Abstract
Objective
The main treatment for essential hypertension at this stage is pharmacotherapy. Long-term pharmacotherapy is costly with some side effects. Tai Chi, a bright star in traditional Chinese arts, relaxes both mind and body and has been shown to relax blood vessels and lower blood pressure. This study aimed to systematically review the therapeutic effectiveness of the Tai Chi exercise cycle on blood pressure and cardiovascular risk factors of patients with essential hypertension.
Methods
Searching CNKI, VIP, CBM, PubMed, EBSCO, Embase, Cochrane Library, and Web of Science to collect randomized controlled trials about Tai Chi exercise in the treatment of patients with essential hypertension according to the inclusion and exclusion criteria. The search time ranged from the date of database construction to December 2022. The Cochrane risk-of-bias tool was used to evaluate the included trials. The meta-analysis was performed with RevMan5.3 and Stata12.0 software.
Results
According to the meta-analysis, compared with the controls, Tai Chi exercise with a cycle of more than 12 weeks may be better for the reduction of systolic blood pressure (SBP) [MD = −11.72, 95% CI (−15.52, −7.91)] and diastolic blood pressure (DBP) [MD = −4.68, 95% CI (−7.23, −2.12)], as well as increasing the content of nitric oxide (NO) [MD = 0.99, 95% CI (0.69, 1.28)]. The blood lipid metabolism ability may also be improved after more than 12 weeks of Tai Chi exercise, total cholesterol (TC) [SMD = −0.68, 95% CI (−0.89, −0.46), triglyceride (TG) [SMD = −0.84, 95% CI (−1.25, −0.43)], low-density lipoprotein cholesterol (LDL-C) [SMD = −1.58, 95% CI (−2.29, −0.86)]. However, the improvement of high-density lipoprotein cholesterol (HDL-C) [SMD = 0.54, 95% CI (0.28, 0.79)] was better with a less than 12 weeks exercise cycle. A subgroup analysis for exercise frequency and time showed that the exercise frequency should preferably be more than or equal to 5 times per week for patients with hypertension, and for patients with hypertension plus hyperlipidemia, the exercise frequency less than 5 times per week with exercise time less than 60 min each day may be more beneficial.
Conclusion
The meta-analysis indicated that a more than 12 weeks Tai Chi exercise cycle with less than 60 min each time and more than 5 times per week may be more beneficial in blood pressure reduction, NO level increasing and blood lipid metabolism improving in the comparison with the other exercise cycles. For patients with hypertension plus hyperlipidemia, exercise frequency of less than 5 times per week may be better.
Systematic Review Registration
[http://www.crd.york.ac.uk/prospero], identifier [CRD42022352035].
Keywords: Tai Chi, essential hypertension, exercise cycle, blood lipid metabolism, meta-analysis
1. Introduction
Essential hypertension (EH) is a clinical syndrome characterized by elevated systemic arterial pressure (1). EH is not only the disease with the highest incidence, but it is also the major risk factor for heart and cerebrovascular disease. According to statistics, there are 270 million patients with EH in China (2019). The incidence rate of hypertension is expected to climb to 29% (2). At this stage, drug therapy is the main treatment for hypertension. However, the long-term expense of taking prescriptions is so high, and the side effects of the medications are so considerable that individuals with hypertension have poor compliance (3). Aerobics activities such as walking, jogging, and swimming for at least 30 min per day, 5 days per week may effectively reduce blood pressure in patients with hypertension and prehypertension (4–6). In addition to pharmacotherapy and physical exercise, changing unhealthy lifestyles is also an important approach for the prevention of cardiovascular disease (CVD), favoring the control of blood pressure, such as a low salt diet, reduced intake of red meat, sugar, and trans-fat, etc. (7–9). According to the World Health Organization 2020 guidelines on physical activity and sedentary behavior, physical activity can reduce cardiovascular disease mortality, postpone disease progression, improve bodily function, and improve the quality of life for individuals with hypertension (10).
Tai Chi is a prominent traditional Chinese martial art as well as a popular Chinese aerobic exercise. It's also recognized as a traditional type of rehabilitative training. Tai Chi is conducive to maintaining the stability of the vasomotor nerve, improving vascular compliance, reducing blood pressure, enhancing cardiorespiratory ability, and improving the quality of life (11). Compared with drug therapy, Tai Chi has fewer negative effects on patients with hypertension. Tai Chi encourages the production of nitric oxide, improves vasodilation, and lowers blood lipid levels in patients (12). Among numerous traditional Chinese methods, Tai Chi is the most effective one in improving the quality of life in patients with essential hypertension (13, 14). A meta-analysis of Tai Chi for EH patients reported significant reductions in SBP and DBP with an exercise cycle of 12–24 weeks (15). Guan et al. suggested that Tai Chi can reduce SBP and DBP while exercising cycles at both less than 12 weeks and more than or equal to 12 weeks (16). Through a collation of the available literature, we found that previous systematic reviews only made a rough summary of the effects of Tai Chi exercise cycles on blood pressure, and did not analyze blood lipid metabolic ability, as a relevant indicator of cardiovascular risk factors, of patients with hypertension. In addition, the time and frequency of each exercise were not described in detail, making it impossible to effectively formulate a reasonable exercise prescription.
In summary, considering the different influences on blood pressure, blood lipid, and serum NO levels in EH patients caused by the differences in Tai Chi exercise cycle, time, and frequency, we used meta-analysis to integrate the recent research results of Tai Chi exercise intervention in essential hypertension and carried out systematic, objective and quantitative statistical analysis. We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) of Tai Chi Exercise on hypertension in domestic and international databases to see whether the cycle of Tai Chi exercise has different effects on patients with essential hypertension, in order to provide more objective and scientific exercise prescriptions in the future.
2. Materials and methods
2.1. Retrieval strategy
This meta-analysis was planned and implemented according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (17). The protocol was registered on the international prospective register of systematic reviews (http://www.crd.york.ac.uk/PROSPERO) with a registration number CRD42022352035.
A search of CNKI, VIP, CBM, PubMed, EBSCO, Embase, Cochrane Library, and Web of Science for RCTs on Tai Chi exercise on patients with essential hypertension published from the time of the databases established to December 2022 was conducted on December 13, 2022. We also searched to retrieve all potential relevant unpublished reported materials and conference proceedings referred to the topic. Search terms included “tai-ji”, “tai chi”, “chi, tai”, “tai ji quan”, “ji quan, tai”, “quan, tai ji”, “taiji”, “taijiquan”, “t’ai chi”, “tai chi chuan”, “hypertension”, “blood pressure, high”, “high blood pressure”, “hypertension, essential”, “essential hypertension”, “primary hypertension”, “human essential hypertension”, “idiopathic hypertension”. The full search strategies of each database were presented in Supplementary Material S1.
2.2. Literature inclusion, exclusion criteria, and outcome indicator
Inclusion criteria: (1) The study design was a randomized controlled trial (RCT). (2) The research objects were patients with essential hypertension (unlimited sex, age, race, and nationality) according to the diagnostic criteria such as 1999/2005/2010/2016 Chinese guidelines for the management of hypertension, WHO-ISH (i.e., SBP ≥140 mmHg and/or DBP ≥90 mmHg) (18–23). Patients with secondary hypertension and other severe cardio-cerebrovascular disease were required to be excluded. (3) The main intervention methods were Tai Chi exercise or other intervention methods combined with Tai Chi exercise. The intervention methods of the controls included pharmacotherapy, usual care, other exercise methods, or no treatment. (4) Raw data were complete and could be extracted directly or indirectly for analysis. (5) The publication language of the articles was Chinese or English.
Exclusion criteria: (1) Duplicate published literature; (2) Inability to efficiently extract data and access the literature of original articles; (3) Animal studies or cross-sectional studies; (4) Experiments with nonclinical and nonintervention designs.
Outcome indicators included systolic blood pressure (SBP), diastolic blood pressure (DBP), total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) and serum nitric oxide (NO).
The abnormality of TC, TG, LDL-C, and HDL-C can induce or aggravate hypertension. The abnormality of blood lipids may lead to hypertrophy of smooth muscle cells on the vascular wall and deposition of collagen, thus causing structural changes in the large artery vessels. At the same time, the damage of renal microvessels caused by dyslipidemia is also one of the causes of hypertension.
2.3. Literature screening and information extraction
Step 1: Import retrieved literature to the literature management software Endnote X9 (www.endnote.com). Step 2: Exclude duplicate materials. Step 3: Perform the first round of screening by reading titles and abstracts. Step 4: After downloading full texts, conduct the second round of screening to determine if the inclusion criteria were met.
Two independent reviewers, ZY and YY, conducted the literature screening and data extraction. Then cross-checking was performed. When a possible disagreement occurred, we solved it through discussion or negotiation with a third independent reviewer, JW. In literature screening, we first read the title to exclude irrelevant literature. And then, we further read the abstract and the full text to determine whether to include it. If necessary, we would contact the author of the original research by email or telephone to obtain the unconfirmed information. The extraction data included general information about the included literature (the title, the first author, and the year of publication), general characteristics of the patients (the number of cases in each group, the age, and the duration of the disease), treatment specifics and the follow-up time, key elements of bias risk assessment, and focused outcome indicators.
2.4. Quality assessment
Two independent reviewers, ZY and YY, used the Cochrane Collaboration tool to examine the risk of bias for the included studies (24, 25), and cross-checking was conducted. A literature quality grade was performed according to the Jadad Scale. A score of 1–3 was considered low quality, and a score of 4–7 was considered high quality. The grading was also conducted by two independent reviewers, with the disagreement consulting the opinions of a third independent reviewer, JW.
2.5. Statistical analysis
The statistical analysis was based on RevMan5.4 (the Review Manager software 5.4, The Nordic Cochrane Center, The Cochrane Collaboration). If the results included in the literature were continuous variables and from the same assessment method, use the mean difference (MD) and 95% confidence interval (CI) for statistics. If the results were not from the same assessment method, the standard mean difference (SMD) and 95% confidence interval (CI) were conducted. The p-value and the I2 index were used as indicators to assess the heterogeneity among studies. There was no heterogeneity between studies when p ≥ 0.10, while p < 0.10 indicates that there was heterogeneity between studies. The I2 index represented the degree of heterogeneity between studies. If I2 < 50%, it indicates that there was slight heterogeneity between the studies, and the fixed effect model was used for analysis. If I2 ≥ 50%, there was heterogeneity in the study, and the random effect model was used for analysis (26). The α value was set at 0.05. And Stata 12.0 software was used to conduct the publication bias analysis and sensitivity analysis of Begg's test for the studies with more than 5 included outcome indicators. The threshold for statistical significance was set at p < 0.05.
3. Results
3.1. Study selection
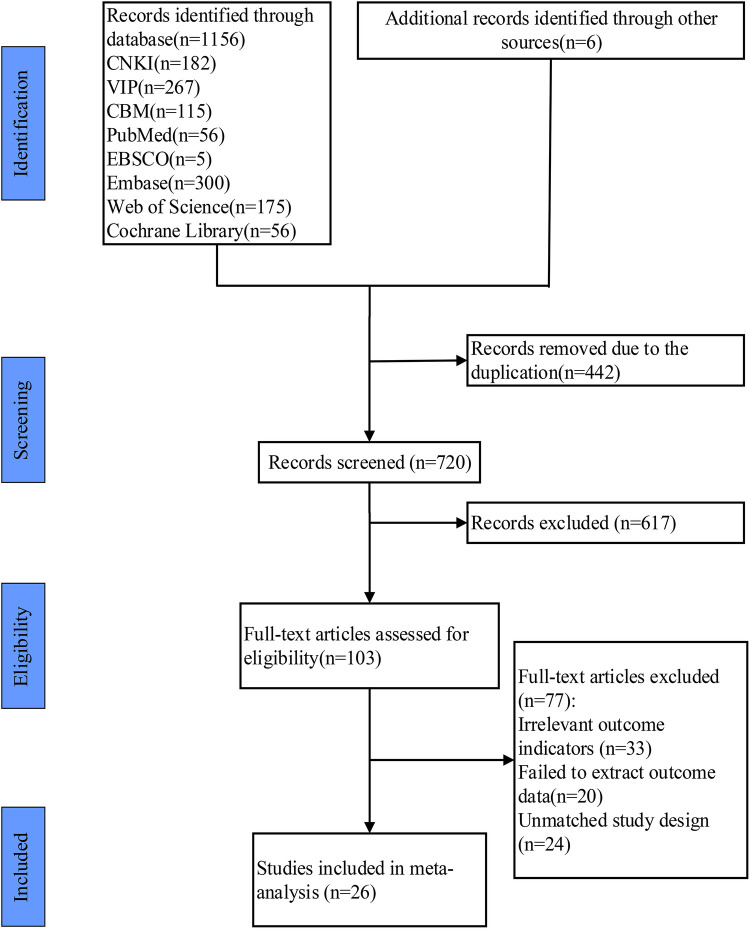
Through the database search, 1,162 articles were preliminarily collected and 6 articles were obtained through a retrospective review of the references. Then we eliminated duplicate publications, 720 articles were left. Determining the research content by reading the titles and abstracts, we screened out 103 articles. After reading the full text, we finally selected 26 articles (23, 27–51) according to the inclusion and exclusion criteria. The literature screening process and results were shown in Figure 1.
Figure 1.
Study selection represented by PRISMA flowchart.
3.2. Assessment of publication bias
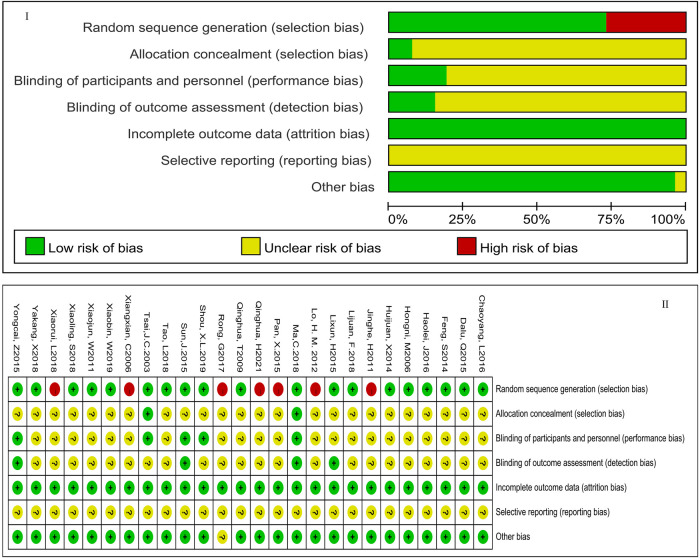
The results of the risk assessment are shown in Figure 2. According to the Jadad scale, 5 articles were judged to be of low quality, and the remaining articles were considered to be of high quality. The detailed information was presented in Supplementary Material S2.
Figure 2.
The risk of publication bias. Figure 1 showed the overall risk of bias in the included studies. Figure 2 showed the specific risk of bias in each study. The green part meant low-risk bias, the red part meant high-risk bias, and the yellow part meant that risk bias was not clear; “+” meant low-risk bias; “−” meant low-risk bias; “?” meant risk bias is not clear.
3.3. Basic characteristics of the article
According to the inclusion and exclusion criteria, a total of 26 articles were finally included, with a total of 2,370 participants. The exercise cycle ranged from 5 weeks to 1 year. In most studies, the intervention method of experimental groups was Tai Chi exercise alone. In a small number of studies, the intervention methods of experimental groups were Tai Chi exercise combined with pharmacotherapy, aerobic exercise, usual care, walking, or the Numan health care system. For the controls, the intervention method in most included studies was no treatment. And in the remaining studies, the method was the way after the removal of Tai Chi exercise. The characteristics and the main results of the studies were presented in Table 1.
Table 1.
The details of research characteristics.
| Author and year of publication | Year | Sample size (E/C) | Diagnostic criteria | Intervention (E) | Intervention (C) | Frequency/week | Exercise time/day | Exercise cycle | Outcome indicators | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| (27) | 35–65 | 39/37 | – | Tai Chi | No exercise intervention | 3/W | 50 min | 12 w | ①②④⑤⑥⑦ | yes |
| (28) | 45–70/52–72 | 51/11 | GMH-1999 | Tai Chi | No exercise intervention | 6/w | 60 min | 8 w | ①②③⑨ | no |
| (29) | 64.3/60.7 | 20/20 | CGMH-2005 | Tai Chi + nifedipine | nifedipine | 7/W | 40 min | 10 w | ①②③ | no |
| (30) | 63.65 ± 8.71/62·79 ± 7·43 | 16/16 | WHO-ISH | Tai Chi | hypotensor | 3–5/W | 30–60 min | 6 m | ①② | no |
| (31) | 51.6 ± 5.3/49.6 ± 7.5 | 33/16 | CGMH-2009 | Tai Chi | No exercise intervention | 6/w | 40–50 min | 20 w | ①②④⑤⑧ | no |
| (32) | 50–70 | 30/30 | – | Tai Chi | No exercise intervention | 5/W | 45 min | 16 w | ①② | no |
| (33) | 58.47 ± 7.46 | 27/31 | – | Tai Chi | Conventional treatment | 3/W | 60 min | 8 w | ①② | no |
| (34) | 68.16 ± 4.43 /69.10 ± 4.28 | 38/42 | CGMH-2010 | Tai Chi | Conventional treatment | 7/W | 120 min | 8 w | ①② | no |
| (35) | 60–70 | 25/25 | CGMH-2005 | Tai Chi | No exercise intervention | 5/W | 60 min | 12 w | ①②③ | no |
| (36) | 52.62–68.74 | 30/30 | CGMH-2005 | Tai Chi | No exercise intervention | 5/W | 60 min | 12 w | ①② | no |
| (37) | 64.10 ± 7.03/64.21 ± 6.12 | 55/55 | – | Tai Chi + Walking | No exercise intervention | 5/W | 45 min | 3 m | ①②④⑤⑥⑦ ⑧ | no |
| (38) | 56.371 ± 3.95 /56.88 ± 3.95 | 24/16 | CGMH-2010 | Tai Chi | No exercise intervention | 6/W | 60 min | 12 w | ①②③④⑤⑥⑦⑧ | no |
| (39) | 45–80 | 136/130 | – | Tai Chi | No exercise intervention | 5/W | 60 min | 12 m | ①②④⑤⑥⑦⑧ | no |
| (40) | 54.71 ± 5.43/55.77 ± 6.24 | 49/49 | CGMH-2010 | Tai Chi + nifedipine | nifedipine | 4–8/W | 40–60 min | 12 w | ①②④⑤⑥⑦ | no |
| (41) | 62.0 ± 2.2 | 60/60 | CGMH-2010 | Tai Chi | captopril | 14/W | 80 min | 2 m | ①② | no |
| (42) | 56.9 ± 5.7 | 27/27 | CGMH-2010 | Tai Chi | Amlodipine | 7/W | 40 min | 6 w | ①②③⑨ | no |
| (43) | 75.38 ± 5.69/74.29 ± 4.58 | 54/54 | – | Tai Chi + NuMan system | Conventional treatment | – | – | 6 m | ①② | no |
| (23) | 60–80 | 41/41 | CGMH-2016 | Tai Chi | Walking exercise | 3/W | 60 min | 12 w | ①②④⑤⑥⑦ | no |
| (44) | 70.24 ± 10.25/ 69.71 ± 10.84 | 55/58 | – | Tai Chi | Conventional treatment | 3–5/W | 60 min | 24 w | ①② | no |
| (45) | 62.4 ± 2.4/63.1 ± 2.1 | 35/35 | CGMH-2010 | Tai Chi + cilazapril | cilazapril | 7/W | 40–60 min | 24 w | ①② | yes |
| (46) | 52.35 ± 3.26/51.35 ± 4.21 | 98/100 | CGMH-2010 | Tai Chi | No exercise intervention | 7–14/W | 45–60 min | 12 w | ①② | no |
| (47) | 51.08 ± 8.77/50.51 ± 8.68 | 61/61 | – | Tai Chi | Conventional treatment | 5–8/W | 50–60 min | 12 w | ①② | no |
| (48) | 60.2 ± 4.6/60.5 ± 4.9 | 42/42 | CGMH-2010 | Tai Chi + aerobic exercise | aerobic exercise | 5/W | 50 min | 12 w | ①②③⑧⑨ | no |
| (49) | 51.5 ± 6.78 51.5 ± 8.26 |
104/104 | CGMH-2010 | Tai Chi | No exercise intervention | 6/W | 40–90 min | 3 m | ①②④⑤⑥⑦ | no |
| (50) | 67.6 ± 4.5/67.4 ± 4.2 | 50/50 | CGMH-2010 | Tai Chi | Conventional treatment | 3/W | 40–60 min | 12 w | ①②④⑤⑥⑦⑧ | yes |
| (51) | 54 ± 6/53 ± 8 | 15/15 | – | Tai Chi | No exercise intervention | 3/W (1–6 W) | 40–60 min | 12 w | ① ② ③ | no |
E, Experimental group; C, Control group; w, week; m, month; y, year; ①, Systolic blood pressure (SBP);②, Diastolic blood pressure (DBP); ③, Nitric oxide (NO); ④, Total cholesterol (TC); ⑤, Triglycerides (TG); ⑥, Low-density lipoprotein cholesterol (LDL-C); ⑦, High-density lipoprotein cholesterol (HDL-C); ⑧, Blood glucose; ⑨, Vascular endothelin “–”, not mentioned.; d, day; m, month; y, year.
3.4. Meta-analysis results
3.4.1. The effect of Tai Chi exercise cycle on blood pressure
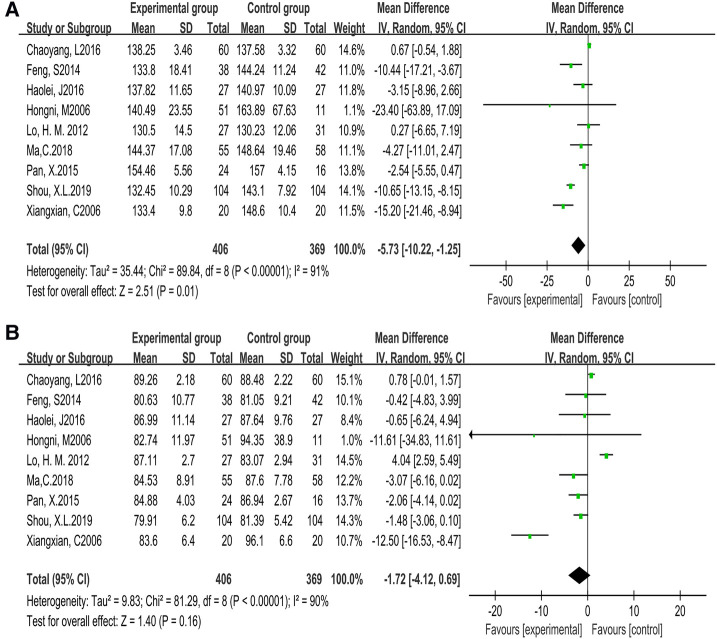
Based on 9 studies (775 participants), we found there was heterogeneity in systolic blood pressure (P < 0.00001, I2 = 91%) [MD = −5.73, 95% CI (−10.22, −1.25), P = 0.01] and diastolic blood pressure (P < 0.00001, I2 = 90%) [MD = −1.72, 95% CI (−4.12, 0.69), P = 0.16] while the cycle was less than 12 weeks, which was analyzed by random effects model. The result was not statistically significant, which meant that compared with the control group, Tai Chi exercise failed to effectively reduce the systolic and diastolic blood pressure levels. The results were displayed in Figure 3.
Figure 3.
Forest plot of meta-analysis on the effect of Tai Chi exercise cycle on blood pressure (cycle <12 weeks). A, systolic blood pressure (SBP); B, diastolic blood pressure (DBP).
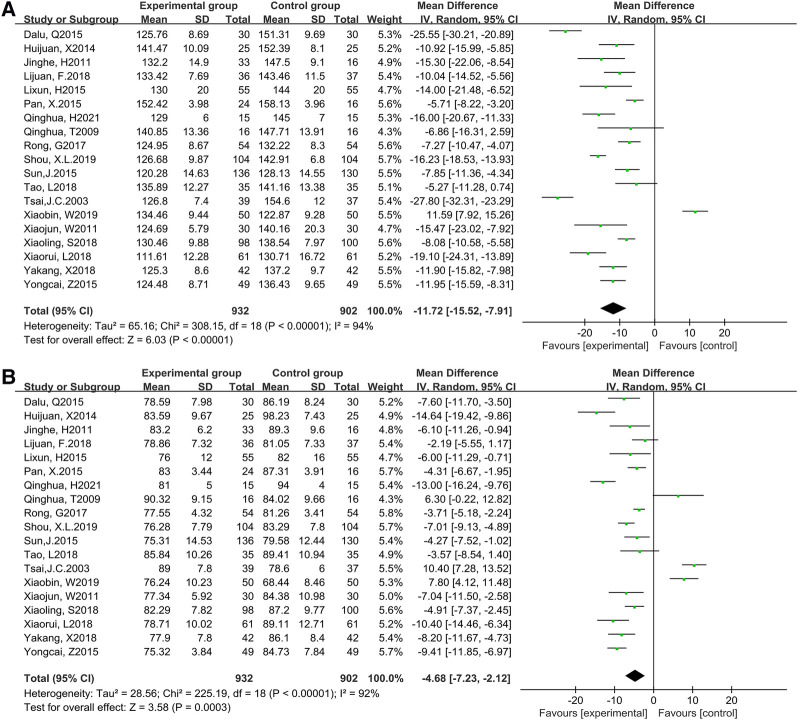
Based on 19 studies (1,825 participants), we found there was heterogeneity in systolic blood pressure (P < 0.00001, I2 = 94%) [MD = −11.72, 95% CI (−15.52, −7.91), P < 0.00001] and diastolic blood pressure (P < 0.00001, I2 = 92%) [MD = −4.68, 95% CI (−7.23, −2.12), P < 0.00001] while the cycle was more than or equal to 12 weeks, which was analyzed by random effects model. The result was statistically significant, which meant that compared with the controls, Tai Chi exercises effectively reduced SBP and DBP. The results were displayed in Figure 4.
Figure 4.
Forest plot of meta-analysis on the effect of Tai Chi exercise cycle on blood pressure (cycle≥12 weeks). A, systolic blood pressure (SBP); B, diastolic blood pressure (DBP).
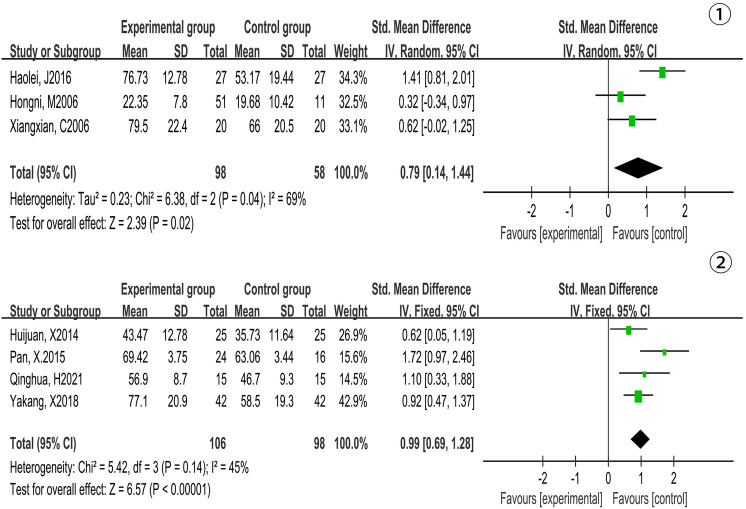
3.4.2. The effect of Tai Chi exercise cycle on NO
Based on 3 studies (156 participants), we found there was heterogeneity in NO (P = 0.04, I2 = 69%) [MD = 0.79, 95% CI (0.14, 1.44), P = 0.02] while the cycle of Tai Chi exercise was less than 12 weeks, which was analyzed by random effects model. The result was not significant, which meant that compared with the control group, Tai Chi exercises failed to effectively increase the level of NO. The results were displayed in Figure 5-①.
Figure 5.
Forest plot of meta-analysis on the effect of Tai Chi exercise cycle on NO. Figure Notes:①, Cycle <12 weeks; ②, Cycle≥12 weeks.
Based on 4 studies (204 participants), we found there was low heterogeneity in NO (P = 0.14, I2 = 45%) [MD = 0.99, 95% CI (0.69, 1.28), P < 0.00001] while the cycle of Tai Chi exercise was more than or equal to 12 weeks, which was analyzed by fixed effects model. The result was significant, which meant that compared with the control group, Tai Chi exercise effectively increased the level of NO. The results were displayed in Figure 5-②.
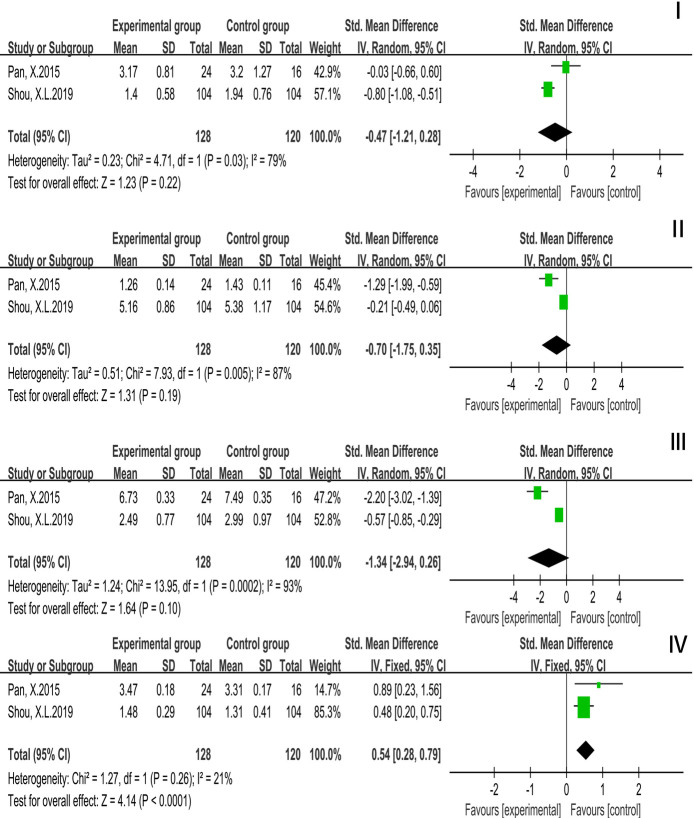
3.4.3. The effect of Tai Chi exercise cycle on blood lipid
Based on 2 studies (248 participants), we used random effects model analysis to draw conclusions: TC (P = 0.03, I2 = 79%) [SMD = −0.47, 95% CI (−1.21, 0.28), P = 0.22], TG (P = 0.005, I2 = 87%) [SMD = −0.70, 95% CI (−1.75, 0.35), P = 0.19], LDL-C (P = 0.0002, I2 = 93%) [SMD = −1.34, 95% CI (−2.94, 0.26), P = 0.10] and HDL-C (P = 0.26, I2 = 21%) [SMD = 0.54, 95% CI (0.28, 0.79), P < 0.0001]. The results were not significant, which meant that compared with the controls, TC, TG, and LDL-C were not improved but HDL-C was improved while Tai Chi exercise cycle was less than 12 weeks. The results were displayed in Figure 6.
Figure 6.
Forest plot of meta-analysis on the effect of Tai Chi exercise cycle on blood lipid related indexes (cycle <12 weeks). I, Total Cholesterol (TC); II, Triglyceride (TG); III, Low Density Lipoprotein (LDL-C); IV, High Density Lipoprotein (HDL-C).
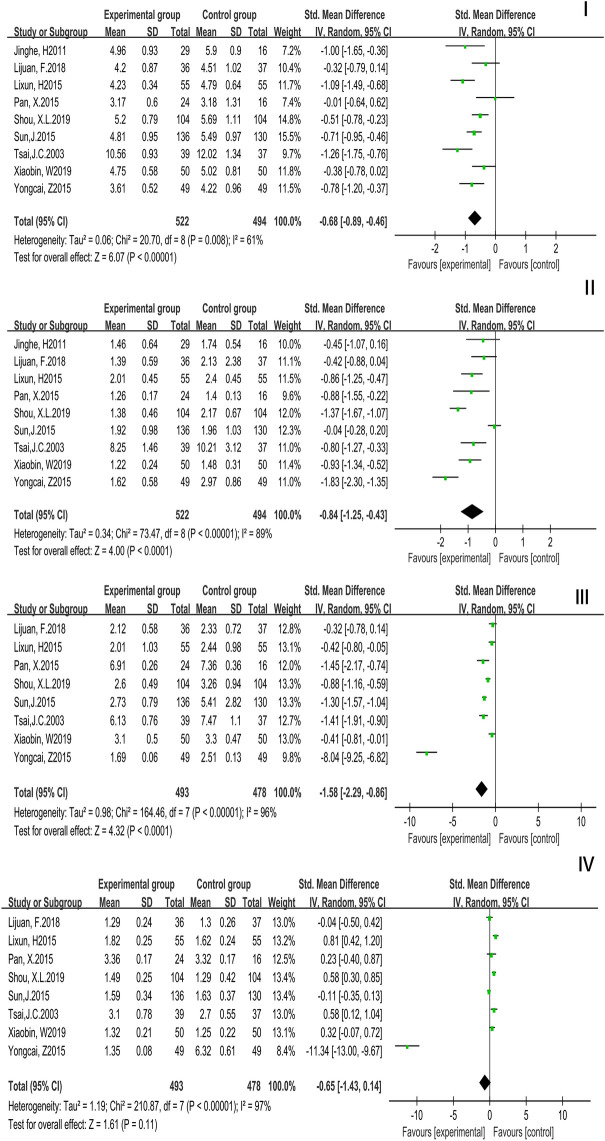
A total of 9 studies with 1,016 patients reported TC and TG while Tai Chi exercise cycle was more than or equal to 12 weeks. A random effects model was used. TC (P = 0.03, I2 = 79%) (SMD = −0.68, 95% CI (−0.89, −0.46), TG (P = 0.005, I2 = 87%) [SMD = −0.84, 95% CI (−1.25, −0.43), P < 0.0001]. The results were statistically significantly different, which showed that compared with the controls, TC and TG were improved. A total of 8 studies with 971 patients reported LDL-C and HDL-C while Tai Chi exercise cycle was more than or equal to 12 weeks. A random effects model was used. LDL-C (P = 0.0002, I2 = 93%) [SMD = −1.58, 95% CI (−2.29, −0.86), P < 0.0001], HDL-C (P < 0.0001, I2 = 97%) [SMD = −0.65, 95% CI (−1.43, 0.14), P = 0.11]. The result of LDL-C was statistically significantly different while the result of HDL-C was not statistically significantly different, which showed that compared with the controls, LDL-C was improved but HDL-C was not. The results were displayed in Figure 7.
Figure 7.
Forest plot of meta-analysis on the effect of Tai Chi exercise cycle on blood lipid related indexes (cycle ≥ 12 weeks). I, Total Cholesterol (TC); II, Triglyceride (TG); III, Low Density Lipoprotein (LDL-C); IV, High Density Lipoprotein (HDL-C).
3.5. Subgroup analysis
Considering that variables such as exercise frequency and duration may alter the blood pressure and lipid metabolism of people with essential hypertension, a subgroup analysis was carried out. The impact of decreasing diastolic blood pressure level is substantial when the exercise frequency is less than 5 times per week, according to the subgroup analysis of the above components. When the exercise frequency is greater than 5 times per week, the effect on blood lipid metabolism is more noticeable. In terms of blood pressure, when exercise time is less than 60 min per day, the effect of decreasing blood pressure and enhancing blood lipid metabolism is more noticeable. Tables 2, 3 show the results.
Table 2.
The subgroup analysis of blood pressure.
| Index | Variable | Group | Sample size | Homogeneity test | Effect size and 95% CI | Two-tailed test | |||
|---|---|---|---|---|---|---|---|---|---|
| C2 | P | I2 | Z | P | |||||
| SBP | Frequency | ≥5/W | 1,515 | 293.56 | 0.00 | 95% | −10.02 (−14.27, −5.77) | 6.94 | 0.04 |
| <5/W | 589 | 220.40 | 0.00 | 97% | −10.03 (−19.54, −0.53) | 6.19 | 0.00 | ||
| Time | ≥60 min/d | 932 | 159.86 | 0.00 | 94% | −8.43 (−13.67, −3.18) | 5.25 | 0.00 | |
| <60 min/d | 1,172 | 238.85 | 0.00 | 95% | −11.20 (−16.54, −5.86) | 2.06 | 0.04 | ||
| DBP | Frequency | ≥5/W | 1,515 | 163.08 | 0.00 | 91% | −5.51 (−8.08, −2.95) | 5.56 | 0.00 |
| <5/W | 589 | 252.38 | 0.00 | 97% | −0.88 (−6.97, 5.21) | 1.90 | 0.78 | ||
| Time | ≥60 min/d | 932 | 102.91 | 0.02 | 91% | −3.97 (−7.40, −0.55) | 4.20 | 0.02 | |
| <60 min/d | 1,172 | 217.83 | 0.01 | 94% | −4.13 (−8.17, −0.10) | 0.93 | 0.04 | ||
Table 3.
The subgroup analysis of lipid metabolism.
| Index | Variable | Group | Sample size | Homogeneity test | Effect size and 95% CI | Two-tailed test | |||
|---|---|---|---|---|---|---|---|---|---|
| C2 | P | I2 | Z | P | |||||
| TC | Frequency | ≥5/W | 248 | 0.24 | 0.62 | 0% | −0.19 (−0.45, 0.07) | 1.47 | 0.14 |
| <5/W | 347 | 16.88 | 0.00 | 82% | −0.63 (−1.06, −0.19) | 2.22 | 0.00 | ||
| Time | ≥60 min/d | 113 | 0.44 | 0.51 | 0% | −0.23 (−0.60, 0.14) | 1.23 | 0.22 | |
| <60 min/d | 482 | 19.72 | 0.00 | 85% | −0.59 (−1.01, −0.17) | 2.76 | 0.00 | ||
| TG | Frequency | ≥5/W | 248 | 13.21 | 0.00 | 92% | −0.35 (−0.71, 0.02) | 1.87 | 0.06 |
| <5/W | 347 | 55.79 | 0.00 | 95% | −1.00 (−1.79, −0.21) | 2.48 | 0.01 | ||
| Time | ≥60 min/d | 113 | 1.98 | 0.16 | 49% | −0.23 (−0.60, 0.14) | 4.45 | 0.00 | |
| <60 min/d | 482 | 56.66 | 0.00 | 95% | −0.86 (−1.37, −0.35) | 3.28 | 0.00 | ||
| LDL-C | Frequency | ≥5/W | 248 | 2.51 | 0.11 | 60% | −0.63 (−0.89, −0.38) | 4.89 | 0.00 |
| <5/W | 347 | 59.88 | 0.00 | 95% | −0.62 (−1.05, −0.19) | 2.82 | 0.00 | ||
| Time | ≥60 min/d | 113 | 8.51 | 0.00 | 88% | −0.50 (−1.03, 0.04) | 1.81 | 0.07 | |
| <60 min/d | 482 | 51.18 | 0.00 | 94% | −0.68 (−1.06, −0.31) | 4.57 | 0.00 | ||
| HDL-C | Frequency | ≥5/W | 248 | 0.02 | 0.89 | 0% | 0.17 (0.09, 0.24) | 4.47 | 0.00 |
| <5/W | 347 | 2,858.42 | 0.00 | 100% | −1.13 (−3.25, 0.99) | 1.04 | 0.30 | ||
| Time | ≥60 min/d | 113 | 4.39 | 0.04 | 77% | 0.08 (−0.09, 0.24) | 0.89 | 0.37 | |
| <60 min/d | 482 | 2,979.81 | 0.00 | 100% | −1.08 (−3.11, −0.94) | 1.05 | 0.30 | ||
3.6. Publication bias
Begg's test was conducted to analyze publication bias for the outcome indicators of SBP and DBP. The results showed that there was both no significant publication bias while Tai Chi exercise cycle was less than 12 weeks or more than or equal to 12 weeks. SBP (t = −1.42, P = 0.173, P > 0.05), DBP (t = −0.62, P = 0.543, P > 0.05); SBP (t = 0.10, P = 0.927, P > 0.05), DBP (t = −0.47, P = 0.652, P > 0.05).The details were presented in Supplementary Figure S1–S4.
4. Discussion
Aerobic exercise may be an effective way to improve blood pressure in hypertensive patients (52). Aerobic exercise for 12 weeks resulted in a significant fall in blood pressure, which stabilized at 36 weeks (53). After 3 months of Tai Chi exercise, TC, TG, and LDL-C decreased and HDL-C increased in the hypertensive patients (40, 50). This meta-analysis indicated that when the Tai Chi exercise cycle was more than or equal to 12 weeks, the improvements in blood pressure and blood lipid metabolism were all significantly better than the situation when the exercise cycle was less than 12 weeks. Thus, for patients with essential hypertension, to achieve better blood pressure decreasing and blood lipid metabolism improving, the Tai Chi exercise cycle may need to be more than or equal to 12 weeks.
Normal persons and hypertension sufferers both experience a brief drop in blood pressure after vigorous activity. Exercise-induced hypotension is the term for this occurrence (54). Exercise-induced hypotension would last 18–24 h. As a result, exercising more than twice a week might have a superior antihypertensive impact (55). However, according to a study (56), there is no link between blood pressure drop and weekly exercise frequency, and blood pressure cannot be efficiently reduced by exercising more than 3 times a week. And aerobic exercise no less than 3 times a week is beneficial for the improvement of lipid metabolism in hypertensive patients (57). This meta-analysis indicated that when the Tai Chi exercise frequency was more than or equal to 5 times per week, the improvements in blood pressure and blood lipid metabolism were more obvious than when the frequency was less than 5 times per week. Thus, exercise frequency is positively correlated with the effects on blood pressure lowering and lipid metabolism improvement. The recommended frequency for patients with essential hypertension of Tai Chi exercise may be more than or equal to 5 times per week. For patients with hypertension combined with hyperlipidemia, efforts should probably also be made to guarantee an exercise frequency greater than or equal to 5 times per week.
The included studies focused on the 30 to 120 min of Tai Chi exercise time, which covered both preparation and completion time. Simply 20 min of effective exercise can have a significant antihypertensive impact (58). However, there are few research on the effect of exercise duration on blood lipids in hypertensive individuals. Studies have shown that there is not a positive correlation between Tai Chi exercise time and blood pressure lowering effect, and that the blood pressure lowering effect of Tai Chi exercise time of 120 min is not superior to that of exercise time of 91–120 min (55). This meta-analysis indicated that when the Tai Chi exercise time was less than 60 min per day, the improvements in blood pressure and blood lipid metabolism were better than when the time was more than or equal to 60 min per day. Therefore, the best exercise time of Tai Chi for patients with essential hypertension may be less than 60 min per day.
Hypertension is often accompanied by metabolic abnormalities such as hyperlipidemia, diabetes, obesity, and insulin resistance, and effective control of blood pressure can significantly reduce the occurrence of cardiovascular events (27, 59–61). Blood lipid metabolic disorders may cause damage to the vascular endothelium, which hypertrophies smooth muscle cells in the vessel wall, thereby causing structural changes in the vessels of large arteries, leading to an increase in blood pressure and the risk of cardiovascular disease (62, 63). Dyslipidemia induced damage to the renal microvasculature, is also one of the causes of hypertension (64). And the increase of blood pressure level with the consequent organism sympathetic excitability negatively affects lipid metabolism, exacerbating dyslipidemia. From this, a vicious circle of elevated blood pressure and dyslipidemia arises (65, 66). Long-term aerobic exercise improves lipoprotein protease activity and the ability of the skeletal muscle to utilize fatty acid supply, promoting lipid metabolism (67). Exercise may regulate the synthesis, transport, and catabolism of lipoprotein by regulating the activity of lecithin-cholesterol acyltransferase (LCAT), lipoprotein lipase (LPL), and hepatic-triglyceride lipase (HTGL). In addition, exercise-induced lipid utilization is regulated by lipolysis of TG within adipose tissue and muscle to deliver fatty acids (FA) to muscle and regulate FA transmembrane transport and mitochondrial metabolism in muscle cells for the purpose of improving lipid metabolism (68–70).
Tai Chi pays attention to three key elements, consisting of soul, power, and idea, and emphasizes on breath transmission and the use of thoughts (71). Tai Chi belongs to the group of low to moderate intensity aerobic exercise with low requirements for basic physical fitness and muscle strength, and is considered a type of physical exercise that is highly beneficial to health (72). When patients with essential hypertension perform Tai Chi, their muscles are relaxed, and nervous system function is modulated, thereby reflexively causing vasodilation for the purpose of reducing blood pressure (73). Vasodilator and constrictor factors secreted by vascular endothelium regulate the degree of vasodilation. And there is a direct relationship between high and low BP and vasodilation (12). Studies have shown that regular aerobic exercise in sedentary middle-aged and older adults can reduce CVD risk by preventing elastic artery stiffness and endothelial dysfunction through modulation of structural proteins, reduction of oxidative stress and inflammation, and restoration of nitric oxide bioavailability (74, 75).
5. Conclusion
According to Chinese Guidelines for the Prevention and Treatment of Hypertension, Tai Chi exercise is best when performed 3 times per week for 30–120 min per session in patients with essential hypertension. However, this meta-analysis indicated that a more than 12 weeks Tai Chi exercise cycle with less than 60 min each time and more than 5 times per week may be more beneficial in blood pressure reduction, NO level increasing and blood lipid metabolism improving in the comparison with the other exercise cycles. For patients with hypertension plus hyperlipidemia, exercise frequency of less than 5 times per week may be better. In the future, it is suggested that the standardized exercise prescription of Tai Chi should be explored more deeply to provide better evidence-based medical support for the use of Tai Chi in the clinic.
6. Limitation
-
1)
The included studies were mainly published in Chinese. The differences in the studies may have impacts on the results of the meta-analysis.
-
2)
Less follow-up was reported in the included studies. It is suggested that more attention should be paid to the prognostic situation in the future.
-
3)
The implementation of blinding was not explicitly stated in part of the included studies. This may have contributed to a decrease in the level of evidence for the meta-analysis.
-
4)
There were certain flaws in the design and implementation process of partially included studies, which may lead to bias in measurement and implementation.
Funding Statement
This work is supported by the national key R&D project “Research on key technologies for the prevention and control of sports injuries in racing and confrontation winter events” (2019YFF0301704).
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: CNKI(https://www.cnki.net/). Wan Fang Databases (https://www.wanfangdata.com.cn/index.html). PubMed (https://pubmed.ncbi.nlm.nih.gov/). Web Of Science (https://clarivate.com/products/web-of-science/). Science Direct (https://www.sciencedirect.com/). Accession numbers can be found in the Supplementary Material.
Author contributions
YY and JS designed the systematic review and supervised the entire program; JW reviewed all the studies and extracted the information from the eligible trials; YY and JW analyzed the data and prepared the figures and table; YY, JW, and ZY wrote the manuscript; YY, ZY, and JS revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1016629/full#supplementary-material.
References
- 1.Srivastava K, Narang R, Bhatia J, Saluja D. Expression of heat shock protein 70 gene and its correlation with inflammatory markers in essential hypertension. PLoS One. (2016) 11(3):e0151060. 10.1371/journal.pone.0151060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of hypertension (ESH) and of the European society of cardiology (ESC). Eur Heart J. (2013) 34(28):2159–219. 10.1093/eurheartj/eht151 [DOI] [PubMed] [Google Scholar]
- 3.Jing L, Fan L, Huaqi, Jun C, Luyuan C, Weiwei C, et al. China Elderly hypertension management guidelines 2019. Chin J Hypertens. (2019) 27(2):111–35. 10.16439/j.cnki.1673-7245.2019.02.008 [DOI] [Google Scholar]
- 4.Cononie CC, Graves JE, Pollock ML, Phillips MI, Sumners C, Hagberg JM. Effect of exercise training on blood pressure in 70- to 79-yr-old men and women. Med Sci Sports Exerc. (1991) 23(4):505–11. 10.1249/00005768-199104000-00018 [DOI] [PubMed] [Google Scholar]
- 5.Lee LL, Mulvaney CA, Wong YKY, Chan ES, Watson MC, Lin HH. Walking for hypertension. Cochrane Database Syst Rev. (2021) 2(2):Cd008823. 10.1002/14651858.CD008823.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valenzuela PL, Carrera-Bastos P, Gálvez BG, Ruiz-Hurtado G, Ordovas JM, Ruilope LM, et al. Lifestyle interventions for the prevention and treatment of hypertension. Nat Rev Cardiol. (2021) 18(4):251–75. 10.1038/s41569-020-00437-9 [DOI] [PubMed] [Google Scholar]
- 7.Strilchuk L, Cincione RI, Fogacci F, Cicero AFG. Dietary interventions in blood pressure lowering: current evidence in 2020. Kardiol Pol. (2020) 78(7–8):659–66. 10.33963/kp.15468 [DOI] [PubMed] [Google Scholar]
- 8.Cicero AFG, Veronesi M, Fogacci F. Dietary intervention to improve blood pressure control: beyond salt restriction. High Blood Press Cardiovasc Prev. (2021) 28(6):547–53. 10.1007/s40292-021-00474-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu X, Shi M, Pang H, Cheang I, Zhu Q, Guo Q, et al. Inverse association of serum carotenoid levels with prevalence of hypertension in the general adult population. Front Nutr. (2022) 9:971879. 10.3389/fnut.2022.971879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54(24):1451–62. 10.1136/bjsports-2020-102955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meilan G, Xin Z, Mingxin S, Yanjun W. Research progress on the treatment effect of traditional health preserving techniques on primary hypertension. Chin J Gerontol. (2020) 40(18):4019–22. CNKI:SUN:ZLXZ.0.2020-18-068 [Google Scholar]
- 12.Weiying F, Liwei Z. Research progress of traditional exercise therapy on vascular endothelial function in patients with hypertension. Chin Nurs Res. (2020) 34(6):1021–5. 10.12102/j.issn.1009-6493.2020.06.022 [DOI] [Google Scholar]
- 13.Liang H, Luo S, Chen X, Lu Y, Liu Z, Wei L. Effects of Tai Chi exercise on cardiovascular disease risk factors and quality of life in adults with essential hypertension: a meta-analysis. Heart Lung. (2020) 49(4):353–63. 10.1016/j.hrtlng.2020.02.041 [DOI] [PubMed] [Google Scholar]
- 14.Song Y, Li J, István B, Xuan R, Wei S, Zhong G, et al. Current evidence on traditional Chinese exercises for quality of life in patients with essential hypertension: a systematic review and meta-analysis. Front Cardiovasc Med. (2020) 7:627518. 10.3389/fcvm.2020.627518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhong D, Li J, Yang H, Li Y, Huang Y, Xiao Q, et al. Tai Chi for essential hypertension: a systematic review of randomized controlled trials. Curr Hypertens Rep. (2020) 22(3):25. 10.1007/s11906-020-1031-y [DOI] [PubMed] [Google Scholar]
- 16.Guan Y, Hao Y, Guan Y, Wang H. Effects of Tai Chi on essential hypertension and related risk factors: a meta-analysis of randomized controlled trials. J Rehabil Med. (2020) 52(5):jrm00057. 10.2340/16501977-2683 [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4(1):1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin J, Guigui W. 1999 World health organization/international union for hypertension guidelines on treatment of hypertension. Chin J Hypertens. (1999) 7(2):4–7. 10.16439/j.cnki.1673-7245.1999.02.002 [DOI] [Google Scholar]
- 19.Yuqing Z, Guozhang L. Guidelines for prevention and treatment of hypertension in China (for trial implementation). Chin J Intern Med. (2000) 39(2):67–71. 10.3760/j.issn:0578-1426.2000.02.031 [DOI] [Google Scholar]
- 20.Whitworth JA, Chalmers J. World health organisation-international society of hypertension (WHO/ISH) hypertension guidelines. Clin Exp Hypertens. (2004) 26(7–8):747–52. 10.1081/ceh-200032152 [DOI] [PubMed] [Google Scholar]
- 21.Huaqi. Interpretation of “guidelines for prevention and treatment of hypertension in China” (revised edition in 2005) (I) new progres in diagnosis and treatment of hypertension. Chin J Cardiovasc Rev. (2006) (2):85–8. [Google Scholar]
- 22.Lisheng L. 2010 Chinese guidelines for the management of hypertension. Chin J Hypertens. (2011) 19(8):701–43. 10.16439/j.cnki.1673-7245.2011.08.009 [DOI] [Google Scholar]
- 23.Lijuan F, Li G, DaiLiang Z, Zhongchun L, Mengxiao L, Rongjiang J. Clinical evaluation of 24-type Tai Ji Chuan on antihypertensive effect and blood lipid level in elderly patients with primary hypertension. Chin J Convalescent Med. (2018) 27(10):1009–13. 10.13517/j.cnki.ccm.2018.10.001 [DOI] [Google Scholar]
- 24.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. Br Med J. (2011) 343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. (2019) 10:Ed000142. 10.1002/14651858.Ed000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cochrane M, Mitchell E, Hollingworth W, Crawley E, Trépel D. Cost-effectiveness of interventions for chronic fatigue syndrome or myalgic encephalomyelitis: a systematic review of economic evaluations. Appl Health Econ Health Policy. (2021) 19(4):473–86. 10.1007/s40258-021-00635-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsai JC, Wang WH, Chan P, Lin LJ, Wang CH, Tomlinson B, et al. The beneficial effects of Tai Chi Chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J Altern Complement Med. (2003) 9(5):747–54. 10.1089/107555303322524599 [DOI] [PubMed] [Google Scholar]
- 28.Hongni M, Peng S. Effect of Tai Chi exer cise on blood pr essur e, plasma nitrogen-monoxidum and endothelin in hyper tensive patients. Chin J Clin Rehabil. (2006) 10(48):65–7. CNKI:SUN:XDKF.0.2006-48-025 [Google Scholar]
- 29.Xiangxian C, Qing LH. Effects of taijiquan exercise on hypertension Patients’ NO consistency in plasma, the activity of RBC Na+-K+ ATPase and Ca2+-Mg2+ ATPase. J Beijing Sport Univ. (2006) 29(10):1359–61. 10.19582/j.cnki.11-3785/g8.2006.10.023 [DOI] [Google Scholar]
- 30.Qinghua T. Effects of traditional sports on clinical symptom of aged intellectual patients with essential hypertension. J Beijing Sport Univ. (2009) 32(2):67–9. 10.19582/j.cnki.11-3785/g8.2009.02.017 [DOI] [Google Scholar]
- 31.Jinghe H, Li Y, Zhen C, Guannan L. Effect of Tai Ji Chuan intervention on primary hypertension. Chin J Rehabil Med. (2011) 26(10):968–71. 10.3969/j.issn.1001-1242.2011.10.019 [DOI] [Google Scholar]
- 32.Xiaojun W, Zhikun J, Ningning Z. Effects of taichi exercises of various intensities on essential hypertension. J Shenyang Sport Univ. (2011) 30(4):82–5. 10.3969/j.issn.1004-0560.2011.04.020 [DOI] [Google Scholar]
- 33.Lo HM, Yeh CY, Chang SC, Sung HC, Smith GD. A Tai Chi exercise programme improved exercise behaviour and reduced blood pressure in outpatients with hypertension. Int J Nurs Pract. (2012) 18(6):545–51. 10.1111/ijn.12006 [DOI] [PubMed] [Google Scholar]
- 34.Feng S, Chunfeng S. Intervention effect of Tai Ji Chuan exercise on senile hypertension. Chin J Gerontol. (2014) 34(24):6862–4. CNKI:SUN:ZLXZ.0.2014-24-005 [Google Scholar]
- 35.Huijuan X, Caiqin B. Gaseous signal molecular mechanism of Taijiquan’s intervention in aged-essential hypertension. J Wuhan Inst Phys Educ. (2014) 48(2):51–4+63. 10.15930/j.cnki.wtxb.2014.02.001 [DOI] [Google Scholar]
- 36.Dalu Q, Yongming L, Xinghui Y. Influence of Taijiquan on eight patients with hypertension blood pressure levels. Sichuan Sports Sci. (2015) 34(5):24–6+39. 10.13932/j.cnki.sctykx.2015.05.07 [DOI] [Google Scholar]
- 37.Lixun H, Jianquan Y. Effects of vigorous walk combined with Taijiquan on blood glucose and lipid, blood pressure in elderly hypertensive patients. Hainan Med J. (2015) 26(14):2053–5. 10.3969/j.issn.1003-6350.2015.14.0742 [DOI] [Google Scholar]
- 38.Pan X, Zhang Y, Tao S. Effects of Tai Chi exercise on blood pressure and plasma levels of nitric oxide, carbon monoxide and hydrogen sulfide in real-world patients with essential hypertension. Clin Exp Hypertens. (2015) 37(1):8–14. 10.3109/10641963.2014.881838 [DOI] [PubMed] [Google Scholar]
- 39.Sun J, Buys N. Community-based mind-body meditative Tai Chi program and its effects on improvement of blood pressure, weight, renal function, serum lipoprotein, and quality of life in Chinese adults with hypertension. Am J Cardiol. (2015) 116(7):1076–81. 10.1016/j.amjcard.2015.07.012 [DOI] [PubMed] [Google Scholar]
- 40.Yongcai Z, Liang C, Jianquan Y. Taijiquan systematic reviews of primary effects on blood pressureand ouality of life of patients with hypertension. J Liaoning Uni TCM. (2015) 17(4):143–6. 10.13194/j.issn.1673-842x.2015.04.050 [DOI] [Google Scholar]
- 41.Chaoyang L, Liang W, Ruiling L. The influence of exercise treatment on typeⅠhypertension of elders. J Henan Univ (Med Sci). (2016) 35(4):287–9. 10.15991/j.cnki.41-1361/r.2016.04.017 [DOI] [Google Scholar]
- 42.Haolei J, Jiajia P. Effects of taijiquan on 24-hour dynamic blood pressure and vascular function in patients with primary mild hypertension. Chin J Sports Med. (2016) 35(3):224–7. 10.16038/j.1000-6710.2016.03.004 [DOI] [Google Scholar]
- 43.Rong G, Xiuqin H, Fengling W, Juan W. Effect of Tai Ji Chuan exercise combined with newman system health care model on blood pressure and quality of life of elderly patients with hypertension. Chin J Ctrl Endem Dis. (2017) 32(7):823–5. CNKI:SUN:DYBF.0.2017-07-059 [Google Scholar]
- 44.Ma C, Zhou W, Tang Q, Huang S. The impact of group-based Tai Chi on health-status outcomes among community-dwelling older adults with hypertension. Heart Lung. (2018) 47(4):337–44. 10.1016/j.hrtlng.2018.04.007 [DOI] [PubMed] [Google Scholar]
- 45.Tao L, Qidong H, Weizhong L. Effect of Tai Ji Chuan exercise on blood pressure, hemorheology and long-term quality of life in elderly patients with hypertension. Chin J Gerontol. (2018) 38(6):1396–8. CNKI:SUN:ZLXZ.0.2018-06-051 [Google Scholar]
- 46.Xiaoling S, Wang L, Liyue Z, Hua R, Wanzhen W, Ping XS, et al. Effect of Tai Ji Chuan exercise on emotion and heart rate variability in patients with hypertension. Mod Chin Doctor. (2018) 56(29):95–9. [Google Scholar]
- 47.Xiaorui L. Effect of Tai Ji Chuan exercise combined with comprehensive nursing intervention on blood pressure control and quality of life of patients with essential hypertension. Chin J Convalesc Med. (2018) 27(1):19–21. 10.13517/j.cnki.ccm.2018.01.007 [DOI] [Google Scholar]
- 48.Yakang X. Effects of eight-Tai Ji Chuan exercise on blood pressure level, vascular endothelial function and quality of life of patients with essential hypertension. Chin J Gerontol. (2018) 38(10):2403–5. 10.3969/j.issn.1005-9202.2018.10.041 [DOI] [Google Scholar]
- 49.Shou XL, Wang L, Jin XQ, Zhu LY, Ren AH, Wang QN. Effect of T’ai Chi exercise on hypertension in young and middle-aged in-service staff. J Altern Complement Med. (2019) 25(1):73–8. 10.1089/acm.2018.0011 [DOI] [PubMed] [Google Scholar]
- 50.Xiaobin W, Luping Y. Effect of 24-type simplified Tai Ji Chuan on primary hypertension with mild anxiety in the elderly. Fujian J TCM. (2019) 50(4):73–5. 10.13260/j.cnki.jfjtcm.011881 [DOI] [Google Scholar]
- 51.Qinghua H, Youling G, Xiaoli L, Huan Z, Jiewen X. Effects of 12-week Tai Chi exercise on the microvascular reactivityof the middle-aged and elderly patients with mild hypertensionand its mechanism. Chin J Appl Physiol. (2021) 37(6):683–7. 10.12047/j.cjap.6164.2021.080 [DOI] [PubMed] [Google Scholar]
- 52.Cao L, Li X, Yan P, Wang X, Li M, Li R, et al. The effectiveness of aerobic exercise for hypertensive population: a systematic review and meta-analysis. J Clin Hypertens (Greenwich). (2019) 21(7):868–76. 10.1111/jch.13583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Motoyama M, Sunami Y, Kinoshita F, Kiyonaga A, Tanaka H, Shindo M, et al. Blood pressure lowering effect of low intensity aerobic training in elderly hypertensive patients. Med Sci Sports Exerc. (1998) 30(6):818–23. 10.1097/00005768-199806000-00007 [DOI] [PubMed] [Google Scholar]
- 54.Morrison WL, Petch MC. Exercise-induced hypotension. Lancet. (1987) 2(8565):969. 10.1016/s0140-6736(87)91448-6 [DOI] [PubMed] [Google Scholar]
- 55.Junwei W, Qiongjia Y, Yangpengpai, Jixin S, Tao FJ, Guangwen S, et al. Effect of exercise therapy on primary hypertension in China: meta analysis. Chin J Rehabil Med. (2017) 32(4):454–60. 10.3969/j.issn.1001-1242.2017.04.016 [DOI] [Google Scholar]
- 56.Ishikawa-Takata K, Ohta T, Tanaka H. How much exercise is required to reduce blood pressure in essential hypertensives: a dose-response study. Am J Hypertens. (2003) 16(8):629–33. 10.1016/s0895-7061(03)00895-1 [DOI] [PubMed] [Google Scholar]
- 57.He L, Renwei W, Can Z, Liangliang X. Effects of 12-week walking on blood pressure and lipid of hypertensive patients. Sport Sci Res. (2016) 37(1):76–9+84. CNKI:SUN:TYKA.0.2016-01-012 [Google Scholar]
- 58.An LJ. Exercise therapy for hypertension. Mod Rehabil. (2001) 5(5):6–21. 10.3321/j.issn:1673-8225.2001.05.002 [DOI] [Google Scholar]
- 59.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. (2005) 365(9468):1415–28. 10.1016/s0140-6736(05)66378-7 [DOI] [PubMed] [Google Scholar]
- 60.Yanai H, Tomono Y, Ito K, Furutani N, Yoshida H, Tada N. The underlying mechanisms for development of hypertension in the metabolic syndrome. Nutr J. (2008) 7:10. 10.1186/1475-2891-7-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Silveira Rossi JL, Barbalho SM, Reverete de Araujo R, Bechara MD, Sloan KP, Sloan LA. Metabolic syndrome and cardiovascular diseases: going beyond traditional risk factors. Diabetes Metab Res Rev. (2022) 38(3):e3502. 10.1002/dmrr.3502 [DOI] [PubMed] [Google Scholar]
- 62.Helkin A, Stein JJ, Lin S, Siddiqui S, Maier KG, Gahtan V. Dyslipidemia part 1--review of lipid metabolism and vascular cell physiology. Vasc Endovascular Surg. (2016) 50(2):107–18. 10.1177/1538574416628654 [DOI] [PubMed] [Google Scholar]
- 63.Waclawovsky G, Pedralli ML, Eibel B, Schaun MI, Lehnen AM. Effects of different types of exercise training on endothelial function in prehypertensive and hypertensive individuals: a systematic review. Arq Bras Cardiol. (2021) 116(5):938–47. 10.36660/abc.20190807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hanna RM, Ahdoot RS, Kim MS, Jhaveri KD, Kalantar-Zadeh K, Kurtz IB. Intravitreal vascular endothelial growth factors hypertension, proteinuria, and renal injury: a concise review. Curr Opin Nephrol Hypertens. (2022) 31(1):47–56. 10.1097/mnh.0000000000000760 [DOI] [PubMed] [Google Scholar]
- 65.Xiaobei S, Wei L. The relationship between arterial stiffness and complex profiles of blood lipid in hypertensions. Chin J Dis Control Prev. (2019) 23(8):956–60. 10.16462/j.cnki.zhjbkz.2019.08.014 [DOI] [Google Scholar]
- 66.Yuanyuan C, Zengwu W, Li JJ, Yeping, Yuqing Z, Yong L, et al. China Expert consensus on comprehensive management of blood pressure and lipid in patients with hypertension. Chin J Hypertens (2019) 27(7):605–14. 10.16439/j.cnki.1673-7245.2019.07.002 [DOI] [Google Scholar]
- 67.Tessier S, Riesco E, Lacaille M, Pérusse F, Weisnagel J, Doré J, et al. Impact of walking on adipose tissue lipoprotein lipase activity and expression in pre- and postmenopausal women. Obes Facts. (2010) 3(3):191–9. 10.1159/000314611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jeppesen J, Kiens B. Regulation and limitations to fatty acid oxidation during exercise. J Physiol. (2012) 590(5):1059–68. 10.1113/jphysiol.2011.225011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.He N, Ye H. Exercise and hyperlipidemia. Adv Exp Med Biol. (2020) 1228:79–90. 10.1007/978-981-15-1792-1_5 [DOI] [PubMed] [Google Scholar]
- 70.Muscella A, Stefàno E, Marsigliante S. The effects of exercise training on lipid metabolism and coronary heart disease. Am J Physiol Heart Circ Physiol. (2020) 319(1):H76–H88. 10.1152/ajpheart.00708.2019 [DOI] [PubMed] [Google Scholar]
- 71.Ma J, Zhang JW, Li H, Zhao LS, Guo AY, Chen ZH, et al. Safety and effectiveness of a Tai Chi-based cardiac rehabilitation programme for chronic coronary syndrom patients: study protocol for a randomised controlled trial. BMJ Open. (2020) 10(7):e036061. 10.1136/bmjopen-2019-036061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhou S, Zhang Y, Kong Z, Loprinzi PD, Hu Y, Ye J, et al. The effects of Tai Chi on markers of atherosclerosis, lower-limb physical function, and cognitive ability in adults aged over 60: a randomized controlled trial. Int J Environ Res Public Health. (2019) 16(5):753–64. 10.3390/ijerph16050753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yunjian Z, Dongmei L, Songbo Z. Effects of single acute Taijiquan exercise on essen tial hypertension. J Fourth M ilM ed Univ. (2009) 30(24):3136–9. CNKI:SUN:DSJY.0.2009-24-107 [Google Scholar]
- 74.Santos-Parker JR, LaRocca TJ, Seals DR. Aerobic exercise and other healthy lifestyle factors that influence vascular aging. Adv Physiol Educ. (2014) 38(4):296–307. 10.1152/advan.00088.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Seals DR, Edward F. Adolph distinguished lecture: the remarkable anti-aging effects of aerobic exercise on systemic arteries. J Appl Physiol (1985). (2014) 117(5):425–39. 10.1152/japplphysiol.00362.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: CNKI(https://www.cnki.net/). Wan Fang Databases (https://www.wanfangdata.com.cn/index.html). PubMed (https://pubmed.ncbi.nlm.nih.gov/). Web Of Science (https://clarivate.com/products/web-of-science/). Science Direct (https://www.sciencedirect.com/). Accession numbers can be found in the Supplementary Material.