Abstract
Background
Inflammation, oxidative stress and an imbalance between proteases and protease inhibitors are recognized pathophysiological features of chronic obstructive pulmonary disease (COPD). The aim of this study was to evaluate serum levels of matrix metalloproteinase-9 (MMP-9) and tissue inhibitor of metalloproteinase-1 (TIMP-1) in patients with COPD and to assess their relationship with lung function, symptom severity scores and recent acute exacerbations.
Methods
In this observational cohort study, serum levels of MMP-9 and TIMP-1 and the MMP-9/TIMP-1 ratio in the peripheral blood of COPD patients with stable disease and healthy controls were determined, and their association with lung function (postbronchodilator spirometry, body plethysmography, single breath diffusion capacity for carbon monoxide), symptom severity scores (mMRC and CAT) and exacerbation history were assessed.
Results
COPD patients (n = 98) had significantly higher levels of serum MMP-9 and TIMP-1 and a higher MMP-9/TIMP-1 ratio than healthy controls (n = 47) (p ≤ 0.001). The areas under the receiver operating characteristic curve for MMP-9, TIMP-1 and the MMP-9/TIMP-1 ratio for COPD diagnosis were 0.974, 0.961 and 0.910, respectively (all p < 0.05). MMP-9 and the MMP-9/TIMP-1 ratio were both negatively correlated with FVC, FEV1, FEV1/FVC, VC, and IC (all p < 0.05). For MMP-9, a positive correlation was found with RV/TLC% (p = 0.005), and a positive correlation was found for the MMP-9/TIMP-1 ratio with RV% and RV/TLC% (p = 0.013 and 0.002, respectively). Patients with COPD GOLD 3 and 4 presented greater MMP-9 levels and a greater MMP-9/TIMP-1 ratio compared to GOLD 1 and 2 patients (p ≤ 0.001). No correlation between diffusion capacity for carbon monoxide and number of acute exacerbations in the previous year was found.
Conclusions
COPD patients have elevated serum levels of MMP-9 and TIMP-1 and MMP-9/TIMP-1 ratio. COPD patients have an imbalance between MMP-9 and TIMP-1 in favor of a pro-proteolytic environment, which overall indicates the importance of the MMP-9/TIMP-1 ratio as a potential biomarker for COPD diagnosis and severity.
Keywords: Chronic obstructive pulmonary disease, Matrix metalloproteinase-9, Tissue inhibitor of metalloproteinase-1, Biomarkers, Airflow limitation, Lung hyperinflation
Background
Chronic obstructive pulmonary disease (COPD) is a heterogeneous disorder characterized by airflow limitation associated with an abnormal inflammatory response in the lungs [1]. Inflammation and oxidative stress can affect protease homeostasis, causing enhanced extracellular matrix (ECM) degradation and leading to progressive alveolar destruction and airway remodeling [2]. Matrix metalloproteases (MMPs) have been implicated as one of the many inflammatory mediators involved in COPD pathogenesis. MMPs degrade the ECM and have a complex relationship with cytokines, chemokines, adhesion receptors, growth factors and their receptors and a variety of enzymes [3–5]. Matrix metalloproteinase-9 (MMP-9) is a type IV collagen-degrading MMP secreted in the lungs by neutrophils, alveolar macrophages, bronchial epithelial cells and eosinophils [6, 7]. MMP-9 plays a significant role in augmenting the inflammatory process, matrix turnover and lung repair [8]. Its activity is regulated in three ways: transcription, proteolytic activation of the zymogen form and inhibition of the active enzyme by a host of natural inhibitors [9–11]. Inflammation and lung tissue destruction are intensified by the synergistic action of proteinases and reactive oxygen species [12]. It is well documented that pro-oxidants can activate the proenzyme form of MMPs and subsequently inactivate MMPs to reach homeostatic balance in affected tissue [13]. Tissue inhibitor of metalloproteinase (TIMP-1) is an inhibitor of MMP-9 that binds to MMP-9 precursors and to the active form. Deregulation and imbalance between the activity of proteases and protease inhibitors has implications for COPD pathogenesis.
Expiratory flow limitation (EFL) in COPD arises due to emphysema and airway disorder [14]. The current diagnosis and classification of COPD relies significantly on the degree of EFL derived by spirometric forced expiratory volume in 1 second (FEV1) measurement. Spirometry is the gold standard for accurate and reproducible measurements of lung function [15]. Lung hyperinflation is an important clinical phenomenon and is related to expiratory airflow limitation. Body plethysmography remains a reliable gold standard for the measurement of lung volumes and other compartments related to lung hyperinflation [16]. Diffusing capacity for carbon monoxide (DLCO) is one of the established physiological measurements of emphysema severity [17].
The aim of this study was to evaluate serum levels of both MMP-9 and TIMP-1 in COPD patients and to assess their relationship with lung function, symptom severity scores and acute exacerbations of chronic obstructive pulmonary disease (AECOPD). We hypothesized that elevated MMP-9 and an increased MMP-9/TIMP-1 ratio would be identified in patients with the most pronounced lung function impairment, increased burden of symptoms and more frequent AECOPD.
Material and methods
Study population
In this prospective study, COPD patients and healthy controls who were referred to the hospital-based Outpatient Pulmonology Department in the University Clinical Center of Serbia, Belgrade, between May 2017 and January 2018 were enrolled.
Subject enrollment and assessment of MMP-9 and TIMP-1
In this observational cohort study, 98 COPD patients and 47 healthy subjects were enrolled.
Inclusion and exclusion criteria for COPD patients are summarized in Table 1. All COPD patients’ inhalation therapy and exacerbation history in the previous year were recorded. Symptoms were assessed by the Modified Medical Research Council Dyspnea Scale (mMRC) and COPD Assessment Test (CAT), translated and validated [18]. COPD exacerbation was defined as acute worsening of respiratory symptoms that results in the requirement of additional therapy. A frequent exacerbator was a COPD patient with ≥ 2 exacerbations per year [19].
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Adults ≥ 40 years of age | Diagnosis of asthma or any other chronic respiratory disease |
| Diagnosis of COPD at least 6 months prior to enrollment | Immunosuppression of any kind |
| Diagnosis according to the Global Initiative for Chronic Obstructive Disease (GOLD) | Refusal to give informed consent |
| At least one spirometry measurement in the last year with a postbronchodilator, FEV1/FVC < 0.70 | Any acute or chronic condition that would limit the ability of the patient to participate in the study |
| Stable disease (no recent exacerbation for at least 4 weeks prior to enrollment) |
The control group included 47 healthy adults ≥ 40 years of age with no pulmonary, cardiovascular or other chronic disease, infection or inflammation that could influence inflammatory and oxidative status.
In all subjects (COPD patients and healthy controls), age, sex, smoking status (defined as current/former/never and reported in pack/years), and self-reported comorbidities were recorded. A current smoker was defined as someone who either smokes every day (daily smoker) or who currently smokes but not every day (occasional or nondaily smoker) [20]. Former smoker referred to someone who has smoked more than 100 cigarettes in their lifetime but has not smoked in the last 12 months.
All subjects underwent blood sampling and determination of serum MMP-9 and TIMP-1 levels with a minimum time frame of 4 weeks after previous AECOPD. Blood samples were collected and evaluated for complete blood count (CBS) and white blood cell count (WBC) using an LH750® Hematology Analyzer (Beckman Coulter, Inc., Brea, California, USA) and for serum separation. After collection of whole blood using Vacutainer tubes, samples were stored undisturbed at room temperature for 30 min and then centrifuged at 1000 × g for 10 min. Serum samples were aliquoted into 0.5 mL portions and stored at − 80 °C until analysis. MMP-9 and TIMP-1 were measured using enzyme-linked immunosorbent assay (ELISA) kits according to the manufacturer’s instructions (Quantikine ELISA, R&D Systems, Minneapolis, USA).
Pulmonary function tests
Pulmonary function tests were performed according to American Thoracic Society/European Respiratory Society (ATS/ERS) criteria [21–24]. Postbronchodilator spirometry was recorded on a JAEGER® MasterScreen Pneumo, single breath diffusion capacity for carbon monoxide (CO) on a JAEGER® MasterScreen Diffusion and body plethysmography on a JAEGER® MasterScreen Body. The analyzed parameters were forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), the FEV1/FVC ratio, diffusion capacity for carbon monoxide (DLCO), carbon monoxide transfer coefficient (KCO), total lung capacity (TLC), residual volume (RV), vital capacity (VC), inspiratory capacity (IC), expiratory reserve volume (ERV) and total resistance (R tot).
Statistical analysis
Descriptive statistics, including measures of central tendency (arithmetic mean, median and mode), measures of variability (range, interquartile range and standard deviation) and relative numbers (structure indicators), were calculated for all study variables of interest. Graphical and mathematical procedures were used to test the normality of distribution. To test the statistical hypothesis, in accordance with the type and distribution of variables, the t test, Mann‒Whitney U test, chi-square test and Fisher’s test were used. To assess the correlation between variables, Pearson’s correlation analyses or Spearman rank correlation were performed. A receiver operating characteristic (ROC) curve was used to determine cutoff values for continuous variables. To identify potential predictors of COPD, univariate and multivariate logistic regression analyses were performed. All statistical tests were executed using a significance level of P < 0.05. Analyses were performed in IBM SPSS Statistics for Windows, version 26.0 (Armonk, NY: IBM Corp., 2019). MedCalc for Windows, version 19.4 (MedCalc Software, Ostend, Belgium), was used for figure presentation.
Results
Clinical characteristics and comparison between COPD patients and healthy subjects
In this observational cohort study, 98 COPD patients (mean age 63.4 years [95% CI 62.1–65.8], male 58.2%, current smokers 35.7% [median 40 (10–100) pack/years), former smokers 64.3% [median 30 (5–100) pack/years]) were enrolled and compared to 47 healthy subjects (mean 61.7 years [95% CI 60.5–63 years], male 46.8%, current smokers 29.8%).
There were no significant differences in age, sex or smoking status between the two study groups. Serum MMP-9 and TIMP-1 levels and the MMP-9/TIMP-1 ratio were significantly higher in COPD patients than in healthy controls (p ≤ 0.001) (Table 2).
Table 2.
Demographics, MMP-9 and TIMP-1 levels and the MMP-9/TIMP-1 ratio in COPD patients and healthy controls
| COPD (n = 98) | Healthy controls (n = 47) | p | |
|---|---|---|---|
| Age, years, mean ± SDa | 63.4 ± 4.3 | 61.7 ± 4.3 | 0.123 |
| Male, n (%)b | 58.2% | 46.8% | |
| Female, n (%) | 41.8% | 53.2% | 0.199 |
| Current smokers, n (%)b | 35 (35.7%) | 14 (29.8%) | 0.489 |
| MMP-9 (ng/ml), med (95% CI)c | 848.7 (728.6–981.5) | 58.7 (47.9–76.2) | p ≤ 0.001 |
| TIMP 1 (ng/ml), med (95% CI)c | 234.7 (222.5–246.1) | 82.3 (73.0–89.7) | p ≤ 0.001 |
| MMP-9/TIMP-1 ratio, med (95% CI)c | 3.4 (2.9–4.2) | 0.40 (0.3–0.5) | p ≤ 0.001 |
SD standard deviation, MMP-9 matrix metalloproteinase 9, TIMP-1 tissue inhibitor of metalloproteinase 1
aData were compared by independent T test
bData were compared by chi-square test
cData were compared by Mann‒Whitney test
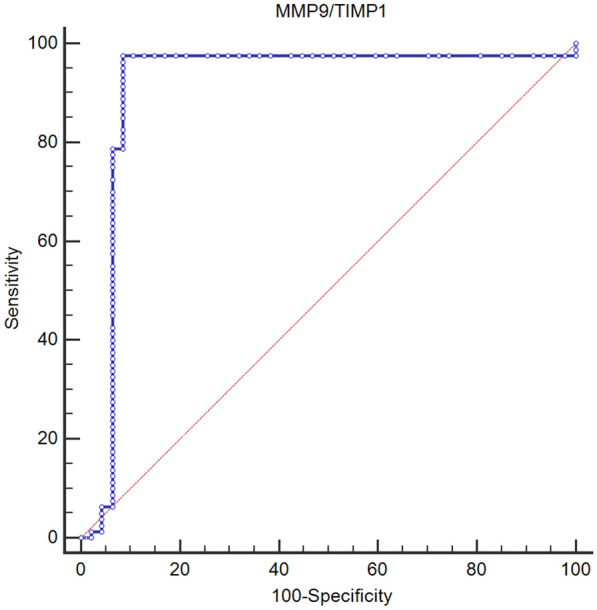
Sensitivity and specificity of MMP-9 and TIMP-1 for COPD diagnosis
The ROC curves for MMP-9, TIMP-1 and the MMP-9/TIMP-1 ratio for COPD diagnosis are presented in Table 3, with areas under the curve (AUCs) of 0.974, 0.961 and 0.910, respectively. An MMP-9 value of 612.8 ng/ml or greater was 70.0% sensitive and 100% specific for COPD diagnosis. TIMP-1 equal to or greater than 110.7 ng/ml was 100% sensitive and 81% specific for COPD diagnosis. An MMP-9/TIMP-1 ratio value of 1.16 or greater was 96% sensitive and 91% specific for COPD diagnosis (Fig. 1).
Table 3.
Areas under the curve (AUCs) for MMP-9, TIMP-1 and the MMP-9/TIMP-1 ratio for COPD diagnosis
| AUC | p | 95% CI | UL | |
|---|---|---|---|---|
| LL | ||||
| MMP-9 (ng/ml) | 0.974 | p ≤ 0.001 | 0.941 | 1.000 |
| TIMP-1(ng/ml) | 0.961 | 0.022 | 0.918 | 1.000 |
| MMP-9/TIMP-1 ratio (ng/ml) | 0.91 | p ≤ 0.001 | 0.836 | 0.984 |
AUC area under the curve, LL lower limit, UL upper limit
Fig. 1.
ROC curve for MMP-9/TIMP-1 ratio for COPD diagnosis
Association of MMP-9, TIMP-1 and MMP-9/TIMP-1 ratio with lung function, disease severity, COPD symptoms and exacerbation history
Functional and clinical characteristics of the COPD patients
The functional and clinical characteristics of the COPD patients are presented in Table 4. Of all COPD patients, 65.3% had comorbidities, and 50% had cardiovascular comorbidities. COPD patients had severe airflow limitation, impaired diffusion capacity, lung hyperinflation and elevated symptom scores (Table 4).
Table 4.
Clinical parameters in COPD patients
| n = 98 | 95% CI | ||
|---|---|---|---|
| lower CI | upper CI | ||
| AECOPD/previous year, med (IQR) | 2 (2) | 2.0 | 3.0 |
| COPD duration in years, med (IQR) | 7 (6) | 6.0 | 8.0 |
| CAT score, med (IQR) | 18.5 (14.2) | 16.0 | 20.0 |
| mMRC score, med (IQR) | 2.0 (2.0) | 2.0 | 3.0 |
| CRP, med (IQR) | 3.4 (6.2) | 2.4 | 4.6 |
| WBC (10 ^ 9/l), mean ± SD | 8.4 ± 2.6 | 7.9 | 8.9 |
| Serum neutrophils (10 ^ 9/l), mean ± SD | 5.4 ± 2.3 | 5.0 | 5.9 |
| Serum eosinophils (10 ^ 9/l), mean ± SD | 0.2 ± 0.2 | 0.2 | 0.2 |
| Serum eosinophils, (%) | 2.3 ± 1.7 | 2.0 | 2.7 |
| Serum lymphocytes (10 ^ 9/l), mean ± SD | 2.1 ± 0.8 | 1.9 | 2.3 |
| FEV1/FVC, mean ± SD | 43.7 ± 12.6 | 41.2 | 46.3 |
| Post-BD FVC% predicted, mean ± SD | 85.6 ± 19.4 | 81.7 | 89.5 |
| Post-BD FEV1% predicted, mean ± SD | 47 ± 18.6 | 43.3 | 50.8 |
| DLCO% predicted, mean ± SD | 50.1 ± 21.8 | 45.8 | 54.5 |
| KCO% predicted, mean ± SD | 60.8 ± 24.1 | 55.8 | 65.7 |
| TLC% predicted, mean ± SD | 125.5 ± 23.5 | 120.7 | 130.3 |
| RV% predicted, mean ± SD | 194.6 ± 63.4 | 181.7 | 207.6 |
| VC% predicted, mean ± SD | 91.3 ± 19.5 | 87.3 | 95.3 |
| RV% TLC predicted, mean ± SD | 146.4 ± 28.1 | 140.7 | 152.1 |
| R tot, mean ± SD | 0.6 ± 0.3 | 0.5 | 0.6 |
| IC% predicted, mean ± SD | 85.1 ± 30 | 79.0 | 91.3 |
| ERV% predicted, mean ± SD | 112.0 (66.0) | 97.9 | 121.4 |
Data are expressed as the mean ± SD, n (%) or med (95% CI)
BD bronchodilator, AECOPD acute exacerbation of chronic obstructive disease, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, DLCO diffusion capacity for carbon monoxide (CO), KCO carbon monoxide transfer coefficient, TLC total lung capacity, RV residual volume, VC vital capacity, IC inspiratory capacity, ERV expiratory reserve volume, R tot total resistance, WBC count white blood cell count, CRP C-reactive protein, CAT COPD Assessment Test, MMP-9 matrix metalloproteinase 9, TIMP-1 tissue inhibitor of metalloproteinase 1
Association of MMP-9, TIMP-1 and the MMP-9/TIMP-1 ratio with lung function, COPD symptoms and CBC
Negative correlations were identified between MMP-9, the MMP-9/TIMP-1 ratio and the following post-BD spirometry and body plethysmography parameters: FVC, FEV1, FEV1/FVC, VC and IC (Table 5). Positive correlations were identified between both MMP-9 and the MMP-9/TIMP-1 ratio with RV and RV% TLC (Table 5). No correlation was found between serum TIMP-1 and any lung function parameter.
Table 5.
Correlation of MMP-9, TIMP-1, and MMP-9/TIMP-1 ratio with lung function, clinical and CBC parameters
| MMP-9 | TIMP-1 | MMP-9/TIMP-1 | ||||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| FEV1/FVC | − 0.308 | 0.005 | − 0.085 | 0.456 | − 0.330 | 0.003 |
| FVC (%) pred | − 0.294 | 0.008 | − 0.043 | 0.704 | − 0.282 | 0.011 |
| FEV1 (%) pred | − 0.367 | p ≤ 0.001 | − 0.054 | 0.636 | − 0.392 | p ≤ 0.001 |
| DLCO (%) pred | − 0.154 | 0.172 | − 0.117 | 0.302 | − 0.153 | 0.175 |
| TLC (%) pred | 0.012 | 0.918 | − 0.119 | 0.293 | 0.105 | 0.355 |
| RV (%) pred | 0.220 | 0.050 | − 0.031 | 0.786 | 0.277 | 0.013 |
| VC (%) pred | − 0.323 | 0.003 | − 0.152 | 0.178 | − 0.263 | 0.018 |
| RV% TLC pred | 0.308 | 0.005 | 0.015 | 0.895 | 0.335 | 0.002 |
| IC (%) pred | − 0.359 | p ≤ 0.001 | − 0.148 | 0.189 | − 0.291 | 0.009 |
| BMI (kg/m2) | 0.157 | 0.164 | 0.289 | 0.009 | 0.043 | 0.703 |
| CRP (mg/l) | 0.301 | 0.007 | 0.370 | 0.001 | 0.164 | 0.148 |
| WBC (10 ^ 9/l) | 0.462 | p ≤ 0.001 | 0.293 | 0.009 | 0.339 | 0.002 |
| Ne (10 ^ 9/l) | 0.478 | p ≤ 0.001 | 0.346 | 0.002 | 0.322 | 0.004 |
| Ne (%) | 0.315 | 0.005 | 0.225 | 0.046 | 0.194 | 0.086 |
| Eo (10 ^ 9/l) | 0.016 | 0.890 | 0.007 | 0.949 | 0.045 | 0.698 |
| Eo (%) | − 0.140 | 0.222 | − 0.175 | 0.125 | −0.038 | 0.743 |
| Hgb (g/l) | 0.352 | 0.002 | 0.263 | 0.020 | 0.243 | 0.032 |
| CAT | 0.273 | 0.014 | 0.053 | 0.641 | 0.312 | 0.005 |
| mMRC | 0.288 | 0.010 | 0.103 | 0.365 | 0.281 | 0.011 |
FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, DLCO diffusion capacity for carbon monoxide (CO), KCO carbon monoxide transfer coefficient, TLC total lung capacity, RV residual volume, VC vital capacity, IC inspiratory capacity, ERV expiratory reserve volume, R tot total resistance, WBC count white blood cell count, CRP C- reactive protein, Ne absolute neutrophil count, Hgb hemoglobin, CAT COPD Assessment Test, mMRC modified Medical Research Council, MMP-9 matrix metalloproteinase 9, TIMP-1 tissue inhibitor of metalloproteinase 1
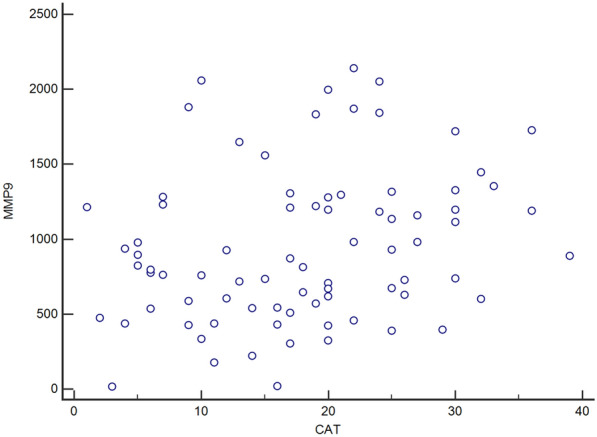
No statistically significant correlation between MMP-9, TIMP-1, the MMP-9/TIMP-1 ratio and diffusion capacity for carbon monoxide (DLCO) or transfer coefficient for carbon monoxide (KCO) was found (Table 5). CAT and mMRC scores were positively associated with MMP-9 and the MMP-9/TIMP-1 ratio (Fig. 2). MMP-9 and TIMP-1 were positively associated with CRP. MMP-9, TIMP-1 and the MMP-9/TIMP-1 ratio were positively associated with leukocytes, absolute neutrophil count and hemoglobin levels.
Fig. 2.
Correlation of MMP-9 with CAT
Association of MMP-9, TIMP-1 and the MMP-9/TIMP-1 ratio with disease severity and exacerbation history
Both MMP-9 and the MMP-9/TIMP-1 ratio were statistically greater in COPD patients in GOLD stages 3 and 4 (p = 0.003; p ≤ 0.001) and were also higher in the patients with AECOPD ≥ 2 but failed to reach statistical significance (Table 6).
Table 6.
MMP-9, TIMP-1, and the MMP-9/TIMP-1 ratio according to GOLD stages and number of AECOPD (events/year)
| GOLD 1 and 2 N = 40 | GOLD 3 and 4 N = 58 | p | Exacerbations < 2 N = 41 | Exacerbations ≥ 2 N = 57 | p | |
|---|---|---|---|---|---|---|
| MMP-9 (ng/ml), med (95% CI)b | 596.8 (437.9–761.5) | 980 (825.5–1195.6) | 0.003 | 778.5 (540.6–981.5) | 892.3 (728.6–1188.9) | 0.196 |
| TIMP-1(ng/ml), med (95% CI)b | 223.9 (208–245.2) | 238.9 (228.9–249.3) | 0.552 | 222.7 (198.9–253.9) | 236.6 (228.9–248.4) | 0.669 |
| MMP-9/TIMP-1b ratio (ng/ml), med (95% CI) | 2.4 (2–3.2) | 4.2 (3.3–5) | p ≤ 0.001 | 3.2 (2.4–4.8) | 3.5 (3.1–4.6) | 0.222 |
aData were compared by independent t test
bData were compared by Mann‒Whitney test
Association of MMP-9, TIMP-1 and the MMP-9/TIMP-1 ratio with inhalation therapy
Triple therapy consisting of a fixed-dose combination inhaler containing an inhaled corticosteroid and long-acting beta2 agonist (ICS/LABA) and a long-acting muscarinic antagonist inhaler (LAMA) was reported by 65 subjects (63.7%). Bronchodilator therapy was reported by 33 subjects (32.3%). Bronchodilators included LAMA monotherapy (11.8%), LABA monotherapy (0.9%), LAMA plus LABA inhalers (16.7%) and short-acting beta2 agonist (SABA) (2.9%). COPD patients receiving ICS/LABA and LAMA triple therapy had higher serum MMP-9 (958.7 ng/ml [95% CI 737.3–1198.6]) and a higher MMP-9/TIMP-1 ratio (3.8 [95% CI 3.1–5]) compared with COPD patients receiving bronchodilator therapy (MMP-9, 726.7 ng/ml [95% CI 473.7–889.4]; MMP-9/TIMP-1 ratio, 3 [95% CI 2.1–3.4]). The difference, however, neared statistical significance for MMP-9 (P = 0.063) and the MMP-9/TIMP-1 ratio (p = 0.098) for both treatment groups.
MMP-9/TIMP-1 as a predictor for COPD diagnosis and COPD severity
Logistic regression analysis for COPD diagnosis prediction (no COPD versus COPD) adjusted for age and sex identified the MMP-9/TIMP-1 ratio as a significant predictor for COPD presence (Table 7). When we analyzed predictors for COPD severity according to GOLD criteria (COPD GOLD I + II versus COPD GOLD III + IV), the MMP-9/TIMP-1 ratio was a significant predictor of severe COPD and remained significant after adjustment for age, sex and AECOPD (Table 8).
Table 7.
MMP-9/TIMP-1 ratio as a predictor for COPD diagnosis
| B | OR | 95% CI for OR | p | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| MMP-9/TIMP-1 | 0.664 | 1.943 | 1.481 | 2.551 | < 0.001 |
| Sex | − 0.341 | 0.711 | 0.3 | 1.681 | 0.437 |
| Age (years) | 0.051 | 1.053 | 0.987 | 1.123 | 0.118 |
| Constant | − 3.678 | 0.025 | 0.092 | ||
Table 8.
MMP-9/TIMP-1 as a predictor of COPD severity
| B | OR | 95% CI for OR | p | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Exacerbations ≥ 2 | − 0.5 | 0.607 | 0.212 | 1.739 | 0.353 |
| MMP-9/TIMP-1 | 0.375 | 1.456 | 1.086 | 1.951 | 0.012 |
| Sex | 0.139 | 1.150 | 0.415 | 3.183 | 0.788 |
| Age (years) | 0.018 | 1.018 | 0.958 | 1.081 | 0.566 |
| Constant | − 1.732 | 0.177 | 0.46 | ||
Discussion
Chronic exposure to tobacco smoke causes oxidative stress and airway inflammation, resulting in deregulation of protease activity, extracellular matrix degradation, progressive alveolar destruction and airway remodeling with significant functional impairment and irreversible loss of lung function. Airway remodeling includes structural changes caused by repeated injury and repair processes and longstanding airway inflammation [25]. Such deregulation is a hallmark of COPD pathogenesis [26].
Our study is the first to examine serum MMP-9, TIMP-1 and the MMP-9/TIMP-1 ratio for their predictive value for the presence of COPD and to assess the relationship with the full range of functional lung parameters obtained by spirometry, single breath diffusion capacity for CO, body plethysmography and clinical COPD indicators.
We found that serum values of MMP-9 and TIMP-1 and the MMP-9/TIMP-1 ratio were significantly higher in COPD patients than in healthy controls. This suggests protease/antiprotease deregulation and increased proteolytic activity in COPD patients. Similar results were presented in a meta-analysis published by Li and coworkers that included twenty relevant studies of a total of 923 COPD patients and 641 healthy controls (serum MMP-9 and TIMP-1 values were greater in COPD patients than in healthy controls) [27]. In the study by Gilowska and coauthors, COPD patients were predisposed to synthesize more MMP-9 and MMP-9/TIMP-1 complexes than healthy controls, most likely due to the diseased lung environment rather than to genetic features of the MMP-9 gene [28]. The study by Linder and coworkers found greater MMP-9 values in COPD patients and a significant correlation with productive cough and decreased FEV1, consistent with our findings [29]. Ilumets and coworkers demonstrated that MMP-9 levels did not change with age but were elevated in smokers and COPD patients compared to nonsmokers, providing a clear link to cigarette smoke-induced lung remodeling and COPD [30]. In a study by Piesiak and coworkers, serum MMP-9 and TIMP-1 levels were higher in COPD patients than in healthy controls, and both biomarkers correlated with CRP level and FEV1, which corresponds to the findings of our study [31]. However, serum MMP-9 levels and the MMP-9/TIMP-1 ratio seem to be associated with COPD. Several studies that investigated the potential role of MMP-9 in COPD demonstrated elevated MMP-9 in systemic and local compartments other than serum: sputum [32, 33], bronchoalveolar lavage fluid (BALF) [34] and plasma [35, 36]. The potential role of MMP-9 was assessed according to disease state, either stable or AECOPD. In a study by Wells and coworkers, an elevated plasma MMP-9 level was independently associated with AECOPD risk [37], and Stanojkovic and coworkers demonstrated that oxidant/antioxidant imbalance was significantly pronounced in patients with COPD exacerbation [38].
In the current study, we found the areas under the receiver operating characteristic curves for MMP-9, TIMP-1 and the MMP-9/TIMP-1 ratio for COPD diagnosis to be 0.974, 0.961 and 0.910, respectively. These results suggest that serum-based MMP-9 biomarkers add additional value to clinical characteristics predicting COPD.
Furthermore, we evaluated the association of MMP-9 and TIMP-1 with lung function parameters and found a negative correlation between serum MMP-9 level and the MMP-9/TIMP-1 ratio and the spirometric parameters FEV1/FVC ratio, FVC and FEV1. We failed to find a correlation between serum TIMP-1 and any lung function parameter. In a study by Ólafsdottir and coworkers, lower FEV1 values correlated with increased serum levels of MMP-9, MMP-9/TIMP-1 ratio and TIMP-1 [39]. The explanation could be related to the age of participants (888 participants over 70 years of age) and the fact that serum TIMP-1 level is age dependent. A negative correlation between MMP-9 and FEV1 has also been identified in the lung parenchyma in COPD patients [40] and airway secretions (sputum and BAL), as mentioned above. This suggests that serum MMP-9 and an increased MMP-9/TIMP 1 ratio are associated with airway dysfunction severity. In our study, MMP-9 increased significantly with the severity of airway obstruction, and TIMP-1 changed slightly, suggesting an imbalance between proteases and protease inhibitors culminating in enhanced proteolytic activity and indicating the importance of the MMP-9/TIMP-1 ratio as a potential biomarker in airway remodeling and COPD development.
Diffusion capacity for CO (DLCO) is considered a useful tool to assess emphysema severity. DLCO was significantly higher in COPD patients with lower GOLD stages (I and II) than in those with higher GOLD stages (III and IV). These results suggest that COPD patients with greater airway obstruction and higher GOLD stages had greater diffusion capacity impairment, indicating emphysema. However, we failed to substantiate our initial assumption that MMP-9, due to its role in ECM turnover, would correlate with DLCO as a functional measure of emphysema. Similarly, Beeh and colleagues demonstrated that both MMP-9 and TIMP-1 were elevated in COPD patient sputum, and MMP-9 negatively correlated with airway obstruction but not with either diffusion capacity or vital capacity [41]. Additionally, Papakonstantinou and colleagues demonstrated that MMPs and TIMPs failed to correlate with DLCO [42]. In the study by D’Armiento and coworkers, changes in MMP levels in plasma and bronchoalveolar lavage fluid correlated poorly with parameters of disease severity or progression, although they were greater in patients with emphysema [43]. Tsay and colleagues reported that serum MMP levels provided minimal additional information to improve the detection of mild emphysema [44]. Therefore, it is possible that the role of MMP-9 in the pathophysiology of COPD is more complex than previously considered and not only related to the development of emphysema.
In our study, circulating leukocytes and neutrophils positively correlated with serum MMP-9 and TIMP-1 levels and the MMP-9/TIMP-1 ratio and positively correlated with the number of AECOPD events. Sniteker and coworkers identified an increased correlation between MMP-9 and WBC count in smokers, supporting the theory that leukocytes are a potential source of circulating MMP-9 in vivo and that smoking affects the levels of both [45].
In the present study, triple therapy was the therapy of choice for patients with the most pronounced airway limitation and COPD symptoms. COPD patients on ICS/LABA + LAMA triple therapy had higher serum MMP-9 levels and a higher MMP-9/TIMP-1 ratio. In a study by Vlahos and coworkers, MMP-9 activity was elevated in severe COPD, closely related to neutrophilic inflammation, and in vivo, neutrophil activation was associated with glucocorticoid refractory release of MMP-9 [46] It is tempting to speculate that higher serum MMP-9 levels and a greater MMP-9/TIMP-1 ratio in patients with triple therapy is related to advanced disease and more exacerbations, but it is potentially an altered response to glucocorticoids.
COPD patients had a greater number of symptoms and more pronounced dyspnea as determined by mMRC and CAT. We found a significant association between MMP-9, the MMP-9/TIMP-1 ratio and mMRC and CAT scores but not with the number of recorded AECOPD cases in the previous year. Taking everything into consideration, it is possible that COPD patients with more stable phenotypes, who are not frequent exacerbators but experience increased dyspnea and symptom burden, exhibit greater proteolytic activity.
There are a few limitations to our study. First, ELISA was used to measure both total and pro-MMP-9. Therefore, it is possible that increased serum MMP-9 was not necessarily related to increased activity. Second, as blood samples were collected once, long-term elevation of serum MMP-9 cannot be substantiated. Third, the effects of serum MMP-9 and TIMP-1 reflect systemic features. We did not perform simultaneous analysis of MMP-9 and TIMP-1 in airway secretions as a reflection of the local compartment. The latter could potentially provide a more comprehensive assessment and should be the subject of future studies.
Conclusion
COPD patients have elevated serum levels of MMP-9 and TIMP-1 and MMP-9/TIMP-1 ratio. COPD patients have an imbalance between MMP-9 and TIMP-1 in favor of a pro-proteolytic environment, which overall indicates the importance of the MMP-9/TIMP-1 ratio as a potential biomarker for COPD diagnosis and severity.
Acknowledgements
We would like to express gratitude to our colleague Igor Barjaktarevic, MD, PhD, for his valuable and constructive suggestions during the development of this research work. We are grateful to Sanja Jelic and Djurdjica Maravic-Tomic for their excellent support with blood sampling. This work was supported by the Ministry of Education, Science and Technological Development of Serbia (contract no. 451-03-68/2020-14/200161), the Respiratory Society of Serbia and the Respiratory Educational Center.
Abbreviations
- COPD
Chronic obstructive pulmonary disease
- MMP-9
Matrix metalloproteinase-9
- TIMP-1
Tissue inhibitor of metalloproteinase-1
- ECM
Extracellular matrix
- GOLD
Global Initiative for Chronic Obstructive Disease
- ELISA
Enzyme-linked immunosorbent assay
- EFL
Expiratory flow limitation
- AECOPD
Acute exacerbation of chronic obstructive pulmonary disease
- mMRC
Modified Medical Research Council Dyspnea Scale
- CAT
COPD Assessment Test
- FEV1
Forced expiratory volume in 1 second
- FVC
Forced vital capacity
- DLCO
Diffusion capacity for carbon monoxide
- KCO
Carbon monoxide transfer coefficient
- TLC
Total lung capacity
- RV
Residual volume
- VC
Vital capacity
- IC
Inspiratory capacity
- ERV
Expiratory reserve volume
- R tot
Total resistance
- CRP
C-reactive protein
- LAMA
Long-acting muscarinic antagonist
- IC
Inhaled corticosteroid
- LABA
Long-acting beta2 agonist
- BALF
Bronchoalveolar lavage fluid
Author contributions
SDJ contributed to the concept, design, supervision, resources, materials, data collection and processing, analysis, literature search, writing manuscript, and critical review; MAH and DG contributed to the literature search, writing manuscript, and critical review; BM, MS, SP and JJ contributed to the concept, design, resources, materials, data collection, and critical review; JKS and MM contributed to the design, data collection and processing, analysis, and critical review; JML, NDJ, DM, and IM contributed to the data collection and processing, analysis, and critical review; all authors read and approved the final manuscript.
Funding
This study received no external funding.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of University Clinical Center of Serbia (No. 81/22; the 24th of March 2016). Informed written consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Eur Respir J. 2017;49:3. doi: 10.1183/13993003.00214-2017. [DOI] [PubMed] [Google Scholar]
- 2.Barnes PJ. Cellular and molecular mechanisms of chronic obstructive pulmonary disease. Clin Chest Med. 2014;35(1):71–86. doi: 10.1016/j.ccm.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Löffek S, Schilling O, Franzke CW. Biological role of matrix metalloproteinases: a critical balance. Eur Respir J. 2011;38(1):191–208. doi: 10.1183/09031936.00146510. [DOI] [PubMed] [Google Scholar]
- 4.Starr AE, Dufour A, Maier J, Overall CM. Biochemical analysis of matrix metalloproteinase activation of chemokines CCL15 and CCL23 and increased glycosaminoglycan binding of CCL16. J Biol Chem. 2012;287(8):5848–5860. doi: 10.1074/jbc.M111.314609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Young D, Das N, Anowai A, Dufour A. Matrix metalloproteases as influencers of the cells’ social media. Int J Mol Sci. 2019;20:16. doi: 10.3390/ijms20163847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jasper AE, McIver WJ, Sapey E, Walton GM. Understanding the role of neutrophils in chronic inflammatory airway disease. F1000Res. 2019;8:557. doi: 10.12688/f1000research.18411.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu X, Jackson PL, Tanner S, Hardison MT, Roda MA, Blalock JE, et al. A self-propagating matrix metalloprotease-9 (MMP-9) dependent cycle of chronic neutrophilic inflammation. PLoS ONE. 2011;6(1):e15781. doi: 10.1371/journal.pone.0015781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D W, T S, J D. Collagenolytic matrix metalloproteinases in chronic obstructive lung disease and cancer. Cancers. 2015;7(1):329–41. doi: 10.3390/cancers7010329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murthy S, Ryan A, He C, Mallampalli RK, Carter AB. Rac1-mediated mitochondrial H2O2 generation regulates MMP-9 gene expression in macrophages via inhibition of SP-1 and AP-1. J Biol Chem. 2010;285(32):25062–25073. doi: 10.1074/jbc.M109.099655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murthy S, Ryan AJ, Carter AB. SP-1 regulation of MMP-9 expression requires serine-586 in the PEST domain. Biochem J. 2012;445(2):229–236. doi: 10.1042/BJ20120053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vandooren J, den Steen PEV, Opdenakker G. Biochemistry and molecular biology of gelatinase B or matrix metalloproteinase-9 (MMP-9): the next decade. Crit Rev Biochem Mol Biol. 2013;48(3):222–272. doi: 10.3109/10409238.2013.770819. [DOI] [PubMed] [Google Scholar]
- 12.Owen CA. Proteinases and oxidants as targets in the treatment of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005;2(4):373–385. doi: 10.1513/pats.200504-029SR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ra HJ, Parks WC. Control of matrix metalloproteinase catalytic activity. Matrix Biol. 2007;26(8):587–596. doi: 10.1016/j.matbio.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Donnell DE, Webb KA, Neder JA. Lung hyperinflation in COPD: applying physiology to clinical practice. COPD Res Pract. 2015;1(1):4. doi: 10.1186/s40749-015-0008-8. [DOI] [Google Scholar]
- 15.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 16.Gagnon P, Guenette JA, Langer D, Laviolette L, Mainguy V, Maltais F, et al. Pathogenesis of hyperinflation in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;15(9):187–201. doi: 10.2147/COPD.S38934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barjaktarevic I, Springmeyer S, Gonzalez X, Sirokman W, Coxson HO, Cooper CB. Diffusing capacity for carbon monoxide correlates best with tissue volume from quantitative CT scanning analysis. Chest. 2015;147(6):1485–1493. doi: 10.1378/chest.14-1693. [DOI] [PubMed] [Google Scholar]
- 18.Milenkovic B, Dimic-Janjic S, Kotur-Stevuljevic J, Kopitovic I, Jankovic J, Stjepanovic M, et al. Validation of serbian version of chronic obstructive pulmonary disease assessment test. VSP. 2020;77(3):294–299. doi: 10.2298/VSP180220094M. [DOI] [Google Scholar]
- 19.Miravitlles M, Calle M, Soler-Cataluña JJ. Clinical phenotypes of COPD: identification, definition and implications for guidelines. Arch Bronconeumol. 2012;48(3):86–98. doi: 10.1016/j.arbres.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 20.NHIS - Adult Tobacco Use - Glossary. 2019. https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm
- 21.Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 22.Celli BR, MacNee W, Agusti A, Anzueto A, Berg B, Buist AS, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932–946. doi: 10.1183/09031936.04.00014304. [DOI] [PubMed] [Google Scholar]
- 23.Graham BL, Brusasco V, Burgos F, Cooper BG, Jensen R, Kendrick A, et al. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J. 2017;49(1):1600016. doi: 10.1183/13993003.00016-2016. [DOI] [PubMed] [Google Scholar]
- 24.MacIntyre N, Crapo RO, Viegi G, Johnson DC, van der Grinten CPM, Brusasco V, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26(4):720–735. doi: 10.1183/09031936.05.00034905. [DOI] [PubMed] [Google Scholar]
- 25.Hirota N, Martin JG. Mechanisms of airway remodeling. Chest. 2013;144(3):1026–1032. doi: 10.1378/chest.12-3073. [DOI] [PubMed] [Google Scholar]
- 26.Fischer BM, Pavlisko E, Voynow JA. Pathogenic triad in COPD: oxidative stress, protease–antiprotease imbalance, and inflammation. Int J Chron Obstruct Pulmon Dis. 2011;6:413–421. doi: 10.2147/COPD.S10770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Y, Lu Y, Zhao Z, Wang J, Li J, Wang W, et al. Relationships of MMP-9 and TIMP-1 proteins with chronic obstructive pulmonary disease risk: a systematic review and meta-analysis. J Res Med Sci. 2016 doi: 10.4103/1735-1995.178737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gilowska I, Kasper Ł, Bogacz K, Szczegielniak J, Szymasek T, Kasper M, et al. Impact of matrix metalloproteinase 9 on COPD development in polish patients: genetic polymorphism, protein level, and their relationship with lung function. BioMed Res Int. 2018 doi: 10.1155/2018/6417415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Linder R, Rönmark E, Pourazar J, Behndig A, Blomberg A, Lindberg A. Serum metalloproteinase-9 is related to COPD severity and symptoms—cross-sectional data from a population based cohort-study. Respir Res. 2015;16(1):28. doi: 10.1186/s12931-015-0188-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ilumets H, Mazur W, Toljamo T, Louhelainen N, Nieminen P, Kobayashi H, et al. Ageing and smoking contribute to plasma surfactant proteins and protease imbalance with correlations to airway obstruction. BMC Pulm Med. 2011;11(1):19. doi: 10.1186/1471-2466-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Piesiak P, Brzecka A, Kosacka M, Passowicz-Muszyńska E, Dyła T, Jankowska R. Concentrations of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinases-1 in serum of patients with chronic obstructive pulmonary disease. Pol Merkur Lekarski. 2011;31(185):270–273. [PubMed] [Google Scholar]
- 32.Mercer P, Shute J, Bhowmik A, Donaldson G, Wedzicha J, Warner J. MMP-9, TIMP-1 and inflammatory cells in sputum from COPD patients during exacerbation. Respir Res. 2005;6(1):151. doi: 10.1186/1465-9921-6-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Esa SA, Rawy AM, El-Behissy MM, Kamel MH, El-Hwaitty HMMM. Study of the level of sputum matrix metalloproteinase-9 (MMP-9) and tissue inhibitor metalloproteinase-1 (TIMP-1) in COPD patients. Egypt J Chest Dis Tubercul. 2014;63(4):861–7. doi: 10.1016/j.ejcdt.2014.06.014. [DOI] [Google Scholar]
- 34.Ostridge K, Williams N, Kim V, Bennett M, Harden S, Welch L, et al. Relationship between pulmonary matrix metalloproteinases and quantitative CT markers of small airways disease and emphysema in COPD. Thorax. 2016;71(2):126–132. doi: 10.1136/thoraxjnl-2015-207428. [DOI] [PubMed] [Google Scholar]
- 35.Sng JJ, Prazakova S, Thomas PS, Herbert C. MMP-8, MMP-9 and neutrophil elastase in peripheral blood and exhaled breath condensate in COPD. COPD J Chronic Obstr Pulm Dis. 2017;14(2):238–44. doi: 10.1080/15412555.2016.1249790. [DOI] [PubMed] [Google Scholar]
- 36.Hk K, Y H, Mn L, Jj Y, Wj K. Relationship between plasma matrix metalloproteinase levels, pulmonary function, bronchodilator response, and emphysema severity. Int J Chron Obstruct Pulmon Dis. 2016;11:1129–37. doi: 10.2147/COPD.S103281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wells JM, Parker MM, Oster RA, Bowler RP, Dransfield MT, Bhatt SP, et al. Elevated circulating MMP-9 is linked to increased COPD exacerbation risk in SPIROMICS and COPDGene. JCI Insight. 2018;3:22. doi: 10.1172/jci.insight.123614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stanojkovic I, Kotur-Stevuljevic J, Milenkovic B, Spasic S, Vujic T, Stefanovic A, et al. Pulmonary function, oxidative stress and inflammatory markers in severe COPD exacerbation. Respir Med. 2011;105(Suppl 1):S31–37. doi: 10.1016/S0954-6111(11)70008-7. [DOI] [PubMed] [Google Scholar]
- 39.Ólafsdóttir IS, Janson C, Lind L, Hulthe J, Gunnbjörnsdóttir M, Sundström J. Serum levels of matrix metalloproteinase-9, tissue inhibitors of metalloproteinase-1 and their ratio are associated with impaired lung function in the elderly: a population-based study. Respirology. 2010;15(3):530–535. doi: 10.1111/j.1440-1843.2010.01718.x. [DOI] [PubMed] [Google Scholar]
- 40.Kang MJ, Oh YM, Lee JC, Kim DG, Park MJ, Lee MG, et al. Lung matrix metalloproteinase-9 correlates with cigarette smoking and obstruction of airflow. J Korean Med Sci. 2003;18(6):821–827. doi: 10.3346/jkms.2003.18.6.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beeh KM, Beier J, Kornmann O, Buhl R. Sputum matrix metalloproteinase-9, tissue inhibitor of metalloprotinease-1, and their molar ratio in patients with chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis and healthy subjects. Respir Med. 2003;97(6):634–639. doi: 10.1053/rmed.2003.1493. [DOI] [PubMed] [Google Scholar]
- 42.Papakonstantinou E, Klagas I, Karakiulakis G, Prince SS, Roth M, Tamm M, et al. Activation of MMP-9 in BAL is increased in COPD exacerbation independently of smoking, lung function, microbiology and treatment. Eur Respir J. 2014;44:58. [Google Scholar]
- 43.D’Armiento JM, Goldklang MP, Hardigan AA, Geraghty P, Roth MD, Connett JE, et al. Increased matrix metalloproteinase (MMPs) levels do not predict disease severity or progression in emphysema. PLoS ONE. 2013;8:2. doi: 10.1371/journal.pone.0056352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tsay JCJ, Hu Y, Goldberg JD, Wang B, Vijayalekshmy S, Yie TA, et al. Value of metalloproteinases in predicting COPD in heavy urban smokers. Respir Res. 2020;21(1):228. doi: 10.1186/s12931-020-01496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Snitker S, Xie K, Ryan KA, Yu D, Shuldiner AR, Mitchell BD, et al. Correlation of circulating MMP-9 with white blood cell count in humans: effect of smoking. PLoS ONE. 2013;8(6):e66277. doi: 10.1371/journal.pone.0066277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vlahos R, Wark PAB, Anderson GP, Bozinovski S. Glucocorticosteroids differentially regulate MMP-9 and neutrophil elastase in COPD. PLoS ONE. 2012;7(3):e33277. doi: 10.1371/journal.pone.0033277. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


