Abstract
Purpose:
Children with hearing loss (CHL) are considered at risk for listening-related fatigue and its negative consequences. We collected data via focus groups and interviews from three stakeholder groups—CHL, their parents, and teachers/school professionals—in order to define the construct of listening-related fatigue from the perspective of CHL and key stakeholders. This is an important first step in our long-term goal to construct and validate a measure (i.e., scale) of listening-related fatigue for the pediatric population, with a focus on CHL. This article provides an overview of the data gathering process, analysis of qualitative reports, and the development of a theoretical framework for understanding the experience of listening-related fatigue in CHL.
Method:
We conducted focus groups and interviews in school-age children exhibiting bilateral, moderate-to-profound hearing loss (n = 43), their parents (n = 17), and school professionals who work with CHL (n = 28). The discussions were audio-recorded, transcribed, and coded using a hierarchical coding system. Qualitative analysis was conducted using an iterative inductive–deductive approach.
Results:
We identified primary themes from the focus group/interview discussions to develop a theoretical framework of listening-related fatigue in CHL. The framework demonstrates the complex interaction among situational determinants that impact fatigue, symptoms or manifestations of fatigue, and the utilization of, and barriers to, coping strategies to reduce listening-related fatigue.
Conclusions:
Participant discussion suggests that listening-related fatigue is a significant problem for many, but not all, CHL. Qualitative data obtained from these stakeholder groups help define the construct and provide a framework for better understanding listening-related fatigue in children.
Subjective fatigue can be defined as a mood state associated with feelings of weariness, extreme tiredness, a lack of energy, and/or lack of motivation to continue on with a task (Aaronson et al., 1999; Hockey, 2013; Hornsby et al., 2016; Tiesinga et al., 1996). Feelings of fatigue often develop in response to sustained application of mental or physical effort (see Davis et al., 2020, and Hornsby & Kipp, 2016, for review). Research suggests that when the fatigue is severe and recurrent, as is common in some chronic health conditions (e.g., cancer, diabetes, multiple sclerosis), it can have significant negative social, emotional, and cognitive effects that impact quality of life (Curt, 2000; Evans & Wickstrom, 1999; Flechtner & Bottomley, 2003; Hardy & Studenski, 2010). Adults in a fatigued state demonstrate degraded attention/concentration and reduced cognitive processing speed, which can impair decision-making abilities (Bryant et al., 2004; DeLuca, 2005; van der Linden et al., 2003). Likewise, severe fatigue in older adults is associated with reduced social activity and increased depression (Amato et al., 2001; Eddy & Cruz, 2007; Johnson, 2005). Research in children with other chronic health conditions suggests a similar negative impact of fatigue. Severe fatigue in children and adolescents is associated with an increase in school absences and stress, a decrement in academic performance, and negative effects on quality of life (Bess & Hornsby, 2014; Elena Garralda & Rangel, 2004). In addition, childhood fatigue may have long-term effects, as it is considered a risk factor for developing mental and emotional disorders in adulthood (Fukuda et al., 2010).
A growing body of research supports the hypothesis that, compared to adults without hearing loss, adults with hearing loss (AHL) are more likely to experience significant fatigue, specifically listening-related fatigue (Alhanbali et al., 2017; Davis et al., 2020; Dwyer et al., 2019; Hornsby & Kipp, 2016; Pichora-Fuller et al., 2016). Listening-related fatigue is a type of fatigue associated with the application of effort during listening tasks (Davis et al., 2020; Pichora-Fuller et al., 2016). In other words, listening in challenging situations requires individuals with hearing loss to allocate additional cognitive resources to auditory tasks in order to understand speech (Bess et al., 2020; McGarrigle et al., 2019; Pichora-Fuller et al., 2016). For children with hearing loss (CHL), the high level of listening effort required to remain engaged and attentive may increase their risk for developing listening-related fatigue. The modern-day classroom, with fast-paced instruction, use of multimedia, and small group interactions, can be mentally challenging for all children—but especially for CHL who, in addition to reduced audibility, may also present with language delays (Camarata et al., 2018; Tomblin et al., 2015) or other disabilities (Gallaudet Research Institute, 2014) that have the potential to affect their ability to process spoken language. Comorbid disabilities, such as a language delay, may require additional cognitive effort, resulting in a compound effect on the child's fatigue levels while listening. Anecdotal reports by parents and school professionals have reported the effects of fatigue on children and students with HL. Additionally, recent studies clearly show that, compared to children without HL, CHL (a) expend more mental effort (i.e., listening effort) when processing speech in noise (Hicks & Tharpe, 2002; Howard et al., 2010; Lewis et al., 2016; McGarrigle et al., 2019; Prodi et al., 2019); (b) are 2–2.5 times more likely to experience moderate-to-severe listening-related fatigue (Bess et al., 2020); and, (c) exhibit greater signs of stress as characterized by elevated salivary cortisol levels in the early morning (Bess et al., 2016).
Few studies have focused on the subjective perspectives of listening-related fatigue in CHL. One method for identifying patient self-perceptions of health-related problems is through the use of patient reported outcome measures. There are several standardized measures designed to assess subjective fatigue (Thayer, 1986; Whitehead, 2009); however, none thus far have been designed to specifically measure listening-related fatigue in CHL (Hornsby et al., 2017). Some studies utilizing generic fatigue scales with AHL and CHL have revealed variable findings, suggesting that such scales may not target or be sensitive enough to capture the unique problems that listening-related fatigue creates for those with HL (Alhanbali et al., 2017; Dwyer et al., 2019; Hornsby & Kipp, 2016; Hornsby et al., 2017). For example, Hornsby et al. (2017) collected subjective data from CHL (n = 60), children with no hearing loss (n = 43), and their parents using a generic fatigue scale—the Pediatric Quality of Life Inventory Multidimensional Fatigue Scale (PedsQl-MFS; Varni et al., 2002). The scale assesses three domains of fatigue (general, sleep/rest, and cognitive fatigue) yielding three subscale scores and an overall (total) fatigue score. Findings revealed that while CHL reported more fatigue than control groups, groups differences were relatively small compared to prior work (Hornsby et al., 2014). Importantly, a comparison of the fatigue reported by the CHL to that of children with other chronic health conditions for whom fatigue is a primary complaint (e.g., cancer, multiple sclerosis) revealed that CHL experienced fatigue that was comparable to, or greater than, these other groups. The finding that hearing loss increased the likelihood of severe fatigue, and thus, its potential negative effects, is consistent with other work in adults (Hornsby & Kipp, 2016) and children (Bess et al., 2020).
Although significant effects of hearing loss were reported, Hornsby et al. (2017) noted that between-group differences in some domains on the PedsQl-MFS (general and sleep/rest fatigue) were relatively small, particularly when compared to previous findings (Hornsby et al., 2014). The exact cause for the discrepancy was unclear, but the authors speculated that utilizing a generic fatigue scale, lacking items that specifically assessed listening-related fatigue, could have contributed to the results (see Hornsby et al., 2017, for details). Dwyer et al. (2019), using generic (nonspecific) fatigue and vigor scales, also found no significant differences between young adults with severe-to-profound hearing loss and an age-matched control group, supporting this conclusion. In contrast to the results for generic fatigue items, when using questions that asked specifically about fatigue associated with listening difficulties, Dwyer et al. (2019) found large and significant differences—with the AHL reporting more fatigue-related problems. These findings, and others, suggest that generic fatigue scales may not be optimal for detecting and quantifying listening-related fatigue associated with hearing loss (see Davis et al., 2020, for additional discussion) and underscore the need for a targeted scale for children. A first step in the process of developing a scale targeting listening-related fatigue is to understand the construct from the perspective of those most affected—CHL and their adult proxy-reporters (e.g., parents and school professionals).
Using focus groups and interviews to obtain insight from the patients' perspective has become increasingly common among health care researchers, including researchers in audiology, who are interested in developing high-quality scales with good content validity (Hoffman et al., 2019; Hughes et al., 2018; Knudsen et al., 2012; Peterson-Sweeney, 2005; Pope et al., 2002). For example, Davis et al. (2020) obtained qualitative data via focus groups in AHL to further understand their experiences with listening-related fatigue. Qualitative data analysis and review led to the development of a theoretical framework for listening-related fatigue in AHL (see Figure 1 in Davis et al., 2020). The framework suggests listening-related fatigue in AHL is a complex construct that includes physical, cognitive, social, and emotional experiences. The experiences of AHL were moderated by several external (e.g., background noise, speaker characteristics) and internal factors (e.g., motivation to listen, perceived effort to listen). In addition, the framework underscored the importance of coping strategies utilized by AHL to ameliorate or avoid fatigue resulting from effortful listening. The authors suggested that listening-related fatigue associated with hearing loss in adults was well modeled by the Motivation Control Theory of Fatigue (Hockey, 2013). Briefly, the model suggests that feelings of fatigue, under certain conditions, are a direct result of the sustained application of effort toward achievement of a task or goal (e.g., understand a concept by listening intently to teacher). An underlying assumption is that feelings of fatigue act as a protective mechanism. Unpleasant feelings of tiredness, or the reduced desire to continue on a task, essentially force the individual to review whether the effort being applied toward achieving a goal is worth the potential reward if attained. A variety of factors play a role in determining the development and severity of fatigue (e.g., the difficulty, duration, and effort required to achieve the goal, individual motivation and reward, control over task activities while achieving the goal). All things being equal, increasing applied effort generally increases the likelihood that fatigue will develop. Given that hearing loss is often associated with a need for increased effort on listening tasks, listening-related fatigue would be expected to be especially problematic for both AHL and CHL. We hypothesize that listening-related fatigue in CHL could also be explained by this model (Hockey, 2013); however, CHL may experience and describe fatigue somewhat differently given their unique listening situations and motivations, as well as differences in their developmental, cognitive, and language abilities compared to adults.
Figure 1.
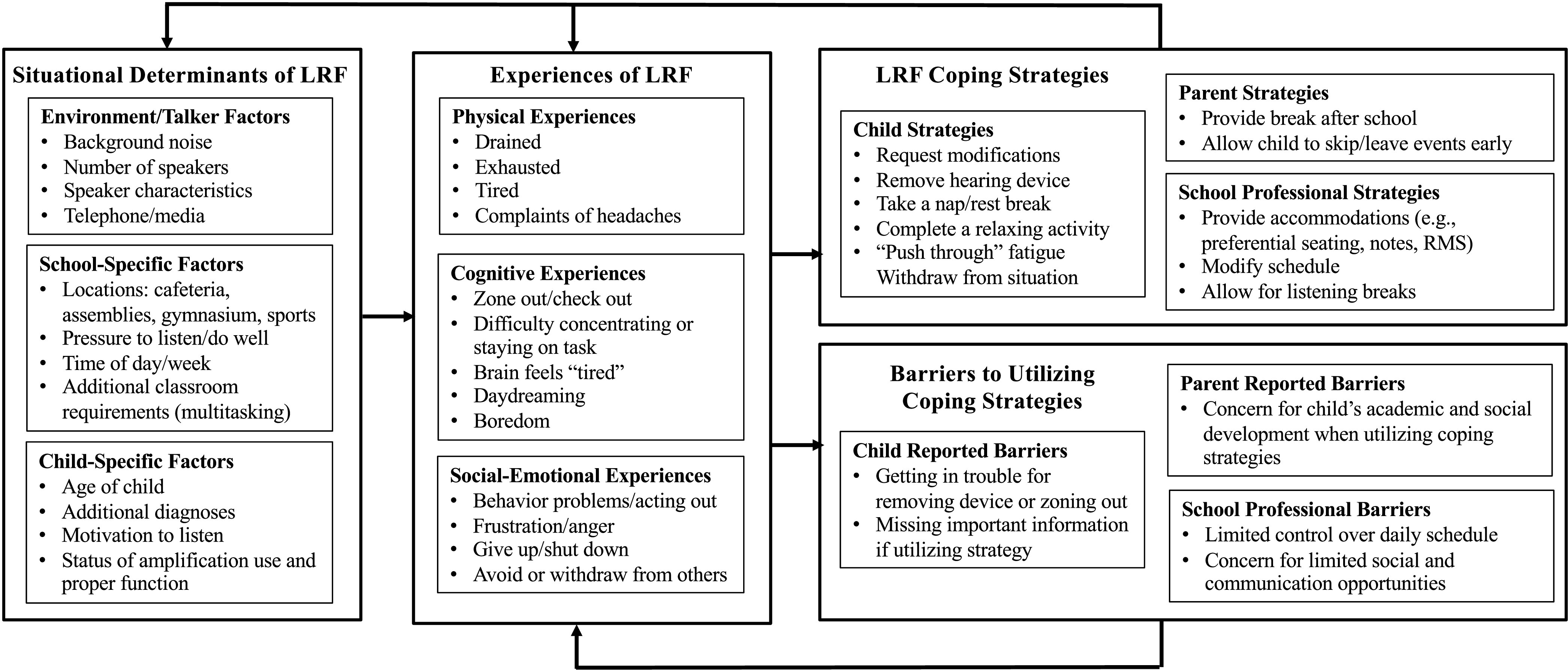
Theoretical framework of listening-related fatigue (LRF) in children with hearing loss. RMS = remote microphone system.
Research in the adult population (Davis et al., 2020) and our own clinical experiences suggest that listening-related fatigue in CHL may be diverse and that current, generic, fatigue scales are not optimal for quantifying the problem of listening-related fatigue in CHL. We believe a measure specifically designed to target listening-related fatigue will be of clinical and educational importance and best serve the needs of CHL. Thus, our long-term goal is to construct and validate a suite of fatigue measures specific to hearing loss in the pediatric population (referred to as the Vanderbilt Fatigue Scales). As a first step toward this goal, data regarding the construct of listening-related fatigue were collected via focus groups and interviews from three stakeholder groups (CHL, their parents, and their teachers/school professionals). This article describes the focus group and interview process, qualitative data analysis, and the integration of our results into a theoretical framework for describing listening-related fatigue in CHL.
Method
This study was reviewed and approved by the Vanderbilt Institutional Review Board (IRB#150769). All participants provided informed consent or assent prior to participation and were compensated for their time.
Focus Group Participants
A total of 88 individuals participated in a focus group or interview. Participants from three target groups were recruited, including (a) CHL (n = 43), (b) parents of CHL (n = 17), and (c) teachers and school professionals who work with CHL (n = 28). The child participants group had bilateral, moderate-to-profound hearing loss and ranged in age from 7 to 17 years (M = 12.4 years). Based on parental report, 19 of the 43 child participants (44%) had an additional disability/diagnosis (e.g., speech-language delay, cerebral palsy, attention deficit/hyperactivity disorder. Additional demographic information concerning these children is detailed in Table 1.
Table 1.
Demographics of child participants in focus groups and interviews.
| Characteristic | n = 43 |
|---|---|
| Gender | |
| Male | 22 (51%) |
| Female | 21 (49%) |
| Age group (in years) | |
| 7–9 | 4 (9%) |
| 10–12 | 20 (47%) |
| 13–17 | 19 (44%) |
| Mean age (years) | 12.4 (SD = 2.6) |
| Race/Ethnicity | |
| Asian | 3 (7%) |
| African American | 12 (28%) |
| White | 24 (56%) |
| Other | 4 (9%) |
| Device type | |
| Hearing aids | 18 (28%) |
| Bone-anchored devices | 4 (9%) |
| Cochlear implants | 10 (23%) |
| Bimodal | 10 (23%) |
| No device | 1 (2%) |
| Additional diagnosis (AD) | |
| Yes, one AD | 10 (23%) |
| Yes, more than one AD | 9 (21%) |
| No | 24 (56%) |
| Classroom type | |
| General education | 26 (61%) |
| General education with pullout classes | 6 (14%) |
| School for deaf and hard of hearing | 7 (16%) |
| Homeschooled | 4 (9%) |
| Repeated a grade | |
| Yes | 11 (26%) |
| No | 31 (72%) |
| Unknown | 1 (2%) |
| Mode of communication | |
| Oral | 33 (77%) |
| Total communication | 8 (19%) |
| Other/not indicated | 2 (4%) |
Child and parents were recruited through the Vanderbilt Bill Wilkerson audiology clinic via phone or in person during a clinical appointment. A small group of CHL were recruited through a local school for CHL (n = 7). A CHL could participate even if their parent did not (n = 31); conversely, some parents participated even if their child did not (n = 7). During the recruitment and consenting process, parents confirmed that their child was able to communicate orally in a group situation. Twenty-eight school professionals (e.g., speech-language pathologists, teachers of the deaf/hard of hearing, general educators, etc.) participated in the study. Potential participants were contacted via e-mail after approval was obtained from the participating school districts. Additional information about the adult-proxy reporters (i.e., parents and school professionals) can be found in Table 2.
Table 2.
Demographics of adult proxies (school professionals and parents) in focus groups and interviews.
| School professionals | n = 28 | Parents | n = 17 |
|---|---|---|---|
| Gender | Gender | ||
| Male | 0 (0%) | Male | 4 (24%) |
| Female | 28 (100%) | Female | 13 (76%) |
| Education | Education | ||
| Some high school/GED | 0 (0%) | Some high school/GED | 3 (18%) |
| Some college/postsecondary | 0 (0%) | Some college/postsecondary | 8 (46%) |
| Bachelor's degree | 9 (32%) | Associate's or bachelor's | 3 (18%) |
| Master's degree | 19 (64%) | Graduate or professional | 3 (18%) |
| Job title | |||
| SLP | 9 (32%) | ||
| General educator | 6 (21%) | ||
| Special educator | 1 (4%) | ||
| Teacher of deaf | 10 (36%) | ||
| Other | 2 (7%) | ||
| Years in profession | |||
| 2–5 years | 10 (36%) | ||
| 6–14 years | 9 (32%) | ||
| 15–24 years | 5 (18%) | ||
| 25 or more years | 4 (14%) | ||
| Years working with CHL | |||
| 2–5 years | 10 (36%) | ||
| 6–14 years | 8 (28%) | ||
| 15–24 years | 5 (18%) | ||
| 25 or more years | 4 (14%) | ||
| Did not disclose | 1 (4%) |
Note. GED = General Educational Development; SLP = speech-language pathologist; CHL = children with hearing loss.
A convenience sampling approach was used to recruit parents and school professionals based on practical criteria, including geographical proximity to focus group locations and availability at scheduled group times (Etikan, 2016). A stratified (by age) purposeful sampling technique was utilized for pediatric recruitment to ensure only children with specific degrees of hearing loss and age ranges were included. Additional participant factors, such as gender, socioeconomic status, education, and ethnicity, could not be feasibly utilized for stratification purposes due to participant scheduling limitations. All participants were native English speakers.
Data Collection
Participation required a single study visit. Separate focus groups were held for each participant type (e.g., CHL, parents of CHL, school professionals working with CHL). Participants were seated for optimal access to visual cues during discussions and CHL wore their prescribed hearing devices (i.e., hearing aids, cochlear implants) throughout the session. Pediatric participants were asked to raise their hand prior to speaking and comments and directions were repeated as needed for clarification and understanding within the group.
Each focus group and interview were conducted by a trained moderator (author D. S., parent groups; author H. D., teacher and child groups/interviews) using open-ended scripted questions in moderator's guides. Initial guides were developed based on a literature review of fatigue and stress in children, expert opinion of our research team, and findings from our prior work in AHL (Davis et al., 2020). The guides were reviewed and modified based on input from primary stakeholders (i.e., parents of CHL, professionals with hearing loss, and those working with CHL). As new information was obtained from group discussions, additional modifications to the guides were made on an iterative basis (Merriam & Tisdell, 2016). All sessions began with an explanation of the study and a prompt to start the discussion. Examples of open-ended questions used to initiate and guide the discussions are shown in Table 3. Notes were taken during focus groups by the moderator and/or a secondary research assistant and were organized by themes and key discussion points. Focus group sessions ranged from 60 to 90 min.
Table 3.
Excerpts from moderator's guides.
| 1. Children: Do any activities where you must listen make you feel tired? [If the child's response was “yes,” they were asked to describe the situations.] |
| 2. Parents: Do you help your child cope with hearing loss/and or fatigue? Does your child use self-coping mechanisms? [If the parents response was “yes,” they were asked to describe their methods and coping strategies.] |
| 3. School professionals: What alerts you to your student feeling worn out from listening? What behaviors/symptoms do you notice? |
Sixteen parents participated in one of three parent focus groups and 27 school professionals attended one of five focus groups. Due to scheduling constraints, one parent and one teacher of the deaf participated in an interview instead of a focus group, providing a total of 17 parent participants and 28 school professional participants. Child focus groups were held by age (7–9 years; 10–12 years; 13–17 years) with the assumption that fatigue experiences may vary by age and that children would better connect with peers in the same age range. A total of 17 children participated in the four focus groups. Limited participant responses were obtained in these initial groups, leading the team to significantly edit the pediatric moderator's guide. A toolbox of activities was developed to better establish rapport with the participants and facilitate an understanding of listening-related fatigue in the participants (Kirk, 2007; Spratling et al., 2012). Activities included slide shows with pictures, handouts, and board games to discuss and explore challenging listening situations that may result in listening-related fatigue. Following completion of four pediatric focus groups, the team turned to collecting data one-on-one via open-ended interviews for the remainder of pediatric participants (n = 28). The addition of interviews allowed for greater scheduling flexibility and a substantial increase in the quantity and quality of self-disclosures from the children. Interviews averaged 20 min in length. Table 4 outlines the three participant categories and the method of data collection (i.e., focus group or interview).
Table 4.
Composition of participant groups and interviews.
| Participants | Focus groups | Interviews | Total participants |
|---|---|---|---|
| Parents | 3 groups (n = 16) | 1 (n = 1) | 17 |
| School professionals | 5 groups (n = 27) | 1 (n = 1) | 28 |
| Children | 4 groups (n = 15) | 28 (n = 28) | 43 |
| Total | 12 groups | 30 interviews | 88 |
All sessions were audio recorded on two Olympus WS-823 Digital Voice Recorders. Participants were encouraged to offer any additional comments or topics at the end of each session. Termination of the sessions occurred when data saturation was reached, per the moderator's observations of no new information being brought forward by the participants. Data collection ceased when data saturation across sessions was reached, per ongoing team review of the coding strategy (see Data Analysis section below).
Data Analysis
Approximately 21 hr of recordings were transcribed verbatim by an outside independent agency (www.rev.com). Participant comments were deidentified. After transcription was completed, trained research personnel reviewed the written transcript for accuracy and completion, and then edited the files as needed if segments were incomplete or inaccurate. An iterative, inductive/deductive approach to qualitative data analysis (Azungah, 2018; Fereday & Muir-Cochrane, 2006; Tjora, 2019) was utilized. Author D. S. led the data review and analysis. Our methods mirror the procedures used in a previous study examining listening-related fatigue in AHL (Davis et al., 2020). In this section, we describe those methods following recommendations provided in the Consolidated Criteria for Reporting Qualitative Studies guidelines (Booth et al., 2014). A preliminary coding strategy was developed to capture recurring themes discussed in the focus groups and interviews to best organize and analyze the comments. Initial themes were identified using evidence from the literature, our experience conducting similar work in AHL, and the development of the focus group and interview moderator guides. These preliminary themes were refined following an initial review of the first three focus group transcripts. An iterative process was utilized to review and revise the coding strategy with the addition of new themes as they emerged. The final coding strategy consisted of (a) theme and subtheme headers, (b) definitions for each theme, and (c) rules for inclusion/exclusion of the quote as needed (Guest et al., 2006). Regular research meetings were held to discuss coding questions and to ensure consistency in the process.
Research team members were trained to review and organize participant comments using the finalized coding system. Two trained coders read each transcript line-by-line and assigned a code to each unique participant quote. After coding, transcripts were reviewed to ensure quality and consistency of coding among reviewers; any discrepancies were reviewed and rectified by a third coder. Relevant quotes from all sessions were then combined and reordered by code for further analysis; participant comments not related to listening-related fatigue and hearing loss were removed.
Results
The most prominent themes and subthemes identified during analysis of participant comments (CHL, their parents, and school professionals working with CHL) were used to develop a theoretical framework for understanding listening-related fatigue in CHL (see Figure 1). Briefly, the left side of the figure highlights important factors referred to as “situational determinants” that, based on participant report, may impact the development of listening-related fatigue in CHL. The middle section shows the diverse subjective experiences (physical, cognitive, and social–emotional) of listening-related fatigue in CHL, as described by the participants. Lastly, the right-hand column lists common coping strategies reportedly utilized by CHL, or those who work with them, to alleviate or avoid fatigue (upper section), as well as perceived barriers to utilizing such coping strategies (bottom section). Lines with arrows indicate the potential interactions and effects these factors may have on a CHL's fatigue experiences. We discuss key components of the framework, supported by examples and quotes from participants, in the following sections.
Situational Determinants of Listening-Related Fatigue
Several key situational factors associated with experiences of listening-related fatigue were identified (left panel in Figure 1). Importantly, not all listening situations were deemed equally fatiguing, although specific environmental and talker factors had an impact. As anticipated, environments considered noisy were often considered more fatiguing for CHL—background noise was one of the most commonly reported fatigue-related problems across all focus groups and interviews. Noisy situations included social events involving several talkers, such as family and church functions, as well as restaurants, driving in the car, and in the mall. In addition to in-person communication, CHL are frequently connected to others via media devices. Many reported telephone calls and listening to videos, both in school and for leisure, as more fatiguing due to poor audibility and lack of consistent visual cues. One teen reported the following.
I feel more focused when there's a one-on-one conversation and I feel more talkative. But when there's a lot of friends—that makes me more tired. Trying to focus on conversations and then trying to think about it and process it makes me a little tired.
Parents observed fatigue when their child was listening to talkers with a faster rate of speech, when they were at an increased distance from the speaker, or had reduced access to visual cues from the speaker's face. One parent shared the following observations from a museum visit with her child.
The gentleman [tour guide] was great, but he spoke so fast—she was still missing stuff in a very hectic environment…I can tell it's a lot for her. She has to make an effort and it wears her out.
Because CHL spend much of their time in the educational setting, school-specific situational factors were included separately in the theoretical framework (see Figure 1, left panel, middle box). CHL reported fatigue when listening in situations with significant noise, such as assemblies and pep rallies and school professionals reported that the cafeteria, gymnasium, and school hallways were noisy and potentially fatiguing environments. Some CHL noted internal pressure (“I want to hear everything”) and external pressure (“My parents want me to do well academically”) as contributors to fatigue—that they must focus intently and stay engaged even when tired from listening. One participant shared “I just have to really go in and try to listen to them…to put my focus on them to zoom everything out just to hear what they're saying…it's kind of a lot of work for me.” Outside of the classroom, listening for directions from coaches and interacting with team members on the field/court while playing sports was also considered fatiguing by CHL.
Increased listening-related fatigue was reported at the end of the school day compared to the beginning of the day, with participants citing additional fatigue following the need to listen throughout many class periods. In addition, students with hearing loss were reportedly more fatigued by the end of the school week (school professionals and parents comparing behaviors on Friday to observations earlier in the week). Students appeared more likely to experience fatigue when engaged in group discussion or when multitasking was required. One teacher of the deaf shared that “if my kids are expected to listen to a lecture, understand what's being said, and take notes…they freak out. They just give up and won't do anything.”
In addition, school professionals identified several individual, child-specific factors that may lead to fatigue in CHL while at school (Figure 1, left panel, lower box). Participants reported that CHL with additional disabilities or diagnoses appeared more fatigued following auditory tasks than their peers. The age of the CHL appeared to play a role; however, some participants felt that younger CHL were more susceptible to fatigue, while others believed the manifestations of fatigue were more prevalent in middle and high school age students. School professionals reported that motivated, engaged students concerned about academics and hearing “every little thing” in class were more likely to experience listening-related fatigue. One educator proffered the following comment regarding how her student's fatigue experiences were related to her motivation to achieve future goals.
Her parents would talk at IEP meetings about how typically tired she would be when school was finished—that she didn't know if she could go to soccer practice or not. And it was like a mental tired. Not so much the physical part, just that she was worn out from having to engage so hard all day long to try to stay on grade level…so [she] can get to college to play soccer. You know, because those things had to happen for her to get in.
The use (and nonuse) of personal amplification devices, such as hearing aids and cochlear implants, as well as remote microphone technology, resulted in reduced engagement and additional fatigue. In such instances, when a child forgot or refused to wear their device, school professionals reported that the CHL seemed to struggle to keep up with the classroom instruction and subsequently experienced listening-related fatigue. Some school professionals reported they felt that CHL were more on-task and less fatigued when utilizing their remote microphone systems in the classroom.
Experiences of Listening-Related Fatigue
The reported subjective experiences of listening-related fatigue were unique and varied for CHL but with several recurring themes. Focus group and interview comments fell into the following categories: physical, cognitive, and social–emotional experiences (see Figure 1, middle panel). Many, but not all, of the children were able to describe their experiences and use common terms such as “tired,” “drained,” and “exhausted” to indicate a physical aspect of fatigue. A teen with hearing loss reported, “when I get tired of listening to things, I just tell my friends—‘I'm tired of listening to you, I'm going to turn you down [her hearing aid]. If you need me, tap me.’ And I will do that for fifteen, thirty min.” Conversely, some pediatric participants struggled to understand the definition of fatigue and, when queried, used terms such as “sickness,” “sleepy,” going to “Lalaloopsy land,” “droopy,” and “attitude.” This issue was especially true for younger children; however, some of the older participants also displayed difficulty with the concept of fatigue. For example, one teenage participant reported that she was unsure what fatigue meant, but that the word fatigue “sound[ed] like phantom, so maybe a squid?”
Adults observed physical fatigue in their CHL, calling them “worn out” and “exhausted.” Parents reported more frequent complaints of headaches and the need for rest breaks after school for their CHL, compared to the child's siblings without hearing loss. One parent reported the following:
She [the child with hearing loss] struggles with the last class period of the day that usually has some type of video aspect in it. That's when she'll come home with more of a headache, and she will admit it's just too hard to drown out everything else and listen to the video.
In addition to physical tiredness, some CHL experienced cognitive fatigue during or after difficult listening situations. This type of fatigue was expressed as difficulty concentrating and problems with staying focused and often occurred when multitasking skills were required, such as listening to a lecture in class while simultaneously taking notes. Parents and school professionals observed that CHL had problems with “zoning out” and “reduced motivation” especially at the end of the school day. Many children were categorized as having attention and behavior problems in the class, displaying behaviors associated with listening-related fatigue, such as daydreaming, being off-task, and being easily distracted.
Listening-related fatigue was associated with negative effects on social and emotional behaviors (see Figure 1, middle panel). Children reported feeling annoyed, frustrated, and angry when listening in challenging environments. School professionals observed frustration in CHL when they experienced communication breakdowns with peers. Adult participants reported that when younger CHL became fatigued they often exhibited emotional signs, such as acting out, frustration, or defiance. A speech-language pathologist had to give her student with hearing loss a break after a fatiguing listening task because “he needs a moment to not have to listen and to tune out. If he doesn't get that break, his behavior is significantly impacted.” As fatigue develops, school professionals and parents note that CHL may begin to show signs of giving up by avoiding and withdrawing from situations. A parent reported that “When [my CHL] is tired, he looks like he doesn't care” and he doesn't “pursue further interaction with adults or peers.” Many said that their CHL did not want to participate in social, extracurricular, or family outings after school, limiting communication opportunities and relationship development. While fatigue-related disengagement occurs in children without hearing loss as well, parents and school professionals felt this was more common among CHL due to listening demands throughout the school day.
Listening-Related Fatigue Coping Strategies
CHL reported using strategies for avoiding fatigue, such as asking for environmental modifications to the listening situation (e.g., asking to talk in a quieter environment, sitting closer to the teacher) or “zoning out” during class (see right hand side of Figure 1; top box). Some CHL asked to go to a quiet classroom or take an extended bathroom break in order to recover following fatigue. At times, CHL would push through their fatigue in a challenging listening situation while other CHL would withdraw or shut down once tired. School professionals observed CHL initiating coping strategies at school, such as removing a hearing device or resting one's head on their desk, in order to take a listening break and thus attempt to manage their fatigue. At the end of the school day, many CHL reported feeling exhausted and wanting a break—what parents described as their child “completely shutting down” or “going into a bubble.” After school, some reported taking off their hearing device, falling asleep in the car, or taking a nap or break at home to cope with fatigue.
In addition to child-led coping strategies, parents provided assistance with fatigue relief for the CHL (see Figure 1, right panel, top box). One parent shared that when her teenager comes home after school “…she would usually go in her room, lights off, [and] decompress for half an hour…By the time she comes home in the afternoon from school she's just very exhausted.” Of note, parents reported that the strategies and coping mechanisms used by their CHL were not employed by their siblings without hearing loss. According to the parents, CHL often wished to avoid large groups at school dances or youth group activities, asking to skip or leave the events early, as a coping mechanism that the parents permitted. One parent noted that her child “does not put himself in situations to get stressed out by listening” and avoids attending social events completely after a few frustrating attempts. In general, in an effort to help their child recover, parents reported the need to “give [the] child space” to do a quiet, individual activity (e.g., reading a book, taking a rest time) after being in a difficult listening situation.
School professionals also provided interventions to help the student reduce or avoid listening-related fatigue. One teacher reported recognizing that her student “…doesn't know how to advocate—to say, ‘I'm tired…I need a break.’” She would therefore allow the student to take periodic breaks following auditory-heavy content prior to starting the next task. Additional strategies included pulling CHL out for individualized instruction in the morning rather than the afternoon and scheduling “listening breaks” throughout the day. An elementary school speech-language pathologist stated, “I feel like, if I'm doing a specific auditory task, I like to get the kids in the morning. At the end of the day, their ability to focus…becomes nearly impossible.” CHL were often given preferential seating near the teacher and were provided with notes and supplemental materials prior to the class period. School professionals felt these accommodations not only helped the child focus on the verbal instruction during class; they also seemed useful for minimizing listening-related fatigue in the classroom.
Perceived Barriers to Coping Strategies
Some CHL reported a desire to utilize coping strategies, such as removing a hearing device or “zoning out”; however, external barriers kept them from doing so in some cases (see right lower panel of Figure 1). Many CHL felt that they would get in trouble, or miss important information, if they utilized these options. A significant barrier was the perceived, and actual, lack of control over their schedules. CHL reported that even if they wanted a break from listening, they could not take it and did not know who, or how, to ask for such accommodations.
Although parents recognized the importance of coping strategies to reduce fatigue, some felt that long-term consequences of utilizing these strategies may be a potential barrier to consistent use—citing negative academic and psychosocial effects. For example, a parent of a child in elementary school reported that her child was getting in trouble for using a coping strategy (putting her head on the desk when she was tired), leading the teacher to believe she was not paying attention/did not care about the classroom structure and rules. This led to increased problems, both academically and socially.
School professionals attempted to initiate coping strategies for their CHL by scheduling auditory-heavy lessons in the morning; however, limited flexibility in schedules and other school-related constraints were considered barriers. Like parents, school professionals reported that some coping strategies, although crucial for reducing the negative effects of fatigue, may impact the student's ability to socialize or participate in the classroom setting. For instance, one teacher's student with hearing loss came to her room in the morning rather than wait in the gym with the other students to avoid the noisy environment, communication difficulties, and subsequent fatigue. This meant that the students did not play or talk with their classmates prior to the start of the school day. Overall, parent and school professionals were more aware of, and concerned about, the negative effects of potential coping strategies than the CHL themselves.
Discussion
In this article, we used focus groups and interviews to investigate the experience of listening-related fatigue in CHL from the perspective of the child, their parents, and school professionals. Information obtained from the participants was used to develop a theoretical framework for understanding listening-related fatigue in this population. This process is a critical first step toward the long-term goal of developing valid and sensitive measures of listening-related fatigue in CHL.
Results from this study suggest that the experience of listening-related fatigue in CHL is complex and can be expressed in multiple ways, including in physical (e.g., extreme tiredness, needing a listening break), cognitive (e.g., difficulty concentrating), and social–emotional domains (e.g., frustration, anger, withdrawal/shutting down). Experiences of fatigue among CHL are impacted by various internal (e.g., motivation, pressure to listen) and external factors (e.g., background noise, speaker characteristics). Predictably, background noise and poor acoustics were challenging and fatiguing factors for both AHL and CHL. Similar to findings in AHL (Davis et al., 2020), reports of listening-related fatigue by CHL are consistent with the Motivation Control Theory of Fatigue (Hockey, 2013). This theory suggests that fatigue is likely a direct consequence of applied effort under certain conditions. Relevant to CHL, the model predicts fatigue is more likely to develop when high levels of effort are applied toward a required task (e.g., listen and take notes in class), as compared to when a similar amount of effort is applied toward a personally desired goal (e.g., trying to follow an interesting movie). Likewise, the model suggests fatigue is more likely to occur when a person's motivation to achieve a goal is high and control over how the specific task/goal is accomplished is low.
Given the impact effort, motivation, control, and preferences play in the school setting and in the development of fatigue, it is not surprising that school settings can be fatiguing, even for typically developing children (e.g., Fukuda et al., 2010). To do well in school settings, where auditory and language processing demands are high, CHL must apply high levels of (listening) effort on school-related tasks (as opposed to personally desired goals). Adding to these high effort demands, all children experience external and internal pressures to maintain their effort over time (i.e., pressure to keep motivation high), in order to do well in the school setting, which also increases risk for fatigue. Finally, the limited control many children have over how to do or engage in school-related tasks limits their ability to enact coping strategies to minimize their fatigue should it begin to develop. These factors, in conjunction with the high levels of listening effort required of CHL, may work together in the school setting to increase their risk for fatigue.
As noted above, an important distinction between AHL and CHL, and the resultant theoretical frameworks, relates to availability and utilization of coping strategies to prevent, reduce, or avoid the development of listening-related fatigue. Some CHL reportedly felt limited control in their ability to employ certain coping strategies for fear of retribution from authority figures (e.g., if they took a break or removed a listening device at school). This lack of control means some CHL must rely on their parents or school professionals to implement strategies to help ameliorate their fatigue; however, school professionals also reported barriers that limited their ability to help CHL cope (e.g., scheduling limitations). Likewise, parents and school professionals were concerned that implementing coping strategies could potentially have negative psychosocial and academic effects. This highlights the need to develop and validate multiple intervention strategies that are not only effective, but also acceptable for use in school settings. In contrast, AHL reported feeling more control over their ability to implement coping strategies to reduce or prevent the development of listening-related fatigue. For example, some AHL proactively scheduled the day to include listening breaks, removed their hearing devices on occasion, or avoided specific listening situations to limit or ameliorate fatigue (Davis et al., 2020). Clearly, these options may be challenging for some CHL to implement themselves in a school setting.
In addition, comments from CHL indicated a closer connection between social and emotional fatigue-related experiences compared to AHL. These findings resulted in a combined social–emotional category for the pediatric theoretical framework compared to two separate categories for AHL. Differences in fatigue experiences reported by CHL and AHL may be due to variability in required listening tasks, self-perceived difficulties, and/or other individual factors. It is also possible that CHL may not be as attuned to their social or emotional difficulties (i.e., internalized states) compared to physical or cognitive difficulties (i.e., externalized behaviors, change in function) as AHL. Of note, CHL could provide us with emotion-based words (angry, frustrated, sad) but rarely discussed difficulties in social settings related to fatigue—this consideration was mainly presented by parents and school professionals. Subjective reports of fatigue from young children being treated for cancer revealed a focus on physical manifestations of fatigue (being weak or tired) while adolescents noted both physical and mental effects, emphasizing differences in reports based on developmental levels (Hockenberry-Eaton et al., 1998). Recall that some of our child participants had significant difficulty defining “fatigue,” especially beyond a physical change, and may similarly have difficulty identifying its social or emotional effects. This may be due, in part, to the child's language skills as they attempt to describe fatigue and should be considered when discussing fatigue with a CHL.
Thus far, we have compared findings from this study in CHL to our previous work with AHL; however, others have provided reports of subjective listening-related fatigue in individuals with hearing loss. In fact, the concepts of listening-related fatigue and effort associated with hearing loss have incidentally emerged as common discussion points in other studies utilizing focus groups with AHL (Holman et al., 2019; Hughes et al., 2018; McRackan et al., 2017) and CHL, parents, and professionals (Hoffman et al., 2019), despite not being the primary focus of the discussions. Findings in these studies echo the reports in the current study about the negative impact of fatigue and effort on overall quality of life. For example, McRackan et al. (2017) included “listening effort” as a central theme in a quality of life item bank after collecting data from adults with cochlear implants. Participants in their study similarly reported difficulties with feeling exhausted after listening all day, citing significant mental energy expenditure when communicating, especially in background noise. In another study, adult participants with hearing loss reported varied experiences and levels of listening-related fatigue and subsequent negative effects (Holman et al., 2019). Interview participants felt weariness due to additional concentration and mental effort needed to listen and, for those who reported struggling with fatigue, they emphasized the importance of coping strategies, such as the need for breaks from listening. Hoffman et al. (2019) collected responses from children with cochlear implants and their parents about quality of life for a health-related quality of life scale. The authors reported that “fatigue” was one of the major themes discussed in their focus groups and, subsequently, the construct of fatigue was included as one of eight key domains on their pediatric scale. Consistent with parent reports in our study, a parent of a child with cochlear implants noted that her child “comes home exhausted because he has to give 110% toward trying to focus” (Hoffman et al., 2019). Findings from these studies underscore that, although variable in nature, subjective listening-related fatigue is prevalent in both AHL and CHL and has the potential to negatively impact quality of life and overall functional status in these populations. Importantly, the availability and consistent use of coping strategies may currently be limited for CHL.
Strengths and Limitations
Strengths of the study include the adherence to expert guidelines for designing, developing, and reporting high level qualitative research (Booth et al., 2014). A second strength is the implementation of focus groups and interviews from three stakeholder groups (CHL, their parents, and school professionals) to provide us with a broad, more comprehensive perspective of listening-related fatigue in CHL. To our knowledge, this is the first qualitative study to examine listening-related fatigue from the perspective of these three stakeholder groups.
Limitations of the study are also noteworthy. First, participants were recruited primarily from an urban area in Middle Tennessee. Although we believe fatigue will ultimately prove to be a universal construct, the dominant experiences of the respondents may not be representative of those in other areas. In addition, children with mild and/or unilateral hearing loss were not included in the sample; this population of children may have yielded additional and varying perspectives on listening-related fatigue. A third limitation is the relatively small number of younger CHL who participated. The participants in this study ranged in age from 7 to 17 years, but only four CHL were between the ages of 7–9 years. Hence, the perspectives of CHL reported herein may not fully capture the experience of these younger children. Also, recall that CHL participants often had additional diagnoses and disabilities. It is possible that these children may have perspectives of listening-related fatigue that differ in some ways from the population of CHL without such additional disabilities. However, because additional disabilities are common among CHL (Cupples et al., 2014; Gallaudet Research Institute, 2014; Picard, 2004), we believe that inclusion of these children actually increases the relevance of our work to a broader population of CHL—a primary goal in qualitative research (Giacomini & Cook, 2000).
Conclusions
CHL are at risk for significant fatigue and its sequelae; therefore, the need for a child-centered scale targeting listening-related fatigue is essential (Bess et al., 2020; Camarata et al., 2018; Werfel & Hendricks, 2016). Therefore, the long term goal of this project is to create scales that are sensitive to listening-related fatigue in CHL and appropriate for use in clinical, educational, and research settings. The results from this study provide a foundation for the development of assessment instruments that have high relevance and construct validity. Responses from the focus group participants will be utilized to develop test items for these scales; the items will then be tested by large cohorts of participants to identify high-quality, valid questions to include in the final versions of the scales.
In addition, study findings stress the importance of counseling/training CHL about listening-related fatigue. Recall that although some CHL could define fatigue, many others were not even aware it was a problem for them—despite parents proffering detailed insight regarding observations of their child's struggle with fatigue. These findings suggest that some CHL may not be aware of the relationship between their hearing difficulties and certain negative feelings, behaviors, and/or experiences that arise from, or are related to, listening-related fatigue. Additionally, some CHL may struggle to describe their fatigue symptoms due to comorbid language or cognitive delays. Professionals working with CHL need to become familiar with listening-related fatigue associated with pediatric hearing loss, including its causes, challenges, and potential interventions to better counsel CHL and their parents.
Acknowledgments
This work was supported by the Institute of Education Sciences, U.S. Department of Education, Vanderbilt University Medical Center (Grant R324A150029, awarded to Bess, PI). The opinions expressed are those of the authors and do not represent the views of the Institute or the U.S. Department of Education. The authors would like to thank the families and school professionals that participated in the focus groups and interviews. We are grateful to Ronan McGarrigle for his insight and collaboration throughout this study and to the graduate students from the Department of Hearing and Speech Sciences, Vanderbilt University School of Medicine, who participated in data review and project development.
Funding Statement
This work was supported by the Institute of Education Sciences, U.S. Department of Education, Vanderbilt University Medical Center (Grant R324A150029, awarded to Bess, PI). The opinions expressed are those of the authors and do not represent the views of the Institute or the U.S. Department of Education.
References
- Aaronson, L. S. , Teel, C. S. , Cassmeyer, V. , Neuberger, G. B. , Pallikkathayil, L. , Pierce, J. , Press, A. N. , Williams, P. D. , & Wingate, A. (1999). Defining and measuring fatigue. Journal of Nursing Scholarship, 31(1), 45–50. https://doi.org/10.1111/j.1547-5069.1999.tb00420.x [DOI] [PubMed] [Google Scholar]
- Alhanbali, S. , Dawes, P. , Lloyd, S. , & Munro, K. J. (2017). Self-reported listening-related effort and fatigue in hearing-impaired adults. Ear and Hearing, 38(1), e39–e48. https://doi.org/10.1097/aud.0000000000000361 [DOI] [PubMed] [Google Scholar]
- Amato, M. P. , Ponziani, G. , Rossi, F. , Liedl, C. L. , Stefanile, C. , & Rossi, L. (2001). Quality of life in multiple sclerosis: The impact of depression, fatigue, and disability. Multiple Sclerosis Journal, 7(5), 340–344. https://doi.org/10.1177/135245850100700511 [DOI] [PubMed] [Google Scholar]
- Azungah, T. (2018). Qualitative research: Deductive and inductive approaches to data analysis. Qualitative Research Journal, 18(4), 383–400. https://doi.org/10.1108/qrj-d-18-00035 [Google Scholar]
- Bess, F. H. , Davis, H. , Camarata, S. , & Hornsby, B. W. Y. (2020). Listening-related fatigue in children with unilateral hearing loss. Language, Speech, and Hearing Services in Schools, 51(1), 84–97. https://doi.org/10.1044/2019_lshss-ochl-19-0017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bess, F. H. , Gustafson, S. J. , Corbett, B. A. , Lambert, E. W. , Camarata, S. M. , & Hornsby, B. W. Y. (2016). Salivary cortisol profiles of children with hearing loss. Ear and Hearing, 37(3), 334–344. https://doi.org/10.1097/AUD.0000000000000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bess, F. H. , & Hornsby, B. W. (2014). Commentary. Listening can be exhausting—Fatigue in children and adults with hearing loss. Ear and Hearing, 35(6), 592–599. https://doi.org/10.1097/AUD.0000000000000099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth, A. , Hannes, K. , Harden, A. , Noyes, J. , Harris, J. , & Tong, A. (2014). COREQ (Consolidated Criteria for Reporting Qualitative Studies). In Moher D., Altman D. G., Schulz K. F., Simera I., & Wager E. (Eds.), Guidelines for reporting health research: A user's manual (pp. 214–226). Wiley. https://doi.org/10.1002/9781118715598.ch21 [Google Scholar]
- Bryant, D. , Chiaravalloti, N. D. , & DeLuca, J. (2004). Objective measurement of cognitive fatigue in multiple sclerosis. Rehabilitation Psychology, 49(2), 114–122. https://doi.org/10.1037/0090-5550.49.2.114 [Google Scholar]
- Camarata, S. , Werfel, K. , Davis, T. , Hornsby, B. W. Y. , & Bess, F. H. (2018). Language abilities, phonological awareness, reading skills, and subjective fatigue in school-age children with mild to moderate hearing loss. Exceptional Children, 84(4), 420–436. https://doi.org/10.1177/0014402918773316 [Google Scholar]
- Cupples, L. , Ching, T. Y. C. , Crowe, K. , Seeto, M. , Leigh, G. , Street, L. , Day, J. , Marnane, V. , & Thomson, J. (2014). Outcomes of 3-year-old children with hearing loss and different types of additional disabilities. Journal of Deaf Studies and Deaf Education, 19(1), 20–39. https://doi.org/10.1093/deafed/ent039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curt, G. A. (2000). The impact of fatigue on patients with cancer: Overview of FATIGUE 1 and 2. The Oncologist, 5(S2), 9–12. https://doi.org/10.1634/theoncologist.5-suppl_2-9 [DOI] [PubMed] [Google Scholar]
- Davis, H. , Schlundt, D. , Bonnet, K. , Camarata, S. , Bess, F. H. , & Hornsby, B. (2020). Understanding listening-related fatigue: Perspectives of adults with hearing loss. International Journal of Audiology, 60(6), 458–468. https://doi.org/10.1080/14992027.2020.1834631 [DOI] [PubMed] [Google Scholar]
- DeLuca, J. (Ed.). (2005). Fatigue as a window to the brain. MIT Press. https://doi.org/10.7551/mitpress/2967.001.0001 [Google Scholar]
- Dwyer, R. T. , Gifford, R. H. , Bess, F. H. , Dorman, M. , Spahr, A. , & Hornsby, B. W. (2019). Diurnal cortisol levels and subjective ratings of effort and fatigue in adult cochlear implant users: A pilot study. American Journal of Audiology, 28(3), 686–696. https://doi.org/10.1044/2019_aja-19-0009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddy, L. , & Cruz, M. (2007). The relationship between fatigue and quality of life in children with chronic health problems: A systematic review. Journal for Specialists in Pediatric Nursing, 12(2), 105–114. https://doi.org/10.1111/j.1744-6155.2007.00099.x [DOI] [PubMed] [Google Scholar]
- Elena Garralda, M. , & Rangel, L. (2004). Impairment and coping in children and adolescents with chronic fatigue syndrome: A comparative study with other paediatric disorders. Journal of Child Psychology and Psychiatry, 45(3), 543–552. https://doi.org/10.1111/j.1469-7610.2004.00244.x [DOI] [PubMed] [Google Scholar]
- Etikan, I. (2016). Comparison of convenience sampling and purposive sampling. American Journal of Theoretical and Applied Statistics, 5(1), 1. https://doi.org/10.11648/j.ajtas.20160501.11 [Google Scholar]
- Evans, E. J. , & Wickstrom, B. (1999). Subjective fatigue and self-care in individuals with chronic illness. MEDSURG Nursing, 8(6), 363–369. [PubMed] [Google Scholar]
- Fereday, J. , & Muir-Cochrane, E. (2006). Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. International Journal of Qualitative Methods, 5(1), 80–92. https://doi.org/10.1177/160940690600500107 [Google Scholar]
- Flechtner, H. , & Bottomley, A. (2003). Fatigue and quality of life: Lessons from the real world. The Oncologist, 8(Suppl. 1), 5–9. https://doi.org/10.1634/theoncologist.8-suppl_1-5 [DOI] [PubMed] [Google Scholar]
- Fukuda, S. , Yamano, E. , Joudoi, T. , Mizuno, K. , Tanaka, M. , Kawatani, J. , Takano, M. , Tomoda, A. , Imai-Matsumura, K. , Miike, T. , & Watanabe, Y. (2010). Effort-reward imbalance for learning is associated with fatigue in school children. Behavioral Medicine, 36(2), 53–62. https://doi.org/10.1080/08964281003774919 [DOI] [PubMed] [Google Scholar]
- Gallaudet Research Institute. (2014). Regional and National summary report of data from the 2013–14 annual survey of deaf and hard of hearing children and youth. https://www.gallaudet.edu/documents/Research-Support-and-International-Affairs/Intl%20Affairs/Demographics/AS14_RegNat.pdf
- Giacomini, M. K. , & Cook, D. J. (2000). Users' guides to the medical literature: XXIII. Qualitative research in health care B. What are the results and how do they help me care for my patients. JAMA, 284(4), 478–482. https://doi.org/10.1001/jama.284.4.478 [DOI] [PubMed] [Google Scholar]
- Guest, G. , Bunce, A. , & Johnson, L. (2006). How many interviews are enough? Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822x05279903 [Google Scholar]
- Hardy, S. E. , & Studenski, S. A. (2010). Qualities of fatigue and associated chronic conditions among older adults. Journal of Pain and Symptom Management, 39(6), 1033–1042. https://doi.org/10.1016/j.jpainsymman.2009.09.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks, C. B. , & Tharpe, A. M. (2002). Listening effort and fatigue in school-age children with and without hearing loss. Journal of Speech, Language, and Hearing Research, 45(3), 573–584. https://doi.org/10.1044/1092-4388(2002/046) [DOI] [PubMed] [Google Scholar]
- Hockenberry-Eaton, M. , Hinds, P. S. , Alcoser, P. , O'Neill, J. B. , Euell, K. , Howard, V. , Gattuso, J. , & Taylor, J. (1998). Fatigue in children and adolescents with cancer. Journal of Pediatric Oncology Nursing, 15(3), 172–182. https://doi.org/10.1016/S1043-4542(98)90086-8 [DOI] [PubMed] [Google Scholar]
- Hockey, R. (2013). The psychology of fatigue: Work, effort, and control. Cambridge University Press. https://doi.org/10.1017/CBO9781139015394 [Google Scholar]
- Hoffman, M. F. , Cejas, I. , & Quittner, A. L. (2019). Health-related quality of life instruments for children with cochlear implants: Development of child and parent-proxy measures. Ear and Hearing, 40(3), 592–604. https://doi.org/10.1097/aud.0000000000000631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman, J. A. , Drummond, A. , Hughes, S. E. , & Naylor, G. (2019). Hearing impairment and daily-life fatigue: A qualitative study. International Journal of Audiology, 58(7), 408–416. https://doi.org/10.1080/14992027.2019.1597284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornsby, B. W. Y. , Gustafson, S. J. , Lancaster, H. , Cho, S.-J. , Camarata, S. , & Bess, F. H. (2017). Subjective fatigue in children with hearing loss assessed using self- and parent-proxy report. American Journal of Audiology, 26(3S), 393–407. https://doi.org/10.1044/2017_aja-17-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornsby, B. W. Y. , & Kipp, A. M. (2016). Subjective ratings of fatigue and vigor in adults with hearing loss are driven by perceived hearing difficulties not degree of hearing loss. Ear and Hearing, 37(1), e1–e10. https://doi.org/10.1097/aud.0000000000000203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornsby, B. W. Y. , Naylor, G. , & Bess, F. H. (2016). A taxonomy of fatigue concepts and their relation to hearing loss. Ear and Hearing, 37(1), 136S–144S. https://doi.org/10.1097/aud.0000000000000289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornsby, B. W. Y. , Werfel, K. , Camarata, S. , & Bess, F. H. (2014). Subjective fatigue in children with hearing loss: Some preliminary findings. American Journal of Audiology, 23(1), 129–134. https://doi.org/10.1044/1059-0889(2013/13-0017) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard, C. S. , Munro, K. J. , & Plack, C. J. (2010). Listening effort at signal-to-noise ratios that are typical of the school classroom. International Journal of Audiology, 49(12), 928–932. https://doi.org/10.3109/14992027.2010.520036 [DOI] [PubMed] [Google Scholar]
- Hughes, S. E. , Hutchings, H. A. , Rapport, F. L. , McMahon, C. M. , & Boisvert, I. (2018). Social connectedness and perceived listening effort in adult cochlear implant users: A grounded theory to establish content validity for a new patient-reported outcome measure. Ear and Hearing, 39(5), 922–934. https://doi.org/10.1097/aud.0000000000000553 [DOI] [PubMed] [Google Scholar]
- Johnson, S. (2005). Depression and fatigue. In DeLuca J. (Ed.), Fatigue as a window to the brain (pp. 157–172). MIT Press. [Google Scholar]
- Kirk, S. (2007). Methodological and ethical issues in conducting qualitative research with children and young people: A literature review. International Journal of Nursing Studies, 44(7), 1250–1260. https://doi.org/10.1016/j.ijnurstu.2006.08.015 [DOI] [PubMed] [Google Scholar]
- Knudsen, L. V. , Laplante-Lévesque, A. , Jones, L. , Preminger, J. E. , Nielsen, C. , Lunner, T. , Hickson, L. , Naylor, G. , & Kramer, S. E. (2012). Conducting qualitative research in audiology: A tutorial. International Journal of Audiology, 51(2), 83–92. https://doi.org/10.3109/14992027.2011.606283 [DOI] [PubMed] [Google Scholar]
- Lewis, D. , Schmid, K. , O'Leary, S. , Spalding, J. , Heinrichs-Graham, E. , & High, R. (2016). Effects of noise on speech recognition and listening effort in children with normal hearing and children with mild bilateral or unilateral hearing loss. Journal of Speech, Language, and Hearing Research, 59(5), 1218–1232. https://doi.org/10.1044/2016_JSLHR-H-15-0207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGarrigle, R. , Gustafson, S. J. , Hornsby, B. W. , & Bess, F. H. (2019). Behavioral measures of listening effort in school-age children: Examining the effects of signal-to-noise ratio, hearing loss, and amplification. Ear and Hearing, 40(2), 381–392. https://doi.org/10.1097/aud.0000000000000623 [DOI] [PubMed] [Google Scholar]
- McRackan, T. R. , Velozo, C. A. , Holcomb, M. A. , Camposeo, E. L. , Hatch, J. L. , Meyer, T. A. , Lambert, P. R. , Melvin, C. L. , & Dubno, J. R. (2017). Use of adult patient focus groups to develop the initial item bank for a cochlear implant quality-of-life instrument. JAMA Otolaryngology–Head & Neck Surgery, 143(10), 975–982. https://doi.org/10.1001/jamaoto.2017.1182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merriam, S. B. , & Tisdell, E. J. (2016). Qualitative research—A guide to design and implementation (4th ed.). Jossey-Bass. [Google Scholar]
- Peterson-Sweeney, K. (2005). The use of focus groups in pediatric and adolescent research. Journal of Pediatric Health Care, 19(2), 104–110. https://doi.org/10.1016/j.pedhc.2004.08.006 [DOI] [PubMed] [Google Scholar]
- Picard, M. (2004). Children with permanent hearing loss and associated disabilities: Revisiting current epidemiological data and causes of deafness. The Volta Review, 104(4), 221–236. https://www.proquest.com/openview/f23e75818a68361dd80a7a6d3765d062/1?pq-origsite=gscholar&cbl=41448 [Google Scholar]
- Pichora-Fuller, M. K. , Kramer, S. E. , Eckert, M. A. , Edwards, B. , Hornsby, B. W. Y. , Humes, L. E. , Lemke, U. , Lunner, T. , Matthen, M. , Mackersie, C. L. , Naylor, G. , Phillips, N. A. , Richter, M. , Rudner, M. , Sommers, M. S. , Tremblay, K. L. , & Wingfield, A. (2016). Hearing impairment and cognitive energy: The framework for understanding effortful listening FUEL. Ear and Hearing, 37, 5S–27S. https://doi.org/10.1097/AUD.0000000000000312 [DOI] [PubMed] [Google Scholar]
- Pope, C. , van Royen, P. , & Baker, R. (2002). Qualitative methods in research on healthcare quality. BMJ Quality & Safety, 11(2), 148–152. https://doi.org/10.1136/qhc.11.2.148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prodi, N. , Visentin, C. , Peretti, A. , Griguolo, J. , & Bartolucci, G. B. (2019). Investigating listening effort in classrooms for 5- to 7-year-old children. Language, Speech, and Hearing Services in Schools, 50(2), 196–210. https://doi.org/10.1044/2018_LSHSS-18-0039 [DOI] [PubMed] [Google Scholar]
- Spratling, R. , Coke, S. , & Minick, P. (2012). Qualitative data collection with children. Applied Nursing Research, 25, 47–53. https://doi.org/10.1016/j.apnr.2010.02.005 [DOI] [PubMed] [Google Scholar]
- Thayer, R. E. (1986). Activation-deactivation adjective check list: Current overview and structural analysis. Psychological Reports, 58(2), 607–614. https://doi.org/10.2466/pr0.1986.58.2.607 [Google Scholar]
- Tiesinga, L. J. , Dassen, T. W. , & Halfens, R. J. (1996). Fatigue: A summary of the definitions, dimensions, and indicators. Nursing Diagnosis, 7(2), 51–62. https://doi.org/10.1111/j.1744-618x.1996.tb00293.x [DOI] [PubMed] [Google Scholar]
- Tjora, A. (2019). Qualitative research as stepwise-deductive induction. Routledge. https://doi.org/10.4324/9780203730072 [Google Scholar]
- Tomblin, J. B. , Harrison, M. , Ambrose, S. E. , Walker, E. A. , Oleson, J. J. , & Moeller, M. P. (2015). Language outcomes in young children with mild to severe hearing loss. Ear and Hearing, 36, 76S–91S. https://doi.org/10.1097/AUD.0000000000000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Linden, D. , Frese, M. , & Meijman, T. F. (2003). Mental fatigue and the control of cognitive processes: Effects on preservation and planning. Acta Psychologica, 113(1), 45–65. https://doi.org/10.1016/S0001-6918(02)00150-6 [DOI] [PubMed] [Google Scholar]
- Varni, J. W. , Burwinkle, T. M. , Katz, E. R. , Meeske, K. , & Dickinson, P. (2002). The PedsQL in pediatric cancer: Reliability and validity of the pediatric quality of life inventory generic core scales, multidimensional fatigue scale, and cancer module. Cancer, 94(7), 2090–2106. https://doi.org/10.1002/cncr.10428 [DOI] [PubMed] [Google Scholar]
- Werfel, K. L. , & Hendricks, A. E. (2016). The relation between child versus parent report of chronic fatigue and language/literacy skills in school-age children with cochlear implants. Ear and Hearing, 37(2), 216–224. https://doi.org/10.1097/AUD.0000000000000242 [DOI] [PubMed] [Google Scholar]
- Whitehead, L. (2009). The measurement of fatigue in chronic illness: A systematic review of unidimensional and multidimensional fatigue measures. Journal of Pain and Symptom Management, 37(1), 107–128. https://doi.org/10.1016/j.jpainsymman.2007.08.019 [DOI] [PubMed] [Google Scholar]


