Abstract
Nicolaou, Laura, Anne Steinberg, Rodrigo M. Carrillo-Larco, Stella Hartinger, Andres G. Lescano, and William Checkley. Living at high altitude and COVID-19 mortality in Peru. High Alt Med Biol. 23:146–158, 2022.
Background:
Previous studies have reported a lower severity of COVID-19 infections at higher altitudes; however, this association may be confounded by various factors. We examined the association between living at altitude and COVID-19 mortality in Peru adjusting for population density, prevalence of comorbidities, indicators of socioeconomic status, and health care access.
Methods:
Utilizing administrative data across 196 provinces located at varying altitudes (sea level to 4,373 m), we conducted a two-stage analysis of COVID-19 deaths between March 19 and December 31, 2020, Peru's first wave. We first calculated cumulative daily mortality rate for each province and fit lognormal cumulative distribution functions to estimate total mortality rate, and start, peak, and duration of the first wave. We then regressed province-level total mortality rate, start, peak, and duration of the first wave as a function of altitude adjusted for confounders.
Results:
There were 93,528 recorded deaths from COVID-19 (mean age 66.5 years, 64.5% male) for a cumulative mortality of 272.5 per 100,000 population between March 19 and December 31, 2020. We did not find a consistent monotonic trend between living at higher altitudes and estimated total mortality rate for provinces at 500 − 1,000 m (−12.1 deaths per 100,000 population per 100 m, 95% familywise confidence interval −27.7 to 3.5) or > 1,000 m (−0.3, −2.7 to 2.0). We also did not find consistent monotonic trends for the start, peak, and duration of the first wave beyond the first 500 m.
Conclusions:
Our findings suggest that living at high altitude may not confer a lower risk of death from COVID-19.
Keywords: high altitude, COVID-19, mortality
Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) was first reported in the Hubei region of China in December 2019 (Lu et al., 2020a) and has since spread globally, causing over 220 million cases of the disease known as COVID-19 and over 4.5 million deaths as of September 04, 2021 (Dong et al., 2020). As a disease that commonly manifests in respiratory distress and pneumonia (Huang et al., 2020), risk factors for severe outcomes include age (Zhang et al., 2020), comorbidities, poverty (Mena et al., 2021), air pollution (Zhu et al., 2020), and high-altitude environments (Quevedo-Ramirez et al., 2020; Arias-Reyes et al., 2021).
Studies have shown that SARS-CoV-2 infects the host cell by binding to the angiotensin-converting enzyme 2 (ACE2) receptor (Lu et al., 2020b; Ren et al., 2020). High-altitude environments result in hypobaric hypoxia and have been shown experimentally to lower ACE2 receptor levels (Hampl et al., 2015; Dang et al., 2020). A lower expression of ACE2 receptors may, in turn, result in a lower viral burden, lower likelihood of symptomatic infections, and lower transmission (Bourgonje et al., 2020). This leaves the possibility that populations living at high altitudes (>2,500 m) may have reduced susceptibility to SARS-CoV-2 and less severe outcomes.
An observational study in Peru early during the pandemic found that COVID-19 mortality decreased with higher altitude (Quevedo-Ramirez et al., 2020). Additionally, across the Americas, COVID-19 incidence and severity have been found to decrease significantly starting at 1,000 m above sea level (Arias-Reyes et al., 2021). Ecological data should be approached with caution, however, as findings are mixed (Woolcott and Bergman, 2020) and lower case rate and mortality could be confounded by factors such as population density, socioeconomic status, and availability or lack of access to health care services, particularly tertiary, specialized care (Burtscher et al., 2020; Pun et al., 2020). Peru is uniquely suited to study the association between COVID-19 mortality and high altitude given that it has communities that span from sea level to over 4,000 m. We sought to examine the association between altitude and COVID-19 mortality in Peru adjusting for population density and indicators of socioeconomic status and health care access.
Methods
Study setting
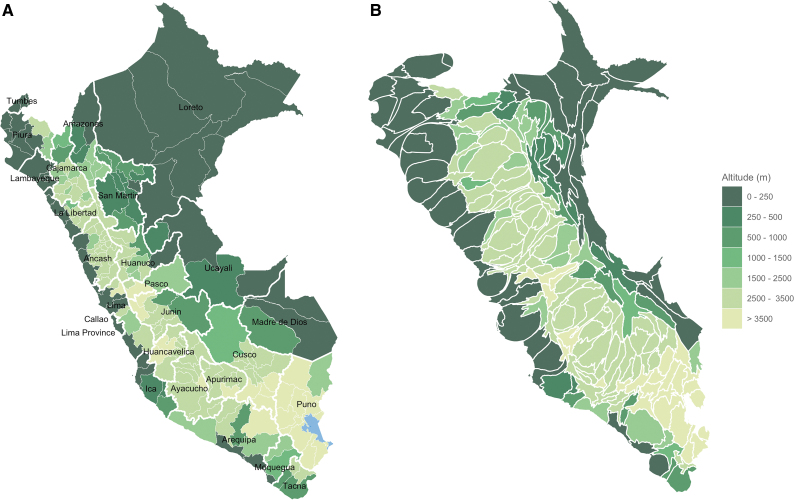
We conducted an analysis of administrative data in Peru between March 19 and December 31, 2020, roughly the first wave of the COVID-19 pandemic. Peru is divided into 24 departments and the Constitutional Province of Callao, which in turn are divided into 196 provinces (Fig. 1A). The country has a wide altitude range, with departments located between 9 and 4,373 m above sea level. Of the 25 departments (196 provinces), 12 (71 provinces) are at <1,000 m, 4 (29 provinces) are between 1,000 and 2,500 m, and 9 (96 provinces) are ≥2,500 m. Population density is highest in the coastal region, especially in Callao and Lima Province, and decreases with distance from the coast, from the highland region (Andes), which occupies the center of the country to the sparsely populated jungle regions (Amazon) in the east (Fig. 1B).
FIG. 1.
Altitude by province. (A) Map of departments (labeled) and provinces; (B) population density cartogram by province.
Data sources
We obtained sociodemographic and geographic data (population, population density, human development index [HDI], percent of population in total poverty, altitude) from Peru's National Center of Strategic Planning (CEPLAN for its acronym in Spanish), which aggregated data by department and by province from multiple sources. We used the population data for 2019, obtained from the National Registry of Identification and Civil Status (RENIEC, 2019). The HDI for 2019 was obtained from the United National Development Program (Yufra and Huerta, 2019). The HDI ranges between 0 and 1 and is composed of three main indicators for health (life expectancy at birth), education (percentage of the population over 18 years of age with secondary education and mean years of schooling), and standard of living (household income per capita). The percentage of population in total poverty and altitude was obtained from the National Institute of Statistics and Information (INEI) using data from 2019 at department level (INEI, 2020a) and from 2018 at province level (INEI, 2020b). Department and province altitudes correspond to the altitude of the department and province capitals, respectively.
The prevalence of overweight (body mass index [BMI] >1 standard deviation above the median for children 15–17 years of age, ≥25 kg/m2 in adults 18–59 years of age, and BMI ≥28 kg/m2 in adults ≥60 years of age, and excluded pregnant women) and the percentage of current smokers ≥15 years of age were available at department level only and were obtained from INEI for 2019 (INEI, 2019). The percentage of current smokers was determined as the proportion of the population ≥15 years who smoked at least one cigarette in the last 30 days.
We computed the percentage of population over 60 years of age using the 2019 modeled population based on 2017 census data (Ministerio de Salud, 2019); and the mean persons per room as a measure of crowding using the average number of persons per household by the average number of rooms per household from 2017 census data (INEI, 2017). We determined total number of hospital beds and adult intensive care unit (ICU) ventilators by department and by province from daily data provided by the National Superintendence of Health of the Peruvian Ministry of Health (SUSALUD for its acronym in Spanish) for all health facilities in Peru since April 8, 2020 (Plataforma Nacional de Datos Abiertos, 2021a). Since the reported number of beds and ventilators in many of the health facilities varied during this time period as they expanded their capacity to manage the increase in hospitalizations due to COVID-19, we computed total numbers at each health facility based on the modes.
Outcomes
We obtained death counts from the daily registry of COVID-19 deaths published by the Peruvian Ministry of Health (MINSA for its acronym in Spanish) (Plataforma Nacional de Datos Abiertos, 2021b). The criteria used to define COVID-19 as the cause of death are listed in the Supplementary Data S1. We used data between March 19 and December 31, 2020, and aggregated deaths by day at both department and province. We excluded the 20 deaths that were registered before March 19, 2020, the date of the first confirmed death due to COVID-19 in Peru (Plataforma Digital Única del Estado Peruano, 2020). Daily mortality rate (DMR) was computed as the daily number of deaths per 100,000 inhabitants. Cumulative daily mortality rate (CDMR) was determined as the total number of deaths up to and including that day, per 100,000 inhabitants. We used regression models outlined below to fit these data and estimate our four primary outcomes: total mortality rate, and start, end, and peak of the first wave of COVID-19 deaths. We hypothesized that altitude does not only reduce total mortality but may also result in a lower peak of deaths, later start, and shorter duration of the wave.
Biostatistical methods
We conducted our analysis in two stages. First, we modeled CDMR by department and by province as a lognormal cumulative distribution function with three parameters (A, , and ):
where t is time in calendar days, A represents the total mortality rate, and and are the mean and standard deviation of the DMR, respectively, both on the log scale. We fitted this distribution using nonlinear least-squares to estimate model parameters. We estimated parameters separately for each of the 196 provinces and 25 departments. From these parameters we then estimated the days at which the start, end, and peak of deaths occurred. Peak of deaths was calculated as . The start and end of the first wave were approximated by the 2.5th and 97.5th percentiles, respectively: , , and the duration of the first wave was computed as the time between these two values, .
Provinces where the difference between estimated and observed total mortality rate was more than 50% (n = 11) were merged with the neighboring province with the most similar altitude within the same department (Huacaybamba with Marañon, Antonio Raymondi with Huari, Asunción with Carlos F. Fitzcarrald, San Pablo with San Miguel, Bolivar with Pataz, Castrovirreyna with Huancavelica, Chincheros with Andahuaylas, Condesuyos with La Unión, Huamalies with Dos de Mayo, Paucar del Sara Sara with Parinacochas, Santa Cruz with Chota) and a new fit was obtained for the CDMR across the two provinces.
In a second stage, we used linear regression models for the total mortality rate, start, peak, and duration of the first wave as a function of altitude separately for all provinces/merged provinces (n = 192) adjusted for the following a priori selected confounders: log-transformed population, log-transformed population density, HDI, percent of the population in total poverty, mean number of people per room, prevalence of overweight >15 years of age by department, percent of current smokers >15 years by department, percent of the population >60 years of age, total number of hospital beds per 100,000 inhabitants, and total number of adult ICU ventilators per 100,000 inhabitants. For the merged provinces, we used the mean altitude between the two provinces and population-weighted averages for the HDI, percent of the population in total poverty, mean number of people per room, and percent >60 years. We assumed equal weights for all provinces/merged provinces.
We generated two models for each of our four outcomes: one with altitude included as a piecewise linear spline with knots at 500 and 1,000 m, and another with altitude categorized into the following bins: 0–250 m, 250–500 m, 500–1,000 m, 1,000–1,500 m, 1,500–2,500 m, 2,500–3,500 m, and >3,500 m. We calculated Bonferroni-adjusted p-values and 95% familywise confidence intervals (CIs) given that our four primary outcomes are interrelated. To verify the robustness of our results against outliers, we performed two sensitivity analyses. First, we used rank-based regression (Hettmansperger and McKean, 2011) to model our four outcomes as a function of altitude adjusting for the same potential confounders. Second, we used linear regression but excluded the 50 provinces where CDMR did not fully plateau in 2020, and our model predicted the end of the first wave beyond the end of 2020 (Supplementary Fig. S1). All statistical analyses were conducted in R28. The analyses were approved by the Institutional Review Board of Universidad Peruana Cayetano Heredia (SIDISI code 205876).
Results
Regional characteristics
We summarize the cumulative mortality rate in 2020 and the date of the first recorded death due to COVID-19 along with sociodemographic variables and health risk factors in the 25 departments (Table 1). The number of COVID-19 deaths per 100,000 population in 2020 ranged from 82.6 in Apurimac to 392.8 in Callao, the dates of the first death ranged between March 19, 2020 (Lima) and April 25, 2020 (Madre de Dios). Population density varied from 2 inhabitants per km2 in Madre de Dios to 7,859 inhabitants per km2 in Callao. The HDI was highest in Lima (0.71), Moquegua (0.66), Callao (0.64), and Arequipa (0.64), and lowest in Huancavelica (0.38), Apurimac (0.41), and Amazonas (0.42). Prevalence of overweight in individuals >15 years of age ranged from 30.6% (Huancavelica) to 40.9% (Moquegua), smoking prevalence from 5.6% (Puno) to 19.1% (Madre de Dios), and percent of population >60 years from 6.5% (Madre de Dios) to 12.5% (Moquegua). The total number of beds per 100,000 population varied between 29.9 (Tumbes) and 125.6 (Callao) and number of adult ICU ventilators per 100,000 population ranged from 0.0 (Moquegua) to 5.2 (Pasco).
Table 1.
COVID-19 Mortality and Related Covariates by Department Ordered by Ascending Altitude
| Department | Number of provinces | COVID-19 deaths in 2020 | COVID-19 deaths per 100,000 inhabitants | First COVID-19 death (mm-dd) | Altitude (m) | Population | Population density per km2 | HDI | Poverty (%) | Persons per room | Population over 60 years old (%) | Overweight (%) | Smokers (%) | Hospital beds per 100,000 inhabitants | Adult ICU ventilators per 100,000 inhabitants |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tumbes | 3 | 766 | 309.1 | 03–30 | 9 | 247,778 | 53.07 | 0.56 | 13.3 | 1.30 | 8.7 | 40.1 | 13.1 | 29.87 | 1.61 |
| Callao | 1 | 5,214 | 454.7 | 03–22 | 27 | 1,146,773 | 7,859.45 | 0.64 | 13.3 | 1.52 | 12.3 | 39.3 | 18.4 | 125.57 | 2.09 |
| Lambayeque | 3 | 4,626 | 332.7 | 03–19 | 28 | 1,390,570 | 96.16 | 0.53 | 13.3 | 1.20 | 11.9 | 36.2 | 8.0 | 54.80 | 1.51 |
| Piura | 8 | 6,325 | 305.8 | 03–21 | 57 | 2,068,288 | 58.01 | 0.51 | 23.6 | 1.32 | 10.0 | 39.4 | 7.3 | 41.05 | 1.21 |
| La Libertad | 12 | 4,870 | 237.7 | 03–24 | 74 | 2,049,071 | 80.37 | 0.55 | 23.6 | 1.11 | 10.7 | 39.5 | 7.6 | 61.20 | 1.07 |
| Loreto | 8 | 2,740 | 236.9 | 03–20 | 107 | 1,156,517 | 3.14 | 0.48 | 30.5 | 1.73 | 7.7 | 33.7 | 13.5 | 43.75 | 1.21 |
| Lima | 10 | 42,145 | 374.8 | 03–19 | 162 | 11,245,182 | 322.92 | 0.71 | 13.3 | 1.13 | 12.0 | 39.3 | 12.5 | 103.38 | 1.90 |
| Ucayali | 4 | 1,577 | 252.6 | 03–21 | 162 | 624,257 | 6.11 | 0.48 | 13.3 | 1.63 | 8.9 | 36.1 | 14.4 | 40.05 | 1.92 |
| Madre De Dios | 3 | 452 | 256.9 | 03–23 | 204 | 175,969 | 2.06 | 0.61 | 13.3 | 1.35 | 6.5 | 39.5 | 19.1 | 55.12 | 2.84 |
| Ica | 5 | 3,690 | 395.5 | 03–28 | 432 | 932,965 | 43.79 | 0.60 | 2.6 | 1.21 | 11.6 | 35.2 | 9.7 | 72.24 | 1.29 |
| Tacna | 4 | 798 | 210.5 | 04–01 | 583 | 379,129 | 23.58 | 0.59 | 13.3 | 1.04 | 10.0 | 37.2 | 7.3 | 84.40 | 1.85 |
| San Martin | 10 | 1,575 | 164.4 | 03–30 | 895 | 957,992 | 18.67 | 0.48 | 23.6 | 1.43 | 8.2 | 36.5 | 10.8 | 47.08 | 0.84 |
| Moquegua | 3 | 883 | 447.4 | 04–24 | 1,428 | 197,367 | 12.54 | 0.66 | 13.3 | 1.04 | 12.5 | 40.9 | 9.6 | 121.09 | 0.00 |
| Huanuco | 11 | 1,078 | 125.2 | 04–05 | 1,921 | 861,293 | 23.11 | 0.45 | 30.5 | 1.28 | 9.1 | 34.5 | 9.7 | 35.99 | 1.04 |
| Amazonas | 7 | 573 | 121.2 | 04–05 | 2,338 | 472,870 | 12.05 | 0.42 | 30.5 | 1.45 | 8.8 | 36.8 | 9.2 | 52.45 | 0.21 |
| Arequipa | 8 | 4,257 | 274.1 | 03–29 | 2,429 | 1,553,291 | 24.52 | 0.64 | 13.3 | 1.02 | 12.3 | 39.7 | 10.8 | 88.97 | 2.45 |
| Apurimac | 7 | 360 | 78.9 | 04–06 | 2,500 | 456,233 | 21.83 | 0.41 | 30.5 | 1.17 | 9.3 | 33.8 | 6.1 | 81.98 | 2.41 |
| Cajamarca | 13 | 1,608 | 100.4 | 04–01 | 2,731 | 1,600,862 | 48.07 | 0.43 | 36.8 | 1.37 | 9.2 | 34.4 | 5.8 | 35.79 | 0.69 |
| Ayacucho | 11 | 834 | 121.2 | 04–08 | 2,797 | 688,137 | 15.71 | 0.43 | 36.8 | 1.24 | 8.2 | 36.4 | 9.2 | 94.02 | 1.31 |
| Ancash | 20 | 2,885 | 231.3 | 03–24 | 3,073 | 1,247,193 | 34.76 | 0.52 | 13.3 | 1.11 | 11.0 | 39.0 | 7.3 | 65.59 | 0.88 |
| Junin | 9 | 2,414 | 171.8 | 03–30 | 3,294 | 1,405,124 | 31.70 | 0.51 | 23.6 | 1.21 | 9.7 | 35.1 | 11.8 | 79.57 | 2.06 |
| Cusco | 13 | 1,595 | 109.5 | 03–24 | 3,439 | 1,456,231 | 20.23 | 0.51 | 23.6 | 1.13 | 10.6 | 34.9 | 8.0 | 91.88 | 1.92 |
| Huancavelica | 7 | 391 | 90.0 | 04–09 | 3,746 | 434,592 | 19.64 | 0.38 | 36.8 | 1.18 | 7.0 | 30.6 | 7.3 | 51.08 | 0.69 |
| Puno | 13 | 1,533 | 119.8 | 03–24 | 3,848 | 1,279,979 | 19.11 | 0.47 | 36.8 | 1.11 | 9.7 | 33.6 | 5.6 | 58.83 | 1.17 |
| Pasco | 3 | 339 | 116.3 | 04–08 | 4,373 | 291,509 | 11.65 | 0.48 | 30.5 | 1.22 | 7.8 | 36.4 | 11.1 | 68.61 | 5.15 |
HDI, human development index; ICU, intensive care unit.
The percentage of population in poverty increased with altitude, while prevalence of overweight, smoking prevalence, and percentage of the population >60 years was lower at higher altitudes. Excluding Lima and Callao, the number of people living in each department was similar. Population density, on the other hand, was lower at higher altitudes.
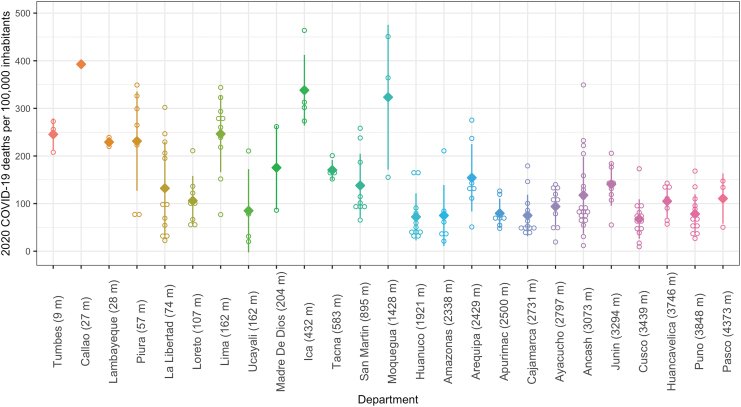
COVID-19 mortality by department and by province
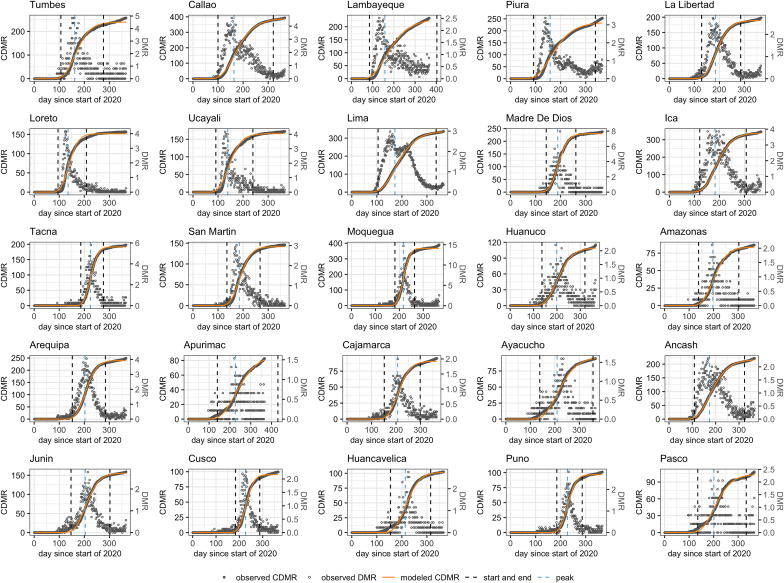
We display observed CDMR for COVID-19 per 100,000 population in 2020 for all provinces and the mean and standard deviation by department ordered by ascending altitude (Fig. 2). Mean CDMR is highest in Callao (27 m), Ica (432 m), and Moquegua (1,428 m), and lowest in Cusco (3,439 m), Huanuco (1,921 m), and Cajamarca (2,731 m). There does not appear to be a consistent monotonic trend in CDMR means by altitude, especially when the department with the highest population density (Callao) is ignored. In Figure 3, we show the observed CDMR and DMR by department along with the modeled CDMR and the predicted start, end, and peak of the first wave. There is excellent agreement between observed and modeled CDMRs. Our predictions of the peak of deaths and the start and end of the first wave, computed from the model parameters, also show good agreement with the observed data.
FIG. 2.
2020 total COVID-19 deaths per 100,000 inhabitants in all provinces and mean and standard deviation by department ordered by ascending altitude.
FIG. 3.
CDMR and DMR by department showing predicted start, end and peak of first wave, and sorted by altitude. CDMR, cumulative daily mortality rate; DMR, daily mortality rate.
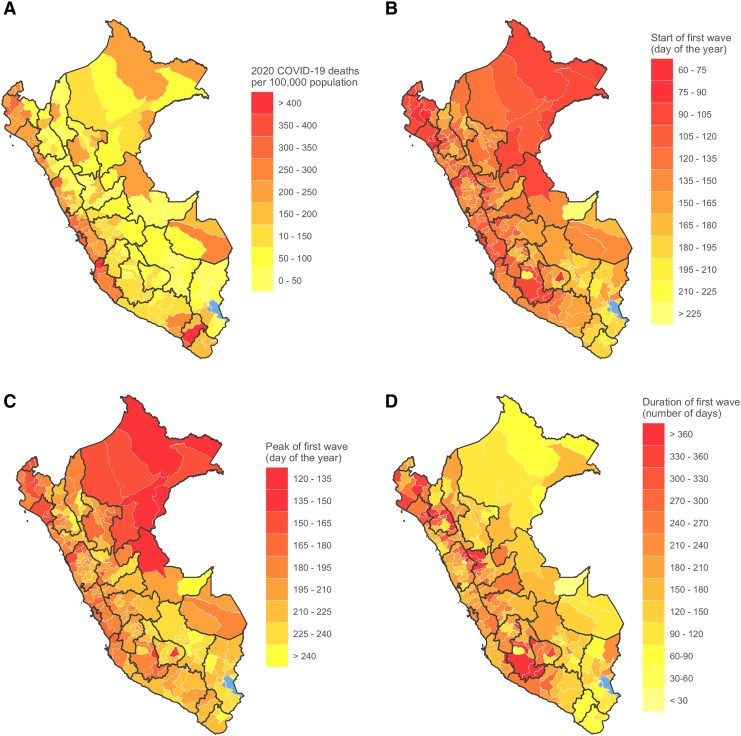
We display maps of the total mortality rate, and the start, peak, and duration of the first wave by province in Figure 4. Mortality rates were highest in provinces along the northern (Tumbes, Piura, Lambayeque) and central (La Libertad, Ancash, Lima, Callao) coast, and in the capital provinces of Amazon Basin regions near the borders with Colombia to the northeast (Maynas in Loreto), Brazil to the east (Coronel Portillo in Ucayali), and Bolivia to the southeast (Tambopata in Madre de Dios) (Fig. 4A). The start of the first wave presented in Figure 4B suggests how COVID-19 could have spread through the major ports of entry and the borders with neighboring countries in the north and east (Ecuador, Colombia and Brazil), with the first wave starting first in provinces in Lima, Tumbes, Loreto, and Ucayali. Peak mortality rate occurred earliest in the northeast Amazon region (provinces in Loreto, and neighboring province Coronel Portillo in Ucayali), in two of the least populated departments in the country (Fig. 4C). The low population density is a likely contributing factor to the shorter duration of the first wave in these regions (Fig. 4D), as there is evidence to suggest that contact rates are associated with population density.
FIG. 4.
Maps by province: (A) 2020 COVID-19 deaths per 100,000 population; (B) start of first wave; (C) peak of first wave; (D) duration of first wave.
Associations between COVID-19 mortality and altitude
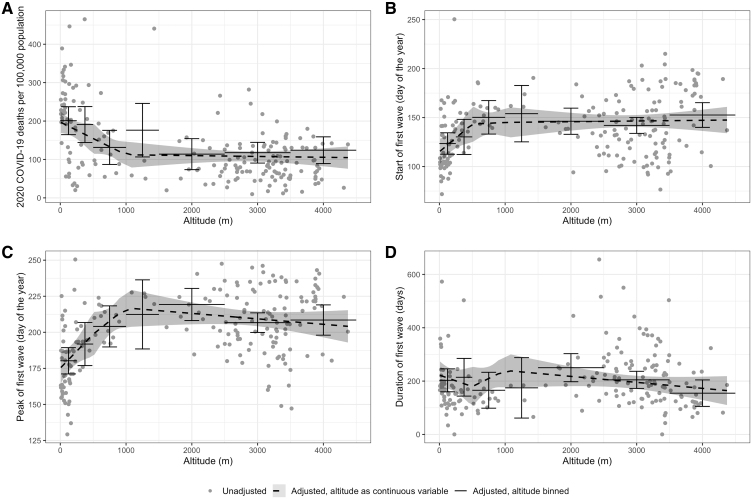
We plot the total mortality rate, and the start, peak, and duration of the first wave as a function of altitude in Figure 5. The results include both the unadjusted estimates obtained from our CDMR models by province, and the adjusted estimates from our linear regression models with altitude as a continuous variable and with altitude discretized into bins. Both adjusted models show that there is no consistent association between altitude and any of our outcomes beyond the first 500 m. There is a change of −12.1 deaths per 100,000 population per 100 m (95% familywise CI −27.7 to 3.5) between 500 and 1,000 m, and −0.3 (95% familywise CI −2.7 to 2.0) above 1,000 m. The start of the first wave appears to increase by 1.3 days per 100 m (95% familywise CI −4.0 to 6.6) between 500 and 1,000 m, and remains the same above 1,000 m (change of 0.1 days per 100 m; 95% familywise CI −0.9 to 0.7), while the peak increases by 5.9 days per 100 m between 500 and 1,000 m (95% familywise CI 1.4 to 10.4) but decreases by 0.7 days per 100 m above 1,000 m (95% familywise CI −1.3 to 0.0).
FIG. 5.
Variables as a function of altitude: (A) 2020 COVID-19 deaths per 100,000 population; (B) start of first wave; (C) peak of first wave; (D) duration of first wave. Multivariable adjusted models showing mean and 95% familywise CIs. CI, confidence interval.
Similarly, there is no significant trend with altitude for the duration of the wave between 500–1,000 m (change of 15.2 days per 100 m, 95% familywise CI −9.5 to 40.0) and >1,000 m (−1.8 days per 100 m, 95% familywise CI −5.5 to 2.0). In Table 2, we summarize the mean differences in CDMR, start, peak, and duration of the first wave across altitude bins. The results show that CDMRs are lower above 500 m when compared with CDMRs below 500 m. However, this trend is not consistently linear with altitude. Above 500 m, all comparisons of CDMR are not significant. Likewise, there are no significant differences in the start, peak, or duration of the first wave across any altitude bins above 500 m. Altogether, these findings suggest that high altitude does not offer a protective effect against COVID-19 mortality.
Table 2.
Differences in Cumulative Daily Mortality Rate, Start, Peak, and Duration of First Wave Across Altitude Bins
| Lower altitude | Higher altitude | CDMR |
Start |
Peak |
Duration |
||||
|---|---|---|---|---|---|---|---|---|---|
| Mean difference (95% familywise CI) | p | Mean difference (95% familywise CI) | p | Mean difference (95% familywise CI) | p | Mean difference (95% familywise CI) | p | ||
| 0–250 m | 250–500 m | −21.4 (−76.9 to 34.1) | 1 | 9.7 (−9.8 to 29.2) | 0.8 | 10.1 (−6.5 to 26.7) | 0.51 | −22.0 (−111.8 to 67.8) | 1 |
| 0–250 m | 500–1,000 m | −95.9 (−147.3 to −44.4) | <0.001 | 21.8 (3.7 to 39.9) | 0.01 | 24.5 (9.1 to 39.9) | <0.001 | −16.0 (−99.2 to 67.3) | 1 |
| 0–250 m | 1,000–1,500 m | −41.6 (−128.0 to 44.8) | 0.90 | 36.2 (5.9 to 66.5) | 0.01 | 37.3 (11.4 to 63.2) | <0.01 | −36.3 (−176.1 to 103.4) | 1 |
| 0–250 m | 1,500–2,500 m | −126.6 (−177.4 to −75.8) | <0.001 | 23.0 (5.2 to 40.8) | <0.01 | 42.9 (27.7 to 58.1) | <0.001 | 44.3 (−37.9 to 126.4) | 0.70 |
| 0–250 m | 2,500–3,500 m | −120.6 (−166.2 to −75.0) | <0.001 | 22.7 (6.7 to 38.7) | <0.01 | 34.1 (20.4 to 47.7) | <0.001 | 12.0 (−61.8 to 85.8) | 1 |
| 0–250 m | >3,500 m | −117.0 (−169.6 to −64.3) | <0.001 | 25.8 (7.3 to 44.3) | <0.01 | 27.2 (11.4 to 43.0) | <0.001 | −15.8 (−101.0 to 69.5) | 1 |
| 250–500 m | 500–1,000 m | −74.5 (−140.4 to −8.5) | 0.02 | 12.1 (−11.0 to 35.3) | 0.75 | 14.4 (−5.3 to 34.2) | 0.27 | 6.0 (−100.7 to 112.8) | 1 |
| 250–500 m | 1,000–1,500 m | −20.2 (−116.8 to 76.4) | 1 | 26.5 (−7.4 to 60.4) | 0.20 | 27.2 (−1.7 to 56.2) | 0.07 | −14.3 (−170.7 to 142.0) | 1 |
| 250–500 m | 1,500–2,500 m | −105.2 (−170.6 to −39.8) | <0.001 | 13.3 (−9.7 to 36.3) | 0.58 | 32.8 (13.2 to 52.4) | <0.01 | 66.3 (−39.6 to 172.1) | 0.46 |
| 250–500 m | 2,500–3,500 m | −99.2 (−158.8 to −39.6) | <0.001 | 13.0 (−7.9 to 34.0) | 0.47 | 24.0 (6.1 to 41.9) | <0.01 | 34.9 (−62.5 to 130.5) | 1 |
| 250–500 m | >3,500 m | −95.6 (−160.9 to −30.3) | <0.01 | 16.1 (−6.8 to 39.0) | 0.31 | 17.1 (−2.4 to 36.7) | 0.11 | 6.2 (−99.4 to 111.9) | 1 |
| 500–1,000 m | 1,000–1,500 m | 54.3 (−39.4 to 148.0) | 0.58 | 14.4 (−18.5 to 47.2) | 1 | 12.8 (−15.3 to 40.8) | 1 | −20.4 (−172.0 to 131.2) | 1 |
| 500–1,000 m | 1,500–2,500 m | −30.7 (−94.3 to 32.9) | 0.90 | 1.2 (−21.1 to 23.5) | 1 | 18.4 (−0.7 to 37.4) | 0.06 | 60.2 (−42.7 to 163.1) | 0.57 |
| 500–1,000 m | 2,500–3,500 m | −24.7 (−83.9 to 34.5) | 1 | 0.9 (−19.9 to 21.7) | 1 | 9.6 (−8.2 to 27.3) | 0.70 | 27.9 (−67.9 to 123.8) | 1 |
| 500–1,000 m | >3,500 m | −21.1 (−84.0 to 41.8) | 1 | 4.0 (−18.1 to 26.0) | 1 | 2.7 (−16.2 to 21.5) | 1 | 0.2 (−101.6 to 102.0) | 1 |
| 1,000–1,500 m | 1,500–2,500 m | −85.0 (−175.1 to 5.1) | 0.07 | −13.2 (−44.8 to 18.4) | 1 | 5.6 (−21.4 to 32.6) | 1 | 80.6 (−65.1 to 226.4) | 0.66 |
| 1,000–1,500 m | 2,500–3,500 m | −79.0 (−165.1 to 7.1) | 0.09 | −13.4 (−43.7 to 16.8) | 1 | −3.2 (−29.0 to 22.6) | 1 | 48.3 (−91.0 to 187.7) | 1 |
| 1,000–1,500 m | >3,500 m | −75.4 (−164.6 to 13.8) | 0.14 | −10.4 (−41.7 to 20.9) | 1 | −10.1 (−36.8 to 16.6) | 1 | 20.6 (−123.7 to 164.9) | 1 |
| 1,500–2,500 m | 2,500–3,500 m | 6.0 (−39.1 to 51.1) | 1 | −0.3 (−16.1 to 15.6) | 1 | −8.8 (−22.3 to 4.7) | 0.41 | −32.3 (−105.2 to 40.7) | 1 |
| 1,500–2,500 m | >3,500 m | 9.6 (−43.1 to 62.3) | 1 | 2.8 (−15.7 to 21.3) | 1 | −15.7 (−31.5 to 0.1) | 0.05 | −60.0 (−145.3 to 25.2) | 0.31 |
| 2,500–3,500 m | >3,500 m | 3.6 (−36.8 to 44.1) | 1 | 3.0 (−11.2 to 17.2) | 1 | −6.9 (−19.0 to 5.3) | 0.62 | −27.7 (−93.2 to 37.7) | 1 |
CDMR, cumulative daily mortality rate; CI, confidence interval.
Sensitivity analyses
We show the results from both sensitivity analyses in Supplementary Figures S2 and S3, and summarize mean changes and 95% familywise CIs for our four outcomes in Supplementary Table S1. Except for the change in the peak of the first wave between 500 and 1,000 m (change of 5.2 deaths per 100,000 population per 100 m; 95% familywise CI 1.0–9.5) when using rank-based regression, all other results from both analyses are consistent with those from the main analysis and show no evidence of a monotonic trend with altitude beyond 500 m.
Discussion
In this analysis of administrative data of COVID-19 deaths in Peru for 2020, we did not observe a consistent monotonic trend in mortality with altitude. Specifically, we did not find significant differences with altitude in the CDMRs or the start, peak, or duration of the first wave of COVID-19 deaths above 500 m. The monotonic trends observed between sea level and 500 m are likely due to residual confounding, given that there is no evidence of an association with altitude above 500 m. Since Peru has provinces at altitudes ranging from sea level to 4,373 m and an overall high COVID-19 mortality rate, our analysis provides compelling evidence that living at higher altitudes does not offer a protective effect against death from COVID-19.
Evidence for a relationship between COVID-19 mortality outcomes and altitude remains mixed (Burtscher et al., 2020; Cano-Pérez et al., 2020; Pun et al., 2020; Seclén et al., 2020; Segovia-Juarez et al., 2020; Woolcott and Bergman, 2020; Arias-Reyes et al., 2021; Stephens et al., 2021; Thomson et al., 2021). One potential explanation for heterogeneity in findings is that some of the analyses used early COVID-19 mortality data before the end of the first wave. Two analyses of mortality data in Peru between March and July 2020 found a lower rate of deaths at higher altitudes when analyzed at the department (Seclén et al., 2020) and district levels (Thomson et al., 2021). However, there are some potential shortcomings with these analyses. First, they included data for a short period of time and missed the bulk of data from the first wave in many departments. Therefore, these analyses may suffer from a period time bias. Our analysis identified that the peak of deaths did not occur until after July 2020 in many provinces, especially those located at a high altitude. Second, neither Seclén et al. nor Thomson et al. used time-series analyses, which are the best methodological approach to account for temporal trends.
Finally, Seclén et al. only adjusted for age and sex and did not account for other important potential confounders such as population density, socioeconomic status, and availability of health services. In contrast, another analysis of data in Peru between March and June 2020 found that while COVID-19 infection rates were lower with altitude, case fatality rate was not affected (Segovia-Juarez et al., 2020). This analysis did not account for potential confounders other that sex. Another study utilizing administrative data from 70 municipalities in Colombia, another Andean country with a similar range of altitudes as Peru, also found lower unadjusted death rates with altitude; however, this study also used data early in the pandemic between March and July 2020 and authors reported that their findings were better explained by population density (Cano-Pérez et al., 2020). A subsequent analysis of mortality data in the United States between January and August 2020 also found a similar relationship of lower death rates with higher altitude comparing counties with an average elevation greater than 2,133 m against counties with an average elevation less than 914 m in a matched death count analysis (Stephens et al., 2021).
While the authors adjusted for potential confounders, including degree of urbanization and number of persons per household, they did not include population density or access to health services by country. This study also suffers from the same limitations as the previous studies in Peru in that 19 states had not yet completed the first wave by August 2020 (James and Menzies, 2020). In contrast, another analysis utilizing administrative data in the United States between January and April 2020 found the opposite effect: counties located at 2,000 m or above had higher mortality rates than those located below 1,500 m (Woolcott and Bergman, 2020). The same authors also analyzed data from Mexico between March and May 2020 and found that mortality rate was also higher with altitude. These analyses also identified that the association between altitude and COVID-19 mortality rates was significant only in men and those younger than 65 years of age.
The evidence of an association between altitude and COVID-19 mortality remains mixed with some studies suggesting a positive correlation, others a negative correlation, and a handful reporting null results. Our work expands on this body of research, by covering a longer period of time, accounting for several confounders and examining not only the association of altitude with cumulative mortality rate, but also the start, peak, and duration of the first wave.
The geographical distribution of the start of the COVID-19 epidemic in Peru follows a similar pattern to previous pandemics such as that of cholera in 1991 (Smirnova et al., 2020) and H1N1 influenza in 2009 (Chowell et al., 2011). Specifically, the onset of COVID-19 deaths happened earliest primarily in the main ports of entry, such as Lima and Callao, and the northern borders of Tumbes, Piura, and Loreto. One salient difference with other epidemics, however, was the high CDMR observed in Moquegua, specifically in the Provinces of Ilo and Mariscal Nieto. Since 2011, the city of Ilo has become the terminus for the Interoceanic Highway, a 2,600 km passageway that connects provinces in Moquegua with departments in southeastern Peru and with Brazil. Increased trade and travel through the Interoceanic Highway may explain the high mortality rates in this region.
Our analysis has several strengths. First, the range of altitudes in Peruvian provinces from sea level to 4,337 m provides a natural experiment to study the association between altitude and COVID-19 mortality. There are few countries in the world that have high population density at an altitude. Indeed, 23% of the population of Peru lives at altitudes ≥2,500 m, only second to Bolivia and Ecuador (Tremblay and Ainslie, 2021). In contrast, <1% of the population in the United States lives at ≥2,000 m above sea level (Woolcott and Bergman, 2020). Second, we utilized time series models to characterize not only total mortality rates but also the start, peak, and duration of the first wave of COVID-19 by province. Such modeling approach allowed us to provide a comprehensive characterization of the relationship between COVID-19 mortality outcomes and altitude. Third, we utilized data for all of 2020 and most provinces (∼75%) had already experienced the end of the first wave.
Our analyses also have some potential shortcomings. First, we utilized administrative data, which can be affected by underreporting especially in lower resource areas. However, deaths are less prone to underreporting and unlike cases, do not depend on availability of COVID-19 testing. Second, we cannot exclude confounding. We utilized data on potential confounders available at the province or department level, but it is possible that our adjusted analyses did not comprehensively capture all potential confounders and there may still be residual confounding when using province- or department-level averages. For example, we assigned the altitude of the province capital to the entire province; however, we acknowledge that altitudes may vary widely even within a province (e.g., altitudes by district in Arequipa province range from 9 to 4,470 m).
While district data were available, many districts had sparse time series of death data that complicated analysis. Finally, we cannot rule out that this study may suffer from ecological fallacy as it utilized population-level data. Therefore, a well-designed cohort study that includes individual-level data may be the best epidemiological design to ultimately address whether altitude confers protection against mortality from COVID-19 infection.
In conclusion, our analyses do not provide evidence of a relationship between living at higher altitudes and lower risk of death from COVID-19.
Supplementary Material
Author Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Supplementary Material
References
- Arias-Reyes C, Carvajal-Rodriguez F, Poma-Machicao L, Aliaga-Raduán F, Marques DA, Zubieta-DeUrioste N, Accinelli RA, Schneider-Gasser EM, Zubieta-Calleja G, Dutschmann M, and Soliz J. (2021). Decreased incidence, virus transmission capacity, and severity of COVID-19 at altitude on the American continent. PLoS One 16:e0237294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgonje AR, Abdulle AE, Timens W, Hillebrands J, Navis GJ, Gordijn SJ, Bolling MC, Dijkstra G, Voors A A, Osterhaus AD, Voort PH, Mulder DJ, and Goor H. (2020). Angiotensin-converting enzyme 2 (ACE2), SARS-CoV -2 and the pathophysiology of coronavirus disease 2019 (COVID -19). J Pathol 251:228–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burtscher J, Burtscher M, and Millet GP. (2020). Caution is needed on the effect of altitude on the pathogenesis of SAR-CoV-2 virus. Respir Physiol Neurobiol 279:103464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano-Pérez E, Torres-Pacheco J, Fragozo-Ramos MC, García-Díaz G, Montalvo-Varela E, and Pozo-Palacios JC. (2020). Negative correlation between altitude and COVID-19 pandemic in Colombia: A preliminary report. Am J Trop Med Hygiene 103:2347–2349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowell G, Viboud C, Munayco CV, Gómez J, Simonsen L, Miller MA, Tamerius J, Fiestas V, Halsey ES, and Laguna-Torres VA. (2011). Spatial and temporal characteristics of the 2009 A/H1N1 influenza pandemic in Peru. PLoS One 6:e21287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dang Z, Su S, Jin G, Nan X, Ma L, Li Z, Lu D, and Ge R. (2020). Tsantan Sumtang attenuated chronic hypoxia-induced right ventricular structure remodeling and fibrosis by equilibrating local ACE-AngII-AT1R/ACE2-Ang1-7-Mas axis in rat. J Ethnopharmacol 250:112470. [DOI] [PubMed] [Google Scholar]
- Dong E, Du H, and Gardner L. (2020). An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 20:533–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampl V, Herget J, Bíbová J, Baňasová A, Husková Z, Vaňourková Z, Jíchová Š, Kujal P, Vernerová Z, Sadowski J, and Červenka L. (2015). Intrapulmonary activation of the angiotensin-converting enzyme type 2/angiotensin 1–7/G-protein-coupled mas receptor axis attenuates pulmonary hypertension in Ren-2 transgenic rats exposed to chronic hypoxia. Physiol Res 64:25–38. [DOI] [PubMed] [Google Scholar]
- Hettmansperger TP, and McKean JW. (2011). Robust Nonparametric Statistical Methods, 2nd ed. CRC Press, Boca Raton, FL. [Google Scholar]
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, and Cao B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- INEI. (2017). Censos Nacionales 2017: XII de población, VII de Vivienda y III de comunidades indígenas. Available at: https://censos2017.inei.gob.pe/redatam/ (accessed February 14, 2022).
- INEI. (2019). Perú: Enfermedades no transmisibles y transmisibles, 2019. Instituto Nacional de Estadística e Informática. Available at: https://proyectos.inei.gob.pe/endes/2019/SALUD/ENFERMEDADES_ENDES_2019.pdf (accessed February 14, 2022).
- INEI. (2020a). Informe Técnico: Evolución de la Pobreza Monetaria 2008–2019. Instituto Nacional de Estadística e Informática. Available at: https://www.inei.gob.pe/media/cifras_de_pobreza/informe_pobreza2019.pdf (accessed February 14, 2022).
- INEI. (2020b). Mapa de Pobreza Monetaria Provincial y Distrital 2018. Instituto Nacional de Estadística e Informática. Available at: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1718/Libro.pdf (accessed February 14, 2022).
- James N, and Menzies M. (2020). COVID-19 in the United States: Trajectories and second surge behavior. Chaos 30:091102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H, Stratton CW, and Tang Y. (2020a). Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol 92:401–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. (2020b). Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 395:565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mena GE, Martinez PP, Mahmud AS, Marquet PA, Buckee CO, and Santillana M. (2021). Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science 372:eabg5298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministerio de Salud. (2019). Estadística Poblacional. Available at: https://www.minsa.gob.pe/reunis/data/poblacion_estimada.asp (accessed February 14, 2022).
- Plataforma Digital Única del Estado Peruano. (2020). Minsa lamenta el sensible fallecimiento del primer paciente a causa de infección COVID-19 (Comunicado N°20). Available at: https://www.gob.pe/institucion/minsa/noticias/109580-minsa-lamenta-el-sensible-fallecimiento-del-primer-paciente-a-causa-de-infeccion-covid-19-comunicado-n-20 (accessed February 14, 2022).
- Plataforma Nacional de Datos Abiertos. (2021a). Data histórica del Registro de Camas diarias disponibles y ocupadas del formato F500.2—V.2 desde el 31/03/2021—SUSALUD. Available at: https://www.datosabiertos.gob.pe/dataset/data-hist%C3%B3rica-del-registro-de-camas-diarias-disponibles-y-ocupadas-del-formato-f5002-v2 (accessed February 14, 2022).
- Plataforma Nacional de Datos Abiertos. (2021b). Fallecidos por COVID-19—MINSA. Available at: https://www.datosabiertos.gob.pe/dataset/fallecidos-por-covid-19-ministerio-de-salud-minsa (accessed February 14, 2022).
- Pun M, Turner R, Strapazzon G, Brugger H, and Swenson ER. (2020). Lower incidence of COVID-19 at high altitude: Facts and confounders. High Altitude Med Biol 21:217–222. [DOI] [PubMed] [Google Scholar]
- Quevedo-Ramirez A, Al-kassab-Córdova A, Mendez-Guerra C, Cornejo-Venegas G, and Alva-Chavez KP. (2020). Altitude and excess mortality during COVID-19 pandemic in Peru. Respir Physiol Neurobiol 281:103512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren L-L, Wang Y-M, Wu Z-Q, Xiang Z-C, Guo L, Xu T, Jiang Y-Z, Xiong Y, Li Y-J, Li X-W, Li H, Fan G-H, Gu X-Y, Xiao Y, Gao H, Xu J-Y, Yang F, Wang X-M, Wu C, , Chen L, Liu YW, Liu B, Yang J, Wang XR, Dong J, Li L, Huang CL, Zhao JP, Hu Y, Cheng ZS, Liu LL, Qian ZH, Qin C, Jin Q, Cao B, Wang J-W. (2020). Identification of a novel coronavirus causing severe pneumonia in human: A descriptive study. Chin Med J 133:1015–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RENIEC. (2019). Información Estadística. Available at: https://portales.reniec.gob.pe/web/estadistica/baseDatos (accessed February 14, 2022).
- Seclén SN, Nunez-Robles E, Yovera-Aldana M, and Arias- Chumpitaz A. (2020). Incidence of COVID-19 infection and prevalence of diabetes, obesity and hypertension according to altitude in Peruvian population. Diabetes Res Clin Pract 169:108463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segovia-Juarez J, Castagnetto JM, and Gonzales GF. (2020). High altitude reduces infection rate of COVID-19 but not case-fatality rate. Respir Physiol Neurobiol 281:103494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smirnova A, Sterrett N, Mujica OJ, Munayco C, Suárez L, Viboud C, and Chowell G. (2020). Spatial dynamics and the basic reproduction number of the 1991–1997 Cholera epidemic in Peru. PLOS Negl Trop Dis 14:e0008045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens KE, Chernyavskiy P, and Bruns DR. (2021). Impact of altitude on COVID-19 infection and death in the United States: A modeling and observational study. PLoS One 16:e0245055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson TM, Casas F, Guerrero HA, Figueroa-Mujíca R, Villafuerte FC, and Machicado C. (2021). Potential protective effect from COVID-19 conferred by altitude: A longitudinal analysis in Peru during full lockdown. High Alt Med Biol 22:209–224. [DOI] [PubMed] [Google Scholar]
- Tremblay JC, and Ainslie PN. (2021). Global and country-level estimates of human population at high altitude. Proc Natl Acad Sci 118:e2102463118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolcott OO, and Bergman RN. (2020). Mortality attributed to COVID-19 in high-altitude populations. High Alt Med Biol 21:409–416. [DOI] [PubMed] [Google Scholar]
- Yufra S, and Huerta P. (2019). El Reto de la Igualdad: Una lectura de las dinámicas territoriales en el Perú. Lima: Programa de las Naciones Unidas para el Desarrollo. UNDP. Available at: https://www.pe.undp.org/content/peru/es/home/library/poverty/el-reto-de-la-igualdad.html (accessed February 14, 2022).
- Zhang J, Dong X, Cao Y, Yuan Y, Yang Y, Yan Y, Akdis CA, and Gao Y. (2020). Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 75:1730–1741. [DOI] [PubMed] [Google Scholar]
- Zhu Y, Xie J, Huang F, and Cao L. (2020). Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci Total Environ 727:138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.