Abstract
Introduction
Multimorbidity, the presence of multiple chronic health conditions, generally starts in middle and older age but there is considerable heterogeneity in the trajectory of morbidity accumulation. This study aimed to clarify the number of distinct trajectories and the potential associations between race/ethnicity and socioeconomic status and these trajectories.
Methods
Data from 13,699 respondents (age ≥51) in the Health and Retirement Study between 1998 and 2016 were analyzed with growth mixture models. Nine prevalent self-reported morbidities (arthritis, cancer, cognitive impairment, depressive symptoms, diabetes, heart disease, hypertension, lung disease, stroke) were summed for the morbidity count.
Results
Three trajectories of morbidity accumulation were identified: low [starting with few morbidities and accumulating them slowly (i.e., low intercept and low slope); 80% of sample], increasing (i.e., low intercept and high slope; 9%), and high (i.e., high intercept and low slope; 11%). Compared to non-Hispanic (NH) White adults in covariate-adjusted models, NH Black adults had disadvantages while Hispanic adults had advantages. Our results suggest a protective effect of education for NH Black adults (i.e., racial health disparities observed at low education were ameliorated and then eliminated at increasing levels of education) and a reverse pattern for Hispanic adults (i.e., increasing levels of education was found to dampen the advantages Hispanic adults had at low education). Compared with NH White adults, higher levels of wealth were protective for both NH Black adults (i.e., reducing or reversing racial health disparities observed at low wealth) and Hispanic adults (i.e., increasing the initial health advantages observed at low wealth).
Conclusion
These findings have implications for addressing health disparities through more precise targeting of public health interventions. This work highlights the imperative to address socioeconomic inequalities that interact with race/ethnicity in complex ways to erode health.
Keywords: Racial health disparities; Chronic illness; Morbidity; Socioeconomic status; Education; Wealth, Older adults; Growth mixture model
Highlights
-
•
Three trajectories of morbidity accumulation were identified among older adults.
-
•
The morbidity trajectories were: high, increasing and low.
-
•
Race, ethnicity, and education were associated with morbidity trajectory.
-
•
Education and wealth interacted in distinct ways with race/ethnicity to predict trajectory.
-
•
Racial health disparities ameliorated or even reversed with increasing wealth.
1. Introduction
Multimorbidity, the co-occurrence of multiple chronic morbidities, is associated with greater healthcare costs, poorer quality of life, and higher risk of mortality (Marques et al., 2018; Schiøtz et al., 2017; Wei & Mukamal, 2018). Multimorbidity generally starts in middle and old age, but younger generations have been developing multimorbidity at earlier ages than their predecessors, signaling a growing problem (Bishop et al., 2022; Canizares et al., 2018; Violan et al., 2014). Even in the same age group, the prevalence of multimorbidity has been found to vary greatly (Strauss et al., 2014). The elevated risks of multimorbidity necessitate a more complete understanding of how morbidities accumulate and the social and economic inequality that may put some individuals at greater risk of multimorbidity (Pathirana & Jackson, 2018; Quiñones et al., 2019). Studies seeking to identify homogenous latent classes demonstrating distinct trajectories of morbidity accumulation from within the larger population have generally found three to four classes consisting of a relatively morbidity-free trajectory, a relatively high morbidity trajectory, and at least one trajectory that is rapidly accumulating morbidities over time (e.g., Lee et al., 2021; Tarraf et al., 2020; Wickrama et al., 2013). The variation found in both the number and types of trajectories may be due to differences in sample (e.g., age group) and methodology (e.g., morbidity operationalization). It is critical to understand how these changes occur over time for populations at most at risk for multimorbidity.
1.1. Racial, ethnic, and socioeconomic differences in morbidity accumulation
Race/ethnicity and SES are highly correlated and are each important social determinants of health (LaVeist, 2005). Social inequality creates conditions that erode health (e.g., heavy pollution, interpersonal discrimination, occupational hazards) while limiting access to resources that protect and promote health (e.g., healthcare, nutritious food) for marginalized racial/ethnic groups and for individuals with low socioeconomic status (SES) (e.g., Williams & Sternthal, 2010). Little research has explored how these racial/ethnic and socioeconomic factors interact to produce different trajectories of morbidity accumulation. It is important to disentangle the effects of race/ethnicity and SES as they are often overlapping yet independent social determinants of health (LaVeist, 2005). Understanding how these factors interplay can help identify the most at-risk populations so that preventative care can be delivered early and to provide further rationale and direction for policies and programs that reduce social inequality.
Research about the prevalence of multimorbidity and the rate of morbidity accumulation has found largely consistent patterns by race/ethnicity (e.g., Ashworth et al., 2019; Quiñones et al., 2011, 2019; St Sauver et al., 2015; Tarraf et al., 2020). Non-Hispanic (NH) Black adults have the greatest prevalence of multimorbidity in each age category of any racial/ethnic group whereas Hispanic adults had lower prevalence rates than their NH White counterparts (Caraballo et al., 2021). St Sauver et al. (2015) found that the incidence of multimorbidity increased more rapidly among NH Black patients than NH White patients. NH Black middle-aged and older adults had higher initial morbidities than NH White adults but accumulated morbidities at a slower rate (Quiñones et al., 2011, 2019). Hispanic Americans have sometimes been found to have equivalent or better health than their NH White counterparts despite having a higher likelihood of experiencing SES conditions that are predictive of poorer health (e.g., higher poverty rates). This phenomenon is commonly referred to as the ‘Hispanic health paradox’ (Markides & Eschbach, 2005), which has received mixed support in research examining morbidity trajectories. Although Hispanic adults tend to have fewer initial morbidities than NH White adults, one area of uncertainty with respect to the differences between Hispanic and NH White health differences is in multimorbidity accumulation such that some studies have found slower accumulation while others have found faster accumulation (Quiñones et al., 2011, 2019). Tarraf et al. (2020) found that Hispanic participants had greater likelihood of being in the healthy versus the nonaccelerated trajectory class but also had greater likelihood of being in the high versus the nonaccelerated trajectory class than their NH White counterparts. Illuminating the SES conditions under which the Hispanic health paradox is observed in morbidity accumulation studies may help explain the apparent discrepancies in this area.
Meta-analyses have found that SES is inversely associated with the prevalence of multimorbidity such that having less education, income, and wealth are associated with greater odds of having multimorbidity (Pathirana & Jackson, 2018; Violan et al., 2014). Taken together, social inequalities are reflected in disproportionately high prevalence of multimorbidity in NH Black adults, those with fewer financial resources, and those with lower educational attainment.
1.2. The interplay between SES and race/ethnicity on morbidity accumulation
Sociological research has documented that SES interacts with race/ethnicity in complex ways to impact health (Williams & Sternthal, 2010). SES factors can account for some racial health disparities (Clark et al., 2016; Khullar & Chokshi, 2018). However, some research has shown that Black-White racial health disparities remain or are more pronounced at higher levels of income, potentially because White adults see relatively greater health gains at higher levels of income (Colen et al., 2018). Accordingly, the diminishing returns hypothesis asserts that marginalized racial/ethnic groups see decreasing returns in their health improvement as their SES increases (Farmer & Ferraro, 2005). Further work is needed to investigate the possible interaction between race/ethnicity and SES on morbidity accumulation.
1.3. Current study
The purpose of this study is to identify latent subpopulations with distinct trajectories of morbidity accumulation within a sample of middle-aged to older adults, elucidate the connections between race/ethnicity and morbidity trajectories, and investigate how SES moderates (i.e., modifies) the associations between race/ethnicity and morbidity trajectories. Specifically, we conceptualized education and wealth to be moderators of the connections between race/ethnicity and morbidity trajectories. Four research questions were examined: (1) what are the distinctive trajectories of morbidity accumulation in older adults aged ≥51, (2) what is the influence of race/ethnicity on these morbidity trajectories, (3) how does education moderate the association between race/ethnicity and morbidity trajectory, and (4) how does wealth moderate the association between race/ethnicity and morbidity trajectory? Answering these questions would help researchers, policymakers, and clinicians better understand how older adults from these racial, ethnic, and socioeconomic backgrounds vary in their patterns of morbidity accumulation. This study will make several contributions by investigating how race/ethnicity, education, wealth, and the intersection of these factors account for differences in the trajectory of morbidity accumulation.
2. Material and methods
2.1. Data
Analyses used eighteen years of data from the Health and Retirement Study (HRS) (1998–2016), a nationally representative sample of community-based adults aged 51 years and older. Residents of nursing homes, those who did not participate in the initial wave, and those who did not contribute to the morbidity outcome for the first wave were excluded. Additionally, participants with missing race/ethnicity (n = 497) or who indicated American Indian, Asian, or “other” race/ethnicities (n = 1,088 across these groups) were excluded due to small group sizes. The final analytic sample (N = 13,699) was 63.05 years of age on average (SD = 8.90) in 1998; 59.30% female; 76.84% NH White, 13.22% NH Black, and 8.21% Hispanic; 91.05% U.S. born; with an average of 12.25 years of education (SD = 3.28); median wealth (USD) of $143,000 (interquartile range: $50,000 - $352,000); and an average of 1.58 morbidities (SD = 1.29) in 1998.
2.2. Measures
Morbidity. Morbidity was measured as the sum of nine possible self-reported chronic conditions available from the data source. Respondents were asked “Has a doctor ever told you that you have/had … ?” the following conditions: arthritis, cancer (excluding skin cancer), cognitive impairment, depressive symptoms, diabetes, heart disease, hypertension, lung disease (excluding asthma), and stroke. Cutoff values were used to determine the presence of high depressive symptoms (CESD 8-item score ≥4; Radloff, 1977; Turvey et al., 1999) and cognitive impairment (≤10 or less on the 35-point scale for the Telephone Interview for Cognitive Status). We utilized an adjudication method for resolving inconsistent reports of morbidity over time for somatic morbidities (Cigolle et al., 2018).
Education. Educational attainment was assessed as number of years of schooling (range 0–17).
Wealth. Wealth was assessed in 1998 with the RAND household net worth variable (i.e., total wealth minus total debt; in US dollars) to encapsulate the total level of financial resources for retired individuals or those nearing retirement age (LaVeist, 2005).
Race/ethnicity. Race/ethnicity were recoded into mutually exclusive categories, using NH White adults as the referent group: Hispanic vs. NH White (0 = NH White, 1 = Hispanic) and NH Black vs. NH White (0 = NH White, 1 = NH Black).
Covariates. Models included the following covariates assessed in 1998: age (in years), alcoholic drinks consumed per week (number drinking days/week * number drinks/day), body mass index (BMI, computed with self-reported height and weight), nativity (0 = foreign-born, 1 = born in the U.S.), physical activity (0 = no regular vigorous physical activity over the last year, 1 = engaged in such physical activity), sex (0 = male, 1 = female), current smoker, and former smoker. Covariate selection was guided by prior research and includes covariates that might be confounded with race/ethnicity.
2.3. Statistical methodology
Analyses were conducted with Mplus (version 8; Muthén & Muthén, 2018) using full information maximum likelihood (FIML) for missing data with robust estimation (Yuan & Bentler, 2000), which has been shown to produce less biased parameter estimates and more accurate standard errors than listwise deletion (Collins et al., 2001). Baseline sample weights and sampling design adjustments were applied to all analyses (Heeringa & Connor, 1995).
Analyses were conducted in three phases, each employing growth mixture models (GMMs), where the outcome for each model was probable membership in a morbidity trajectory class versus another relative to the referent racial/ethnic group (NH White adults). In the first phase, we used unconditional GMMs to identify homogeneous sub-populations where separate trajectories are based on initial number of morbidities (intercept) and rate of accumulation (slope) for each sub-population (Jung & Wickrama, 2008). We assessed three to five morbidity trajectories for goodness of fit based on previous studies (e.g., Tarraf et al., 2020), following recommendations for optimal class enumeration by examining several fit indices including the Bayesian information criterion (BIC), bootstrapped likelihood ratio test (BLRT), and entropy (Collins & Lanza, 2010; Nylund et al., 2007). We also tested multiple forms (linear, quadratic) in the one-class solution.
In the second phase, we examined how race/ethnicity and SES are associated with class membership. Estimates of these associations (between primary study variables and the likelihood of belonging to each trajectory class) are multinomial logistic path coefficients in which one outcome class serves as the comparison group. In the third phase, we used these models to detect and probe interactions of race/ethnicity and SES on class membership. Separate models were estimated for SES variables (education, wealth) while controlling for the other SES variable along with other covariates. In this way, both education and wealth were included as a predictor/covariate in all associative models. For each model an interaction term was computed for race/ethnicity and SES. Significant interaction coefficients do not provide information about the nature and direction of the differences, so we conducted a series of simple effects tests to probe the nature of these interactions (Aiken & West, 1991; Jaccard, 2001). The simple effects tests assessed 6 separate models to obtain estimates for each level (i.e., low, medium, and high) of education and wealth. To categorize levels of education, we used conventional values of one standard deviation below the mean for low education (9.1 years of education), the mean for medium education (12.4 years), and one standard deviation above the mean for high education (15.7 years). Because wealth was highly skewed, we used quartiles for the levels. The 25th percentile was assigned for low wealth ($50,000.00), the median for medium wealth ($143,000.00), and the 75th percentile for high wealth ($342,000.00). The methodological approach is more complicated than a standard interaction model because we were interested in interactions between SES variables, which are continuous, and race/ethnicity, which involves two categorical dummy variables, on their association with trajectories rather than association with a cross-sectional outcome. To improve interpretability of class membership probabilities and simple effects, most predictors/covariates were grand mean-centered except race/ethnicity, sex, nativity, physical activity, and smoking status.
3. Results
3.1. Phase 1: Unconditional GMM models
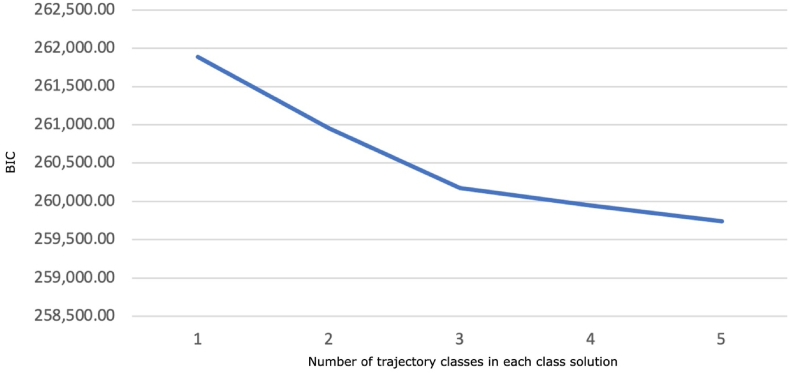
Unconditional (i.e., which include no predictors) latent class models were first used to investigate the number of latent trajectory classes. The initial model that included a quadratic trajectory along with a linear trajectory of the morbidity index (BIC = 255,775.37) fit better than the model with just a linear effect alone (BIC = 261,884.91). Although the quadratic effect was significant in the initial model, its magnitude was small (β = -0.001, β* = -0.045, p < .01) compared with the linear effect (β = 0.215, β* = 0.682, p <. 001). Given that the small effect size of the quadratic effect was likely to have minimal statistical impact on the other estimates while being of little clinical importance, we proceeded to investigate latent trajectory classes specifying a linear trajectory. Fit indices obtained from the class enumeration process are presented in Table 1. Although the BLRT was significant for every model, indicating better fit than preceding models with fewer classes, the statistical power of these tests was high due to the large sample size. Prior work documents a general tendency to overestimate the number of classes (Bauer & Curran, 2003; Nylund-Gibson & Choi, 2018), therefore distinguishing between statistical significance and practical differences in fit is important. Following recommendations (Nylund-Gibson & Choi, 2018), we plotted each model’s BIC values (Fig. 1). The plot shows gradually decreasing BIC values up to three class and then a plateau after three classes (i.e., the ‘elbow’ of the line). This suggests that three-class solution was the optimal and most parsimonious representation of the data.
Table 1.
Class enumeration of latent multimorbidity trajectories (N = 13,699).
| Number of Trajectories | BIC | BLRT p | Entropy |
|---|---|---|---|
| 1 | 261,884.91 | – | – |
| 2 | 260,956.55 | .000 | .717 |
| 3 | 260,175.42 | .000 | .707 |
| 4 | 259,946.25 | .000 | .703 |
| 5 | 259,741.28 | .000 | .700 |
Abbreviations: BIC = Bayesian Information Criteria, BLRT p = bootstrapped likelihood ratio test p-value.
Fig. 1.
Scree plot comparing the BIC model fit of class solutions with an increasing number of trajectory classes.
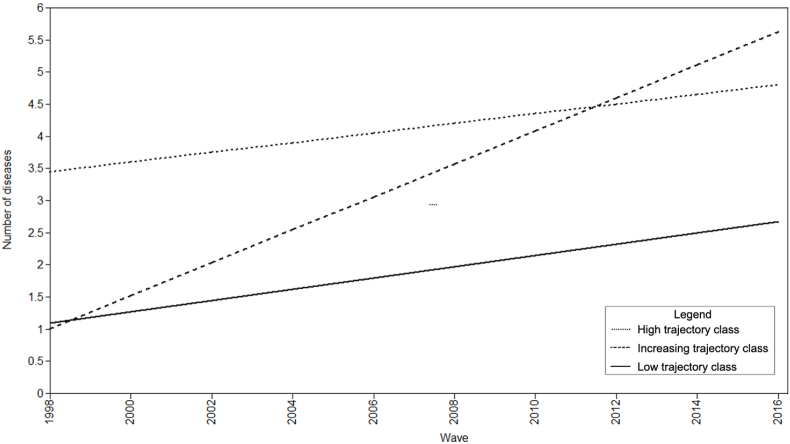
The three-class model had three meaningful morbidity trajectory patterns, which we refer to as “low trajectory class,” “increasing trajectory class,” and “high trajectory class.” Individuals in the low trajectory class started with relatively few morbidities (intercept: β = 1.09, SE = 0.03, p < .001) that increased gradually (slope: β = 0.18, SE = 0.00, p < .001). This was the healthiest group and included most of the sample (n = 10,950; 80%). Individuals in the increasing trajectory class (n = 1,175; 9%) started with relatively few morbidities (intercept: β = 1.00, SE = 0.06, p < .001) but increased rapidly (slope: β = 0.51, SE = 0.02, p < .001), acquiring approximately 0.51 morbidities per wave. Individuals in the high trajectory class (n = 1,574, 11%) started with the most morbidities (intercept: β = 3.45, SE = 0.10, p < .001) and increased slowly (slope: β = 0.15, SE = 0.01, p < .001). Fig. 2 presents a line graph of the trajectories. Entropy for the three-class model was 0.707. Table 2 presents overall and class-specific demographic information.
Fig. 2.
Graph of the low, increasing, and high trajectories from the unconditional model (N = 13,699).
Table 2.
Demographic characteristics of the total study sample at 1998 (N = 13,699).
| Variable | Overall Sample | Class 1 |
Class 2 |
Class 3 |
|---|---|---|---|---|
| Low Trajectory | Increasing Trajectory | High Trajectory | ||
| N (% of sample) | 13,699 (100%) | 10,950 (80%) | 1,175 (9%) | 1,574 (11%) |
| Age, mean (SD) | 63.05 (8.90) | 62.35 (8.79) | 65.06 (8.92) | 65.83 (8.81) |
| Female, n (%) | 8,124 (59.30%) | 6,323 (59.30%) | 625 (51.61%) | 1,176 (64.40%) |
| Race/Ethnicity | ||||
| Hispanic, n (%) | 1,103 (8.21%) | 829 (7.93%) | 102 (8.52%) | 172 (9.59%) |
| NH Black, n (%) | 1,811 (13.22%) | 1,287 (12.32%) | 140 (11.70%) | 384 (21.42%) |
| NH White, n (%) | 10,525 (76.84%) | 8,333 (79.75%) | 955 (79.78%) | 1,237 (68.99%) |
| Socioeconomic status | ||||
| Years of education, mean (SD) | 12.25 (3.28) | 12.54 (3.15) | 11.90 (3.29) | 10.84 (3.57) |
| Wealth (USD), median (IQR) | $143,000 ($50,000 - $352,000) | $161,350 ($59,000 – $389,000) | $126,000 ($43,200-$303,500) | $66,400 ($9,400-$195,500) |
| Nativity | ||||
| U.S.-born, n (%) | 12,458 (91.05%) | 9,670 (90.82%) | 1,115 (92.15%) | 1,673 (91.67%) |
| Health and lifestyle | ||||
| Number of morbidities, mean (SD) | 1.58 (1.29) | 1.25 (0.99) | 1.27 (1.00) | 3.73 (1.02) |
| No morbidities at baseline, n (%) | 3,025 (22.08%) | 2,718 (25.82%) | 307 (26.13%) | 0 (0%) |
| No morbidities at final wave, n (%) | 285 (2.08%) | 285 (2.60%) | 0 (0%) | 0 (0%) |
| BMI, mean (SD) | 27.39 (5.21) | 26.98 (4.86) | 27.83 (5.69) | 29.47 (6.21) |
| Engaged in regular physical activity in the last year, n (%) | 6,644 (48.51%) | 5,474 (51.36%) | 565 (46.66%) | 605 (33.15%) |
| Alcoholic drinks per week, mean (SD) | 2.31 (5.86) | 2.46 (6.01) | 2.48 (6.12) | 1.37 (4.52) |
| Current smoker, n (%) | 2,220 (16.2%) | 1,603 (15.04%) | 322 (26. 61%) | 295 (16.16%) |
| Former smoker, n (%) | 7,831 (57.70%) | 5,897 (55.87%) | 809 (67.25%) | 1,125 (61.95%) |
Note. NH – Non-Hispanic. Note that in the overall sample, there were missing data for race/ethnicity (n = 260; 0.02%) and nativity (n = 17; 0.00%).
3.2. Phase 2: Associative models
We next examined how race/ethnicity and SES are associated with membership into morbidity trajectories. The first associative model regressed probable class membership on race/ethnicity (Table 3). Multiple significant effects were evident for NH Black adults but not Hispanic adults. For example, NH Black adults were almost three times as likely as NH White adults to belong to the high versus the low trajectory (OR = 2.925, 95% CI [2.419, 3.537], p < .001).
Table 3.
Unconditional likelihood of class membership into trajectory for racial and ethnic comparisons (N = 13,439).
| Trajectory comparison | Racial/ethnic group | OR | CI | p-value |
|---|---|---|---|---|
| High versus low | ||||
| NH Black | 2.925 | 2.419, 3.537 | .000 | |
| Hispanic | 1.238 | 0.977, 1.567 | .077 | |
| Increasing versus low | ||||
| NH Black | 1.203 | 0.914, 1.582 | .187 | |
| Hispanic | 1.252 | 0.941, 1.666 | .123 | |
| High versus increasing | ||||
| NH Black | 2.432 | 1.837, 3.219 | .000 | |
| Hispanic | 0.988 | 0.721, 1.355 | .943 | |
Note. Low – Low trajectory, Increasing – Increasing trajectory, High – High trajectory, NH – Non-Hispanic. NH White is the referent group. This model was not adjusted for additional covariates beyond race/ethnicity. All estimates are unstandardized. Significant effects are bolded.
The second associative model built on the first by adding SES variables and covariates (Table 4). Across the outcome comparisons, significant effects were evident for NH Black adults (i.e., disadvantages compared with NH White adults) while only one significant effect was observed for Hispanic adults (i.e., an advantage compared with NH White adults). Notably, the health advantage for Hispanic adults reflected a difference in the initial number of morbidities [less likely to belong to the high versus the low trajectory class than NH White adults (OR = 0.416, 95% CI (0.238, 0.728), p < .01)] but not the rate of morbidity accumulation [less likely to belong to the increasing versus the low trajectory class (OR = 0.935, 95% CI [0.503, 1.739], p = ns)]. Significant effects emerged for education but not wealth: a unit increase in education resulted in a moderate reduction of the likelihood of belonging to the high rather than low trajectory (OR = 0.780, 95% CI [0.724, 0.840], p < .001).
Table 4.
Direct effects of predictors on trajectory membership (N = 13,424).
| Trajectory comparison | Log Coeff. | OR (95% CI) | p-value |
|---|---|---|---|
| High versus Low | |||
| Age | 0.189 | 1.208 (1.139, 1.281) | .000 |
| Female | 0.319 | 1.376 (1.064, 1.778) | .015 |
| US born | 0.466 | 1.594 (0.955, 2.663) | .075 |
| BMI | 0.282 | 1.325 (1.213, 1.448) | .000 |
| Physical activity | -1.140 | 0.320 (0.245, 0.418) | .000 |
| Drinks per week | -0.035 | 0.966 (0.939, 0.993) | .015 |
| Current smoker | 0.553 | 1.738 (1.093, 2.763) | .019 |
| Former smoker | 0.964 | 2.623 (1.933, 3.561) | .000 |
| NH Black | 0.705 | 2.024 (1.335, 3.069) | .001 |
| Hispanic | -0.877 | 0.416 (0.238, 0.728) | .002 |
| Education | -0.248 | 0.780 (0.724, 0.840) | .000 |
| Wealth | -0.168 | 0.845 (0.669, 1.068) | .159 |
| Increasing versus Low | |||
| Age | 0.157 | 1.170 (1.114, 1.228) | .000 |
| Female | 0.068 | 1.070 (0.887, 1.291) | .480 |
| US born | 0.436 | 1.546 (1.132, 2.111) | .006 |
| BMI | 0.215 | 1.240 (1.152, 1.335) | .000 |
| Physical activity | -0.426 | 0.653 (0.549, 0.778) | .000 |
| Drinks per week | -0.012 | 0.988 (0.967, 1.010) | .276 |
| Current smoker | 0.552 | 1.738 (1.138, 2.652) | .010 |
| Former smoker | 0.511 | 1.667 (1.261, 2.203) | .000 |
| NH Black | 0.491 | 1.634 (1.125, 2.374) | .010 |
| Hispanic | -0.067 | 0.935 (0.503, 1.739) | .831 |
| Education | -0.137 | 0.872 (0.821, 0.925) | .000 |
| Wealth | -0.015 | 0.985 (0.969, 1.001) | .075 |
| High versus Increasing | |||
| Age | -0.157 | 0.855 (0.814, 0.898) | .000 |
| Female | -0.068 | 0.935 (0.775, 1.128) | .480 |
| US born | -0.436 | 0.647 (0.474, 0.883) | .006 |
| BMI | -0.215 | 0.806 (0.749, 0.868) | .000 |
| Physical activity | 0.426 | 1.531 (1.286, 1.822) | .000 |
| Drinks per week | 0.012 | 1.012 (0.991, 1.034) | .276 |
| Current smoker | -0.552 | 0.576 (0.377, 0.878) | .010 |
| Former smoker | -0.511 | 0.600 (0.454, 0.793) | .000 |
| NH Black | -0.491 | 0.612 (0.421, 0.889) | .010 |
| Hispanic | 0.067 | 1.070 (0.575, 1.990) | .831 |
| Education | 0.137 | 1.147 (1.081, 1.218) | .000 |
| Wealth | 0.015 | 1.015 (0.999, 1.032) | .075 |
Note. Low – Low trajectory, Increasing – Increasing trajectory, High – High trajectory, NH – Non-Hispanic. NH White is the referent group for the racial/ethnic group comparisons while nonsmoking status is the referent group for the smoking status variables. All estimates are unstandardized. Each predictor/covariate was grand mean-centered except for nativity, physical activity, dummy variables for race/ethnicity, and sex, smoking variables to aid in interpretation. All estimates are unstandardized. Significant effects are bolded.
3.3. Phase 3: Moderation detection and probing models
We next examined potential interactions of race/ethnicity and SES on membership of morbidity trajectories and present these in Table 5. A significant interaction was detected between education and the Hispanic/NH White comparison, and significant interactions were detected between wealth and the Hispanic/NH White and the NH Black/NH White comparisons.
Table 5.
Detecting interactions between race/ethnicity and socioeconomic status moderators on trajectory membership (N = 13,120).
| Trajectory comparison | Model 1: Education as moderator |
Model 2: Wealth as moderator |
||||
|---|---|---|---|---|---|---|
| Log coeff. | OR (95% CI) | p-value | Log coeff. | OR (95% CI) | p-value | |
| High versus Low | ||||||
| Age | 0.190 | 1.209 (1.144, 1.278) | .000 | 0.180 | 1.197 (1.135, 1.262) | .000 |
| Female | 0.324 | 1.382 (1.069, 1.788) | .014 | 0.314 | 1.368 (1.054, 1.776) | .018 |
| US born | 0.378 | 1.460 (0.911, 2.339) | .116 | 0.398 | 1.489 (0.872, 2.543) | .145 |
| Physical activity | -1.140 | 0.320 (0.243, 0.420) | .000 | -1.147 | 0.318 (0.243, 0.415) | .000 |
| Drinks per week | -0.035 | 0.966 (0.939, 0.994) | .016 | -0.033 | 0.968 (0.943, 0.993) | .014 |
| Current smoker | 0.547 | 1.727 (1.100, 2.713) | .018 | 0.480 | 1.615 (1.041, 2.506) | .032 |
| NH Black | 0.653 | 1.921 (1.260, 2.927) | .002 | -1.626 | 0.197 (0.042, 0.914) | .038 |
| Hispanic | -0.426 | 0.653 (0.353, 1.210) | .176 | -1.332 | 0.264 (0.091, 0.764) | .014 |
| Education | -0.265 | 0.767 (0.712, 0.826) | .000 | -0.227 | 0.797 (0.745, 0.852) | .000 |
| Wealth | -0.166 | 0.847 (0.658, 1.091) | .200 | -0.213 | 0.809 (0.692, 0.944) | .007 |
| BMI | 0.284 | 1.328 (1.223, 1.442) | .000 | 0.268 | 1.308 (1.204, 1.420) | .000 |
| NH Black*Education | -0.103 | 0.902 (0.792, 1.027) | .118 | – | – | – |
| Hispanic*Education | 0.137 | 1.147 (1.025, 1.284) | .017 | – | – | – |
| NH Black*Wealth | – | – | – | -0.765 | 0.465 (0.287, 0.754) | .002 |
| Hispanic*Wealth | – | – | – | -0.185 | 0.831 (0.572, 1.207) | .330 |
| Increasing versus Low | ||||||
| Age | 0.158 | 1.171 (1.117, 1.228) | .000 | 0.150 | 1.162 (1.113, 1.213) | .000 |
| Female | 0.069 | 1.071 (0.891, 1.287) | .464 | 0.070 | 1.072 (0.893, 1.288) | .455 |
| US born | 0.369 | 1.446 (1.078, 1.938) | .014 | 0.451 | 1.571 (1.164, 2.119) | .003 |
| BMI | 0.216 | 1.242 (1.158, 1.331) | .000 | 0.206 | 1.229 (1.150, 1.313) | .000 |
| Physical activity | -0.424 | 0.655 (0.548, 0.782) | .000 | -0.423 | 0.655 (0.554, 0.774) | .000 |
| Drinks per week | -0.012 | 0.988 (0.967, 1.010) | .286 | -0.013 | 0.987 (0.968, 1.007) | .202 |
| Current smoker | 0.547 | 1.728 (1.142, 2.615) | .010 | 0.489 | 1.631 (1.096, 2.427) | .016 |
| Former smoker | 0.507 | 1.660 (1.254, 2.198) | .000 | 0.519 | 1.681 (1.300, 2.173) | .000 |
| NH Black | 0.470 | 1.599 (1.075, 2.381) | .021 | 0.054 | 1.055 (0.293, 3.800) | .935 |
| Hispanic | 0.204 | 1.226 (0.739, 2.035) | .431 | -1.243 | 0.288 (0.125, 0.664) | .003 |
| Education | -0.156 | 0.856 (0.806, 0.909) | .000 | -0.124 | 0.883 (0.837, 0.931) | .000 |
| Wealth | -0.014 | 0.986 (0.970, 1.001) | .073 | -0.014 | 0.986 (0.972, 1.001) | .061 |
| NH Black*Education | -0.093 | 0.911 (0.799, 1.038) | .161 | – | – | – |
| Hispanic*Education | 0.121 | 1.128 (1.000, 1.273) | .050 | – | – | – |
| NH Black*Wealth | – | – | – | -0.166 | 0.847 (0.562, 1.277) | .429 |
| Hispanic*Wealth | – | – | – | -0.438 | 0.646 (0.467, 0.892) | .008 |
| High versus Increasing | ||||||
| Age | 0.032 | 1.033 (1.018, 1.048) | .000 | 0.030 | 1.030 (1.014, 1.046) | .000 |
| Female | 0.255 | 1.291 (1.065, 1.565) | .009 | 0.244 | 1.276 (1.044, 1.559) | .017 |
| US born | 0.010 | 1.010 (0.652, 1.565) | .965 | -0.053 | 0.948 (0.598, 1.505) | .821 |
| BMI | 0.067 | 1.070 (1.045, 1.094) | .000 | 0.062 | 1.064 (1.039, 1.090) | .000 |
| Physical activity | -0.717 | 0.488 (0.390, 0.612) | .000 | -0.723 | 0.485 (0.387, 0.608) | .000 |
| Drinks per week | -0.023 | 0.977 (0.955, 1.000) | .053 | -0.020 | 0.980 (0.958, 1.003) | .092 |
| Current smoker | 0.000 | 1.000 (0.716, 1.397) | .999 | -0.009 | 0.991 (0.731, 1.342) | .952 |
| Former smoker | 0.458 | 1.581 (1.311, 1.907) | .000 | 0.442 | 1.555 (1.281, 1.889) | .000 |
| NH Black | 0.183 | 1.201 (0.885, 1.630) | .240 | -1.679 | 0.187 (0.038, 0.924) | .040 |
| Hispanic | -0.629 | 0.533 (0.320, 0.888) | .016 | -0.089 | 0.915 (0.527, 1.591) | .754 |
| Education | -0.110 | 0.896 (0.858, 0.936) | .000 | -0.103 | 0.902 (0.875, 0.930) | .000 |
| Wealth | -0.151 | 0.859 (0.668, 1.106) | .239 | -0.199 | 0.820 (0.703, 0.956) | .011 |
| NH Black*Education | -0.010 | 0.990 (0.935, 1.049) | .735 | – | – | – |
| Hispanic*Education | 0.017 | 1.017 (0.925, 1.118) | .729 | – | – | – |
| NH Black*Wealth | – | – | – | -0.599 | 0.549 (0.325, 0.928) | .025 |
| Hispanic*Wealth | – | – | – | 0.252 | 1.287 (1.050, 1.578) | .015 |
Note. Log coeff. – Logistic coefficient, Low – Low trajectory, Increasing – Increasing trajectory, High – High trajectory, NH – Non-Hispanic. NH White is the referent group for the racial/ethnic group comparisons while nonsmoking status is the referent group for the smoking status variables. Each predictor/covariate was grand mean-centered except for nativity, physical activity, dummy variables for race/ethnicity, and sex, smoking variables to aid in interpretation. All estimates are unstandardized. All covariates were included in this model, but only the effects of the primary study variables are presented here for clarity. Significant interactions are bolded.
Analyses probing the interactions at low, medium, and high SES levels are presented in Table 6. Health advantages for Hispanic adults diminished as education increased, suggesting that education did not provide protective effects for this group. Hispanic adults with lower levels of education were significantly less likely to belong to the high versus the low trajectory class (OR = 0.398, 95% CI [0.236, 0.671], p < .01) than NH White adults, whereas there was no such difference at medium or high levels of education. In contrast, education provided protective effects for NH Black adults such that the detrimental effects that emerged at the low and medium levels of education disappeared at the high level of education. For example, NH Black adults with a low level of education were more than two and a half times as likely to belong to the high versus the low trajectory class (OR = 2.790, 95% CI [1.430, 5.446], p < .01) whereas there was no such difference for those with a high level of education (OR = 1.398, 95% CI [0.813, 2.403], p = ns). A similar pattern was found for NH Black compared with NH White adults belonging to the increasing versus the low trajectory class, such that the large difference at the low level of education (OR = 2.242, 95% CI [1.186, 4.239], p < .05), a smaller difference at the medium level of education (OR = 1.599, 95% CI [1.075, 2.381], p < .05), and no difference at the high level of education (OR = 1.200, CI 95% [0.695, 2.073], p = ns).
Table 6.
Probing interactions between race/ethnicity and socioeconomic status moderators on trajectory membership (N = 13,120).
| Models 1a-c: Education as the moderator | Models 2a-c: Wealth as the moderator | |||||
|---|---|---|---|---|---|---|
| Trajectory comparison | Log coeff. | OR (95% CI) | p-value | Log coeff. | OR (95% CI) | p-value |
| Low level | ||||||
| High versus Low | ||||||
| NH Black | 1.026 | 2.790 (1.430, 5.446) | .003 | 0.664 | 1.942 (1.312, 2.876) | .001 |
| Hispanic | -0.922 | 0.398 (0.236, 0.671) | .001 | -0.777 | 0.460 (0.257, 0.822) | .009 |
| Increasing versus Low | ||||||
| NH Black | 0.807 | 2.242 (1.186, 4.239) | .013 | 0.550 | 1.732 (1.250, 2.402) | .001 |
| Hispanic | -0.232 | 0.793 (0.448, 1.401) | .424 | 0.066 | 1.068 (0.548, 2.081) | .846 |
| High versus Increasing | ||||||
| NH Black | 0.219 | 1.245 (0.883, 1.754) | .211 | 0.114 | 1.121 (0.817, 1.538) | .478 |
| Hispanic | -0.690 | 0.502 (0.336, 0.749) | .001 | -0.843 | 0.430 (0.263, 0.704) | .001 |
| Medium level | ||||||
| High versus Low | ||||||
| NH Black | 0.653 | 1.921 (1.260, 2.927) | .002 | -0.048 | 0.953 (0.510, 1.782) | .881 |
| Hispanic | -0.426 | 0.653 (0.353, 1.210) | .176 | -0.950 | 0.387 (0.220, 0.679) | .001 |
| Increasing versus Low | ||||||
| NH Black | 0.470 | 1.599 (1.075, 2.381) | .021 | 0.395 | 1.485 (0.891, 2.475) | .129 |
| Hispanic | 0.204 | 1.226 (0.739, 2.035) | .431 | -0.341 | 0.711 (0.403, 1.254) | .239 |
| High versus Increasing | ||||||
| NH Black | 0.183 | 1.201 (0.885, 1.630) | .240 | -0.443 | 0.642 (0.359, 1.148) | .135 |
| Hispanic | -0.629 | 0.533 (0.320, 0.888) | .016 | -0.609 | 0.544 (0.355, 0.834) | .005 |
| High level | ||||||
| High versus Low | ||||||
| NH Black | 0.335 | 1.398 (0.813, 2.403) | .226 | -1.647 | 0.193 (0.041, 0.906) | .037 |
| Hispanic | -0.003 | 0.997 (0.423, 2.347) | .994 | -1.337 | 0.263 (0.090, 0.767) | .014 |
| Increasing versus Low | ||||||
| NH Black | 0.182 | 1.200 (0.695, 2.073) | .513 | 0.049 | 1.050 (0.288, 3.824) | .941 |
| Hispanic | 0.575 | 1.777 (0.877, 3.597) | .110 | -1.256 | 0.285 (0.123, 0.660) | .003 |
| High versus Increasing | ||||||
| NH Black | 0.153 | 1.165 (0.801, 1.694) | .425 | -1.696 | 0.183 (0.036, 0.922) | .040 |
| Hispanic | -0.578 | 0.561 (0.271, 1.162) | .120 | -0.081 | 0.922 (0.528, 1.608) | .774 |
Note. Log coeff. – Logistic coefficient, Low – Low trajectory, Increasing – Increasing trajectory, High – High trajectory, NH – Non-Hispanic. NH White is the referent group for the racial/ethnic group comparisons. Each predictor/covariate was grand mean-centered except for nativity, physical activity, dummy variables for race/ethnicity, and sex, smoking variables to aid in interpretation. All estimates are unstandardized. All covariates were included in this model but only simple effects are presented here for clarity. Significant simple effects are bolded. For the education, the low level was 1 SD below the mean (9.11 years of education), the medium level was the mean (12.39 years), and the high level was 1 SD above the mean (15.673 years). In contrast, for wealth, the low level was the lower quartile ($50,000.00), the medium level was the median ($143,000.00), and the high level was the upper quartile ($352,000.00).
Results suggested that increasing wealth plays a protective role for NH Black adults and Hispanic adults. For low wealth, NH Black adults had almost twice the likelihood of belonging to the high versus the low trajectory class than NH White adults (OR = 1.942, 95% CI [1.312, 2.876], p < .01). For medium wealth, no significant differences were found. At high wealth, NH Black adults had substantially lower likelihood of belonging to the high versus the low trajectory class than NH White adults (OR = 0.193, 95% CI [0.041, 0.906], p < .05) (i.e., the racial health disparity seemed to reverse). At low wealth, Hispanic adults were about half as likely to belong to the high versus the low trajectory class (OR = 0.460, 95% CI [0.257, 0.822], p < .01). At medium wealth, Hispanic adults were even less likely to belong to the high versus the low trajectory class (OR = 0.387, 95% CI [0.220, 0.679], p < .01). At high wealth, Hispanic adults were substantially less likely to belong to the high versus the low trajectory class (OR = 0.263, 95% CI [0.090, 0.767], p < .05).
3.4. Attrition
A total of 6,382 respondents dropped out after the first wave or a later wave of the study. After 2006, an average of 1,276 respondents dropped out at each wave (Range: 1,062-1,529). Dropouts significantly differed from non-dropouts on several variables indicating greater risk factors: being older, having less wealth, and smoking (Appendix A). It is likely that if the dropouts remained in the study, more of the sample would be categorized into the increasing trajectory and/or the high trajectory rather than the low trajectory. It is unclear what impact an overall higher prevalence of membership in the less healthy classes would have on the associations between race/ethnicity, SES, and trajectory class, however. Our results above indicated that NH Black adults and those with lower SES would be more likely to belong to these unhealthy classes, so the differences between groups in their morbidity accumulation may have increased if the dropouts remained in the study. We present sensitivity analyses concerning attrition in the supplemental materials (Appendix B).
4. Discussion
4.1. Summary and interpretation
Findings suggest that trajectories of morbidity accumulation over an 18-year period in middle and later life fall into three distinct trajectories—those who begin with relatively few morbidities and accumulate additional morbidities slowly (low trajectory), those who begin with relatively few morbidities and accumulate rapidly (increasing trajectory), and those who begin with many morbidities and accumulate slowly (high trajectory). We found that NH Black adults and those with lower education were the most likely to belong to less healthy morbidity trajectories (e.g., high compared with low trajectory) while Hispanic adults were most likely to belong to the healthy morbidity trajectory (the low trajectory). This study extends prior work by investigating the interplay between SES and race/ethnicity. Our results suggest a protective effect of education for NH Black adults such that racial health disparities observed at low education were ameliorated and eliminated with increasing levels of education; In contrast, a reverse pattern emerged for Hispanic adults such that increasing levels of education dampened advantages observed at low education. Increasing levels of wealth were found to be beneficial across groups such that racial health disparities observed at lower levels of wealth were diminished and then reversed for NH Black adults while Hispanic health advantages observed at lower levels of wealth were further increased. When considering these findings, it is important to recognize that the slightly higher likelihood that NH Black adults belonged to healthier classes when SES is high should not be misconstrued as a health advantage overall. The fact that NH Black adults were far more likely to be predicted members of the high morbidity and increasing morbidity classes compared with NH White adults at average SES, suggests critical racial disparities overall instead.
4.2. Contributions
We analyzed data spanning nearly two decades utilizing a robust statistical approach. Therefore, our work builds upon findings from cross-sectional and shorter longitudinal studies. This study further contributes to the literature by using a multiple chronic condition approach that allows for a more holistic view of disease accumulation, which valuably complements research which commonly focuses on a single disease. Finally, our work explored interactions between race/ethnicity and SES factors on morbidity trajectories, which, to our knowledge, has not been previously explored.
There are important differences between our findings and those from other studies using growth mixture models to investigate morbidity trajectories. We identified three trajectories like some previous work (Wickrama et al., 2013) whereas other studies identified four (Lee et al., 2021; Tarraf et al., 2020). The discrepancies in the number of classes may be due to differences in the sample (e.g., age group, racial/ethnic composition), length of data collection [8 years (Wickrama et al., 2013) to 16 years (Tarraf et al., 2020)], and morbidity operationalization both in terms of the number of morbidities included [6 morbidities (Tarraf et al., 2020) to 9 morbidities (Lee et al., 2021)] as well as whether depression was included (Lee et al., 2021; Tarraf et al., 2020) or analyzed it separately (Wickrama et al., 2013). The variability in the morbidity operationalization reflects the methodological debate occurring in the larger research community (Suls et al., 2021). We include depressive symptoms because it poses a compound risk for a myriad of physical and psychological outcomes (Quiñones et al., 2018). Authors have cautioned against a tendency to over-extract classes in growth mixture models because several fit indices and class enumeration approaches result are known to result bias toward concluding too many classes (Bauer & Curran, 2003; Nylund-Gibson & Choi, 2018). The classes in our study are theoretically meaningful, sufficiently distinct, and representative of a reasonable proportion of the sample. We present sensitivity analyses conducted for the four-class model in the supplemental materials (Appendix C), which provide further discussion of our adoption of the three-class model.
Our findings help to clarify some of the ongoing debate about the relative importance of education and wealth in reducing health disparities (Lutz & Kebede, 2018). We found that increasing levels of wealth more consistently contributed to better health outcomes for racial/ethnic marginalized populations. Our examination of interactions between race/ethnicity and SES provides nuanced results that may help elucidate the conditions under which pertinent theories apply. Our findings about the increasing health advantages of having greater wealth and education for NH Black adults and greater wealth for Hispanic adults seems to be inconsistent with the diminishing returns hypothesis (Farmer & Ferraro, 2005) while the finding about Hispanic adults with greater education having lower health advantages seems consistent with it. Hispanic adults had the advantage of a lower initial risk of morbidity but no advantage in the rate of accumulation aligns with previous findings (e.g., Quiñones et al., 2019; Tarraf et al., 2020) and provides some support the Hispanic health paradox (Markides & Eschbach, 2005). Our findings suggest that SES variables interplay with Hispanic health advantages in distinct ways. We observed diminished advantages with greater education, but increased advantages with greater wealth. These seemingly counterintuitive results may have occurred because less education is associated with engaging in more physically demanding work [and thus greater regular physical activity, which is a factor associated with Hispanic-White health differences (Chung et al., 2009)]. Other plausible explanations include greater SES being associated with more exposure to discrimination for marginalized racial/ethnic groups [which can erode health (Colen et al., 2018)] and with greater access to healthcare (and thus a lower likelihood of underdiagnosis; Weissman et al., 1991). Indeed, one study found no evidence for the Hispanic health paradox when examining biological risk profiles (e.g., blood pressure) rather than doctor-affirmed, self-reported disease (Crimmins et al., 2007), suggesting underdiagnosed health problems. More research is needed to understand the complexities about the interplay of SES and racial/ethnic health differences in morbidity accumulation.
4.3. Limitations
Self-reported diagnoses were used to calculate the morbidity count, which may be subject to biases that threaten validity. However, the validity of morbidity self-reporting has been established (e.g., Skinner et al., 2005). More research is needed to better understand the impact of access to care and potential underdiagnosis on morbidity accumulation. There may be a ceiling effect for the high trajectory group because the small number of morbidities included in our count and their increased risk of mortality. Differential survival rates by race/ethnicity may potentially introduce biases (Whitfield et al., 2019). Consequently, our models may have survivor bias, although use of FIML analysis and inclusion in auxiliary factors associated with attrition would likely help mitigate such biases. Attrition in studies of older adults is often health-related, but inclusion of the morbidity measure for all cases at baseline for timepoints prior to dropout should serve as a rough proxy for later health status and improve the likelihood of meeting the MAR assumption conditionally (Little, 2008; Newsom, 2015).
4.4. Conclusion
We identified three distinct trajectories of morbidity accumulation in older American adults: low, increasing, and high. In covariate-adjusted models, we found racial/ethnic disparities suggesting disadvantages for NH Black adults (higher likelihood of belonging to the high rather than low trajectory class) and advantages for Hispanic adults (lower likelihood of belonging to the high rather than low trajectory class) relative to NH White adults. Education and wealth moderate associations between race/ethnicity and the likelihood of multimorbidity class membership. Specifically, increasing levels of education and wealth each displayed protective effects for NH Black adults. For Hispanic adults, health advantages seemed to diminish as education increased whereas health advantages became more pronounced as wealth increased. These findings have implications for reducing health disparities between NH Black and NH White adults through clinical and public health efforts. This work could inform the more precise targeting of public health interventions so that they can be delivered to those that would benefit most (e.g., NH Black adults with low level of education). Additionally, this work highlights the imperative to address SES inequalities that interact with race/ethnicity in complex ways to undermine health (Williams & Sternthal, 2010).
Funding
This work was supported by funding from the National Institute on Aging at the National Institutes of Health (grant numbers R01AG055681 and R01AG058545 to A. R. Quiñones).
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
CRediT authorship contribution statement
AnnaMarie S.O'Neill: Conceptualization, Methodology, Software, Formal analysis, Writing – original draft, Writing – review & editing, Visualization, Project administration. Jason T. Newsom: Conceptualization, Methodology, Software, Formal analysis, Writing – original draft, Writing – review & editing, Supervision. Em F. Trubits: Software, Formal analysis, Data curation, Writing – original draft, Writing – review & editing. Miriam R. Elman: Software, Data curation, Writing – original draft, Writing – review & editing. Anda Botoseneanu: Writing – original draft, Writing – review & editing. Heather G. Allore: Writing – original draft, Writing – review & editing. Corey L. Nagel: Writing – original draft, Writing – review & editing. David A. Dorr: Writing – original draft, Writing – review & editing. Ana R. Quiñones: Conceptualization, Resources, Writing – original draft, Writing – review & editing, Supervision, Funding acquisition.
Declaration of competing interest
We have no conflicts of interest or financial interests to report.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2023.101375.
Appendix. Supplementary data
The following is the Supplementary data to this article:
Data availability
We used publicly available data (link: https://hrs.isr.umich.edu/data-products). We can provide syntax code upon request.
References
- Aiken L.S., West S.G. Sage; 1991. Multiple regression: Testing and interpreting interactions. [Google Scholar]
- Ashworth M., Durbaba S., Whitney D., Crompton J., Wright M., Dodhia H. Journey to multimorbidity: Longitudinal analysis exploring cardiovascular risk factors and sociodemographic determinants in an urban setting. BMJ Open. 2019;9(12) doi: 10.1136/bmjopen-2019-031649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer D.J., Curran P.J. Distributional assumptions of growth mixture models: Implications for overextraction of latent trajectory classes. Psychological Methods. 2003;8(3):338–363. doi: 10.1037/1082-989X.8.3.338. [DOI] [PubMed] [Google Scholar]
- Bishop N.J., Haas S.A., Quiñones A.R. Cohort trends in the burden of multiple chronic conditions among aging US adults. The Journals of Gerontology: Series B. 2022;77(10):1867–1879. doi: 10.1093/geronb/gbac070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canizares M., Hogg-Johnson S., Gignac M.A., Glazier R.H., Badley E.M. Increasing trajectories of multimorbidity over time: Birth cohort differences and the role of changes in obesity and income. The Journals of Gerontology: Series B. 2018;73(7):1303–1314. doi: 10.1093/geronb/gbx004. [DOI] [PubMed] [Google Scholar]
- Caraballo C., Mahajan S., Massey D., Lu Y., Ndumele C.D., Drye E.E.…Krumholz H.M. 2021. Trends in racial and ethnic disparities in multimorbidity prevalence, 1999-2018.medRxiv. [DOI] [PubMed] [Google Scholar]
- Chung S., Domino M.E., Stearns S.C., Popkin B.M. Retirement and physical activity: Analyses by occupation and wealth. American Journal of Preventative Medicine. 2009;36(5):422–428. doi: 10.1016/j.amepre.2009.01.026. [DOI] [PubMed] [Google Scholar]
- Cigolle C.T., Nagel C.L., Blaum C.S., Liang J., Quiñones A.R. Inconsistency in the self-report of chronic diseases in panel surveys: Developing an adjudication method for the health and retirement study. The Journals of Gerontology: Series B. 2018;73(5):901–912. doi: 10.1093/geronb/gbw063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark C.R., Ommerborn M.J., A Coull B., Pham D.Q., Haas J.S. Income inequities and medicaid expansion are related to racial and ethnic disparities in delayed or forgone care due to cost. Medical Care. 2016;54(6):555–561. doi: 10.1097/MLR.0000000000000525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colen C.G., Ramey D.M., Cooksey E.C., Williams D.R. Racial disparities in health among nonpoor African Americans and Hispanics: The role of acute and chronic discrimination. Social Science & Medicine. 2018;199:167–180. doi: 10.1016/j.socscimed.2017.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins L.M., Lanza S.T. Vol. 718. John Wiley & Sons; 2010. (Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences). [Google Scholar]
- Collins L.M., Schafer J.L., Kam C.M. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychological Methods. 2001;6:330–351. doi: 10.1037/1082-989X.6.4.330. [DOI] [PubMed] [Google Scholar]
- Crimmins E.M., Kim J.K., Alley D.E., Karlamangla A., Seeman T. Hispanic paradox in biological risk profiles. American Journal of Public Health. 2007;97(7):1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer M.M., Ferraro K.F. Are racial disparities in health conditional on socioeconomic status? Social Science & Medicine. 2005;60(1):191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- Heeringa S.G., Connor J. Institute for Social Research, University of Michigan; Ann Arbor, Michigan: 1995. Technical description of the health and retirement study sample design. 1995. [DOI] [Google Scholar]
- Jaccard J. Interaction effects in logistic regression. SAGE Publications, Inc; 2001. Interactions between qualitative and quantitative/continuous predictors; pp. 31–41. [DOI] [Google Scholar]
- Jung T., Wickrama K.A.S. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2(1):302–317. doi: 10.1111/j.1751-9004.2007.00054.x. [DOI] [Google Scholar]
- Khullar D., Chokshi D.A. Health, income, & poverty: Where we are & what could help. Health Affairs, Health Policy Brief. 2018 doi: 10.1377/hpb20180817.901935. [DOI] [Google Scholar]
- LaVeist T.A. Disentangling race and socioeconomic status: A key to understanding health inequalities. Journal of Urban Health. 2005;82(3):iii26–iii34. doi: 10.1093/jurban/jti061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A., Joo S., Chai H.W., Jun H.J. Patterns of multimorbidity trajectories and their correlates among Korean older adults. Age and Ageing. 2021;50(4):1336–1341. doi: 10.1093/ageing/afab002. July 2021. [DOI] [PubMed] [Google Scholar]
- Little R.J. In: Longitudinal data analysis. Fitzmaurice G., Davidian M., Verbeke G., Molenberghs G., editors. Chapman & Hall/CRC Press; Boca Raton: 2008. Selection and pattern-mixture models; pp. 409–431. [Google Scholar]
- Lutz W., Kebede E. Education and health: Redrawing the preston curve. Population and Development Review. 2018;44(2):343–361. doi: 10.1111/padr.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides K.S., Eschbach K. Aging, migration, and mortality: Current status of research on the Hispanic paradox. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60(Special Issue 2):S68–S75. doi: 10.1093/geronb/60.Special_Issue_2.S68. [DOI] [PubMed] [Google Scholar]
- Marques A., Santos D.A., Peralta M., Sardinha L.B. Regular physical activity eliminates the harmful association of television watching with multimorbidity. A cross-sectional study from the European Social Survey. Preventive Medicine. 2018;109:28–33. doi: 10.1016/j.ypmed.2018.01.015. [DOI] [PubMed] [Google Scholar]
- Muthén L.K., Muthén B.O. 8th ed. Muthén & Muthén; Los Angeles, CA: 2018. Mplus user’s guide. [Google Scholar]
- Newsom J.T. Longitudinal structural equation modeling. Routledge; 2015. Missing data and attrition; pp. 368–406. [Google Scholar]
- Nylund-Gibson K., Choi A.Y. Ten frequently asked questions about latent class analysis. Translational Issues in Psychological Science. 2018;4(4):440–461. doi: 10.1037/tps0000176. [DOI] [Google Scholar]
- Nylund K.L., Asparouhov T., Muthén B.O. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(4):535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- Pathirana T.I., Jackson C.A. Socioeconomic status and multimorbidity: A systematic review and meta‐analysis. Australian & New Zealand Journal of Public Health. 2018;42(2):186–194. doi: 10.1111/1753-6405.12762. [DOI] [PubMed] [Google Scholar]
- Quiñones A.R., Botoseneanu A., Markwardt S., Nagel C.L., Newsom J.T., Dorr D.A., Allore H.G. Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLoS One. 2019;14(6) doi: 10.1371/journal.pone.0218462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quiñones A.R., Liang J., Bennett J.M., Xu X., Ye W. How does the trajectory of multimorbidity vary across Black, White, and Mexican Americans in middle and old age? Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2011;66(6):739–749. doi: 10.1093/geronb/gbr106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quiñones A.R., Markwardt S., Thielke S., Rostant O., Vásquez E., Botoseneanu A. Prospective disability in different combinations of somatic and mental multimorbidity. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2018;73(2):204–210. doi: 10.1093/gerona/glx100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychology and Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Schiøtz M.L., Høst D., Christensen M.B., Domínguez H., Hamid Y., Almind M.…Frølich A. Quality of care for people with multimorbidity–a case series. BMC Health Services Research. 2017;17(1):1–9. doi: 10.1186/s12913-017-2724-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner K.M., Miller D.R., Lincoln E., Lee A., Kazis L.E. Concordance between respondent self-reports and medical records for chronic conditions: Experience from the Veterans Health Study. The Journal of Ambulatory Care Management. 2005;28(2):102–110. doi: 10.1097/00004479-200504000-00002. [DOI] [PubMed] [Google Scholar]
- St Sauver J.L., Boyd C.M., Grossardt B.R., Bobo W.V., Rutten L.J.F., Roger V.L.…Rocca W.A. Risk of developing multimorbidity across all ages in an historical cohort study: Differences by sex and ethnicity. BMJ Open. 2015;5(2) doi: 10.1136/bmjopen-2014-006413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss V.Y., Jones P.W., Kadam U.T., Jordan K.P. Distinct trajectories of multimorbidity in primary care were identified using latent class growth analysis. Journal of Clinical Epidemiology. 2014;67(10):1163–1171. doi: 10.1016/j.jclinepi.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suls J., Bayliss E.A., Berry J., Bierman A.S., Chrischilles T., Farhat M., Young-Hyman C.N. Measuring multimorbidity. Medical Care. 2021;59(8):743–756. doi: 10.1097/MLR.0000000000001566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarraf W., Jensen G.A., Dillaway H.E., Vásquez P.M., González H.M. Trajectories of aging among US older adults: Mixed evidence for a hispanic paradox. The Journals of Gerontology: Series B. 2020;75(3):601–612. doi: 10.1093/geronb/gby057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turvey C.L., Wallace R.B., Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics. 1999;11(2):139–148. doi: 10.1017/S1041610299005694. [DOI] [PubMed] [Google Scholar]
- Violan C., Foguet-Boreu Q., Flores-Mateo G., Salisbury C., Blom J., Freitag M., Valderas J.M. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS One. 2014;9(7) doi: 10.1371/journal.pone.0102149. –e102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei M.Y., Mukamal K.J. Multimorbidity, mortality, and long-term physical functioning in 3 prospective cohorts of community-dwelling adults. American Journal of Epidemiology. 2018;187(1):103–112. doi: 10.1093/aje/kwx198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman J.S., Stern R., Fielding S.L., Epstein A.M. Delayed access to health care: Risk factors, reasons, and consequences. Annals of Internal Medicine. 1991;114(4):325–331. doi: 10.7326/0003-4819-114-4-325. [DOI] [PubMed] [Google Scholar]
- Whitfield K.E., Forrester S., Thorpe R.J., Jr. A comparison of variances in age cohorts to understand longevity in African Americans. The Journals of Gerontology: Series A. 2019;74(Supplement 1):S27–S31. doi: 10.1093/gerona/glz214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama K.K., Mancini J.A., Kwag K., Kwon J. Heterogeneity in multidimensional health trajectories of late old years and socioeconomic stratification: A latent trajectory class analysis. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2013;68:290–297. doi: 10.1093/geronb/gbs111. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Sternthal M. Understanding racial-ethnic disparities in health: Sociological contributions. Journal of Health and Social Behavior. 2010;51(Supplement 1):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K.H., Bentler P.M. Three likelihood-based methods for mean and covariance structure analysis with non-normal missing data. Sociological Methodology. 2000;30:165–200. doi: 10.1111/0081-1750.00078. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
We used publicly available data (link: https://hrs.isr.umich.edu/data-products). We can provide syntax code upon request.