Abstract
Purpose
The aim of this study was to determine correlation between the spinopelvic parameters in sitting and standing positions (sacral slope [SS], lumbar lordosis [LL], spinopelvic tilt [SPT], pelvic incidence [PI], and pelvic femoral angle [PFA]), with hip function assessed using the modified Harris hip scores (mHHs) in patients with symptomatic femoroacetabular impingement (FAI) at diagnosis.
Materials and Methods
A retrospective study of 52 patients diagnosed with symptomatic FAI was conducted. Evaluation of the spinopelvic complex in terms of SS, LL, SPT, PI and PFA was performed using lateral radiographs of the pelvis and lumbosacral spine in standing and sitting positions. Assessment of hip function at diagnosis was performed using the mHHs. Calculation of spinopelvic mobility was based on the difference (Δ) between measurements performed in standing and sitting position.
Results
The median time of pain evolution was 11 months (interquartile range [IQR], 5-24 months) with a median mHHs of 66.0 points (IQR, 46.0-73.0) at diagnosis. The mean change of LL, SS, SPT, and PFA was 20.9±11.2°, 14.2±8.6°, 15.5±9.0°, and 70.7±9.5°, respectively. No statistically significant correlation was observed between spinopelvic parameters and the mHHs (P>0.05).
Conclusion
Radiological parameters of the spinopelvic complex did not show correlation with hip function at the time of diagnosis in patients with symptomatic FAI. Conduct of further studies will be required in the effort to understand the effect of the spinopelvic complex and its compensatory mechanics, primarily between the hip and spine, in patients with FAI before and after hip arthroscopy.
Keywords: Femoroacetabular impingement, Spinopelvic mobility, Lumbar lordosis, Hip function
INTRODUCTION
Knowledge regarding pathologies of the hip has evolved with passage of time from an isolated approach to one involving the interaction with the pelvis and the spine, known as the spinopelvic complex. Appropriate interaction between these structures determines the correct sagittal balance of each person, which can be evaluated in different anatomical positions using radiological parameters, such as sacral slope (SS), lumbar lordosis (LL), spinopelvic tilt (SPT), pelvic incidence (PI), and pelvic femoral angle (PFA)1,2,3).
In the last decade, femoroacetabular impingement (FAI), which is attributed to abnormal contact between the acetabulum and the femoral head-neck junction, has been identified as a primary cause of hip pain and functional limitation4). Abnormalities in spinopelvic parameters, with reduced SPT and PI, and increased SS, as well as a lower lumbar range of movement have been reported in patients with FAI compared to those without FAI5,6,7). These findings suggest that a change in any of the structures of the spinopelvic complex can lead to modification of the optimal balance between the femur and the acetabulum, resulting in development of intra-articular pathology.
In contrast, authors including Fader et al.5) and Yin et al.8) evaluated the effect of spinopelvic parameters on the occurrence of hip pain. Fader et al.5) reported no significant differences in LL, PI, and SS values between patients with asymptomatic FAI and those with symptomatic FAI. However, they reported that the group with symptomatic FAI showed lower lumbar mobility compared to the control group without FAI. In addition, Yin et al.8) reported lower PI and SS in patients with symptomatic FAI, which is reflected in a reduced capacity for pelvic adaptation during movement from a sitting to a standing position. However, they did not evaluate the relationship between SPT and LL with hip pain.
In summary, despite the reported findings described above, evidence regarding the relationship between spinopelvic parameters and FAI symptomatology is still inconclusive. Only studies on its relationship with the occurrence of hip pain, not with perceived hip function, have been reported. Therefore, in the effort to obtain more favorable results from conservative and surgical treatment, attaining a more in depth understanding of the dynamic effect of the spinopelvic complex on the severity of FAI symptomatology could be helpful in the development of physical rehabilitation protocols.
Therefore, the aim of this study was to determine correlation between the spinopelvic parameters in sitting and standing positions (SS, LL, SPT, PI, and PFA), with hip function assessed using the modified Harris hip scores (mHHs) in patients with symptomatic FAI at diagnosis. According to our hypothesis, there is an association of better lumbar mobility and pelvic adaptability with a higher level of perceived function in patients with symptomatic FAI.
MATERIALS AND METHODS
This study was approved by the Institutional Ethics Committee of Clínica Imbanaco Grupo QuirónSalud (approval code: CEI-595) and conducted under the agreements of the Declaration of Helsinki (2013). A retrospective review of a consecutive cohort of patients who consulted for hip pain and were diagnosed with FAI at Clínica Imbanaco Grupo QuirónSalud by the lead author (B.A.B) from 2020 to 2021 was conducted. Patients with lateral radiographs of the pelvis and lumbosacral spine in standing and sitting positions were considered eligible for inclusion in this study. Patients with osteoarthritis (Tönnis grade 2-3), previous fractures of the femur or pelvis, hip dysplasia, or a history of lumbar pathologies were excluded.
Confirmation of the diagnosis of FAI was based on findings from physical examination (FADDIR: flexion, adduction, and internal rotation) and imaging including hip radiograph (anteroposterior pelvis, 45° and 90° Dunn projection, and false profile) and 3-Tesla magnetic resonance imaging. Spine radiographs taken in a standing and seated position became an indication in all cases in January 2020 due to the increasing interest in the spinopelvic complex in pathologies of the hip. In addition, assessment of hip function was performed using mHHs prior to deciding on a specific treatment; mHHs is regarded as a valid and reliable scale for quantifying hip function in patients with FAI9,10). The mHHs values range from 0 (worst) to 100 (best).
Both standing and seated radiographs were extracted from the institutional medical records system. All radiological measurements were performed using the tools included in the Weasis visualization program (ver. 3.5.3; Weasis Team)11). According to the institutional protocol, the standing radiographs were taken with a focus on perpendicularity of both femoral heads and when taken in the seated position both femurs were aligned in parallel in order to obtain an apparent hip flexion of 90°.
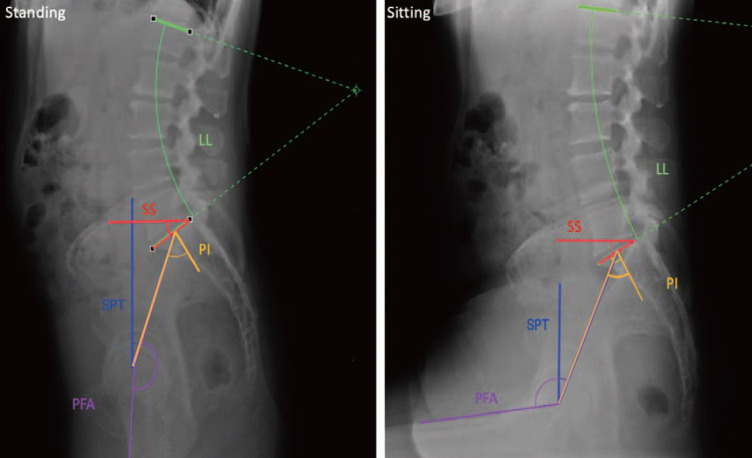
Evaluation of the spine was performed through the LL and measurement was based on the angle between the zone of greatest lumbar inflection (superior endplate of L1) and the superior endplate of S1. PI, which corresponds to the sum of SS and SPT, was used in assessment of pelvic morphology; use of these two parameters enables evaluation of the pelvic alignment in relation to the sacrum and femoral heads, respectively. Measurement of SPT was based on the angle formed between the line from the midpoint of the sacral plateau to the femoral head and a vertical reference line drawn from the same point, and SS was measured as the angle between the horizontal line and the superior plate of S1. Assessment of the hip was performed through the PFA, which was measured as the angle between a line defined by the anterior cortex of the most protruding femur toward the mid zone and the superior S1, using the center of the femoral head as a reference point (Fig. 1).
Fig. 1. Radiographic measurements of the spinopelvic complex in sitting and standing positions.
SS: sacral slope, LL: lumbar lordosis, SPT: spinopelvic tilt, PI: pelvic incidence, PFA: pelvic femoral angle.
Assessment of the mobility of the spine, pelvis, and hip was performed using the parameters of the spinopelvic complex and was defined as the difference between measurements taken in standing and sitting positions (ΔX_(standing/sitting)=Xstanding-Xsitting).
A ΔLL less than 20° was regarded as a stiff lumbar spine12). Sagittal alignment was classified as flatback if the difference between standing PI and LL (PI-LL) was >10° and hyperlordotic if PI-LL <–10°1,12). ΔSPT less than 10° was defined as stiff mobility of the spinopelvic complex and ΔSPT >30° was defined as hypermobile1,12). All measurements were performed simultaneously and independently by two evaluators. Calculation of standing PFA and sitting LL could not be performed in all cases. Most lateral radiographs taken in standing position did not include visualization of the anterior cortex of the femur and lateral radiographs taken in a seated position did not include the superior endplate of L1, so that data measurement could not be performed.
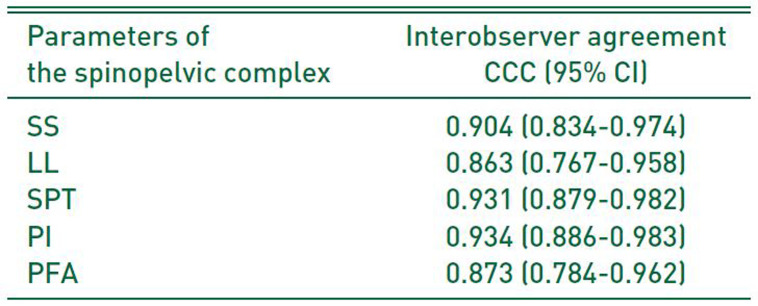
Stata 17.0 (StataCorp, College Station, TX, USA) was used in performance of all statistical analyses. Testing of the assumption of normality was performed using the Shapiro–Wilk test. Normally distributed variables were indicated with mean±standard deviation and otherwise, with median (interquartile range [IQR]). Assessment of interobserver agreement was performed using Lin’s concordance correlation coefficient (CCC). Values of CCC >0.75 were regarded as an indicator of good reliability13).
Analysis of the correlation between hip function (mHHs) and spinopelvic parameters was performed using Spearman’s correlation coefficient. All analyses were performed using a complete case approach, which implies that calculation of each correlation coefficient was performed using the observations without missing values for the variables of interest. A P-value <0.05 was considered statistically significant.
RESULTS
Lateral radiographs of the pelvis and lumbosacral spine taken in standing and sitting positions for 58 patients diagnosed with FAI between 2020 and 2021 were available for analysis. Five patients with a history of lumbar pathology and one patient who had previously undergone hip surgery were excluded from the study. Therefore, 52 patients with FAI with a mean age of 44.3±13.9 years were included; 59.6% (31 patients) of the patients were female and the right hip was affected in half of these patients. The median time of pain evolution was 11 months (IQR, 5-24 months) with a median mHHs of 66.0 points (IQR, 46.0-73.0) at diagnosis (Table 1).
Table 1. Characteristics of FAI Patients (n=52).
| Variable | Value | |
|---|---|---|
| Age (yr) | 44.3±13.9 | |
| Sex | ||
| Female | 31 (59.6) | |
| Male | 21 (40.4) | |
| Laterality | ||
| Right | 26 (50.0) | |
| Left | 26 (50.0) | |
| FAI | ||
| Pincer | 23 (44.2) | |
| Cam | 5 (9.6) | |
| Mixed | 24 (46.2) | |
| mHHs | 66.0 (46.0-73.0) | |
Values are presented as mean±standard deviation, number (%), or median (interquartile range).
FAI: femoroacetabular impingement, mHHs: modified Harris hip score.
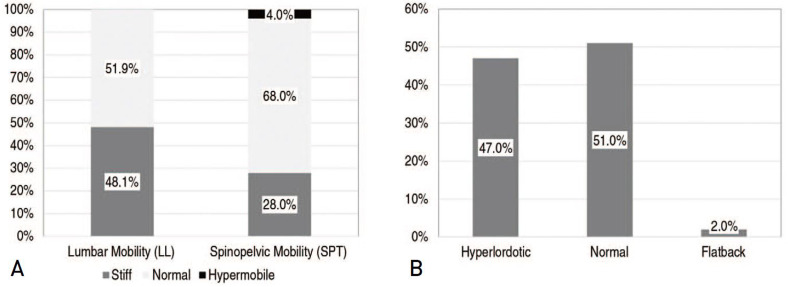
As shown in Table 2, the mean change in dynamics of the spinopelvic complex based on LL, SS, SPT, and PFA was 20.9±11.2°, 14.2±8.6°, 15.5±9.0°, and 70.7±9.5°, respectively. The interobserver reliability for all measures ranged from 0.863 to 0.934 (Appendix 1). Stiff lumbar mobility was detected in 48.1% (13/27) of patients with ΔLL (°) measurements. Results from measurement of the spinopelvic complex using SPT showed stiffness in 28.0% (14/50) of FAI patients during movement from a standing to a sitting position (Fig. 2A). Abnormal sagittal spinopelvic balance was observed in 49.0% of the patients, predominantly the hyperlordotic type; only one patient had a flatback deformity (Fig. 2B).
Table 2. Description of Spinopelvic Parameters in Standing and Sitting Positions.
| Parameter | Standing | Sitting | Change from a standing to a seated position | P-value | |
|---|---|---|---|---|---|
| LL, No. | 51 | 27 | 27 | ||
| Mean±SD (°) | 59.1±10.9 | 38.4±13.9 | 20.9±11.2 | <0.001 | |
| SS, No. | 52 | 52 | 52 | <0.001 | |
| Mean±SD (°) | 38.4±8.7 | 24.1±11.2 | 14.2±8.6 | ||
| SPT, No. | 50 | 52 | 50 | ||
| Mean±SD (°) | 11.6±6.6 | 26.9±10.2 | 15.5±9.0 | <0.001 | |
| PI, No. | 50 | 52 | 50 | ||
| Mean±SD (°) | 50.3±10.1 | 51.1±11.3 | –1.3±5.5 | 0.093 | |
| PFA, No. | 14 | 52 | 14 | ||
| Mean±SD (°) | 183.5±12.6 | 113.6±12.8 | 70.7±9.5 | <0.001 | |
No.: number of cases with non-missing values, LL: lumbar lordosis, SS: sacral slope, SPT: spinopelvic tilt, PI: pelvic incidence, PFA: pelvic femoral angle, SD: standard deviation.
Fig. 2. (A) Distribution of femoroacetabular impingement (FAI) patients according to lumbar and spinopelvic mobility. Measurements of lumbar lordosis (LL) and spinopelvic tilt (SPT) were available in 27 and 50 cases, respectively. (B) Distribution of FAI patients according to sagittal alignment.
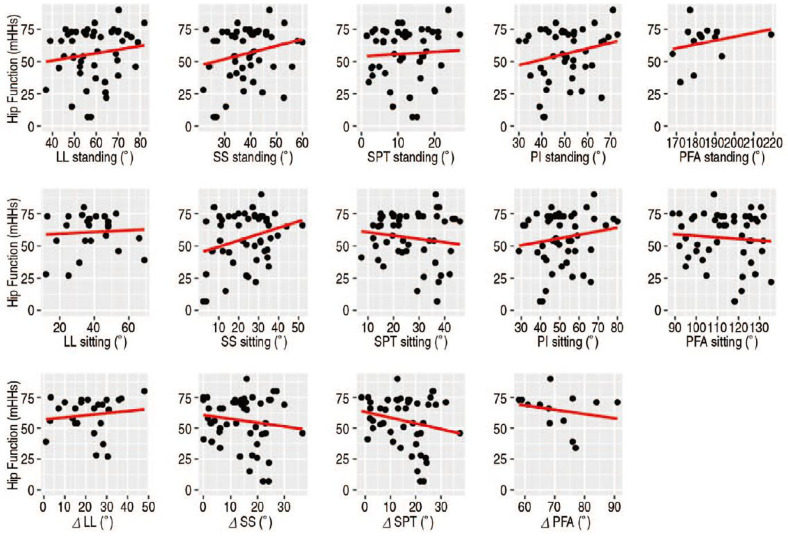
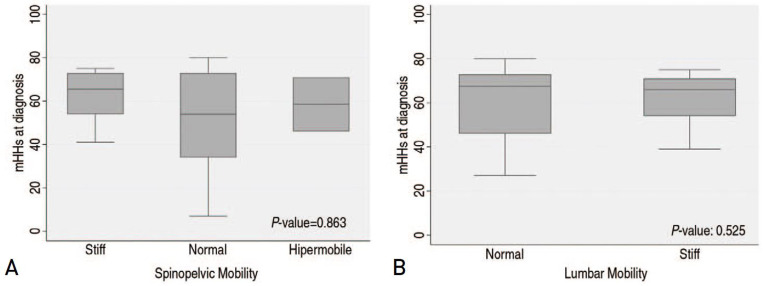
Results of the correlation analysis between spinopelvic parameters and hip function are shown in Table 3 and Fig. 3. No statistically significant correlation was observed between spinopelvic radiographic parameters and mHHs in standing and sitting positions. In addition, no evidence of a significant relationship was found between symptoms at diagnosis of FAI (mHHs) and mobility of the spinopelvic complex (Δ) ( P>0.05). The median of mHHs among patients with stiff, normal, and hypermobile spinopelvic complex was 65.5 points (IQR, 53.7-73.0), 54.0 points (IQR, 32.5-73.0), and 58.5 points (IQR, 46.0-71.0), respectively, and no statistically significant differences were observed between spinopelvic mobility groups (Fig. 4A). Similarly, no significant change in mHHs at diagnosis was observed between FAI patients with stiff lumbar mobility and those with normal lumbar mobility (Stiff, 66.0 points [IQR, 54.0-71.0] vs. Normal, 67.5 points [IQR, 43.7-73.0]) (Fig. 4B).
Table 3. Correlation between Radiological Parameters of the Spinopelvic Complex and Hip Function with Modified Harris Hip Score.
| Parameters of spinopelvic complex | No. of observations | Spearman coefficient | P-value |
|---|---|---|---|
| LL standing | 51 | 0.100 | 0.483 |
| SS standing | 52 | 0.169 | 0.231 |
| SPT standing | 50 | 0.031 | 0.829 |
| PI standing | 50 | 0.104 | 0.472 |
| PFA standing | 14 | 0.066 | 0.822 |
| LL sitting | 27 | 0.028 | 0.889 |
| SS sitting | 52 | 0.138 | 0.330 |
| SPT sitting | 52 | –0.063 | 0.656 |
| PI sitting | 52 | 0.144 | 0.307 |
| PFA sitting | 52 | –0.062 | 0.661 |
| ΔLL | 27 | 0.049 | 0.805 |
| ΔSS | 52 | –0.117 | 0.409 |
| ΔSPT | 50 | –0.119 | 0.409 |
| ΔPFA | 14 | –0.286 | 0.321 |
No.: number of cases with non-missing values, LL: lumbar lordosis, SS: sacral slope, SPT: spinopelvic tilt, PI: pelvic incidence, PFA: pelvic femoral angle.
Fig. 3. Correlation plot for the relationship between hip function at diagnosis and spinopelvic parameters. The red line represents the trend line using linear regression analysis.
mHHs: modified Harris hip score, LL: lumbar lordosis, SS: sacral slope, SPT: spinopelvic tilt, PI: pelvic incidence, PFA: pelvic femoral angle.
Fig. 4. (A) Boxplot showing the values of modified Harris hip score (mHHs) according to the classification of spinopelvic mobility. (B) Boxplot showing the values of mHHs according to lumbar mobility.
DISCUSSION
Differences in the radiological parameters of the spinopelvic complex have been associated with the presence of morphological findings of FAI; however, no studies using patient-reported outcomes measures (PROMs) to determine their relationship with hip function have been conducted. The results of this study indicated that LL, SS, SPT, PI, and PFA values did not show correlation with perceived functional disability in patients with FAI. This finding is similar to that reported in patients with advanced osteoarthritis of the hip, for whom similar scores on preoperative PROMs have been reported according to the type of spinopelvic mobility14).
Although we found no direct relationship between lumbar mobility (ΔLL [°]) and hip function, a greater range of lumbar mobility has been associated with a decrease in pelvic tilt or anteversion, resulting in a lower functional demand on the hip joint15). Patients with greater lumbar mobility are also known as “spine users”, who, according to one hypothesis, may be endowed with a protective effect against the risk of hip injury. For example, as suggested by Fader et al.5), even patients with radiographic FAI who have optimal lumbar mobility may remain pain-free, with avoidance of excessive hip flexion and, consequently, the onset of pain. In addition, an association of lumbar stiffness with higher complications rates following total hip replacement, such as wear and dislocation of the prosthesis, has been reported16,17).
In this study, abnormal mobility of the spinopelvic complex was detected in one third of FAI patients at diagnosis, with a stiffness pattern predominating in most cases. No specific pattern of spinopelvic mobility has been described in patients with advanced osteoarthritis of the hip, with an equal percentage of stiff or hypermobile patterns (-20%)1). However, compared to patients without osteoarthritis of the hip, the percentage of patients with a hypermobile pattern is higher, which has been interpreted as a compensatory mechanism for more posterior tilting of the pelvis to match the reduced range of hip flexion.
Several studies evaluating the influence of the spinopelvic complex on the clinical outcomes after total hip replacement have been reported16). However, thorough study of functional outcomes after hip arthroscopy and their relationship to parameters of the spinopelvic complex in cases of FAI has not been conducted. Jimenez et al.18), in a study of 51 patients who underwent hip arthroscopy at one-year follow-up, reported that lumbopelvic mobility is not a predictor of worse functional outcomes based on the dynamics of SS during position changes (ΔSS <10°). However, SPT and LL may be better indicators of pelvic and lumbar motion, respectively, thus this finding should be interpreted with caution1). In addition, through conduct of a case-control study, Beck et al.19) reported lower PROMs scores at two-year follow-up in FAI patients with a history of lumbar pathology compared to FAI patients without spinal pathology, indicating that lumbar mobility could be considered a poor prognostic factor in FAI patients treated with hip arthroscopy19,20,21).
This study has several limitations. First, measurement of parameters of interest could not be performed due to the retrospective nature of this study and the quality of the radiological images in all patients, which decreased the sample size and the statistical power. Nonetheless, these findings denote a starting point in the effort to attain a more in depth understanding of the role of the spinopelvic complex in FAI. Second, computation of a prior sample size was not performed in this study. However, the number of patients included is sufficient for detection of a strong correlation of at least 0.70 with a power of 80% and a one-sided level test of 5%. Third, no stratified analyses according to the type of FAI were performed because the sample size was not large enough.
CONCLUSION
Radiological parameters of the spinopelvic complex in patients with symptomatic FAI did not show correlation with hip function at diagnosis. However, conduct of further studies will be required in the effort to understand the effect of the spinopelvic complex and its compensatory mechanics, primarily between the hip and spine, in patients with FAI before and after hip arthroscopy.
Appendix 1
Interobserver Agreement of Radiological Measurements of the Spinopelvic Complex
CCC: concordance correlation coefficient, CI: confidence interval, SS: sacral slope, LL: lumbar lordosis, SPT: spinopelvic tilt, PI: pelvic incidence, PFA: pelvic femoral angle.
Footnotes
FUNDING: No funding to declare.
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Innmann MM, Merle C, Phan P, Beaulé PE, Grammatopoulos G. Differences in spinopelvic characteristics between hip osteoarthritis patients and controls. J Arthroplasty. 2021;36:2808–2816. doi: 10.1016/j.arth.2021.03.031. [DOI] [PubMed] [Google Scholar]
- 2.Innmann MM, Reichel F, Schaper B, Merle C, Beaulé PE, Grammatopoulos G. How does spinopelvic mobility and sagittal functional cup orientation affect patient-reported outcome 1 year after THA?- a prospective diagnostic cohort study. J Arthroplasty. 2021;36:2335–2342. doi: 10.1016/j.arth.2021.02.014. [DOI] [PubMed] [Google Scholar]
- 3.Rivière C, Hardijzer A, Lazennec JY, Beaulé P, Muirhead-Allwood S, Cobb J. Spine-hip relations add understandings to the pathophysiology of femoro-acetabular impingement: a systematic review. Orthop Traumatol Surg Res. 2017;103:549–557. doi: 10.1016/j.otsr.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 4.Chambers CC, Zhang AL. Outcomes for surgical treatment of femoroacetabular impingement in adults. Curr Rev Musculoskelet Med. 2019;12:271–280. doi: 10.1007/s12178-019-09567-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fader RR, Tao MA, Gaudiani MA, et al. The role of lumbar lordosis and pelvic sagittal balance in femoroacetabular impingement. Bone Joint J. 2018;100-B:1275–1279. doi: 10.1302/0301-620X.100B10.BJJ-2018-0060.R1. [DOI] [PubMed] [Google Scholar]
- 6.Weinberg DS, Gebhart JJ, Liu RW, Salata MJ. Radiographic signs of femoroacetabular impingement are associated with decreased pelvic incidence. Arthroscopy. 2016;32:806–813. doi: 10.1016/j.arthro.2015.11.047. [DOI] [PubMed] [Google Scholar]
- 7.Mascarenhas VV, Rego P, Dantas P, et al. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: a systematic review. Eur J Radiol. 2016;85:73–95. doi: 10.1016/j.ejrad.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 8.Yin QF, Zhang J, Liang T, Liu YJ, Zhang SX, Li CB. The evaluation of sagittal pelvic-femoral kinematics in patients with cam-type femoracetabular impingement. Orthop Surg. 2021;13:1748–1754. doi: 10.1111/os.13038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindman I, Nikou S, Öhlin A, et al. Evaluation of outcome reporting trends for femoroacetabular impingement syndrome- a systematic review. J Exp Orthop. 2021;8:33. doi: 10.1186/s40634-021-00351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aprato A, Jayasekera N, Villar RN. Does the modified Harris hip score reflect patient satisfaction after hip arthroscopy? Am J Sports Med. 2012;40:2557–2560. doi: 10.1177/0363546512460650. [DOI] [PubMed] [Google Scholar]
- 11.Weasis. Weasis DICOM medical viewer [Internet] 2022. [cited 2022 Sep 28]. Available from: https://nroduit.github.io/en/
- 12.Innmann MM, Merle C, Phan P, Beaulé PE, Grammatopoulos G. How can patients with mobile hips and stiff lumbar spines be identified prior to total hip arthroplasty? A prospective, diagnostic cohort study. J Arthroplasty. 2020;35(6S):S255–S261. doi: 10.1016/j.arth.2020.02.029. [DOI] [PubMed] [Google Scholar]
- 13.Liljequist D, Elfving B, Skavberg Roaldsen K. Intraclass correlation- a discussion and demonstration of basic features. PLoS One. 2019;14:e0219854. doi: 10.1371/journal.pone.0219854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Innmann MM, Merle C, Gotterbarm T, Ewerbeck V, Beaulé PE, Grammatopoulos G. Can spinopelvic mobility be predicted in patients awaiting total hip arthroplasty? A prospective, diagnostic study of patients with end-stage hip osteoarthritis. Bone Joint J. 2019;101-B:902–909. doi: 10.1302/0301-620X.101B8.BJJ-2019-0106.R1. [DOI] [PubMed] [Google Scholar]
- 15.Pizones J, García-Rey E. Pelvic motion the key to understanding spine-hip interaction. EFORT Open Rev. 2020;5:522–533. doi: 10.1302/2058-5241.5.200032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heckmann ND, Lieberman JR. Spinopelvic biomechanics and total hip arthroplasty: a primer for clinical practice. J Am Acad Orthop Surg. 2021;29:e888–e903. doi: 10.5435/JAAOS-D-20-00953. [DOI] [PubMed] [Google Scholar]
- 17.Lee SH, Lim CW, Choi KY, Jo S. Effect of spine-pelvis relationship in total hip arthroplasty. Hip Pelvis. 2019;31:4–10. doi: 10.5371/hp.2019.31.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jimenez AE, Fox JD, Miecznikowski K, et al. Limited lumbopelvic mobility does not influence short-term outcomes after primary hip arthroscopy: a propensity-matched controlled study. J Hip Preserv Surg. 2021;8:177–184. doi: 10.1093/jhps/hnab056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beck EC, Nwachukwu BU, Chapman R, Gowd AK, Waterman BR, Nho SJ. The influence of lumbosacral spine pathology on minimum 2-year outcome after hip arthroscopy: a nested case-control analysis. Am J Sports Med. 2020;48:403–408. doi: 10.1177/0363546519892916. [DOI] [PubMed] [Google Scholar]
- 20.Feingold JD, Heaps B, Turcan S, Swartwout E, Ranawat A. A history of spine surgery predicts a poor outcome after hip arthroscopy. J Hip Preserv Surg. 2019;6:227–233. doi: 10.1093/jhps/hnz029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heaps BM, Feingold JD, Swartwout E, et al. Lumbosacral transitional vertebrae predict inferior patient-reported outcomes after hip arthroscopy. Am J Sports Med. 2020;48:3272–3279. doi: 10.1177/0363546520961160. [DOI] [PubMed] [Google Scholar]