Abstract
Laws regarding cannabis are rapidly changing in the United States as more states legalize nonmedical cannabis for adults age 21 and older. Previous research has examined whether legalization has led to an increase in cannabis use as well as the use of other substances. The current study examined changes in cannabis- and alcohol-specific risk factors following legalization of nonmedical cannabis. We used six years of annual cross-sectional data (2014–2019) from 12,951 young adults age 18 to 25 who resided in Washington state. Risk factors examined include perceiving that use was common among same-age peers, believing use was acceptable, having easy access, and low perceived physical and psychological harm from use. Logistic regression models estimated annual rate of increase in these risk factors. All cannabis-specific risk factors increased among those age 21+ (range of ORs for annual rate of change: 1.07–1.31) while significant increase in cannabis-related risk factors among those under age 21 was limited to perceptions of cannabis use being common (medical use: OR=1.08, 95% CI: 1.03, 1.12; nonmedical use: OR=1.13, 95% CI: 1.08, 1.18) and low perceived physical harm of occasional use (OR=1.08, 95% CI: 1.03, 1.13). Although descriptive norms for past-year use of alcohol among those age 21+ increased (OR = 1.09, 95% CI: 1.02, 1.17), other risk factors for alcohol did not change significantly or, in the case of low perceived physical and psychological harm, decreased among both those under age 21 and those aged 21+ (range of ORs = 0.90–0.94). Given these findings show an increase in cannabis-specific risk factors since legalization was implemented, particularly among those young adults age 21+, preventive interventions correcting risk misperceptions and related risk factors among young adults age 21+ may prove efficacious in reducing use and resultant negative consequences.
INTRODUCTION
Cannabis represents the most commonly used federally proscribed substance in the United States and, according to data from the National Survey on Drug Use and Health, cannabis is most frequently used among young adults relative to other age groups (SAMHSA, 2020). According to Monitoring the Future’s nationally representative data, prevalence of past-year cannabis use among young adults age 19–28 increased from 27.6% in 1999 to 40.1% in 2019 (Schulenberg et al., 2020). Past year use has remained relatively flat among young adults age 18 (37.8% in 1999, 35.7% in 2019) and 19 to 20 (37.9% in 1999, 39.8% in 2019) but has increased considerably among each of the age groups 21–22 (31.5% in 1999, 45.3% in 2019), 23–24 (27.4% in 1999, 40.8% in 2019) and 25–26 (21.8% in 1999, 28.5% in 2019) (Schulenberg et al., 2021).
The relationship between risk factors and health-risking behaviors is well documented and clear. Cannabis- and other substance-specific risk factors include descriptive and injunctive norms, ease of access, and perceptions of harms and risks (e.g., Catalano et al., 2011; 2012; 2018). Social norms surrounding substance use have a long history of association with use both in substance use generally (Borsari & Carey, 2001; Bertholet et al., 2013; Hawkins et al., 1992) and cannabis specifically (e.g., Fleming et al., 2016; Guttmannova et al., 2019b; Neighbors, Geisner & Lee, 2008). Perceived descriptive norms involving the perception that cannabis use is prevalent among friends and same-age peers is associated with increased frequency of use (e.g., Buckner, 2013) as is higher perceived prevalence of peer use (e.g., Koval, Kerr, & Bae, 2019). Injunctive norms favorable to or accepting of cannabis use have been found to be associated with increased cannabis use (e.g., Wu et al., 2015). Easy access to cannabis is also positively associated with cannabis use (e.g., Turel, 2020). Low perceptions of risk and harm are associated with increased behaviors that can cause harm. One ready explanation for this relationship can be found in the theory of planned behavior (Azjen, 1985) which states that as risk perceptions increase so too does the cost of engaging in the behavior such that outcome expectancies decrease and attitudes toward the behavior decrease resulting in a decrease in the behavior. Research has also found that low perceptions of harm and perceptions that cannabis is easy to obtain are associated with more cannabis use (e.g., Fleming et al., 2016). These findings highlight the continued importance of monitoring cannabis-specific risk factors as salient targets of prevention and intervention efforts.
The past decade has ushered in changes to the legal status of cannabis in the United States (Johnson & Guttmannova, 2019). Legalization of nonmedical cannabis began with Washington and Colorado in 2012 and, as of November 29, 2021, eighteen states, two territories and the District of Columbia have legalized the sale and nonmedical use of the drug for adults over the age of 21 (National Conference of State Legislatures [NCSL], 2021). Although legalization represents a dramatic shift in state policy, the effect of legalization on use may be difficult to immediately discern as the impact might manifest itself as a gradual process governed by such factors as regulation and expansion of the retail market rather than being tied solely to the change in legal status (Hammond et al., 2020). Increases in the prevalence of cannabis use and in frequent use have been observed in Washington state since legalization of nonmedical cannabis was enacted (Kilmer et al., 2022). From the perspective of prevention science, it is important to know whether risk perceptions have also changed during this period of implementation of legalized cannabis as those risk factors are targets of intervention efforts and could signal sustained or further elevations in cannabis use (Bachman et al., 1998; Hall & Lynskey, 2016).
Our earlier analyses of data drawn from the same dataset used for the current study found that, in the five years following the opening of nonmedical cannabis stores in Washington state, prevalence of cannabis use (past year, at least monthly, at least weekly, and daily) increased (Kilmer et al., 2022). Closer examination revealed these increases were largely restricted to those age 21+, suggesting that cannabis use among young adults age 18 to 20 may have been less affected by the creation and growth of a retail cannabis market. We also found that prevalence of alcohol use and heavy episodic drinking (HED) decreased between 2014 and 2019 among young adults ages 18−20 and 21−25 (Fleming et al., 2022). Focusing solely on use, these papers did not consider whether cannabis-specific or alcohol-specific risk factors increased or decreased during this same time period.
Recent reviews have examined the impact of cannabis policies, including legalization of nonmedical cannabis, on other substances (e.g., Darnell, 2020; Guttmannova et al., 2016; Smart & Pacula, 2019). These efforts largely focused on whether liberalization of cannabis laws increased or decreased the use of other substances, with alcohol featured prominently among these, framing cannabis as either its complement or substitute. Left unconsidered is whether the easing of restrictions on cannabis affected risk factors specific to other substances, such as perception of harm from alcohol use and the descriptive norms about use of alcohol. Finding an increase in cannabis-specific risk factors without a corresponding increase in alcohol-specific risk factors would suggest legalization is playing an important role and that changes do not reflect a broader change in risk perceptions related to substance use.
The present study built upon our prior papers by examining cannabis- and alcohol-specific risk factors during implementation of legalized nonmedical cannabis. Using annual repeated cross-sectional survey data of young adults from 2014 to 2019, we examined changes in cannabis-specific risk factors before and after widespread implementation of nonmedical cannabis legalization (i.e., opening of the legal cannabis retail market in July 2014) in Washington state. In addition, this study examined risk factors associated with alcohol use during this same time period. Because both alcohol and cannabis are legal for those 21 and older in Washington state, and the perceptions of harm and other risk factors might differ for those below and above the minimum legal use age (Guttmannova et al., 2019), we stratified our analyses by this age cut-off. We hypothesized that implementation of legalization will be associated with an increase in prevalence of risk factors for cannabis use as the change in legal status and commercial sales becomes more widely available and entrenched. We explored whether a similar increase in risk factors for alcohol followed the legalization of cannabis.
METHODS
Sample and Procedures
Data for the present study were collected as part of the Washington Young Adult Health Study (YAHS). The YAHS surveyed young adults age 18 to 25 living in Washington state and included surveys of six cohorts from 2014 to 2019. Participants were recruited across all geographic regions of Washington state through a combination of direct mail and online advertising. See Kilmer et al. (2022) for a more comprehensive description of the YAHS and procedures. While nonmedical or “recreational” cannabis was legalized through voter initiative (I-502) in 2012, the retail sales component of the initiative was first implemented in July 2014 when commercial sale of cannabis commenced with the opening of the first retail stores. The first wave of data was largely collected before retail stores opened with 69.3% of this cohort completing data collection before the first retail shop opened. Although the remaining 30.7% completed the data collection after the first retail shop opened, only 18 retail outlets opened statewide in July 2014 and only 13 additional stores opened in August 2014, meaning most communities did not have legal access to nonmedical cannabis. The analytic sample used in this paper required nonmissing data on at least one of the risk factors and study covariates. The 2014 cohort (n=2,101) completed the baseline survey between April and August of 2014 and additional cohorts were surveyed annually in 2015 (n=1,675), 2016 (n=2,492), 2017 (n=2,338), 2018 (n=2,408), and 2019 (n=1,937). Surveys were online and included questions related to substance use and other health risking behaviors and related risk factors. Surveys took approximately 20 minutes to complete, and participants received a $10 gift card for completing them. All measures and procedures were reviewed and approved by the University of Washington Institutional Review Board.
Demographic information.
The average age of participants at baseline was 21.5 (SD = 2.26) and 67.2% of participants were female. A description of the weighted and unweighted sample can be found in Table 1. Consistent with our analytic strategy to analyze those under age 21 (i.e., age 18–20) separately from those age 21+ (i.e., age 21–25), the sample description in this table is stratified into these two age groups.
Table 1.
Weighted and unweighted distribution of study participant characteristics by age group
| Under 21 |
Age 21+ |
|||
|---|---|---|---|---|
| % or Mean (SD) | % or Mean (SD) | |||
| N = 4,745 | N = 8,206 | |||
| Weighted | Unweighted | Weighted | Unweighted | |
|
| ||||
| Female sex | 47.8 | 66.2 | 49.2 | 67.8 |
| Race/Ethnicity | ||||
| White, non-Hispanic | 64.1 | 60.9 | 67.9 | 66.5 |
| Asian, non-Hispanic | 8.3 | 12.7 | 7.4 | 10.6 |
| Other race, non-Hispanic | 10.3 | 10.8 | 11.1 | 10.5 |
| Hispanic, any race | 17.3 | 15.6 | 13.6 | 12.4 |
| Geographic region | ||||
| 1 (East) | 26.1 | 21.9 | 24.2 | 20.8 |
| 2 (Northwest) | 43.8 | 51.1 | 45.5 | 52.3 |
| 3 (Southwest) | 30.1 | 27.0 | 30.3 | 26.9 |
| Age | 19.1 (0.80) | 19.0 (0.80) | 23.0 (1.41) | 23.0 (1.41) |
| Attending 4-year college | 47.6 | 51.9 | 20.6 | 20.4 |
| Employed full-time | 17.7 | 15.8 | 46.4 | 45.7 |
Measures
Key Outcomes
All outcomes in this paper were coded as risk factors and were transformed into binary variables (i.e., a 1 indicated greater risk).
Descriptive norms.
Participants indicated their perceptions of the frequency of past year use for a typical person their age for three different types of substances: alcohol, medical marijuana, and “recreational” marijuana. The stem item asked, “How often do you think the typical person your age living in Washington state used the following substances (in any form) during the past 12 months?” and this stem was followed by the name of a substance. Responses for each type of substance use included a ten-item ordinal scale that ranged from “Never” to “Every day.” Each item was recoded as a binary variable indicating 0 = no or low (“once a month” or fewer) use or 1 = higher levels of use (“2 to 3 times a month” or greater) to create measures of perceiving that use was common among same-age peers.
Injunctive norms.
Attitudes favorable to and accepting of cannabis use were assessed with two items. The root question asks, “How acceptable or unacceptable is it for someone your age in your community to use cannabis or marijuana in any form...” The first item asked about the acceptability of using cannabis “once or twice” and the second item asked about the acceptability of using cannabis “regularly (nearly every day).” Response options for both items included a four-point ordinal scale that ranged from “Totally acceptable” to “Totally unacceptable.” Each item was recoded as a binary variable 0 = totally/somewhat unacceptable and 1= totally/somewhat acceptable.
Access.
Participants were asked to rate on a five-point ordinal scale how easy it would be to obtain cannabis and alcohol, “How easy or difficult do you think it would be for someone your age, in your community, to obtain from ANY source?” Responses ranged from “Very easy” to “Probably impossible.” Binary variables were created by recoding responses into 0 = “Probably impossible”, “Very difficult” or “Fairly difficult” and 1 = “Fairly easy” or “Very easy” to create measures of having easy access to the given substance.
Perceived risk of harm.
Participants were asked separately to rate risk of physical harm and psychological (including emotional or cognitive) harm on a four-point ordinal scale from “No risk” to “Great risk” for each of the following forms of substance use: daily alcohol use (“one or two drinks nearly every day”); heavy episodic drinking (“5 or more drinks of alcohol once or twice each weekend”); regular marijuana use (“use marijuana or cannabis regularly”); and, occasional marijuana use (“use cannabis or marijuana in any form... just once or twice”). Responses ranged from “No risk” to “Great risk.” Binary variables were created for each item by recoding responses into 0 = moderate/great risk and 1 = no/slight risk.
Covariates
Covariates accounted for in models were biological sex at birth (0=male, 1=female), indicators for a four-category race/ethnicity variable (White [reference], Asian, Hispanic any race and Other race), indicator variables for state region (East [reference], Northwest, Southwest), age, 4-year college status (0= not currently attending, 1= currently attending), and full-time work status (0= not currently employed full time, 1= currently employed full time).
Data Analysis
Changes in risk factors were examined using logistic regression models. The primary predictor of interest in these models was study year, and this was assessed as a linear term with year coded 0 to 5. Sensitivity analyses were also run with study years coded as indicator variables with 2014 coded as the reference (results for these models are presented in two supplemental tables). Prevalence estimates reported in the text below for 2014 and 2019 were based on linear trends models and the average predicted probabilities at these time points across the distribution of other covariates in the sample. Owing to the fact that the change in Washington state’s cannabis law explicitly applies to adults age 21+ and previously reported results that indicated change in cannabis use was largely restricted to young adults age 21+ (see Kilmer et al., 2022), the analyses in this study were stratified by the age 21 cutoff (i.e., models were estimated separately for participants who were under the age of 21 [n=4,747] and for those who were age 21 and older [n=8,206]).
Weighting.
Although efforts were taken to collect data on a representative sample of young adults, the sample distribution differed somewhat from the young adult population in Washington state. Specifically, females were overrepresented in our sample as were Asian Americans and participants from the Northwest region of the state. Therefore, post-stratification weights were developed based on the 2010 US Census such that individuals in sex x region x race strata that were over-represented in this sample relative to the general population were given less weight and individuals in under-represented strata were given greater weight. Post-stratification weighting by sex at birth, geographic region and race/ethnicity was used for all analyses to better ensure that the sample was representative of the young adult population in Washington state.
RESULTS
Table 2 provides estimates of linear changes in risk factors from 2014 to 2019, and the odds ratios represent the yearly change in odds of the given risk factor. Linear trends are also depicted in terms of model-predicted prevalence across years in Figures 1–3. As shown in the Figures, estimates from linear trend models provided a good fit to estimates based on models with an indicator coding of year (see also Supplemental Tables 1 and 2).
Table 2.
Odds ratios for yearly change in risk factors in five years since legalization of nonmedical cannabis was implemented by age group.
| Under 21 |
Age 21+ |
|||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
|
| ||||
| Descriptive Norms: Perception of Common Use | ||||
| Medical Cannabis | 1.08 *** | 1.03, 1.12 | 1.15 *** | 1.12, 1.19 |
| Nonmedical Cannabis | 1.13 *** | 1.08, 1.18 | 1.27 *** | 1.23, 1.32 |
| Alcohol | 1.01 | 0.97, 1.06 | 1.09 * | 1.02, 1.17 |
| Injunctive Norms: Perceived Acceptability of Use | ||||
| Occasional Cannabis | 0.99 | 0.94, 1.04 | 1.15 *** | 1.09, 1.21 |
| Regular Cannabis | 1.03 | 0.99, 1.07 | 1.14 *** | 1.10, 1.18 |
| Access: Easy to Obtain | ||||
| Cannabis | 0.99 | 0.93, 1.05 | 1.31 *** | 1.19, 1.43 |
| Alcohol | 1.01 | 0.94, 1.08 | 0.90 | 0.77, 1.04 |
| Low Perceived Physical Harm | ||||
| Occasional Cannabis | 1.08 *** | 1.03, 1.13 | 1.07 *** | 1.03, 1.11 |
| Regular Cannabis | 1.01 | 0.97, 1.05 | 1.09 *** | 1.06, 1.13 |
| Regular Alcohol | 0.92 *** | 0.88, 0.96 | 0.94 *** | 0.92, 0.97 |
| HED | 0.98 | 0.93, 1.03 | 0.99 | 0.96, 1.03 |
| Low Perceived Psychological Harm | ||||
| Occasional Cannabis | 1.04 | 1.00, 1.08 | 1.08 *** | 1.04, 1.11 |
| Regular Cannabis | 1.04 | 1.00, 1.08 | 1.08 *** | 1.04, 1.11 |
| Regular Alcohol | 0.90 *** | 0.96, 0.94 | 0.93 *** | 0.90, 0.96 |
| HED | 0.96 | 0.91, 1.01 | 0.99 | 0.95, 1.03 |
Notes. Bold indicates p <0.05. Models included student age, gender, geographic region of residence, race/ethnicity, 4-year college status and full-time employment status as covariates. Under 21 includes young adults age 18 to 20, Age 21+ includes young adults age 21 to 25.
p <0.05
p <0.001.
Figure 1.
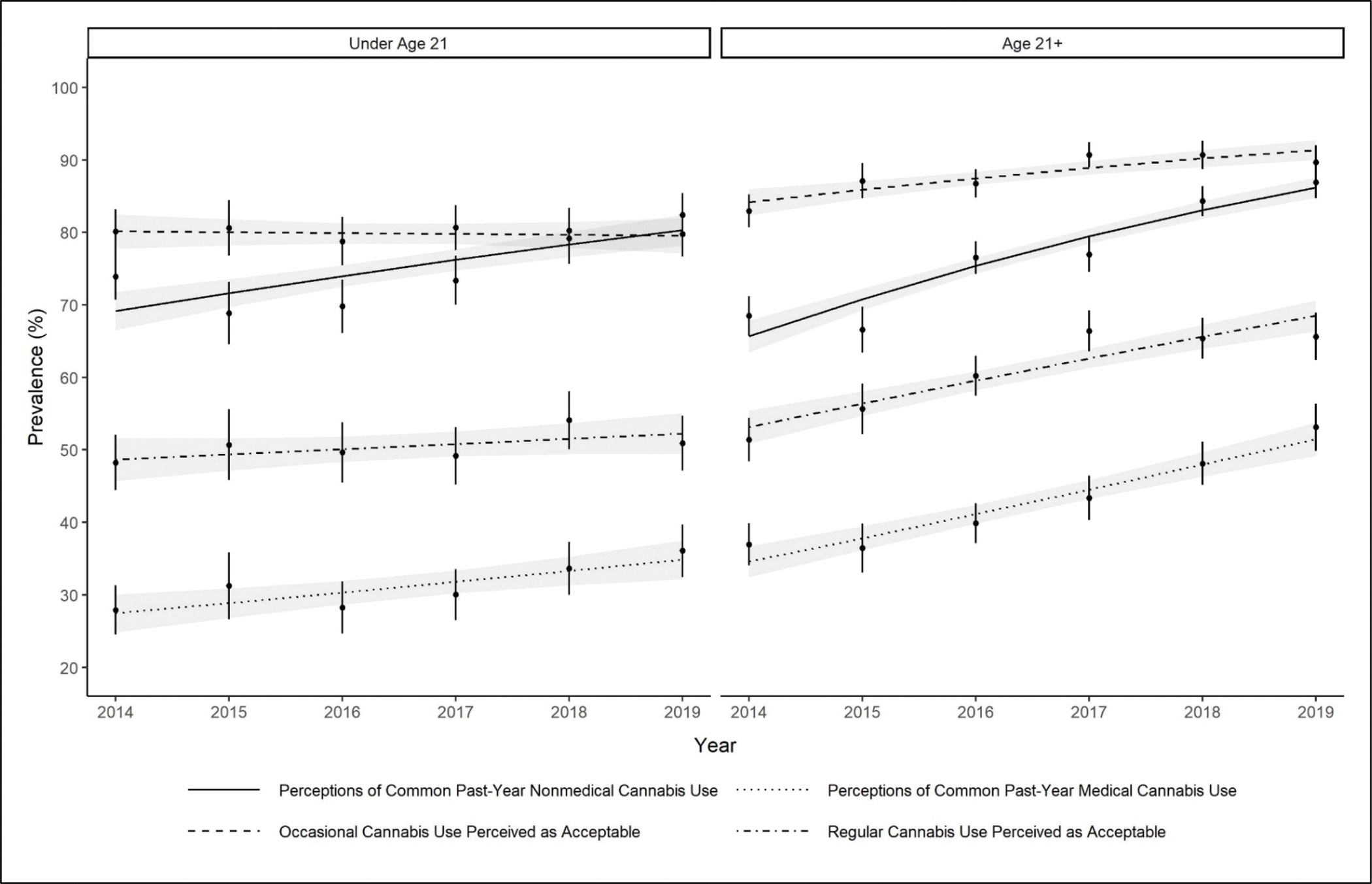
Perceptions that cannabis use is common and acceptable from 2014–2019 in Washington State by age group.
Notes. Observed prevalence for risk factors (points) and model-predicted prevalence estimated from logistic regression models (line) each include confidence bands representing 95% confidence intervals. Among those under age 21, the linear trend for descriptive norms was positive and significant (p <0.001). All linear trends were positive and significant among those age 21+ (p < 0.001).
Figure 3.

Perceptions that cannabis use causes low harms from 2014–2019 in Washington State by age group.
Notes. Observed prevalence for risk factors (points) and model-predicted prevalence estimated from logistic regression models (line) each include confidence bands representing 95% confidence intervals. Among those under age 21, only the linear trend for low physical harm from occasional cannabis use was positive and significant (p <0.001). All linear trends were positive and significant among those age 21+ (p < 0.001).
Descriptive norms
Perceptions of common past year use for both medical and nonmedical cannabis increased significantly over time for both young adults under age 21 and those age 21+ (Table 2 and Figure 1). For example, for those under age 21 the odds ratio for the effect of year on the likelihood of perceiving that a typical person their age used medical cannabis more than once per month during the past year indicates an 8% increase in odds per year (Table 2), while the model-predicted prevalence (Figure 1) indicates this risk factor increased by 26.5% between 2014 and 2019, from 27.5% to 34.8%. The proportion of young adults under age 21 that perceived that monthly nonmedical cannabis was common increased by 16.1% during the study period. Among young adults age 21+, perceptions of common past year use for both medical and nonmedical cannabis increased by 48.8% and 31.2%, respectively. Perceptions of common past year use of alcohol among young adults under age 21 changed little over time, with the effect of year in the linear model indicating a 1% change in odds per year. Among those age 21+, an increase in perceptions of common past year alcohol use was statistically significant, with this measure having a high prevalence in 2014 of 94.0% that increased to 96.1% in 2019.
Injunctive norms.
Perceived acceptability of both occasional and regular cannabis use remained stable across years among young adults under age 21 (see Figure 1). At both margins, change in perceived acceptability was not significant (Table 2). In contrast, for young adults age 21+ this risk factor significantly increased both with respect to occasional use (from 84.2% in 2014 to 91.3% in 2019) and regular use (from 53.1% in 2014 to 68.5% in 2019).
Access
There was no statistically significant change in perceptions that cannabis was easy to obtain among young adults under age 21 (Table 2), with the prevalence changing by less than one percentage point during the study period (Figure 2). Perceptions that it was easy to obtain alcohol in this age group were similarly stable over time. Among individuals age 21+, ease of obtaining cannabis increased significantly from 91.7% in 2014 to 97.6% in 2019. Nearly all participants age 21+ in 2014 (98.5%) reported that they perceived alcohol to be easy to obtain, and this changed little across years.
Figure 2.

Perceptions that cannabis is easy to obtain from 2014–2019 in Washington State by age group.
Notes. Observed prevalence of easy access to cannabis (points) and model-predicted prevalence estimated from logistic regression models (line) each include confidence bands representing 95% confidence intervals. The linear trend for those aged 21+ increased significantly (p <0.001)
Perceived risk of physical harm
Among young adults under age 21, estimates of change in low perceived physical harm from occasional cannabis use were positive and statistically significant with a prevalence of 72.3% in the 2014 increasing to 79.0% in 2019 (see Figure 3). Low risk of harm for regular cannabis use was relatively unchanged from 2014 to 2019, and the linear trend over time was nonsignificant. Among young adults age 21+, the perception of low risk of physical harm for occasional cannabis use increased significantly from 75.7% in 2014 to 81.2% in 2019. Similarly, among young adults age 21+, the linear trend for low risk of physical harm from regular cannabis use was positive and significant, with prevalence increasing from 43.4% to 54.1%.
Low risk of physical harm for regular alcohol use decreased significantly both for young adults under age21 and those age 21+. These trends indicate that a decreasing proportion of young adults were perceiving regular alcohol use to be without serious risk to physical health. For both age groups, the proportion of young adults who perceived that HED posed low risk of physical harm changed little over the study period.
Perceived risk of psychological harm
For adults under age 21, perceptions of low psychological harm from both occasional and regular cannabis use increased slightly during the study period, but these increases were not statistically significant. Increases in these risk factor measures were larger and statistically significant among young adults age 21+, increasing from 66.0% to 73.7% for occasional use and 32.0% to 40.2% for regular use.
For both age groups, the proportion of young adults perceiving low psychological risk from regular alcohol use decreased significantly, from 31.2% to 24.4% for those age under age 21 and 43.7% to 34.1% for those age 21+. With respect to HED, neither age group changed significantly in its perception of low psychological harm.
DISCUSSION
Years of research have shown a robust, positive association between risk factors and actual substance use (e.g., Guttmannova et al., 2019; Koval et al., 2019; Perkins, et al., 1999; Turel, 2020). With legalization of cannabis for nonmedical purposes in Washington state, those over 21 years of age saw dramatic changes in access to substances in a relatively short time. The current study demonstrated that, in the years following the opening of retail cannabis stores in Washington state, perceptions of medical and nonmedical cannabis use increased significantly over time among young adults, both for those under age 21 and those age 21+ with legal access to cannabis retail stores. Our results found that for those over 21, perceptions of more than monthly alcohol use by peers also increased over time. Because descriptive norms, or the perceptions of what others do, are strongly related to people’s own behavior related to substance use (Kilmer, et al., 2006), these perceptions can be associated with initiating use and/or accelerating whatever use is already occurring. It is possible that as visible retail outlet density increased and advertisements (especially for cannabis) entered the market for the first time, this had an impact on perceived norms (Scribner, et al., 2011).
Among young adults ages under age 21, perceived ease of obtaining cannabis did not change over time as it was consistently viewed as easy to obtain. However, it is important to note that part of the justification for legalization was that it would reduce or eliminate the illicit market, reducing availability to those under age 21 (e.g., Darnell et al., 2019) and this purpose was not supported by these data, at least with regard to perceptions of access. Not surprisingly, among those young adults age 21+, for whom legal purchases of cannabis could now be made, perceived ease of obtaining cannabis did significantly increase over time.
While perceptions of alcohol use among young adults age 21 and older increased, ease of access did not, likely because for this age group, ease of access started exceptionally high (98.5% in 2014 reporting alcohol is easy to get) and did not change across cohorts. However, there were changes to how alcohol was sold in Washington that could have contributed to higher normative perceptions for those over 21 years of age during this study’s time frame. Specifically, in 2011, Washington voters approved Initiative 1183, which privatized alcohol sales in Washington that were enacted on June 1, 2012, resulting in a shift from 329 retail establishments selling liquor pre-privatization to 1,406 retail liquor stores within two years (Office of Financial Management, 2015). Scribner and colleagues (2011) suggested that in addition to outlet density, signs, advertising, and direct observation of alcohol use can heighten perceived norms for alcohol, and as Initiative 1183 continues to see amendments and addendums expanding where alcohol can be sold, this could contribute to increasing perceived norms of use by peers. Future research could examine the degree to which exposure to various points of sale, advertisements, and settings in which alcohol is offered relates to potential changes in normative perceptions for this age group.
Perceived psychological harm as well as perceived physical harm associated with the use of cannabis and alcohol were also assessed, and it is clear that substances were viewed differently over time. Among those young adults under age 21, occasional cannabis use was perceived as less physically harmful over time. Conversely, regular alcohol use was seen as more harmful both physically and psychologically over time. Among those over age 21, for whom access to cannabis is legal, there were significant reductions in perceived harm over time for all cannabis-related variables (i.e., physical and psychological harm of occasional and regular cannabis use). Much like with young adults under age 21, perceived harm of regular alcohol use was increasingly seen as more risky both physically and emotionally/psychologically. However, there were no changes in perceived physical or psychological harm associated with heavy episodic drinking. The findings about perceived harm associated with cannabis use are concerning given the body of research suggesting that as perceptions of harms go down, use increases.
Notably, the increase in perception of cannabis as presenting a low risk of harm is not consistent with emerging research on the risks associated with cannabis, particularly high potency cannabis (which dominates the retail market in Washington state). Over 97% of the Washington nonmedical retail market consists of high potency products with THC levels above 10% (Cash, Cunnane, Fan, & Romero-Sandoval, 2020) and young people are particularly vulnerable to negative impacts of cannabis use (Carlini, Firth, & Garrett, 2020), especially with use of high potency cannabis. Prevention messages about substance use often focus on identifying potential harms of alcohol misuse yet there is less messaging around potential harms resulting from cannabis use. The challenge, of course, is that with alcohol, decades of research (starting with Hanson, 1982) shows that providing information tends to increase knowledge without changing behavior; thus, future studies could explore ways to disseminate findings related to harms and risks associated with cannabis use in a way that could translate to behavior change or, at the very least, to increased perceptions of potential harms.
Limitations
One potential limitation of this study is that the time frame studied is limited to the period following legalization and all changes that occurred were during the period of implementation rather than reflecting changes prior to legalization and leading up to implementation. The lack of data from years prior to legalization reduces the certainty that changes are due to implementation of legalization. For example, an alternate possibility is that these results simply reflect a trend that began prior to legalization. It is possible that these trends are due not to legalization but to a broader increase in tolerance toward and acceptance of cannabis use. Given this limitation, caution should be exercised in concluding that the increase in cannabis-specific risk factors is attributable to legalization. Similarly, data were limited solely to a state implementing legalization. The lack of comparison in trends to a state without legalization leaves open the possibility that trends in risk factors may not be limited to states legalizing cannabis. Future research comparing trends in risk perception in states that have not legalized cannabis would be helpful in examining whether these perceptions behaved similarly. Finally, while efforts were made to ensure that young adults were recruited throughout the state, participants were not a random sample (e.g., women were overrepresented in our sample) and this may limit generalizability to the general young adult population. This concern was ameliorated by post-stratification weighting along key demographic variables to improve representativeness of the sample.
Conclusions
Cannabis-specific risk factors have increased, particularly among those young adults age 21 and older, during the implementation of legalization of nonmedical cannabis. A similar increase in alcohol specific risk factors was not observed during the same time. This study suggests that legalization may have contributed to an increase in cannabis-specific risk factors. If young adults are equating “legal” with “safe,” then prevention efforts need to focus on highlighting the harms associated with cannabis use. In reality, research indicates that there is not a “safe” level of cannabis use, rather all cannabis use necessarily incurs some risk and harms (Fischer et al., 2021). In addition, given research has demonstrated risks associated with increasingly potent cannabis use, a gap may be growing between young adult risk perceptions and realities that may be exacerbated by legalization. This presents an opportunity for intervention wherein misperceptions around risks are corrected. This could be accomplished through personalized normative feedback like those that have proven efficacious with alcohol use (e.g., Dotson et al., 2015) or through other means that provide young adults with accurate and up to date information about actual risks and harms associated with cannabis use. Future research examining the pathways between reductions in perceived harm and any potential increases in actual use could be helpful in informing interventions.
Supplementary Material
Funding:
This research was supported by National Institute on Drug Abuse grant R01DA047996–01 awarded to Katarina Guttmannova and T32AA007455. Partial support for this research also came from a Eunice Kennedy Shriver National Institute of Child Health and Human Development research infrastructure grant, P2C HD042828, to the Center for Studies in Demography & Ecology at the University of Washington. Data used in these analyses were from the Washington state Young Adult Health Survey, funded by a contract awarded to Jason Kilmer from Washington’s Division of Behavioral Health and Recovery (DBHR) within the Health Care Authority (HCA). The content of this research is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Footnotes
Conflicts of interest/Competing interests: The authors declare no competing interests.
COMPLIANCE WITH ETHICAL STANDARDS
Ethics approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All measures and procedures were reviewed and approved by the University of Washington Institutional Review Board.
Consent to participate: Informed consent was obtained from all individual participants included in the study.
References
- Bachman JG, Johnston LD, & O’Malley PM (1998). Explaining recent increases in students’ marijuana use: impacts of perceived risks and disapproval, 1976 through 1996. American journal of public health, 88, 887–892. 10.2105/AJPH.88.6.887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachman JG, Johnston LD, O’Malley PM, & Humphrey RH (1988). Explaining the recent decline in marijuana use: Differentiating the effects of perceived risks, disapproval, and general lifestyle factors. Journal of Health and Social Behavior, 29, 92–112. [PubMed] [Google Scholar]
- Bertholet N, Faouzi M, Studer J, Daeppen JB, & Gmel G (2013). Perception of tobacco, cannabis, and alcohol use of others is associated with one’s own use. Addiction science & clinical practice, 8(1), 1–9. doi: 10.1186/1940-0640-8-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, & Carey KB (2001). Peer influences on college drinking: A review of the research. Journal of Substance Abuse, 13(4), 391–424. 10.1016/S0899-3289(01)00098-0 [DOI] [PubMed] [Google Scholar]
- Buckner JD (2013). College cannabis use: The unique roles of social norms, motives, and expectancies. Journal of studies on alcohol and drugs, 74(5), 720–726. 10.15288/jsad.2013.74.720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlini B, Firth C, & Garrett S (Eds.) (2020). Cannabis concentration and health risks: A report for the Washington state prevention research subcommittee (PRSC). Available at: https://adai.uw.edu/wordpress/wp-content/uploads/2020/11/Cannabis-Concentration-and-Health-Risks-2020.pdf [Google Scholar]
- Cash MC, Cunnane K, Fan C, & Romero-Sandoval EA (2020). Mapping cannabis potency in medical and recreational programs in the United States. PLoS ONE 15(3): e0230167. 10.1371/journal.pone.0230167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano RF, Fagan AA, Gavin LE, Greenberg MT, Irwin CE Jr, Ross DA, & Shek DT (2012). Worldwide application of prevention science in adolescent health. Lancet (London, England), 379(9826), 1653–1664. 10.1016/S0140-6736(12)60238-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano RF, Haggerty KP, Hawkins JD, & Elgin J (2011). Prevention of substance use and substance use disorders: The role of risk and protective factors. In Kaminer Y & Winters KC (Eds.), Clinical manual of adolescent substance abuse treatment (pp. 25–63). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Catalano RF, Speaker EC, Skinner ML, Bailey JA, Hong G, Haggerty KP, et al. (2018). Risk and protective factors for adolescent marijuana use. In Winters KC & Sabet KA (Eds.), Contemporary health issues on marijuana (pp. 219–235). New York: Oxford University Press. [Google Scholar]
- Darnell AJ (2020). Review of scientific evidence on effects of medical and non-medical marijuana legalization on public health in the United States. French Monitoring Center for Drugs and Drug Addiction: Paris. [Google Scholar]
- Darnell AJ, Hirsch M, & Wanner P (2019). Suppressing illicit cannabis markets after state marijuana legalization. (Document Number 19– 08–3201). Olympia: Washington State Institute for Public Policy. [Google Scholar]
- DiForti M, Quattrone D, Freeman TP, Tripoli G, et al. (2019). The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): A multicenter case-control study. Lancet Psychiatry, 6 (5), 426–436. 10.1016/S2215-0366(19)30048-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dotson KB, Dunn ME, & Bowers CA (2015). Stand-alone personalized normative feedback for college student drinkers: A meta-analytic review, 2004 to 2014. PloS one, 10(10), e0139518. 10.1371/journal.pone.0139518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer B, Robinson T, Bullen C, Curran V, Jutras-Aswad D, Medina-Mora ME, Pacula RL, Rehm J, Room R, van den Brink W, & Hall W (2021). Lower-risk cannabis use guidelines (LRCUG) for reducing health harms from non-medical cannabis use: A comprehensive evidence and recommendations update. International Journal of Drug Policy, 103381. 10.1016/j.drugpo.2021.103381 [DOI] [PubMed] [Google Scholar]
- Fleming CB, Guttmannova K, Cambron C, Rhew IC, & Oesterle S (2016). Examination of the divergence in trends for adolescent marijuana use and marijuana-specific risk factors in Washington State. Journal of Adolescent Health, 59(3), 269–275. 10.1016/j.jadohealth.2016.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming CB, Ramirez JJ, Rhew IC, Hultgren BA, Hanson KG, Larimer ME, ... & Guttmannova K. (2022). Trends in alcohol, cigarette, e-cigarette, and nonprescribed pain reliever use among young adults in Washington State after legalization of nonmedical cannabis. Journal of Adolescent Health. 10.1016/j.jadohealth.2022.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrys R (2020). Clearing the Smoke on Cannabis: Edible Cannabis Products, Cannabis Extracts and Cannabis Topicals. Canadian: Centre on Substance Use and Addiction. [Google Scholar]
- Guttmannova K, Jones AA, Johnson JK, Oesterle S, Johnson RM, & Martins SS (2019). Using Existing Data to Advance Knowledge About Adolescent and Emerging Adult Marijuana Use in the Context of Changes in Marijuana Policies. Prevention Science, 20(2), 291–299. 10.1007/s11121-019-00991-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmannova K, Lee CM, Kilmer JR, Fleming CB, Rhew IC, Kosterman R, & Larimer ME (2016). Impacts of changing marijuana policies on alcohol use in the United States. Alcoholism: Clinical and Experimental Research, 40, 33–46. 10.1111/acer.12942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmannova K, Skinner ML, Oesterle S, White HR, Catalano RF, & Hawkins JD (2019). The interplay between marijuana-specific risk factors and marijuana use over the course of adolescence. Prevention Science, 20(2), 235–245. doi: 10.1007/s11121-018-0882-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Lynskey M (2016). Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction, 111, 1764–1773. 10.1111/add.13428 [DOI] [PubMed] [Google Scholar]
- Hammond D, Goodman S, Wadsworth E, Rynard V, Boudreau C, & Hall W (2020). Evaluating the impacts of cannabis legalization: The international cannabis policy study. International Journal of Drug Policy, 77, 102698. 10.1016/j.drugpo.2020.102698 [DOI] [PubMed] [Google Scholar]
- Hanson DJ (1982). The effectiveness of alcohol and drug education. Journal of Alcohol and Drug Education, 27(2), 1–13. [Google Scholar]
- Hawkins JD, Catalano RF, & Miller JY (1992). Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin, 112,64–105. 10.1037/0033-2909.112.1.64 [DOI] [PubMed] [Google Scholar]
- Hines LA, Freeman TP, Gage SH, Zammit S, Hickman M, Cannon M, Munafo M, MacLeod J, & Heron J (2020). Association of high-potency cannabis use with mental health and substance use in adolescence. JAMA Psychiatry, 77(10), 1044–1051. doi: 10.1001/jamapsychiatry.2020.1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes A, Lipari RN, Williams M (2015). The CBHSQ Report: State estimates of adolescent marijuana use and perceptions of risk of harm from marijuana use: 2013 and 2014. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. [PubMed] [Google Scholar]
- Kilmer JR, Hunt SB, Lee CM, Neighbors C (2007). Marijuana use, risk perception, and consequences: is perceived risk congruent with reality? Addictive Behaviors, 32, 3026–3033. 10.1016/j.addbeh.2007.07.009 [DOI] [PubMed] [Google Scholar]
- Kilmer JR, Rhew IC, Guttmannova K, Fleming CB, Hultgren B, Gilson MS, Cooper RL, Dilley J, & Larimer ME (2022). Cannabis use among young adults in Washington state after legalization of nonmedical cannabis. American Journal of Public Health, 112 (4), 638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer JR, Walker DD, Lee CM, Palmer RS, Mallett KA, Fabiano P, & Larimer ME (2006). Misperceptions of college student marijuana use: Implications for prevention. Journal of Studies on Alcohol, 67, 277–281. 10.15288/jsa.2006.67.277 [DOI] [PubMed] [Google Scholar]
- Koval AL, Kerr DCR, & Bae H (2019). Perceived prevalence of peer marijuana use: Changes among college students before and after Oregon recreational marijuana legalization. The American Journal of Drug and Alcohol Abuse, 45(4), 392–399. 10.1080/00952990.2019.1599381 [DOI] [PubMed] [Google Scholar]
- Marijuana Business Daily. (2020, April 2). US markets that have allowed marijuana businesses to remain open during coronavirus pandemic stay-at-home orders. https://mjbizdaily.com/states-that-have-allowed-marijuana-businesses-to-remain-open-during-coronavirus-pandemic/.
- National Conference of State Legislatures [NCSL]. (2022). State medical marijuana Laws. Retrieved October 18, 2018. From http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx. Accessed 26 Jan 2022.
- National Governors Association. (2020). Reference chart on state essential business designations. www.nga.org/wp-content/uploads/2020/03/Reference-Chart-on-State-Essential-Business-Designations_3-25.pdf.
- Neighbors C, Geisner IM, & Lee CM (2008). Perceived marijuana norms and social expectancies among entering college student marijuana users. Psychology of addictive behaviors, 22(3), 433. 10.1037/0893-164X.22.3.433 [DOI] [PubMed] [Google Scholar]
- Office of Financial Management. Washington State privatization of liquor: The impact of Initiative 1183. Available at: https://ofm.wa.gov/sites/default/files/public/legacy/fiscal/pdf/liquor_privatization_initiative1183.pdf
- Perkins HW, Meilman PW, Leichliter JS, Cashin JR, & Presley CA (1999). Misperceptions of the norms for the frequency of alcohol and other drug use on college campuses. Journal of American College Health, 47(6), 253–258. 10.1080/07448489909595656 [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA & Patrick ME (2020). Monitoring the Future national survey results on drug use, 1975–2019: Volume II, College students and adults ages 19–60. Ann Arbor: Institute for Social Research, The University of Michigan. Available at http://monitoringthefuture.org/pubs.html#monographs [Google Scholar]
- Schulenberg JE, Patrick ME, Johnston LD, O’Malley PM, Bachman JG, & Miech RA (2021). Monitoring the Future national survey results on drug use, 1975–2020: Volume II, College students and adults ages 19–60. Ann Arbor: Institute for Social Research, The University of Michigan. Available at http://monitoringthefuture.org/pubs.html#monographs [Google Scholar]
- Scribner RA, Theall KP, Mason K, Simonsen N, Schneider SK, Towvim LG, & DeJong W (2011). Alcohol prevention on college campuses: The moderating effect of the alcohol environment on the effectiveness of social norms marketing campaigns. Journal of Studies on Alcohol and Drugs, 72, 232–239. 10.15288/jsad.2011.72.232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart R, & Pacula RL (2019). Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: findings from state policy evaluations. The American journal of drug and alcohol abuse, 45(6), 644–663. 10.1080/00952990.2019.1669626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AL, (2020). Adolescent cannabis use and perceived social norm trends pre- and post-implementation of Washington state’s liberalized recreational cannabis policy: Healthy Youth Survey, 2008–2018. Prevention Science, 21, 772–783. 10.1007/s11121-020-01136-0 [DOI] [PubMed] [Google Scholar]
- Subbaraman MS (2016) Substitution and Complementarity of Alcohol and Cannabis: A Review of the Literature, Substance Use & Misuse, 51, 1399–1414. DOI: 10.3109/10826084.2016.1170145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2020). Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20–07-01–001, NSDUH Series H-55). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/ [Google Scholar]
- Turel O (2020). Perceived ease of access and age attenuate the association between marijuana ad exposure and marijuana use in adolescents. Health Education & Behavior, 47(2), 311–320. 10.1177/1090198119894707 [DOI] [PubMed] [Google Scholar]
- Wu LT, Swartz MS, Brady KT, Hoyle RH, & Workgroup NA (2015). Perceived cannabis use norms and cannabis use among adolescents in the United States. Journal of psychiatric research, 64, 79–87. 10.1016/j.jpsychires.2015.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


