Abstract
Objective
The purpose of the study was to assess the clinical efficacy and safety of a combined perfusion suction platform with pressure feedback control function and an ureteroscopic suction sheath that can measure the ureteropelvic pressure in implementing lithotripsies.
Methods
Fifty-two patients who underwent lithotripsy under intelligent monitoring of ureteral intraluminal pressure from June 2016 to January 2018 were retrospectively recruited. The inclusion standard was stone diameter >1.5 cm but <2.5 cm. After the 12/14 Fr suction sheath was placed, manometer interface and suction interface of the sheath were connected to the platform via the pressure sensor and suction tube, respectively. The ureteroscope was connected to the platform perfusion pump, and the crushed stones were aspirated out under negative pressure.
Results
According to the location of the stone, 21 (40.4%) cases were classified as upper ureteral stones, 19 (36.5%) were midureteral stones, and 12 (23.1%) were lower ureteral stones. Forty-seven patients underwent successful primary sheath placement and lithotripsy with a mean operative time of 34.5 (standard deviation 18.3) min. Retrograde stone migration did not occur. There were eight patients with hematuria postoperatively. Serious complication was 1.9% with one case of ureteral perforation. Stone clearance was 95.7% at Day 1–2 postoperatively, and 100% at Day 30 postoperatively.
Conclusion
Ureteroscopic lithotripsy with intelligent pressure control using our device improved the efficiency of the lithotripsy and rate of stone clearance. The safety of the operation can be ensured. It is worth popularization and application in clinical practice.
Keywords: Suction, Ureteroscopy, Intelligent pressure control, Ureteral calculi
1. Introduction
Large volume ureteral stones can be managed by ureteroscopic laser lithotripsy, laparoscopic lithotripsy, percutaneous nephrolithotomy as well as small incision open lithotomy. There has been no uniform standard treatment. Laparoscopic lithotomy has a high-definition stone removal rate but with a certain degree of trauma, which is suitable for only a small number of patients. Extracorporeal shock wave lithotripsy with less trauma but lower stone clearance rate is primarily for ureteral stones of <1.0 cm and those patients without ureteral stenosis or compacted stones. Ureteroscopic holmium laser lithotripsy through natural lumen is of high stone clearance efficiency, low incidence of complications, and no skin wounds. It is the major method for the treatment of large ureteral stones [1,2].
As early as 1974, Takayasu and Aso [3] applied the ureteral access sheath (UAS) to ureteroscopic lithotripsy [3]. Studies have shown that UAS can significantly shorten the operation time, reduce the intraluminal pressure of the renal pelvis, effectively protect the scope, and reduce the cost of surgery [4]. Previously, Zeng et al. [5] did further improvement on the UAS by designing a UAS with negative pressure suction function. This UAS was found to be capable of preventing the upward movement of stones, ameliorating the stone clearance rate, having a clear vision, and reducing intraluminal pressure [5]. Regardless, the traditional UAS still does not function perfectly, and the efficiency of stone clearance can be further improved. There was no available methods to monitor and control intraluminal pressure during the operation, which limits the clinical application of the UAS. Given the deficiency of traditional UAS, we have designed a perfusion suction platform with pressure feedback control function (abbreviated as platform) and a ureteral suction sheath (abbreviated as suction sheath) that can measure the intraluminal pressure of ureter. With the combination of the two devices, we were able to perform suction lithotripsy with intelligent monitoring and control ureteral and intrarenal pressure. In this retrospective study, we sought to assess its clinical efficacy and safety in treating ureteral stones with a diameter of >1.5 cm but <2.5 cm.
2. Patients and methods
2.1. General information
The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Ethical and regulatory approvals were sought and obtained from the Affiliated Ganzhou Hospital of Nanchang University (Approval #2016–009). Informed consents were obtained from all individual participants included in the study. Fifty-two patients who underwent lithotripsy with intelligent monitoring of ureteral intraluminal pressure from June 2016 to January 2018 were retrospectively analyzed.
2.2. Platform and suction sheath introduction
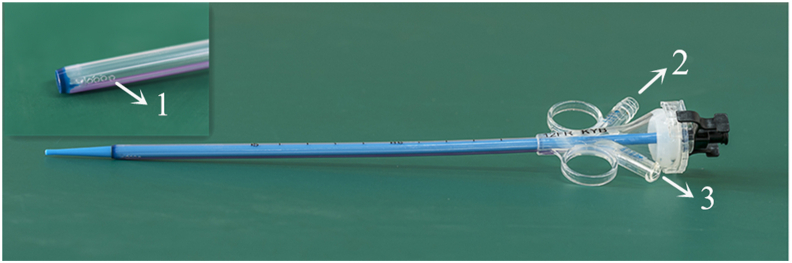
The medical perfusion suction platform (patent No. ZL201420055766.5, Fig. 1) consists of a major control unit, a perfusion device, a suction device, and a pressure feedback device, which can set perfusion flow, control pressure value, alert pressure value, and limit value. The platform is with four operating modes, which are automatic (e.g., perfusion, suction, pressure monitoring, and pressure feedback control), semi-automatic (e.g., perfusion and pressure monitoring), simple perfusion, and simple suction, with ability to display the actual suction pressure and intraluminal pressure of the renal pelvis in real time. The flexible pressure-measuring ureteroscopic sheath (Fig. 2) is 12 Fr in inner diameter, 14 Fr in outer diameter, and 25 cm or 35 cm in length. It employs a transparent material to better and directly observe the mucosal condition through the ureteral sheath. The suction sheath is outfitted with a built-in baroreceptor to measure the intraluminal pressure. There are two connecting channels at the back end, which are connected to the negative pressure suction device and the pressure monitoring feedback device. In these channels, the negative pressure suction channel is capable of automatically aspirating the stone, and the pressure monitoring feedback channel can monitor and automatically obtain feedback of the intraluminal pressure.
Figure 1.
The medical perfusion suction platform.
Figure 2.
Structure of the ureteral access sheath with the function of suction and pressure monitor. 1. Pressure-sensitive tip; 2. The suctioning channel; 3. The pressure monitoring feedback channel.
After rigorous in vitro testing and animal experiments to achieve the desired goal [[6], [7], [8]], the above platform and suction sheath were approved by the Ethics Committee of Nanchang University (Approval #2016–009).
2.3. Surgical methods
All patients were given general anesthesia. For the middle and lower ureteral stones, a 25 cm or 35 cm suction sheath ureteroscope and the lithotomy position were employed. For the upper ureteral stones, a 35 cm suction sheath ureteroscope was employed and the contralateral oblique supine position was taken (Fig. 3). A zebra guidewire was placed under direct vision under semi-rigid ureteroscopy with a 7.5 Fr semirigid ureteroscope (Karl Storz, Tuttlingen, Germany) to confirm that there was no significant stenosis and distortion of the ureter. The 12/14 Fr suction sheath was then placed under the guidance of the zebra guide wire. Under ureteroscopy, the front end of the suction sheath was confirmed to be 0.5 cm below the ureteral stones. The suction sheath manometer interface and the suction interface were connected to the platform through the pressure sensor and the suction tube, respectively. After water injection, pressure sensing system was set to zero through the platform. The platform was adopted in a fully automated mode with an intracavitary pressure control value of −9 mmHg to −2 mmHg (1 mmHg=0.133 kPa), with a perfusion flow of 50 mL/min to 100 mL/min, an intracavitary pressure alert value of 20 mmHg, and a limit value of 30 mmHg [[9], [10], [11], [12]]. The ureteroscope was then connected to a platform perfusion pump. During the operation, a 200-micron holmium laser fiber (Lumenis Inc, San Jose CA, USA) was employed for lithotripsy. The power of the lithotripsy was set at 0.6−0.8 J and 20–30 Hz. During the lithotripsy, the scope was continuously moved back and forth inside the sheath, and the distance between the front and the back ranged from 2 mm to 3 mm, which did well in the aspiration of stones that could pass the gap between the lens and the sheath. Stone gravels larger than the lens sheath space but smaller than the inner diameter of the suction sheath could be aspirated by negative pressure after slowly withdrawing the lens. A 4.6 Fr or 5.0 Fr double-J tube was left in place for 3–4 weeks after operation. These operations were performed by experienced senior doctors with intraoperative real-time observation of changes in ureteral pressure. Blood routine, renal function, and electrolytes were postoperatively reviewed in the 1st day. If there were postoperative fever, low blood pressure, etc., the blood routine, electrolytes, and procalcitonin should be checked. Immediately after the surgery from Day 1 to Day 3 and Day 30, kidneys, ureters and bladder examination was performed to rule out residual stones. For X-ray negative stones, computed tomography (CT) scan was performed. No residual stones or residual stone diameter <4 mm was defined as stone-free. The operative time is defined as the time from the placement of the suction sheath to the end of surgery.
Figure 3.
Contralateral oblique supine position.
2.4. Statistical methods
SPSS 22.0 statistical software (IBM, New York, NY, USA) was employed to analysis the data. Measurement data meeting normal distribution were denoted as mean±standard deviation (SD); paired t-test was employed to compare preoperative and postoperative blood index values. Furthermore, p<0.05 was considered statistically significant.
3. Results
Of the 52 cases, there were 18 males and 34 females with a mean age of 42.0 years and SD of 16.3 years. There were surgical indications for all the patients without absolute contraindications. The diameter of stone was greater than 1.5 cm but less than 2.5 cm for all the patients. Stone size was defined as the largest linear diameter of the index stone with a mean diameter of 18.8 mm and SD of 3.5 mm. There were 12 cases of lower ureteral stones, 19 cases of middle ureteral stones, and 21 cases of upper ureteral stones. There were 41 cases of incarceration compacted stones, two cases of bilateral ureteral stones, four cases with relatively solitary kidney, and three cases of renal dysfunction. There were 38 cases with 10–20 white blood cells (WBCs) per high-power field (HPF) in urine sediment and six cases of severe urinary tract infection with 30–40 WBCs per HPF in urine sediment. All the urinary tract infection patients were treated with antibiotics for 1–3 days before surgery and those with urine WBCs negative or <20 WBCs per HPF were considered for surgery. Demographic data and stone characteristics are summarized in Table 1.
Table 1.
Demographic data and stone characteristics.
| Variable | Value |
|---|---|
| Patient, n | 52 |
| Age, mean±SD, year | 42.0±16.3 |
| Gender, n | |
| Male | 34 |
| Female | 18 |
| Stone position, n (%) | |
| Upper ureter | 21 (40.4) |
| Middle ureter | 19 (36.5) |
| Lower ureter | 12 (23.1) |
| Stone size, mean±SD, mm | 18.8±3.5 |
| CT value, mean±SD, HU | 835±318 |
| Compact stone, n (%) | 41 (78.8) |
CT, computed tomography; HU, Hounsfield unit; SD, standard deviation.
Among the 52 patients, the sheaths were successfully placed in 47 cases (33 females and 14 males) at Stage 1 with a success rate of approximately 90%. The success rate of sheath placement for females was 97.1% (33/34), and that of males was 77.8% (14/18). There were five cases with failed sheath placement. Two cases of ureteral stricture were successfully treated with pediatric ureteroscopic lithotripsy, and three cases of upper ureteral stones were treated with percutaneous nephrolithotomy. None of the patients had ureteral stones retrogradely moved to the kidney. Eight cases were complicated by significant hematuria after surgery, which was graded as Grade I by the Clavien-Dindo grading [13]. One of them had abnormal liver function and three had abnormal renal function, which improved with conservative treatment for 1–2 days. None of the patient received blood transfusion after surgery. One patient (1.9%) had an intraoperative sheath injury to the ureter, resulting in ureteral perforation, a Grade III injury according to Traxer classification [14]. One of the patients experienced ureteral stent migrating down to the bladder shortly after surgery, and presented low back pain after the operation and fever with a temperature up to 39.1 °C. CT examination disclosed extravasation of fluid around the ureter. The patient underwent emergency ureteral stenting and abdominal catheter placement for drainage. Mean operative time was 34.5 (SD: 18.3) min; mean length of hospital stay was 2.1 (SD: 1.1) days. Review of abdominal plain films 1–2 days after surgery showed that the stone clearance rate was 95.7% (45/47), and the stone clearance rate was 100% (47/47) at Day 30 after surgery. Stone specimens were successfully collected in 45 patients after surgery for stone composition analysis, in which 84.4% (38/45) of the stones were calcium oxalate; four were calcium phosphate stones; two were calcium carbonate stones; and one was uric acid stone. Intraoperative and postoperative outcomes are summarized in Table 2.
Table 2.
Intraoperative and postoperative outcomes.
| Parameter | Value |
|---|---|
| Operative time, mean±SD, min | 34.5±18.3 |
| Failed semi-rigid ureteroscope, n (%) | 5 (9.6) |
| Ureteral stricture | 2 (3.8) |
| Excessive kink of the ureter | 3 (5.8) |
| Stone-free rate, n (%) | |
| Immediate after operation (Day 1–2) | 45 (95.7) |
| One month after operation (Day 30) | 47 (100.0) |
| Postoperative complication, n (%) | 9 (19.1) |
| Complication (Clavien-Dindo categorization), n (%) | |
| Hematuria (Clavien Grade I) | 8 (17.0) |
| Stone upward migration (Clavien Grade III) | 0 |
| Ureteral extravasation (Trexer Grade III) | 1 (2.1) |
| Postoperative hospitalization duration, mean±SD, day | 2.1±1.1 |
SD, standard deviation.
Note: among the 52 patients, the sheaths were successfully placed in 47 cases.
4. Discussion
In 1912, ureterorenoscopy (URS) was first employed to treat ureteral stones successfully [15]. With the improvement of optical technology, the gradual reduction of scope body size, and the advent of holmium laser, the lithotripsy efficiency of URS has been greatly improved, which has become the main method for ureteral stones. Heers and Turney [16] showed that the number of ureteroscopies performed for stone disease in England increased by as much as 49.7% from 12 062 in 2009–2010 to 18 055 in 2014–2015 [16]. Despite of this, deficiencies remained in ureteroscopies during the treatment of large volume stones. Normal pathological intrarenal pressures (IRPs) ranged from zero to a few cmH2O (1 cmH2O=0.098 kPa). Pyelovenous backflow may occur at pressure range of 13.6–27.2 cmH2O. During upper tract endourology, pyelorenal backflow, sepsis, and renal damage were related to increasing IRPs [17]. Currently, it is recommended that IRP should be controlled at a value less than 30 cmH2O during URS surgery, preventing high ureteral and renal pelvic perfusion pressure during surgery. However, low flow perfusion often leads to unclear vision, and insufficient fluid circulation in the lumen. Continuous excitation of the holmium laser is prone to generate a large amount of heat, causing thermal damage to the ureteral mucosa, and in a long-term leading to ureteral stricture. Therefore, the Holmium laser must be intermittently excited during the operation but lithotripsy time was extended. There are two major methods for the removal of residual stones during the operation. One method is to clean the residual stones immediately during the operation and to repeatedly withdraw the lens or cleaning the residual stones using a set of stone baskets and stone clamps. These methods extend the operation time and easily induce edema and injury of the ureteral mucosa. Also, in the traditional URS, after indwelling a ureteral stent after in situ lithotripsy, it takes a long time to discharge the stone fragments spontaneously with a risk of “stone street” formation, requiring secondary operation. In addition, some stones move up to the kidney during the surgery. It has been reported that about 8.0%–37.5% of stones in traditional URS for massive ureteral stones moved up to the kidney, resulting in the need for other auxiliary methods to clean up stones [18], which is associated with increasing the cost of treatment and the possibility of secondary trauma. The above reasons obviously affect the efficiency of URS.
There are relatively few studies on ureteroscopic treatment of large ureteral stones. In a prospective randomized controlled study by Kumar et al. [19], 50 patients with ureteral stones of >2 cm underwent URS with mean operative time of 47 min, retreatment rate of 8%, stone upward migration rate of 8%, auxiliary procedure rate of 26%, and stone-free rate of 76% at 3 months after surgery. The rate of complications with Clavien Grade ≥III was 18.3% [19]. In the study by Kadyan et al. [20], URS was performed in 60 patients with stones of >1.5 cm with mean operative time of 62.8 min, retreatment rate of 8%, auxiliary procedure rate of 10%, and stone-free rate of 71.6% at 3 months after surgery. Rate of proximal migration of stone was 15%. The rate of complications with Clavien Grade ≥III was 10.0% [20]. For 41 patients with ureteral stones of >1.5 cm who underwent URS in the study by Bozkurt et al. [21], their operation time was 92 min; stone upward migration happened in 15 cases, and the rate of complications with Clavien Grade ≥IIIa was 36.6%; stone-free rate at 1 month after surgery was 82.9%. Given the fact that it often requires a long duration of surgery for large ureteral stones using the existing URS treatment, the stones can easily move up into the kidney, and part of them requires secondary surgery (adjuvant therapy). It is an urgent situation requiring us to develop new surgical approach to improving the lithotripsy efficiency.
Given the deficiency of traditional UAS, we designed a perfusion suction platform with pressure feedback control function and a flexible ureteroscopic suction sheath that can measure the ureteral pressure of the renal pelvis. Using the combination of the two methods, the suction and lithotripsy of the ureter and the internal pressure of the renal pelvis can be intelligently monitored, and certain clinical efficacy has achieved in treating upper urinary tract stones. The suction sheath we designed includes a manometer channel and a suction channel. The sheath is made of transparent hydrophilic material, which is capable of monitoring the intrarenal pressure during the operation and also giving the pressure feedback. The intraoperative ureteral pressure is set to a negative pressure state. When the intraluminal pressure is less than the control value, the negative pressure suction stops working; when the intraluminal pressure is within the control value and the alert value, the negative pressure suction adjusts the attraction size according to the intraluminal pressure value. When the intraluminal pressure is higher than the pressure alert value, the platform automatically alarms and implements a protective shutdown, and the intraluminal pressure value should decrease to a safe range before it can be restarted. Previous animal experiments and clinical applications of ureteroscope for the treatment of kidney stones have achieved good results [6,22].
For the middle and lower ureteral stones, lithotomy position was adopted. When the intraluminal pressure of the ureter was a negative value, the stones would be absorbed into the front end of the sheath and did not move upwards. There was no need to change the body position to prevent the stones from moving upwards. For treating upper segmental ureteral stone using the contralateral oblique supine position, the position of the ureteral orifice and the ureter tend to be in a straight line. Intraoperative renal pelvis outlet was at a lower level; the upper segment of the ureter and renal pelvis formed a slope angle; the gravity of the stone itself and negative pressure suction made the stone difficult to move up into the kidney [23]. Stone fragments were immediately attracted and cleared. In this study, none of the patients had ureteral stone moving up into the kidney. This result was superior to the traditional URS treatment of large ureteral calculi. One (1.9%) of the patients had ureteral perforation, which was primarily due to severe distortion, ureteral stiffness, and poor activity. Although the zebra guidewire was successfully placed, there was still a ureteral perforation. We recommend that if the ureter is severely distorted, it is necessary to change the operation to percutaneous nephrolithotomy or laparoscopic ureterolithotomy as soon as possible. It is not allowed to be forced or repeatedly placed on the sheath, otherwise ureteral injury will be caused. Nevertheless, the incidence of serious complications of Traxer Grade ≥III was lower than that of traditional URS.
Compared with the traditional URS, intelligent pressure-controlled ureteroscopic lithotripsy is safer for maintaining ureteral intraluminal pressure as negative pressure in implementing lithotripsy intraoperatively, and reducing intraoperative bacterial and endotoxin reflux absorption. In this study, there was no case of postoperative sepsis and bacteremia. This novel surgical technique also shortened the operation time. The intraoperative flow rate here was controlled at 50–150 mL/min, with a purpose to maintain a high flow perfusion state and avoid thermal damage to the ureteral mucosa with continuous holmium laser excitation during lithotripsy, with a maintained clear operative field but without “haze” phenomenon. The efficiency of lithotripsy is therefore improved, with a shorter operative time without excessive water absorption and complications such as hypothermia comparing to traditional URS for the treatment of large-volume ureteral calculi [[19], [20], [21]]. In this study, intraoperative holmium laser lithotripsy was set to be as high-frequency low-energy. The stone was broken into pieces below 2 mm. Small gravels were sucked out via the gap between the lens body and sheath under negative pressure. Gravel particles larger than the sheath gap but less than the UAS in diameter were sucked out by withdrawing the scope intermittently. The residual stones could be cleaned immediately during the operation. In this study, the stone clearance rate immediately (Day 1–2) after surgery was 95.7%, while it was 100% at Day 30 after surgery. No case of ureteral stone street occurred. Compared with conventional URS [[19], [20], [21]], the stone clearance rate was significantly improved.
In this study, the use of intelligent pressure-controlled URS is preliminarily explored; the number of studied cases is small; and postoperative follow-up time is still short. Whether the ischemia of ureteral mucosa caused by UAS sheath placement will cause ureteral stricture is being followed up. A randomized controlled study with a larger case number is warranted to further assess the clinical value of this intelligent pressure-controlled URS technique.
5. Conclusion
Ureteroscopic lithotripsy using an intelligent pressure-controlled device (platform and suction sheath) is capable of maintaining negative pressure in the ureteral lumen and renal pelvis, maintaining high flow perfusion during surgery, and having a clear surgical visualization. During the lithotripsy, the holmium laser can continuously excite the lithotripsy without causing thermal damage to the ureter. The residual stones can be cleaned immediately during the operation, thereby improving the efficiency of lithotripsy and stone clearance and ensuring the safety of the operation. It is worth popularization and application in clinical practice.
Author contributions
Study design: Leming Song, Donghua Xie.
Data acquisition: Yuming Zhong, Chunxiang Luo, Xiaohui Liao, Tairong Liu, Xiaoling Deng, Lunfeng Zhu.
Data analysis: Yuming Zhong, Chunxiang Luo, Xiaohui Liao, Donghua Xie.
Drafting of manuscript: Yuming Zhong, Donghua Xie.
Critical revision of the manuscript: Donghua Xie, Leming Song.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
This study was funded by Major Science and Technology Projects of Jiangxi Provincial Science and Technology Department (20152ACG70009).
Footnotes
Peer review under responsibility of Tongji University.
References
- 1.Türk C., Neisius A., Petřík A., Seitz C., Skolarikos A., Somani B., et al. EAU guidelines on urolithiasis. 2017. https://uroweb.org/guideline/urolithiasis Available at:
- 2.Taguchi K., Cho S., Ng A., Usawachintachit M., Tan Y., Deng Y., et al. The Urological Association of Asia clinical guideline for urinary stone disease. Int J Urol. 2019;26:688–709. doi: 10.1111/iju.13957. [DOI] [PubMed] [Google Scholar]
- 3.Takayasu H., Aso Y. Recent development for pyeloureteroscopy: guide tube method for its introduction into the ureter. J Urol. 1974;112:176–178. doi: 10.1016/s0022-5347(17)59675-5. [DOI] [PubMed] [Google Scholar]
- 4.Santos J.M.R. Ureteroscopy from the recent past to the near future. Urolithiasis. 2018;46:31–37. doi: 10.1007/s00240-017-1016-8. [DOI] [PubMed] [Google Scholar]
- 5.Zeng G., Wang D., Zhang T., Wan S. Modified access sheath for continuous flow ureteroscopic lithotripsy: a preliminary report of a novel concept and technique. J Endourol. 2016;30:992–996. doi: 10.1089/end.2016.0411. [DOI] [PubMed] [Google Scholar]
- 6.Zhu X., Song L., Xie D., Peng Z., Guo S., Deng X., et al. Animal experimental study to test application of intelligent pressure control device in monitoring and control of renal pelvic pressure during flexible ureteroscopy. Urology. 2016;91:242.e11–242.e15. doi: 10.1016/j.urology.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 7.Deng X., Song L., Xie D., Fan D., Zhu L., Yao L., et al. A novel flexible ureteroscopy with intelligent control of renal pelvic pressure: an initial experience of 93 cases. J Endourol. 2016;30:1067–1072. doi: 10.1089/end.2015.0770. [DOI] [PubMed] [Google Scholar]
- 8.Chen H., Qiu X., Du C., Xie D., Liu T., Wang G., et al. The comparison study of flexible ureteroscopic suctioning lithotripsy with intelligent pressure control versus minimally invasive percutaneous suctioning nephrolithotomy in treating renal calculi of 2 to 3 cm in size. Surg Innovat. 2019;26:528–535. doi: 10.1177/1553350619849782. [DOI] [PubMed] [Google Scholar]
- 9.Zeng G., Zhong W., Li X., Chen W., He Y., He Z., et al. The influence of minimally invasive percutaneous nephrolithotomy on renal pelvic pressure in vivo. Surg Laparosc Endosc Percutaneous Tech. 2007;17:307–310. doi: 10.1097/SLE.0b013e31806e61f4. [DOI] [PubMed] [Google Scholar]
- 10.Zhong W., Zeng G., Wu K., Li X., Chen W., Yang H. Does a smaller tract in percutaneous nephrolithotomy contribute to high renal pelvic pressure and postoperative fever? J Endourol. 2008;22:2147–2151. doi: 10.1089/end.2008.0001. [DOI] [PubMed] [Google Scholar]
- 11.Tokas T., Herrmann T.R.W., Skolarikos A., Nagele U. Pressure matters: intrarenal pressures during normal and pathological conditions, and impact of increased values to renal physiology. World J Urol. 2018;33:1–7. doi: 10.1007/s00345-018-2378-4. [DOI] [PubMed] [Google Scholar]
- 12.Thomsen H.S. Pyelorenal backflow. Clinical and experimental investigations. Radiologic, nuclear, medical and pathoanatomic studies. Dan Med Bull. 1984;31:438–457. [PubMed] [Google Scholar]
- 13.Dindo D., Demartines N., Clavien P.A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Traxer O., Thomas A. Prospective evaluation and classification of ureteral wall injuries resulting from the insertion of a ureteral access sheath during, retrograde intra-renal surgery (RIRS) J Urol. 2012;189:580–584. doi: 10.1016/j.juro.2012.08.197. [DOI] [PubMed] [Google Scholar]
- 15.Young H.H., McKay R.W. Congenital valvular obstruction of the posterior urethra. Surg Gynecol Obstet. 1929;48:509–535. [Google Scholar]
- 16.Heers H., Turney B.W. Trends in urological stone disease: a 5-year update of hospital episode statistics. BJU Int. 2016;118:785–789. doi: 10.1111/bju.13520. [DOI] [PubMed] [Google Scholar]
- 17.Tokas T., Herrmann T.R.W., Skolarikos A., Nagele U. Training and Research in Urological Surgery and Technology (T.R.U.S.T.)-Group. Pressure matters: intrarenal pressures during normal and pathological conditions, and impact of increased values to renal physiology. World J Urol. 2019;37:125–131. doi: 10.1007/s00345-018-2378-4. [DOI] [PubMed] [Google Scholar]
- 18.Kallidonis P., Ntasiotis P., Knoll T., Sarica K., Papatsoris A., Somani B.K., et al. Minimally invasive surgical ureterolithotomy versus ureteroscopic lithotripsy for large ureteric stones: a systematic review and meta-analysis of the literature. Eur Urol Focus. 2017;3:554–566. doi: 10.1016/j.euf.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Kumar A., Vasudeva P., Nanda B., Niraj Kumar N., Kumar S.J., Singh H. A prospective randomized comparison between laparoscopic ureterolithotomy and semirigid ureteroscopy for upper ureteral stones >2 cm: a single-center experience. J Endourol. 2015;29:1248–1252. doi: 10.1089/end.2013.0791. [DOI] [PubMed] [Google Scholar]
- 20.Kadyan B., Sabale V., Mane D., Satav V., Mulay A., Thakur N., et al. Large proximal ureteral stones: ideal treatment modality? Urol Ann. 2016;8:189–192. doi: 10.4103/0974-7796.157963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bozkurt I.H., Yonguc T., Arslan B., Degirmenci T., Gunlusoy B., Aydogdu O., et al. Minimally invasive surgical treatment for large impacted upper ureteral stones: ureteroscopic lithotripsy or percutaneous nephrolithotomy? Can Urol Assoc J. 2015;9:E122–E125. doi: 10.5489/cuaj.2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deng X., Song L., Xie D., Zhu L., Peng Z. Suctioning flexible ureteroscopy with automatic control of renal pelvic pressure. J Endourol. 2015;195:e782. doi: 10.1016/j.juro.2016.02.813. [DOI] [Google Scholar]
- 23.Peng G., Song L., Xie D., Huang J., Zhong Y., Tan W., et al. Suctioning flexible ureteroscopic lithotripsy in the oblique supine lithotomy position and supine lithotomy position: a comparative retrospective study. Minerva Urol Nefrol. 2018;70:612–616. doi: 10.23736/S0393-2249.18.03144-2. [DOI] [PubMed] [Google Scholar]