Abstract
Background:
It is undetermined which factors predict return to work after arthroscopic rotator cuff repair.
Purpose:
To identify which factors predicted return to work at any level and return to preinjury levels of work 6 months after arthroscopic rotator cuff repair.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
Multiple logistic regression analysis of prospectively collected descriptive, preinjury, preoperative, and intraoperative data from 1502 consecutive primary arthroscopic rotator cuff repairs, performed by a single surgeon, was performed to identify independent predictors of return to work at 6 months postoperatively.
Results:
Six months after arthroscopic rotator cuff repair, 76% of patients had returned to work, and 40% had returned to preinjury levels of work. Return to work at 6 months was likely if patients were still working after their injuries but before surgery (Wald statistic [W] = 55, P < .0001), were stronger in internal rotation preoperatively (W = 8, P = .004), had full-thickness tears (W = 9, P = .002), and were female (W = 5, P = .030). Patients who continued working postinjury but presurgery were 1.6 times more likely to return to work at any level at 6 months compared to patients who were not working (P < .0001). Patients who had a less strenuous preinjury level of work (W = 173, P < .0001), worked at a mild to moderate level post injury but presurgery, had greater preoperative behind-the-back lift-off strength (W = 8, P = .004), and had less preoperative passive external rotation range of motion (W = 5, P = .034) were more likely to return to preinjury levels of work at 6 months postoperatively. Specifically, patients who worked at a mild to moderate level postinjury but presurgery were 2.5 times more likely to return to work than patients who were not working, or who were working strenuously postinjury but presurgery (p < 0.0001). Patients who nominated their preinjury level of work as “light” were 11 times more likely to return to preinjury levels of work at 6 months compared to those who nominated it as “strenuous” (P < .0001).
Conclusion:
Six months after rotator cuff repair, patients who continued to work after injury but presurgery were the most likely to return to work at any level, and patients who had less strenuous preinjury levels of work were the most likely to return to their preinjury levels of work. Greater preoperative subscapularis strength independently predicted return to work at any level and to preinjury levels.
Keywords: rotator cuff repair, rotator cuff tear, return to work, determinants, predictors
Rotator cuff tears are a common cause of shoulder pain and dysfunction.8,21,28,29 Several authors have evaluated rates of return to work after rotator cuff repair and explored the factors associated with higher rates of return to work. Specifically, several studies have found that patients who had more physically intensive jobs before sustaining rotator cuff tears were less likely to return to work after an arthroscopic rotator cuff repair.1,5,12,13,15,23
Aagaard et al1 and Gutman et al12 found that patients who sustained rotator cuff tears on the side of their dominant arm were less likely to return to work than were patients who sustained tears on their nondominant side. Collin et al5 and Imai et al15 found that female patients were less likely to return to work after a rotator cuff repair than were male patients. Furthermore, it has been well established that patients who had workers’ compensation experience poorer outcomes and delayed return to work compared with those who did not have workers’ compensation.2,3,14,16
It is not clear, however, how other factors, such as preoperative patient-rated pain and function, range of motion, strength, tear size, tear thickness, tissue mobility, or repair quality, influence a patient’s ability to return to work after a rotator cuff repair. Our clinical practice has prospectively collected these descriptive, preoperative, intraoperative, and level of work data in a systematic manner.
The aims of this study, therefore, were to determine which descriptive, preoperative, and intraoperative factors predicted (1) return to work at any level and (2) return to preinjury level of work at 6 months after primary arthroscopic rotator cuff repair.
Methods
A post hoc analysis of prospectively collected data was performed to identify which factors were associated with return to work 6 months after primary arthroscopic rotator cuff repair. This study was undertaken after ethics approval was granted by the South Eastern Sydney Local Health District Human Research Ethics Committee (reference No.: HREC/11/STG/37).
Inclusion and Exclusion Criteria
Patients who underwent primary arthroscopic rotator cuff repair, performed by a single surgeon (G.A.C.M.) between January 2005 and December 2020, and who declared that they were still working, including patients who were working in a nonemployed capacity (ie, housewife/husband), were eligible for inclusion.
Patients who had (1) irreparable rotator cuff tears, (2) partially repaired rotator cuff tears, (3) rotator cuff tears repaired using interposition grafts or onlay biological patches, (4) isolated subscapularis repairs, (5) rotator cuff repairs associated with calcific tendinitis, or (6) associated fractures or (7) who had undergone concurrent stabilization procedures were excluded. Patients who underwent another operation not related to their index surgery (eg, rotator cuff repair on the other side within 6 months of the index surgery) that would have delayed return to work were also excluded. When a patient required revision or reoperation due to the index procedure, the failed index procedure was included, but the revision case was excluded. Patients who declared that they were retired or did not disclose their preinjury, preoperative, or 6-month postoperative level(s) of work were also excluded.
Surgical Technique
All rotator cuff repairs were performed arthroscopically. Patients were positioned in the upright beach-chair position and received an interscalene block and sedation. An arthroscope was inserted into the glenohumeral joint through a posterior portal. Debridement of the tendon and footprint was performed using an arthroscopic shaver. All partial-thickness tears, which in this cohort were at least 50% in thickness, were converted to full-thickness tears. A knotless inverted mattress repair was performed using a suture passer (OPUS SmartStitch; Smith & Nephew) and secured using knotless suture anchors (Opus Magnum 2; Smith & Nephew) from the articular side.7
Postoperative Care
Patients used a sling with an abduction pillow (UltraSling; DJO) for 6 weeks. From day 1 until 6 weeks postoperatively, pendular reach, elbow flexion and extension, and grip and scapula exercises were recommended. From day 8 until 6 weeks, passive shoulder external-internal rotation, flexion, and extension exercises were recommended. Active shoulder movements and isometric exercises were recommended from week 6. Overhead activity and lifting >5 kg were allowed after 3 months. Patients returned for follow-up at 1 week, 12 weeks, and 6 months postoperatively.
Data Collection
Patient Characteristics
At first visit, patients nominated their age, sex, occupation, insurance status, which shoulder was affected, if they had a specific initiating injury, whether the shoulder problem was work related, whether the shoulder had ever been dislocated, if the shoulder had ever been previously treated, and date of onset of symptoms.
Preinjury
Patients completed a standardized 12-item functional questionnaire based on the L’Insalata Shoulder Rating Questionnaire, which, in addition to being administered at the first consultation, was administered at every subsequent visit.17 In addition, patients answered the questions, “What was your previous level of work?” (preinjury level of work) using a 4-point Likert scale (none, light activity, moderate activity, strenuous labor) and “What was your previous level of sport?” using a 4-point scale (none, hobby, club, national).
Preoperative (Postinjury, Presurgery)
Frequency of pain with activity and with sleep and extreme pain were graded using a 5-point scale (never, monthly, weekly, daily, always). Levels of shoulder pain at rest, with overhead activity, and during sleep and difficulty with reaching behind the back and reaching overhead were graded using a 5-point scale (none, mild, moderate, severe, very severe). Stiffness was graded using a 5-point scale (not at all, a little, moderate, quite, very). Overall rating of the shoulder was graded using a 5-point scale (very bad, bad, poor, fair, good).
Passive shoulder range of motion in forward flexion, abduction, external rotation, and internal rotation, and shoulder strength in abduction, adduction, internal rotation, external rotation, and lift-off from behind the back were measured using a handheld dynamometer (HFG 110; Transducer Techniques), per previously validated protocols.6,18,24
Intraoperative
The diagnosis of a full- or partial-thickness tear and the presence of osteoarthritis was made intraoperatively. Tear dimensions were estimated with reference to the diameter of the arthroscopic shaver. Tissue quality, tissue mobility, and repair quality were graded using a 4-point scale (fair, good, very good, excellent) by the surgeon as previously described.25,27
Six Months Postoperative
At 6 months postoperatively, the questionnaires and functional assessments were repeated, in addition to assessment of the integrity of the repair by a specialist musculoskeletal sonographer (M.S.).4
Statistical Analysis
Return to work was calculated by comparing patients’ preinjury level of work to their 6-month postoperative level of work. If they rated their 6-month postoperative level of work as “none,” then they were considered not to have returned to work, whereas if they had rated it as “light,”“moderate,” or “strenuous,” they were considered to have returned to work at any level.
Patients were considered to have returned to their preinjury level of work if their 6-month postoperative level of work was (1) greater than “none” and if it was (2) greater than or equal to their preinjury level of work.
Multiple regression analysis allows for identification of independent variables associated with the dependent variable (return to work at any level or return to preinjury levels of work). In the backward regression technique, all potential variables are assessed and gradually eliminated to generate the best equation. The remaining variables are classified as “independent.” All the tested variables are included in the Appendix Table A1 (available in the online version of this article).
Categorical variables were compared using the chi-square test. Nonparametric continuous variables were compared using the Mann-Whitney U test or the Kruskal-Wallis test where appropriate. P < 0.05 was considered statistically significant. All analyses were performed using SPSS Version 26 (IBM Corp., Armonk, NY).
Results
Patient Selection
Between January 2005 and December 2020, a single surgeon performed 2407 primary arthroscopic rotator cuff repairs. Those who had partially or fully irreparable tears that required use of an interposition graft or superior capsular reconstruction (n = 69); underwent concurrent stabilization procedures (n = 42); had isolated subscapularis tears (n = 29), calcific tendinitis (n = 12), or fractures of the affected shoulder (n = 9); received another surgical procedure, such as rotator cuff repair of the contralateral shoulder, within 6 months of index surgery that would have delayed return to work (n = 12); nominated their occupation as “retired” (n = 470); or did not disclose their preinjury, preoperative, or 6-month postoperative level(s) of work (n = 262) were excluded. Ultimately, this study included 1502 cases of primary arthroscopic rotator repairs that were performed in 1453 patients for analysis.
Patient Characteristics
At the time of surgery for the affected shoulder, the mean ± SD age was 55 ± 10 years. In this cohort, 62% (900/1453) of patients were male, 66% (991/1502) of cases were in privately insured patients, 28% (422/1502) of cases were in patients with workers’ compensation claims, 3% (44/1502) of cases were in self-funded patients, and 3% of cases (45/1502) were performed in a public hospital.
Return to work 6 months after primary arthroscopic rotator cuff repair was achieved in 76% (1142/1502) of cases; in 40% (602/1502) of cases, patients returned to their preinjury levels of work.
Return to Work at Any Level at 6 Months
A multivariate analysis was performed to determine which descriptive, preoperative, and intraoperative factors were associated with a patient’s ability to return to work at any level 6 months after primary arthroscopic rotator cuff repair.
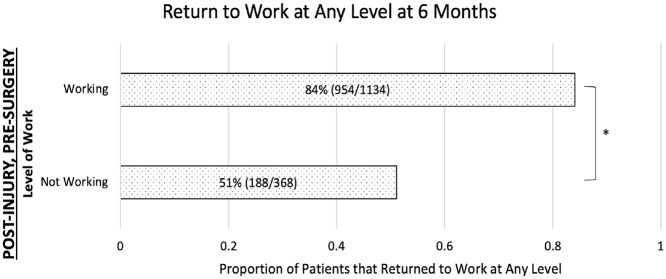
The multivariate analysis identified that the strongest independent predictor of return to work at any level at 6 months postoperatively was if patients were working more strenuously after their injury but before surgery than those who were working at a less strenuous level in the same after-injury, presurgery state (Table 1). Patients who returned to work at any level 6 months postoperatively were more likely to have continued working after their injuries but before surgery (Figure 3).
Table 1.
Independent Descriptive, Preoperative, and Intraoperative Factors Associated With Return to Work at Any Level at 6 Months Postoperatively, Ranked by Wald Statistic
| Descriptive, Preoperative, and Intraoperative Factors | More Likely to Return to Work if | Wald Statistic | B Coefficient | P Value |
|---|---|---|---|---|
| Level of work (postinjury, preoperative) | More strenuous | 28 | 0.7 | <.0001 |
| Strength in internal rotation (preoperative) | Stronger | 14 | 0.01 | <.0001 |
| Sex | Female | 8 | −0.7 | .006 |
| Tear thickness (intraoperative) | Full thickness | 8 | 0.6 | .006 |
| Level of pain with overhead activities (preoperative) | Lower | 6 | −0.3 | .011 |
| Tissue mobility (intraoperative) | More mobile | 5 | 0.5 | .023 |
| Repair quality (intraoperative) | Higher quality | 5 | −0.6 | .031 |
| Passive external rotation range of motion (preoperative) | Less range | 3 | −0.008 | <.0001 |
Figure 3.
Proportion of patients who returned to work at any level, stratified by whether or not a patient was working after the development of a shoulder problem but before receiving surgery. Statistical analysis was performed using the chi-square test. *P < .05.
Patients were more likely to return to work at any level if they were stronger in internal rotation (vs weaker internal rotation) preoperatively, were female (NB: females were 63% less likely to perform strenuous work than males in this cohort), had full-thickness tears (vs partial-thickness tears) intraoperatively, had less pain with overhead activities preoperatively, had more mobile tissues (vs immobile tissues) and higher repair quality (vs lower repair quality) per intraoperative surgeon assessment, and had less passive external rotation range of motion (vs greater passive external rotation range of motion) preoperatively (Table 1).
Return to Preinjury Levels of Work at 6 Months
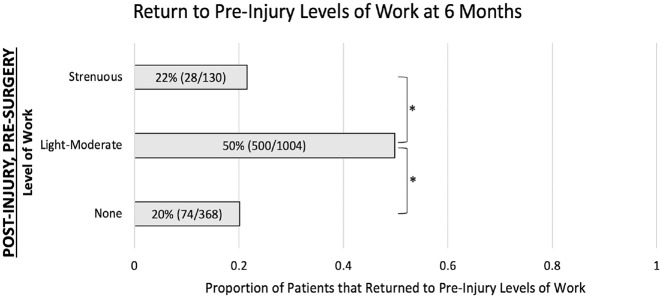
Patients who returned to preinjury levels of work were more likely to have worked less strenuously before their injuries (Table 2). They were also more likely to return to preinjury levels of work if they worked at a “light” or “moderate” level after injury before surgery. They were less likely to return to work at their preinjury level if they did not work (“none”) between the time of their injury and the time of the surgery or if they worked at a “strenuous” level after injury before the surgery (Figure 4).
Table 2.
Independent Descriptive, Preoperative, and Intraoperative Factors Associated With Return to Preinjury Levels of Work at 6 Months Postoperatively, Ranked by Wald Statistic
| Descriptive, Preoperative, and Intraoperative Factors | More Likely to Return to Preinjury Levels of Work if | Wald Statistic | B Coefficient | P Value |
|---|---|---|---|---|
| Level of work (preinjury) | Less strenuous | 173 | −3 | <.0001 |
| Level of work (postinjury, preoperative) | More strenuous | 22 | 0.8 | <.0001 |
| Lift-off strength (preoperative) | Stronger | 8 | 0.01 | .004 |
| Passive external rotation range of motion (preoperative) | Less range | 5 | −0.01 | .034 |
Figure 4.
Proportion of patients who returned to preinjury levels of work, stratified by level of work after the development of a shoulder problem but before receiving surgery. Statistical analysis was performed using the chi-square test. *P < .05.
Patients were also more likely to return to preinjury levels of work if they had greater behind-the-back lift-off strength (vs less lift-off strength) preoperatively and had less passive external rotation range of motion (vs greater passive external rotation range of motion) preoperatively (Table 2).
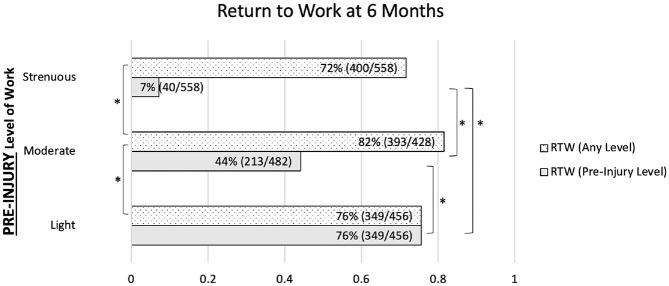
Preinjury Level of Work
A significantly smaller proportion of patients returned to preinjury levels of work 6 months after rotator cuff repair if they had nominated their preinjury level of work as “strenuous” than if they had nominated it as “light” (P < .0001) or “moderate” (P < .0001) or if they had nominated their preinjury level of work as “moderate” instead of “light” (P < .0001) (Figure 1).
Figure 1.
Proportion of patients who returned to work at any level (dotted) and to preinjury levels (gray), stratified by level of work before the development of a shoulder problem. Statistical analysis was performed using the chi-square test. RTW, return to work. *P < .05.
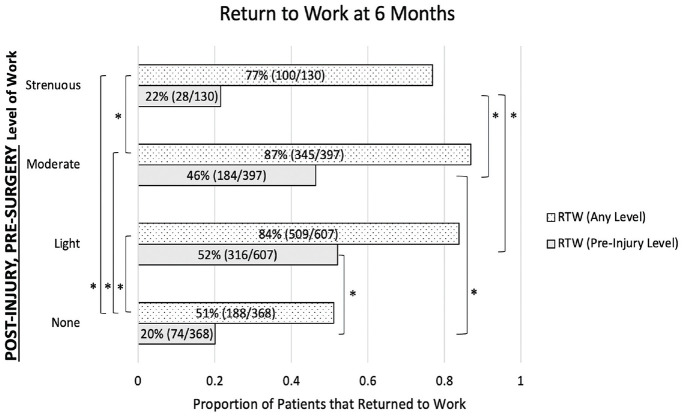
Postinjury, Preoperative Level of Work
The proportion of patients who returned to work at any level at 6 months postoperatively was significantly greater if they were still working after developing a shoulder injury but before surgery than if they were not working (P < .0001) (Figure 3).
The proportion of patients who returned to preinjury levels of work followed a bell-curve pattern according to their level of work after developing a shoulder problem but before receiving surgery, with those most likely to return to preinjury duties nominating their level as “light” or “moderate” (Figure 2 and Figure 4). Patients who nominated their postinjury, preoperative level of work as “none” or “strenuous” experienced a similar rate of return to preinjury levels of work, whereas patients who continued to work at a “light” or “moderate” (P < .0001) level were 2.5 times more likely to return to their preinjury levels of work (Figure 2).
Figure 2.
Proportion of patients who returned to work at any level (dotted) and to preinjury levels (gray), stratified by level of work after the development of a shoulder problem but before receiving surgery. Statistical analysis was performed using the chi-square test. RTW, return to work. *P < .05.
Further Analysis
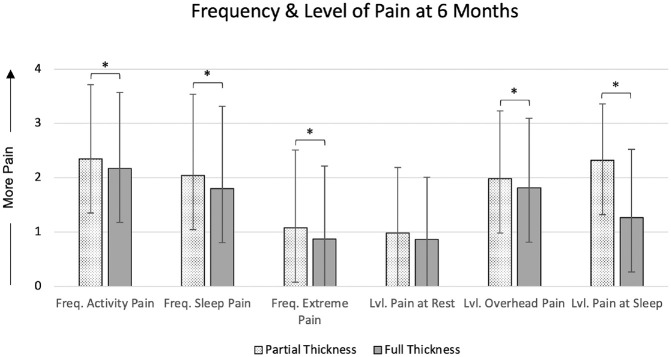
Patients who had partial-thickness tears reported experiencing significantly more frequent pain during activity (P = .0205) and at sleep (P = .0037), had more frequent episodes of extreme pain (P = .0119), and had significantly higher levels of pain with overhead activities (P = .0136) and during sleep (P < .0001) compared with patients who had full-thickness tears (Figure 5).
Figure 5.
Frequency and level of pain at 6 months after rotator cuff repair, grouped by tear thickness. Data are means ± SDs. Statistical analysis was performed using the Mann-Whitney U test. Freq., frequency of; Lvl., level of. *P < .05.
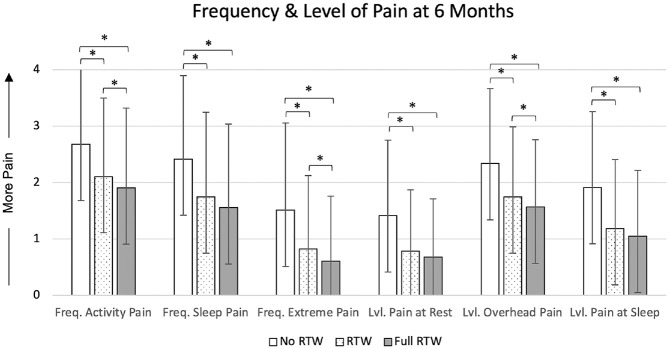
At 6 months postoperatively, patients who returned to preinjury levels of work reported experiencing less frequent pain with activity and at sleep, fewer episodes of extreme pain, and lower levels of pain at rest, with overhead activities, and during sleep compared with patients who returned to work at any level (Figure 6).
Figure 6.
Frequency and level of pain at 6 months after rotator cuff repair, stratified by return-to-work status. Statistical analysis was performed using the Kruskal-Wallis test with Dunn post hoc test for multiple comparisons. Freq., frequency of; Full RTW, return to preinjury levels of work; Lvl., level of; RTW, return to work at any level. *P < .05.
Discussion
A major finding of the present study was that the strongest predictor of a patient returning to work 6 months after primary arthroscopic rotator cuff repair was if they had continued to work despite having a rotator cuff tear but before receiving surgery. Patients who continued to work despite their injury were 1.6 times more likely to return to work than those who did/could not work after sustaining a tear. However, the strongest predictor of a patient returning to preinjury levels of work, was having a less strenuous work level to begin with, as patients who nominated their preinjury level of work as “light” were 11 times more likely to return to preinjury levels of work than those who had nominated it as “strenuous.”
Patients who continued to work at a strenuous level in their postinjury, presurgery state were just as likely to return to preinjury levels of work as those who were not working in their postinjury, presurgery state. In comparison, patients who continued to work at a light or moderate level despite sustaining a rotator cuff tear were 2.5 times more likely to return to preinjury levels of work 6 months after surgery than those who did not work in this time period or who worked strenuously in the period between injury and surgery.
Several studies have reported that female patients were less likely to return to work.5,15 However, this study found that female sex was an independent predictor of return to work at any level at 6 months. It is important to note, however, that in this cohort, females were 63% less likely than males to perform strenuous work before developing shoulder problems. This suggests that sex per se may not independently predict return to work but that female patients, in general, had less strenuous jobs and were therefore more likely to return to work after rotator cuff repair.
Interesting, unexpected factors identified were that patients who had greater preoperative internal rotation strength were more likely to return to work at any level and patients who had greater preoperative behind-the-back lift-off strength were more likely to return to preinjury levels of work. These data suggest that subscapularis function may be important in return to work.
Stiffness in external rotation has been associated with a healing rotator cuff repair.19,20 Unexpectedly, patients who had less preoperative passive external rotation range were more likely to return to preinjury levels of work. These data imply that increased stiffness after rotator cuff repair was associated with an increased rate of return to work.
Interestingly, having a full-thickness rotator cuff tear was an independent predictor of return to work. Patients who had partial-thickness tears reported more severe and more frequent pain 6 months after rotator cuff repair compared to patients who had full-thickness tears. Our findings affirmed the observation that patients with partial-thickness tears experience more preoperative pain than patients with full-thickness tears.9-11,26 In addition, there was an inverse relationship between return to work and pain levels, with patients not returning to work experiencing the most pain and those who returned to preinjury levels of work experiencing the least pain. While having a full-thickness tear predicted return to work after rotator cuff repair, tear size was not identified as a significant predictor. Imai et al15 similarly found no correlation between tear size and return to work.
Interestingly, age and workers’ compensation status were not significant predictors of return to work in this study. Similarly, a meta-analysis of 13 studies involving 1224 patients with rotator cuff repair by Haunschild et al13 found no difference in the rate of return to work, irrespective of a patient’s workers’ compensation status. In contrast, other studies have reported a negative association between increased age or workers’ compensation and return to work.2,3,14,16,22
A strength of this study was that it was, to our knowledge, the largest in terms of cohort size and number of factors analyzed for association with return to work after arthroscopic rotator cuff repair. Another strength was that these were consecutive cases performed by a single surgeon, and all assessments of repair integrity were performed by a single sonographer. In addition, the data were prospectively collected in a standardized, systematic manner. The high internal validity of our results may limit its external validity.
A weakness of our study was that asking patients to nominate their preinjury level of work at the first consultation may have been subject to recall bias. Another limitation was that factors like diabetes mellitus or smoking status that may have influenced return to work were not collected and not included in the analysis. Furthermore, 6 months is a relatively short follow-up period, and any changes to patients’ work status beyond this point were not captured. However, a longer follow-up period may introduce additional variables that may be independent of surgery, such as work performance or retirement. In addition, patients’ decision to return to work may have been affected by their interpretation of the recommended rehabilitation protocol.
Conclusion
Patients who continued to work despite sustaining a rotator cuff tear but before surgery were 1.6 times more likely to return to work 6 months after primary arthroscopic rotator cuff repair than were those who were not working in their injured state. Patients who reported less pain with overhead activities preoperatively, had intraoperatively diagnosed full-thickness tears, had higher surgeon-ranked tissue mobility, and had higher repair quality were the most likely to return to work 6 months after primary arthroscopic rotator cuff repair. Patients who rated their work as less strenuous before their injury were the most likely to return to preinjury levels of work. Patients who continued to work at a light or moderate level after their injury but before their surgery were > 2 times more likely to return to preinjury levels of work 6 months postoperatively than were patients who either continued to work strenuously despite their injuries or were not working in their injured state. Greater preoperative subscapularis strength and decreased preoperative passive external rotation range of motion were independent predictors of both return to work at any level and return to preinjury levels 6 months after rotator cuff repair.
Supplemental Material
Supplemental material, sj-pdf-1-ajs-10.1177_03635465231152479 for Predictors of Return to Work Following Primary Arthroscopic Rotator Cuff Repair: An Analysis of 1502 Cases by Ryan S. Ting, Ron Rosenthal, Yaerhim Shin, Mina Shenouda, Hilal S. A. Al-Housni, Patrick H. Lam and George A. C. Murrell in The American Journal of Sports Medicine
Acknowledgments
The authors would like to sincerely thank Linda Dodd and Marina Zimmermann for their contributions and the continuous support that they have provided throughout this project.
Footnotes
Submitted August 10, 2022; accepted December 19, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: G.A.C.M. has received consulting fees and research support from Smith+Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
ORCID iD: Ryan S. Ting  https://orcid.org/0000-0003-0106-3129
https://orcid.org/0000-0003-0106-3129
References
- 1. Aagaard KE, Randeblad P, Abu-Zidan FM, Lunsjö K. Return to work after early repair of acute traumatic rotator cuff tears. Eur J Trauma Emerg Surg. 2020;46(4):817-823. [DOI] [PubMed] [Google Scholar]
- 2. Balyk R, Luciak-Corea C, Otto D, Baysal D, Beaupre L. Do outcomes differ after rotator cuff repair for patients receiving workers’ compensation? Clin Orthop Relat Res. 2008;466(12):3025-3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cancelliere C, Donovan J, Stochkendahl MJ, et al. Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropr Man Therap. 2016;24(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cole B, Twibill K, Lam P, Hackett L, Murrell GA. Not all ultrasounds are created equal: general sonography versus musculoskeletal sonography in the detection of rotator cuff tears. Shoulder Elbow. 2016;8(4):250-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Collin P, Abdullah A, Kherad O, et al. Prospective evaluation of clinical and radiologic factors predicting return to activity within 6 months after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2015;24(3):439-445. [DOI] [PubMed] [Google Scholar]
- 6. Duong JKH, Lam PH, Murrell GAC. Anteroposterior tear size, age, hospital, and case number are important predictors of repair integrity: an analysis of 1962 consecutive arthroscopic single-row rotator cuff repairs. J Shoulder Elbow Surg. 2021;30(8):1907-1914. [DOI] [PubMed] [Google Scholar]
- 7. Elkins A, Lam PH, Murrell GAC. A novel, fast, safe, and effective all-inside arthroscopic rotator cuff repair technique: results of 1000 consecutive cases. Orthop J Sports Med. 2019;7(8):2325967119864088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fehringer EV, Sun J, VanOeveren LS, Keller BK, Matsen FA, III. Full-thickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elbow Surg. 2008;17(6):881-885. [DOI] [PubMed] [Google Scholar]
- 9. Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone Joint Surg Br. 2003;85(1):3-11. [DOI] [PubMed] [Google Scholar]
- 10. Fukuda H. Partial-thickness rotator cuff tears: a modern view on Codman’s classic. J Shoulder Elbow Surg. 2000;9(2):163-168. [PubMed] [Google Scholar]
- 11. Gschwend N, Ivosević-Radovanović D, Patte D. Rotator cuff tear—relationship between clinical and anatomopathological findings. Arch Orthop Trauma Surg (1978). 1988;107(1):7-15. [DOI] [PubMed] [Google Scholar]
- 12. Gutman MJ, Patel MS, Katakam A, et al. Understanding outcomes and the ability to return to work after rotator cuff repair in the workers’ compensation population. Cureus. 2021;13(3):e14213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Haunschild ED, Gilat R, Lavoie-Gagne O, et al. Return to work after primary rotator cuff repair: a systematic review and meta-analysis. Am J Sports Med. 2021;49(8):2238-2247. [DOI] [PubMed] [Google Scholar]
- 14. Henn RF, III, Tashjian RZ, Kang L, Green A. Patients with workers’ compensation claims have worse outcomes after rotator cuff repair. J Bone Joint Surg Am. 2008;90(10):2105-2113. [DOI] [PubMed] [Google Scholar]
- 15. Imai T, Gotoh M, Hagie K, et al. Factors affecting return to work in patients undergoing arthroscopic rotator cuff repair. Prog Rehabil Med. 2019;4:20190006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kemp KAR, Sheps DM, Luciak-Corea C, et al. Systematic review of rotator cuff tears in workers’ compensation patients. Occup Med. 2011;61(8):556-562. [DOI] [PubMed] [Google Scholar]
- 17. L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am. 1997;79(5):738-748. [PubMed] [Google Scholar]
- 18. Le BT, Wu XL, Lam PH, Murrell GA. Factors predicting rotator cuff retears: an analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med. 2014;42(5):1134-1142. [DOI] [PubMed] [Google Scholar]
- 19. McNamara WJ, Lam PH, Murrell GAC. The relationship between shoulder stiffness and rotator cuff healing: a study of 1,533 consecutive arthroscopic rotator cuff repairs. J Bone Joint Surg Am. 2016;98(22):1879-1889. [DOI] [PubMed] [Google Scholar]
- 20. Millican CR, Lam PH, Murrell GAC. Shoulder stiffness after rotator cuff repair: the fate of stiff shoulders up to 9 years after rotator cuff repair. J Shoulder Elbow Surg. 2020;29(7):1323-1331. [DOI] [PubMed] [Google Scholar]
- 21. Minagawa H, Yamamoto N, Abe H, et al. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: from mass-screening in one village. J Orthop. 2013;10(1):8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nové-Josserand L, Liotard JP, Godeneche A, et al. Occupational outcome after surgery in patients with a rotator cuff tear due to a work-related injury or occupational disease: a series of 262 cases. Orthop Traumatol Surg Res. 2011;97(4):361-366. [DOI] [PubMed] [Google Scholar]
- 23. Pichené-Houard A, Paysant J, Claudon L, et al. Predictive factors for the duration until return to work after surgery for work-related rotator cuff syndrome: a prospective study of 92 workers. Am J Ind Med. 2021;64(12):1028-1039. [DOI] [PubMed] [Google Scholar]
- 24. Robinson HA, Lam PH, Walton JR, Murrell GAC. The effect of rotator cuff repair on early overhead shoulder function: a study in 1600 consecutive rotator cuff repairs. J Shoulder Elbow Surg. 2017;26(1):20-29. [DOI] [PubMed] [Google Scholar]
- 25. Tse AK, Lam PH, Walton JR, Hackett L, Murrell GA. Ultrasound determination of rotator cuff tear repairability. Shoulder Elbow. 2016;8(1):14-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wolff AB, Sethi P, Sutton KM, et al. Partial-thickness rotator cuff tears. J Am Acad Orthop Surg. 2006;14(13):715-725. [DOI] [PubMed] [Google Scholar]
- 27. Wu XL, Briggs L, Murrell GA. Intraoperative determinants of rotator cuff repair integrity: an analysis of 500 consecutive repairs. Am J Sports Med. 2012;40(12):2771-2776. [DOI] [PubMed] [Google Scholar]
- 28. Yamaguchi K, Ditsios K, Middleton WD, et al. The demographic and morphological features of rotator cuff disease: a comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699-1704. [DOI] [PubMed] [Google Scholar]
- 29. Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116-120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ajs-10.1177_03635465231152479 for Predictors of Return to Work Following Primary Arthroscopic Rotator Cuff Repair: An Analysis of 1502 Cases by Ryan S. Ting, Ron Rosenthal, Yaerhim Shin, Mina Shenouda, Hilal S. A. Al-Housni, Patrick H. Lam and George A. C. Murrell in The American Journal of Sports Medicine