Abstract
Aim of the study
Regular refresher skill courses are necessary to maintain competence in basic life support. The utilization of these training programs strongly depends on the motivation to learn. Learning motivation may be affected by overconfidence and clinical tribalism, as they both imply a higher competence compared to others, and therefore, a lower demand for training. This study aimed to assess how overconfidence in basic life support competencies affects learning motivation.
Methods
We conducted a cross-sectional, observational, multicenter, anonymous online questionnaire survey using validated psychometric tests for healthcare professionals in Germany. Further, we tested participants’ knowledge and attitude regarding international basic life support guidelines. The study was conducted between March and April 2022, and healthcare providers from 22 German emergency medical services and hospitals at all levels were assessed.
Results
Of 2,000 healthcare professionals assessed, 407 completed the assessment (response rate, 20.4%). We confirmed the presence of overconfidence and clinical tribalism (identity differentiation between social groups) among the 407 physicians, nurses, and emergency medical service providers who completed the survey. Three different learning-motivation groups emerged from cluster analysis: “experts” (confident and motivated), “recruitables” (overconfident and motivated), and “unawares” (overconfident and unmotivated). The three groups were present in all professional groups, independent of the frequency of exposure to cardiac arrest and educational level.
Conclusions
These findings showed the presence of overconfidence effects and different learning motivation types in individuals learning basic life support, even in instructors.
Keywords: Basic Life Support, Cardiopulmonary Resuscitation, Lifelong Learning, Overconfidence, Clinical Tribalism
Introduction
Competency in basic life support (BLS) is fundamental in recognizing and treating cardiac arrest to achieve the best possible outcomes.1, 2, 3 To do so, healthcare workers need regular training to maintain their BLS proficiency, which requires sufficient motivation.
The self-determination theory is a model that describes human motivation and links motivation to the three needs that drive behavior, e.g., in learning: autonomy, competence, and relatedness. Generally, individuals are motivated to learn and develop when their basic needs are met. If not, individuals can feel unmotivated or need external stimuli (rewards or punishments) to drive their behavior. According to this theory, motivation is a product of the interaction between extrinsic environmental stimuli and individual’s intrinsic needs. This theory describes different types of motivation4, 5 (e.g., applied to learning): intrinsic (“I want to learn”) and extrinsic motivation (“I have to learn”). Furthermore, the latter encompasses “identified regulation” (“I have to learn because it is my duty as a medical expert”), “external regulation” (“I have to learn because my boss says I have to”), and “amotivation” (“I do not want to learn”). A tool for assessing learning motivation is the Situational Motivation Scale (SIMS).6 Intrinsic motivation generally achieves improved learning, but a combination of strong intrinsic motivation and moderate extrinsic motivation7 is optimal.
One key point is awareness of the necessity for further training, which is only realized through the self-assessment of one’s competencies. Unfortunately, self-assessment is a poor predictor of competencies,8 and may be influenced by three overconfidence effects.9 Overestimation is the belief to be better than assessments or reality would show. Overplacement is the belief of being better than others, while overprecision is an exaggerated belief that is accurate in these estimations. A subcategory of overplacement is believing that colleagues from one’s profession are superior to those from other professions. This effect is called the Clinical Tribalism Phenomenon (“We are better than them”), which can be compared to an in-group bias.10
These effects have been demonstrated in various fields of human behavior studies, including economics, education, transport, health, and crime.9, 11, 12, 13, 14, 15 In the healthcare sector, our research group demonstrated the impact of overconfidence on different aspects of infection control and communication.16, 17, 18, 19 In a recent study, we correlated learning motivation with overconfidence in hand hygiene training. Therein, the cluster analyses revealed three groups of healthcare workers: “experts” (confident and motivated), “recruitables” (overconfident and motivated), and “unawares” (highly overconfident and unmotivated).20
Because BLS is a medical core competency, we raised the question of whether learning motivation and overconfidence play a role in BLS training motivation. Thus, this study aimed to examine the correlations between overconfidence effects and learning motivation in healthcare workers’ BLS competencies. Hence, we aim to falsify the following null hypotheses:
i) Primarily
-
a)
H01a: Overplacement for BLS is not present in healthcare workers.
H01b: Overestimation for BLS is not present in healthcare workers.
ii) Secondarily
-
b)
H02: Learning motivation, measured by SIMS, does not correlate with overplacement.
-
c)
H03: Correlation between overestimation and learning motivation did not show the three groups of healthcare workers (unaware, experts, and recruitables).
-
d)
H04: Clinical tribalism for BLS is not present among healthcare workers and does not correlate with learning motivation.
Methods
According to the ethics committee of the Physicians’ Association of Baden-Wurttemberg, Germany, no ethical approval was required for this study.
We adapted the pre-existing instrument20 and pre-tested it with six Advanced Cardiovascular Life Support (ACLS) instructors. Next, we pre-tested the face and content validity within a group of eight American Heart Association (AHA) and European Resuscitation Council (ERC) instructors by answering a test version of the questionnaire and screening the International Liaison Committee on Resuscitation, AHA, and ERC guidelines on BLS. Furthermore, we conducted a pre-test for content and constructed validity among 152 healthcare workers recruited through an online social media convenience sampling. Subsequently, we assessed 2,000 healthcare workers in 22 institutions in Germany directly via e-mail. The institutions reported the number of individuals assessed. The survey was conducted between March and April 2022 on the platform “umfrageonline.com,” Enuvo GmbH Zurich, Switzerland.
Physicians, nurses, and emergency medical service (EMS) providers were eligible to participate. We contacted individuals with repetitive exposure to BLS situations at different educational levels, including undergraduates, postgraduate providers, and instructors. The survey was accessed on any device (personal computer, tablet, or smartphone).
The survey consisted of 33 questions. Eight demographic variables (gender, actual age [birthdate], subjective age [feeling], years of experience, profession, grade of qualification, area of work, and qualification in resuscitation courses) were collected (see Table AQ1 in Appendix A).
Motivation to learn was measured with the German translation of the SIMS instrument described in detail in Section CS1 of Appendix C.6, 20
Self-reported competencies regarding BLS: We used a five-item instrument to measure BLS for one’s own competencies (Cronbach’s alpha [α] = 0.75) and professionals of the same profession (α = 0.85), physicians (α = 0.75), nurses (α = 0.78), and emergency service personnel (α = 0.76). The scale includes competencies regarding cardiopulmonary resuscitation (CPR), cardiac arrest recognition, error identification, corrective interventions, and feedback reception. The instruments were scored on a five-point rating scale, ranging from one (“completely disagree”) to five (“completely agree”).
Overplacement: The overplacement score (α = 0.80) was computed as an index of the differences between the corresponding items of self-reported competencies and reported competencies of other professionals regarding the BLS, with a possible range of −4 to 4.
Patients’ safety attitudes were measured by two separate items using the ISO 31000 matrix,21 which assessed the perceived maximum credible harm of a risk and actual occurrence thereof, as described in detail in Section CS2 of Appendix C.
Knowledge test: We presented 20 questions with four response options, including certainly false, maybe false, maybe true, and certainly true. We used two scores to determine the participants’ knowledge level regarding BLS. The first score was computed as a dichotomous variable, referring to passing or failing the core test. The core knowledge test consisted of three questions chosen by a panel of instructors22, 23, 24:
-
1.
“Cardiopulmonary resuscitation in adults is conducted with a compression frequency of at least 120 per minute” (certainly false).
-
2.
“Compression depth should be 5–6 cm (2–2.5 inch) in adults” (certainly true).
-
3.
“If an automated external defibrillator is available, the rhythm analysis should be conducted as fast as possible” (certainly true).
The participants were required to correctly answer all the three core questions in order to pass the core test. We considered response options that were certainly true or perhaps true as true, and those that were certainly false or maybe false as false. Participants who failed the core test were assigned a value of 0, and those who passed the core test were assigned a value of 1.
The second score was calculated using “non-core” knowledge test to determine the knowledge level of the participants regarding BLS. The score was computed as an index of the sum of 12 correctly answered questions that were labeled as relevant but non-core questions. For every correctly answered question (certainly or maybe a response option), the participants were assigned one point. The worst possible score was 0 (answering all the 12 non-core questions incorrectly), and the best possible score was 1 (answering all the 12 non-core questions correctly). Five questions were excluded from the non-core knowledge test score because they could not be answered precisely and unambiguously according to both the AHA and ERC guidelines. All the 20 questions are shown in Table AQ2, Appendix A.
Overestimation was assumed for those individuals who judged their competencies highly (Mean [M] = 4–5), but failed the core test (answering at least one of the three core questions, A, D, and E, incorrectly; see Table AQ2, Appendix A).
Clinical Tribalism was calculated separately for nurses (nurses vs. physicians α = 0.77; nurses vs. EMS α = 0.76), physicians (physicians vs. nurses α = 0.79; physicians vs. EMS α = 0.74), and EMS providers (EMS vs. nurses α = 0.75; EMS vs. physicians α = 0.70), as an index of differences between the corresponding items of reported BLS competencies of one professional group and BLS competencies of the other two professional groups. The scales were computed as the difference between the three corresponding items regarding CPR performance, corrective interventions, and feedback reception.
The next set of items asked whether the participant would correct others in case of an observed error during BLS. More specifically, whether a naïve person, lay rescuer, nursing student, nurse, instructor, medical student, registrar, consultant, and head of the department would be corrected was assessed using the same five-point Likert scale, ranging from one (“completely disagree”) to five (“completely agree”), as in the competencies section.
We performed data analyses using SPSS 28.0 by IBM. Effect sizes were estimated using Cohen’s Dz (the standardized mean difference effect size for within-subject designs25) with interpretation according to Lakens (Dz < 0.3 equals weak, 0.3 ≤ Dz < 0.8 moderate, and strong Dz ≥ 0.8).25 The presence of overplacement and clinical tribalism was tested using the paired sample t-test with bootstrapping at 95% confidence intervals (bias-corrected and accelerated [BCa] based on 1,000 samples). Linear correlations were evaluated using Pearson’s product-moment correlation matrix with bootstrapping at 95% confidence intervals (BCa based on 1,000 samples). Additionally, we performed quadratic regressions with bootstrapping at 95% confidence intervals (BCa based on 1,000 samples) to evaluate quadratic correlations between overplacement and motivation to learn as well as clinical tribalism and motivation to learn. Therein, SIMS-dimensions (intrinsic motivation, identified regulation, external regulation and amotivation) served as a criterion variable in combination with predictor variables overplacement or clinical tribalism and their corresponding quadratic terms. Hypothesis H03 was tested by performing a two-step cluster analysis26, 27 (see Section CS3 in Appendix C for detailed information on this method).
For two-tailed paired sample t-test with statistical power 1-β = 0.8 and a medium effect size (Cohen’s Dz = 0.5), the calculated minimum sample size was n = 128 (Hypotheses H01a and H01b). For multiple regressions with three predictors (quadratic regressions), a medium effect size (f2 = 0.15), and statistical power 1-β = 0.8, the calculated minimum sample size was n = 77 (Hypotheses H02 and H04). Additionally, according to Formann (1984), the minimum sample size for cluster analysis with k = 7 included variables 2k = 12828 (Hypothesis H03).
Additionally, to present demographic results and descriptive statistics with mean (M) and standard deviations (SD) for continuous variables and number (n) with percentage (%) for categorical variables, the data analysis was planned to be conducted by comparing one’s own competencies with others using the Bonferroni-corrected significance tests and presentation of correlations between learning motivation and overplacement and learning motivation and clinical tribalism, respectively. A two-tailed p value of < 0.05 was considered significant. Further, we presented effect sizes (Cohen’s Dz for intra-individual tests) as low (Dz < 0.3), moderate (0.3 ≤ Dz < 0.8), or strong (Dz ≥ 0.8) effects, and the Pearson product-moment correlation coefficient (r) with r < 0.3 as weak, 0.3 ≤ r < 0.5 as moderate, and r ≥ 0.5 as strong effect size. The cluster analysis results showed the cluster efficiency and quality of clustering, variables that influenced the clustering process most strongly, description of the cluster profiles, and internal and external validity of the cluster solution.
Results
Six hundred (30%) healthcare workers responded to the survey, and 407 (20.4%) completed the questionnaire. However, only 397 (97.5%) of the 407 participants responded to all the relevant variables and were included in the cluster analysis. Descriptive statistics of the variables and measurements are displayed in Table 1, Table 2.
Table 1.
Descriptive statistics of demographic variables for the whole sample and three clusters.
| All participants (n=407) |
Experts |
Recruitables |
Unawares |
||||||
|---|---|---|---|---|---|---|---|---|---|
| M/n | SD/% | M/n | SD/% | M/n | SD/% | M/n | SD/% | ||
| Gender | Women | 146 | 35.9% | 41 | 29.1% | 81 | 64.3% | 19 | 13.5% |
| Men | 260 | 63.9% | 105 | 41.2% | 99 | 38.8% | 51 | 20% | |
| Non-Binary | 1 | 0.2% | 0 | 0% | 0 | 0% | 0 | 0% | |
| Age (objective) in years | 36.6 | 11.1 | 37 | 10.7 | 36.5 | 10.9 | 37.1 | 11.2 | |
| Age (subjective) in years | 33.2 | 10 | 34 | 9.5 | 33.1 | 10 | 34.8 | 11 | |
| Work Experience in years | 16.7 | 11.3 | 16.8 | 10.8 | 15.2 | 11.3 | 16.4 | 11.3 | |
| All CLUSTERS* | EXPERTS | RECRUITABLES | UNAWARES | ||||||
| (N= 397) | (n=146) | (n=181) | (n=70) | ||||||
| Profession | 1.Anesthesia Nurse | 1 | 0 | 0.00% | 0 | 0.00% | 1 | 0.00% | |
| 2.Others | 9 | 1 | 12.50% | 7 | 87.50% | 0 | 12.50% | ||
| 3.Physicians (registrars) | 38 | 15 | 42.10% | 17 | 47.40% | 69 | 10.50% | ||
| 4.Physicians (consultants) | 57 | 26 | 45.60% | 22 | 40.40% | 0 | 14.00% | ||
| 5.no answer | 12 | 0 | 0.00% | 1 | 100.00% | 0 | 0.00% | ||
| 6.medical assistants | 3 | 0 | 0.00% | 3 | 100.00% | 7 | 0.00% | ||
| 7.nurses | 51 | 16 | 31.30% | 28 | 56.90% | 3 | 11.80% | ||
| 8.ICU-nurses | 47 | 15 | 31.90% | 29 | 63.80% | 31 | 4.30% | ||
| 9.EMS-Paramedics | 121 | 52 | 43.00% | 38 | 33.90% | 13 | 23.10% | ||
| 10.EMS-Basics | 70 | 21 | 29.60% | 36 | 50.70% | 18.30% | |||
| Profession | Nurses (Profession 1, 6, 7, 8) | 102 | 31 | 30.30% | 60 | 55.90% | 11 | 9.80% | |
| 3 Groups | Physicians (Profession 3,4) | 95 | 41 | 28.30% | 39 | 23.10% | 15 | 21.70% | |
| EMS Providers (Professions 9,10) | 191 | 73 | 50.30% | 74 | 43.50% | 44 | 68.30% | ||
| Education | Undergraduate | 38 | 17 | 44.70% | 17 | 44.70% | 4 | 10.50% | |
| Postgraduate | 240 | 83 | 34.60% | 113 | 47.10% | 44 | 18.30% | ||
| Educator | 106 | 43 | 40.60% | 42 | 49.60% | 210 | 19.80% | ||
| No answer | 13 | 4 | 30.80% | 9 | 69.20% | 0.00% | |||
| Workplace | Ambulance and General practitioner | 6 | 3 | 50.00% | 3 | 50.00% | 0 | 0.00% | |
| No answer | 2 | 1 | 50.00% | 1 | 50.00% | 0 | 0.00% | ||
| Primary Hospital | 28 | 14 | 50.00% | 13 | 46.30% | 1 | 3.60% | ||
| Secondary Hospital | 35 | 16 | 45.70% | 15 | 42.90% | 4 | 11.40% | ||
| Tertiary Hospital | 86 | 26 | 30.20% | 48 | 55.80% | 12 | 14.00% | ||
| Tertiary Hospital (University Clinic) | 45 | 12 | 26.70% | 29 | 64.40% | 4 | 8.90% | ||
| N/A | 4 | 2 | 50.00% | 1 | 25.00% | 1 | 25. 0% | ||
| Emergency Medical Services | 190 | 72 | 37.90% | 78 | 41.10% | 40 | 21.50% | ||
| Rehabilitation Hospital | 1 | 1 | 100.00% | 0 | 0.00% | 0 | 0.00% | ||
| Exposure to CPR | low-exposure to CPR (Professions 7,10,6) | 124 | 37 | 29.80% | 67 | 54.80% | 20 | 15.30% | |
| high-exposure to CPR (Professions 8,9,1,3,4) | 264 | 108 | 41.30% | 106 | 42.40% | 50 | 16.30% | ||
| Instructor Status according to ERC or AHA | Status not according to ERC or AHA | 60 | 32 | 53.30% | 21 | 35.00% | 7 | 11.70% | |
| BLS | 36 | 21 | 58.30% | 11 | 30.60% | 4 | 11.10% | ||
| ALS/ACLS | 33 | 17 | 51.50% | 14 | 42.40% | 2 | 6.10% | ||
| EPLS/PALS | 8 | 4 | 50.00% | 3 | 37.50% | 1 | 12.50% | ||
*Please note those 10 participants could not be included in the cluster analysis because of relevant missing data (for in depth description of the cluster analysis method see Section CS3, Appendix C), ICU: Intensive care unit, EMS: Emergency Medical Service, CRP: Cardiopulmonary Resuscitation, BLS: Basic Life Support, AHA: American Heart Association, ERC: European Resuscitation Council, ALS: Advanced Life Support, ACLS: Advanced Cardiovascular Life Support, EPLS: European Paediatric Life Support, PALS: Pediatric Advanced Life Support Provider, continuous variables are presented with Means (M) and Standard Deviations (SD) and categorical variables with numbers (n) and percentages (%).
Table 2.
Descriptive statistics of variables included in the study with the Mean (M) and standard deviation (SD) for continuous and n (%) for categorical variables.
| All participants |
Experts |
Recruitables |
Unawares |
|||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |
| Motivation | ||||||||
| Intrinsic | 5.4 | 5.6 | 5.6 | 0.2 | 5.9 | 0.9 | 3.3 | 1.2 |
| Identified | 1.3 | 1.4 | 5.9 | 1.0 | 6.2 | 0.9 | 3.4 | 1.5 |
| Extrinsic | 5.4 | 5.6 | 3.0 | 1.3 | 3.3 | 1.5 | 4.4 | 1.8 |
| Amotivation | 1.3 | 1.4 | 1.8 | 0.8 | 1.5 | 0.6 | 4.3 | 1.2 |
| SELF ASSESSMENT | ||||||||
| Self: performing CPR | 4.4 | 0.6 | 4.5 | 0.5 | 4.3 | 0.7 | 4.5 | 0.6 |
| Self: recognizing cardiac arrest and the indication to start CPR | 4.8 | 0.5 | 4.8 | 0.4 | 4.8 | 0.5 | 4.8 | 0.5 |
| Self: error identification | 4.8 | 0.5 | 4.5 | 0.5 | 4.5 | 0.5 | 4.3 | 0.7 |
| Self: corrective interventions | 4.1 | 0.8 | 4.8 | 0.4 | 4.8 | 0.4 | 4.8 | 0.5 |
| Self: feedback reception | 4.3 | 0.8 | 4.3 | 0.7 | 4.3 | 0.7 | 4.1 | 0.8 |
| Self-reported competencies | 4.5 | 0.5 | 4.6 | 0.4 | 4.4 | 0.5 | 4.5 | 0.5 |
| COLLEAGUES | ||||||||
| Colleagues: performing CPR | 4.7 | 0.5 | 4.4 | 0.7 | 4.4 | 0.7 | 4.2 | 0.9 |
| Colleagues: recognizing cardiac arrest and the indication to start CPR | 4.4 | 0.7 | 4.4 | 0.7 | 4.5 | 0.6 | 4.3 | 0.7 |
| Colleagues: error identification | 4.0 | 0.7 | 4.8 | 0.5 | 4.8 | 0.5 | 4.8 | 0.5 |
| Colleagues: corrective interventions | 4.4 | 0.7 | 4.0 | 0.7 | 4.0 | 0.7 | 4.1 | 0.7 |
| Colleagues: feedback reception | 3.8 | 0.8 | 4.5 | 0.6 | 4.5 | 0.7 | 4.4 | 0.7 |
| Overplacement | 0.5 | 0.7 | 0.6 | 0.7 | 0.4 | 0.7 | 0.6 | 0.7 |
| PHYSICIANS | ||||||||
| Physicians: performing CPR | 3.7 | 0.9 | 3.8 | 0.7 | 3.8 | 0.7 | 3.9 | 0.8 |
| Physicians: corrective interventions | 3.6 | 0.8 | 3.5 | 0.9 | 3.5 | 0.9 | 3.6 | 1.0 |
| Physicians: feedback reception | 3.6 | 1.0 | 3.1 | 0.9 | 3.1 | 0.9 | 3.3 | 1.0 |
| Reported competencies of physicians | 3.4 | 0.7 | 3.4 | 0.6 | 3.5 | 0.8 | 3.3 | 0.8 |
| Clinical tribalism Physicians vs. Nurses | 1 | 0.9 | 1.2 | 0.8 | 0.8 | 1 | 1.2 | 0.9 |
| Clinical tribalism Physicians vs. EMS Providers | 1.2 | 0.9 | 1.3 | 0.9 | 1 | 1 | 1.3 | 0.8 |
| Nurses: performing CPR | 3.2 | 1.0 | 3.4 | 0.8 | 3.4 | 0.8 | 3.5 | 0.8 |
| Nurses: corrective interventions | 2.9 | 1.1 | 2.8 | 1.1 | 2.8 | 1.1 | 3.0 | 1.1 |
| Nurses: feedback reception | 3.5 | 0.9 | 3.5 | 1.0 | 3.5 | 1.0 | 3.5 | 1.0 |
| Reported competencies of nurses | 3.3 | 0.8 | 3.2 | 0.8 | 3.4 | 0.8 | 3.2 | 0.8 |
| Clinical tribalism Nurses vs. Physicians | 1 | 0.9 | 1.2 | 0.8 | 0.8 | 1 | 1.2 | 0.9 |
| Clinical tribalism Nurses vs. EMS Providers | 0.7 | 0.8 | 0.7 | 0.7 | 0.6 | 0.9 | 0.8 | 0.8 |
| EMS providers: performing CPR | 4.0 | 0.7 | 4.09 | 0.6 | 4.1 | 0.6 | 4.0 | 0.8 |
| EMS providers: corrective interventions | 3.5 | 1.0 | 3.6 | 1.0 | 3.7 | 0.8 | 3.0 | 1.1 |
| EMS providers: feedback reception | 3.7 | 0.8 | 3.7 | 0.8 | 4.8 | 0.5 | 3.5 | 1.0 |
| Reported competencies of EMS providers | 3.7 | 0.7 | 3.8 | 0.6 | 3.7 | 0.8 | 3.7 | 0.7 |
| Clinical tribalism EMS Providers vs. Physicians | 0.9 | 1 | 1.1 | 0.8 | 0.7 | 1 | 1.1 | 1 |
| Clinical tribalism EMS Providers vs. Nurses | 1.15 | 0.9 | 1.3 | 0.9 | 1 | 1 | 1.3 | 0.8 |
| Patient Safety attitudes Maximum credible risk for incorrect CPR | 4.8 | 0.6 | 4.8 | 0.5 | 4.8 | 0.5 | 4.0 | 0.8 |
| Patient Safety attitudes Experienced Occurrence of this risk | 2.6 | 1.1 | 2.7 | 1.2 | 2.5 | 1.0 | 2.5 | 1.0 |
| Core knowledge test | ||||||||
| Passed | n = 171 | 43.1% | n = 146 | 100% | n = 0 | 0% | n = 25 | 35.7% |
| Failed | n = 226 | 56.9% | 0 | 0% | 181 | 100% | 45 | 64.3% |
| Non-core knowledge test | 0.71 | 0.17 | 0.77 | 0.15 | 0.68 | 0.16 | 0.75 | 0.15 |
| Self-Estimation of corrective interventions of lay helpers | 1.2 | 0.6 | 1.1 | 0.4 | 1.2 | 0.6 | 1.2 | 0.6 |
| Self-Estimation of corrective interventions of first aid helpers | 1.7 | 0.7 | 1.2 | 0.5 | 1.3 | 0.7 | 1.2 | 0.6 |
| Self-Estimation of corrective interventions of nursing students | 1.2 | 0.6 | 1.1 | 0.5 | 1.2 | 0.7 | 1.2 | 0.6 |
| Self-Estimation of corrective interventions of nurses | 1.3 | 0.7 | 1.2 | 0.6 | 1.4 | 0.8 | 1.3 | 0.7 |
| Self-Estimation of corrective interventions of nursing trainers | 1.6 | 0.9 | 1.4 | 0.8 | 1.6 | 1.0 | 1.6 | 0.9 |
| Self-Estimation of corrective interventions of medical students | 1.3 | 0.7 | 1.2 | 0.6 | 1.6 | 0.8 | 1.3 | 0.5 |
| Self-Estimation of corrective interventions of interns | 1.6 | 1.0 | 1.5 | 0.9 | 1.7 | 1.0 | 1.7 | 1.1 |
| Self-Estimation of corrective interventions of consultants | 2 | 1.3 | 1.8 | 1.14 | 2.10 | 1.3 | 2.1 | 1.4 |
| Self-Estimation of corrective interventions of heads of departments | 2.1 | 1.4 | 1.9 | 1.3 | 2.2 | 1.5 | 2.1 | 1.5 |
EMS: Emergency Medical Services, CRP: Cardiopulmonary resuscitation, Motivation was measured with Situational Motivational Scale comprising four dimensions (intrinsic motivation, identified regulation, external regulation and amotivation) as an index of four items using an ascending 7-Point Likert scale ranging from completely disagree (1) to completely agree (7), self-reported competencies: index of five items referring to Self: performing CRP, Self: recognizing cardiac arrest and the indication to start CPR, Self: error identification, Self: corrective interventions and Self: feedback reception on an ascending 5-Point Likert scale ranging from completely disagree (1) to completely agree (5), reported competencies of physicians, nurses and EMS providers: index of the five items referring to performing CPR, recognizing cardiac arrest and the indication to start CPR, error identification, corrective interventions and feedback reception of physicians, nurses or EMS Providers on an ascending 5-Point Likert scale ranging from completely disagree (1) to completely agree (5), overplacement score is calculated as the mean of the differences between corresponding items of self-assessment and assessment of colleagues of the same profession (e.g., the values of Colleagues: performing CPR were subtracted from the Self: performing CPR) ranging from – 4 to 4, clinical tribalism is calculated as the mean difference between the reported competencies for one own profession and other professionals (e.g., Clinical tribalism physicians vs. nurses: mean of the differences between each five items referring to physicans’ and nurses’ competencies rated only by physicians) ranging from – 4 to 4, patient safety attitudes-maximum credible risk for incorrect CPR: measures the risk on an ascending 5-Point Likert scale from (1) without consequence (1) to lethal (5), Patient Safety attitudes-Experienced Occurrence of this risk: an ascending 5-Point Likert scale from uncommon (1x > 3 years) (1) to very often (once per month) (5), core knowledge test: results of three core questions (see Table AQ2) with passed-participant answered all three core questions correctly and failed-participant failed at least one core question, non-core knowledge test: the proportion of correctly answered 12 non-core questions (see Table AQ2, Appendix A) ranging from 0 to 1, self-estimation of corrective interventions of lay helpers, first aid helpers, nursing students, nurses, medical students, interns, consultants and head of the departments: ascending 5-Point Likert scale from completely disagree (1) to completely agree (5).
Participants rated themselves better than their colleagues in performing CPR (t(225) = 4.75; p = 0.001; Dz = 0.43), accurately recognizing cardiac arrest, indication to start CPR (t(225) = 7.75; p = 0.001; Dz = 0.51), recognizing a colleagues’ errors when performing CPR (t(225) = 6.83, p = 0.001; Dz = 0.34), corrective interventions (t(225) = 4.98; p = 0.001; Dz = 0.45), and feedback reception (t(225) = 14.91; p = 0.001; Dz = 0.99) (see Table A1, Appendix A). This rejects the null hypothesis 1a and shows that the overplacement effect is present.
Of the 397 participants, 226 (56.9%) failed the core test by answering one of the core questions incorrectly, and 171 (43.1%) passed. High self-estimation (4–5 certainty points) in BLS competencies was present in 160 (93.5%) of the participants who failed the test, thereby rejecting the primary null hypothesis 1b that overestimation was not present. However, we could not identify any linear or quadratic correlation between overplacement and learning motivation (p > 0.05), confirming the null hypothesis H02 that learning motivation does not correlate with overplacement (see Tables A2-A6, Appendix A).
After performing a two-step cluster analysis with both the Bayes and Akaike information criteria, the algorithm showed that the three-cluster solution was optimal with an acceptable average Silhouette coefficient (>0.3), which suggests an adequate clustering quality. We provided further information on the quality of the analysis in Section CS4 in Appendix C. The three clusters obtained showed the following profiles:
-
1.
Group one (n = 181) showed high intrinsic motivation (mean [M] = 6 of 7 points), high identified regulation (M = 6.2 of 7 points), little extrinsic regulation (M = 3.3 of 7), low amotivation (M = 1.4 of 7 points), and no competency (all members of this cluster failed the core-knowledge test and had only 68% of all the non-core questions correctly answered), but had confidence in their own competencies (M = 4.4 of 5 maximum points for self-reported competencies).
-
2.
Group two (n = 146) was intrinsically motivated (M = 5.7 of 7 points), showed high internal motivation (M = 5.9 of 7 points), low external regulation (M = 3 of 7 points), and amotivation (M = 1.6 of 7 points), and was competent (all members passed the core-knowledge test and had an average of 77% of all the non-core questions correctly answered) and confident (self-reported competencies M = 4.6 of 5 points).
-
3.
Group three (n = 70) showed little intrinsic motivation (M = 3.4 of 7), low identified regulation (M = 3.6), high external regulation (M = 4.3 of 7), and high amotivation (M = 4.1 of 7). Additionally, 45 (64.3%) participants in this cluster failed the core knowledge test and had an average of 74% of all the non-core questions correctly answered. This group rated their competencies in BLS highly (M = 4.5 of 5). According to the AHA and ERC, 8.7% participants had an instructor certificate.
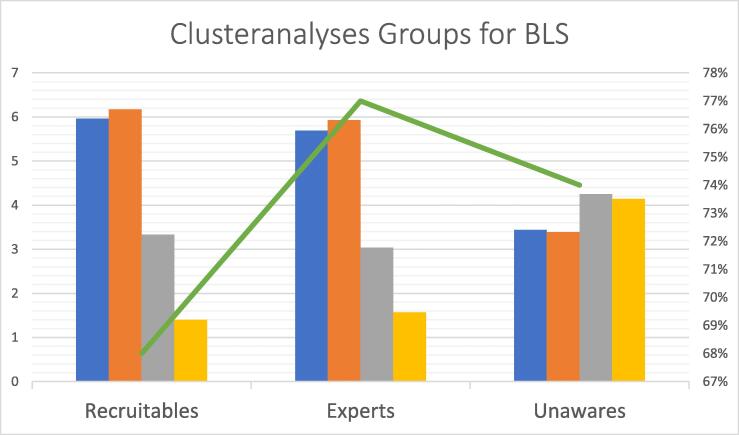
These findings reject the null hypothesis H03 and showed that in the present study, the three-cluster structure explains the associations between overestimation and learning motivation. Thus, the participants can be grouped according to their overestimation and learning motivation as “recruitables” (group one), “experts” (group two), and “unawares” (group three). The proportion of participants who reported being certified instructors differed across the clusters (χ2(2,397) = 7.83, p = 0.02). The proportion of certified instructors was higher than expected in group two (“experts”) and lower in group one (“recruitables”), which demonstrates the external validity of the cluster solution. The cluster profiles are listed in Table 1, Table 2. Fig. 1 illustrates the distribution of the four motivational dimensions, as well as the non-core knowledge test across the clusters. The results of the post-hoc tests for the paired differences of Tamhane for the four motivational dimensions, self-reported competencies, and non-core knowledge test are shown in Tables B1–6 (Appendix B).
Fig. 1.
Three clusters yielded from a two-step cluster analysis based on motivation to learn and overestimation (self-reported competencies and expressed knowledge level) regarding basic life support (BLS), (see Section CS3 and CS4, Appendix C, for detailed information on the method). Left y-axis shows four dimensions (intrinsic motivation, identified regulation, external motivation and amotivation) of the Situational Motivation Scale (SIMS) (ascending from 1 to 7 points). Colors indicate for the motivation type: Blue for intrinsic motivation, orange for identified regulation, grey for extrinsic motivation and yellow for amotivation. Right y-axis shows percentage of correct answers in Non-Core-Questions (green line, ranging from 0-1). Core questions were correctly answered only by “experts” n = 181, whereas all “recruitables” n = 146 failed the core test and 45 (64.3%) of n = 70 “unawares” failed this test. However, intrinsic motivation (“I want to learn”), identified regulation (“It’s my duty to learn”), external regulation (“my boss wants me to learn”), amotivation (“I do not want to learn”) and results of the non-core knowledge test differed significantly (p < 0.05) between at least two of three clusters (one way-analysis of variance with the Tamhane-T2 post-hoc pair comparison test using bias-corrected and accelerated (BCa) 95% Confidence Intervals in all five variables intrinsic motivation, identified regulation, extrinsic regulation, amotivation and non-core knowledge test: F (2,396) = 5.50–336.47, p < 0.001, with eta-squared (ƞ2) = 0.47–0.63 indicating strong effect sizes for dependent variables intrinsic motivation, identified regulation and amotivation, ƞ2 = 007–0.08 indicating medium effect size for external regulation and non-core knowledge test). Regarding intrinsic motivation and identified regulation the Tamhane-T2 post-hoc test revealed that “experts” were significantly stronger intrinsic motivated and showed stronger identified regulation to attend a training refreshing BLS in comparison to “unawares” and “recruitables”, p < 0.01. In addition, “recruitables” showed stronger intrinsic motivation and identified regulation compared to “unawares” p < 0.01. Regarding external regulation and amotivation “experts” and “recruitables” did not significantly differ, p > 0.05. However, in comparison to “unawares” both “experts” and “recruitables” showed lower external regulation as well as amotivation p < 0.01. “Experts” showed significantly better performance on the non-core knowledge test than “unawares” and “recruitables” p < 0.01, wherein there was no significant difference in the performance between “unawares” and “recruitables” p > 0.05. For more information on the results of the Tamhane-T2 post-hoc contrast tests see Tables B4-B9, Appendix B.
Hypothesis HO4 (presence of clinical tribalism) was partially rejected, as our results confirmed the presence of clinical tribalism. Nurses estimated competencies of other nurses above those of physicians in performing CPR (t(102) = 8.21, p < 0.001; Dz = 0.64), corrective interventions (t(102) = 2.99; p < 0.01, Dz = 0.30), and feedback reception (t(102) = 15.83; p < 0.001; Dz = 1.56, see Table A7, Appendix A. This was also the case for comparison with EMS providers concerning performing CPR (t(101) = 5.09; p < 0.01; Dz = 0.50,), corrective interventions (t(101) = 5.69, p < 0.001, Dz = 0.57), and feedback reception (t(101) = 12.99, p < 0.001; Dz = 1.29 see Table A13, Appendix A). The nurses’ clinical tribalism did not correlate with the four aspects of learning motivation, which partially accepts the null hypothesis HO4 (see Tables A8–12, A14–A18, Appendix A).
The physicians showed similar results as they overplaced their colleagues above nurses in performing CPR (t(95) = 9.55; p < 0.001; Dz = 0.98), corrective interventions (t(95) = 10.85, p < 0.001; Dz = 1.11), and feedback reception (t(95) = 10.70; p < 0.001; Dz = 1.09, see Table A19), as well as over EMS providers (t(95) = 3.26–11.05; p < 0.001, Dz = 0.33–1.13, see Table A25) in all the three competencies. Additionally, the physicians showed a moderate but significant correlation of clinical tribalism with the nurses (r = − 0.29; BCa 95% CI [−0,39; −0.07]; p = 0.03) and a weak correlation of clinical tribalism with the EMS providers (r = − 0.23; BCa 95% CI [−0.44; −0.12]; p = 0.04), which resulted in lower extrinsic motivation (see Tables A20-A24 and A26-30, Appendix A).
Similarly, the EMS providers also showed a high estimation of their professional group for all the three competencies versus nurses (t(193) = 17.17–21.32; p < 0.001; Dz = 1.23–1.53, see Table A31) and physicians (t(193) = 16.21–24.05; p < 0.001, Dz = 0.73–1.73, see Table A37). The EMS providers’ clinical tribalism did not correlate with learning motivation (see Tables A32–A36 and A38–A42, Appendix A).
Discussion
To our knowledge, this is the first study to show overconfidence effects, such as overplacement and overestimation in BLS and their relationship to learning motivation.
We were able to show that some professionals (29%) were confident and many (61%) were overconfident. Furthermore, our findings demonstrate that this overplacement is significant, as the effect sizes are regularly above 0.8. A total of 146 participants were competent (“experts” – who justifiably overplaced themselves), whereas others were incompetent, and therefore, overconfident. The overconfident group was divided into highly motivated (181 “recruitables”) and unmotivated learners (70 “unawares”). Our findings are consistent with the findings of our previous work,20 literature on overconfidence in general,9, 11, 12, 14, 15 on clinical tribalism,10 and flawed self-assessment in resuscitation proficiency.29 Unfortunately, the problem of high self-esteem and resistance to educational programs is well-known.9, 15.
Furthermore, we showed that these groups are not limited to the educational status of BLS providers. In all the three clusters, we detected individuals who encountered CPR situations both seldomly and regularly. We found beginners, experienced providers, and even instructors among all the three groups, especially among the “unawares.” Sixty-four instructors failed the core knowledge tests. Of these, 15 were grouped as “unaware instructors” (of which seven were certified AHA or ERC instructors) and 49 were “recruitable instructors” (28 of the 49 were certified AHA or ERC instructors). These groups of overconfident instructors might pose a risk to patients as they might teach BLS that is inconsistent with international recommendations, or they may teach students false, resource-consuming, time-consuming, or unnecessary contents.24 Consequently, BLS quality management, including reassessments of instructors, may be required to transform “recruitable” and “unaware” instructors into “expert” instructors. This might be easier for the “recruitables” than for “unawares,” and it poses the question of whether categorical assessments of instructors should be promoted, as already suggested/demanded by the AHA. According to the AHA official “Program Administration Manual”30 and discipline-specific instructor manuals (e.g. BLS),31 beneath other requirements, all active AHA instructors must be directly re-evaluated (monitored) every-two years by a training faculty member for their teaching qualities and competencies in conducting AHA courses. This accounts for all training course formats (e.g., BLS, ACLS,32 and pediatric advanced life support33) separately.
Moreover, clinical tribalism was present among the participants, which suggests the need for more interprofessional collaboration, as this is known to decrease the harmful effects of clinical tribalism on patient and teams.10 In other words, interprofessional training34 might lower these harmful effects, whereas multi- or mono-professional training might be a source of error, especially in teams with members of different professions.35
Our study has several limitations. First, because we conducted the study within a small group in Germany, it may have caused a selection bias and limited the study’s generalizability across Germany and other countries. This is important because national regulations for BLS differ in countries. However, overconfidence is known to be a worldwide phenomenon that is innate to human nature,9 thereby providing room for future scientific investigations and being acknowledged by training curriculum developers (e.g., ERC and AHA) for train-the-trainer and resuscitation courses, faculty members, instructors, providers, medical supervisors, patient safety officers, and risk and quality managers.
Second, in this study, we did not examine the entire spectrum of essential competencies in BLS providers on overconfidence and learning motivation. Competencies do not only consist of factual knowledge, which we tested as a surrogate parameter for other learning dimensions.36 Moreover, BLS attitudes, psychomotor skills, problem solving, and real-world behavior could not be measured and should be assessed in future research.
Furthermore, the SIMS score6 is an assessment tool developed for school subjects, such as physical education. We transferred the use of the tool to medical education with sufficient face, content, and construct validity (see Fig. B4, Appendix B) in this study and our previous study.20 However, criterion validity may be added in future projects.
Additionally, a sample size of approximately 400 healthcare workers is sufficient for hypothesis generation.37 However, owing to selection bias, response rate, response burden, and ceiling effects, we might not have detected all possible overconfidence effects. For future investigations, closed and complete surveys in more defined populations may be advisable to clarify concealed effects, as there may be further undetected subgroups. However, this survey was not intended to represent the national situation in Germany regarding learning motivation in BLS. In contrast, we intended to generate further hypotheses for research in the field of learning motivation in BLS, which would be especially useful for instructors. First, we hypothesize that overconfidence effects are also present in other learning dimensions, which should be tested using this instrument. The second hypothesis is that real-time observation of BLS on a manikin or in clinical practice (respecting practical and ethical concerns) could provide further insight into the effects of overconfidence. The third hypothesis is that allocation to one of the clusters changes over time. For example, it seems logical that “recruitables” may be beginner learners who then develop into “experts” or “unawares.” Furthermore, we do not know the reasons, triggers, timing, process, and motivation for changing between these groups, or whether it is simply a question of time, experience, or disregard.
Conclusions
In this study, we demonstrated the presence of overconfidence effects in BLS competencies and their rather complex link to different learning motivation types, namely confident and motivated “experts,” overconfident and motivated “recruitables,” and overconfident and unmotivated “unawares.” All the three groups consisted of healthcare workers from different professions and educational backgrounds. There is a need to concentrate on unmotivated and overconfident instructors, as they can potentially transfer false information to learners. Furthermore, we identified the presence of clinical tribalism among all professions and a negative correlation with extrinsic motivation for physicians. Considering the selection bias and using factual knowledge as a surrogate parameter for competence, our findings may impact future investigations of medical education in BLS.
CRediT authorship contribution statement
Stefan Bushuven: Conceptualization. Joachim Bansbach: Validation, Supervision. Michael Bentele: Validation, Supervision. Milena Trifunovic-Koenig: Validation, Statistics. Stefanie Bentele: Validation, Supervision. Bianka Gerber: Validation. Fritz Hagen: Validation. Christian Friess: Validation. Martin R. Fischer: Validation, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
Assistance with the article.
None declared.
Financial support and sponsorship.
This study was funded by the Messmer-Foundation Radolfzell, Germany, and Training Center for Emergency Medicine (NOTIS) Engen, Germany.
Presentation of preliminary data.
Parts of the results were presented at the third International forum for research on second victims in Cluj-Napoca, Romania (2022), Annual national meeting for “Clean Care is safer Care,” Charité Berlin, Germany (2022), and QuMIK Annual Meeting for Patient Safety, Markgroeningen, Germany (2022).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100369.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.AHA, Basic Life Support Provider Manual, International English eBook edition. Available from: American Heart Association 2020, 2022, American Heart Association. AHA, Basic Life Support Provider Course In: Association AH, editor. 2020.
- 2.Olasveengen T.M., Mancini M.E., Perkins G.D., Avis S., Brooks S., Castrén M., et al. Adult Basic Life Support: International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation. 2020;156:A35–A79. doi: 10.1016/j.resuscitation.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olasveengen T.M., Semeraro F., Ristagno G., Castren M., Handley A., Kuzovlev A., et al. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation. 2021;161:98–114. doi: 10.1016/j.resuscitation.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Deci EL, Ryan RM. Self-determination theory. 2012.
- 5.Howard J.L., Bureau J., Guay F., Chong J.X.Y., Ryan R.M. Student Motivation and Associated Outcomes: A Meta-Analysis From Self-Determination Theory. Perspect Psychol Sci. 2021 doi: 10.1177/1745691620966789. 1745691620966789. [DOI] [PubMed] [Google Scholar]
- 6.Østerlie O., Løhre A., Haugan G. The Situational Motivational Scale (SIMS) in physical education: A validation study among Norwegian adolescents. Cogent Education. 2019;6(1):1603613. [Google Scholar]
- 7.Lin Y.-G., McKeachie W.J., Kim Y.C. College student intrinsic and/or extrinsic motivation and learning. Learn Individ Differ. 2003;13(3):251–258. [Google Scholar]
- 8.Dunning D., Heath C., Suls J.M. Flawed Self-Assessment: Implications for Health, Education, and the Workplace. Psychol Sci Public Interest. 2004;5(3):69–106. doi: 10.1111/j.1529-1006.2004.00018.x. [DOI] [PubMed] [Google Scholar]
- 9.Moore D.A., Healy P.J. The trouble with overconfidence. Psychol Rev. 2008;115(2):502–517. doi: 10.1037/0033-295X.115.2.502. [DOI] [PubMed] [Google Scholar]
- 10.Braithwaite J., Clay-Williams R., Vecellio E., Marks D., Hooper T., Westbrook M., et al. The basis of clinical tribalism, hierarchy and stereotyping: a laboratory-controlled teamwork experiment. BMJ Open. 2016;6(7):e012467. doi: 10.1136/bmjopen-2016-012467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dunlosky J., Rawson K. Overconfidence produces underachievement: Inaccurate self evaluations undermine students’ learning and retention. Learn Instr. 2012;22 [Google Scholar]
- 12.Krause R. The Effect Of Experience On Reducing The Overconfidence Effect In Teachers. Problems of Education in the 21st Century. 2021;79(2):220-8.
- 13.Loughran T.A., Paternoster R., Piquero A.R., Fagan J. “A Good Man Always Knows His Limitations”: The Role of Overconfidence in Criminal Offending. J Res Crime Delinq. 2012;50(3):327–358. [Google Scholar]
- 14.Malmendier U., Tate G. CEO Overconfidence and Corporate Investment. J Financ. 2005;60(6):2661–2700. [Google Scholar]
- 15.Sandroni A. A Survey on Overconfidence. Insurance and Self-Assessment Training Programs. 2018 [Google Scholar]
- 16.Bushuven S., Dettenkofer M., Sippel S., Koenig S., Bushuven S., Schneider-Brachert W. Speaking up behavior and cognitive bias in hand hygiene: Competences of German-speaking medical students. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239444. e0239444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bushuven S., Juenger J., Moeltner A., Dettenkofer M. Overconfidence in infection control proficiency. Am J Infect Control. 2019;47(5):545–550. doi: 10.1016/j.ajic.2018.10.022. [DOI] [PubMed] [Google Scholar]
- 18.Bushuven S., Juenger J., Moeltner A., Dettenkofer M. Overconfidence in infection control proficiency. Am J Infect Control. 2018 doi: 10.1016/j.ajic.2018.10.022. [DOI] [PubMed] [Google Scholar]
- 19.Bushuven S., Weidenbusch M., Mohr S., Delis A., Fischer M.R., Juenger J., et al. Cognitive bias in professional hand hygiene and feedback: A national online-survey on overconfidence in Germany. Infect Control Hosp Epidemiol. 2019;40(8):943–946. doi: 10.1017/ice.2019.156. [DOI] [PubMed] [Google Scholar]
- 20.Trifunovic-Koenig M., Bushuven S., Gerber B., Otto B., Dettenkofer M., Salm F., et al. Correlation between Overconfidence and Learning Motivation in Postgraduate Infection Prevention and Control Training. Int J Environ Res Public Health. 2022;19(9) doi: 10.3390/ijerph19095763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chiozza M.L., Ponzetti C. FMEA: a model for reducing medical errors. Clin Chim Acta. 2009;404(1):75–78. doi: 10.1016/j.cca.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 22.Nolan J.P., Sandroni C., Böttiger B.W., Cariou A., Cronberg T., Friberg H., et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post-resuscitation care. Intensive Care Med. 2021;47(4):369–421. doi: 10.1007/s00134-021-06368-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vadakkencherry Ramaswamy V., Abiramalatha T., Weiner G.M., Trevisanuto D. A comparative evaluation and appraisal of 2020 American Heart Association and 2021 European Resuscitation Council neonatal resuscitation guidelines. Resuscitation. 2021;167:151–159. doi: 10.1016/j.resuscitation.2021.08.039. [DOI] [PubMed] [Google Scholar]
- 24.Wagner P., Lingemann C., Arntz H.R., Breckwoldt J. Official lay basic life support courses in Germany: is delivered content up to date with the guidelines? An observational study. Emerg Med J. 2015;32(7):547–552. doi: 10.1136/emermed-2014-203736. [DOI] [PubMed] [Google Scholar]
- 25.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. doi: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Benassi M., Garofalo S., Ambrosini F., Sant Angelo R.P., Raggini R., De Paoli G., et al. Using Two-Step Cluster Analysis and Latent Class Cluster Analysis to Classify the Cognitive Heterogeneity of Cross-Diagnostic Psychiatric Inpatients. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.01085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kent P., Jensen R.K., Kongsted A. A comparison of three clustering methods for finding subgroups in MRI, SMS or clinical data: SPSS TwoStep Cluster analysis, Latent Gold and SNOB. BMC Med Res Method. 2014;14:113. doi: 10.1186/1471-2288-14-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Formann A.K. Die latent-class-analyse: Einführung in Theorie und Anwendung. Beltz. 1984 [Google Scholar]
- 29.Massoth C., Röder H., Ohlenburg H., Hessler M., Zarbock A., Pöpping D.M., et al. High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Med Educ. 2019;19(1):29. doi: 10.1186/s12909-019-1464-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.AHA. Emergency Cardiovascular Care Program Administration Manual Guidelines for Program Administration and Training. International Version: American Heart Association; 2022 [Available from: https://www.heart.org/-/media/BDD5142CCDEE4490A577770FC7EBE670.ashx.
- 31.AHA Basic Life Support Instructor Manual, International English eBook edition. American Heart Association. 2020 https://ebooks.heart.org/product/ive-bls-instructor-manual-ebook-international-english50160945 Available from: [Google Scholar]
- 32.AHA, Advanced Cardiovascular Life Support Instructor Manual, International English eBook edition. Available from: American Heart Association 2020, 2022, American Heart Association.
- 33.AHA . eBook edition. American Heart Association; 2020. Pediatric Advanced Life Support Instructor Manual, International English. [Google Scholar]
- 34.Gilbert J.H., Yan J., Hoffman S.J. A WHO report: framework for action on interprofessional education and collaborative practice. J Allied Health. 2010;39(Suppl 1):196–197. [PubMed] [Google Scholar]
- 35.Lillebo B., Faxvaag A. Continuous interprofessional coordination in perioperative work: an exploratory study. J Interprof Care. 2015;29:125–130. doi: 10.3109/13561820.2014.950724. [DOI] [PubMed] [Google Scholar]
- 36.Miller G.E. The assessment of clinical skills/competence/performance. Acad Med. 1990;65:S63–S67. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 37.Anthoine E., Moret L., Regnault A., Sébille V., Hardouin J.B. Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. Health Qual Life Outcomes. 2014;12:176. doi: 10.1186/s12955-014-0176-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.