Abstract
Masks have been widely recommended as a precaution against COVID-19 transmission. Several studies have shown the efficacy of masks at reducing droplet dispersion in lab settings. However, during the early phases of the pandemic, the usage of masks varied widely across countries. Using individual response data from the Imperial College London—YouGov personal measures survey, this study investigates the effect of mask use within a country on the spread of COVID-19. The survey shows that mask-wearing exhibits substantial variations across countries and over time during the pandemic’s early phase. We use a reduced form econometric model to relate population-wide variation in mask-wearing to the growth rate of confirmed COVID-19 cases. The results indicate that mask-wearing plays an important role in mitigating the spread of COVID-19. Widespread mask-wearing associates with an expected 7% (95% CI: 3.94%—9.99%) decline in the growth rate of daily active cases of COVID-19 in the country. This daily decline equates to an expected 88.5% drop in daily active cases over 30 days compared to zero percent mask-wearing, all else held equal. The decline in daily growth rate due to the combined effect of mask-wearing, reduced outdoor mobility, and non-pharmaceutical interventions averages 28.1% (95% CI: 24.2%-32%).
1. Introduction
In response to the COVID-19 pandemic, multiple countries curbed the spread of the disease by enforcing strict policy measures such as lockdowns and shelter-in-place orders [1]. The non-pharmaceutical interventions (NPIs) included closures of schools, restaurants, bars, retail outlets, and other non-essential businesses, as well as shelter-in-place policies and the prohibition of large gatherings (e.g., limited to 10 people) [2]. These institutional measures aimed to reduce the exposure of susceptible individuals to symptomatic and asymptomatic infected individuals by decreasing outdoor mobility (e.g., going out to movies, concerts, and restaurants, and assembling in large groups) and encouraging social distancing (e.g., 1m-2m physical distancing) [3, 4].
Unlike the widespread and proactive implementation of lockdowns and physical distancing measures, the usage of masks varied widely across countries. Some countries quickly adopted guidelines for mask usage (e.g., Malaysia, Singapore, Taiwan, and Thailand), while others did not recommend using face masks unless sick [5–7]. Indeed, the World Health Organization only updated its mask-wearing guidelines on June 5, 2020 [8], to recommend that “The general public should wear non-medical masks where there is widespread transmission and when physical distancing is difficult, such as on public transport, in shops or other confined or crowded environments”. Due to these changing guidelines and uneven implementations, mask-wearing varied dramatically across countries and over time during the early phases of the pandemic [9].
Multiple studies have investigated the impact of various governmental NPIs [3, 10–13] that encourage physical distancing and other restrictions. In each case, the studies find that NPIs and physical distancing reduce the transmission of COVID-19. Studies on the effectiveness of face masks [14–16] also show that face masks could contribute to the mitigation of COVID-19. However, a recent study [17] uses a randomized control trial to investigate the effect of masks. The authors find that infection with SARS-CoV-2 occurred in 1.8% of the participants in the treated group (recommended masks for three hours per day) versus 2.1% of the participants in the control group. A difference of about 17% over 60 days appears statistically insignificant. Despite this conclusion, as noted by [18], the trial in [17] points to “a likely benefit of mask-wearing to the wearer—it did not examine the wider potential benefit of the reduced spread of infection to others—and this even in a population where mask-wearing isn’t mandatory and prevalence of infection is low.” In another cluster-randomized trial study [19] conducted in rural Bangladesh, an increase from 13.3% mask-wearing in the control group to 42.3% in the treatment group over five to nine weeks resulted in an 11.6% point reduction in individuals with COVID-19-like symptoms. In addition, the interventions, government policies, individual measures, and exposures to infection due to outdoor mobility seldom act in isolation. Treating these measures in isolation could lead to under- or over-estimation of their effectiveness at reducing the spread of the disease, biasing the assessments of the measure’s impact. This study fills these gaps by investigating the association of population-wide mask-wearing with the number of COVID-19 cases concurrent with other individual and institutional measures.
In sum, because mask-wearing varied dramatically in early 2020, we restrict this study to examine the mitigating role that mask-wearing played during the early phases of the pandemic. Specifically, we expand on the current stream of research by simultaneously considering the effects of NPIs and outdoor mobility in combination with a population’s reported usage of face masks in public places in a reduced-form econometric model (see examples in [3] and [10]). Using data from 24 countries, we identify the effect of each measure by exploiting the country-wise differences in (1) the percentage of the population who report wearing a face mask in public places (YouGov Survey Data [9]), (2) outdoor mobility across multiple categories such as Parks and Transit Locations (using Google Mobility Reports [20]) and (3) the NPI implementations (using CoronaNet-Project [1]). The results re-affirm the importance of mask-wearing in combating the spread of COVID-19.
2. Methods
This study is a cross-sectional analysis of the effects of personal and governmental measures across 24 countries on mitigating COVID-19 disease spread. The data used in this study were collected from February 21, 2020 to July 8, 2020, representing 139 days of data for each country. All analysis presented in this paper uses publicly available data. Subsequently, we present the data on the three measures, namely, mask-wearing, outdoor mobility, and NPIs, and then discuss the model-based analysis.
Key variables of interest
Mask-wearing
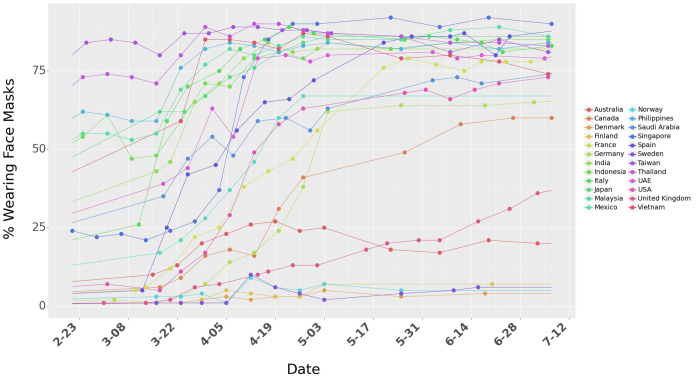
We study the impact of mask-wearing behavior using survey data across multiple countries released by the Institute of Global Health Innovation (IGHI) at Imperial College London and YouGov [9]. The survey covers 25 countries and Hong Kong (as of July 8, 2020), with around 21,000 people interviewed each week. Further details about the survey design can be found in S1 Text. We restrict our analysis to 24 countries because China and Hong Kong do not have publicly available data on outdoor mobility, which we control for in this study. The data present global insights on people’s reported behavior in response to COVID-19. The dataset provides the percentage of the population in each country who report wearing a mask in public places. Because these surveys were conducted at an interval of several days, we interpolate (linearly) to estimate the percentage of the population that would wear masks in public spaces for days when the data are unavailable (Fig 1). We use the significant variation of mask-wearing across countries to measure the association of people reporting mask-wearing to the spread of COVID-19.
Fig 1. Percentage of people who say they are wearing a face mask in public spaces.
Outdoor mobility
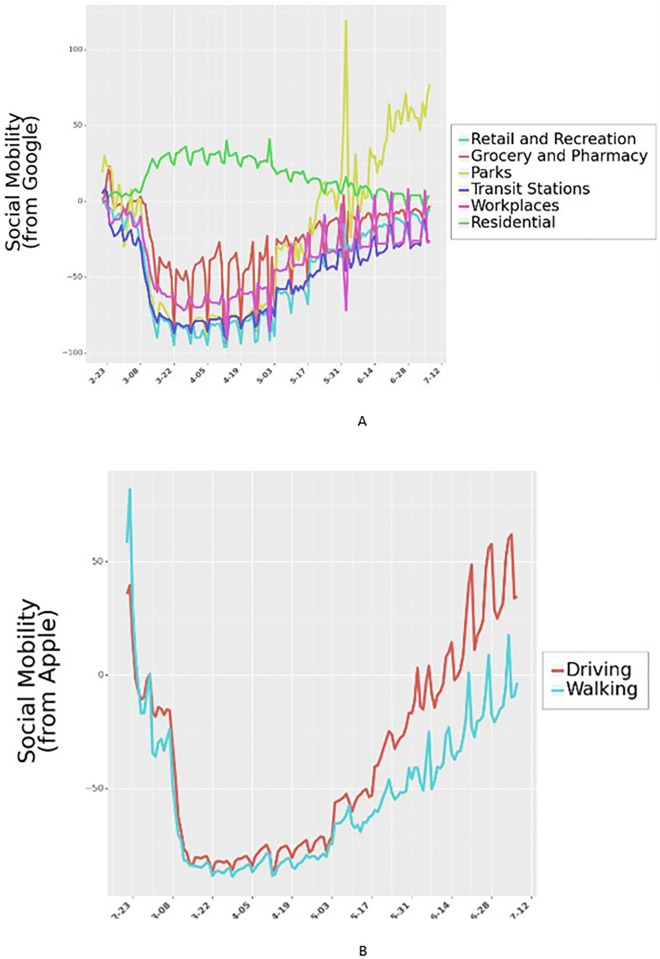
Google Community Mobility Reports provide data on relative mobility changes with respect to an internal baseline across multiple categories, namely, retail and recreation, groceries and pharmacies, parks, transit stations, workplaces, and residential (Fig 2). Table B in S1 Text shows the summary of the community mobility. Apart from the Google Mobility reports, we also utilize mobility data from Apple to test the robustness of the model to different measures of mobility. We note that neither Google nor Apple provide absolute mobility measures, but rather present relative changes to benchmarks they use internally. Finally, drops in mobility could be driven by both individual actions (e.g., cautious behavior) and institutional actions due to NPIs enacted by governments. To control for mobility declines due to institutional actions, we also include country-specific interventions enacted both nationally and provincially.
Fig 2. Outdoor mobility from Google Mobility Reports and Apple Mobility Reports for Italy.
Outdoor mobility for all 24 countries is shown in Fig H in S1 Text.
Non-pharmaceutical interventions
Governments across the 24 countries enforced different policies to control the spread of COVID-19. Prior research has shown that these policies played a significant role in reducing the human to human physical contact and led to a slowdown in the spread of the disease. However, these policies were implemented at different levels, some nationally, some provincially. We use data from the COVID-19 Government Response Event Dataset [1] to control for government policies in estimating the effect of masks. Fig J in S1 Text lists the types and counts of national and provincial government policies implemented across the 24 countries we consider in this study. The dataset contains 5,816 entries on policies at the national and provincial levels. Finally, the inclusion of these interventions helps control for some of the observed drops in mobility that are not necessarily associated with individual actions but with the presence of institutional policies. S1 Text includes the detailed information about the interventions.
Covariates
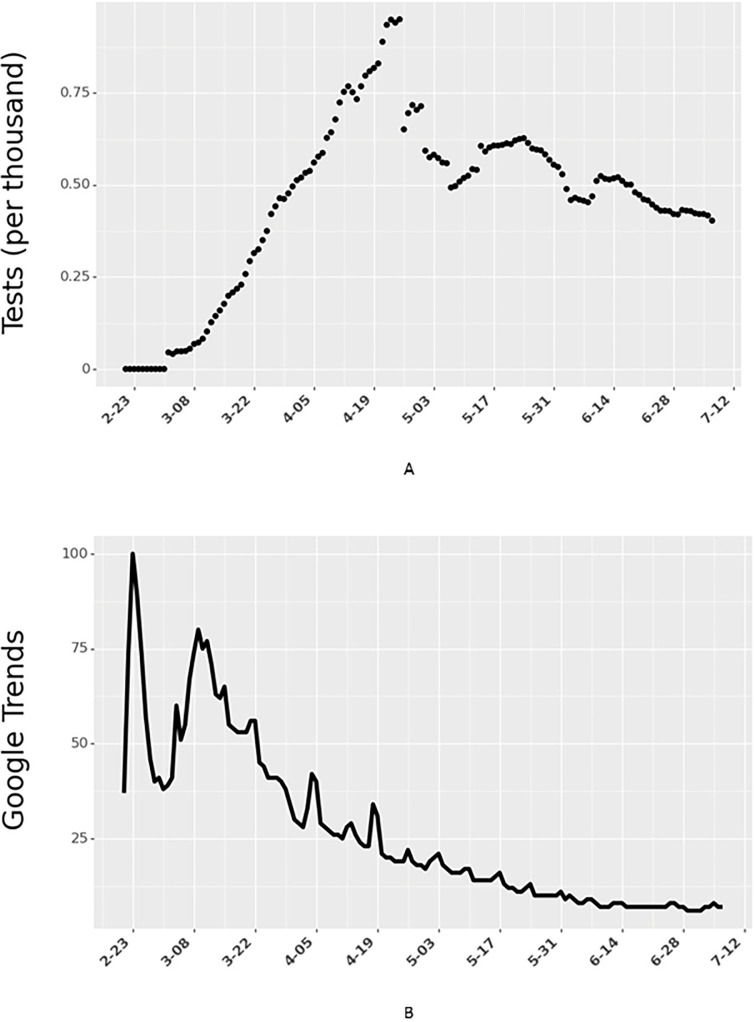
Because the data span multiple countries and weeks, we include time and country fixed effects in the model. The model controls for country-level heterogeneity using fixed-effects, where the variable for a country assumes a value of one if the data considered are specific to that country and zero otherwise. This variable allows for control of country-level characteristics that are not in the model and helps reduce the errors due to omitted variables in our analysis. In addition to country-level differences, we also control for time-based differences (e.g., people are more aware and cautious over time) by incorporating time-fixed effects, where the variable Weekt takes a value of one if the data are from week ‘t’ (where t = 1 represents the first week for a given country in the data). In addition, we control for each country’s testing capability (Fig 3A) by accounting for the country’s total number of daily tests. Finally, we also control for people’s actions to educate themselves by including the Google Trends (Fig 3B) data for the search term ‘coronavirus’.
Fig 3. Number of COVID-19 tests (per thousand people) and Google Trends for Italy.
Data for all 24 countries is shown in Figs M and N in S1 Text, respectively.
Outcome variable
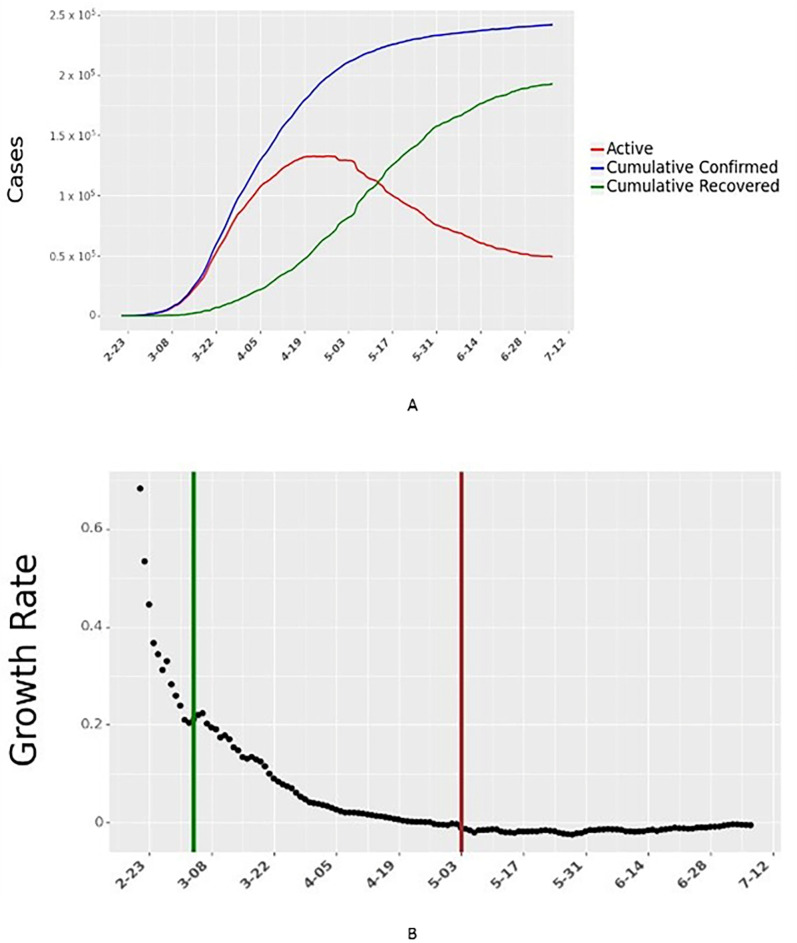
Data for the number of active daily cases in each country were obtained from the Johns Hopkins University School of Public Health [21]. We use a seven-day moving average of cumulative confirmed cases and cumulative recovered cases to compute daily active cases and daily growth rates. The daily growth rate is the ratio of active infections today to active infections the day before. The dataset aggregates this information across multiple national, state, and local health departments within each country. The daily growth rate is then related to the independent variables described earlier through a reduced-form econometric model. We describe the derivation in detail (Section S1Text). We illustrate the daily cases and growth rate for one country, Italy, in Fig 4.
Fig 4. Daily active cases and growth rate of active cases for Italy.
The vertical green line in Fig 4B shows the start of data collection for Italy. The vertical red line in Fig 4B shows the end of 60 days of data collection for Italy. Data for all 24 countries are shown in Figs F and G in S1 Text, respectively.
Analysis
We use a reduced form econometrics model to relate the growth rate of daily active infections to the independent variables described earlier. Similar models have been used by [3] to determine the effect of anti-contagion policies on the spread of COVID-19. In brief, the model assumes that the daily growth rate (ratio of active infections today to active infections the day before) is affected by institutional measures such as NPIs and individual measures such as outdoor mobility and mask-wearing. The covariates listed above help control for other factors that could affect growth over time. The method also has roots in compartmental epidemiology models—SIR (Susceptible, Infectious, Recovered). Because the epidemiological parameters for new diseases such as COVID-19 might not be well understood, reduced form techniques allow for the estimation of the impact of governmental and personal measures to help contain the spread of the virus. To filter out the high variation in growth rates when the number of cases is very low at the beginning of the pandemic, our model for each country initializes when a country reaches 20% of peak new cases, as observed by July 8, 2020. For robustness, we also test other starting times in the Supplements and find results in line with the ones presented here.
SIR growth rate model
Eqs 1–4 describe the SIR model where Sj,t, Ij,t, and Rj,t show the active susceptible, infectious, and recovered population at time t in country j. βj is the rate of transmission and γj is the rate of recovery in country j. Since we do not consider reinfection and deaths, γj can be considered as the rate of removal from infectious population. Nj is the total population of the country j. Eq 1 shows how infections spread from the infectious individuals to susceptible individuals. Eq 2 shows how the infectious population changes over time as some susceptible individuals contract the disease while some already infectious individuals recover from the disease and test negative. Eq 3 shows how the number of recovered individuals increase over time as individuals recover after testing negative for the virus. Eq 4 is a feasibility constraint which ensures that the total population is accounted for in the model. Addition of Eqs 1–3 yields Eq 4.
| (1) |
| (2) |
| (3) |
| (4) |
Since we model only the growth rate in the total confirmed cases, we consider Eq 2 in our analysis. Assuming Sj,t≈Nj (at the early stages of the pandemic), we can solve Eq 2 by integration. Details of analysis are provided in the S1 Text. If we consider daily growth rate (t2−t1 = 1), the growth rate model can be simplified as shown in Eq 5, where gj is the growth rate and it is given by βj−γj.
| (5) |
Wearing face masks, reducing social mobility, and the implementing of NPIs can alter the growth rate by changing gj. Eq 6 represents the growth rate model (P is the set of policies; M is the set of indicators of social mobility, W is the set of weeks for the duration of our analysis, and J is the set of countries in our analysis). mobilityj,t,m is the mth indicator for social mobility, weekj,t,w = 1 if day t in country j is in week w after the initialization point for country j. The starting point of analysis for each country could vary as explained earlier. ϵt is the gaussian error term in Eq 6. The rest of variables are as described earlier (and with more detail in the S1 Text).
| (6) |
The econometrics approach of using the growth rate to estimate the effects of masks, social mobility, and NPIs has several advantages. The model can estimate the effect of the exogenous independent variables on the dependent outcome variable (growth rate). Since the left-hand side of Eq 5 can be empirically calculated, it does not explicitly require the knowledge of the relationship between exogenous variables and Ij,t. Thus, the model does not need to know the link between masks, NPIs, and social mobility on daily active cases (or cumulative confirmed cases) but can still estimate their effect on the growth rate of infectious cases. Using the growth rate, Ij,t can be estimated by integrating it from time 0 (or using previous integration up to the day t−1). Thus, this model is forward-looking. The S1 Text also provide further details about the methodological approach and model formulation used in this paper.
We provide some brief notes on the operationalization of the independent variables and the model initialization below:
The growth rate model is able to handle underreporting in COVID-19. In the COVID-19 pandemic, data for an individual is recorded when only they are tested. Total confirmed cases (deaths and recovered cases) in publicly available datasets only provide information on the individuals who got themselves tested. Due to various reasons, e.g., lack of testing, lack of motivation to get tested, or lack of visible symptoms in asymptomatic cases, it is being estimated that there is a massive underreporting in total confirmed positive cases. However, the growth rate model is agnostic to underreporting as it models the first difference in the log of confirmed cases. If the underreporting is a constant proportion of the reported cases, we can multiply Ij,t and Ij,t−1 with a constant factor, and it would not affect our estimation of growth rate (Eq 5).
Responses to the survey about mask-wearing are subject to biases. For example, individuals might overestimate the efficacy of their mask or their wearing pattern. To alleviate some of these concerns, we compute the natural log of the mask-wearing variable to discount its impact on the growth rate of daily active cases. This transformation yields a curve that grows at a slower rate as the values of mask-wearing increase, thereby diminishing the impact of higher levels of mask-wearing. We also test for other functional forms (square-root and linear) and present those results (Table G in S1 Text).
Due to the high correlation across the different mobility data categories obtained from Google, we only include the categories of Mobility: Parks and Mobility: Transit Stations in the model. Because we are interested in determining the impact of mobility in general, these two mobility variables suffice in capturing the individual’s movement patterns during this time. In S1 Text, we present results including other mobility types and also run the model with Apple Mobility data in place of Google Mobility Reports.
The CoronaNet dataset from [1] collected information on all the government policies introduced by different countries across the world. They categorized the policies into 19 different policy types. We use their categorization in the model. From February 21, 2020 to July 8, 2020, we check if a policy p was implemented in a country j on the day t. If the policy was implemented, we assign a value of 1 to sj,t,p, where s represents the level of policy coverage. If the policy was introduced at a provincial level, we normalize sj,t,p by the population of the state. Because several policies were introduced simultaneously or close together, they suffered from collinearity issues. To minimize multicollinearity issues, we choose only a specific set of policies to include in the analysis; S1 Text discusses this selection mechanism.
Due to the uncertainty of the lag in COVID-19 incidences and the difficulties in detection during the early days of the disease [22, 23], similar to prior research, we tested the focal model across multiple lag periods (shift) from zero to 14 days and for different initialization thresholds (th) for each country (0% to 20% of a country’s peak daily cases by July 08, 2020). We chose the best shift and th values using a k-fold cross-validation process (k = 5). The chosen model had the highest maximum likelihood estimate of the data and the lowest prediction error. We discuss this procedure (Section S1 Text). The results presented in the next section correspond to a model with a shift of nine days and a th of 20% of peak new cases by July 08, 2020. Finally, we train the model on 1,422 daily case observations across 24 countries. These observations span from the day each country’s daily cases reached 20% of its peak to July 08, 2020. We restrict our analysis to the first 60 days after model initialization based on th. However, we test the robustness of the findings for other lengths of data. This allows for greater variation in mask usage within the data.
In the next section, we describe our results and their policy implications.
3. Results
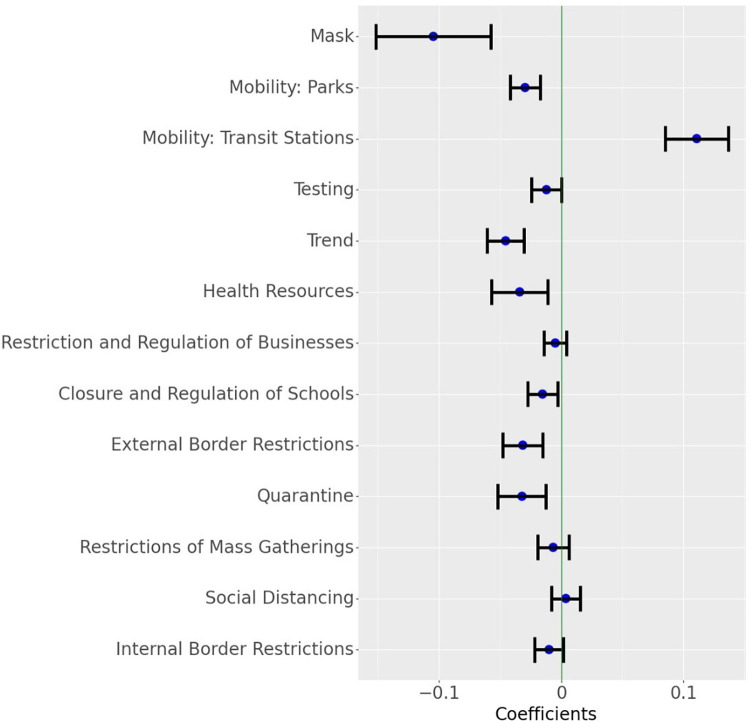
The results indicate that individual measures such as mask-wearing and outdoor mobility combined with institutional measures (NPIs) play a role in mitigating the spread of COVID-19. Fig 5 shows the estimates from the focal reduced-form model for these measures and their corresponding confidence intervals. The full table of results, along with results for all robustness checks, are provided in S1 Text. We first list the results of the key measures we consider and then discuss their implications.
Fig 5. Parameter estimates for the growth rate model.
The blue dot indicates the point estimates and the horizontal lines indicate a 95% confidence interval around the estimate (Masks transformed as ln(1+mask)). Results for different transformations of Mask and other covariates are shown in Fig Q in S1 Text.
Mask-wearing
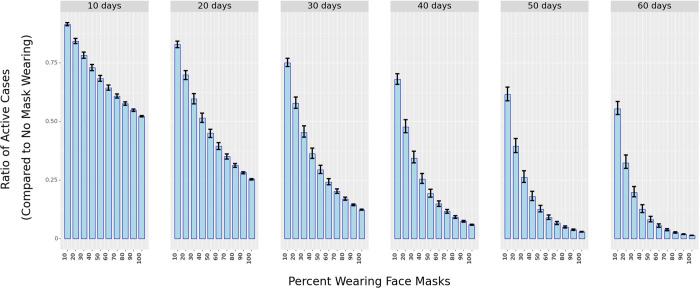
The model finds that reported mask wearing of 100% associates with an average 7% (95% CI: 3.94%—9.99%) drop in the daily growth rate of COVID-19 cases. While this daily effect appears small, 100% reported mask-wearing leads to approximately 88.5% (95% CI: 68.7%—89.2%) decline in active cases over 30 days compared to the situation where 0% of the people report wearing masks (all else remaining the same across the two scenarios). Modifying the functional form of the mask variable did not appreciably change the association. For example, in the linear model, masks are associated with an average 8.69% (95% CI: 5.63%—11.66%) drop in daily growth rate, and for the square root model, the expected daily drop in growth rate was 7.89% (95% CI: 4.81%—10.87%). The stability of the results indicates that mask-wearing plays a significant role in mitigating the spread of the disease. Fig 5 also illustrates that widespread mask-wearing, as an intervention by itself, has the most significant association (by magnitude) with the growth rate of active COVID-19 cases. Fig 6 plots the ratio of active cases under different proportions of respondents who claim to wear masks against no mask-wearing and for various periods.
Fig 6. The ratio of active cases under different percentages of mask-wearing in public spaces as compared to 0% mask-wearing over different periods (in days).
The shaded bars represent in ratio while the black vertical lines represent the 25th and 75th percentile of the ratio (from simulations using the Krinsky-Robb method).
Mobility and NPIs
As expected, the model finds that a rise in mobility links with a rise in the number of cases. Specifically, the selected mobility variables associate with a combined 8.1% (95% CI: 5.6% - 10.6%) drop in daily case numbers. Similarly, we find that the implementation of NPIs is also associated with a drop in daily growth rates across countries. After accounting for mobility declines, the NPI measures ‘Quarantine’, ‘External Border Restrictions’, and ‘Closure and Regulation of Schools’ link with the highest declines in the growth rate of daily active cases. Overall, all NPIs included in the model led to a decrease in the growth rate of COVID-19. This finding confirms multiple studies that investigated the effects of NPIs on limiting the spread of COVID-19 [10, 13, 23, 24]. Overall, we find that if the NPIs were enacted uniformly across the whole country, then the combined association of the NPIs with the decline of growth in daily cases of COVID-19 would average 13% (95% CI: 9.2% - 16.2%). We determine the combined effect using the Krinsky-Robb method, a Monte Carlo simulation used to draw samples from a multivariate normal distribution. S1 Text provides more details on this method.
Controlling for endogeneity using control functions
Due to nearly concurrent enactments and blanket coverage of policies and precautionary behaviors within countries, the individual (e.g., masks, limiting mobility) and institutional (NPIs) measures correlate in time. This precludes the causal identification of each measure’s effect on disease mitigation. In other words, because mask-wearing, mobility reductions, and NPIs occur at similar times, their effects are intertwined and difficult to determine separately. For some variables, such as mobility and NPIs, we lack the necessary data to fully control for these issues. In the case of mask-wearing, even though we cannot eliminate all the possible endogeneity issues, we attempt to alleviate some of the concerns of confounding variables by employing control functions [25]. As noted in [26], control functions make the intervention exogenous in a regression equation. To create a control function, we use mortality data for prior outbreaks of SARS, H1N1, and MERS in each country as instrumental variables to predict the proportion of mask-wearing in each country (see S1 Text for more details). We posit that exposure to prior pandemics would have resulted in a more aware populace that could be amenable to precautionary behaviors such as mask-wearing. Next, we compute the control function by determining the predicted mask-wearing residuals (computed via determining “Predicted Mask-Wearing minus Reported Mask-Wearing”), allowing for better identification of the effect of reported mask-wearing on COVID-19 case numbers.
Using this procedure, we find that if 100% of the population claimed to wear masks, then mask-wearing relates to an average 4.95% (95% CI: 2.26%—7.53%) drop in the daily growth rate of COVID-19, when compared to zero percent reported mask-wearing. Over 30 days, this translates to a 70.4% (95% CI: 62.3%—72.7%) drop in new COVID-19 cases. While we are careful to note that this estimate could still be affected by confounding variables, this result lends stronger support to the magnitude of the disease mitigation that mask-wearing in the general population provides. In summary, widespread mask-wearing leads to a significant decline in the spread of COVID-19.
Robustness checks
To help determine the accuracy and stability of the results, we run several robustness checks (see S1 Text for details):
We vary the lag period (shift) from 0 to 14 days. The results show that the estimates of the individual and institutional measures are relatively stable.
We also vary the length of time we consider in the analysis. The model considered 60 days of data for each country. We vary this to estimate the model on 35, 45, 55, 65, 75, and 85 days of data and find that the results remain stable to these variations.
We replace Google mobility data with Apple mobility data. The model estimates remain robust to this change.
We vary the functional form of how mask-wearing relates to the spread of COVID-19. The results are not statistically different in these cases.
We also test the robustness of the analysis by modifying the data using exponential smoothing. Specifically, for any day t, the focal model in Eq (1) ignores the value of the independent variables from days t-shift+1 to t (discussed in Fig A in S1 Text). In the model we use for the robustness check, we do not ignore values between t-shift and t and use exponential smoothing to average the intervening data. Finally, we also modify the interpolation method of mask-wearing data from linear (current) to quadratic. We find that the results are stable with all these modifications.
The S1 Text detail all the robustness checks and simulations as well as their results.
4. Discussion
Over the past few months, several studies have investigated the efficacy of masks at minimizing droplet dispersion [27, 28] and the potential consequences of their use [14, 29] in the general population. Although a randomized control trial on the efficacy of face mask usage appears to indicate inconclusive results in the general population [15–17] provide evidence for the benefits of face mask usage through a systematic review of the multiple observational studies and the evidence thus far. While the type of face mask, as well as the timing and length of use, can affect its efficacy, its use as a precautionary principle has been strongly advised [30]. Despite the abundant scholarly and some anecdotal evidence [31], face mask use in some countries like Sweden and the United States remains controversial [32–34]. Additionally, as observed in the data, even in countries where masks do not face similar headwinds and as support for mask usage gathers further evidence, face mask use is not as commonplace (e.g., Denmark, Norway, Sweden, Finland), even as a precautionary principle.
This study links the growth rate in active cases of COVID-19 in a country to a population’s reported wearing of face masks in public places over time. The model also includes other measures that could simultaneously impact the spread of the disease as face mask usage changes over time. After accounting for these measures and controlling for other covariates, the results indicate that reported face mask use is associated with a decline in the growth of COVID-19. More precisely, if 100% of the population claimed to wear masks, then mask-wearing is associated with an average 7% decline in the growth of daily active cases of COVID-19. This association persists across multiple robustness checks and model formulations. A decline of 7% corresponds to an 88.5% drop in the number of active cases 30 days later. Together with the other measures (mobility changes, NPIs), the combined association of individual and institutional measures on the decline in the growth rate of daily active cases of COVID-19 is 28.1% (95% CI: 24.2%-32%).
Limitations
Countries enacted multiple NPIs simultaneously. This precludes us from identifying the effectiveness of NPIs separately. Second, the mobility data provided by Google and Apple are only indicative of the relative changes from a benchmark, so their association with disease spread should be interpreted with precaution. Third, we rely on the accuracy of data collected by third parties like YouGov. Inconsistencies in testing, reporting, and recording the data could lead to errors in the results obtained. Additionally, mask types and mask-wearing patterns could vary across countries, individuals, and over time. Finally, individuals might wear masks incorrectly, might wear less effective masks, or might misreport their mask-wearing behavior. For example, using data across the US and Canada, [35] show that mask-wearing differs based on negative attitudes toward SARSCoV2 vaccination, beliefs that the threat of COVID-19 has been exaggerated, disregard for social distancing, and political conservatism. Cultural collectivism has also been shown to have a significant effect on mask usage. For example, [36] show that collective interdependence and state-level differences in collectivism were good predictors of mask usage. Similarly, using data from all US states, 27 countries and from [37] also find that culturally collectivistic regions are more likely to wear masks. These differences and limitations affect the validity of all COVID-19 population-based mask-efficacy studies.
5. Conclusions
The population-wide usage of face masks as a preventative measure against the transmission of COVID-19 varies widely across countries. Using data from 24 countries, this study finds that face mask usage associates with a decline in the growth rate of daily active cases of COVID-19. Over a 30-day period, mask-wearing associates with an 88.5% decline in the number of daily active cases. This result re-affirms the prominent importance of masks in combating the spread of COVID-19.
Supporting information
(DOCX)
Data Availability
All data and code are available here: https://github.com/ashutoshnayakIE/COVID-masks.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Cheng C, Barceló J, Hartnett AS, Kubinec R, Messerschmidt L. COVID-19 government response event dataset (CoronaNet v. 1.0). Nature Human Behaviour. 2020. Jul;4(7):756–68. doi: 10.1038/s41562-020-0909-7 [DOI] [PubMed] [Google Scholar]
- 2.Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020. May 19;323(19):1915–23. doi: 10.1001/jama.2020.6130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsiang S, Allen D, Annan-Phan S, Bell K, Bolliger I, Chong T, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020. Aug;584(7820):262–7. doi: 10.1038/s41586-020-2404-8 [DOI] [PubMed] [Google Scholar]
- 4.Benzell SG, Collis A, Nicolaides C. Rationing social contact during the COVID-19 pandemic: Transmission risk and social benefits of US locations. Proceedings of the National Academy of Sciences. 2020. Jun 30;117(26):14642–4. doi: 10.1073/pnas.2008025117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Transcript for CDC Telebriefing. [Cited 2020 September 9]. Available from: https://www.cdc.gov/media/releases/2020/t0212-cdc-telebriefing-transcript.html
- 6.[Cited 2020 September 9]. Available from: https://twitter.com/Surgeon_General/status/1233725785283932160?s=20
- 7.Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID-19 pandemic. The Lancet Respiratory Medicine. 2020. May 1;8(5):434–6. doi: 10.1016/S2213-2600(20)30134-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. (2020). Advice on the use of masks in the context of COVID-19: interim guidance, 5 June 2020 [Cited 2020 September 9]. World Health Organization. Available from: https://apps.who.int/iris/handle/10665/332293. License: CC BY-NC-SA 3.0 IGO [Google Scholar]
- 9.Personal measures taken to avoid COVID-19. [Cited 2020 September 9]. Available from: https://yougov.co.uk/topics/international/articles-reports/2020/03/17/personal-measures-taken-avoid-covid-19
- 10.Flaxman S, Mishra S, Gandy A, Unwin HJ, Mellan TA, Coupland H, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020. Aug;584(7820):257–61. doi: 10.1038/s41586-020-2405-7 [DOI] [PubMed] [Google Scholar]
- 11.Auger KA, Shah SS, Richardson T, Hartley D, Hall M, Warniment A, et al. Association between statewide school closure and COVID-19 incidence and mortality in the US. JAMA. 2020. Sep 1;324(9):859–70. doi: 10.1001/jama.2020.14348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate: Study evaluates the impact of social distancing measures on the growth rate of confirmed COVID-19 cases across the United States. Health Affairs. 2020. Jul 1;39(7):1237–46. [DOI] [PubMed] [Google Scholar]
- 13.Chang S, Pierson E, Koh PW, Gerardin J, Redbird B, Grusky D, et al. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. 2021. Jan;589(7840):82–7. doi: 10.1038/s41586-020-2923-3 [DOI] [PubMed] [Google Scholar]
- 14.Lyu W, Wehby GL. Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US: Study examines impact on COVID-19 growth rates associated with state government mandates requiring face mask use in public. Health Affairs. 2020. Aug 1;39(8):1419–25. [DOI] [PubMed] [Google Scholar]
- 15.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet. 2020. Jun 27;395(10242):1973–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, van der Westhuizen HM, et al. An evidence review of face masks against COVID-19. Proceedings of the National Academy of Sciences. 2021. Jan 26;118(4):e2014564118. doi: 10.1073/pnas.2014564118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bundgaard H, Bundgaard JS, Raaschou-Pedersen DE, von Buchwald C, Todsen T, Norsk JB, et al. Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask wearers: a randomized controlled trial. Annals of Internal Medicine. 2021. Mar;174(3):335–43. doi: 10.7326/M20-6817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abbasi K. The curious case of the Danish mask study. BMJ 2020; 371:m4586 [Google Scholar]
- 19.Abaluck J, Kwong LH, Styczynski A, Haque A, Kabir MA, Bates-Jefferys E, et al. Impact of community masking on COVID-19: A cluster-randomized trial in Bangladesh. Science. 2022. Jan 14;375(6577):eabi9069. doi: 10.1126/science.abi9069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.COVID-19 Community Mobility Reports. [Cited 2020 September 9]. Available from: https://www.google.com/covid19/mobility/
- 21.Woloshin S, Patel N, Kesselheim AS. False negative tests for SARS-CoV-2 infection—challenges and implications. New England Journal of Medicine. 2020. Aug 6;383(6):e38. doi: 10.1056/NEJMp2015897 [DOI] [PubMed] [Google Scholar]
- 22.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases. 2020. May 1;20(5):533–4. doi: 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aravindakshan A, Boehnke J, Gholami E, Nayak A. Preparing for a future COVID-19 wave: insights and limitations from a data-driven evaluation of non-pharmaceutical interventions in Germany. Scientific Reports. 2020. Nov 18;10(1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davies NG, Kucharski AJ, Eggo RM, Gimma A, Edmunds WJ, Jombart T, et al. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. The Lancet Public Health. 2020. Jul 1;5(7):e375–85. doi: 10.1016/S2468-2667(20)30133-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wooldridge JM. Control function methods in applied econometrics. Journal of Human Resources. 2015. Mar 31;50(2):420–45. [Google Scholar]
- 26.Heckman JJ, Robb R Jr. Alternative methods for evaluating the impact of interventions: An overview. Journal of Econometrics. 1985. Oct 1;30(1–2):239–67. [Google Scholar]
- 27.Bahl P, Bhattacharjee S, de Silva C, Chughtai AA, Doolan C, MacIntyre CR. Face coverings and mask to minimise droplet dispersion and aerosolisation: a video case study. Thorax. 2020. Nov 1;75(11):1024–5. doi: 10.1136/thoraxjnl-2020-215748 [DOI] [PubMed] [Google Scholar]
- 28.Riediker M, Tsai DH. Estimation of viral aerosol emissions from simulated individuals with asymptomatic to moderate coronavirus disease 2019. JAMA Network Open. 2020. Jul 1;3(7):e2013807–. doi: 10.1001/jamanetworkopen.2020.13807 [DOI] [PubMed] [Google Scholar]
- 29.Worby CJ, Chang HH. Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nature Communications. 2020. Aug 13;11(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greenhalgh T, Schmid MB, Czypionka T, Bassler D, Gruer L. Face masks for the public during the covid-19 crisis. BMJ. 2020. Apr 9;369. doi: 10.1136/bmj.m1435 [DOI] [PubMed] [Google Scholar]
- 31.Morbidity and Mortality Weekly Report (MMWR). [Cited 2020 December 1]. Available from: https://www.cdc.gov/mmwr/volumes/69/wr/mm6947e2.htm
- 32.Saey TH. Why scientists say wearing masks shouldn’t be controversial. ScienceNews. 2020. June 26 [Cioted 2020 September 9]. Available from: https://www.sciencenews.org/article/covid-19-coronavirus-why-wearing-masks-controversial [Google Scholar]
- 33.Pancevski B, Douglas J. Masks Could Help Stop Coronavirus. So Why Are They Still Controversial? WSJ. 2020. June 29 [Cited 2020 September 9]. Available from: https://www.wsj.com/articles/masks-could-help-stop-coronavirus-so-why-are-they-still-controversial-11593336601 [Google Scholar]
- 34.Vogel G. Sweden’s Gamble. Science. 2020. October 6 [Cited 2020 December 1]. Available from: https://www.sciencemag.org/news/2020/10/it-s-been-so-so-surreal-critics-sweden-s-lax-pandemic-policies-face-fierce-backlash doi: 10.1126/science.370.6513.159 [DOI] [PubMed] [Google Scholar]
- 35.Taylor S, Asmundson GJ. Negative attitudes about facemasks during the COVID-19 pandemic: The dual importance of perceived ineffectiveness and psychological reactance. PLoS One. 2021. Feb 17;16(2):e0246317. doi: 10.1371/journal.pone.0246317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kemmelmeier M, Jami WA. Mask wearing as cultural behavior: An investigation across 45 US states during the COVID-19 pandemic. Frontiers in Psychology. 2021;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lu JG, Jin P, English AS. Collectivism predicts mask use during COVID-19. Proceedings of the National Academy of Sciences. 2021. Jun 8;118(23):e2021793118. doi: 10.1073/pnas.2021793118 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All data and code are available here: https://github.com/ashutoshnayakIE/COVID-masks.