Abstract
The aim of this systematic review is to analyze the properties of the different types of orthodontic retainers, identify their differences and define which type of device is most effective and less harmful to periodontal health.
Methods
A literature search was carried out by a reviewer by consulting PubMed, Lilacs, Embase, Medline full text, Scopus, Web of Science, Cochrane library, and Science Direct electronic databases for biomedical and health literature as well as the grey literature and setting up the search from December 2010 without any restriction about articles languages.
Results
The results showed that patients who wear retainers for a long period have significant differences in clinical parameters compared to patients without retainers. The type of retainer chosen also significantly influences the overall periodontal health of patients. Fixed retainers, both glass-fibre reinforced and steel wire retainers, proved to be the retainer type with the highest plaque and calculus accumulation values compared to removable retainers. In addition, among fixed retainers, glass-fibre reinforced retainers proved to be those that mostly promote the plaque and calculus accumulation in the application site.
Conclusion
Fixed retainers are the best devices to maintain the alignment of mandibular anterior teeth in the long term. Among these devices, stainless steel lingual retainers, plain or braided, should remain the first choice. Although they are also susceptible to periodontal complications, their effect on periodontal health can be considered statistically insignificant if compared to glass-fibre reinforced retainers which, showing worse periodontal complications, should not be used.
Keywords: Fixed orthodontic appliances, Removable orthodontic appliances, Orthodontic retainers, Periodontal index, Gingivitis
Graphical abstract
1. Introduction
Retention is considered as an important part of orthodontic treatment and is necessary to counteract the orthodontic relapse i.e., the tendency for teeth to return to their pre-treatment position. Retention is also used to limit age-related anterior mandibular crowding.1
After the removal of fixed appliances, teeth present a slight mobility and are unsteady under pressure. Therefore, a full-time retention of at least 3–4 months is mandatory after orthodontic treatment to give the periodontal fibers and periodontal ligament time to reorganize.1,2 Once the first 3–4 months have passed, retainer can only be worn overnight for the next 8 months. After one year, it is possible to discontinue the use of retainer in adult end-of-growth patients although this is not always advisable. In some cases, it is recommended that retention be worn permanently1,3; on the other hand is nowadays demonstrated that patients who wore a retention continuously have better alignment 10 years after the end of orthodontic treatment compared to those who do not wore any kind of retention.4
There are many different types of retainers, mainly divided into two categories, fixed and removable, used by the clinicians to achieve their stability goals.
There is no clear or explicit guideline to help clinicians to use one device over another in each patient.5 Indeed, the decision usually depends on individual clinician preference, patient preference, special clinical needs, economic reasons, and popularity of a device in a specific region of the world.6
In the absence of scientific evidence that would allow a protocol of choice to be drawn up, it could be helpful to evaluate the issue from a different clinical point of view. As the chance of relapse is influenced by several factors such as type of malocclusion, age, level of compliance, quality of treatment outcome, and duration of retention treatment,7 these factors should be considered when deciding which type of retainer is best to use on a given patient.
Specifically, on the prolonged or persistent use of retainers, there is still an important gap in investigation about the consequences of these devices on periodontal health, which should instead represent a very important aspect to evaluate in a long-term view. The prolonged time of retention and the related hindering to perform effective hygiene procedures may indeed pose an increased risk to the periodontium as well as for dental hard tissues. Pending more specific guidelines, it would be then useful to investigate the implications of the long-term use of fixed and removable retainers on the supporting tissues,8, 9, 10 also in view of the expectable decrease of patient cooperation in prolonged retention regimes.
The aim of this systematic review is to analyze the characteristics of different type of orthodontic retainer regards to periodontal health of patients, to determine if there is any difference between the different devices and which type of retainer is more effective and less harmful for periodontal health.
2. Methods
To carry out this research the following criteria have been applied.
-
•
Population. Patients who have undergone orthodontic treatment followed by orthodontic retention;
-
•
Investigated condition. Application of a fixed or removable retention of any kind;
-
•
Comparison condition. None;
-
•
Outcome. Periodontal outcomes;
-
•
Time. Two months post treatment under retention phase.
This framework (PICOT) was used as literature search rationale, as usually requested in systematic reviews.
Search strategy: The literature search was conducted by a reviewer by consulting PubMed, Lilacs, Embase, Medline full text, Scopus, Web of Science, Cochrane library, and Science Direct databases as well as the grey literature databases and setting up the search from December 2010 without any restriction about articles languages.
The search terms entered in the above databases were: “fixed retainer” AND “removable retainers” AND “periodontal outcome” AND “periodontal index” OR “fixed retainer” AND “removable retainers” OR “bonded retainer comparison” OR “periodontal health” AND “orthodontic treatment” OR “periodontal outcome” OR “retainer” AND “gingival index” OR “periodontal index” OR “bleeding on probing” AND “removable retainer” OR “periodontal outcome” OR “vacuum formed retainer" AND “periodontal outcome” OR “gingival index” OR “bleeding on probing”. To avoid inappropriate exclusion, abbreviations of all keywords were used.
The articles found were selected and evaluated for the quality of evidence using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach. The same reviewer screened, assessed, and extracted the quality of the publications.
The protocol of this research was registered with the International Prospective Register of Systematic Reviews (PROSPERO), in accordance with Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) guidelines (PROSPERO CRD42021228305).
Including criteria: The study design has included clinical trials, randomized clinical trials (RCT), prospective studies, and longitudinal studies published on periodontology and orthodontics journals with impact factor at least of 2.00 and up to December 2010.
Only studies with sample of at least 10 patients wearing fixed or removable retainer or both on maxillary and mandibular arches and with at least 2 months of follow-up were included in this review. Articles reporting periodontal outcomes were included.
There was no restriction about the type of retainer used in above articles.
Excluding criteria: Articles published before December 2010, articles published in non-relevant journals, articles were not reporting periodontal outcomes, and articles with a sample of patients less than 10 subjects were excluded.
Articles with less than 2 months follow-up period, as well as articles about subjects not orthodontically treated, retrospective studies, cross sectional studies, and studies not related to the systematic review were not included in the review. Articles unrelated with PICO criteria were also excluded from this work.
Eligibility of the articles identified by each search engine was determined by reading their respective title and abstract. The final selection was completed by the researcher reading the complete articles of those studies that fulfilled the including criteria. Any other article that did not fulfilled the including criteria was rejected.
3. Results
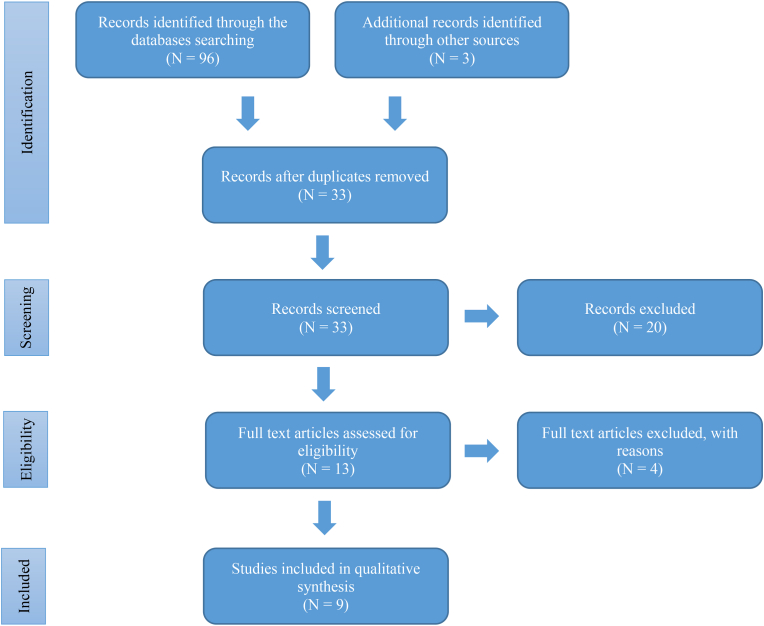
Ninety-nine studies related to orthodontic treatment, retention and periodontal correlations were identified in the electronic databases of the literature and in the grey literature. Sixty-six resulted as duplicated were then removed.
Thirty-three articles were considered potentially relevant to the review and twenty were excluded at initial screening phase because they concerned in some of the exclusion criteria. Thirteen articles were elected for full text analysis and four of them were excluded because they did not meet the including criteria. At the end were selected nine studies which fulfilled the inclusion criteria. The selection process is better represented in the PRISMA flowchart (Fig. 1).
Fig. 1.
PRISMA flow diagram of the literature selection process.
Study characteristics: Among the studies retrieved in the search, seven were RCT,11, 12, 13, 14, 15, 16, 17 one was a prospective study,18 and one was a longitudinal study.19
All the studies had a minimum sample of 15 patients, both male and female, and at least 3 months of follow-up. Four studies had more than 1 year of follow-up.12,14,16,18
Seven studies required patients to wear retainer full-time throughout the study period,11, 12, 13, 14, 15,18,19 one study required patients to wear retainer full-time at the beginning of the trial and then gradually for less and less time,16 and one study requested patients to wear retainer part-time, only overnight.17
Each study used different types of retention, at the same time, for different patients or different types of retention for maxillary and mandibular arches: three studies used fiber reinforced resin as retainer devices,11,12,15 three used exclusively stainless steel retainer,14,18,19 three used vacuum formed retainer,13,16,17 and one study used Hawley retainer.13
Two studies had a control group.12,18
All the characteristics of the studies analyzed in this review are outlined in Table 1.
Table 1.
Characteristics of the studies.
| Authors | Year | Study design | No. of participants | N/group | Interventions | Involved dental arches | Time of wearing | Follow-up | Measured clinical indices |
|---|---|---|---|---|---|---|---|---|---|
| Liu et al.11 | 2010 | RCT | 60 | 30 | 0.75 mm high-strength fiberglass retainer | Mandibular anterior teeth | Full time | 6 months | Periodontal probing dept |
| 30 | 0.9 mm stainless steel three-strand retainer | 12 months | Gingival bleeding index | ||||||
| Tacken et al.12 | 2010 | RCT | 184 | 45 (23 M/22F) | Glass fibre reinforced retainer (500 unidirectional fibres) | Maxillary 2-2 and mandibular anterior teeth | Full time | 6 months | Success rate |
| 48 (23 M/25F) | Glass fibre reinforced retainer (1000 unidirectional glass fibres) | 12 months | Modified gingival index | ||||||
| 91 (44 M/47F) | Six stranded 0.0215″ coaxial wire fixed retainer | 18 months | Bleeding on probing | ||||||
| 90 (45 M/45F) | Untreated control group | 24 months | Plaque index | ||||||
| Xu et al.13 | 2011 | RCT | 45 | 20 (6 M/14F) | 0.0195″ lingual arch wire retainer + Hawley retainer | Maxillary arch and mandibular anterior teeth | Nights only (HR), Full time (FR) | 6 months | Calculus index |
| 25 (10 M/15F) | Vacuum formed retainer | Maxillary and mandibular arches | Full time | 12 months | |||||
| Bazargani et al.14 | 2012 | RCT | 52 | 26 (14 M/12F) | 0.0195″ multistranded orthodontic wire bonded with two-step bonding resin adhesive | Mandibular anterior teeth | Full time | 24 months | Retainer failure Calculus accumulation |
| 26 (12 M/14F) | 0.0195″ multistranded orthodontic wire bonded without liquid resin adhesive | Discoloration around pads | |||||||
| Torkan et al.15 | 2014 | RCT | 30 | 15 (6 M/9F) | Fiber-reinforced resin composit fixed retainer | Maxillary and mandibular anterior teeth | Full time | 6 months | Plaque index Gingival index Calculus index Bleeding on probing |
| 15 (4 M/11F) | Multi-stranded 0.0175″ stainless steel fixed retainer | ||||||||
| Di Venere et al.18 | 2017 | Prospective study | 16 | 8 (2 M/6F)-CG | Triple-stranded 010 steel wire fixed retainer | Mandibular anterior teeth | Full time | 3 months | Plaque index Calculus index Gingival index Periodontal pockets Gingival recession |
| 8 (5 M/3F)-SG | 36 months | ||||||||
| Al-Moghrabi et al.16 | 2018 | RCT | 42 | 21 (7 M/14F) | Vacuum formed retainer | Mandibular arch | Full time for the first 6 months Nights only for the second 6 months Alternate nights 12th to 18th month Intermittent nights-only wear (1–2 nights weekly) from eighteenth month onwards |
4 years | Modified gingival index Plaque index Calculus index Clinical attachment level Bleeding on probing |
| 21 (3 M/18F) | 0.0175''coaxial archwire fixed retainer | Mandibular anterior teeth | Full time | ||||||
| Storey et al.17,20 | 2018 | RCT | 60 | 30 (12 M/18F) | Vacuum formed retainer | Maxillary and mandibular arches | Nights only | 3 months 6 months 12 months |
Plaque index Gingival index Calculus index |
| 30 (15 M/15F) | 0.0195″ 3-stranded twistflex stainless steel wire fixed retainer | Maxillary and mandibular anterior teeth | Full time | ||||||
| Ferreira et al.19 | 2019 | Longitudinal study | 15 | 8 | 0.8 mm orthodontic archwire conventional retainers bonded to canines | Mandibular anterior teeth | Full time for six months | 6 months | Plaque index Gingival index Calculus index Calculus index along the wire |
| 7 | Ortho-FlexTech braided retainer bonded to all anterior teeth | ||||||||
| 8 | Ortho-FlexTech braided retainer bonded to all anterior teeth | Full time for six months | 6 months | ||||||
| 7 | 0.8 mm orthodontic archwire conventional retainers bonded to canines |
RCT, randomized controlled trial; HR, Hawley retainer; FR, fixed retainer; CG control group; SG study group.
Qualitative characteristics: As shown in Table 1, six studies reported gingival index (GI) or the modified gingival index (MGI),12,15,16,18, 19, 20, 21, 22 six studies reported plaque index (PI),12,15,16,18, 19, 20,23 six studies reported calculus index (CI),13,15,16,18, 19, 20,24 and three studies reported the bleeding on probing (BOP).12,15,16,25 As listed in Table 2, one study measured periodontal indices on both full arches,13 the other studies measured periodontal indices on maxillary and mandibular anterior teeth or on the latter only.11,12,14, 15, 16,18, 19, 20
Table 2.
Periodontal outcomes.
| Authors | Year | Interventions | Follow-up | Measured periodontal indices | Examined dental arches | Index calculation method | Results |
|---|---|---|---|---|---|---|---|
| Liu et al.11 | 2010 | 0.75 mm high-strength fiberglass retainer | 6 months 12 months |
Periodontal probing depth Gingival bleeding index |
Six mandibular anterior teeth (proximal, medial and distal site per tooth) | PPD measured were summed and the mean value was calculated GBI scores were summed and the mean score was calculated |
A statistically significant increase in gingival bleeding index (P < 0.05) was found at 6 and 12 months after bonding for both groups. No statistically significant increase in periodontal probing depth was found between the three time points for both groups. No statistically significant difference between the two groups was found at any time point for gingival bleeding index and periodontal probing depth. |
| 0.9 mm stainless steel three-strand retainer | |||||||
| Tacken et al.12 | 2010 | Glass fibre reinforced retainer (500 unidirectional fibres) | 6 months 12 months 18 months 24 months |
Modified gingival index Bleeding on probing Plaque index |
Maxillary 2-2 and mandibular anterior teeth (proximal, medial and distal site per tooth) | MGI was scored as follows: 0 -Absence of inflammation 1 -Part of gingival unit mild inflammation 2 -Complete gingival unit mild inflammation 3 -Moderate inflammation 4 -Severe inflammation BOP was scored as follows: 0 -No bleeding 1 -Point-bleeding 2 -Abundant bleeding PI was scored as follows: 0 -No plaque 1 -Spots of plaque at the cervical margin 2 -Thin continuous band of plaque at the cervical margin 3 -Gingival third of tooth surface covered with plaque 4 -Two-thirds of tooth surface covered with plaque 5 -More than two-thirds of tooth surface covered with plaque |
From the baseline, MGI significantly increased during subsequent follow-ups in all groups. GFR groups showed higher scores (>1.5) in comparison with the multistranded retainer group (∼1). Subjects in the control group showed significantly less gingival inflammation (0.22) in comparison with patients wearing lingual retainers. BOP significantly increased in all groups over time (P ≤ 0.013). Bleeding intensity was systematically higher in the GFR retainer groups in comparison with the multistranded retainer group up to a score above 1 at 24 months. Subjects in the control group showed significantly lower bleeding intensity in comparison with patients wearing lingual retainers (P < 0.001). PI remained virtually unchanged in all groups over the entire study period. There were no significant differences among the retainer groups at any time point. Subjects in the control group showed significantly lower plaque levels in comparison with patients wearing lingual retainers (P ≤ 0.001). |
| Glass fibre reinforced retainer (1000 unidirectional glass fibres) | |||||||
| Six stranded 0.0215″ coaxial wire fixed retainer | |||||||
| Untreated control group | |||||||
| .Xu et al.13 | 2011 | 0.0195″ lingual arch wire retainer + Hawley retainer | 6 months 12 months |
Calculus index | Maxillary arch and mandibular anterior teeth | CI was scored as follows: 0 -Absence of calculus 1 -Calculus covers one third of teeth 2 -Calculus covers two thirds of teeth 3 -Calculus covers over two thirds of teeth |
The calculus in the combined retainer group was significantly more, after 6 months and 1 year, than that in the vacuum formed retainer group (P < 0.05). |
| Vacuum formed retainer | Maxillary and mandibular arches | ||||||
| Bazargani et al.14 | 2012 | 0.0195″ multistranded orthodontic wire bonded with two-step bonding resin adhesive | 24 months | Calculus accumulation | Mandibular anterior teeth | The assessments were done subjectively by the same operator without using any assessment scales; thus, the calculus around the composite pads was rated either present or not | The incidence of calculus accumulation adjacent to the composite pads was significantly higher in the nonresin group (P < 0.05). |
| 0.0195″ multistranded orthodontic wire bonded without liquid resin adhesive | |||||||
| Torkan et al.15 | 2014 | Fiber-reinforced resin composit fixed retainer | 6 months | Plaque index Calculus index Gingival index Bleeding on probing |
Maxillary and mandibular anterior teeth | PI was scored as follows: 0 -Absence of plaque deposits 1 -Plaque disclosed running the probe along the gingival margin 2 -Visible plaque 3 -Abundant plaque CI was scored as follows: 0 -Absence of calculus 1 -Calculus covers one third of teeth 2 -Calculus covers two thirds of teeth 3 -Calculus covers over two thirds of teeth GI was scored as follows: 0 -Absence of inflammation 1 -Mild inflammation 2 -Moderate inflammation 3 -Severe inflammation BOP was scored as follows: 0 -No bleeding 1 -Bleeding on probing |
Significant differences (P < 0.05) in PI were found by Torkan et al. after 6 months from baseline between the spiral wire and the fiber-reinforced groups. Significant differences (P < 0.05) in GI were found in the maxilla by Torkan et al. after 6 months from baseline between the spiral wire and the fiber-reinforced groups when in the mandible only the fiber-reinforced group found significant differences in GI. A statistically significant increase in CI (P < 0,05) was found after 6 months in both study groups in mandibular arch. A statistically significant increase in BOP (P < 0.05) was found after 6 months in fiber-reinforced composite group in both arches. CI and BOP showed no statistically significant difference after 6 months between the two groups. |
| Multi-stranded 0.0175″ stainless steel fixed retainer | |||||||
| Di Venere et al.18 | 2017 | Triple-stranded 010 steel wire fixed retainer | 3 months | Plaque index Gingival index Calculus index Periodontal pockets Gingival recession |
Mandibular anterior teeth | PI was scored as follows: 0 -No plaque 1 -Plaque disclosed running the probe along the gingival margin 2 -Visible plaque 3 -Abundant plaque GI was scored as follows: 0 -Normal gum 1 -Mild inflammation 2 -Moderate inflammation 3 -Severe inflammation CI was scored as follows: 0 -Absence of calculus 1 -Calculus covers one third of teeth 2 -Calculus covers two thirds of teeth 3 -Calculus covers over two thirds of teeth PD was scored as follows: 0 -No pocket (PD ≤ 3 mm) 1 -Presence of pockets (PD > 3 mm) GR was scored recording the millimeters of the recession when the CEJ was visible Mean value for each clinical variable detected was estimated for each patient |
At follow-up, the PI in the Study Group had scores between 0.66 and 3. In the Control Group, were found scores between 0 and 1.66. The GI in the Study Group had its maximum score at 2.83, the minimum score was 0.66. In the Control Group, the maximum score was 2, the minimum score was 0.66. The CI in the Study Group had a scores between 1 and 2. In the Control Group, were found scores between 0 e 1. None of the examined subjects had periodontal sockets or gingival recessions. Statistically significant differences in PI (P > 0.05) and CI (P > 0.1) were thus found in both groups, with higher scores (>2.5) in the Study Group. No statistically significant difference was found for the GI. |
| 36 months | |||||||
| Al-Moghrabi et al.16 | 2018 | Vacuum formed retainer | 4 years | Modified gingival index Calculus index Plaque index Bleeding on probing Clinical attachment level |
Mandibular 3-3 labial and lingual surfaces (6 scores/tooth) | MGI was scored as follows: 0 -Absence of inflammation 1 -Part of gingival unit mild inflammation 2 -Complete gingival unit mild inflammation 3 -Moderate inflammation 4 -Severe inflammation CI was scored as follows: 0 -Absence of calculus 1 -Calculus covers one third of teeth 2 -Calculus covers two thirds of teeth 3 -Calculus covers over two thirds of teeth PI was scored as follows: 0 -No plaque 1 -Spots of plaque at the cervical margin 2 -Thin continuous band of plaque at the cervical margin 3 -Gingival third of tooth surface covered with plaque 4 -two-thirds of tooth surface covered with plaque 5 -More than two-thirds of tooth surface covered with plaque BOP was scored as follows: 0 -No bleeding 1 -Bleeding on probing CAL was measured in millimeters |
At 4-year follow-up, a mean score of 3 in MGI was found in the VFR group, while a mean score of 2.5 was found in the FR group. PI showed a mean score of 3 in the VFR group, while a mean score of 3.5 was found in the FR group. When calculus (CI) was present, 2 was the most common score in both groups. However, about two thirds of tooth surfaces had no calculus in either group. BOP showed a mean score of 1 in both groups. CAL showed a mean score of 1.5 in the VFR group, while a mean score of 2 was found in the FR group. No statistical difference in relation to periodontal parameters was thus found between the fixed and removable retainer groups. |
| 0.0175''coaxial archwire fixed retainer | |||||||
| Storey et al.17,20 | 2018 | Vacuum formed retainer | 3 months 6 months 12 months |
Plaque index Gingival index Calculus index |
Buccal, lingual, mesial, and distal tooth surfaces of all erupted teeth in both arches | PI was scored as follows: 0 -No plaque 1 -Plaque disclosed running the probe along the gingival margin 2 -Visible plaque 3 -Abundant plaque GI was scored as follows: 0 -Normal gum 1 -Mild inflammation 2 -Moderate inflammation 3 -Severe inflammation CI was scored as follows: 0 -Absence of calculus 1 -Calculus covers one third of teeth 2 -Calculus covers two thirds of teeth 3 -Calculus covers over two thirds of teeth |
At 3 months, 6 months, and 12 months, there was a significantly higher PI (P < 0.05) in the intercanine region for BRs compared with VFRs. The median GI after wearing the retainers for 3 months was lower, down to 0.58, than at baseline (debond) for all sites and for both retainer types. The gingival health was worse with BRs after 3 months in the maxillary arch and after 6 months in the mandibular arch. By 6 months, and continuing until 12 months, all regions for both retainer groups had decreased to less than 1.0 suggestive of mild inflammation only. After 3 months, the CI statistically significant increased from baseline in the mandible for both retainer types. Calculus scores were higher for BRs than the VFRs at 3 months though the difference was not statistically significant. Between 3 and 6 months, the median CI reverted back to the baseline measurement of zero at all sites for VFRs; however, the median calculus scores for BRs continued to increase in the mandibular intercanine region. |
| 0.0195″ 3-stranded twistflex stainless steel wire fixed retainer | |||||||
| Ferreira et al.19 | 2019 | 0.8 mm orthodontic archwire conventional retainers bonded to canines | 6 months | Plaque index Calculus index Gingival index |
Mandibular anterior teeth in three areas: two proximal and one lingual | PI was scored as follows: 0 -No plaque 1 -Plaque disclosed running the probe along the gingival margin 2 -Visible plaque 3 -Abundant plaque CI was scored as follows: 0 -Absence of calculus 1 -Calculus covers one third of teeth 2 -Calculus covers two thirds of teeth 3 -Calculus covers over two thirds of teeth GI was scored as follows: 0 -Normal gum 1 -Mild inflammation 2 -Moderate inflammation 3 -Severe inflammation |
There was greater plaque accumulation (PI) when the Ortho-FlexTech retainer was used, and the results showed statistically higher values (P < 0.05) for the proximal and lingual surfaces. The data for CI were statistically higher only for the mesial, distal and lingual surfaces, and the highest indexes (P < 0.05) were found after the use of the Ortho-FlexTech retainer. There was no difference in GI between the retainers for the vestibular surface. Only the proximal and lingual surfaces presented higher scores (P < 0.05) for the conventional retainer. |
| Ortho-FlexTech braided retainer bonded to all anterior teeth | |||||||
| Ortho-FlexTech braided retainer bonded to all anterior teeth | 6 months | ||||||
| 0.8 mm orthodontic archwire conventional retainers bonded to canines |
PPD, periodontal probing depth; GBI, gingival bleeding index; MGI, modified gingival index; BOP, bleeding on probing; PI, plaque index; GFR, glass fibre retainer; CI, calculus index; GI, gingival index; PD, probing depth; GR, gingival recession; CEJ, cement enamel junction; CAL, clinical attachment level; BR, bonded retainer; VFR, vacuum formed retainer.
Periodontal outcomes: Regarding to Gingival Index, Tacken et al. evaluated the MGI.12 According to the authors, it significantly increased from the baseline and during subsequent follow-ups in all groups. More specifically, the glass fibre reinforced retainer groups showed higher scores, more than 1.5, compared to multistranded retainer group who got score nearly 1. With a mean MGI level of 0.22, the subjects in the control group instead, showed significantly less gingival inflammation compared to patients wearing lingual retainers.12
Significant differences (P < 0.05) in GI were found in the maxilla by Torkan et al. after 6 months from baseline between the spiral wire and the fiber-reinforced groups when in the mandible only the fiber-reinforced group found significant differences in GI.15
Di Venere et al. did not find statistically significant difference for the GI in their study samples, though the GI reached a maximum score of 2.83 for the study group as well as of 2 for the control group.18
Again, the MGI was evaluated by Al-Moghrabi et al.16 At 4-year follow-up, a mean score of 3 in MGI was found in the vacuum formed retainer group, while a mean score of 2.5 was found in the fixed retainer group. However, the difference found between the fixed and removable retainer groups was not statistically significant.16
According to Storey et al. the median GI after wearing the retainers for 3 months was lower, down to 0.58, than at baseline for all sites and for both retainer types, though the gingival health became worse in the bonded retainer group after 3 months in the maxillary arch and after 6 months in the mandibular arch.20 Anyway, by 6 months, and continuing until 12 months, all regions for both retainer groups showed a decreasing of GI to less than 1.0 suggestive of mild inflammation only.20
Lastly, Ferreira et al. did not find difference in GI between the retainers for the vestibular surfaces.19 Only the proximal and lingual surfaces presented higher scores (P < 0.05) for the conventional retainer.19
In relation to Plaque Index, Tacken et al. showed that it remained virtually unchanged in all groups over the entire study period.12 There were no significant differences among the retainer groups at any time point. However, subjects in the control group showed significantly lower plaque levels in comparison with patients wearing lingual retainers (P ≤ 0.001).12
Significant differences (P < 0.05) in PI were found by Torkan et al. after 6 months from baseline between the spiral wire and the fiber-reinforced groups.15
At follow-up, statistically significant differences (P > 0.05) were found by Di Venere et al. between fixed retainer and control group, with higher scores, over 2.5, in the study group.18
Al-Moghrabi et al. found a high score, up to 3.5, in PI in the study groups, without statistically significant differences between the fixed and removable retainer groups.16
Significantly higher PI (P < 0.05) in the intercanine region for bonded retainers compared with vacuum formed retainers was found by Storey et al. at different time points.20
Ferreira et al. found a greater PI when the Ortho-FlexTech retainer was used, and the results showed statistically higher values (P < 0.05) for the proximal and lingual surfaces.19
Three studies did not evaluate the PI.11,13,14
Referring to Calculus Index, two studies found no statistically difference between the compared fixed and removable retainer groups,16,20 though the scores found by Storey et al. were higher for bonded retainers than for vacuum formed retainer at 6 months with a P < 0.05 at almost all sites.
Di Venere et al. found statistically significant differences in CI in both groups at follow-up, with higher scores in the study group (up to 1.33) rather than in the control group (up to 0.83).18
The CI data found by Ferreira et al. were statistically higher only for the mesial, distal, and lingual surfaces.19 The highest indexes, up to 2, were found after the use of the Ortho-FlexTech retainer.19
A statistically significant increase in CI (P < 0.05) was found by Torkan et al. in both study groups in mandibular arch after 6 months.15
For Xu et al. the CI in the combined retainer group was significantly higher (P < 0.05) than that in the vacuum formed retainer group after 6 months and 1 year.13
Two studies did not evaluate CI.11,12
Regarding to Bleeding on Probing, Tacken et all. Found that it was significantly increased in all their study groups over time (P ≤ 0.013).12 Bleeding intensity was systematically higher in the glass fibre reinforced retainer groups in comparison with the multistranded retainer group up to a score above 1 at 24 months. Furthermore, the subjects in the control group showed significantly lower bleeding intensity compared to patients wearing lingual retainers of all kinds (P < 0.001).12
A statistically significant increase in BOP (P < 0.05) was found by Torkan et al. after 6 months in fiber-reinforced composite group in both arches though BOP showed no statistically significant difference after 6 months between the two study groups.15
Lastly, Al-Moghrabi et al. found a mean BOP score of 1 in both fixed and removable retainer groups with no statistical difference between the two groups.16
Other periodontal indices were assessed and reported by some of the studies included in this systematic review. Bazargani et al. talk about the incidence of Calculus Accumulation.14 According to their study the calculus accumulation adjacent to the composite pads was significantly higher in the nonresin group (P < 0.05).14 Liu et al. considered the Gingival Bleeding Index.11 They found a statistically significant increase in this index at 6 and 12 months after bonding for both groups though no statistically significant difference was found between the two groups at any time point (P < 0.05).11
Other periodontal indices evaluated in some studies included in this systematic review, such as the Periodontal Probing Depth, the Gingival Recession, the Periodontal Pockets, and the Clinical Attachment Level are represented in Table 2. The data from these indices, however, were not statistically significant.
4. Discussion
This systematic review wanted to investigate the periodontal outcomes derived from long-term wearing of orthodontic retainers, with a view to establish which type of these devices are better for patient periodontal health.
The present study showed that patients who wear retainers for a long period have significant differences in clinical parameters compared to patients without retainers. The type of retainer chosen also significantly influences the overall periodontal health of patients, as well as some clinical differences can be seen between the devices regarding plaque and calculus accumulation. Fixed retainers, both glass-fibre reinforced and steel wire retainers, proved to be the retainer type with the highest plaque accumulation values compared to removable retainers; the same finding being confirmed for calculus accumulation. In addition, among fixed retainers, glass-fibre reinforced retainers proved to be those that mostly promote the plaque and calculus accumulation in the application site.
Plaque and calculus accumulation are considered very important as they directly influence gingival inflammation.26,27 Especially in young adults, gingival inflammation must be taken into serious consideration, as it is a predictor of future periodontal disease.21,28,29 It is therefore crucial in patients who have to wear retainers for a long period to keep plaque and calculus accumulation levels as low as possible.
When the retainers are bonded, they create areas that are more difficult to clean.19 Rody et al. reported an increase in plaque and gingivitis in patients with fixed retainers compared to removable retainers.30 They also highlighted an increase in biochemical markers for periodontal disease in the gingival crevicular fluid in patients with fixed retainers, however, they concluded there was no evidence of severe periodontal disease associated with the wearing of fixed retainers. The same conclusion was reached also from Storey et al.,17 but in both studies the follow-up was short, so the long-term implications are still unknown. In this regard, Artun et al. found similar results from their series of articles investigating the dental and periodontal health effects of various fixed and removable retainers up to 4 years.31,32 Their studies suggest the fixed retainers did not seem to prevent satisfactory oral hygiene along the gingival margin establishing acceptable compatibility of bonded lingual retainers with periodontal health. Unfortunately, the lack of a control group is fundamental. Indeed, the periodontal status of patients provided with bonded lingual retainers was not compared with the status of subjects without retainers in those studies. In a more recent study, however, no bone loss related to fixed retainers in the mandibular anterior area was reported after 10 years.33 This is not in agreement with Pandis et al. who stated that after a period of 10 years, deepening of periodontal pockets and increase of calculus deposits and gingival recession may be expected in patients with bonded lingual retainers.34 It has also to be stated that one would normally expect higher levels of plaque and calculus accumulation in the lower anterior region of patients without any retainer compared to upper anterior region, due to limited access for maintenance of oral hygiene and the proximity of the lower incisal segment to the opening of the submandibular and sublingual salivary glands. As with anything in the medical field, however, risk assessment must be individualized based on the patient's actual periodontal health status, oral hygiene habits and the possible presence of predisposing conditions for periodontal disease.
About the different types of fixed retainers, it has been claimed that fiber-reinforced composite retainers provide a smoother outer surface, while there seems to be more retention areas along the spiral wire retainers which can contribute to the formation of more calculus along the retainer wire.31,34 Torkan et al., however, have found a significant increase in the accumulation of the calculus with the mean scores being worse in the mandibular arch in the fiber-reinforced group.15 The same results were also found by Tacken et al. who also highlighted that patients in the GFR retainer groups showed significantly more gingival inflammation than those in the multistranded retainer groups.12 This might be attributed to the fact that fiber-reinforced composites occupy a wider span on the lingual surface of the teeth compared to spiral wire retainers.
Removable retainers are the retention devices which definitely facilitate the cleaning procedures.35 However, as is well known, these devices will be dependent on patient's cooperation in the long period. Compliance with removable orthodontic components during active treatment is usually limited, with patients routinely failing to reach stipulated levels of wear.36 The expectation that patients might wear removable retainers many years after treatment may be then somewhat optimistic, particularly when much of this period is often not routinely monitored by the clinician.37
All this highlights the importance of periodic check-ups to assess the maintenance of the orthodontic results achieved but also to repeated motivation and reinforcing good oral hygiene instruction at least on a 6 monthly basis, especially in patients wearing a fixed retainer, to avoid deterioration in oral hygiene and consequent periodontal problems. Moreover, Heier et al., suggested that, providing motivation and oral hygiene instruction is reinforced every 6 months, periodontal health should not be compromised by the presence of retainers.38 The same opinion was also held by Artun et al., according to which the presence of a retainer wire, with occasional accumulation of plaque and calculus, does not seem to prevent satisfactory hygiene along the gingival margin.31 In this regard, the patient's own attitude and motivation, possibly acquired under the influence of the orthodontist, is probably the main factor.32
Despite careful initial selection, the studies analyzed in this systematic review were not uniform in design and characteristics. The sample size of some of them was small thus making the effect of individual variation more pronounced with a possible influence on the distribution of certain periodontal variables. Furthermore, the planned follow-up periods of most of these studies was insufficient, potentially risking false-negative results. These reasons did not allow us to fully compare the studies and thus carry out a meta-analysis. However, in our study, significant findings were observed for the main outcome.
Further long-term studies considering all types of retainers, both fixed and removable, with a larger sample size and the involvement of a control group, are needed to assess more significant intergroup differences.
5. Conclusion
Removable retainers are associated with less plaque and calculus accumulation and less gingival inflammation compared to fixed retainer although their limit of effectiveness in preventing relapse is closely linked to the patient's cooperation. Fixed retainers definitely are the approach of choice to maintain the alignment of mandibular anterior teeth in the long term. Among these devices, glass-fibre reinforced retainers have, however, shown worse periodontal complications so their use in clinical practice should be discouraged. Stainless steel lingual retainers, plain or braided, should remain the gold standard for orthodontic retention. Although they are also susceptible to periodontal complications, their effect on periodontal health can be considered statistically insignificant.
Clinicians should therefore carefully consider the patient's characteristics before selecting and applying retainers. It is also important that patients are fully aware of the possible risks, that they are taught accurate oral hygiene especially in the areas surrounding devices, and, lastly, that they undergo regular check-ups at the dentist.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Vincenzo Quinzi, Email: vincenzo.quinzi@univaq.it.
Elisabetta Carli, Email: elisabetta.carli@for.unipi.it.
Alessandra Mummolo, Email: alessandra.mummolo@student.univaq.it.
Federica De Benedictis, Email: federica.debenedictis1@student.univaq.it.
Simone Ettore Salvati, Email: simoneettore.salvati@graduate.univaq.it.
Gianluca Mampieri, Email: gianluca.mampieri@uniroma2.it.
References
- 1.Proffit W.R., Fields H.W.J., Sarver D.M. Mosby Elsevier; 2007. Contemporary Orthodontics. [Google Scholar]
- 2.Sfondrini G., Gandini P. Edizioni Martina; 2008. Ortognatodonzia - Terapia. [Google Scholar]
- 3.Cerny R. Permanent fixed lingual retention. J Clin Orthod JCO. 2001;35(12):728–732. https://pubmed.ncbi.nlm.nih.gov/11822295/ [PubMed] [Google Scholar]
- 4.Egli F., Bovali E., Kiliaridis S., Cornelis M.A. Indirect vs direct bonding of mandibular fixed retainers in orthodontic patients: comparison of retainer failures and posttreatment stability. A 2-year follow-up of a single-center randomized controlled trial. Am J Orthod Dentofacial Orthop. 2017;151(1):15–27. doi: 10.1016/J.AJODO.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 5.Vandevska-Radunovic V., Espeland L., Stenvik A. Retention: type, duration and need for common guidelines. A survey of Norwegian orthodontists. Orthodontics (Chic) 2013;14(1):e110–e117. doi: 10.11607/ORTHO.964. [DOI] [PubMed] [Google Scholar]
- 6.Andriekute A., Vasiliauskas A., Sidlauskas A. A survey of protocols and trends in orthodontic retention. Prog Orthod. 2017;18(1) doi: 10.1186/S40510-017-0185-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaan M., Madléna M. [Retention and relapse. Review of the literature] Fogorv Sz. 2011;104(4):139–146. https://pubmed.ncbi.nlm.nih.gov/22308954/ [PubMed] [Google Scholar]
- 8.Littlewood S.J., Millett D.T., Doubleday B., Bearn D.R., Worthington H.V. Orthodontic retention: a systematic review. J Orthod. 2006;33(3):205–212. doi: 10.1179/146531205225021624. [DOI] [PubMed] [Google Scholar]
- 9.Westerlund A., Daxberg E.L., Liljegren A., et al. Stability and side effects of orthodontic retainers - a systematic review. Dentistry. 2014 doi: 10.4172/2161-1122.1000258. 04(09. [DOI] [Google Scholar]
- 10.Littlewood S.J., Millett D.T., Doubleday B., Bearn D.R., Worthington H.V. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev. 2016;2016(1) doi: 10.1002/14651858.CD002283.PUB4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Y. Application of fiber-reinforced composite as fixed lingual retainer. West China J Stomatol. 2010;28(3):290–293. https://pubmed.ncbi.nlm.nih.gov/20635660/ [PubMed] [Google Scholar]
- 12.Tacken M.P.E., Cosyn J., De Wilde P., Aerts J., Govaerts E., Vannet B Vande. Glass fibre reinforced versus multistranded bonded orthodontic retainers: a 2 year prospective multi-centre study. Eur J Orthod. 2010;32(2):117–123. doi: 10.1093/ejo/cjp100. [DOI] [PubMed] [Google Scholar]
- 13.cen Xu X., mei Li R., Tang G hua. Clinical evaluation of lingual fixed retainer combined with Hawley retainer and vacuum-formed retainer. Shanghai J Stomatol. 2011;20(6):623–626. [PubMed] [Google Scholar]
- 14.Bazargani F., Jacobson S., Lennartsson B. A comparative evaluation of lingual retainer failure bonded with or without liquid resin: a randomized clinical study with 2-year follow-up. Angle Orthod. 2012;82(1):84–87. doi: 10.2319/032811-222.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Torkan S., Oshagh M., Khojastepour L., Shahidi S., Heidari S. Clinical and radiographic comparison of the effects of two types of fixed retainers on periodontium - a randomized clinical trial. Prog Orthod. 2014;15:47. doi: 10.1186/s40510-014-0047-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Moghrabi D., Johal A., O'Rourke N., et al. Effects of fixed vs removable orthodontic retainers on stability and periodontal health: 4-year follow-up of a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2018;154(2):167–174.e1. doi: 10.1016/j.ajodo.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Forde K., Storey M., Littlewood S.J., Scott P., Luther F., Kang J. Bonded versus vacuum-formed retainers: a randomized controlled trial. Part 1: stability, retainer survival, and patient satisfaction outcomes after 12 months. Eur J Orthod. 2018;40(4):387–398. doi: 10.1093/ejo/cjx058. [DOI] [PubMed] [Google Scholar]
- 18.Di Venere D., Pettini P., Nardi G.M., et al. Correlation between parodontal indexes and orthodontic retainers: prospective study in a group of 16 patients. Oral Implant. 2017;10(1):78–86. doi: 10.11138/orl/2017.10.1.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferreira L.A., Sapata D.M., Provenzano M.G.A., Hayacibara R.M., Ramos A.L. Periodontal parameters of two types of 3x3 orthodontic retainer: a longitudinal study. Dental Press J Orthod. 2019;24(3):64–70. doi: 10.1590/2177-6709.24.3.064-070. (oar) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Storey M., Forde K., Littlewood S.J., Scott P., Luther F., Kang J. Bonded versus vacuum-formed retainers: a randomized controlled trial. Part 2: periodontal health outcomes after 12 months. Eur J Orthod. 2018;40(4):399–408. doi: 10.1093/ejo/cjx059. [DOI] [PubMed] [Google Scholar]
- 21.Lang N.P., Schätzle M.A., Löe H. Gingivitis as a risk factor in periodontal disease. J Clin Periodontol. 2009;36(Suppl 1):3–8. doi: 10.1111/J.1600-051X.2009.01415.X. SUPPL. 10. [DOI] [PubMed] [Google Scholar]
- 22.Lobene R.R., Weatherford T., Ross N.M., Lamm R.A., Menaker L. A modified gingival index for use in clinical trials. Clin Prev Dent. 1986;8(1):3–6. https://pubmed.ncbi.nlm.nih.gov/3485495/ [PubMed] [Google Scholar]
- 23.Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(6):610–616. doi: 10.1902/JOP.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 24.Greene J.C., Vermillion J.R. The oral hygiene index: a method for classifying oral hygiene status. J Am Dent Assoc. 1960;61:172–179. https://www.sciencedirect.com/science/article/pii/S0002817760120037 [Google Scholar]
- 25.Ainamo J., Bai I. Parodontalindices for og i praksis. Tandlaegebladet. 1976;80:149–152. [PubMed] [Google Scholar]
- 26.Page R.C. Gingivitis. J Clin Periodontol. 1986;13(5):345–355. doi: 10.1111/J.1600-051X.1986.TB01471.X. [DOI] [PubMed] [Google Scholar]
- 27.Murakami S., Mealey B.L., Mariotti A., Chapple I.L.C. Dental plaque-induced gingival conditions. J Periodontol. 2018;89(Suppl 1):S17–S27. doi: 10.1002/JPER.17-0095. [DOI] [PubMed] [Google Scholar]
- 28.Schätzle M., Löe H., Lang N.P., Bürgin W., Å Ånerud, Boysen H. The clinical course of chronic periodontitis. J Clin Periodontol. 2004;31(12):1122–1127. doi: 10.1111/J.1600-051X.2004.00634.X. [DOI] [PubMed] [Google Scholar]
- 29.Neely A.L., Holford T.R., Löe H., Å Ånerud, Boysen H. The natural history of periodontal disease in man. Risk factors for progression of attachment loss in individuals receiving no oral health care. J Periodontol. 2001;72(8):1006–1015. doi: 10.1902/JOP.2001.72.8.1006. [DOI] [PubMed] [Google Scholar]
- 30.Rody W.J., Elmaraghy S., McNeight A.M., et al. Effects of different orthodontic retention protocols on the periodontal health of mandibular incisors. Orthod Craniofac Res. 2016;19(4):198–208. doi: 10.1111/OCR.12129. [DOI] [PubMed] [Google Scholar]
- 31.Årtun J. Caries and periodontal reactions associated with long-term use of different types of bonded lingual retainers. Am J Orthod. 1984;86(2):112–118. doi: 10.1016/0002-9416(84)90302-6. [DOI] [PubMed] [Google Scholar]
- 32.Årtun J., Spadafora A.T., Shapiro P.A. A 3-year follow-up study of various types of orthodontic canine-to-canine retainers. Eur J Orthod. 1997;19(5):501–509. doi: 10.1093/EJO/19.5.501. [DOI] [PubMed] [Google Scholar]
- 33.Westerlund A., Oikimoui C., Ransjö M., Ekestubbe A., Bresin A., Lund H. Cone-beam computed tomographic evaluation of the long-term effects of orthodontic retainers on marginal bone levels. Am J Orthod Dentofacial Orthop. 2017;151(1):74–81. doi: 10.1016/J.AJODO.2016.06.029. [DOI] [PubMed] [Google Scholar]
- 34.Pandis N., Vlahopoulos K., Madianos P., Eliades T. Long-term periodontal status of patients with mandibular lingual fixed retention. Eur J Orthod. 2007;29(5):471–476. doi: 10.1093/EJO/CJM042. [DOI] [PubMed] [Google Scholar]
- 35.O'Rourke N., Albeedh H., Sharma P., Johal A. Effectiveness of bonded and vacuum-formed retainers: a prospective randomized controlled clinical trial. Am J Orthod Dentofacial Orthop. 2016;150(3):406–415. doi: 10.1016/J.AJODO.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 36.Al-Moghrabi D., Salazar F.C., Pandis N., Fleming P.S. Compliance with removable orthodontic appliances and adjuncts: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2017;152(1):17–32. doi: 10.1016/J.AJODO.2017.03.019. [DOI] [PubMed] [Google Scholar]
- 37.Pratt M.C., Kluemper G.T., Hartsfield J.K., Fardo D., Nash D.A. Evaluation of retention protocols among members of the American Association of Orthodontists in the United States. Am J Orthod Dentofacial Orthop. 2011;140(4):520–526. doi: 10.1016/J.AJODO.2010.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heier E.E., De Smit A.A., Wijgaerts I.A., Adriaens P.A. Periodontal implications of bonded versus removable retainers. Am J Orthod Dentofacial Orthop. 1997;112(6):607–616. doi: 10.1016/S0889-5406(97)70225-7. [DOI] [PubMed] [Google Scholar]