed and in-transition countries: the impact of hospital practices. Nutrients. 2019;11(2):236. doi: 10.3390/nu11020236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joosten K., Hulst J. Prevalence of malnutrition in pediatric hospital patients. Curr Opin Pediatr. 2008;20:590–596. doi: 10.1097/MOP.0b013e32830c6ede. [DOI] [PubMed] [Google Scholar]
- 22.Waterlow J.C. Classification and definition of protein-calorie malnutrition. Br Med J. 1972;3(5826):566–569. doi: 10.1136/bmj.3.5826.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leonberg B.L. second ed. Academy of Nutrition and Dietetics; 2013. Academy of nutrition and Dietetics pocket guide to pediatric nutrition assessment; p. 174. [Google Scholar]
- 24.Parikh K., Marein-Efron G., Huang S., O'Hare G., Finalle R., Shah S.S. Nutritional status of children after a food-supplementation program integrated with routine health care through mobile clinics in migrant communities in the Dominican Republic. Am J Trop Med Hyg. 2010;83(3):559–564. doi: 10.4269/ajtmh.2010.09-0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CDC Using BMI-for-age as a screening tool/advantages to using BMI-for-age as a screening tool for obesity, overweight, and underweight. March 13 2020. https://www.cdc.gov/nccdphp/dnpao/growthcharts/training/bmiage/page2.html
- 26.Barlow S.E. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 27.Growth C.D.C. Chart training/recommended BMI-for-age cutoffs. March 13 2020. https://www.cdc.gov/nccdphp/dnpao/growthcharts/training/bmiage/page4.html
- 28.Malnutrition Pediatric. Frequently asked questions. 2015. http://www.nutritioncare.org/Guidelines_and_Clinical_Resources/Toolkits/Malnutrition_Toolkit/Related_Publications/2020
- 29.Durá-Travé T., San Martin-García I., Gallinas-Victoriano F., Vaquero Iñigo I., González-Benavides A. Prevalence of malnutrition in hospitalised children: retrospective study in a Spanish tertiary-level hospital. JRSM Open. 2016;7(9) doi: 10.1177/2054270416643889. 2054270416643889-2054270416643889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Organization W.H. 2020. WHO child growth standards and the identification of severe acute malnutrition in infants and childrenA Joint Statement by the World Health Organization and the United Nations Children's Fund. 24 March.https://www.who.int/nutrition/publications/severemalnutrition/9789241598163_eng.pdf [PubMed] [Google Scholar]
- 31.El-Mouzan M.I., Al-Herbish A.S., Al-Salloum A.A., Qurachi M.M., Al-Omar A.A. Growth charts for Saudi children and adolescents. Saudi Med J. 2007;28(10):1555–1568. [PubMed] [Google Scholar]
- 32.El Mouzan M.I., Al Herbish A.S., Al Salloum A.A., et al. Comparison of the 2005 growth charts for Saudi children and adolescents to the 2000 CDC growth charts. Ann Saudi Med. Sep-Oct 2008;28(5):334–340. doi: 10.5144/0256-4947.2008.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.El Mouzan M.I., Al Salloum A.A., Alqurashi M.M., Al Herbish A.S., Al Omar A. The LMS and Z scale growth reference for Saudi school-age children and adolescents. Saudi J Gastroenterol. Jul-Aug 2016;22(4):331–336. doi: 10.4103/1319-3767.187608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.El Mouzan M., Salloum A.A., Omer A.A., Alqurashi M., Herbish A.A. Growth reference for Saudi school-age children and adolescents: LMS parameters and percentiles. Ann Saudi Med. Jul-Aug 2016;36(4):265–268. doi: 10.5144/0256-4947.2016.265. [DOI] [PMC free article] [PubMed] [Google Scholar]