To the Editor: Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) is a drug-induced eruption that causes acute and long-term health complications. A survey of adults diagnosed with SJS/TEN showed that long-term physical and mental health sequelae are common.1 Identification of practice gaps provides opportunity for improving care. We evaluated patient perspectives on the health impact of SJS/TEN and posthospital care.
This survey study included adults who registered for the virtual SJS/TEN 2021 Meeting as an SJS/TEN survivor or family member. Potential participants were contacted by email and completed the survey electronically using Research Electronic Data Capture in a deidentified manner. Participants who identified as a family member or a child were excluded. This study was approved by the Institutional Review Board of the University of Pennsylvania.
A total of 66 individuals initiated the survey (Table I), a response rate of 47%. Twelve (18.2%) identifying as family members were excluded, resulting in a total of 54 participants. Of these, 45 (83.3%) completed the survey in its entirety.
Table I.
Demographic and clinical characteristics of survey respondents
| Characteristic | Respondents (n = 54) |
|---|---|
| Age, y (%) | |
| 18-24 | 3 (5.5) |
| 25-34 | 10 (18.5) |
| 35-44 | 19 (35.2) |
| 45-54 | 8 (14.8) |
| 55-64 | 11 (20.4) |
| 65-74 | 3 (5.5) |
| 75-84 | 0 (0) |
| 85-94 | 0 (0) |
| >90 | 0 (0) |
| Years since diagnosis of SJS/TEN (%) | |
| <6 mo | 1 (1.9) |
| 6-12 mo | 7 (13) |
| 1-2 y | 3 (5.6) |
| 3-5 y | 9 (16.7) |
| 6-10 y | 8 (14.8) |
| >10 y | 26 (48.1) |
| Female sex, n (%) | 48 (88.9) |
| Race, n (%) | |
| Asian or Pacific Islander | 13 (24.1) |
| Black or African American | 8 (14.8) |
| Native American or Alaskan Native | 1 (1.9) |
| White or Caucasian | 30 (55.6) |
| Other | 2 (3.7) |
| Ethnicity, n (%) | |
| Hispanic or Latino/Latinx | 5 (9.3) |
| Non-Hispanic or non-Latino/Latinx | 49 (90.7) |
SJS/TEN, Stevens-Johnson syndrome/toxic epidermal necrolysis.
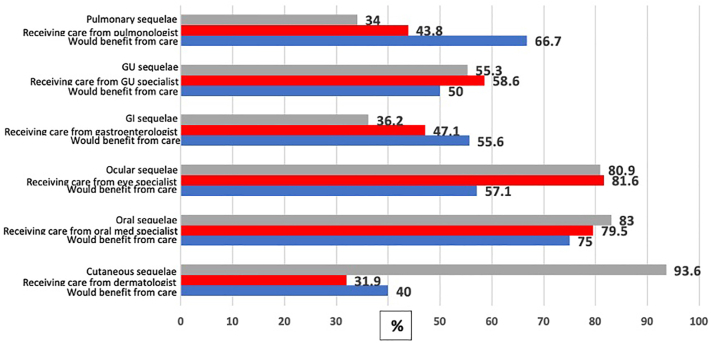
Of participants, 88.2% and 94.1% indicated that their diagnosis of SJS/TEN impacted their physical and mental health respectively; 74.5% of participants follow regularly with a primary care physician and some follow with a medical specialist (Fig 1). Most (70.2%) do not feel their physicians adequately address the long-term health impacts of SJS/TEN.
Fig 1.
Percentage of patients with Stevens-Johnson syndrome/toxic epidermal necrolysis reporting long-term sequelae and who follow with an appropriate health care provider.
Participants reported organ-specific sequelae of their SJS/TEN along with corresponding specialty care received (Fig 1). Of participants who do not see a specialist, the majority felt that they would benefit from specialty care but reported barriers to receiving it.
Thirty-four percent of participants reported receiving assistance with postdischarge care coordination; 87.2% had difficulty establishing care with a provider knowledgeable in SJS/TEN, 63.8% were uncertain regarding which medications or vaccines to avoid in the future, and 76.1% had other unanswered questions regarding their SJS/TEN. Most participants (87%) would like the opportunity to meet with a medical provider with expertise in SJS/TEN; 97.1% of participants believe it would be beneficial to have better SJS/TEN-related care coordination.
This survey serves as a needs assessment regarding postdischarge SJS/TEN care from the patient perspective. Prior work similarly highlights significant long-term care needs and inadequate patient education and support services. SJS/TEN research focuses primarily on acute management. No formal guidelines exist for postdischarge care and management of chronic sequelae. The results of this survey identify ways in which postdischarge care of those with SJS/TEN is inadequate. Survey findings will increase awareness of these practice gaps and inform ongoing work to establish formal guidelines for postdischarge care and education through consensus of disease experts and patient partners.
Survey participants attended the SJS/TEN 2021 Meeting and self-identified as having a history of SJS/TEN. Response rate for the survey was <50%. We acknowledge the potential bias of the survey participants. The data obtained may therefore not be fully generalizable to the larger community of SJS/TEN survivors. Despite these limitations, it is eye opening that survivors who are engaged in the SJS/TEN medical community identify significant barriers to receiving the care they need.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: This study was approved by the Institutional Review Board of the University of Pennsylvania.
Reference
- 1.Hoffman M., Chansky P.B., Bashyam A.R., et al. Long-term physical and psychological outcomes of Stevens-Johnson syndrome/toxic epidermal necrolysis. JAMA Dermatol. 2021;157(6):712–715. doi: 10.1001/jamadermatol.2021.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]