Abstract
Background
The rapid shift to virtual learning in response to the COVID-19 pandemic contributed to high academic stress among health profession students. High academic stress was associated with impaired psychosocial well-being and decreased academic performance.
Objectives
The purpose of this study was to assess the relationship between academic stress, anxiety, sleep disturbances, depressive symptoms, academic performance, and the moderating effect of resourcefulness among undergraduate health profession students.
Methods
This descriptive and cross-sectional study included undergraduate health profession students. The primary investigator distributed the study link to all students through the university's Central Messaging Centre, Twitter account, and WhatsApp. The study variables were measured using the Student Life Stress Inventory, the Generalized Anxiety Disorder-7 questionnaire, the Centre for Epidemiology Scale of Depression, the Pittsburgh Sleep Quality Index, and the Resourcefulness Skills Scale. Pearson R correlation and linear regression analysis were utilized for statistical analysis.
Results
Our sample included 94 undergraduate health profession students, 60 % of which were females with a mean age of 21, and the majority were nursing and medicine students. High academic stress, anxiety, sleep disturbances, depressive symptoms, and resourcefulness were reported among 50.6 %, 43 %, 79.6 %, 60.2 %, and 60 % of the participants, respectively. However, no effect of resourcefulness was found on any of the study variables. Instead, academic stress and sleep disturbances were the strongest predictors of depressive symptoms regardless of the level of resourcefulness.
Conclusion
Adequate academic support during virtual learning and tools to early detect subtle signs of high academic stress, anxiety, depression, and sleep disturbance should be routinely utilized by educational institutions. In addition, incorporating sleep hygiene and resourcefulness training in health professions education is highly indicated.
Keywords: Health professions students, Virtual learning, Resourcefulness, Depressive symptoms, Academic stress, Sleep disturbance
Introduction
Undergraduate health profession students experience academic stress during their college years which is known to be one of the primary sources of chronic stress young adults endure (Liu et al., 2019). In response to the sudden school shut down due to the COVID-19 pandemic, educational institutions were pushed to implement Emergency Remote Teaching (ERT) learning methods (Hodges et al., 2020; Mehmood et al., 2021). However, unlike courses designed for virtual learning, ERT did not consider the essential dimensions of virtual learning, such as teaching modality, instructor role, student ratio, communication methods, feedback sources, and assessment methods (Means et al., 2014). In addition, school shutdown for health profession students meant the loss of clinical training, an essential component of health professions curricula (Rose, 2020). As such, health profession students were faced with tremendous challenges related to digital literacy, access to learning resources, lack of interactivity, disturbed study and sleep routines, and unfamiliarity with virtual learning methods (Agu et al., 2021; Ghamdi et al., 2016; Li, Zou, et al., 2021; Lynn & Ward-Smith, 2021). As the school shutdown remained in effect for several months, health profession students endured exceptionally high levels of academic stress (Abdous, 2019; Loades et al., 2020).
Literature review
Academic stress is defined as the body's response to academic-related demands that exceed the adaptive capabilities of students (Wilks & Spivey, 2010). While a certain level of academic stress is essential and inevitable, chronically high academic stress was found to be associated with high anxiety, sleep disturbances (Zunhammer et al., 2014), depressive symptoms (Jayanthi et al., 2015), and decreased academic performance (Waqas et al., 2015). Academic stress was considered one of the most significant barriers to adequate academic progress (American College Health Association, 2006). While several studies examined anxiety and stress among Saudi health profession students during the pandemic, few studies have examined academic stress using specific tools to quantify the different academic-related stressors (Alsulami et al., 2018) and how COVID-19 has magnified such stressors.
Anxiety is defined as an emotion characterized by feelings of tension, worried thoughts, and physical changes such as increased blood pressure (The American Psychological Association, 2023). Studies indicated that high anxiety levels among college students were associated with lower academic performance (Ren et al., 2021). Anxiety was a highly prevalent (34.9 % to 65 %) mental health condition among Saudi college students during the COVID-19 pandemic (AlAteeq et al., 2020; Bahhawi et al., 2018; Naser et al., 2020).
About 60 % of college students suffer from a sleep disorder (Lund et al., 2010). Others reported that 27 % of all university students were at risk of at least one sleep disorder (Gaultney, 2010). Sleep disorders severely impair academic success by reducing learning skills and daytime functioning (Curcio et al., 2006). While several studies examined sleep disturbance in health profession students, few proposed specialized treatments for college students (Schlarb et al., 2017).
Depression is a disorder that can affect one's overall functioning (Liu et al., 2022) and is a highly prevalent mental health condition affecting health profession students (Zhang et al., 2022). The high academic stress health profession students experience during their years of study contributed to depressive symptoms (Haldorsen et al., 2014; Torres-Berrío et al., 2019). In many studies, depression among health profession students was associated with loss of interest, fatigue, low concentration, and impaired memory and was found to be highly associated with declined academic performance (Liu et al., 2022; Wagner et al., 2022). Few studies examined depressive symptoms related to academic stress among health profession students during COVID-19. As a result, conventional depression treatment approaches rarely target academic-related risk factors.
Studies worldwide have reported high academic stress, anxiety, sleeping disturbances, and depressive symptoms among health profession students during the COVID-19 pandemic (Cao et al., 2020; Huang & Zhao, 2020). However, protective factors such as resourcefulness can help students cope effectively with exceptionally high stress while maintaining their psychological well-being and academic performance (Martos et al., 2021). Differences in resilience can be due to differences in individual copying styles, the availability of support resources, and the skill to seek/utilize such resources, a skill referred to as resourcefulness (Zauszniewski et al., 2006). Students with high resourcefulness were found to cope effectively with stressful situations while maintaining high academic performance (Martos et al., 2021). In Saudi Arabia, no studies examined the role of resourcefulness in moderating the impact of COVID-19 on academic stress among health profession students. Exploring the magnitude of academic stress and its effect on psychological wellbeing, together with assessing resourcefulness among health profession students, can provide insights to educators and guide the design of curricula and the allocation of resources during virtual learning. Therefore, this study aimed to assess the relationship among academic stress, anxiety, sleep disturbances, depressive symptoms, academic performance, and the moderating role of resourcefulness among health profession students. In this study, we hypothesized that: H1) higher academic stress, anxiety, sleep disturbances, and depressive symptoms will be associated with lower Grade Point Average (GPA) (current), H2) high academic stress predicted high depressive symptoms, and H3) the level of resourcefulness moderates the relationship between academic stress and depressive symptoms.
Methods
Design: This was a descriptive, comparative, cross-sectional study.
Sample and sampling procedure: To be included in the study, the participant needed to be a health professions student, actively enrolled in any college at King Saud Bin Abdulaziz University for Health Sciences (KSAU-HS) in any of its campuses during the data collection period, and speaks English. Students in all academic levels were included (levels 1 through 8). Students of health professions who were not enrolled in any KSAU-HS programs or those doing their internship were excluded. KSAU-HS is a publicly funded university specializing in health professions with campuses in Riyadh, Jeddah, and Alahsaa. KSAU-HS includes Colleges of Nursing, Applied Medical Sciences, Pharmacy, Dentistry, Medicine, Public health and Informatics, and Health Sciences and Professions. The total number of undergraduate students in KSAU-HS during the academic year of 2018–2019 was estimated to be 6212 (King Saud Bin Abdulaziz University for Health Sciences Campuses, 2020). The sample size needed for this study based on power analysis using GPower was 240. Convenient sampling and snowballing strategies were used in this study. The study link was sent to all KSAU-HS students via posting the study link on the University's Twitter account and via the Central Messaging Centre and WhatsApp groups. In addition, several reminders were followed until the end of the data collection period, from June 2019 to September 2019.
Instruments: Demographic and health-related data were collected, such as age, gender, specialty, academic level, current GPA out of 5, previous GPA out of 5, monthly family income in Saudi Riyals, paternal and maternal education, and history of mental health conditions (i.e., depression, anxiety, Obsessive Compulsive Disorders (OCD), or Post-Traumatic Stress Syndrome (PTSD).
Academic stress was measured using the Student Life Stress Inventory (SSI) (Gadzella, 1994). SSI consisted of 51 items listed in nine sections indicating different types of stressors (frustrations, conflicts, pressures, changes, and self-imposed stressors) and reactions to the stressors (physiological, emotional, behavioral, and cognitive) as perceived by university students using a 5-point Likert scale (1 = Never, 2 = Seldom, 3 = Occasionally, 4 = Often and 5 = Most of the Time). The possible scores for the SSI range from 51 to 255, 77 to 166 suggest mild stress, 79 to 194 suggest moderate stress, and 110 to 238 suggest severe stress. The discriminant validity of the SSI was well established by comparing the scores of the SSI among three stress groups. Individuals in the severe stress group reported significantly higher ratings on the SSI. In addition, SSI has well-established internal consistency reliability with Cronbach's alpha of 0.76 to 0.92 (Gadzella, 1994; Gadzella et al., 2012; Gadzella & Masten, 2005). The permission to use the SSI was obtained from the author.
Anxiety was measured using the Generalized Anxiety Disorders questionnaire (GAD-7) (Spitzer et al., 2006). GAD-7 is a seven-item, self-reported anxiety questionnaire designed to assess the individual's health status during the previous two weeks using a four-point Likert scale (0 = not at all sure, 1 = several days, 2 = over half the days, 3 = nearly every day). The possible scores for GAD-7 range from 0 to 21, with high scores indicating high anxiety. Scores 5, 10, and 15 are the cutoff points for mild, moderate, and severe anxiety, respectively (Spitzer et al., 2006). The GAD-7 questionnaire has been validated as a screening tool in the general population (Swinson, 2006; Löwe et al., 2008), with Cronbach's alpha ranging from 0.79 to 0.91 (Dear et al., 2011). The GAD-7 is a publicly available tool, and permission was not required.
Sleep disturbances were measured using the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989). The PSQI measures sleep via seven domains: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction over the last month using thee points Likert scale (3= extremely inadequate sleep). Possible scores for the PSQI range from 0 to 21. Low PSQI scores indicate a healthier sleep quality. The PSQI takes 5 to 10 min to be completed. The psychometric properties of the PSQI have been well established with internal consistency reliability >0.70 (Mollayeva et al., 2016) and validity with a sensitivity of 98.7 and a specificity of 84.4 for sleep disturbances (Backhaus et al., 2002; Buysse et al., 2008). The PSQI is a publicly available tool, and permission was not required.
Depressive symptoms were measured using the Centre for Epidemiology Scale of Depression (CES-D 20) (Radloff, 1977). The CES-D is a 20-item tool assessing symptoms of depression over the past week using a four-point Likert scale ranging from 0 = rarely or none of the Time [less than one day] to 3 = most or all of the Time [5–7 days], with possible scores ranging from 0 to 60 with higher scores indicating higher depressive symptoms. The psychometric properties of the CES-D have been well established with Cronbach's α = 0.91 (Carleton et al., 2013). The CES-D is a publicly available tool, and permission was not required (American Psychological Association, 2011).
Resourcefulness was measured using the Resourcefulness Scale (RS), which is a 28-items tool that measures the frequency with which respondents use specific self-help (personal resourcefulness) and help-seeking behaviours (social resourcefulness) when facing challenging situations (Zauszniewski et al., 2006). The scale was rated on a six-point scoring system ranging from 0 (not at all like me) to 5 (very much like me). The possible scores of the RS range from 0 to 140, and high RS scores indicate high resourcefulness. The RS internal consistency reliability was supported by Cronbach's alphas of 0.83, 0.79, and 0.85 for the total scale and personal and social resourcefulness subscales, respectively (Zauszniewski & Bekhet, 2011). The permission to use the RS was obtained from the author.
English proficiency is a requirement for all health professions education in Saudi Arabia, and all health profession students speak, read, and write in English. Thus, all the tools in this study were used in their original English language.
Data collection procedures
The data were collected was conducted using a web-based survey from June 2019 to September 2019, during which schools were switched to virtual learning, and social distancing and travel-banning measures were in effect. Therefore, the data were collected during the summer when no classes were conducted. The study survey link was distributed to all KSAU-HS students via a Centralized Messaging Centre and via posting the link on the University's Twitter account and via WhatsApp, both widely used social media platforms in Saudi Arabia. The data were collected using Redcap data management software, and the data file was downloaded when the data collection period was over. The study link included an introduction to the study, the contact information of the primary investigator, and the informed consent with the Internal Review Board (IRB) committee approval number.
Statistical analysis
Statistical package for social sciences software (SPSS) was used for data analysis. Composite scores for academic stress, sleep disturbance, anxiety, depressive symptoms, and resourcefulness were used and described using means and standard deviation. The composite scores for academic stress, anxiety, sleep disturbances, depressive symptoms, and resourcefulness were then recoded categorically according to cutoffs scores as previously suggested by (Buysse et al., 2008; Gadzella et al., 2012; Radloff, 1991; Spitzer et al., 2006) and described using frequencies and percentages. Correlation analysis was done using Pearson R Product Moment Correlation to test H1, and stepwise linear regression and moderation analysis was used to test for H2 & H3.
In order to use Pearson R statistic, the data for gender, parental education, and history of depression and anxiety were dummy coded (gender: 0 = male, 1 = female; father and mother education: 0 = £ 12 years of education, 1≥ 12 years of education; and history of anxiety/depression: 0 = no, 1 = yes). Data for academic level were considered ratio data since they included more than five categories. An Independent t-test was used to compare the means of academic stress, anxiety, depressive symptoms, sleep disturbances, and resourcefulness based on demographic characteristics.
Ethical considerations
The IRB committee approved the study at King Abdullah International Medical Research Centre (KAIMRC) at KSAU-HS. No student names nor student identification numbers were collected from participants. The informed consent was signed electronically by answering yes or no to participate in the study. The study was not linked to any courses, faculty members, or programs within the University, and only those interested in participating completed the survey. There was no direct engagement between the primary investigator and the students during the data collection. Students were ensured that their participation was voluntary and would not affect their grades. When data collection was complete, the data file was uploaded from Redcap, and the author initiated the data analysis.
Results
Six hundred students agreed to participate, but only 94 provided complete data. Table 1 describes the demographic and medical sample characteristics, and Table 2 describes the sample characteristics for the main study variables.
Table 1.
Demographic and medical sample characteristics (n = 94).
| Variable | Frequency (percentages) |
|---|---|
| Gender | |
| Male | 38 (40.9 %) |
| Female | 55 (59.1 %) |
| Age | |
| M ± SD | 21.3 ± 3.1 |
| Academic year | |
| 1st | 18 (19.4 %) |
| 2nd | 21 (22.5 %) |
| 3rd | 31 (33.3 %) |
| 4th to 6th | 23 (24.7 %) |
| Specialty | |
| Dentistry | 9 (9.7 %) |
| Nursing | 24 (25.8 %) |
| Medicine | 26 (26.9 %) |
| Pharmacy | 3 (3.2 %) |
| Applied Health Sciences | 17 (18.3 %) |
| Pre-professional | 14 (15.1 %) |
| Current GPA | |
| M ± SD | 4.4 ± 0.6 |
| 0 (< 3.5) | 9 (9.7 %) |
| 1 (≥ 3.5) | 84 (90.3 %) |
| Previous GPA | |
| M ± SD | 4.2 ± 0.8 |
| 0 (< 3.5) | 11 (11.8 %) |
| 1 (≥ 3.5) | 81 (87.1 %) |
| Family Income | |
| < 10,000 SR | 18 (19.4 %) |
| 10–20,000 SR | 29 (31.2 %) |
| 20–40,000 SR | 36 (38.7 %) |
| > 40,000 SR | 10 (10.8 %) |
| Mother Education | |
| ≤ 12 years of education | 46 (49.5 %) |
| > 12 years of education | 46 (49.5 %) |
| Father Education | |
| ≤ 12 years of education |
|
| > 12 years of education | 55 (57.2 %) |
| Medical history | |
| Depression | 13 (14 %) |
| Anxiety disorders | 14 (15.1 %) |
| Oppressive Compulsive Disorders | 1 (1.1 %) |
| Medication use | 15 (16.1 %) |
Note. M = mean, SD = Standard deviation, # = frequency, SR = Saudi Riyals.
Table 2.
Sample characteristics for the main study variables (n = 94).
| A | |||||
|---|---|---|---|---|---|
| Variable | Anxiety | Academic stress | Depressive symptoms | Sleep disturbance | Resourcefulness |
| M (SD) | 9 (4.7) | 108.39 (25.6) | 21.8 (12.4) | 11.80 (7.12) | 83.68 (18.7) |
| Min-max | 0–18 | 50–164 | 0–54 | 0–27 | 0–120 |
| Skewness | 0.32 | 0.22 | 0.40 | 0.56 | −0.90 |
| Kurtosis | .49 | −0.7 | −0.6 | −0.47 | 2.9 |
| B | |||
|---|---|---|---|
| Variables |
Frequency (percentages) |
||
| Academic stress | Low (0 = <100) | Moderate (1 = 100–150) | High (2 = ≥150) |
| 46 (49.5 %) | 39 (42 %) | 8 (8.6 %) | |
| Anxiety | Low (0 ≤10) | High (1 = ≥10) | |
| 52 (56 %) | 40 (43 %) | ||
| Sleep Disturbances | High sleep quality (0 ≤ 5) | Poor sleep quality (1 = ≥5) | |
| 19 (20.4 %) | 74 (79.6 %) | ||
| Depressive symptoms | Low (0 ≤ 16) | High (1 = ≥16 | |
| 37 (40 %) | 56 (60.2 %) | ||
| Resourcefulness | Low (0 ≤ 40) | Moderate (1 = 40–80) | High (2 ≥ 80) |
| 2 (2.2 %) | 35 (37.6 %) | 55 (60 %) | |
Note. M = mean, SD = Standard deviation.
Academic stress. Most students in our sample reported mild to moderate academic stress, with a mean of 108.39 (Table 2A). To our surprise, only 8.6 % reported severe academic stress. When analyzing each item within the Student Life Stress Inventory (SSI), it was noticed that students were mostly stressed about academic overload (31 % to 34 %), taking tests (28 % to 29 %), deadlines (27 %), and too many changes at the same time (19 % to 22 %). In addition, psychosomatic symptoms of academic stress were reported, such as sweating (17 % to 19 %), stuttering (14 % to 23 %), trembling (20 to 24 %), rapid movements (15 to 20 %), exhaustion (18 to 29 %), irritable bowels or ulcer (20 %), and headache (19 %). Furthermore, high internalizing symptoms such as fear, anxiety, and worry (30 % to 31 %); anger (29 %); depression and grief (18 % to 22.6 %); and isolation (21 % to 29 %) were also reported. Fortunately, low rate of externalizing symptoms such as abusing others (5 % to 7 %), abusing self (5 % to 7 %), smoking excessively (5 to 12 %), irritability toward others (10 to 11 %), using defense mechanisms (10 to 12 %), and attempting suicide (7 to 8 %) were reported. In addition, academic stress had a high positive correlation with depressive symptoms (0.729), a moderate positive correlation with sleep disturbances (r = 0.435), anxiety (r = 0.425), history of depression (r = 0.238), anxiety (r = 0.207), and a moderate negative correlation with academic level (r = −0.238) and father education (r = −0.217) (Table 3 ).
Table 3.
Correlation analysis using Pearson R Product Moment Correlation (n = 94).
| Variables | Sleep disturbances | Academic stress | Depressive symptoms | Anxiety | GPA |
|---|---|---|---|---|---|
| Resourcefulness | −0.246* | ||||
| Academic Stress | 0.435*** | ||||
| Depressive symptoms | 0.729*** | 0.607*** | |||
| Anxiety | 0.425*** | 0.61*** | 0.627*** | ||
| Academic level | −0.238* | −0.217* | −0.23* | −0.207* | |
| Previous GPA | 0.238*** | 0.27* | 0.880** | ||
| Gender | 0.270** | 0.286** | 0.265* | ||
| History of depression | 0.238* | 0.335*** | 0.238* | −0.27$** | |
| History of anxiety | 0.207* | 0.238*** | −0.222* | ||
| Father education | −0.217* | 0.283* | 0.27* |
Note. *p .05, **p.01, ***p .001 (two-tailed).
Sleep disturbances: High sleep disturbances were reported by about 80 % of students in our sample. Bad dreams (21.5 %) and waking up frequently at night (47 %) were reported. Sleep disturbances had a moderate positive correlation with the female gender and a history of depression and anxiety.
Anxiety: High anxiety level was reported by about 43 % of the students in our sample. When examining each item of the GAD-7 scale, students reported feeling nervous and unable to control worrying (18.3 %), unable to relax almost half the days during lockdown (30 %), irritability (21.5 %), and feelings that negative things might happen reported to occur almost daily (20 %).
Depressive symptoms: The mean for depressive symptoms was 21.8, and about 60 % of our sample reported high depressive symptoms. Students reported sleep disturbances (40 %), loneliness (43 %), fear (22.6 %), poor appetite (21.5 %), difficulty concentrating (20 %), inability to fix their mood (20 %), felt everything was an effort (18 %), were easily irritated in 3–4 days during the last week (18.3 %), and 19.4 % of students reported they felt that they were as good as others only in one day of last week or less. Furthermore, only 55 % of students reported being happy and hopeful about the future on most of the weekdays. About 70 % of students felt that people were friendly only 1–2 days last week (Table 3).
Anxiety and depressive symptoms were negatively moderately correlated with academic level. On the other hand, anxiety and depressive symptoms were positively moderately correlated with previous GPA, female gender, and father education (Table 3).
Resourcefulness: Moderate resourcefulness was reported by 37 % of students reported, while high resourcefulness was reported by 60 %. Nevertheless, when examining the items of the scale separately, students seemed to rate themselves highly at self-help resourcefulness and lower at social resourcefulness. For example, when they were to do a boring task, 53 % of students indicated that they could think of the less boring parts of the job and that approaching complex tasks systematically was much like them (20 % to 35.5 %). In addition, when they were about to do an anxiety-provoking task, about 50 % of students indicated they could visualize how they would overcome the situation. Moreover, thinking about pleasant events (20 % to 24 %), keeping themselves busy (21.5 % to 34.4 %), and changing the way they think about some things (21 % to 32 %) helped when they were feeling depressed. On the other hand, when they were sad, 17 % to 26 % of students indicated that they talked to others, 17 % to 35 % asked for help from others when the students were about to make hard decisions, 31 % went to the doctor when the students felt pain, 16 % to 19.4 % asked others for help when the students were confused, 17.2 % to 23.7 % did not do what others told them to do regarding their health, 17.2 % to 24.7 % did not ask for help when the students had many things to do, 21.5 % to 32.7 % did not borrow money when the students were short, 16.1 % to 20.4 % did not talk things out when the students were angry, and 17.2 % to 19.4 % did not ask for a ride when they needed to go somewhere. It was worth noting that means for sleep disturbances, depressive symptoms, and anxiety among female students were significantly higher than those of their male counterparts (Table 4 ).
Table 4.
Mean difference (independent t-test).
| Gender | Sleep disturbance M (SD) |
Depressive symptoms M (SD) |
Anxiety M (SD) |
|---|---|---|---|
| Males | 9.5(6) | 17.5 (24) | 7.3 (4.7) |
| Females | 13.4 (7.4) | 24.7(12.7) | 10.3(5.7) |
| F | 7.179 | 8.116 | 6.785 |
| Significance | 0.009** | 0.005** | 0.011* |
Note. M = mean, SD = standard deviation. *p .05, **p .01, ***p .001 (two-tailed).
We hypothesized that higher academic stress, anxiety, depressive symptoms, and high sleep disturbances would be associated with lower current GPAs (H1). However, the current GPA did not correlate with any main study variables, which did not support H1. Only anxiety and depressive symptoms were significantly associated with previous GPAs. It was worth noting that the current GPA was only correlated with previous GPA, history of depression, and history of anxiety. We attempted to run a regression analysis to see if a history of depression and anxiety predicted the current GPA. However, when controlling for previous GPA, a history of depression and anxiety did not predict current GPA.
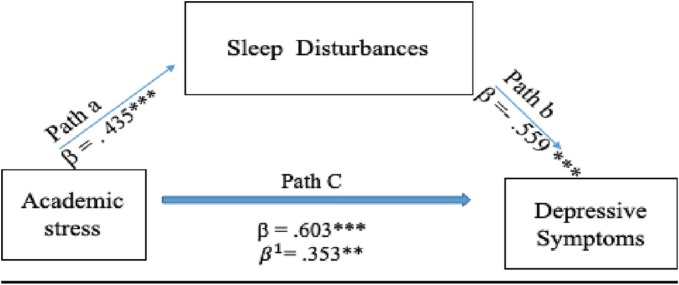
We also hypothesized that high academic stress predicted high depressive symptoms (H2) and level of resourcefulness moderated the relationship between academic stress and depressive symptoms (H3). Academic stress significantly explained 34 % of the variance in depressive symptoms (model 1), which supported H2 (Table 5 ). In model 2, sleep disturbances, resourcefulness, academic level, previous GPA, father education, and history of depression were added to the regression model which significantly explained 66 % of the variance in depressive symptoms. It was worth noting that despite being significantly correlated with depressive symptoms when controlling for academic stress and sleep disturbances, resourcefulness was not a significant predictor of depressive symptoms. In addition, adding resourcefulness to the model did not change the magnitude or the direction of the relationship between academic stress and depressive symptoms, which did not support H3. Instead, when sleep disturbances were added to the model, the regression coefficient (standardized beta) of academic stress dropped from b = 0.603 to b = 0.359 while remaining significant, which suggested a possible partial mediation effect for sleep disturbances. Mediation assumptions were all met (i.e., academic stress predicted sleep disturbances (b = 0.435***) and Fig. 1 depicts the suggested mediation effect. Despite having high resourcefulness, high sleep disturbances remained the strongest predictor of depressive symptoms, followed by academic stress.
Table 5.
Regression analysis (n = 93).
| Model summary | ||||
|---|---|---|---|---|
| Model | Adjusted R square (SE) | R square change | df1 | df2 |
| 1 | 0.33 (10) | 0.342*** | 1 | 83 |
| 2 | 0.663 (7.2) | 0.324*** | 6 | 77 |
| Regression coefficient | |||||
|---|---|---|---|---|---|
| Model | Variable | Unstand. B | Stand. beta | 95.0 % CI for B | |
| 1 | Constant | −8.46 | |||
| Academic stress | 0.279 | 0.603*** | 0.194 | 0.364 | |
| 2 | Constant | −2.845 | |||
| Academic stress | 0.168 | 0.353*** | . 081 | 0.223 | |
| Sleep quality | 0.987 | 0.559*** | 0.688 | 1.199 | |
| Resourcefulness | −0.067 | −0.099 | −0.148 | 0.015 | |
| Previous GPA | 0.071 | 0.012 | 0.453 | 11.20 | |
| Gender | 0.100 | 0.114 | −0.909 | 5.910 | |
| History of depression | −1.63 | −0.044 | −3.972 | 6.856 | |
| Father education | 0.100 | 0.059 | −1.404 | 0.713 | |
= standardized regression coefficient when controlling for the mediator, Unstand. = unstandardized, stand. = standardized, CI = confidence intervals, SE = standard deviation, df = degrees of freedom. *p .05, **p .01, ***p .001 (two-tailed).
Fig. 1.
Mediating effect of sleep disturbances between academic stress and depressive symptoms. By adding Sleep Disturbances to the regression, the association between academic stress and depressive symptoms significantly dropped but remained statistically significant. Therefore, sleep disturbances were suggested as a partial mediator. b = standardized regression coefficient when not controlling for the mediator (Beta). Note. = standardized regression coefficient when controlling for the mediator. *p.05, **p.01, ***p.001 (two-tailed).
Discussion
A cross-sectional design was used to examine the effect of academic stress during schools' shutdown and the switch to virtual learning three months after the surge of the COVID-19 pandemic on anxiety, sleep, and depressive symptoms among health profession students and the buffering effect of resourcefulness.
Overall, students in our sample reported high academic stress mainly due to high academic load (such as overlapping deadlines), unfamiliarity with assessment methods (such as online exams), and the unpredictability of the situation. High academic stress was demonstrated as high internalizing, mild externalizing, and psychosomatic symptoms. In addition, the means for anxiety and depressive symptoms were generally high in our sample. Studies before the pandemic consistently reported high academic stress, anxiety, and depression among health profession students, which have been attributed to the nature of the discipline of study (Rezaei et al., 2018; Slavin, 2016; Tung et al., 2018; Alsulami et al., 2018). However, studies conducted during the pandemic indicated higher rates of anxiety and depression among health profession students compared to rates before the pandemic (AlAteeq et al., 2020; Alshammari et al., 2022; Nakhostin-Ansari et al., 2020; Schindler et al., 2021; Mulyadi et al., 2021; Mehmood et al., 2021). The persistence of such patterns across an extended period can harm mental health, academic progress, career options (Keyes et al., 2012), and quality of life (Alici & Copur, 2021). Several factors may have contributed to the high academic stress, anxiety, and depressive symptoms in our sample. First, the strict social distancing measures coupled with the travel banning was strictly implemented in Saudi Arabia may have resulted in feelings of isolation and loneliness (Li, Zou, et al., 2021; Lynn & Ward-Smith, 2021; Agu et al., 2021). Second, as educational institutions moved from in-person to virtual learning methods in a short time, students had to face many challenges while trying to adjust to the new teaching and assessment methods, such as technology-related issues, lack of interactivity with faculty members and peers, and the lack of the immediacy of feedback which may have further contributed to feelings of isolation, frustration, and helplessness (Ghamdi et al., 2016). Third, the rapid shift to virtual learning entailed a paradigm shift where students were responsible for their learning via actively engaging with the tremendous educational resources provided to them all at once (Ghamdi et al., 2016). The factors mentioned above may have overwhelmed students with the work they had to do to succeed. Fourth, health profession students endured an additional burden related to the suspension of clinical training, which may have resulted in feelings of unpreparedness for clinical practice (Schindler et al., 2021). Moreover, the COVID-19 pandemic has caused health professions students to realize the high risk involved in working in the health field during pandemics (Bahcecioglu Turan et al., 2021), which could have amplified existing anxieties (Alshammari et al., 2022).
Similar to previous studies, the means for anxiety and depressive symptoms were significantly higher among female students than their male counterparts (Alshammari et al., 2022; Cahuas et al., 2020). As such, in addition to high academic stress, the high prevalence of anxiety and depressive symptoms in our sample may have been magnified by the characteristics of our sample, which consisted of predominantly nursing and medicine students, female students, and a high proportion of students with a history of anxiety and depression.
Most students in our sample reported high sleep disturbances consistent with previous studies during the pandemic (Dalcali et al., 2021). In addition, our sample's sleep quality was reported as poor or fair, with a high frequency of nightmares and frequent waking up at night. Many factors could have resulted in sleep disturbance during the lockdown and virtual learning, such as changes in studying and sleeping routines and the lack of structured studying time. High sleep disturbances can result in high anxiety and depressive symptoms, especially among college students. Many studies have indicated low sleep quality is strongly associated with high anxiety (Cellini et al., 2020; Xiao et al., 2020).
More than half of the students in our sample reported high resourcefulness, which can be attributed to many factors. First, despite the unfamiliarity of the situation and the uncertainty it introduced, the school shutdown was a relief from the structured school environment and the daily commute to school as it offered students more time to complete coursework at the convenience of students homes. Second, most college students in Saudi Arabia usually stay in their family homes. As such, the pandemic has fostered stronger family connections, replacing faculty and peer support and limiting feelings of isolation and helplessness among students (Mishra, 2020). Third, despite the rapid shift to virtual learning, KSAU-HS ensured clear, direct, and ongoing communication with students via several channels. As such, we expected that such an approach may have contributed to higher trust and less uncertainty which may have enhanced students' sense of resourcefulness.
Nevertheless, it was worth noting that students in our sample reported high resourcefulness mainly in the form of personal resourcefulness (i.e., cognitive strategies to help individuals cope with stress, such as cognitive reframing, problem-solving, positive self-talk, and advanced planning) rather than social resourcefulness (i.e., to help-seeking skills). One way to explain this pattern is to link it to the fact that 60 % of students in our sample were females. Previous studies have reported that female patients with chronic illness, female caregivers, and young female adults demonstrated higher personal resourcefulness than social resourcefulness (Zauszniewski et al., 2009). However, research has shown that using both types of resourcefulness was equally important and was associated with better adaptive functioning and life satisfaction (Bekhet et al., 2008; Huang et al., 2010).
Fortunately, students in our sample demonstrated high academic performance despite high academic stress, which we hypothesized to be a result of the high resourcefulness among our students, which may have minimized the impacts of high academic stress on academic performance. However, we found no correlation between current GPA, academic stress, anxiety, sleep disturbances, depressive symptoms, and resourcefulness. Our findings were inconsistent with previous studies indicating that high academic stress predicted low academic performance, while high resourcefulness predicted high academic performance among college students (Martos et al., 2021). On the other hand, we noticed that the higher their previous GPAs were, the higher the depressive symptoms and anxiety they reported. We attributed this to the fact that students with high GPAs tended to have a high sense of competition and fear of failure (Conroy & Elliot, 2004). Fear of failure was associated with high anxiety among medical students with high GPAs (Alabduljabbar et al., 2022). Moreover, GPA was not significantly different among students with and without a history of anxiety or depression, which was inconsistent with previous studies reporting a negative correlation between GPA and a history of anxiety (Nakhostin-Ansari et al., 2020). Given that our sample consisted predominantly of students with high GPAs, such a relationship would not have been apparent.
Our results indicated that high academic stress predicted high depressive symptoms, consistent with previous studies (Zhang et al., 2022). In addition, we found that despite having high resourcefulness, students with high sleep disturbances were at a higher risk for depressive symptoms due to high academic stress than those with low sleep disturbances. This finding agreed with Cahuas et al. (2020), who reported that high sleep disturbances were stronger predictors of high depressive symptoms in 1142 college students. Studies indicated that interventions targeting insomnia have helped reduce mood disorders such as depression (Baglioni et al., 2011; Yook et al., 2008). In addition, Zhang et al., 2021, Zhang et al., 2022 reported that low sleep disturbances minimized the effect of academic stress on depressive symptoms in high school students.
Implications for nursing education
Taking into consideration that health profession students may tend to underreport symptoms of depression and severe anxiety (Schindler et al., 2021; Slavin, 2016), tools to early detect subtle signs of high academic stress, anxiety, depression, and sleep disturbance should be routinely utilized by educational institutions for health professions (Mulyadi et al., 2021). Furthermore, students with alarming patterns should be referred to counselling services accordingly.
Given the vital role of sleep quality and resourcefulness skills for health profession students, educational institutions should consider designing curricula (Manning et al., 2021; Schindler et al., 2021; Wald, 2020) and support services to target personal and social resourcefulness skills and sleep quality to help students maximize their academic performance while maintaining their mental health (Cahuas et al., 2020). Moreover, students with high resourcefulness can utilize their skills in training resourcefulness to other students.
In addition, individual preferences for educational styles and level of digital literacy can have a buffering effect on academic stress during virtual education regardless of the COVID-19 pandemic (Bailey et al., 2018; Schindler et al., 2021; Li, Gillies et al., 2021). As such, it is recommended that educational institutions routinely assess students' readiness for virtual learning by assessing digital literacy, access to technology, self-learning, and time management skills (Butnaru et al., 2021) as such factors, among many others; these are essential to the success of virtual education.
Limitations and recommendations for future research
Our study offers insights to health profession educators but has some limitations that must be addressed. First, despite the high response rate we received, the sample of those who provided complete data needed to be bigger, limiting our statistical analysis's power. We attributed this to the length of the survey. As such, future studies are recommended to use shorter versions of the tools to enhance the response rate. Second, the generalizability of our findings was limited due to the inclusion of KSAU-HS students only and the high proportion of students with high GPAs in our sample. Conducting national and multi-centre studies, including a larger sample size of students from all academic performance levels, can yield more generalizable findings. Including students from different schools across the country with diverse socio-economic levels while controlling for teaching and assessment methods, digital literacy, access to technology, and preferred learning styles can help educators identify potential targets for interventions.
Conclusion
The high academic stress endured by health profession students due to the sudden shift to virtual learning during the surge of the COVID-19 pandemic has contributed to alarming rates of anxiety, sleep disturbances, and depressive symptoms. In the long run, such symptoms can lead to psychological burnout and poor academic performance. Therefore, early and routine assessment of academic stress, sleep disturbances, and depressive symptoms are highly indicated. In addition, incorporating resourcefulness and sleep hygiene training in health profession curricula can equip students with the tools needed to manage academic stress, maximize academic performance, and maintain their psychological health.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Abdous M. Influence of satisfaction and preparedness on online students' feelings of anxiety. Internet and Higher Education. 2019 [Google Scholar]
- Agu C.F., Stewart J., McFarlane-Stewart N., Rae T. COVID-19 pandemic effects on nursing education: Looking through the lens of a developing country. International Nursing Review. 2021;68(2):153–158. doi: 10.1111/inr.12663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshammari T., Alseraye S., Alqasim R., Rogowska A., Alrasheed N., Alshammari M. Examining anxiety and stress regarding virtual learning in colleges of health sciences: A cross-sectional study in the era of the COVID-19 pandemic in Saudi Arabia. Saudi Pharmaceutical Journal. 2022;30(3):256–264. doi: 10.1016/j.jsps.2022.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsulami S., Al Omar Z., Binnwejim M.S., Alhamdan F., Aldrees A., Al-Bawardi A., Alsohim M., Alhabeeb M. Perception of academic stress among health science preparatory program students in two saudi universities. Advances in Medical Education and Practice. 2018;9:159–164. doi: 10.2147/AMEP.S143151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alabduljabbar A., Almana L., Almansour A., Alshunaifi A., Alobaid N., Alothaim N., Shaik S.A. Assessment of fear of failure among medical students at King Saud University. Frontiers in Psychology. 2022;13 doi: 10.3389/fpsyg.2022.794700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alici N.K., Copur E.O. Anxiety and fear of COVID-19 among nursing students during the COVID-19 pandemic: A descriptive correlation study. Perspectives in Psychiatric Care. 2021 doi: 10.1111/ppc.12851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AlAteeq D.A., Aljhani S., Althiyabi I., Majzoub S. Mental health among healthcare providers during coronavirus disease (COVID-19) outbreak in Saudi Arabia. Journal of Infection and Public Health. 2020;13(10):1432–1437. doi: 10.1016/j.jiph.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association . 2011. Center for epidemiological studies-depression. Retrieved from Center for Epidemiological Studies Depression (CESD) (apa.org) [Google Scholar]
- American Psychological Association . 2023. Anxiety. Retrieved from anxiety (apa.org) [Google Scholar]
- American College Health Association American college health association National College Health Assessment (ACHA-NCHA) spring 2005 reference group data report (Abridged) Journal of American College Health: J of A.C.H. 2006;55(1):5–16. doi: 10.3200/JACH.55.1.5-16. [DOI] [PubMed] [Google Scholar]
- Bailey D., Lee A., Vorst T. An investigation of differences and changes in L2 writing anxiety between blended and conventional English language learning context. CALL-EJ. 2018;18(1):22–39. [Google Scholar]
- Backhaus J., Junghanns K., Broocks A., Riemann D., Hohagen F. Test-retest reliability and validity of the Pittsburgh sleep quality index in primary insomnia. Journal of Psychosomatic Research. 2002;53(3):737–740. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- Bahhawi T.A., Albasheer O.B., Makeen A.M. Depression, anxiety, and stress and their association with khat use: a cross-sectional study among Jazan University students, Saudi Arabia. Neuropsychiatr. Dis. Treat. 2018 doi: 10.2147/ndt.S182744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahcecioglu Turan G., Özer Z., Çiftçi B. Analysis of anxiety levels and attitudes of nursing students toward the nursing profession during the COVID-19 pandemic. Perspectives in Psychiatric Care. 2021;57(4):1913–1921. doi: 10.1111/ppc.12766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse D.J., Reynolds C.R., Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Buysse D.J., Hall M.L., Strollo P.J., Kamarck T.W., Owens J., Lee L., Reis E., Matthews K.A. Relationships between the Pittsburgh sleep quality index (PSQI), Epworth sleepiness scale (E.S.S.), and clinical/ polysomnographic measures in a community sample. Journal of Clinical Sleep Medicine. 2008;4(6):563–571. [PMC free article] [PubMed] [Google Scholar]
- Baglioni C., Battagliese G., Feige B., et al. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders. 2011;135(1–3):10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Butnaru G.I., Nit a., V., Anichiti A., Brînz˘a G. The effectiveness of online education during Covid-19 pandemic—A comparative analysis between the perceptions of academic students and high school students from Romania. Sustainability. 2021;13:5311. doi: 10.3390/su13095311. [DOI] [Google Scholar]
- Bekhet A., Zauszniewski J.A., Wykle M. Milieu change and relocation adjustment in elders. Western Journal of Nursing Research. 2008;30:13–29. doi: 10.1177/0193945907309309. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Thibodeau M.A., Teale M.J., Welch P.G., Abrams M.P., Robinson T., Asmundson G.J. The center for epidemiologic studies depression scale: A review with a theoretical and empirical examination of item content and factor structure. PloS one. 2013;8(3) doi: 10.1371/journal.pone.0058067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy D.E., Elliot A.J. Fear of failure and achievement goals in sport: Addressing the issue of the chicken and the egg. Anxiety, Stress, and Coping. 2004;17:271–285. doi: 10.1080/1061580042000191642. [DOI] [Google Scholar]
- Cahuas A., He Z., Zhang Z., Chen W. Relationship of physical activity and sleep with depression in college students. Journal of American College Health. 2020;68(5):557–564. doi: 10.1080/07448481.2019.1583653. https://doi-org.sdl.idm.oclc.org/10.1080/07448481.2019.1583653 [DOI] [PubMed] [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. Journal of Sleep Research. 2020;29(4) doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curcio G., Ferrara M., De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Medicine Reviews. 2006;10(5):323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Dalcali B.K., Durgun H., Tas S. Anxiety levels and sleep quality in nursing student during the COVID-19 pandemic. Perspectives in Psyhciatric Care. 2021;57(2):1999–2005. doi: 10.1111/ppc.12839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dear B.F., Titov N., Sunderland M., McMillan D., Andersin T., Lorian C., Robinson E. Psychometric comparison of the generalized anxiety disorders scale-7 and the Penn State worry questionnaire for measuring response during treatment for generalized anxiety disorders. Cognitive Behavioral Therapy. 2011;40(3):216–227. doi: 10.1080/16506073.2011.582138. [DOI] [PubMed] [Google Scholar]
- Gadzella B.M. Student-life stress inventory: Identification of and reactions to stressors. Psychological Reports. 1994;74(2):395–402. doi: 10.2466/pr0.1994.74.2.395. [DOI] [PubMed] [Google Scholar]
- Gadzella B.M., Masten W.G. An analysis of the categories in the student-life stress inventory. American Journal of Psychological Research. 2005;1(1):1–10. [Google Scholar]
- Gadzella B.M., Baloglu M., Masten W.G., Wang Q. Evaluation of the student life-stress inventory-revised. Journal of Instructional Psychology. 2012;39(2):82–91. [Google Scholar]
- Ghamdi A.S., Samarji A.N., Watt A.P. Essential considerations in distance education in K.S.A.: Teacher immediacy in a virtual teaching and learning environment. International Journal of Information and Education Technology. 2016;6:17–22. [Google Scholar]
- Gaultney J.F. The prevalence of sleep disorders in college students: Impact on academic performance. Journal of American College Health. 2010;59(2):91–97. doi: 10.1080/07448481.2010.483708. [DOI] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C.Y., Guo S.E., Hung C.M., Shih S.L., Lee L.C., Hung G.C., Huang S.M. Learned resourcefulness, quality of life, and depressive symptoms for patients with breast cancer. Oncology Nursing Forum. 2010;37(4):E280–E287. doi: 10.1188/10.ONF.E280-E287. [DOI] [PubMed] [Google Scholar]
- Hodges C., Moore S., Lockee B., Trust T., Bond A. The difference between emergency remote teaching and online learning, why IT matters to higher education. 2020. https://er.educause.edu/articles/2020/3/the-difference-betweenemergency-remote-teaching-and-online-learning Available online.
- Haldorsen H., Bak N.H., Dissing A., Petersson B. Stress and symptoms of depression among medical students at the University of Copenhagen. Scandinavian Journal of Public Health. 2014;42(1):89–95. doi: 10.1177/1403494813503055. [DOI] [PubMed] [Google Scholar]
- Jayanthi P., Thirunavukarasu M., Rajkumar R. Academic stress and depression among adolescents: A cross-sectional study. Indian Pediatrics. 2015;52:217–219. doi: 10.1007/s13312-015-0609-y. [DOI] [PubMed] [Google Scholar]
- Keyes C.L.M., Eisenberg D., Perry G.S., Dube S.R., Kroenke K., Dhingra S.S. The relationship of level of positive mental health with current mental disorders in predicting suicidal behavior and academic impairment in college students. Journal of American College Health. 2012;60(2):126–133. doi: 10.1080/07448481.2011.608393. [DOI] [PubMed] [Google Scholar]
- King Saud Bin Abdulaziz University for Health Sciences Campuses . 2020. King Saud Bin Abdulaziz University for Health Sciences Campuses.https://www.ksau-hs.edu.sa/English/AboutUs/Pages/UniversityCampuses.aspx Retrived February 14, 2023 from. [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Medical Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Li D., Zou L., Zhang Z., Zhang P., Zhang J., Fu W., Mao J., Cao S. The psychological effect of COVID-19 on home-quarantined nursing students in China. Original Research. 2021;12(373) doi: 10.3389/fpsyt.2021.652296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Gillies R., He M., Wu C., Liu S., Gong Z., Sun H. Barriers and facilitators to online medical and nursing education during the COVID-19 pandemic: Perspectives from international students from low- and middle-income countries and their teaching staff. Human Resources for Health. 2021;19(1):64. doi: 10.1186/s12960-021-00609-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X.Q., Guo Y.X., Zhang W.J., Gao W.J. Influencing factors, prediction and prevention of depression in college students: A literature review. World Journal of Psychiatry. 2022;12(7):860–873. doi: 10.5498/wjp.v12.i7.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Ping S., Gao W. Changes in undergraduate students' psychological wellbeing as they experience university life. International Journal of Environmental Research and Public Health. 2019;16:2864. doi: 10.3390/ijerph16162864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynn J.J., Ward-Smith P. Teaching during COVID-19: Perceptions of nursing faulty. Journal of Nursing Education and Practice. 2021;11(6):43. doi: 10.5430/jnep.v11n6p43. [DOI] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., Linney C., McManus M.N., Borwick C., Crawley E. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. Journal of the American Academy of Child and Adolescent Psychiatry. 2020;59(11):1218–1239. doi: 10.1016/j.jaac.2020.05.009. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund H.G., Reider B.D., Whiting A.B., Prichard J.R. Sleep patterns and predictors of disturbed sleep in a large population of college students. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2010;46(2):124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Martos T., Jagodics B., Kőrössy J., et al. Psychological resources, dropout risk and academic performance in university students – pattern-oriented analysis and prospective study of hungarian freshmen. Current Psychology. 2021 doi: 10.1007/s12144-021-02073-z. [DOI] [Google Scholar]
- Means B., Bakia M., Murphy R. Routledge; New York: 2014. Learning online: What research tells us about whether, when and how. [Google Scholar]
- Mehmood M.S., Baig W.S., Khan S.A., Khan F., Awan S.A., Babar A. Students perspectives on online medical education during lockdown as a result of the COVID-10 pandemic. Journal of Medical and Dental College, The University of Faisalabad. 2021;12(2):111–118. [Google Scholar]
- Mulyadi M., Tonapa S.I., Luneto S., Lin W.T., Lee B.O. Prevalence of mental health problems and sleep disturbances in nursing students during the COVID-19 pandemic: A systematic review and meta-analysis. Nurse Education in Practice. 2021;57 doi: 10.1016/j.nepr.2021.103228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra S. Social networks, social capital, social support and academic success in higher education: A systematic review with a special focus on 'underrepresented' students. Educational Research Review. 2020;29 [Google Scholar]
- Manning M.L., Gerolamo A.M., Marino M.A., Hanson-Zalot M.E., Pogorzelska- Maziarz M. COVID-19 vaccination readiness among nurse faculty and student nurses. Nursing Outlook. 2021;69:565–573. doi: 10.1016/j.outlook.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollayeva T., Thurairajah P., Burton K., Mollayeva S., Shapiro C.M., Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Medicine Reviews. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- Nakhostin-Ansari A., Sherafati A., Aghajani F., Khonji M.S., Aghajani R., Shahmansouri N. Depression and anxiety among Iranian medical students during COVID-19 pandemic. Iranian Journal of Psychiatry. 2020;15(3):228–235. doi: 10.18502/ijps.v15i3.3815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naser A.Y., Dahmash E.Z., Al-Rousan R., Alwafi H., Alrawashdeh H.M., Ghoul I., Abidine A., Bokhary M.A., AL-Hadithi H.T., Ali D., Abuthawabeh R., Abdelwahab G.M., Alhartani Y.J., Al Muhaisen H., Dagash A., Alyami H.S. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain and Behavior: A Cognitive Neuroscience Perspective. 2020;10(8) doi: 10.1002/brb3.1730. https://doi.org/10.1002/brb3.v10.810.1002/brb3.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Radloff L.S. The use of the Center for Epidemiological Studies of depression scale in adolescents and young adults. Journal of Youth and Adolescents. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Rezaei M., Khormali M., Akbarpour S., Sadeghniiat-Hagighi K., Shamsipour M. Sleep quality and its association with psychological distress and sleep hygiene: A cross-sectional study among pre-clinical medical students. Sleep Science. 2018;11(4):274–280. doi: 10.5935/1984-0063.20180043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323(21):2131. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- Ren Z., Xin Y., Ge J., Zhao Z., Liu D., Ho R.C.M., Ho C.S.H. Psychological impact of COVID-19 on college students after school reopening: A cross-sectional study based on machine learning. Frontiers in Psychology. 2021:12. doi: 10.3389/fpsyg.2021.641806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Schindler A.K., Polujanski S., Rotthoff T. A longitudinal investigation of mental health, perceived learning environment and burdens in a cohort of first-year german medical students' before and during the COVID-19' new normal'. B.M.C. Medical Education. 2021;21:413. doi: 10.1186/s12909-021-02798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinson R.P. The GAD-7 scale was accurate for diagnosing generalized anxiety disorder. Evidence-Based Medicine. 2006;11:184. doi: 10.1136/ebm.11.6.184. [DOI] [PubMed] [Google Scholar]
- Slavin S.J. Medical student mental health: Culture, environment, and the need for change. JAMA. 2016;316(21):2195–2196. doi: 10.1001/jama.2016.16396. [DOI] [PubMed] [Google Scholar]
- Schlarb A.A., Friedrich A., Claßen M. Sleep problems in university students - an intervention. Neuropsychiatric Disease and Treatment. 2017;13:1989–2001. doi: 10.2147/NDT.S142067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres-Berrío A., Issler O., Parise E.M., Nestler E.J. Unraveling the epigenetic landscape of depression: Focus on early life stress. Dialogues in Clinical Neuroscience. 2019;21:341–357. doi: 10.31887/DCNS.2019.21.4/enestle. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung Y.J., Lo K.K.H., Ho R.C.M., Tam W.S.W. Prevalence of depression among nursing students: A systematic review and meta-analysis. Nurse Education Today. 2018;63:119–129. doi: 10.1016/j.nedt.2018.01.009. [DOI] [PubMed] [Google Scholar]
- Wald H.S. Optimizing resilience and wellbeing for healthcare professions trainees and healthcare professionals during public health crises—practical tips for an 'integrative resilience' approach. Medical Teacher. 2020;42(7):744–755. doi: 10.1080/0142159X.2020.1768230. [DOI] [PubMed] [Google Scholar]
- Waqas A., Khan S., Sharif W., Khalid U., Ali A. Association of academic stress with sleeping difficulties in medical students of a pakistani medical school: A cross-sectional survey. PeerJ. 2015;3 doi: 10.1080/0142159X.2020.1768230. 10.7717/peerj.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner F., Wagner R., Kolanisi U. The relationship between depression symptoms and academic performance among first-year undergraduate students at a South African university: A cross-sectional study. BMC Public Health. 2022;22:2067. doi: 10.1186/s12889-022-14517-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilks S.E., Spivey C.A. Resilience in undergraduate social work students: Social support and adjustment to academic stress. Social Work Education. 2010;29(3):276–288. https://doi-org.sdl.idm.oclc.org/10.1080/02615470902912243 [Google Scholar]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in january 2020 in China. Medical Science Monitor. 2020;26 doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yook K., Lee S.H., Ryu M., Kim K.H., Choi T.K., Suh S.Y., Kim Y.W., Kim B., Kim M.Y., Kim M.J. Usefulness of mindfulness-based cognitive therapy for treating insomnia in patients with anxiety disorders: A pilot study. The Journal of Nervous and Mental Disease. 2008;196(6):501–503. doi: 10.1097/NMD.0b013e31817762ac. [DOI] [PubMed] [Google Scholar]
- Zauszniewski J.A., Lai C.Y., Tithiphontumrong S. Development and testing of the resourcefulness scale for older adults. Journal of Nursing Measurement. 2006;14:57–68. doi: 10.1891/jnum.14.1.57. [DOI] [PubMed] [Google Scholar]
- Zauszniewski J., Bekhet A.B., Suresky M.J. Effects on resilience of women family caregivers of adults with serious mental illness: The role of positive cognitions. Archives of Psychiatric Nursing. 2009;23(6):412–422. doi: 10.1016/j.apnu.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Zauszniewski J., Bekhet A.K. Measuring use of resourcefulness skills: Psychometric testing of a new scale. International Scholarly Research Network. 2011;787363:1–9. doi: 10.5402/2011/787363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Gao F., Kang Z., Zhou H., Zhang J., Li J., Yan J., Wang J., Liu H., Wu Q., Liu B. Perceived academic stress and depression: The mediation role of Mobile phone addiction and sleep quality. Frontiers in Public Health. 2022;10 doi: 10.3389/fpubh.2022.760387. https://doi-org.sdl.idm.oclc.org/10.3389/fpubh.2022.760387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Huang P., Li B., Xu W., Li W., Zhou B. The influence of interpersonal relationships on school adaptation among chinese university students during COVID-19 control period: Multiple mediating roles of social support and resilience. Journal of Affective Disorders. 2021;285:97–104. doi: 10.1016/j.jad.2021.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zunhammer M., Eichhammer P., Busch V. Sleep quality during exam stress: The role of alcohol, caffeine and nicotine. PLoS O.N.E. 2014;9 doi: 10.1371/Journal.pone.0109490. [DOI] [PMC free article] [PubMed] [Google Scholar]