Abstract
Background
Oral Lichen Planus (OLP) is a chronic mucocutaneous inflammatory disease of unknown aetiology characterized by T cell mediated autoimmune response which trigger apoptosis of basal cells of an oral epithelium. Corticosteroids are the primary therapeutic option for symptomatic OLP however treatment of lesions unresponsive to corticosteroids that tend to recur are becoming challenging for the clinicians. Currently photodynamic therapy (PDT) is being explored as a new curative option for reduction of pain and/or burning sensation associated with OLP lesions.
Aims and objective
The aim of this systematic review was to analyse studies from literature on the therapeutic effectiveness of PDT in management of symptomatic OLP unresponsive to corticosteroid therapy.
Methods
The electronic retrieval systems and databases PUBMED [MEDLINE], EMBASE, SCOPUS, WEB OF SCIENCE, GOOGLE SCHOLAR, and SCIENCE DIRECT were searched independently by two authors for relevant articles from January 2015 till July 2021. Primary studies focussed on the role of PDT in treatment of symptomatic OLP and published in English were included.
Results
Out of the 370 articles, only ten studies met the selection criteria. Included studies demonstrated PDT as an effective alternative modality to treat symptomatic OLP with no drop outs. In all studies, with PDT reduction in lesion size and VAS score was observed during each follow up sessions and after treatment (approx. 12 weeks) when compared to pre-treatment level (p < 0.001). Four studies noted PDT to be more effective than topical corticosteroids in reduction of signs and symptoms of OLP (p = 0.001).
Conclusion
In the future, long-term studies on larger population should be conducted to establish the clinical effectiveness in PDT in symptomatic OLP. Studies should take into consideration different sources of light and photosensitizers to determine the ideal parameters of PDT treatment for OLP. Wavelength is the most important factor in all types of photo therapies, so the most appropriate wavelength should be selected to obtain better outcome.
Keywords: Corticosteroids, Oral lichen planus, Photodynamic therapy, Treatment
Graphical abstract
1. Introduction
Oral Lichen Planus (OLP) is a chronic mucocutaneous inflammatory disease of multifactorial aetiology. Psychological stress has been attributed as a main etiological factor and genetic, dental materials like silver amalgam restorations, drugs and chemicals, food allergies, smoking, diabetes mellitus, hepatitis C virus infection, etc as other possible causative factors which can result in onset and progression of lesions.1 OLP has been found to affect 0.5%–2.6% of the world's population with predilection for females between 30 and 60 years of age. González-Moles et al. observed the global pooled prevalence of 1.01% for OLP, and risk of developing OLP increases significantly (p < 0.001) for people aged 40 years and older.2
Several pathogenic mechanisms such as non-specific inflammation, humoral immunity and autoimmunity have been proposed however antigen specific cell mediated immunity is regarded as a widely accepted mechanism in which cytotoxic CD 8+ T cells trigger apoptosis of basal cells of an oral epithelium.3 Other pathogenic mechanisms proposed towards initiation of OLP include i) dysregulation of heat shock protein gene expression, ii) basement membrane disruption which triggers keratinocyte apoptosis, and apoptotic keratinocytes may not be able to repair the disrupted basement membrane, iii) higher concentration of matrix metalloproteinases (MMP-9) in OLP lesions has been found which also result in basement membrane disruption, iv) RANTES (regulated on activation, normal T cell expressed and secreted), a member of CC chemokine family has been reported to recruit mast cells in OLP lesions which subsequently undergo degranulation, and v) autoimmunity which can be attributed to the chronic nature of OLP, female predilection, adult onset, association with other autoimmune diseases, and presence of auto-cytotoxic T lymphocytes.3 Occurrence of OLP attributes to six clinical variants that includes reticular, papular, plaque type, erythematous/atrophic/erosive, ulcerative and bullous forms and among these reticular OLP on posterior buccal mucosa has been reported to have common occurrence which is often asymptomatic.4 Considering it as a T cell mediated immunological disease, topical and systemic corticosteroid therapy is being widely used as a primary therapeutic option. Since then, due to adverse effects that may occur with long term corticosteroid therapy various pharmacological therapies such as cyclosporine A, tacrolimus, retinoids, antidepressants, antiepileptics, and antimalarials, alternative therapies such as natural agents like curcumin, aloe vera, green tea, and light based therapies such as photo biomodulation or low-level laser therapy, and PUVA (psoralen and ultraviolet -A) are being recommended with variable success rates.4 However, treatment of symptomatic OLP is becoming a major challenge to clinicians as in majority of cases it tends to be recalcitrant characterized by waxing and waning of lesions that is it tends to recur with periods of exacerbation and remission and are less responsive to above proposed therapeutic modalities.
Phototherapy or light has been used to treat various diseases since1400 B.C. The Swiss doctor Arnold Rikli (1823–1906) was first in the 19th century to introduce the positive effects of sunlight for the treatment of chronic diseases. Oscar Raab introduced the concept of photodynamic therapy (PDT)in 1898 and he observed the therapeutic effects of light and acridine dye on paramecia.5 Currently PDT is being explored as a curative treatment option by the clinicians which employs photochemical reaction between photo sensitizer (PS), visible light of particular wavelength and oxygen that results in apoptosis of abnormal cells. Activation of PS by visible light of selected wavelength results in production of cytotoxic free radicals and subsequently this photochemical reaction ensues destruction of target cells.6 Studies have been conducted which have suggested PDT as a promising therapeutic option for the management of oral premalignant lesions such as oral leukoplakia (OL), OLP, and oral cancer. Reduction in size of OL lesions were observed after treatment with 10% ALA mediated sessions with no side effects. PDT has been found to be a useful alternative therapeutic strategy for recurrent oral cancers as free radicals produced as a result of photochemical reaction have a potential to destroy tumour cells selectively by direct killing or by damaging tumour vasculature. In addition, studies have observed reduction in size of symptomatic OLP with PDT thereby leading to improvement in quality of life of patients.7
Literature has revealed very few systematic reviews focussed in this domain by our search, therefore this systematic review aimed to compile evidence-based studies on evaluation of the therapeutic effectiveness of PDT in management of symptomatic OLP unresponsive to corticosteroid therapy.
2. Focussed research questions
Based on the Preferred Reporting items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, a focused questions were constructed which were.
-
1).
Whether PDT could be an effective treatment modality for reduction in severity of symptomatic OLP?
-
2)
Whether PDT would be more effective in treatment of symptomatic OLP when compared to topical/systemic corticosteroids?
-
3)
Whether PDT could be used to treat refractory OLP cases unresponsive to corticosteroid therapy?
3. Methodology
3.1. Search protocol (search strategy and data extraction)
Electronic databases PUBMED [MEDLINE], EMBASE, SCOPUS, WEB OF SCIENCE, GOOGLE SCHOLAR, and SCIENCE DIRECT were independently searched by two authors for relevant articles from January 2015 till July 2021. The search was done by using combination of various MeSH keywords such as corticosteroids, oral lichen planus, photodynamic therapy, photosensitizer, treatment and also included grey literature. Search was based on PICO model as
-
i)
Participants (P): adult patients (≥18 years old) diagnosed with symptomatic OLP,
-
ii)
Intervention (I): PDT,
-
iii)
Comparator (C): corticosteroids or placebo group (if present), and
-
iv)
Outcome (O): pain (primary outcome) and clinical improvement (secondary outcome).
Randomized clinical trials (RCTs), non RCTs and comparative or controlled clinical trials were included which were focussed on research question “whether PDT could be used as an effective therapeutic option in the treatment of symptomatic OLP cases”. Reviews, Case Reports, Case Series, Commentaries, studies not focused on role of PDT in OLP and primarily focused on oral cancer and other oral potentially malignant disorders like leucoplakia, submucous fibrosis etc. were excluded. OLP treated with steroid sparing immunomodulators and studies not published in English were also excluded from this systematic review.
Fig. 1 shows the search strategy for inclusion of eligible studies in this systematic review and ten studies met our inclusion criteria.
Fig. 1.
Flow chart shows study selection criteria based on Preferred Reporting Items for Systematic Reviews (PRISMA) guideline.
The abstracts of the papers were individually screened by two authors who were calibrated and they both were oral medicine specialists from India with an experience of more than ten years. They reviewed full-text of eligible articles, discussed the selection criteria, and any disagreement was sorted out by mutual discussion. Thereafter they arrived at the agreement about the inclusion and exclusion criteria and only ten studies met our inclusion criteria.
Table 1 summarizes ten eligible studies discussing the clinical effectiveness of PDT as a therapeutic modality for symptomatic OLP based on PICO format, with detailed information on study design, aims and objective, results, and conclusion.7, 8, 9, 10, 11, 12, 13, 14, 15, 16
Table 1.
Characteristics of included studies based on Population, Intervention, Comparison, and Outcome (PICO) model to evaluate effectiveness of PDT for symptomatic OLP.
| AUTHOR (YEAR) | COUNTRY | AIM AND OBJECTIVE | STUDY DESIGN | SAMPLE | SITE OF LESION CRITERIA USED |
RESULTS | CONCLUSION |
|---|---|---|---|---|---|---|---|
| Jajaram et al. (2015)7 | Iran | To compare the effect of toluidine blue-mediated -PDT with local corticosteroids on treatment of erosive-atrophic OLP | RCT (comparative) Topical corticosteroids | 25 patients with clinically and histopathologic ally diagnosed OLP patients i)Group I (n = 11) PDT, 630-nm GaAlAs laserii) Group II control (n = 10) dexamethasone mouthwash | Tongue or buccal mucosa (size ≤3 cm) | The mean amount of improvement in pain was significantly greater in the control group compared with the experimental group (p < 0.001). | Corticosteroid therapy showed better results than TB-PDT. |
| Prasanna et al. (2015)8 | Chennai, India | To evaluate PDT as an alternative/complimentary therapeutic modality for the management of premalignant lesions (OLP and OL). | RCT | Total 16 patients: OLP (4 males and 2 female), and OL (8 male and 2 female) Age:20–80 years, Total 15 OLP lesions and 13 OL lesions MB-PDT (red diode laser, 630 ± 10 nm) OLP lesions: MB-PDT was performed once a week for four weeks and OL lesions: MB-PDT was performed twice a week for three weeks Clinical Evaluation: Baseline, 1 week and 12 weeks (3 months) | Specific site not mentioned/VAS score | 53.3% of complete reduction in the treated OLP lesions and their decrease in size, sign and symptom score after treatment and at follow-up session was statistically significant Complete response for one OL lesion of the 13 treated lesions was noted. | OLP lesions responded much better than that of OL MB-PDT is an effective modality in management of OLP and OL. |
| Aghahosseini et al. criteria for reduction in size of lesion | |||||||
| Bakhtiari et al. (2017)9 | Iran | To compare the clinical effects of the PDT and dexamethasone mouthwash in the treatment of OLP lesions | RCT (comparative) Topical corticosteroids | 30 patients with reticular and erosive OLP, 15 in each group i)PDT group: MB as photosensitizer and light source of LED 630 nm ii)Dexamethasone (0.5 mg in 5 ml) mouthwash group Evaluation:15, 30, 60 and 90 days after start of the treatment | Oral cavity of each individual was divided into 14 Sites Thongprasom sign scoring Clinical severity index (SI) Efficacy indices (EI) of the ulcer size | No significant difference existed between two modalities regarding the treatment efficacy index, sign score, symptom score and clinical severity on follow up visits. | PDT was as effective as the dexamethasone mouth wash in the treatment of OLP |
| Decrease in patient's symptoms (VAS) were statistically significant in both groups. | |||||||
| Mostafa et al. (2017)10 | Riyadh, Saudi Arabia | To evaluate clinically the effect of PDT mediated by methylene blue on signs and symptoms of erosive (E) OLP lesions in comparison with topical corticosteroids | RCT (comparative) Topical Corticosteroids | 20 patients with clinical and histological diagnosis of EOLP Group A:10 patients kenacort A orabase Group B: PDT using diode laser 660 nm mediated by methylene blue Evaluation: 1, 2, 4 weeks and 2 months of treatment | Buccal and lower labial mucosa VAS score Thongprasom sign scores | Highly significant decrease in the VAS in group B than in group A all over the periods of follow up at 1, 2, 4 weeks and 2 months (p = 0.0001). High significant decrease in the mean lesion size score of group B than that of group A was noted. | MB-PDT could be a better treatment for EOLP in comparison with the topical corticosteroids for in pain reduction and lesion regression. |
| Mirza et al. (2018)11 | Riyadh, Saudi Arabia | To compare the effects of PDT and LLLT with topical corticosteroid application in the treatment of erosive-atrophic OLP. | RCT (comparative) Topical Corticosteroids | 45 adult patients with erosive-atrophic biopsy-proven OLP Group-1: patients receiving TB PDT Gallium–Aluminum-Arsenide (GaAlAs) laser was used as a light source (630 nm), Group-2: patients receiving LLLT; and Group-3: dexamethasone mouthwash Two times weekly for month | Tongue or buccal mucosa (size ≤3 cm) Thongprasom sign Efficacy Index VAS score | Mean amount of improvement in pain was significantly greater in the control group in comparison with the PDT and LLLT groups (p < 0.001). The efficacy index of the PDT group improved significantly more than the LLLT (p = 0.001) and corticosteroid groups (p = 0.001). | Results of PDT and LLLT in improving clinical signs and symptoms of OLP is promising. However, corticosteroid is still the gold standard with regard to pain scores in the management of OLP. |
| Lavaee et al. (2019)12 | Shiraj, Iran | To compare the effects of PDT with topical corticosteroid application in the treatment of OLP | RCT (comparative) Sham LASER | 8 sides each for intervention and control group Intervention i)Control group:only sham laser, and ii)Intervention Group: TB PDT 660‐nm diode laser InGaAlP Sessions: Day 1 (session 0), week 3 (session 3), and week 7 (session 4) After three sessions Triamcinoloneacetonide 0.1% three times a day for four weeks Follow up:7 week | VAS score Clinical severity index (SI) Efficacy Index Thongprasom sign scoring, |
Scores improved significantly between sessions 0 and 4 for the intervention (PDT) side. The differences between the changes in almost all scores between sessions 0 and 4 in both the intervention and control sides were significantly considerable (p value < 0.05). | PDT can be used as an adjuvant therapy besides routine treatment methods or as a new modality for refractory OLP lesions. |
| Cosgarea et al. (2020)13 | Germany | To determine the clinical and immunological efficacy of PDT in OLP as an alternative, easy-to-use, safe and non-invasive treatment. | RCT | 20 OLP patients PDT sessions; day 1, 3, 7, and 14 Clinical Parameters: day 1 (baseline) and day 28, 42, and 56 Peripheral blood and lesional T cells before (day 1) and after PDT treatment (day 28). |
Thongprasom-score Lesion size Autoimmune bullous skin disorder intensity score (ABSIS) | PDT treatment led to a highly significant size (P < 0.001) reduction of the mucosal lesion starting from 14 days after PDT (day 28) that correlated with a significant improvement of the ABSIS I score (P < 0.05) at days 42 and 56. CXCL10 plasma levels were decreased and the number of activated peripheral CD4 + CD137+ and CD8 + CD137+ T cells and IL-17-secreting T cells was diminished. | PDT treatment in OLP leads to lesion reduction and improvement of QOL, and induces local and systemic anti-inflammatory effects |
| Sabry et al. (2020)14 | Egypt | To evaluate the effect of PDT on pain reduction in patients suffering from erosive/atrophic OLP | RCT | 30 erosive/atrophic OLP patients (21 females and 9 males, 35–55 years) MB-PDT twice per week for two months with a maximum of 16 sessions (Diode laser of a wave length of 650 nm & power 250 mW) | Tongue\ VAS | The mean VAS score decreased gradually over 16 sessions from 8 ± 1 to 4 ± 2 and there was statistically significant decrease of the mean VAS score at the first month from 7 ± 2 to 5 ± 2 by the end of the second month (p < 0.001). | The use of PDT was found to be an efficient alternative method |
| Saleh et al. (2020)15 | Egypt | To compare the effect of PDT to the effect of topical corticosteroids in the treatment of erosive OLP lesions | RCT (comparative) Topical corticosteroids | 20 patients (16 females and 4 males) with erosive OLP (30–60 years) Group 1 PDT-MB, Red Diode Laser wavelength 660 nm, Group 2: topical betamethasone valerate ointment 100 mg Clinical Evaluation: time zero, after 2 weeks and after 4 weeks from the start of treatments. | No specific site mentioned/VAS Thongprasom sign scoring | MB-PDT showed a higher degree of improvement than topical corticosteroids between time zero and the 4th week of treatment (p < 0.05) | PDT offers improvement of OLP subjective and objective scores without major side effects. |
| Zborowski et al. (2021)16 | Poland | To compare the effectiveness of PDT to steroid therapy in the treatment of OLP | RCT (comparative) Topical corticosteroids | 30 patients with bilateral erythematous or erosive OLP Matrices were prepared incorporated with active substances methylene blue 5% and 0.05% triamcinolone and placed over lesion site After MB, PDT performed (Red diode laser) |
No specific site mentioned/VAS Thongprasom sign scoring ABSIS scoring | Relatively high rates of complete remission of lichen were demonstrated: immediately after treatment, 33.3% with PDT and 22.2% with triamcinolone (TA), and after 3 months, 54.2% with PDT and 62.9% with TA. After 3 months of treatment, a reduction in the area of evaluated lesions of 52.7% for PDT and 41.7% for TA was achieved. | PDT appears to be a very promising treatment option for erosive OLP. |
RCT: Randomized Controlled Trial, PDT: Photodynamic Therapy, TA: Triamcinolone Acetonide, MB: Methylene Blue, TB: Toluidine Blue, LLLT: Low Level Laser Therapy, QOL: Quality of Life, VAS: Visual Analog Scale, OL: Oral Leukoplakia, EOLP: Erosive Oral Lichen Planus, LED: Light Emitting Diode, CXCL10:C-X-C Motif Chemokine 10, CD: Cluster of Differentiation.
3.2. Risk of bias and methodological quality assessment
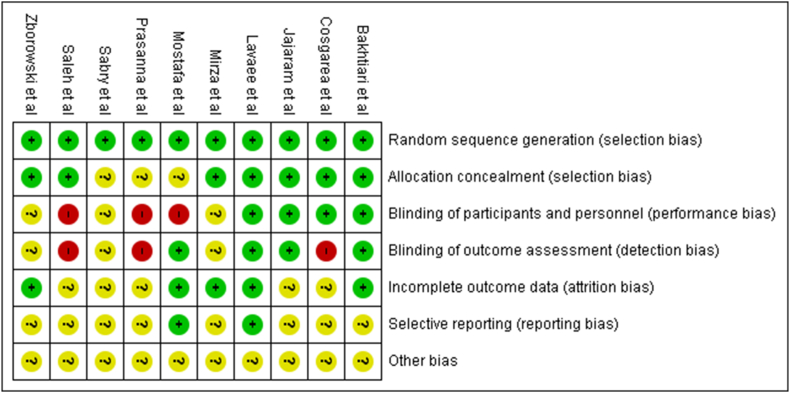
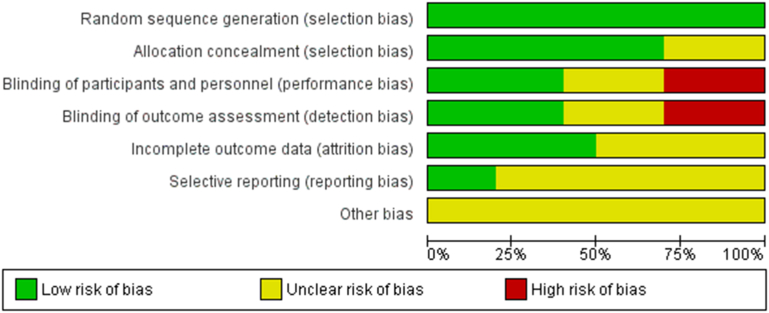
Fig. 2 and b shows a risk of bias across individual studies by Cochrane risk-of-bias tool. 30% studies showed low risk of bias, 75% of studies showed high risk bias and in 30–69% studies bias was unclear. The main shortcomings for high-risk bias in 75% of studies was inadequate sample size calculation and inadequate or lack of blinding of participants or investigator.
Fig. 2.
a and b: Risk of bias summary assessed of included interventional trials by Cochrane risk of bias tool.
4. Results
A total of ten articles were selected from 370 screened articles for systematic review. Out of 10 included studies, seven randomized clinical trials by Prasanna et al. Mostafa et al., Mirza et al. Lavaee et al., Casgarea et al. Sabry et al., Saleh et al. found PDT as a promising treatment modality for symptomatic OLP.8,10, 11, 12, 13, 14, 15 In all studies, with PDT reduction in lesion size and VAS score was observed during each follow up sessions and after treatment (approximately 12 weeks) (p < 0.001). Prasanna et al. performed Methylene Blue (MB-PDT) once a week for four weeks in 16 OLP patients. After 3 months follow up visit, 53.3% showed complete reduction in the treated OLP lesions and their decrease in size, sign and symptom score after treatment and at follow-up session was statistically significant (p < 0.001).8 Mostafa et al. evaluated the clinical effectiveness of MB-PDT (660 nm wavelength) in 20 patients with clinical and histological diagnosis of erosive OLP. Highly significant decrease in the VAS score and mean lesion size score was noted over the periods of follow up at 1, 2, 4 weeks and 2 months (p = 0.0001) when compared to topical corticosteroids. Hence, they suggested MB-PDT could be a better treatment for erosive OLP in comparison with the topical corticosteroids for in pain reduction and lesion regression.10 Later Mirza et al. in their study found that efficacy index of the Toluidine blue (TB) PDT group improved significantly more than the LLLT (p = 0.001) and corticosteroid groups (p = 0.001). However, they suggested that corticosteroid is still the gold standard with regard to reduction in pain scores in the management of OLP.11 Lavee et al. found significant differences between the changes in Vas and pain scores between day 1 (session 0) and week 7 (session 4) in both the intervention and control (sham laser) sides were significantly considerable (p value < 0.05). They concluded that TB-PDT could be used as a adjuvant therapy along with routine treatment for refractory OLP cases.12 Casgarea et al. in their study found that PDT treatment led to a highly significant size (P < 0.001) reduction of the mucosal lesion after day 28. They suggested PDT as a promising modality that aims to improve the quality of life of symptomatic OLP patients which may be attributed to the local and systemic anti-inflammatory effects induced by PDT.13 Similar results were elucidated by Sabry et al. who performed MB-PDT twice per week for two months with a maximum of 16 sessions in 30 patients with erosive or atrophic OLP.14
Out of 6 comparative controlled trials that used topical corticosteroids like dexamethasone mouth wash, triamcinolone 0.1% gel,or betamethasone mouth wash, Jajaram et al.7 found clinical improvement of pain and/or burning sensation more with topical corticosteroids than PDT (p < 0.001), Bakhtiari et al.9 found equal efficacy of topical corticosteroids and topical dexamethasone mouthwash and Mostafa et al.,10 Mirza et al.,11Saleh et al.,14 and Zobrowski et al.16 noted PDT to be more effective than topical corticosteroids in reduction of signs and symptoms of OLP (p = 0.001).However, Mirza et al. suggested that although results of PDT for symptomatic OLP are quite promising but corticosteroid therapy still remains the treatment of choice.11
In all the included studies patients with systemic diseases, drug use, pregnancy, photosensitivity, younger than 18 years, who had lesions with dysplasia or had received treatment for OLP at least 1 month prior to the beginning of the study formed the exclusion criteria. Studies have suggested PDT as a safe alternative treatment with no drop outs. Contrary to this, in three studies, adverse reactions on application of PS were observed. In a study by Bakhtiari et al.9 two patients reported discomfort in the first and second sessions of PDT and one patient in the second and third sessions which may be due to probe tip movement on the affected area. In a study by Mostafa et al.10 edema in eight OLP patients after first session, and mild burning sensation in three patients was observed. In another study, Zborowski et al.16 slight swelling and increased pain was seen after first or second PDT session.
5. Discussion
A wide array of treatment modalities to alleviate pain and/or burning sensation associated with symptomatic OLP are available that include corticosteroids, immunomodulators, and laser ablation etc but none has been found to be curative. Selection of an appropriate therapy for symptomatic OLP should be made on the following basis first with an aim to reduce the duration and severity of symptoms, and to reduce the size of the lesion. The goal of the therapy should be to reduce reticulation, erythema and ulceration associated with the lesion and to improve oral health related quality of life of patients. OLP has been reported to have inflammatory pathogenesis and due to this symptomatic OLP lesions usually respond to corticosteroids.1,2 Although corticosteroids are widely used a first line treatment therapy for symptomatic OLP however prolonged use of topical corticosteroids may result in oral candidiasis or atrophy of the mucosa and with systemic corticosteroids there may be a risk of adrenal suppression.9,10 Several immunosuppressive and immunomodulating agents are being explored but few patients have refractory persistent OLP lesions that have tendency to relapse and reoccur after a period of remission. In addition, long term use of steroid sparing immunomodulatory agents can result in undesirable side effects.10 In this context, included studies in this systematic review have suggested PDT therapy as an effective and safe alternative treatment modality for symptomatic and refractory cases of OLP.
PDT has been studied to have a potential advantage of minimal toxicity to normal cells, repeated doses can be given with minimal side effects, it induces apoptosis of inflammatory CD 8+ T cells, reduces rate of recurrence and size of lesions hence improves the quality of life of patients by decreasing the severity of symptoms.6,17 Additionally, it is non-invasive and has been documented to promote better healing with minimal scarring when compared to photo biomodulation or low-level laser therapy and this finding could be explained by the antibacterial and antifungal effect of PS.12,18 Due to its unique advantages currently PDT is capturing the interest of the researchers and is being explored as a curative treatment option for symptomatic OLP lesions less responsive to corticosteroids.
PDT is based on the concept of photochemical reaction in which PS applied to the lesion site is activated by a visible light of specific wavelength. Upon absorbance of light energy by PS biochemical reaction ensues in presence of molecular oxygen resulting in production of singlet oxygen (1O2) or superoxide (O2 -) that causes cellular destruction, membrane lysis or protein inactivation. Studies have suggested that effectiveness of PDT depends upon type of PS, wavelength of laser or light source used to activate the PS, tissue oxygen availability, duration of irradiation and total duration of treatment.6 The results of efficacy of PDT are heterogeneous for the studies included in this systematic review which may be due to different types of PS i.e. methylene blue in seven studies and toluidine blue in three studies and various types of light sources (diode laser, light emitting diode LED) employed (Table 2). Another PS, 5 aminolaevulinic acid (5-ALA) 5-ALA has been studied to endogenously convert into protoporphyrin IX on incorporation onto the skin or oral mucosa. Exposure of protoporphyrin IX to a light of appropriate wavelength (400–410 nm, 635 nm) results in the production of reactive oxygen species which eventually cause apoptosis of abnormal or dysplastic cells.19,20 However, 5 ALA-PDT has been reported to be a painful therapy and patient may suffer from photo allergies and deeper penetration of 5-ALA into the oral mucosa.6 Other photosensitizers are phenothiazine dyes such as toluidine blue (TB) and methylene blue (MB) (620–700 nm), MB has been studied to have photosensitizing effect on irradiation by light of wavelength around 660 nm and is preferable PS agent due to low cost, selective toxicity and selective bacterial damage.6,8,10 By our search no study was observed to use 5-ALA PDT for symptomatic OLP and this necessitates the need of clinical trials to validate the efficacy of 5-ALA PDT for alleviation of symptoms of pain or burning sensation in OLP patients.
Table 2.
Shows types of photosensitizers and light sources used for PDT in included studies.
| AUTHOR (YEAR) | PDT PARAMETERS |
|---|---|
| Jajaram et al. (2015) | TB-PDT, Red Diode LASER, 630 nm, 10 mW/cm2 |
| Prasanna et al. (2015) | MB-PDT, Red diode LASER, 630 ± 10 nm, 120J/cm2 |
| Bakhtiari et al. (2017) | MB-PDT, LED, 630 nm,7.2–14.4 J/cm2 |
| Mostafa et al. (2017) | MB PDT, Red diode LASER, 600 nm, 100–130 mW/cm2 |
| Mirza et al. (2018) | TB PDT, Red diode LASER, 630 nm, 10 mW/cm2 |
| Lovaee et al. (2019) | TB PDT, Diode LASER, 66 nm, 25 mW |
| Cosgarea et al. (2020) | MB PDT, Red diode LASER, 630 nm |
| Sabry et al. (2020) | MB PDT, Red diode LASER, 650 nm, 250 mW |
| Saleh et al. (2020) | MB PDT, Red diode LASER, 660 nm, 100–130 mW/cm2 |
| Zborowski et al. (2021) | MB PDT, Diode LASER, 650 nm 1034 mW/cm2 |
Diode lasers are more versatile and has been found to be better absorbed by biological tissues, due to potential advantages diode laser was most commonly light source in our studies in comparison to LED which was used in one study by Bakhtiari et al.9 LED is becoming an emerging light source due to low cost and ease of handling however both diode laser and LED have a wavelength range between 630 and 700 nm that is adequate to activate the photosensitizers MB and TB (Table 2). Outcome of PDT to treat symptomatic OLP were found to be promising as suggested by studies conducted by Mostafa et al.,10 Mirza et al.,11 Saleh et al.,15 and Zobrowski et al.16 and they found PDT to be more effective than topical corticosteroids in reduction of signs and symptoms of OLP (p = 0.001). The primary outcome reduction of pain and burning sensation was measured by subjective VAS scale in the studies, whereas secondary outcome reduction in sign scores were assessed by Thongprasom criteria in seven studies and significant reduction in size of OLP lesions was noted during follow up session thereby pointing towards the effectiveness of PDT for the management of OLP lesions. Cosgarea et al. concluded that PDT treatment in OLP also leads to improvement of quality of life of patients, and induces local and systemic anti-inflammatory effects.13 Prasanna et al.8 used Aghahosseini et al. criteria21 by which 53.3% of complete reduction in the treated OLP lesions was observed and decrease in size, sign and symptom score after treatment and at follow-up session was statistically significant (p < 0.001). One study by Mirza et al.11 found that mean amount of improvement in pain was significantly greater with corticosteroids in comparison with the PDT and LLLT (p < 0.001). However, the clinical efficacy index of the PDT group improved significantly more than the LLLT (p = 0.001) and corticosteroid (p = 0.001). They suggested corticosteroids as the gold standard for reduction of pain in OLP patients, and further long term follow up clinical trials should be encouraged to compare the efficacy of PDT with LLLT for symptomatic and refractory OLP lesions. In addition, studies have focussed on erosive or atrophic OLP in buccal mucosa and tongue, as a result more studies should be undertaken to establish the efficacy of PDT for gingival and dysplastic OLP lesions. Results of studies have shown no recurrence of OLP lesions during and after the follow up sessions and PDT could be used as an adjunct therapy along with corticosteroids for refractory OLP lesions for better outcome.7, 8, 9, 10, 11, 12,14, 15, 16 It has been reported that incidence of risk of malignant transformation in atrophic or erosive OLP is in 1–3 years after occurrence of lesions hence long term follow ups up to 4 years and periodic examination is necessary to evaluate the recurrence and malignant changes in OLP after treatment with PDT.20
The main limitations for the studies included in this systematic review were heterogeneity of the outcome which may be because of lack of standardization due to different types of photosensitizes, and sources of light of variable wavelength. Secondly, 75% studies were assessed to have high risk of bias and this may be due to inappropriate sample size calculation and inadequate or lack of blinding of participants and investigator. Due to scarcity of information in the literature, PDT requires further verification on larger population regarding its efficacy with main focus on gingival OLP lesions. Studies should take into account different sources of light and photosensitizers to determine the ideal parameters of PDT treatment for OLP. Wavelength is the most important factor in all types of photo therapies, so the most appropriate wavelength should be selected to obtain better results. In addition, comparative studies to evaluate effectiveness of PDT and LLLT and systemic corticosteroids should be also be the area of research. Although incidence of adverse effects has been reported to be minimal with MB and TB PDT but studies should be conducted by using 5-ALA as an photosensitizer to prove effectiveness and safety of 5-ALA PDT for treatment of symptomatic OLP lesions.
6. Conclusion and future prospects
Results of included studies has concluded PDT to be an effective modality to reduce pain and size of OLP lesions thereby leading to improvement in quality of life of patients. This may be accounted to unique advantages of PDT over other modalities of being non-invasive, and it has selective toxicity for abnormal or dysplastic cells. Studies have elicited that PDT can be safely used as an adjunct therapy with topical or systemic corticosteroids for refractory OLP lesions. However, limited data is available in the literature in this domain by our search therefore future necessitates more of longitudinal long term follow up randomized clinical trials on larger population and sample size comprising of more than 30 subjects followed by allocation of subjects into case and control groups to establish the clinical effectiveness in PDT in OLP treatment. Studies should also focus on efficacy of PDT in gingival and dysplastic OLP lesions taking into account standardization of wavelength of different sources of light used to activate photosensitizers for better treatment outcome. Clinical applications of PDT in oral medicine are rapidly growing and possibilities of combining PDT with other therapies should be explored for effective management of symptomatic and refractory oral lesions, and to improve the quality of life of patients.
Contributor Information
Ravleen Nagi, Email: ravleen2017@gmail.com.
Arvind Muthukrishnan, Email: arvindmuthukrishnan@yahoo.com.
N. Rakesh, Email: drnrakesh@gmail.com.
References
- 1.Silverman S., Jr. Oral lichen planus: a potentially premalignant lesion. J Oral Maxillofac Surg. 2000;58(11):1286–1288. doi: 10.1053/joms.2000.16630. [DOI] [PubMed] [Google Scholar]
- 2.González-Moles, Warnakulasurya S., Gonzalez-Ruiz I., et al. Worldwide prevalence of oral lichen planus: a systematic review and meta-analysis. Oral Dis. 2021 May;27(4):813–828. doi: 10.1111/odi.13323. [DOI] [PubMed] [Google Scholar]
- 3.Roopashree M.R., Gondhalekar R.V., Shashikanth M.C., George J., Thippeswamy S.H., Shukla A. Pathogenesis of oral lichen planus--a review. J Oral Pathol Med. 2010 Nov;39(10):729–734. doi: 10.1111/j.1600-0714.2010.00946.x. [DOI] [PubMed] [Google Scholar]
- 4.Scully C., Eisen D., Carrozzo M. Management of oral lichen planus. Am J Clin Dermatol. 2000;1(5):287–306. doi: 10.2165/00128071-200001050-00004. [DOI] [PubMed] [Google Scholar]
- 5.Abdel-kader Mahmoud H. 2016. CHAPTER 1:The Journey of PDT throughout History: PDT from Pharos to Present , inPhotodynamic Medicine: From Bench to Clinic; pp. 1–21. [Google Scholar]
- 6.Jajarm H.H., Falaki F., Sanatkhani M., et al. A comparative study of toluidine blue-mediated photodynamic therapy versus topical corticosteroids in the treatment of erosive-atrophic oral lichen planus: a randomized clinical controlled trial. Laser Med Sci. 2015;30:1475–1480. doi: 10.1007/s10103-014-1694-1. [DOI] [PubMed] [Google Scholar]
- 7.Saini R., Lee N.V., Liu K.Y., Poh C.F. Prospects in the application of photodynamic therapy in oral cancer and premalignant lesions. Cancers. 2016;8:83. doi: 10.3390/cancers8090083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prasanna S.W., Ingle E., Aruna P.R., Pravada C., Koteeswaran D., Ganesan S. Photodynamic therapy of oral leukoplakia and oral lichen planus using methylene blue: a pilot study. J Innov Opt Health Sci. 2015;8 [Google Scholar]
- 9.Bakhtiari S., Azari-Marhabi S., Mojahedi S.M., Namdari M., Rankohi Z.E., Jafari S. Comparing clinical effects of photodynamic therapy as a novel method with topical corticosteroid for treatment of Oral Lichen Planus. Photodiagnosis Photodyn Ther. 2017;20:159–164. doi: 10.1016/j.pdpdt.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Mostafa D., Moussa E., Alnouaem M. Evaluation of photodynamic therapy in treatment of oral erosive lichen planus in comparison with topically applied corticosteroids. Photodiagnosis Photodyn Ther. 2017 Sep;19:56–66. doi: 10.1016/j.pdpdt.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 11.Mirza S., Rehman N., Alrahlah A., Alamri W.R., Vohra F. Efficacy of photodynamic therapy or low level laser therapy against steroid therapy in the treatment of erosive-atrophic oral lichen planus. Photodiagnosis Photodyn Ther. 2018 Mar;21:404–408. doi: 10.1016/j.pdpdt.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Lavaee F., Shadmanpour M. Comparison of the effect of photodynamic therapy and topical corticosteroid on oral lichen planus lesions. Oral Dis. 2019;25:1954–1963. doi: 10.1111/odi.13188. [DOI] [PubMed] [Google Scholar]
- 13.Cosgarea R., Pollmann R., Sharif J., et al. Photodynamic therapy in oral lichen planus: a prospective case-controlled pilot study. Sci Rep. 2020;10:1667. doi: 10.1038/s41598-020-58548-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sabry M.A., Saafan A.M.E.-H., El-Shenawy H.M., Hussine A.A., El- Aziz D.M.A., Fadeel D.A.A. Effect of photodynamic therapy on pain control in patients with erosive/atrophic oral lichen planus. EurAsia J BioSci. 2020;14:7455–7460. [Google Scholar]
- 15.Saleh W., Tageldin S., Khashaba E., Darwish M., Elnagdy S., Khashaba O. Could photodynamic therapy be utilized as a treatment modality for oral lichen planus? Photodiagnosis Photodyn Ther. 2020;30 doi: 10.1016/j.pdpdt.2020.101677. [DOI] [PubMed] [Google Scholar]
- 16.Zborowski J., Kida D., Szarwaryn A., et al. A comparison of clinical efficiency of photodynamic therapy and topical corticosteroid in treatment of oral lichen planus: a split-mouth randomised controlled study. J Clin Med. 2021;10:3673. doi: 10.3390/jcm10163673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nauta J.M., van Leengoed H.L., Star W.M., Roodenburg J.L., Witjes M.J., Vermey A. Photodynamic therapy of oral cancer. A review of basic mechanisms and clinical applications. Eur J Oral Sci. 1996;104:69–81. doi: 10.1111/j.1600-0722.1996.tb00049.x. [DOI] [PubMed] [Google Scholar]
- 18.Daliri F., Azizi A., Goudarzi M., Lawaf S., Rahimi A. In vitro comparison of the effect of photodynamic therapy with curcumin and methylene blue on Candida albicans colonies. Photodiagnosis Photodyn Ther. 2019;26:193–198. doi: 10.1016/j.pdpdt.2019.03.017. [DOI] [PubMed] [Google Scholar]
- 19.Sulewska M., Duraj E., Sobaniec S., et al. A clinical evaluation of efficacy of photodynamic therapy in treatment of reticular oral lichen planus: a case series. Photodiagnosis Photodyn Ther. 2019;25:50–57. doi: 10.1016/j.pdpdt.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 20.Rakesh N., Clint J.B., Reddy S.S., et al. Clinical evaluation of photodynamic therapy for the treatment of refractory oral Lichen planus - a case series. Photodiagnosis Photodyn Ther. 2018;24:280–285. doi: 10.1016/j.pdpdt.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Aghahosseini F., Arbabi-Kalati F., Fashtami L.A., Fateh M., Djavid G.E. Treatment of oral lichen planus with photodynamic therapy mediated methylene blue: a case report. Med Oral Patol Oral Cir Bucal. 2006;11:E126–E129. [PubMed] [Google Scholar]