Abstract
Background:
Low nursing home staffing in the United States is a growing safety concern. Socioeconomic deprivation in the local areas surrounding a nursing home may be an barrier to improving staffing rates, but has been poorly studied. Thus, the objective of this paper was to assess the relationship between neighborhood deprivation and nursing home staffing in the United States.
Methods:
This cross-sectional study used 2018 daily payroll-based staffing records and address data for 12,609 nursing homes in the United States linked with resident assessment data. Our primary exposure of interest was severe economic deprivation at the census block group (neighborhood) level, defined as an area deprivation index score ≥85/100. The primary outcome was hours worked per resident-day among nursing home employees providing direct resident care. Marginal linear regression models and generalized estimating equations with robust sandwich-type standard errors were used to estimate associations between severe neighborhood deprivation and staffing rates.
Results:
Compared to less deprived neighborhoods, unadjusted staffing rates in facilities located within severely deprived neighborhoods were 38% lower for physical and occupational therapists, 30% lower for registered nurses (RNs), and 5% lower for certified nursing assistants. No disparities in licensed practical nurse (LPN) staffing were observed. In models with state-level and rurality fixed effects and clustered on county, a similar pattern of disparities was observed. Specifically, RN staffing per 100 resident-days was significantly lower in facilities located within severely deprived neighborhoods as compared to those in less deprived areas (mean difference: 5.6 fewer hours, 95% confidence interval [CI] 4.2 to 6.9). Disparities of lower magnitude were observed for other clinical disciplines except LPNs.
Conclusions:
Significant staffing disparities were observed within facilities located in severely deprived neighborhoods. Targeted interventions, including workforce recruitment and retention efforts, may be needed to improve staffing levels for nursing homes in deprived neighborhoods.
Keywords: nursing homes, neighborhood disadvantage, disparities
INTRODUCTION
Nearly 1.3 million older adults in the United States are nursing home residents.1 Residents in nursing homes often have complex medical needs, and prior work has shown nursing homes that maintain higher levels of staffing have better resident outcomes. Greater registered nurse (RN) staffing in nursing homes in particular is associated with lower infection rates and lower mortality rates.2 Higher staffing levels among certified nursing assistants (CNAs) has also shown to be associated with fewer deficiency citations in nursing homes.3 Additionally, greater rehabilitation staffing in nursing homes is associated with fewer falls and better resident activities of daily living performance.4,5 Yet, there are marked disparities in staffing in nursing homes disproportionately disadvantaging racial and ethnic minorities, as well as economically disadvantaged populations.6–8
Emerging evidence also suggests that these inequities in care may be exacerbated by neighborhood-level socioeconomic deprivation. One study of nursing homes in the United States found that those facilities located in counties with the lowest socioeconomic status have lower overall star ratings, fewer staff to care for residents, and poorer ratings on publicly reported quality measures.9 Other work using zip-code tabulated areas found nursing homes located in areas with high proportions of low-income residents had higher facility-level financial strain and lower overall quality ratings.10 Differences in neighborhood characteristics accounted for 40% of the variability in the financial operating ratios in these nursing homes, suggesting higher quality facilities are less likely to provide services in deprived areas.
Research on geographic disparities in nursing home staffing has two major methodological challenges. First, evaluations using county or zip-code level metrics could mask marked disparities that exist between neighborhoods. This may be especially concerning in urban centers where different neighborhoods located within close geographic proximity have starkly different socioeconomic deprivation levels.11 Second, although poverty is an important marker of socioeconomic status, it is only one of many variables relevant to assessing the socioeconomic realities of a neighborhood. Several other neighborhood-level factors, such as housing quality, employment, and income inequality may also influence nursing home staffing rates. To fully understand how nursing home staffing is influenced by environmental context, evaluation of socioeconomic metrics beyond simple measures of poverty measured at smaller geographic areas may be needed.
Thus, our main objective in this paper was to evaluate the magnitude of nursing home staffing differences across levels of neighborhood deprivation at the census block group level. Our analysis leverages data from the Area Deprivation Index (ADI), a composite measure of neighborhood socioeconomic disadvantage linked with publicly available nursing home quality and staffing data at the facility level. We hypothesized that facilities in the most deprived neighborhoods would have lower levels of staffing.
METHODS
Design & Data Sources
This was a retrospective cross-sectional study using publicly available nursing home data from three sources: 1) 2018 Nursing Home Compare (NHC) file, 2) 2018 Payroll Based Journal (PBJ) file, and 3) 2018 Long-Term Care Focus (LTCFocus) file. We also included information from the 2018 Minimum Data Set (MDS) merged at the facility level. Briefly, the NHC file contains detailed facility information, including geographic data, for all nursing homes in the United States. From the NHC file, we extracted facility address information and provider identification numbers. Facility information was then linked to the PBJ File, a Center for Medicare and Medicaid (CMS) mandated report of nursing home staffing hours based on payroll information or other granular details on hours worked. Staffing hours are reported in this file concurrently with resident census data to allow daily evaluations of staffing per resident-day. In each facility, the average daily reported staff hours per resident was calculated in 2018—this time period was selected because 2018 data is the latest full year that avoids confounding preparatory staffing changes that preceded the implementation of the Patient Driven Payment Model (PDPM) in October of 2019 and the additional staffing crises precipitated by the COVID-19 pandemic. PDPM changed the payment structure for skilled nursing facilities in a way that removed direct financial incentives for higher utilization of therapy services and shifted care to nursing staff. PDPM has been associated in prior work with declines in rehabilitation staffing.11
LTCFocus data is a public resource that includes additional information on nursing home characteristics such as the acuity index (a measure of resident medical complexity), number of beds, ownership status, and percent with Medicaid as the primary payer. We supplemented this data with information from the Minimum Data Set (MDS), which is a resident-level assessment collected on all nursing home residents at regular annual intervals. MDS data were specifically used to capture the percentage of residents treated that year who identified as Black or African-American. Using nursing home address data available in facility-level data, we geocoded each to the county and census block-group. At the county level, we used US Department of Agriculture rural-urban continuum codes to categorize each facility as being in a metropolitan area, in a rural area adjacent to a metropolitan area, or a remote rural area consistent with prior research. The study procedures were approved by the New York University Institutional Review Board.
Outcomes:
Our primary outcomes of interest were the number of non-administrative staffing-hours per resident day for key categories of licensed nursing home staff: 1) RNs; 2) CNAs; 3) licensed practical/vocational nurses; and 4) rehabilitation staff including physical therapists (PTs), occupational therapists (OTs), and physical and occupational therapy assistants, and speech-language pathologists. In addition, we evaluated staffing for social workers, given the importance of these providers in connecting residents in nursing homes with services and supports.
For each day of the study period, we calculated the total number of hours recorded in the PBJ. Staffing hours per resident day was calculated as the total number of hours worked each day divided by the recorded resident census count for that day, averaged across the study period. For ease of interpretation, we report staffing hours per 100 resident-days.
Assessment of Neighborhood Socioeconomic Disadvantage
Our indicator of neighborhood deprivation was the area deprivation index (ADI). The ADI is a composite percentile ranking of socioeconomic disadvantage concentrated at the Census block group level (each block group representing 600 to 3000 people). The ADI is scored 1 to 100, with higher scores indicating greater socioeconomic disadvantage. Prior work has suggested the effects of neighborhood poverty on healthcare outcomes are non-linear, with negative effects often observed most consistently when neighborhood deprivation exceeds a critical threshold.12 Consistent with this prior work, we defined facilities as being located in “severely deprived” if they were in a census block with a national ADI ranking ≥ 85th percentile)
Facility Characteristics
From the facility-level LTCFocus dataset, we extracted ownership characteristics, number of beds, and the percentage of residents for whom Medicaid was the primary payer for each facility. Additionally, we calculated average acuity level of the residents at the facility level, based on resident assessment data that indicates needs for activities of daily living assistance and the number of residents receiving special treatments (e.g., intravenous therapy). Higher acuity scores indicate greater complexity of care needed for residents in a facility. We also categorized the rurality of each facility using US Department of Agriculture rural-urban continuum codes. Facilities were categorized as urban, rural but urban adjacent, or rural and non-urban adjacent.
Development of the Analytic Cohort:
There were 15,361 nursing homes identified in the NHC dataset. Of these, 14,448 were able to be geocoded, using address data from NHC and LTCFocus, to census blocks using the PROC GEOCODE feature in SAS statistical software, version 9.4 (SAS Institute, Cary, NC). An additional 91 nursing homes with incorrect or non-specific address data (e.g., PO Boxes) were geocoded based on address data obtained through internet searches or other publicly available data on the facilities. We excluded facilities that were in US territories (e.g., Puerto Rico), hospital-based (as staffing relationships with neighborhoods are likely different than non-hospital based facilities), and facilities located in census blocks where ADI scores were not available or suppressed because of low resident populations or where more than 33% of the population was living in group quarters (e.g. institutions). We also excluded facilities with missing PBJ data, and facilities with missing LTCFocus data leaving a sample of 12,609 facilities (82% of all US nursing homes).
Statistical Analysis
We first descriptively analyzed characteristics of facilities by neighborhood deprivation status, and calculated average staffing hours per resident-day for each clinical personnel grouping of interest. We then calculated an adjusted estimate of staffing differences between facilities in severely deprived neighborhoods and less deprived neighborhoods using marginal linear regression models and generalized estimating equations with robust sandwich-type standard errors to account for clustering of facilities within county. Our primary analysis regression models included fixed effects for state (to account for differences in policy environments) and rurality. We also conducted a sensitivity analysis adjusting additionally for facility-level acuity index, given that facilities who care for more complex patients may need additional staffing to maintain safety. Medicare Star Ratings for nursing homes (public reporting of quality) include an acuity-adjusted nurse staffing measure as part of the calculations. Because Medicare staffing data are publicly reported as both unadjusted for acuity (Payroll-Based Journal) and adjusted for acuity (Medicare Star Ratings for Staffing), we opted to include both in our results. All presented p-values and 95% confidence intervals are two-sided. All data manipulation and analyses were completed using SAS version 9.4 (SAS Institute, Cary, NC), and the ggplot2 package in R version 4.1.0 (R Foundation for Statistical Computing, Vienne, Austria) was used for figure creation.
STUDY RESULTS
Overall, 16% of facilities (n=2070) were in severely deprived neighborhoods. Notably, facilities in severely deprived neighborhoods were more likely to be for-profit, had more residents with Medicaid as a primary payer, and served a higher proportion of Black residents. These facilities were also more likely to be in rural counties as compared to urban counties. Facility size and acuity of the residents were marginally lower within facilities located in deprived neighborhoods. (Table 1).
Table 1.
Facility Characteristic by Neighborhood Socioeconomic Disadvantage
| Facility Characteristics | All (n=12,609) |
Less Disadvantaged1 (n=10,539) | Severely Disadvantaged (n=2070) |
|---|---|---|---|
| Certified Bed Size, mean (SD) | 108.2 (54.6) | 109.4 (56.0) | 102.3 (46.5) |
| Organization Ownership Status, (%) | |||
| For Profit | 73.8 | 73.2 | 76.7 |
| Government | 5.1 | 4.6 | 7.3 |
| Non-Profit | 21.2 | 22.2 | 16 |
| Chain Ownership, (%) | 61.1 | 60.9 | 61.9 |
| Medicaid Primary Payer, (%) | 60.6 | 59.1 | 68.2 |
| Black Residents in Facility, % | |||
| None | 23.1 | 23.3 | 22.0 |
| Less than 5% | 29.2 | 30.7 | 21.4 |
| Between 5 and 19.9% | 26.8 | 27.3 | 24.6 |
| Between 20% and 49.9% | 14.5 | 13.7 | 18.8 |
| Greater than 50% | 5.2 | 3.9 | 11.5 |
| Rural-Urban Continuum Code, % | |||
| Metro area | 72.1 | 76.6 | 48.8 |
| Non-metro area – adjacent to metropolitan area | 16.8 | 14.2 | 29.7 |
| Non-metro area – not adjacent to metro area | 9.7 | 7.9 | 19.0 |
Facilities were defined as severely disadvantaged if the area deprivation index ranking was greater than or equal to the 85th percentile
In severely deprived neighborhoods staffing rates were consistently lower for all clinical personnel except for licensed practical nurses, compared to those in more advantaged neighborhoods (Table 2). In the nursing homes in severely deprived neighborhoods a staffing ratio of 31 RN hours per 100 resident-days was observed as compared to a ratio of 44 RN hours per 100 resident-days in less deprived neighborhoods; overall, this was a 30% lower RN staffing rate for facilities located in deprived neighborhoods. For CNA hours, a ratio of 207 hours per 100 resident-days in the severely deprived neighborhoods was observed as compared to 218 hours per 100 resident-days in less deprived neighborhoods—a relative difference of 5%. Rehabilitation therapists also worked fewer hours on average in severely deprived neighborhoods, with PTs averaging 5 hours per 100-resident days in these areas as compared to 8 hours per 100 resident-days in less deprived neighborhoods—a relative difference of 38%. Similar disparities were observed for OTs (Table 2).
Table 2.
Unadjusted Differences in Nursing Home Staffing by Neighborhood Socioeconomic Disadvantage
| Staffing Hours Per Resident Day, mean | All (n=12,609) |
Less Disadvantaged (n=10,539) | Severely Disadvantaged (n=2070) | Unadjusted Difference (95% CI) |
|---|---|---|---|---|
| Registered Nurse (RN) | 0.42 | 0.44 | 0.31 | 0.13 (0.12–0.14) |
| Licensed Practical Nurse (LPN) | 0.79 | 0.79 | 0.80 | −0.01 (−0.03–0.00) |
| Certified Nursing Assistant (CNA) | 2.16 | 2.18 | 2.07 | 0.11 (0.08–0.13) |
| Physical Therapist (PT) | 0.08 | 0.08 | 0.05 | 0.03 (0.03–0.03) |
| PT Assistant (PTA) | 0.10 | 0.10 | 0.09 | 0.01 (0.01–0.02) |
| Occupational Therapist (OT) | 0.07 | 0.08 | 0.05 | 0.03 (0.03–0.03) |
| OT Assistant (OTA) | 0.09 | 0.09 | 0.08 | 0.01 (0.01–0.01) |
| Speech Language Pathologist (SLP) | 0.05 | 0.05 | 0.04 | 0.01 (0.00–0.01) |
| Medical Social Worker (MSW) | 0.06 | 0.06 | 0.05 | 0.01 (0.01–0.01) |
Disparities in staff utilization among facilities in socioeconomically disadvantaged neighborhoods persisted in adjusted models (Figure 1; Supplementary Table S1). Facilities in disadvantaged neighborhoods were staffed by registered nurses for 5.6 (95% CI 4.2 to 6.9) hours less per 100 resident-days. For CNAs, the disparity was 3.2 (95% CI 0.9 to 5.6) fewer hours over 100 resident-days; a difference in staffing was not observed for LPNs. Among rehabilitation providers, facilities were staffed for 1.5 (95% CI 1.1 to 1.8) fewer hours per 100 resident-days by physical therapists and 1.5 (95% CI 1.1 to 1.8) fewer hours per 100 resident-days by occupational therapists. Similar differences were observed for therapy assistants in both disciplines. Further, speech-language pathologists recorded significantly fewer hours within facilities located in disadvantaged neighborhoods (0.6 fewer hours per 100 resident-days, 95% CI 0.4 to 0.8).
Figure 1. Differences in Hours Worked Per 100 Resident-Days Among Nursing Facilities in Severely Deprived Neighborhoods.
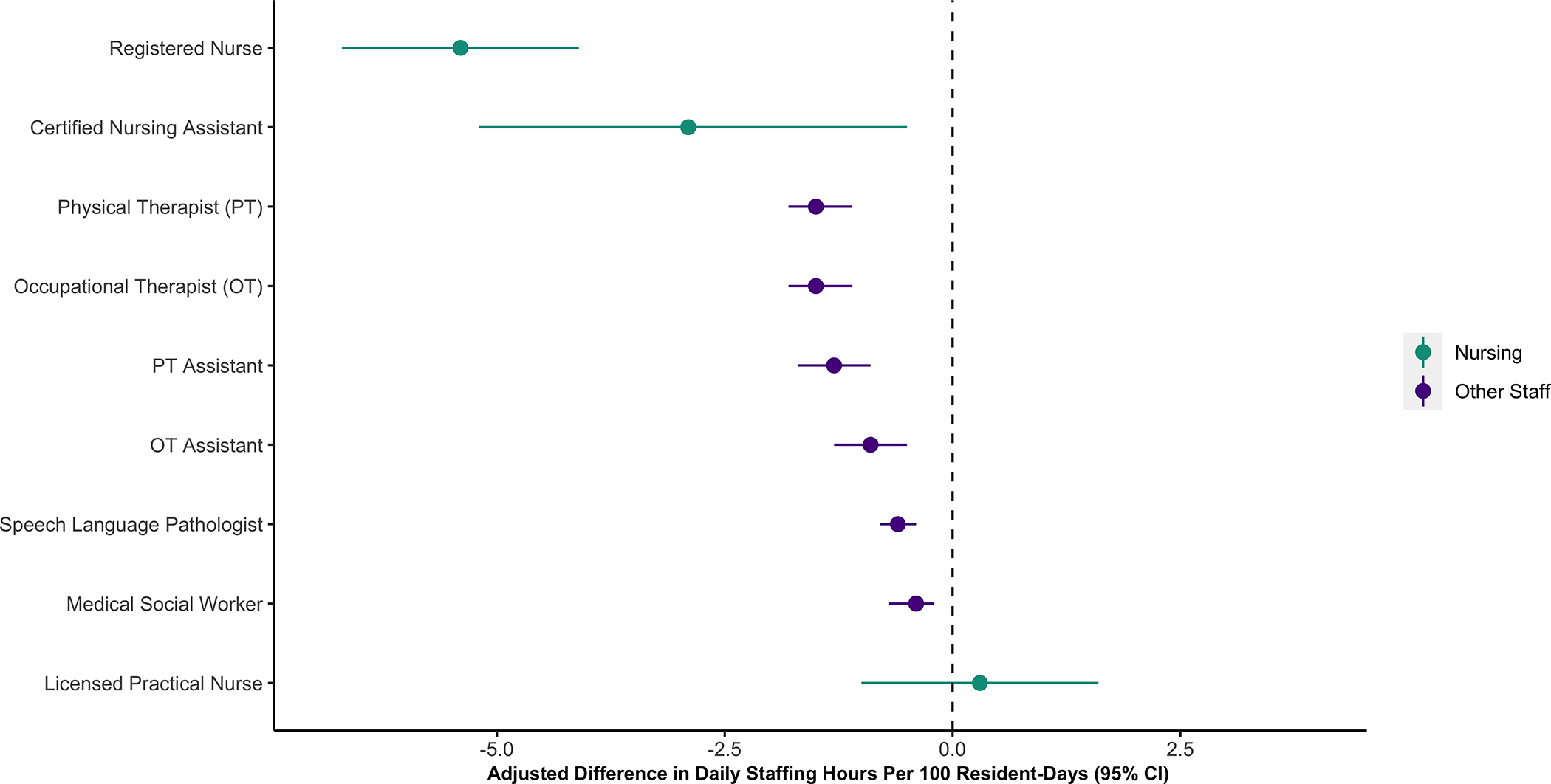
Point estimates and 95% confidence intervals showing the difference in hours worked per 100 resident-days by clinical personnel among nursing homes located in severely deprived neighborhoods (area deprivation index [ADI] scores ≥85/100) as compared to facilities in less disadvantaged neighborhoods (ADI <85/100).
Results from the sensitivity analysis adjusting for acuity index revealed similar trends, with large disparities observed in RN and CNA staffing and no differences in LPN staffing. More modest but statistically significant disparities was observed across the other clinical disciplines (Supplementary Table S2).
DISCUSSION
The results of our national study show that neighborhood socioeconomic disadvantage is associated with significantly lower staffing rates in nursing homes among workers providing direct patient care. Three major findings of this work warrant comment. First, over 16% of nursing homes in the United States are in severely deprived neighborhoods. A disproportionate percentage of these facilities are in rural or remote counties, and overwhelmingly rely on Medicaid as a primary payer for resident stays. These facilities also provide care for a large proportion of Black residents. These findings have implications for policy interventions to reduce inequities in care at both the state and federal level. Second, staffing among nursing home personnel who provide direct resident care was significantly lower in facilities located in disadvantaged neighborhoods, with a striking 30% relative difference in staffing for registered nurses. In a 100-bed nursing facility located within a severely deprived neighborhood, there would be nearly 6 fewer daily hours of RN care provided as compared to a similar facility in a less deprived area. This is a large disparity given the already low RN-to-resident ratios in skilled nursing facilities, and likely has been exacerbated further by the COVID-19 pandemic.13 Third, we saw evidence of care substitution in our data. Nursing staff with generally lower salaries (CNAs and LPNs) had less disparities in staffing than RNs when comparing facilities located in severely deprived neighborhoods to those in less deprived neighborhoods. Even after accounting for differences in medical complexity, substitution of less trained nursing staff providing clinical care remained evident in our findings, raising concerns about quality of care.
Taken together, these findings suggest a negative association between neighborhood level deprivation and nursing home staffing in the United States. The results of our study are consistent with prior work which found associations between county-level and zip-code level socioeconomic status, Medicare star ratings, and facility level financial strain.9,10 Our findings build on this important work by using more granular measures of nursing home staffing (Payroll-Based Journal files) and assessments of neighborhood effects at the census block group level that are more precise and draw on not just measures of poverty, but also other important measures such as housing quality, educational attainment, and employment. Additionally, patterns of nursing care substitution (e.g., relative shifts from RN to LPN hours) we observed in our study were similar to other studies of nursing homes serving a high concentration of minority residents.14
While our study did not evaluate the mechanisms by which neighborhoods influence nursing home staffing, there are several plausible explanations for these disparities. First, facilities in socioeconomically disadvantaged areas may have limited ability to attract and retain qualified healthcare workers. From a labor market standpoint, staff turnover is high in socioeconomically disadvantaged neighborhoods, particularly among RNs.15 Prior work hints at perceptions of higher administrative burden when working with residents who require more care, lower pay in facilities that rely on lower reimbursements from Medicaid, and perhaps greater commuting challenges to facilities.16 Difficulty recruiting and retaining RNs may be one reason we observed substantial differences in RN staffing in our results, and relative shifts in staffing suggesting increased reliance on LPNs. Second, several racially-biased or overtly racist state and federal-level policies have contributed to segregation of minorities into socioeconomically disadvantaged neighborhoods. Prior work has shown that nursing homes with greater concentrations of minority residents have lower levels of staffing.14 This suggests that structural racism may be a potential explanation for the disparities observed in our study, contributing to underinvestment in facilities located within severely deprived neighborhoods and potentially less money to support competitive staff pay and high-quality working conditions.
The urgency of addressing staffing issues in nursing homes has increased since President Joe Biden highlighted the issue as a key priority for his administration in his 2022 State of the Union Address. Inadequate staffing is not just a long-term care concern; it is also a public health concern that limits the ability of our system to deliver quality care to vulnerable nursing home populations. At the same time, as policymakers explore the need for stricter staffing regulations, there is a need to ensure that these requirements do not inadvertently widen disparities by putting undue pressures on nursing homes in severely disadvantaged neighborhoods. Our findings suggest a need for specific policy incentives such as enhanced reimbursement from federal or state payers that directly supports staffing, or other interventions to improve provider recruitment and retention for nursing homes in highly disadvantaged neighborhoods. Similar types of payment enhancement based on geographic location has been implemented for home health care providers treating patients in rural areas.17 Yet, it remains an open question how best to address these staffing inequities in nursing homes.
There are two main avenues for public policy intervention that we believe warrant comment. First, our use of the Area Deprivation Index, an indicator of socioeconomic disadvantage at the census block level, may allow “micro-targeting” of policy interventions or enhanced reimbursements from Medicare and Medicaid to facilities with the worst staffing disparities that would be less expensive and more effective than similar efforts using larger geographic areas.18 This would be especially beneficial in urban areas where wealthy areas and highly disadvantaged neighborhoods are adjacent to one another within the same county or zip code. Using geographic indicators that do not explicitly include racial makeup of the population (such as the Area Deprivation Index) to target care resources may also help reduce inequities without running afoul of legal challenges in the current political environment to race-based allocations of resources.19
Second, states could provide funding to vulnerable facilities through workforce enhancement programs to help recruit and retain healthcare workers for these facilities. These enhancements may be monetary, improvements in nursing home working environments and career advancement opportunities, or transportation-related. Specifically, development of programs that help formally “train-up” staff, such as those training CNAs to become RNs, could help recruit or retain staff who want to commit to working in these underserved areas and build a clinical nurse workforce dedicated to providing high-quality care to nursing home residents.20 Other work has suggested improving transportation access, either through public transportation, ride-sharing, or other innovative models, could be an additional way to help bolster employment in both rural and urban nursing homes.22 More research is needed to explore specific barriers to staffing in these facilities and guide implementation of policy interventions.
Our study is not without limitations. First, staffing data are reported based on paid hours, which does not capture additional time worked by salaried healthcare providers if it exceeds 40 hours per week. This may influence registered nurse and rehabilitation therapist data in our study given their higher likelihood of being represented in salaried positions.16 Second, a small number of nursing homes were unable to be assigned an ADI value because of missing Census data or a disproportionate number of the population living in congregate housing within the Census block group. This may limit generalizability of our findings. Third, we are unable to disentangle from the data how staff is distributed between short-stay and long-stay residents who are treated in the same facility because total resident census is not disaggregated on the Payroll Based Journaling file. This may lead to misestimation of staffing disparities for long-stay residents if they reside in facilities that also treat short-stay residents.
CONCLUSION
Neighborhood deprivation has strong negative associations with staffing within US nursing homes. These findings have several policy implications, especially as accountable care and managed care organizations and other provider networks tighten and often decrease referrals to facilities with lower quality ratings. Penalizing facilities located in disadvantaged communities (and serve more socially vulnerable residents) may exacerbate, instead of ameliorate, disparities in care quality. Targeted policy interventions at the facility and community levels are needed to help address staffing inequities among facilities in socioeconomically disadvantaged neighborhoods.
Supplementary Material
Supplementary Table S1: Adjusted Staffing Differences Between Facilities Located in and Outside of Severely Deprived Neighborhoods
Supplementary Table S2: Acuity-Adjusted Staffing Differences Between Facilities Located in and Outside of Severely Deprived Neighborhoods
Key Points:
Nursing homes located in severely deprived neighborhoods disproportionately serve vulnerable populations of older adults who identify as racial or ethnic minorities or who are socioeconomically disadvantaged
Nursing homes located in deprived neighborhoods are staffed for fewer hours by registered nurses, certified nursing assistants, rehabilitation therapists, and social workers, a disparity that could compromise patient safety
Why Does This Paper Matter:
This paper identifies significant staffing disparities in nursing homes located in severely disadvantaged communities relative to those located in less deprived neighborhoods The use of small census-block group measures for our study, however, highlights potential policy solutions (e.g., payment enhancement, workforce development grants) that could be micro-targeted to facilities in deprived neighborhoods to support more appropriate staffing levels.
ACKNOWLEDGEMENTS:
Funding Support:
This work was supported by an Another Look grant from The Patrick and Catherine Weldon Donaghue Medical Research Foundation awarded to Drs. Jasmine Travers and Jason Falvey. Dr. Travers was supported during the work by the National Institute on Aging (K76AG074922). Dr. Falvey was supported during the work by the National Institute on Aging and the Maryland Claude D. Pepper Center (grant numbers K76AG074926 and P30AG028747). The preliminary results of this study were presented in abstract form at the 2021 Gerontological Society of America Annual Scientific Meeting.
Role of the Funders/Sponsor:
The funders had no role in the design and conduct of the study, data collection, management, and analysis, and interpretation of the data, preparation, review, or approval of the manuscript, and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosure: Drs. Falvey and Travers reported grants from the National Institute on Aging and The Patrick and Catherine Weldon Donaghue Medical Research Foundation during the conduct of the study. The authors have no other disclosures.
REFERENCES:
- 1.National Center for Health Statistics: Nursing Home Care. Retrieved February 22nd, 2022. from https://www.cdc.gov/nchs/fastats/nursing-home-care.htm.
- 2.Harrington C, Dellefield ME, Halifax E, Fleming ML, Bakerjian D. Appropriate Nurse Staffing Levels for U.S. Nursing Homes. Health Services Insights. 2020;13:1178632920934785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hyer K, Thomas KS, Branch LG, Harman JS, Johnson CE, Weech-Maldonado R. The influence of nurse staffing levels on quality of care in nursing homes. Gerontologist. 2011;51(5):610–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Livingstone I, Hefele J, Leland N. Physical and occupational therapy staffing patterns in nursing homes and their association with long-stay resident outcomes and quality of care. Journal of Aging & Social Policy. 2020:1–19. [DOI] [PubMed] [Google Scholar]
- 5.Livingstone I, Hefele J, Nadash P, Barch D, Leland N. The relationship between quality of care, physical therapy, and occupational therapy staffing levels in nursing homes in 4 years’ follow-up. Journal of the American Medical Directors Association. 2019;20(4):462–469. [DOI] [PubMed] [Google Scholar]
- 6.Rivera-Hernandez M, Rahman M, Mukamel DB, Mor V, Trivedi AN. Quality of Post-Acute Care in Skilled Nursing Facilities That Disproportionately Serve Black and Hispanic Patients. The Journals of Gerontology: Series A. 2019;74(5):689–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Travers JL, Schroeder KL, Blaylock TE, Stone PW. Racial/Ethnic Disparities in Influenza and Pneumococcal Vaccinations Among Nursing Home Residents: A Systematic Review. The Gerontologist. 2017;58(4):e205–e217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahman M, Grabowski DC, Gozalo PL, Thomas KS, Mor V. Are Dual Eligibles Admitted to Poorer Quality Skilled Nursing Facilities? Health Services Research. 2014;49(3):798–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yuan Y, Louis C, Cabral H, Schneider JC, Ryan CM, Kazis LE. Socioeconomic and geographic disparities in accessing nursing homes with high star ratings. Journal of the American Medical Directors Association. 2018;19(10):852–859. e852. [DOI] [PubMed] [Google Scholar]
- 10.Park YJ, Martin EG. Geographic Disparities in Access to Nursing Home Services: Assessing Fiscal Stress and Quality of Care. Health services research. 2018;53 Suppl 1(Suppl Suppl 1):2932–2951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prusynski RA, Leland NE, Frogner BK, Leibbrand C, Mroz TM. Therapy Staffing in Skilled Nursing Facilities Declined after Implementation of the Patient-Driven Payment Model. J Am Med Dir Assoc. 2021;22(10):2201–2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kind AJH, Jencks S, Brock J, et al. Neighborhood Socioeconomic Disadvantage and 30-Day Rehospitalization. Annals of Internal Medicine. 2014;161(11):765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buerhaus PI, Staiger DO, Auerbach DI, Yates MC, Donelan K. Nurse Employment During The First Fifteen Months Of The COVID-19 Pandemic. Health Affairs. 2022;41(1):79–85. [DOI] [PubMed] [Google Scholar]
- 14.Li Y, Harrington C, Mukamel DB, Cen X, Cai X, Temkin-Greener H. Nurse staffing hours at nursing homes with high concentrations of minority residents, 2001–11. Health affairs. 2015;34(12):2129–2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gandhi A, Yu H, Grabowski DC. High Nursing Staff Turnover In Nursing Homes Offers Important Quality Information. Health Aff (Millwood). 2021;40(3):384–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fiscella K, Williams DR. Health Disparities Based on Socioeconomic Inequities: Implications for Urban Health Care. Academic Medicine. 2004;79(12). [DOI] [PubMed] [Google Scholar]
- 17.The Impact Of Medicare’s Rural Add-On Payments On Supply Of Home Health Agencies Serving Rural Counties. Health Affairs. 2020;39(6):949–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawk T, White EM, Bishnoi C, Schwartz LB, Baier RR, Gifford DR. Facility characteristics and costs associated with meeting proposed minimum staffing levels in skilled nursing facilities. Journal of the American Geriatrics Society.n/a(n/a). [DOI] [PubMed] [Google Scholar]
- 19.Schmidt H, Gostin LO, Williams MA. Is It Lawful and Ethical to Prioritize Racial Minorities for COVID-19 Vaccines? JAMA. 2020;324(20):2023–2024. [DOI] [PubMed] [Google Scholar]
- 20.Morgan JC, Konrad TR. A mixed-method evaluation of a workforce development intervention for nursing assistants in nursing homes: The case of WIN A STEP UP. The Gerontologist. 2008;48(suppl_1):71–79. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Adjusted Staffing Differences Between Facilities Located in and Outside of Severely Deprived Neighborhoods
Supplementary Table S2: Acuity-Adjusted Staffing Differences Between Facilities Located in and Outside of Severely Deprived Neighborhoods


