Abstract
Objective:
To evaluate the historical descriptive origins of the extracranial transnasal transsphenoidal route to the sphenoid sinus and sella turcica focusing on the works of two otolaryngologists: Markus Hajek (1861–1941) and Oskar Hirsch (1877–1965).
Data Sources:
A collection of primary references of author publications, as well as contemporary references and textbooks.
Review Methods:
Primary references were reviewed with specific focus on surgical routes to the sphenoid sinus and sella turcica. Chronology was cross-referenced with contemporary publications by contemporaries. Translations from German were conducted by author AM when necessary.
Results:
Markus Hajek elegantly described the surgical approach to the posterior ethmoids and sphenoid sinus in 1904 using a transnasal route. Building on this foundation, Oskar Hirsch described the fully extracranial endonasal transethmoid transsphenoidal approach in 1909. He was first to describe surgical entrance to the sella using this exclusively unilateral endonasal route, which he demonstrated on a cadaver. He reports performing this procedure on a live patient in April, 1910 under local anesthesia in stages over 5 weeks. For better exposure, Hirsch consolidated his method with Killian’s submucosal window resection of the posterior nasal septum allowing for bilateral access to the sphenoid sinus and sella, and completed a single stage procedure on a patient in June 1910.
Conclusion:
Oskar Hirsch was the first to describe and perform a stepwise surgical approach to the sella using an exclusively extracranial, endonasal, transethmoid, and transsphenoidal approach. He built upon his mentor Markus Hajek’s approaches to the posterior ethmoid cells and sphenoid sinus.
Keywords: hypophyseal tumor, endonasal approach, sella turcica, historical
Lay Summary:
The surgical approach commonly used today for resecting pituitary tumors was developed by two otolaryngologists: Hajek and Hirsch. Building upon his former chief’s approach to the sphenoid sinus, Hirsch was the first to perform an exclusively endonasal pituitary surgery in 1910.
Level of Evidence:
N/A: Background information, synthesis from multiple sources emphasizing factual information
Introduction
The pituitary gland, and the bony depression where it lies, the sella turcica, is located deep in the medial middle cranial fossa at the body of the sphenoid bone. The anatomical boundaries of the sella include the optic chiasm superiorly, the carotid arteries and cavernous sinuses laterally, the basilar artery with its associated brainstem posteriorly and the clivus inferiorly. Hence, a highly constricted area with critical structures that in modern times requires advanced anatomical knowledge and surgical precision to address intra- and supra-sellar pathology. The armamentarium of modern skull base surgeons includes microscopic and endoscopic technologies that provide clear visualization of these anatomical structures. The operative approaches used widely today find their roots in the early 1900’s when the first successful pituitary surgical operations were being described.
Much has been written regarding the history of pituitary surgery from descriptions of both the intracranial and extracranial routes by surgeons performing pituitary surgery. Pioneering surgeons of the intracranial route consist of Victor Horsley (1906)1, Otto Kiliani (1904)2 and Fedor Krause (1905).3 Surgeons of the extracranial routes include Hermann Schloffer (1907)4, Theodore Kocher (1909)5, Allen Kanavel (1909)6, Albert Halstead (1910)7, R. Proust (1908)8, Ottokar Chiari (1912)9, and Harvey Cushing (1909).10(Table1)
Table 1:
Contemporary Approaches to the Sella Turcica
| Surgeon | Year | Approach | Description |
|---|---|---|---|
| Kiliani | 1904 | Transfrontal | Intracranial, Intradural |
| Horsley | 1904 | Middle Fossa | Intracranial |
| Krause | 1905 | Anterior Fossa | Intracranial, Extradural |
| Schloffer | 1907 | Transsphenoidal, Superior Nasal | Extracranial, nose reflected |
| Proust | 1908 | Supranasal | Extracranial, nose reflected |
| Kocher | 1909 | Transnasal | Extracranial, nose incised |
| Kanavel | 1909 | Infranasal, transsphenoidal | Extracranial, nose reflected |
| Cushing | 1909 | Sublabial Transphenoidal, | Extracranial, Transpalatal, Infranasal |
| Halstead | 1910 | Sublabial | Extracranial, Transoral |
In the current era, the most common approach to pathology affecting the sellar and parasellar region involves an exclusively endonasal (extracranial) transnasal transsphenoidal approach using either microscopic or endoscopic techniques. Two pioneering Viennese otolaryngologists, building on each other’s expertise, were instrumental in the development of the exclusively extracranial transnasal transsphenoidal approach to the pituitary gland: Markus Hajek and Oskar Hirsch. Accordingly, the aim of this study is to outline the descriptive history of the extracranial transnasal route to the pituitary described over one hundred years ago. Specific emphasis was placed on the state of pituitary surgery in the early 20th century, description of surgical approaches to the sphenoid sinus (precursor region to the sella) and ultimately the surgical route to the sella using an exclusively extracranial, transnasal, transsphenoidal approach.
Materials and Methods
A collection of speeches and publications authored by both Hajek and Hirsch as well as contemporary references and textbooks were compiled with specific focus on surgical routes to the sphenoid sinus and sella turcica. We relied exclusively on primary sources relating to sellar approaches. Accurate conceptual translation was performed (AM).
Results
Surgical Techniques of Markus Hajek
Markus Hajek was born in 1861 in Hungary, and he emigrated to Vienna around 1880 to attend medical school, penniless and without knowledge of the German language.11 After graduating medical school, he began working with Johann Schnitzler, chief of the laryngology department.12,13 Building upon the anatomical work of Zuckerkandl and Onodi, he became known for his in depth and precise descriptions of pathologies of the nose, paranasal sinuses, and larynx. He began teaching at the University of Vienna in 1898 and was the author of a popular textbook on diseases of the nasal accessory sinuses that first appeared in 1899, and was widely translated and distributed internationally. He became professor and director of the Rhinolaryngological Hospital of the University of Vienna in 1919, and is known today as one of the fathers of rhinology.14 (Fig. 1)
Figure 1:
Markus Hajek (1861–1941) reprinted with permission from the Annals of Otology, Rhinology, and Laryngology12
In his 1904 paper “Zur Diagnose und intranasalen chirurgischen Behandlung der Eiterungen der Keilbenhohle und der hinteren Siebbenlabyrinthes”15 [For the Diagnosis and Intranasal Surgical Treatment of Suppuration of the Sphenoid Cavity and the Posterior Septal Labyrinth] Hajek described the treatment of six cases of empyema of the sphenoid and ethmoid sinuses. He reviewed treatment options and explains improvements in his methodology for accessing the posterior ethmoid and sphenoid sinuses. Hajek described a stepwise surgery for reaching these deep cavities. The procedures were carried out under local anesthesia with either topical cocaine or chloroform, requiring intermissions lasting days or weeks between operative steps. During these interval periods, he would scrape away granulation tissue that encroached the operative view until a scar would be formed, clearing his operative access from debris and maintaining a permanent route for future drainage of pus and access for rinses. He recounted the existing forceps of Noebel and Loehnberg were not strong enough to tackle thick bone walls, and he was led to engineer his eponymous bone forceps which remain in popular use today.(Fig. 2) Referring to an encounter with a patient with a collection of pus in the sphenoid sinus he stated:
Wenn ich nun die hintere Partie der an die Keilbeinvorderwand sich anlegenden medialen Wand der hinteren Siebbeinzelle eroffne und die Knochensplitter entferne, dann gelingt es mir mit einem Schlage, die vordere Keilbeinhohlenwand in ihrer ganzen Breite freizulegen. Nichts wird mich dann hinder konnen, vom Ostium sphenoidale aus die ganze vordere Keilbeinhohlenwand zu entfernen. Durch eine derartige Eroffnung der Keilbeinhohle alles, was pathologisch verandert ist, entfernen zu konnen.15
If I now open the posterior part of the medial wall of the posterior ethmoid cell, which is adjacent to the anterior wall of the sphenoid bone, I succeed in striking the anterior sphenoid to expose the cave wall in its entire width…nothing will stop me then to remove the entire anterior wall of the sphenoid bone.
After inserting a hook forceps into the sphenoid ostium and taking down the anterior wall of the sphenoid sinus with bone tongs, he was able to inspect and scrape the sphenoid in its entirety with a curette.
Figure 2: The “Hajek” bone forceps.
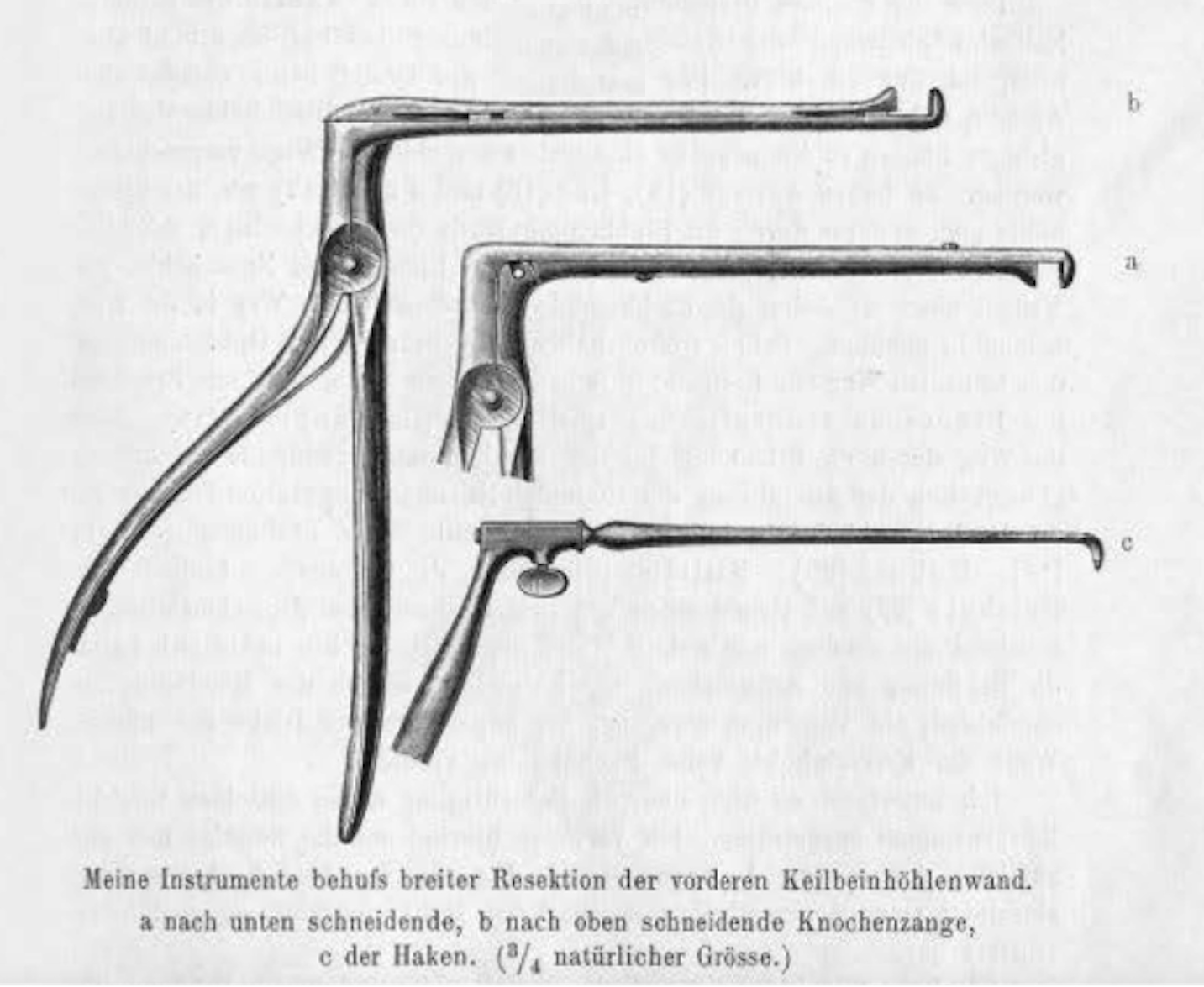
A) Down biting forceps. B) Up-biting forceps. C) The hook (3/4 size). Illustrations reproduced from Hajek’s original paper: Zur Diagnose und intranasalen chirurgischen Behandlung der Eiterungen der Keilbeinhöhle und des hinteren Siebbeinlabyrinthes15
In this account, Hajek proposed the first endonasal method to reach the sphenoid sinus. He stated that previous extracranial methods of reaching the sphenoid sinus required a large external incision, often resulting in unfavorable cosmesis and disfiguring scars. This novel approach had the appeal of accessing both the posterior ethmoid as well as the sphenoid sinuses, allowing for drainage of any hidden locus of infection that would communicate between the two sinuses, leading to lasting remission of symptoms in his patients while avoiding any external incisions. Though he commented that he was eager to explore beyond the opening of the sphenoid sinus, he described scenes of his patients’ jubilation when their symptoms of headache and fetid rhinorrhea were cured, and these positive outcomes precluded him from exploring further. In treating these patients and publishing his findings, Hajek took the first step for the field of rhinology to explore newfound territories to be accessed by the endonasal approach.
Surgical Techniques of Oskar Hirsch
Oskar Hirsch was born in Prerau Czechoslovakia in 1877, and emigrated to Vienna in 1897 for medical school.16,17(Fig. 3) He became interested in the paranasal sinuses early in his career, acquiring a collection of cadaveric specimens with which he conducted a series of annual seminars on the anatomy of the sphenoid sinus and sellar region.17,18 As part of his medical studies, he trained under the direction of Markus Hajek in Vienna.19 Five years after Hajek described the endonasal approach to the sphenoid Oskar Hirsch reports expanding upon Hajek’s approach. In his speech at the Kaiserlich-Königlich (K.K.) Gesellshaft [Society] of Aerzte in Vienna on March 12, 1909, Hirsch credited recent advances in radiology which allowed for the ability to determine hypophyseal tumors extending deep into the sphenoid, and he theorized on a novel method for resecting these tumors without disfigurement:
Die endonasale Methode…bezeichnen wurde sich in praxi folgendermaßen gestalten: Unter Cacainanästhesie wird in einer ersten Sitzung die mittlere Muschel enlfernt, nach einigen Tagen in einer zweiten Sitzung, ebenfalls in Cacainanästhesie, das vordere und hintere Siebbein ausgeräumt, womit die vordere Wand der Keilbeinhöhle in der ganzen Ausdehnung freigelegt erscheint. Nach einer weiteren Pause von einigen Tagen wird wieder in Cacainanästhesie die vordere Keilbeinwand in toto abgetragen und eventuell unter Einschaltung einer weiteren Pause von einigen Tagen die Eröffnung des Hypophysenwulstes und die Schlitzung der Dura vorgenommen.20
The endonasal method…was designed in practice as follows: under cocaine anesthesia, the middle turbinate is removed in a first session, and after a few days in a second session, also with cocaine anesthesia, the front and rear ethmoid are removed, after which the front wall of the sphenoid appears to be exposed in its entire extent. After a further pause of a few days, the anterior sphenoid wall is removed again in total using cocaine anesthesia and, if necessary, a further pause of a few days is used to expose the pituitary gland and its dura.
His idea was met with criticism.20 A few weeks later, on March 26, 1909 he had the opportunity to present his approach at the K.K. Society of Aerzte in Vienna by performing a cadaveric dissection.19 Hirsch credits his former mentor Dr. Hajek in paving the way for this approach:
Diese Methode der Keilbeinhöhleneröffnung durch andere Autoren verbessert und schliesslich von meinen früheren Chef, Herrn Doz. Dr. M. Hajek, so vervollkommnet worden, dass es heutzutage jedem erfahrenen Rhinologen möglich ist, die vordere Wand der Keilbeinhöhle übersicht, ja sogar Polypen aus derselben entfernen kann. Diese von Hajek zur Behandlung des chronischen Keilbeinhöhlenempyems angegebene Operation benütze ich, um mir den Zugang zur Sella turcica zu bahnen.
This method has been improved upon by other authors, and finally, by my former chief, Dr. M. Hajek, it has been so perfected that it is now possible for every experienced rhinologist to survey the anterior wall of the sphenoidal sinus, even to take away polyps from it. I use this operation, described by Hajek for the treatment of chronic sphenoid sinus empyema, to give me access to the sella turcica.
His former mentor, Dr. Hajek was in the audience, and remarked “The rhinologists are grateful to the lecturer for trying to expand the area of their activity by such a delicate and interesting operation as the removal of the pituitary gland.”19 Despite his praise, however, Hajek was critical of Hirsch’s novel method. He questioned the technical feasibility of performing delicate dissection of the pituitary from the minimal accessibility provided via the nostril. He believed the endonasal approach was appropriate for drainage of the sphenoid sinus, but not for the delicate task of dissecting the posterior face of the sphenoid while respecting the cavernous sinus and the internal carotid arteries. He stated, “at such a large distance from the operating area, every small movement at the distal end of an instrument multiplies many times at the proximal end, which could easily become disastrous when the bone cover of the sphenoid sinus was removed.”19 Hajek continued to advocate for the need to open the nose in order to reach and operate safely upon the sella turcica.
Figure 3:
Oskar Hirsch (1877–1965) reprinted with permission from World Neurosurgery
Hirsch was forced to wait until the following year to demonstrate his endonasal approach on a live patient. After a referral from a local ophthalmologist of a 35-year-old female with bilateral optic nerve dysfunction, he was able to perform his novel procedure on March 8, 1910. He first reports successful completion of the procedure in an address to the K.K. Society der Aerzte at Vienna on June 17, 1910. Two months later, on August 27, 1910 he publishes his landmark paper titled Endonasal Method of Removal of Hypophyseal Tumors. With a Report of Two Successful Cases. In this article Hirsch describes in English his experience:21
The operation was done under cocaine anesthesia endonasally and in several sittings…In the first sitting I removed, under cocaine anesthesia, the middle turbinate of the left side…After several days in a second sitting I removed the ethmoid cells… After several days pause I resected in a third sitting the anterior wall of the sphenoidal cavity…After this operation, the hypophyseal prominence, reaching deep into the sphenoidal cavity, was visible…The new feature in my method is the opening of the hypophyseal prominence with a chisel and the exposure of the tumor…I placed on the hypophyseal prominence a small chisel and by careful hammering made a transverse fissure in the bony envelope of the hypophysis tumor. Into this fissure I placed an elevator that is made in the form of a right angle and broke away the bony covering of the hypophyseal prominence in a rather large area. Through this opening in the bone the bluish dura became visible. Although this operation was done without hemorrhage or pain, I did not continue, as I wanted to see if this opening would not suffice to relieve the disturbances caused by the pressure of the tumor. This expectation was not realized and after several days it became necessary to lay bare the tumor itself…With a knife [I] opened the dura along the sphenoidal septum and pulled it away laterally as a flap. Immediately the gray hypophysis tumor arched through the opening into the sphenoidal cavity. I cut into the tumor with a knife and immediately a blood-tinged fluid ran from the nose and mouth. As I again examined the tumor it was smaller and pulsated at the wound margins, between which, on probing, I came into a cavity. I removed a small piece of the cyst wall and did not tampon, but merely placed a small ball of cotton in the anterior nares of the operated side of the nose… Immediately following the operation the patient’s head felt much relieved. She was so slightly disturbed by the operation that she was able to walk with a nurse from the operating room to her ward.21
Hirsch was able to successfully complete his novel endonasal approach over several sittings lasting over five weeks in total. He utilized these interval periods to design new, specialized instruments for the operation, but he estimated that even under the best conditions and after combining stages, the transethmoid transsphenoidal approach to the sella would still require two to three weeks to complete. Hirsch reflects in this 1910 paper that he was unsatisfied with these lengthy interval periods required, citing the dangers of optic atrophy and other progressive symptoms that might develop as a result of the time required to establish adequate access to the sella. After completing his first successful operation he returned to cadaveric dissections to experiment with methods to reduce the operating time.
He reported being influenced by a fellow otolaryngologist Gustav Killian, who had popularized a technique of performing a rapid resection of the nasal septum. Killian’s method required elevating the mucous membrane off the septum with the use of a blunt elevator before resecting the cartilaginous and bony nasal septum.22 Killian reported successfully completing the operation in as little as 20 minutes, and Hirsch theorized that by expanding the elevation of the mucous membrane, he could cleanly resect the rostrum sphenoidale as well as expose the anterior wall of the sphenoid septum without the need for lengthy intervals between steps. In the same 1910 paper that Hirsch described his endonasal transethmoid transsphenoidal approach, he details steps for his improved, single-staged transseptal procedure as follows:
An incision is made along the anterior edge of the quadrangular cartilage and the mucous membrane is raised by means of raspatorium, together with perichondrium and periosteum from the cartilage and bone … the membranes are now held apart by a nasal speculum and in this way a medial nasal cavity forms in which one sees the bare cartilage. This is removed with one sweep of the cartilage knife and the vomer and perpendicular plate of the ethmoid are resected with the aid of a bone forceps…Mucous membrane is separated from the anterior surface of the sphenoid as far as the ostium sphenoidale, so that the raspatorium falls into the sphenoidal cavity. Now, through this sack of mucous membrane one removes [the] posterior part of the vomer and the rostrum sphenoidale with the bone forceps, and with several strokes of a chisel one breaks through the anterior wall of the sphenoid cavity and after removing the sphenoidal septum one sees the hypophyseal prominence in its entirety. After opening the sella turcica and the dura of the hypophysis, respectively, the hypophyseal tumor lies free in the sphenoidal cavity.21
By bypassing the ethmoid sinuses, Hirsch was able to avoid the time needed for fibrosis and healing between stages, establishing access to the pituitary in as little as one sitting. This alternative approach of elevating the mucous membrane from its smooth architecture was relatively simple and if performed properly in an avascular plane would cause minimal bleeding, thereby maintaining the access and visibility to the sphenoid. By incorporating Killian’s technique, Hirsch was able to easily resect the nasal septum and create a common compartment where bimanual instruments could communicate with direct access to the anterior wall of the sphenoid sinus.(Fig. 4)
Figure 4: Schematic of Hirsch’s Single Stage Approach.
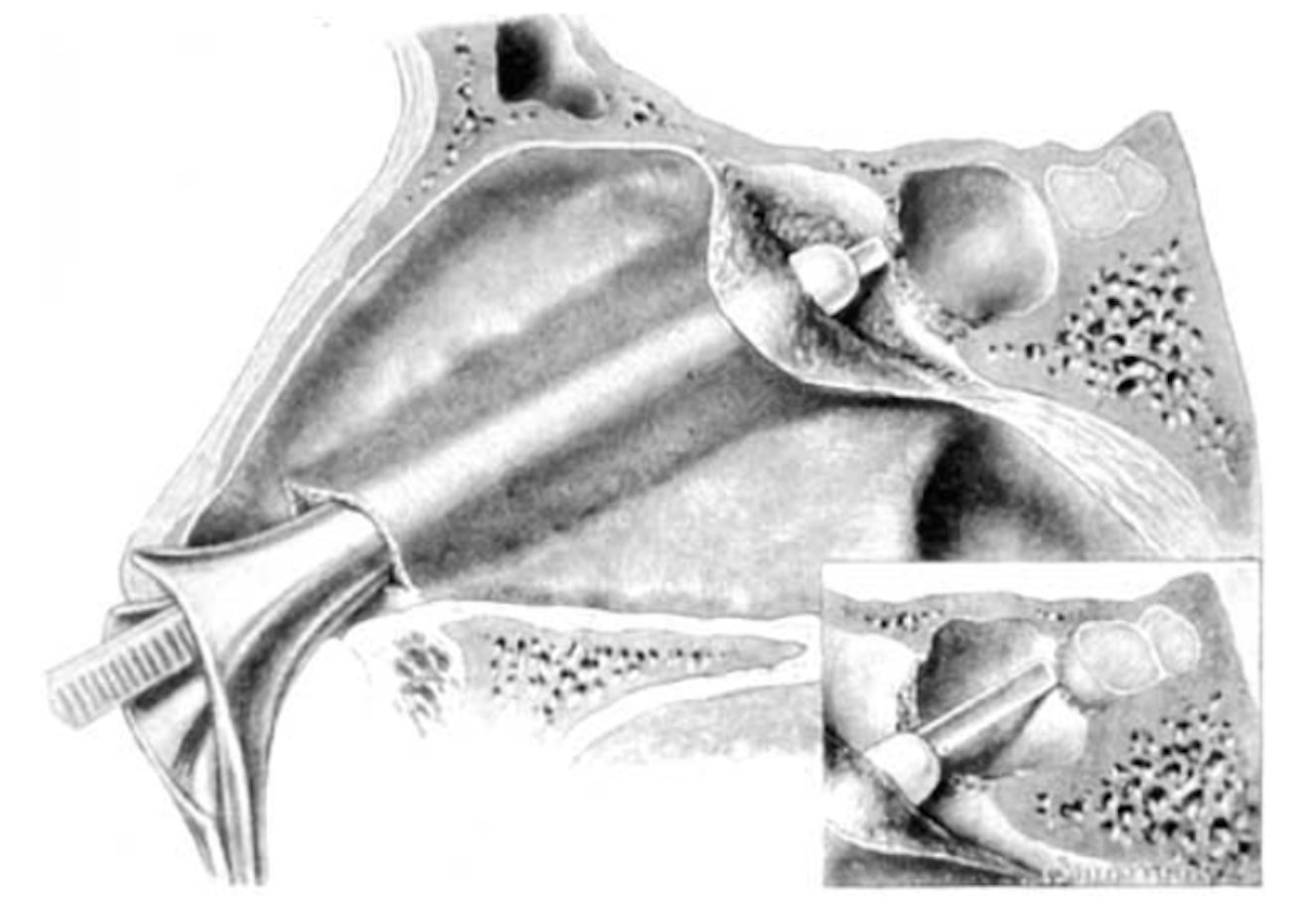
Illustration demonstrating Hirsch’s endonasal submucosal transseptal approach to the sella turcica, inspired by Killian. Reproduced from a slide in Dr. Laws’ collection
Discussion
In his 1910 paper, Hirsch described performing a novel procedure that required five weeks and multiple intervals. Within three months Hirsch modified the approach to be completed in one sitting, and successfully performed the procedure on a live patient.(Fig. 5) It is remarkable that in just under two pages of text, Oskar Hirsch redefines the field of pituitary surgery, describing both his original and his shortened approaches in the same article.
Figure 5: Timeline of Events.
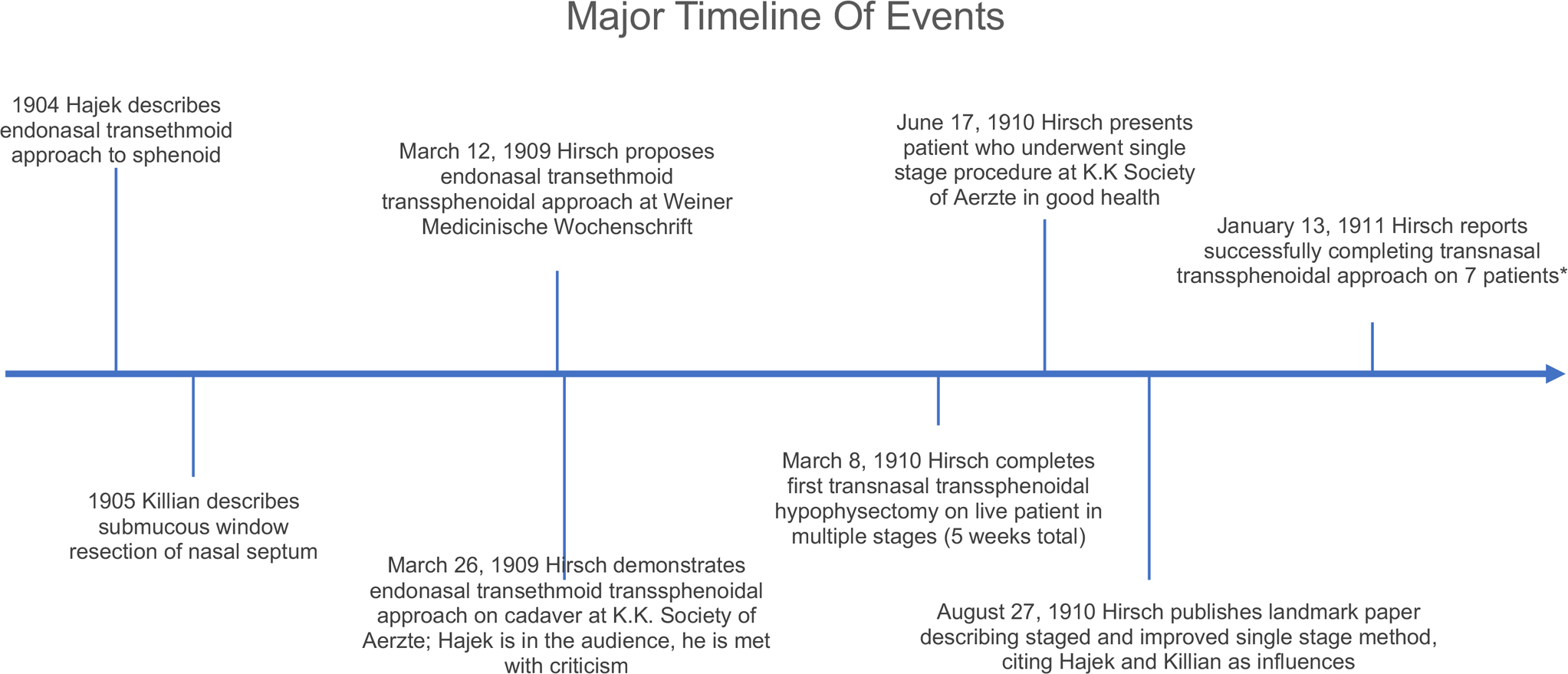
*Six of the seven patients who underwent the operation survived. Hirsch emphasizes that none of these patients had meningitis and the one patient who died did so due to cardiac failure and not aspiration pneumonia. Dates not represented to scale
In 1938, Hirsch emigrated to Boston after being expelled from Austria by the Nazi regime. Hirsch collaborated with Hannibal Hamlin as he was not allowed to operate independently at Massachusetts General Hospital.23 Together they promulgated the advantages of the endonasal transsphenoidal approach for resection of pituitary tumors in a time when transcranial approaches were favored by the vast majority of neurosurgeons in the United States.24
Over the remainder of his career, Hirsch would perform his endonasal transseptal transsphenoidal approach on 413 patients, with outstanding results. Between 1919 to 1937 he reported a mortality rate of 5.4% after operating on 277 patients. In the decade after World War II with the introduction of antibiotics, his mortality rates dropped to 1.4%, and he began to introduce radium implants into the sella postoperatively to prevent tumor recurrence.25,26
At the turn of the century there was a multitude of voices attempting to describe the optimal route for accessing the sella turcica. There were many trailblazers describing novel approaches for removing hypophyseal tumors, and the authors would be remiss to exclude the names of other contemporary contributors to the field including Schloffer, Cushing, Horsley, Halstead, Kanavel, and others.(Table 1) In few of these contemporary approaches was it possible to remove the entirety of the tumor, but even partial resection was often sufficient in improving patient symptoms.27
It was the innovations of two otolaryngologists, however, who paved the way for the endonasal transsphenoidal approach that has since become the foundation of the resection of hypophyseal tumors that is widely used today. This approach was favored by very few neurologic surgeons until almost four decades after Hirsch’s landmark paper.28,29 Coincidentally, Harvey Cushing performed his first sublabial transseptal transsphenoidal hypophysectomy within the same month as Hirsch’s first approach, borrowing from Kanavel’s inferior nasal approach, Halstead’s sublabial incision, and Kocher’s submucous septal resection, but Cushing favored the transcranial approach for greater visibility of the sella, and he completely abandoned the transsphenoidal approach altogether by 1929.23 Eventually the endonasal transseptal transsphenoidal approach became the mainstay of surgical practice due to the advantages of providing extensive access to the sella turcica, avoiding severe disfigurement, and resulting in favorable survival outcomes. Though great technological strides have been made in the past century, today’s endonasal approach for the resection of pituitary tumors maintains many of the core themes from Hirsch’s original method first described in 1909.
One might criticize our study on several grounds. Limitation of our methodology includes relying on relatively few historical records with their associated contextual translation. However, we felt confident that the references studied provided enough confirmation for our conclusions. Lastly, the relationship of mentor-mentee between Hajek and Hirsch is implied from primary references as very few references were discovered relating specifically to their academic careers.
Oskar Hirsch’s two major influences, Markus Hajek and Gustav Killian, were both Otolaryngologists, and each provided crucial pieces to devising his novel endonasal transsphenoidal approach. In contrast to the extracranial approaches his neurosurgery colleagues were proposing at the time, his otolaryngology training under Hajek encouraged Hirsch to explore the limits of the endonasal approach. Proceeding endonasally allowed him to devise a rapid, minimally invasive approach to the sella turcica that avoided major facial disfigurement, and drawing heavily upon Hajek’s approach to the ethmoid and sphenoid sinuses, he was the first to propose a purely endonasal approach to the pituitary gland in 1909. In order to expedite the operation, he incorporated fellow otolaryngologist Killian’s techniques in devising his novel transseptal approach to the sphenoid sinus, which he successfully completed the following year.
Acknowledgments
This project was supported in part by the National Institutes of Health (NIH) Institutional National Research Award, T32 #5T32DC000040 (NB)
Footnotes
Conflict of Interest Statement: The authors have no conflicts of interest to disclose
References
- 1.Horsley V Address in surgery delivered at the seventy-fourth annual meeting of the British Medical Association, on the technique of operations on the central nervous system. The British Medical Journal 1906:411–423. [Google Scholar]
- 2.Kiliani OG II. Some remarks on tumors of the chiasm, with a proposal how to reach the same by operation. Annals of Surgery 1904; 40:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krause F. Hirnchirurgie [Brain surgery]. Dtsch Klin 1905; 8:953–1024. [Google Scholar]
- 4.Schloffer H. Zur frage der Operationen an der Hypophyse. Beitr Klin Chir 1906; 50:767–817. [Google Scholar]
- 5.Kocher T Ein fall von hypophysis-tumor mit operativer heilung. Deutsche Zeitschrift für Chirurgie 1909; 100:13–37. [Google Scholar]
- 6.Kanavel AB. The removal of tumors of the pituitary body by an infranasal route: A proposed operation with a description of the technic. Journal of the American Medical Association 1909; 53:1704–1707. [Google Scholar]
- 7.Halstead AE. Remarks on an operative treatment of tumors of the hypophysis. Gynecology and Obstetrics 1910; 10:494–502. [Google Scholar]
- 8.Proust R La chirurgie de l’hypophyse. J Chir (Paris) 1908; 1:665–680. [Google Scholar]
- 9.Chiari O Ueber eine modifikation der schlofferschen operation von tumoren der hypophyse. Wien Klin Wochenschr 1912; 25:5–6. [Google Scholar]
- 10.Cushing H III. Partial hypophysectomy for acromegaly: with remarks on the function of the hypophysis. Annals of surgery 1909; 50:1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Professor Marcus Hajek 1861–1941. The Laryngoscope 1941; 51:470–475. [Google Scholar]
- 12.Hajek Markus. Annals of Otology, Rhinology & Laryngology 1941; 50:581–583. [Google Scholar]
- 13.Freud E, Lederer FL, Berberich J et al. Marcus Hajek 1861–1941. ORL 1942; 4:175–176. [Google Scholar]
- 14.Seitz PR. Markus Hajek, his students and friends (1907–1941). Otolaryngology--Head and Neck Surgery 1997; 116:279–284. [DOI] [PubMed] [Google Scholar]
- 15.Hajek M Zur Diagnose und intranasalen chirurgischen Behandlung der Eiterung der Keilbeinhohle und des hinteren Siebbeinlabyrinths. Arch Laryngol Rhinol 1905; 18:H1. [Google Scholar]
- 16.Hamlin H In memory of Prof. Oskar Hirsch. Monatsschrift fur Ohrenheilkunde und Laryngo-Rhinologie 1967; 101:51–53. [PubMed] [Google Scholar]
- 17.Hirsch HHO. Hirsch 1877–1965. Surg Neurol 1981; 16:391–393. [DOI] [PubMed] [Google Scholar]
- 18.Hirsch O Demonstration eines nach einer neuen methode operiten hypophysentumors. Verh Dtsch Ges Chir 1910; 39:51–56. [Google Scholar]
- 19.Hirsch O Offizielles Protokoll der k.k. Gesellschaft der Aerzte in Wien. Wiener Klinische Wochenschrift 1909; 13:473–474. [Google Scholar]
- 20.Hirsch O Eine neue Methode der endonasalen Operation von Hypophysentumoren. Wien Med Wochenschr 1909; 59:636–638. [Google Scholar]
- 21.Hirsch O Endonasal Method of Removal of Hypophyseal Tumors With Report of Two Successful Cases. Journal of the American Medical Association 1910; 55:772–774. [Google Scholar]
- 22.Killlan G, Foster EE XXIII. The submucous window resection of the nasal septum. Annals of Otology, Rhinology & Laryngology 1905; 14:363–393. [Google Scholar]
- 23.Cohen-Gadol AA, Laws ER, Cole CD, Kan P, Couldwell WT. Harvey Cushing and Oskar Hirsch: early forefathers of modern transsphenoidal surgery. Journal of neurosurgery 2005; 103:1096–1104. [DOI] [PubMed] [Google Scholar]
- 24.Lanzino G, Laws ER. Pioneers in the development of transsphenoidal surgery: Theodor Kocher, Oskar Hirsch, and Norman Dott. Journal of neurosurgery 2001; 95:1097–1103. [DOI] [PubMed] [Google Scholar]
- 25.Hirsch O. Symptoms and treatment of pituitary tumors. AMA Archives of Otolaryngology 1952; 55:268–306. [DOI] [PubMed] [Google Scholar]
- 26.Hirsch O Pituitary tumors: A borderland between cranial and trans-sphenoidal surgery. New England Journal of Medicine 1956; 254:937–939. [DOI] [PubMed] [Google Scholar]
- 27.Hirsch O Ueber hypophysentumoren und deren behandlung. Klin Monastsbl Augenheilkd 1930; 85:609. [Google Scholar]
- 28.Greenblatt SH. A history of neurosurgery: in its scientific and professional contexts. Thieme, 1997. [Google Scholar]
- 29.Stone JL, Meglio G, Laws ER. Development of pituitary surgery: the Chicago contributions. Journal of the American College of Surgeons 2005; 201:784–805. [DOI] [PubMed] [Google Scholar]


