Abstract
Laparoscopic radical prostatectomy (LRP) is traditionally characterized as a technically difficult procedure with a long learning curve but it is successfully performed worldwide. The aim of this paper was to assess the initial learning curve and clinical outcomes for LRP in our center. We performed a retrospective study including 63 LRP cases, in the course of 22 months, performed by 2 urologists, with no previous LRP experience. All patients were previously assessed by a multidisciplinary team and were selected on the basis of low and intermediate risk disease attributes according to the classification of prostate cancer risk groups of the European Association of Urology. The main outcomes of follow-up are procedure duration, estimated blood loss, complications, positive surgical margins, biochemical relapse and urinary continence. The median follow-up was 19.6 months. The median procedure duration was 196.8 minutes and median blood loss 257.1 mL. Significant decrease in both outcomes was observed when comparing first and last cases in the series. There were 5 (7.9%) Clavien Dindo grade II complications. Undetectable prostate specific antigen (PSA) was observed in 59 (93.6%) patients, and fifty-five patients (87.3%) were continent. Following a methodical learning approach, LRP can be safely mastered with favorable outcomes.
Key words: Laparoscopy, Radical prostatectomy, Learning curve, Case series
Introduction
Robot-assisted radical prostatectomy (RARP) has almost reached the status of a gold standard in the treatment of localized prostate cancer (1, 2), but only in developed countries. High purchase cost, expensive maintenance and single-use instruments discourage hospitals with lower budgets, as well as the developing countries to initiate such surgical programs, despite ever present aspirations for this technology. Laparoscopic radical prostatectomy (LRP) is a less expensive, minimally invasive approach, and there is no conclusive clinical evidence supporting its inferiority to RARP (3). LRP has traditionally been associated with a long learning curve and considered a lengthy and difficult procedure without major advantages compared to open prostatectomy (4). Today, after two decades of technical refinements and technological advantages (high-definition cameras, 3D vision), LRP is performed in many urologic centers across the globe with excellent oncological and functional results (5). Our center is a high-volume center for upper urinary tract laparoscopic surgery (6), adrenalectomies (7) and retroperitoneal lymphadenectomy (8).
The aim of this paper is to report the oncological and functional outcomes and document the initial learning curve of a case series of LRP in our center where this procedure has not been routinely performed so far.
Methods
We performed a retrospective study of LRP cases. The surgeries were performed by two urologists with proficient experience in laparoscopic urological surgery, however, with minimal LRP experience since the procedure hasn’t been routinely performed so far in our center. The technique used was a standard extraperitoneal descending LRP using 5 ports (9). and the vesicourethral anastomosis was formed using two running barbed sutures. The drainage tube was placed in the Retzius space and removed when the secretion was <100mL/24hours.
Every patient with prostate cancer at our center is discussed by a multidisciplinary tumor care team proposing the optimal treatment option for each individual. Clinical staging and treatment modalities are indicated according to the classification of prostate cancer risk groups (3) given by the European Association of Urology. The risk of lymph node involvement is calculated using the Novel Briganti Nomogram (10), and for the patients with the risk >7%, we performed laparoscopic limited pelvic lymphadenectomy.
The collected preoperative data included patient demographics, preoperative PSA, clinical stage, Gleason Score and grade according to the International Society of Urological Pathology (ISUP). The preoperative prostate volume was estimated using transabdominal ultrasound. Perioperative data included mean operative time and estimated blood loss (EBL), transfusion rate, addition of lymphadenectomy and nerve sparing (NS) procedures, and the length of hospital stay. Postoperative data included catheter removal time, final pathologic stage, positive surgical margin (PSM) status and Clavien Dindo complications during the postoperative period of 30 days.
The analyzed oncological outcomes were biochemical relapse (BCR), adjuvant and salvage radiotherapy rates. The analyzed functional outcomes were continence rate defined by a number of pads/day (continent: 0-1 pads/day and mild stress incontinence (SI): 2 pads/day), and erectile disfunction (ED) rate based on the questionnaire (11) of Sexual Health Inventory for Men.
The data was obtained from hospital and outpatient records and from telephone interview with the patients during the follow-up period. The study was approved by the Ethical Review Board and conducted in compliance with the ethical principles of the Declaration of Helsinki. Data analysis and visualization was performed using descriptive statistics in Microsoft Excel.
Results
In the period from January 2020 to October 2021, we performed 63 laparoscopic radical prostatectomies. All patients had localized, low and intermediate risk prostate cancer and no contraindications for laparoscopic surgery. Demographic, preoperative and perioperative data are shown in Table 1.
Table 1. Patient demographic, preoperative and perioperative data.
| Demographic and preoperative data | |
|---|---|
| Age | Mean 62.6 years (IQR 59-68) |
| Preoperative PSA | Mean 6.75 ng/mL (IQR 4.76-7.97) |
| Prostate volume | Mean 37.8 cm3 (IQR 30-42) |
|
Preoperative clinical T stage |
|
| cT1c | N=32 (50.8%) |
| cT2a | N=10 (15.9%) |
| cT2b | N=18 (28.6%) |
| cT2c | N=3 (4.8%) |
| Preoperative biopsy report | |
| ISUP I (GS 3+3) | N=35 (55.5%) |
| ISUP II (GS 3+4) | N=24 (38.1%) |
| ISUP III (GS 4+3) | N=4 (6.4%) |
| Perioperative data | |
| Operative time (minutes) | Median 196.8 (IQR 165-225) |
| Estimated blood loss (mL) | Median 257.1 (IQR 180-300) |
| Blood transfusions | 0 |
| Hospitalization length (days) | Median 5.8 (IQR 5-6) |
| Catheter removal (days) | Median 13 (IQR 12-13) |
IQR = interquartile range; PSA = prostate specific antigen; N = number, ISUP = The International Society of Urological Pathology; GS = Gleason score
There were no conversions to open surgery, lymphadenectomy was performed in 2 (2.6%) cases, and we performed 2 (2.6%) NS procedures. Positive surgical margin rate was 23.8% for the whole group (N=15), whereas 11 patients in the pT2 group (N=54) had PSM (20.3%), 4 patients in the pT3a group (N=8) had PSM (50%) and no PSM was reported in the pT3b group (N=1). During the first 30 postoperative days, we observed 5 (7.9%) Clavien Dindo grade I complications (prolonged drainage (N=3), fever (N=1), urinary retention after catheter removal (N=1)) and 5 (7.9%) Clavien Dindo grade II complications (epididymitis & UTI (N=4), hematoma (N=1)). The median follow-up period was 19.6 months (IQR 18-24).
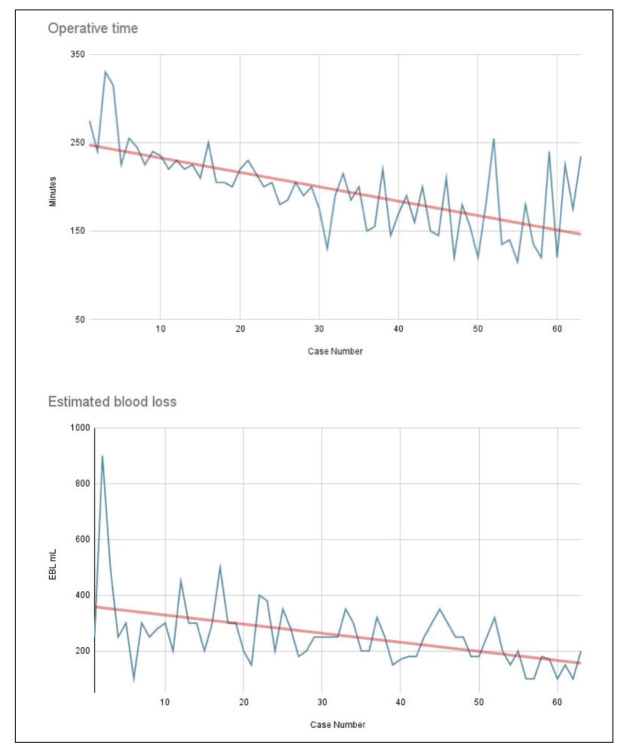
Undetectable PSA (<0.1ng/mL) was observed in 59 (93.6%) patients, 4 (6.3%) patients had biochemical relapse (PSA >0.2ng/mL) and subsequent salvage radiotherapy, while one patient (1.5%) underwent adjuvant radiotherapy. Fifty-five patients (87.3%) were continent and 7 (11.1%) reported mild SI. An artificial urinary sphincter was implanted in one (1.6%) case of severe SI. Mild ED was reported by 6 (9.6%) patients, mild to moderate ED by 2 (3.2%), moderate and severe ED by 51 (80.9%) patients, while ED data were unavailable for 4 (6.3%) patients. The operative time and estimated blood loss learning curves are displayed in Figure 1.
Figure 1.
Operative time and estimate blood loss learning curve (EBL = estimated blood loss).
Discussion
The learning curve of LRP is considered challenging, and the procedure to be the pinnacle of urologic laparoscopy. Various authors report a range of learning curves, from 38 to 250 cases (12, 13), but this depends on previous laparoscopic experience and measured outcome. The reasonable figure is proposed by Vallancien et al. (14), suggesting at least 50 operations, minimally one case/week during the first year, in order to master urological laparoscopy. We decided to highlight the operative time and estimated blood loss as the primary learning curves because this is an initial series of LRP in our center, and the proper analysis of oncological and functional learning curves requires a larger number of cases and longer follow-up period. Our operative time learning curve represents the collective curve of the whole team engaged in the procedure, including surgeons, assistants, scrub nurses and supporting staff, because such a complex procedure is definitely a team effort. Two senior urologists with >10 years of experience in urology spent two weeks observing and assisting LRP in a high-volume center in Slovenj Gradec, Slovenia, prior to starting the programe in our center. There was a significant reduction in operative time from around 250 minutes in initial cases to around 150 minutes in the last few cases in the series. Handmer et al. (15) report a decrease in mean operative time needed by the Australian urologists from 193 minutes in the first 100 cases to 163 minutes in the second 100 cases. Since we achieved a similar trend in operative time decrease after a few cases, further reduction of time can be expected with more cases. The median operative time was 196.8 minutes, which is between other reported results, such as 235 minutes by Guazzoni et al. (16) and 180 minutes by Jurczok et al. (17), but they both included lymphadenectomies more frequently.
Although LRP compared to open radical prostatectomy requires more operative time, LRP has significantly smaller EBL and transfusion rates (1). We report a median EBL of 257.1 mL and no transfusions, compared favorably to international series - EBL from 200mL (17) to 378mL (15) and transfusion rate from 0.8% (15) to 13.3% (16). The EBL learning curve depicts a clear decrease of intraoperative blood loss for the first few cases compared to the last cases. This fact, combined with a low complication rate of 15.8% (and only five (7.9%) Clavien Dindo grade II complications), allows us to state that we have established a safe LRP programme with a minimal risk of serious complications. Jurczok et al. report 9.2% (17) and Stolzenburg et al. 21% (2) of overall complications, the latter being mostly low grade.
Positive surgical margins are mostly emphasized as the oncological measure of the quality of the LRP because they are considered an adverse oncological outcome. However, they should be compared and analyzed only on the basis of a subset analysis of the pathological T2 stage and should be minimal, but in reality, the PSM rate of 15% is considered respectable (18). The rate of PSM in our series for pT2 was 20.3% (11/54), which is comparable to international series - Handmer et al. report 9.5% (15), Guillonneau et al. 15.4% (120/775) (19), Magheli et al. 17.5% (21/120) (20), and Jurczok et al. 22.9% (16/70) (17). The PSM learning curve is described to plateau after 200 cases (21).
Biochemical relapse occurred in 6.3% patients, similar to Dahl et al. 6.9% (22), but this depends on the length of the follow-up and the definition of BCR. Since we report a low incidence of salvage radiotherapy in our cohort, even though the follow-up period was relatively short, this proves the statement that “the impact of PSM on long term survival is highly variable and dependent on other risk modifiers” (23).
The continence affects the quality of life and is an important outcome but it was not reported for LRP in the recent systematic review (1). The most common method of reporting is pad usage (1). In our series with a median follow-up of 19.6 months, the continence rate was 87.3%, which is as good as 88% at 12 months reported by Good et al. (21), 85.5% at 12 months by Guillonneau et al. (24) and 90% one year after surgery reported by Salomon et al. (25), but all these reports included more patients (550, 235 and 350, respectively), and NS procedures.
The least successful outcome in our series was the erectile function, but since we performed only 2 NS procedures, it was expected. Post-prostatectomy erectile function depends on various factors that have not been investigated in this report, one of them being the ED before surgery. Every outcome has its own learning curve, and it increases with the complexity of the outcome, with the most complex outcome being erectile function. The pentafecta outcome measure includes: the biochemical recurrence, erectile function, continence, positive surgical margins and complications (26). Good et al. analyzed the combined learning curve of the pentafecta for NS LRP and concluded that the curve follows the pattern of the most complex outcome (erectile function) which continues to improve even after 250 cases (21). The erectile function at 3 and 12 months after the procedure is reported at 6.7% (2) and 52% (21), respectively, for bilateral NS procedure.
Although RARP is reported to facilitate a shorter learning curve (1), the availability has been its downside since the Da Vinci has been the only robotic system available on the market until recently. Novel robotic systems are emerging, and the one with most RARP reports is the Senhace (27, 28), with the learning curve reported for 40 procedures (28). Laparoscopic surgery isn’t a prerequisite for the DaVinci RARP, but can be a major advantage for Senhance RARP, facilitating a fast and intuitive transition from LRP to RARP (28).
Step-wise teaching protocols and formal training, as described in Brazil (29) and Australia (15), can be used to optimize and abbreviate the learning curve and effectively teach safe and successful LRP with regard to oncology. Along with the growth of the capacity of surgical technique, the perioperative outcomes are upgrading and the hospital stay getting shorter. The most advanced form of LRP today is day case surgery (30), but this approach needs specific organizational requirements regarding patient education and accommodation.
The limitations of our study are related to its design, mainly the lack of control group and randomization, and to a limited number of cases and a relatively short follow-up period, resulting in a low level of clinical evidence for reported results. Nevertheless, this case series represents a real-life initiation of a novel operative technique with favorable and safe surgical results, comparable oncological and functional outcomes. The effort behind such a project must be made at all levels: the patronage of the hospital and department leadership, the enthusiasm of surgeons and assistants, and the support of the operative room staff.
Laparoscopic radical prostatectomy has a traditional reputation of being a difficult procedure with a challenging learning curve, however, with a methodical and diligent approach, the technique can be learned appropriately to benefit the patients with prostate cancer.
References
- 1.Cao L, Yang Z, Qi L, Chen M. Robot-assisted and laparoscopic vs open radical prostatectomy in clinically localized prostate cancer: perioperative, functional, and oncological outcomes: A Systematic review and meta-analysis. Medicine (Baltimore). 2019. May;98(22):e15770. 10.1097/MD.0000000000015770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stolzenburg JU, Holze S, Neuhaus P, Kyriazis I, Do HM, Dietel A, et al. Robotic-assisted Versus Laparoscopic Surgery: Outcomes from the First Multicentre, Randomised, Patient-blinded Controlled Trial in Radical Prostatectomy (LAP-01). Eur Urol. 2021. June;79(6):750–9. Epub 2021 Feb 9. 10.1016/j.eururo.2021.01.030 [DOI] [PubMed] [Google Scholar]
- 3.Mottet N, Bellmunt J, Briers E, Bolla M, Bourke L, Cornford P, et al. members of the EAU – ESTRO – ESUR –SIOG Prostate Cancer Guidelines Panel. EAU – ESTRO – ESUR – SIOG Guidelines on Prostate Cancer. [Internet] [cited 2022 Jan 29] Available from: https://uroweb.org/guideline/prostate-cancer/
- 4.Schuessler WW, Schulam PG, Clayman RV, Kavoussi LR. Laparoscopic radical prostatectomy: initial short-term experience. Urology. 1997. December;50(6):854–7. 10.1016/S0090-4295(97)00543-8 [DOI] [PubMed] [Google Scholar]
- 5.Brassetti A, Bollens R. Laparoscopic radical prostatectomy in 2018: 20 years of worldwide experiences, experimentations, researches and refinements. Minerva Chir. 2019. February;74(1):37–53. Epub 2018 Apr 13. 10.23736/S0026-4733.18.07740-4 [DOI] [PubMed] [Google Scholar]
- 6.Knezevic N, Kulis T, Maric M, Grkovic MT, Krhen I, Kastelan Z. Laparoscopic partial nephrectomy with diode laser: a promising technique. Photomed Laser Surg. 2014. February;32(2):101–5. Epub 2014 Jan 24. 10.1089/pho.2013.3646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kulis T, Knezevic N, Pekez M, Kastelan D, Grkovic M, Kastelan Z. Laparoscopic adrenalectomy: lessons learned from 306 cases. J Laparoendosc Adv Surg Tech A. 2012. January-February;22(1):22–6. Epub 2011 Dec 13. 10.1089/lap.2011.0376 [DOI] [PubMed] [Google Scholar]
- 8.Hudolin T, Kastelan Z, Knezevic N, Goluza E, Tomas D, Coric M. Correlation between retroperitoneal lymph node size and presence of metastases in nonseminomatous germ cell tumors. Int J Surg Pathol. 2012. February;20(1):15–8. Epub 2011 Dec 16. 10.1177/1066896911431452 [DOI] [PubMed] [Google Scholar]
- 9.Stolzenburg JU, Andrikopoulos O, Kallidonis P, Kyriazis I, Do M, Liatsikos E. Evolution of endoscopic extraperitoneal radical prostatectomy (EERPE): technique and outcome. Asian J Androl. 2012. March;14(2):278–84. Epub 2011 Dec 19. 10.1038/aja.2011.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gandaglia G, Fossati N, Zaffuto E, Bandini M, Dell’Oglio P, Bravi CA, et al. Development and Internal Validation of a Novel Model to Identify the Candidates for Extended Pelvic Lymph Node Dissection in Prostate Cancer. Eur Urol. 2017. October;72(4):632–40. Epub 2017 Apr 12. 10.1016/j.eururo.2017.03.049 [DOI] [PubMed] [Google Scholar]
- 11.Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999. December;11(6):319–26. 10.1038/sj.ijir.3900472 [DOI] [PubMed] [Google Scholar]
- 12.Stolzenburg JU, Rabenalt R, Do M, Horn LC, Liatsikos EN. Modular training for residents with no prior experience with open pelvic surgery in endoscopic extraperitoneal radical prostatectomy. Eur Urol. 2006. March;49(3):491–8, discussion 499–500. Epub 2005 Dec 6. 10.1016/j.eururo.2005.10.022 [DOI] [PubMed] [Google Scholar]
- 13.Secin FP, Savage C, Abbou C, de La Taille A, Salomon L, Rassweiler J, et al. The learning curve for laparoscopic radical prostatectomy: an international multicenter study. J Urol. 2010. December;184(6):2291–6. Epub 2010 Oct 16. 10.1016/j.juro.2010.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vallancien G, Cathelineau X, Baumert H, Doublet JD, Guillonneau B. Complications of transperitoneal laparoscopic surgery in urology: review of 1,311 procedures at a single center. J Urol. 2002. July;168(1):23–6. 10.1016/S0022-5347(05)64823-9 [DOI] [PubMed] [Google Scholar]
- 15.Handmer M, Chabert C, Cohen R, Gianduzzo T, Kearns P, Moon D, et al. The Australian laparoscopic radical prostatectomy learning curve. ANZ J Surg. 2018. January;88(1-2):100–3. Epub 2017 May 16. 10.1111/ans.14025 [DOI] [PubMed] [Google Scholar]
- 16.Guazzoni G, Cestari A, Naspro R, Riva M, Centemero A, Zanoni M, et al. Intra- and peri-operative outcomes comparing radical retropubic and laparoscopic radical prostatectomy: results from a prospective, randomised, single-surgeon study. Eur Urol. 2006. July;50(1):98–104. Epub 2006 Mar 9. 10.1016/j.eururo.2006.02.051 [DOI] [PubMed] [Google Scholar]
- 17.Jurczok A, Zacharias M, Wagner S, Hamza A, Fornara P. Prospective non-randomized evaluation of four mediators of the systemic response after extraperitoneal laparoscopic and open retropubic radical prostatectomy. BJU Int. 2007. June;99(6):1461–6. 10.1111/j.1464-410X.2007.06849.x [DOI] [PubMed] [Google Scholar]
- 18.Bollens R, Sandhu S, Roumeguere T, Quackels T, Schulman C. Laparoscopic radical prostatectomy: the learning curve. Curr Opin Urol. 2005. March;15(2):79–82. 10.1097/01.mou.0000160620.28613.b1 [DOI] [PubMed] [Google Scholar]
- 19.Guillonneau B, el-Fettouh H, Baumert H, Cathelineau X, Doublet JD, Fromont G, et al. Laparoscopic radical prostatectomy: oncological evaluation after 1,000 cases at Montsouris Institute. J Urol. 2003. April;169(4):1261–6. 10.1097/01.ju.0000055141.36916.be [DOI] [PubMed] [Google Scholar]
- 20.Magheli A, Busch J, Leva N, Schrader M, Deger S, Miller K, et al. Comparison of surgical technique (open vs. laparoscopic) on pathological and long term functional outcomes following radical prostatectomy. BMC Urol. 2014. February 7;14:18. 10.1186/1471-2490-14-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Good DW, Stewart GD, Stolzenburg JU, McNeill SA. Analysis of the pentafecta learning curve for laparoscopic radical prostatectomy. World J Urol. 2014. October;32(5):1225–33. Epub 2013 Dec 11. 10.1007/s00345-013-1198-9 [DOI] [PubMed] [Google Scholar]
- 22.Dahl DM, Barry MJ, McGovern FJ, Chang Y, Walker-Corkery E, McDougal WS. A prospective study of symptom distress and return to baseline function after open versus laparoscopic radical prostatectomy. J Urol. 2009. September;182(3):956–65. Epub 2009 Jul 17. 10.1016/j.juro.2009.05.044 [DOI] [PubMed] [Google Scholar]
- 23.Yossepowitch O, Briganti A, Eastham JA, Epstein J, Graefen M, Montironi R, et al. Positive surgical margins after radical prostatectomy: a systematic review and contemporary update. Eur Urol. 2014. February;65(2):303–13. Epub 2013 Aug 3. 10.1016/j.eururo.2013.07.039 [DOI] [PubMed] [Google Scholar]
- 24.Guillonneau B, Cathelineau X, Doublet JD, Vallancien G. Laparoscopic radical prostatectomy: the lessons learned. J Endourol. 2001. May;15(4):441–5, discussion 447–8. 10.1089/089277901300189510 [DOI] [PubMed] [Google Scholar]
- 25.Salomon L, Anastasiadis AG, Katz R, De La Taille A, Saint F, Vordos D, et al. Urinary continence and erectile function: a prospective evaluation of functional results after radical laparoscopic prostatectomy. Eur Urol. 2002. October;42(4):338–43. 10.1016/S0302-2838(02)00360-3 [DOI] [PubMed] [Google Scholar]
- 26.Patel VR, Sivaraman A, Coelho RF, Chauhan S, Palmer KJ, Orvieto MA, et al. Pentafecta: a new concept for reporting outcomes of robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2011. May;59(5):702–7. Epub 2011 Jan 25. 10.1016/j.eururo.2011.01.032 [DOI] [PubMed] [Google Scholar]
- 27.Venckus R, Jasenas M, Telksnys T, Venckus M, Janusonis V, Dulskas A, et al. Robotic-assisted radical prostatectomy with the Senhance® robotic platform: single center experience. World J Urol. 2021. December;39(12):4305–10. Epub 2021 Jul 27. 10.1007/s00345-021-03792-5 [DOI] [PubMed] [Google Scholar]
- 28.Kulis T, Hudolin T, Penezic L, Zekulic T, Saic H, Knezevic N, et al. Comparison of extraperitoneal laparoscopic and extraperitoneal Senhance radical prostatectomy. Int J Med Robot. 2022. February;18(1):e2344. Epub 2021 Nov 3. 10.1002/rcs.2344 [DOI] [PubMed] [Google Scholar]
- 29.Tobias-Machado M, Pazeto CL, Neves-Neto OC, Nunes-Silva I, Zampolli HC. A Safe teaching protocol of LRP (laparoscopic radical prostatectomy). Int Braz J Urol. 2018. March-April;44(2):273–9. 10.1590/s1677-5538.ibju.2017.0137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abboudi H, Doyle P, Winkler M. Day case laparoscopic radical prostatectomy. Arch Ital Urol Androl. 2017. October 3;89(3):182–5. 10.4081/aiua.2017.3.182 [DOI] [PubMed] [Google Scholar]