ABSTRACT
Immunocompetent adults with certain medical and behavioral factors are at increased risk of pneumococcal disease. In some countries, sequential vaccination with 13-valent pneumococcal conjugate vaccine (PCV13) followed by 23-valent pneumococcal polysaccharide vaccine (PPSV23) is recommended for at-risk adults. This subgroup analysis from a phase 3 study evaluated the safety, tolerability, and immunogenicity of sequential administration of either V114 (a 15-valent PCV containing serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, 22F, 23F, and 33F) or PCV13, followed 6 months later by PPSV23, in immunocompetent adults 18–49 years of age with pre-defined risk factors for pneumococcal disease. Safety and immunogenicity post-vaccination were analyzed by type and baseline number of risk factors for pneumococcal disease (1 and ≥2 risk factors). This analysis included 1,131 participants randomized 3:1 to receive either V114 or PCV13, followed by PPSV23. The majority (73.1%) of participants had at least one risk factor. Safety and tolerability profiles of V114 and PCV13 were similar across risk factor groups. V114 administered either alone or sequentially with PPSV23 6 months later was immunogenic for all 15 serotypes, including those not contained in PCV13, regardless of the number of baseline risk factors. V114 has the potential to broaden serotype coverage for at-risk adults.
KEYWORDS: Pneumococcal vaccine, V114, 15-valent PCV, PCV13, PPSV23, at-risk adults
Introduction
The risk of pneumococcal disease is increased in individuals with chronic health conditions (e.g., chronic heart, liver, and lung disease, and diabetes mellitus) and certain behavioral habits (e.g., cigarette smoking and alcoholism).1–3 The clinical sequelae of, and some therapies used to manage, these chronic conditions are thought to be associated with immune impairment, which may result in decreased resistance to infections.2,4–6 The presence of risk factors has also been shown to be a predictor of hospitalization and mortality.1,2,7–10
Immunocompetent individuals with one or more risk factors for pneumococcal disease are classified as “at risk,” in contrast to immunocompromised individuals who are considered “high risk.”1,3 Accumulation of concurrent at-risk conditions (risk stacking) in immunocompetent individuals is associated with a higher incidence of pneumococcal disease,1,2,10–13 approaching rates seen in immunocompromised individuals.1,12,14 Furthermore, socioeconomic inequities in disadvantaged communities can also contribute to an increased burden of pneumococcal disease.15,16
Pneumococcal vaccines are included in many adult national immunization programs, with the goal of providing protection against the serotypes most frequently associated with severe pneumococcal disease.17 National guidelines on pneumococcal immunization of at-risk individuals vary by country and include two classes of vaccine: pneumococcal conjugate vaccines (PCVs) and pneumococcal polysaccharide vaccines.18,19 The 23-valent pneumococcal polysaccharide vaccine (PPSV23) contains the 23 serotypes responsible for causing up to 90% of invasive pneumococcal infections in industrialized countries and is indicated for adults ≥50 years of age and persons ≥2 years of age at increased risk of pneumococcal disease.3,17,18,20 The 13-valent pneumococcal conjugate vaccine (PCV13) contains 13 serotypes and is indicated for persons ≥6 weeks of age.21
With the widespread use of pneumococcal vaccines in immunization schedules, rates of invasive pneumococcal disease (IPD) caused by non-PCV serotypes have increased,22–25 as have associated morbidity, mortality, and healthcare costs, particularly in at-risk individuals,26 which highlights a need for new PCVs with broader serotype coverage.
V114 (VAXNEUVANCE™, Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA [MSD]) is a 15-valent PCV that contains the 13 serotypes in PCV13 in addition to 22F and 33F, two epidemiologically significant serotypes that cause IPD. Based on safety and immunogenicity data from phase 3 clinical trials,27–29 V114 was approved for use in the United States and the European Union in 2021 for the prevention of pneumococcal disease in adults ≥18 years of age.30,31 The Advisory Committee on Immunization Practices (ACIP) recommends vaccination with either V114 followed by PPSV23 ≥ 1 years later or a single dose of 20-valent pneumococcal conjugate vaccine (PCV20) for adults ≥19 years of age with certain underlying medical conditions or other risk factors.32
Immune responses to vaccination vary substantially based on host factors; the presence of comorbidities or certain behavioral factors, such as smoking or alcohol consumption, may have implications for the protective effect provided by vaccines.33 In this subgroup analysis of the descriptive V114–017 phase 3 study, we assessed the safety, tolerability, and immunogenicity of V114 and PCV13 administered on Day 1, and PPSV23 6 months later, based on the number and type of pre-defined risk factors for pneumococcal disease in immunocompetent adults 18–49 years of age.
Methods
Study design
Details of the study design have been previously described.29 This phase 3 trial evaluated the safety, tolerability, and immunogenicity of V114 compared with those of PCV13 in pneumococcal vaccine-naïve immunocompetent adults 18–49 years of age with or without risk factors for pneumococcal disease (Protocol V114–017; NCT03547167 and EudraCT 2017–004915–38). Participants were randomized in a 3:1 ratio to receive a single dose of V114 or PCV13 on Day 1, followed by a single dose of PPSV23 at Month 6. This study was descriptive and was conducted between July 2018 and July 2020 at 79 sites worldwide (the full lists of study sites and investigators are described in Hammitt et al.).29 The study protocol and any amendments, information provided to participants, and any recruitment materials were reviewed and approved by the appropriate institutional review boards and regulatory agencies. Written informed consent was obtained from each participant prior to any study procedure.
Participants
For this subgroup analysis, immunocompetent adults 18–49 years of age with one or more risk factors for pneumococcal disease were eligible for the study if they were verified as pneumococcal vaccine-naïve by medical history and record review (Table 1). Protocol-defined inclusion criteria had to be met for the risk factors of diabetes mellitus, chronic liver disease, chronic lung disease, chronic heart disease, alcohol use disorder, and current tobacco use (Supplemental Table S1).
Table 1.
Subgroup analysis inclusion and exclusion criteria.
| Inclusion criteria | |
| |
| Key exclusion criteria | |
| |
| |
| |
| |
|
Further details on eligibility criteria can be found in Supplemental Table S1.
AUDIT-C: Alcohol Use Disorder Identification Test – Consumption; COPD: chronic obstructive pulmonary disease; FEV1: forced expiratory volume in 1 second; FVC: forced vital capacity; GOLD: Global Initiative for Chronic Obstructive Lung Disease; HbA1c: glycated hemoglobin; NYHA: New York Heart Association.
Vaccines and administration
V114 (VAXNEUVANCE™, MSD) is a 15-valent PCV. Each 0.5 mL dose contains 2 µg of pneumococcal capsular polysaccharide from serotypes 1, 3, 4, 5, 6A, 7F, 9V, 14, 18C, 19A, 19F, 23F, 22F, and 33F, and 4 µg of serotype 6B, all conjugated to CRM197 carrier protein and adjuvanted with 125 µg aluminum phosphate.
PCV13 (Prevnar 13©, Wyeth LLC, marketed by Pfizer, New York, NY, USA) is a 13-valent PCV. Each 0.5 mL dose contains 2.2 µg of pneumococcal capsular polysaccharide from serotypes 1, 3, 4, 5, 6A, 7F, 9V, 14, 18C, 19A, 19F, and 23F, and 4.4 µg of serotype 6B, all conjugated to CRM197 carrier protein and adjuvanted with 125 µg aluminum phosphate.
PPSV23 (PNEUMOVAX® 23, MSD) is a 23-valent pneumococcal polysaccharide vaccine. Each dose of PPSV23 contains 25 µg of pneumococcal capsular polysaccharide from serotypes 1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19A, 19F, 20, 22F, 23F, and 33F.
V114 and PCV13 were supplied as sterile suspensions and PPSV23 was supplied as a sterile solution. All study vaccines were supplied in pre-filled syringes and stored at 2–8 °C. A 0.5 mL dose of V114 (lot number 00068290) or PCV13 (lot numbers 0000793304, 0000921112, and 0000814723) and PPSV23 (lot number 0000794346) was administered intramuscularly using needles suited for intramuscular injection.
Study assessments and analyses
Safety
Adverse events (AEs) experienced following receipt of each study vaccine were self-recorded using a Vaccination Report Card and subsequently assessed by the investigators. Injection-site reactions (erythema, swelling, and pain) and systemic AEs (muscle pain/myalgia, joint pain/arthralgia, headache, and fatigue) were solicited following each vaccination; non-solicited injection-site and systemic AEs were also recorded. Information for serious AEs (SAEs) and deaths, regardless of attribution, were collected from the time of signed consent through to the end of the study. All injection-site AEs were considered related to the vaccines. For systemic AEs, relatedness to the study vaccine was assessed by the investigators.
Safety subgroup analyses were conducted on the all-participants-as-treated population, which comprised all randomized participants who received the relevant study vaccine for the timepoint of interest. Safety analyses were conducted by the number of risk factors for pneumococcal disease at baseline (1 or ≥2 risk factors) and were assessed following administration of V114 or PCV13, as previously described.29
Immunogenicity
Serum samples were collected pre-vaccination with PCV (Day 1), 30 days post-PCV vaccination (Day 30), pre-vaccination with PPSV23 (Month 6), and 30 days post-PPSV23 vaccination (Month 7) to assess immune responses. Immunogenicity subgroup analyses were conducted by the number of risk factors for pneumococcal disease at baseline (1 or ≥2 risk factors) in the per-protocol population and comprised all randomized participants without protocol deviations that could substantially affect the results of immunogenicity endpoints. Immunogenicity analyses were conducted using serotype-specific opsonophagocytic activity (OPA) geometric mean titers (GMTs) and observed serotype-specific immunoglobulin G (IgG) geometric mean concentrations (GMCs) at Day 30, Month 6, and Month 7, as previously described in Hammitt et al.29 Geometric mean fold rises (GMFRs) and the proportions of participants with a ≥4-fold rise in OPA responses from pre-vaccination to Day 30 following vaccination were also assessed within each vaccination group separately.
In adult populations, no serotype-specific IgG concentrations or OPA titers have been defined as the threshold values that correlate with protection; therefore, both GMFRs and the proportion of participants with a ≥4 fold rise in serotype-specific antibodies for both OPA and IgG are commonly assessed as serologic response markers to pneumococcal vaccination.34,35
Results
Study population
A total of 1,131 randomized participants were included in this analysis (Figure 1). Of the participants who received PCV on Day 1, 848 received V114 and 283 received PCV13. Most participants (91.2%) received PPSV23 approximately 6 months later. The majority of participants (91.8%) completed the study. The proportion of participants who discontinued the study and reasons for discontinuation were generally comparable across vaccination groups.
Figure 1.
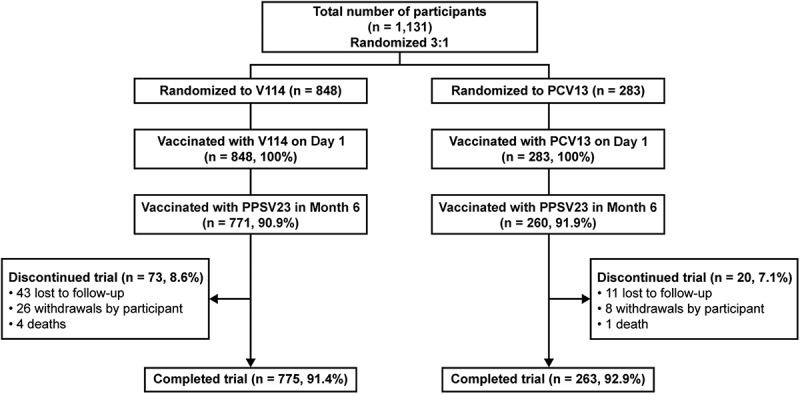
Participant disposition.
Percentages are calculated based on the number of participants randomized. Participants could have been considered to complete the study without receipt of PPSV23. PCV13: 13-valent pneumococcal conjugate vaccine; PPSV23: 23-valent pneumococcal polysaccharide vaccine; V114: 15-valent pneumococcal conjugate vaccine.
Demographic and baseline characteristics were generally comparable across vaccination groups (Table 2). More than half of the participants were White and 18.7% were American Indian/Alaska Native. In the V114 group, 73.1% had a single risk factor for pneumococcal disease at screening and 26.9% had ≥2 risk factors. The PCV13 group showed a similar distribution. The most common single risk factors were tobacco use (19.5%), chronic lung disease (19.1%), and diabetes mellitus (18.4%). The number of risk factors increased with increasing age in both vaccination groups.
Table 2.
Participant baseline characteristics.
| V114 |
PCV13 |
Total |
||||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Vaccinated participants | 848 | 283 | 1131 | |||
| Sex | ||||||
| Male | 455 | (53.7) | 141 | (49.8) | 596 | (52.7) |
| Female | 393 | (46.3) | 142 | (50.2) | 535 | (47.3) |
| Age (years) | ||||||
| Mean | 37.2 | 37.4 | 37.2 | |||
| Range | 18–49 | 18–49 | 18–49 | |||
| Race | ||||||
| White | 580 | (68.4) | 191 | (67.5) | 771 | (68.2) |
| American Indian/Alaska Native | 160 | (18.9) | 52 | (18.4) | 212 | (18.7) |
| Black/African American | 43 | (5.1) | 18 | (6.4) | 61 | (5.4) |
| Native Hawaiian/other Pacific Islander | 33 | (3.9) | 11 | (3.9) | 44 | (3.9) |
| Asian | 15 | (1.8) | 8 | (2.8) | 23 | (2.0) |
| Multiple | 17 | (2.0) | 3 | (1.1) | 20 | (1.8) |
| Ethnicity | ||||||
| Not Hispanic/Latino | 709 | (83.6) | 247 | (87.3) | 956 | (84.5) |
| Hispanic/Latino | 123 | (14.5) | 33 | (11.7) | 156 | (13.8) |
| Not reported | 8 | (0.9) | 1 | (0.4) | 9 | (0.8) |
| Unknown | 8 | (0.9) | 2 | (0.7) | 10 | (0.9) |
| Participants by risk factors†,‡ | ||||||
| With single risk factor | 620 | (73.1) | 207 | (73.1) | 827 | (73.1) |
| Tobacco use | 165 | (19.5) | 56 | (19.8) | 221 | (19.5) |
| Chronic lung disease | 163 | (19.2) | 53 | (18.7) | 216 | (19.1) |
| Diabetes mellitus | 157 | (18.5) | 51 | (18.0) | 208 | (18.4) |
| Chronic heart disease | 57 | (6.7) | 20 | (7.1) | 77 | (6.8) |
| Alcohol consumption§ | 50 | (5.9) | 18 | (6.4) | 68 | (6.0) |
| Chronic liver disease | 28 | (3.3) | 9 | (3.2) | 37 | (3.3) |
| With ≥2 risk factors | 228 | (26.9) | 76 | (26.9) | 304 | (26.9) |
| Participants by risk factors and age group‡ | ||||||
| 18–29 years | 198 | (23.3) | 56 | (19.8) | 254 | (22.5) |
| With single risk factor | 147 | (17.3) | 40 | (14.1) | 187 | (16.5) |
| With ≥2 risk factors | 51 | (6.0) | 16 | (5.7) | 67 | (5.9) |
| 30–39 years | 252 | (29.7) | 86 | (30.4) | 338 | (29.9) |
| With single risk factor | 194 | (22.9) | 63 | (22.3) | 257 | (22.7) |
| With ≥2 risk factors | 58 | (6.8) | 23 | (8.1) | 81 | (7.2) |
| 40–49 years | 398 | (46.9) | 141 | (49.8) | 539 | (47.7) |
| With single risk factor | 279 | (32.9) | 104 | (36.7) | 383 | (33.9) |
| With ≥2 risk factors | 119 | (14.0) | 37 | (13.1) | 156 | (13.8) |
Table includes all vaccinated participants. Pre-defined risk factors include chronic liver, lung, and heart disease, diabetes mellitus, tobacco use, and alcohol consumption.
AUDIT-C: Alcohol Use Disorders Identification Test – Consumption; PCV13: 13-valent pneumococcal conjugate vaccine; V114: 15-valent pneumococcal conjugate vaccine.
†Participant is counted for each applicable row and column.
‡Actual strata assignments were used in the summaries of risk factors.
§The risk factor of alcohol consumption is defined as an AUDIT-C score ≥5.
Safety
Following administration of PCV, most participants in the V114 and PCV13 vaccine groups experienced at least one AE, regardless of the number of baseline risk factors (Table 3). Four deaths were reported in participants who had one or more risk factors, none of which were considered by the investigator to be related to the study vaccine. The causes of death were suicide at 102 days, multiple injuries following a road traffic accident at 129 days, liver disorder at 169 days, and cardiac arrest at 220 days post-vaccination. Among these deaths, one participant each had a single risk factor of either chronic heart disease, tobacco use, or chronic liver disease/alcohol consumption, and one participant had multiple risk factors. No correlation was observed between risk of death and the number or absence of risk factors for pneumococcal disease, although the number of deaths is small. The proportions of participants with solicited AEs were generally comparable across the two risk factor groups (1 or ≥2 risk factors), with injection-site pain being the most common (Figure 2). In both vaccination groups, most solicited AEs were transient (≤3 days; data not shown) and mild in severity (Figure 2).
Table 3.
Summary of adverse events following vaccination with V114 or PCV13 by number of risk factors (Day 1–Month 6).
| n (%) | 1 risk factor |
≥2 risk factors |
||
|---|---|---|---|---|
| V114 n = 620 |
PCV13 n = 207 |
V114 n = 229 |
PCV13 n = 75 |
|
| Any AE | 528 (85.2) | 180 (87.0) | 198 (86.5) | 61 (81.3) |
| Injection-site† | 495 (79.8) | 155 (74.9) | 182 (79.5) | 55 (73.3) |
| Systemic | 390 (62.9) | 138 (66.7) | 150 (65.5) | 45 (60.0) |
| Any vaccine-relatedAE‡ | 516 (83.2) | 168 (81.2) | 188 (82.1) | 60 (80.0) |
| Systemic | 309 (49.8) | 101 (48.8) | 114 (49.8) | 34 (45.3) |
| Any SAE | 23 (3.7) | 5 (2.4) | 12 (5.2) | 3 (4.0) |
| Any vaccine-relatedSAE‡ | 0 | 0 | 0 | 0 |
| Deaths | 2 (0.3) | 1 (0.5) | 1 (0.4) | 0 |
Pre-defined risk factors include chronic liver, lung, and heart disease, diabetes mellitus, tobacco use, and alcohol consumption. The risk factor of alcohol consumption is defined as an AUDIT-C score ≥5. Reported AEs include non-serious AEs at Days 1–14 post-vaccination and SAEs at Day 1–Month 6.
AE: adverse event; AUDIT-C: Alcohol Use Disorders Identification Test – Consumption; PCV13: 13-valent pneumococcal conjugate vaccine; SAE: serious adverse event; V114: 15-valent pneumococcal conjugate vaccine.
†All injection-site AEs were considered related to the vaccine by the investigator.
‡Determined by the investigator to be related to the vaccine.
Figure 2.
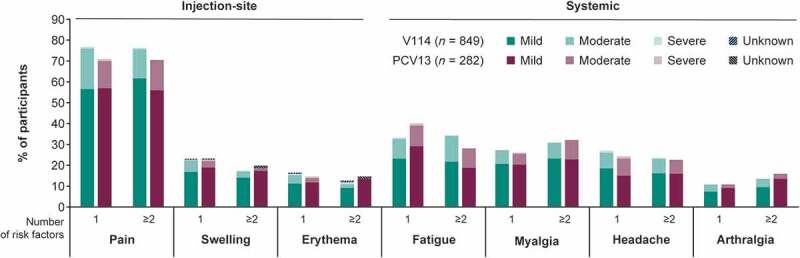
Proportion of participants with solicited AEs following vaccination with V114 or PCV13 by number of baseline risk factors and maximum intensity.
Solicited AEs by number of baseline risk factors collected post-vaccination with V114 (n = 849) or PCV13 (n = 282). Injection-site events were solicited from Day 1–5 following vaccination. For solicited injection-site erythema and injection-site swelling, mild events measured >0 to ≤5 cm, moderate events measured >5 to ≤10 cm, and severe events measured >10 cm. Systemic events were solicited from Day 1–14 following vaccination. Pre-defined risk factors include chronic liver, lung, and heart disease, diabetes mellitus, tobacco use, and alcohol consumption. The risk factor of alcohol consumption is defined as an AUDIT-C score ≥5. AE: adverse event; AUDIT-C: Alcohol Use Disorders Identification Test – Consumption; PCV13: 13-valent pneumococcal conjugate vaccine; V114: 15-valent pneumococcal conjugate vaccine.
Among participants who had a single risk factor of chronic heart disease, chronic liver disease or alcohol consumption, chronic lung disease, diabetes mellitus, or tobacco use, V114 was well tolerated in subgroups by risk factor (data not shown).
Following administration of PPSV23 (Month 6–Month 7), most participants experienced at least one AE, irrespective of the number of baseline risk factors. The AEs recorded were generally comparable to the safety profile observed following vaccination with PCV (Table 4). One vaccine-related SAE of generalized tonic-clonic seizure was reported in the PCV13 group for a participant who had one risk factor for pneumococcal disease; no deaths were reported in either risk factor or vaccination groups. The proportions of participants with solicited AEs following administration of PPSV23 were comparable across the two risk factor (1 or ≥2 risk factors) and vaccination groups.
Table 4.
Summary of adverse events following vaccination with PPSV23 by number of risk factors (Month 6–month 7).
| n (%) | 1 risk factor |
≥2 risk factors |
||
|---|---|---|---|---|
| V114 n = 561 |
PCV13 n = 190 |
V114 n = 211 |
PCV13 n = 69 |
|
| Any AE | 454 (80.9) | 158 (83.2) | 170 (80.6) | 52 (75.4) |
| Injection-site† | 428 (76.3) | 142 (74.7) | 167 (79.1) | 49 (71.0) |
| Systemic | 313 (55.8) | 114 (60.0) | 102 (48.3) | 29 (42.0) |
| Any vaccine-relatedAE‡ | 446 (79.5) | 149 (78.4) | 169 (80.1) | 50 (72.5) |
| Systemic | 274 (48.8) | 99 (52.1) | 84 (39.8) | 23 (33.3) |
| Any SAE | 1 (0.2) | 2 (1.1) | 1 (0.5) | 0 (0.0) |
| Any vaccine-relatedSAE† | 0 (0.0) | 1 (0.5) | 0 (0.0) | 0 (0.0) |
| Deaths | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Solicited AE | 447 (79.7) | 155 (81.6) | 169 (80.1) | 50 (72.5) |
| Solicited injection-site AE | 427 (76.1) | 142 (74.7) | 166 (78.7) | 49 (71.0) |
| Injection-site erythema | 151 (26.9) | 56 (29.5) | 45 (21.3) | 16 (23.2) |
| Injection-site pain | 417 (74.3) | 138 (72.6) | 156 (73.9) | 46 (66.7) |
| Injection-site swelling | 190 (33.9) | 71 (37.4) | 68 (32.2) | 21 (30.4) |
| Solicited systemic AE | 293 (52.2) | 107 (56.3) | 100 (47.4) | 26 (37.7) |
| Arthralgia | 66 (11.8) | 24 (12.6) | 29 (13.7) | 6 (8.7) |
| Fatigue | 182 (32.4) | 72 (37.9) | 64 (30.3) | 15 (21.7) |
| Headache | 128 (22.8) | 46 (24.2) | 39 (18.5) | 12 (17.4) |
| Myalgia | 154 (27.5) | 58 (30.5) | 54 (25.6) | 17 (24.6) |
Pre-defined risk factors include chronic liver, lung, and heart disease, diabetes mellitus, tobacco use, and alcohol consumption. The risk factor of alcohol consumption is defined as an AUDIT-C score ≥5.
AE: adverse event; AUDIT-C: Alcohol Use Disorders Identification Test – Consumption; PCV13: 13-valent pneumococcal conjugate vaccine; PPSV23: 23-valent pneumococcal polysaccharide vaccine; SAE: serious adverse event; V114: 15-valent pneumococcal conjugate vaccine.
†All injection-site AEs were considered related to the vaccine by the investigator.
‡Determined by the investigator to be related to the vaccine.
Immunogenicity
Regardless of the number of baseline risk factors, V114 and PCV13 were immunogenic for the 13 shared serotypes based on OPA GMTs (Figure 3, Supplemental Tables S2 and S3) and IgG GMCs (Supplemental Tables S4 and S5) at 30 days post-vaccination with PCV (Day 30). In addition, V114 induced a robust immune response to the two additional serotypes (22F and 33F) in both risk factor groups (1 or ≥2 risk factors). Regardless of the number of baseline risk factors, PPSV23 administered 6 months after PCV was immunogenic for all 15 serotypes contained in V114, as assessed by OPA GMTs (Figure 4, Supplemental Tables S2 and S3) and IgG GMCs (Supplemental Tables S4 and S5) at 30 days post-PPSV23 vaccination (Month 7). Results observed for OPA GMTs following vaccination with V114 or PCV13, and PPSV23, were consistent with results observed for OPA serotype-specific GMFRs and proportions of participants with a ≥4-fold rise from Day 1 to Day 30 and from Day 1 to Month 7, respectively (Supplemental Tables S6 and S7).
Figure 3.
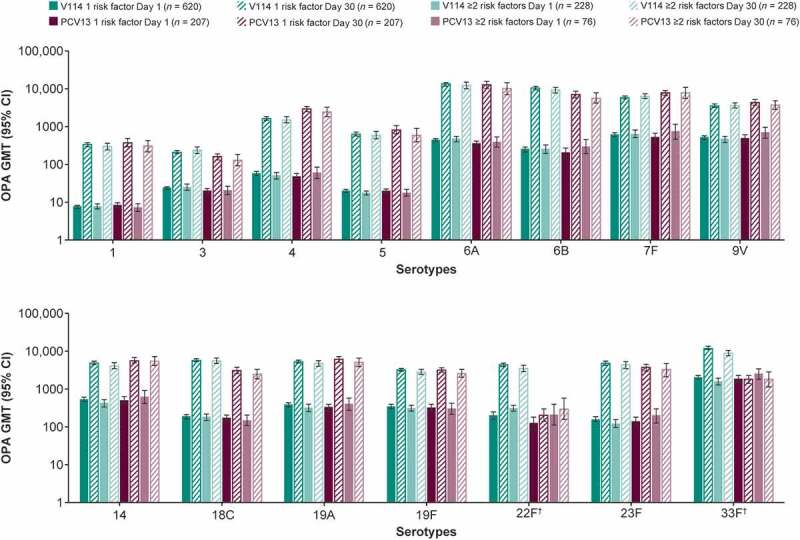
Serotype-specific OPA GMTs at baseline (Day 1) and 30 days post-vaccination (Day 30) with V114 or PCV13 by number of baseline risk factors.
Pre-defined risk factors include chronic liver, lung, and heart disease, diabetes mellitus, tobacco use, and alcohol consumption. The within-group 95% CIs were obtained by exponentiating the CIs of the mean of the natural log values based on the t-distribution. n is the number of participants randomized and vaccinated with PCV. †Additional serotypes in V114. CI: confidence interval; GMT: geometric mean titer (1/dilution); OPA: opsonophagocytic activity; PCV: pneumococcal conjugate vaccine; PCV13: 13-valent pneumococcal conjugate vaccine; V114: 15-valent pneumococcal conjugate vaccine.
Figure 4.
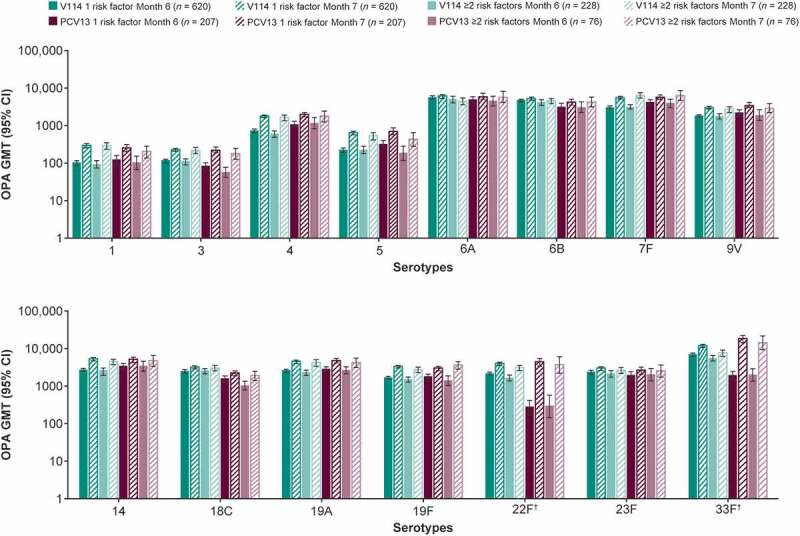
Serotype-specific OPA GMTs prior to vaccination with PPSV23 (Month 6) and 30 days post-vaccination (Month 7) with PPSV23 by number of baseline risk factors.
Pre-defined risk factors include chronic liver, lung, and heart disease, diabetes mellitus, tobacco use, and alcohol consumption. The within-group 95% CIs were obtained by exponentiating the CIs of the mean of the natural log values based on the t-distribution. n is the number of participants randomized and vaccinated with PCV. †Additional serotypes in V114. CI: confidence interval; GMT: geometric mean titer (1/dilution); OPA: opsonophagocytic activity; PCV: pneumococcal conjugate vaccine; PCV13: 13-valent pneumococcal conjugate vaccine; PPSV23: 23-valent pneumococcal polysaccharide vaccine; V114: 15-valent pneumococcal conjugate vaccine.
In participants with a single risk factor of chronic heart disease, chronic liver disease or alcohol consumption, chronic lung disease, diabetes mellitus, or tobacco use, V114 was immunogenic, as assessed by OPA GMTs (Supplemental Tables S8–S12) and IgG GMCs (Supplemental Tables S13–S17) for all 15 serotypes contained in V114 at 30 days post-vaccination with PCV (Day 30). In addition, immune responses were generally comparable between participants with a specific single risk condition (Figure 5). For each single risk factor, serotype-specific OPA GMTs and IgG GMCs at 30 days post-vaccination with PCV were generally comparable between recipients of V114 and PCV13 for the 13 shared serotypes and higher in recipients of V114 for the two additional serotypes. Similarly, V114 followed by PPSV23 was immunogenic for all 15 serotypes contained in V114, as assessed by OPA GMTs (Supplemental Tables S8–S12) and IgG GMCs (Supplemental Tables S13–S17) at 30 days post-PPSV23 vaccination (Month 7). Serotype-specific OPA GMTs and IgG GMCs were also generally comparable between the two vaccination groups at Month 7 for all 15 serotypes included in V114 across both risk factor groups (1 or ≥2 risk factors).
Figure 5.
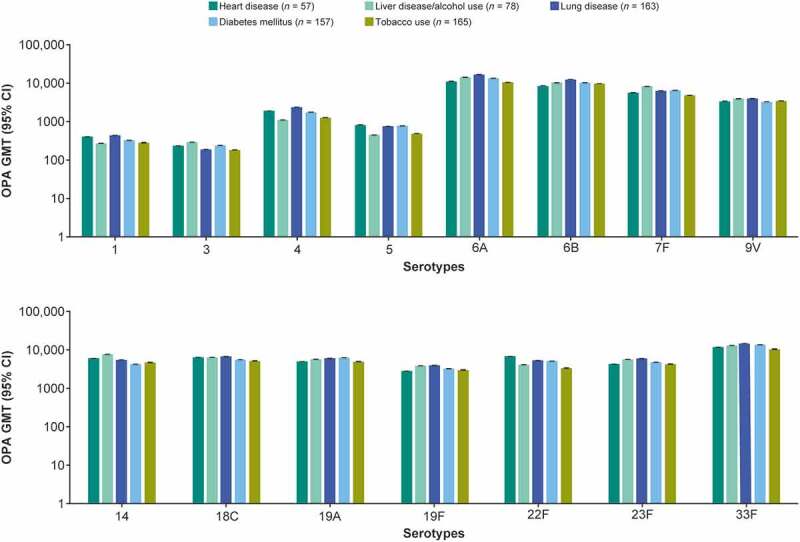
Serotype-specific OPA GMTs at 30 days post-vaccination with V114 by specific single risk conditions.
The within-group 95% CIs were obtained by exponentiating the CIs of the mean of the natural log values based on the t-distribution. n is the number of participants contributing to the analysis. Participants with chronic liver disease and alcohol consumption were grouped together due to low numbers in each individual group. CI: confidence interval; GMT: geometric mean titer (1/dilution); OPA: opsonophagocytic activity; PCV: pneumococcal conjugate vaccine; V114: 15-valent pneumococcal conjugate vaccine.
Discussion
This subgroup analysis supports the safety, tolerability, and immunogenicity profiles of V114 in pneumococcal vaccine-naïve immunocompetent adults 18–49 years of age, regardless of the number of certain baseline risk factors for pneumococcal disease, including chronic liver, lung, and heart disease, diabetes mellitus, and tobacco or alcohol use. Results are consistent with those described for the overall study population.29 Adults living with chronic conditions enrolled in this study are at higher risk of serious pneumococcal infection than healthy age-matched adults, with increased rates of hospitalization and death.1,2,7–10 Stacking of these risk factors is associated with increased risk of pneumococcal disease,1,2,10–12 with the risk approaching that seen in immunocompromised individuals.12 Unlike immunocompromised individuals, most immunocompetent adults with medical conditions associated with an increased risk of pneumococcal disease respond well to vaccination.36–38
Studies have shown that pneumococcal vaccines have cardioprotective effects in populations at high cardiovascular risk.39,40 Pneumococcal vaccination has also been shown to have a positive effect on the course of chronic obstructive pulmonary disease by reducing exacerbations and improving quality of life.41 Therefore, at-risk adults would benefit greatly from protection against pneumococcal disease, particularly when vaccinated against a broader range of serotypes. Despite the many advantages of pneumococcal vaccination in this population, there is a lack of robust randomized clinical trials in individuals with defined risk factors and risk factor stacking.
Among adults with 1 or ≥2 risk factors for pneumococcal disease, V114 induced immune responses against serotypes 22F and 33F, the two additional serotypes in V114 that are now among the most common serotypes that cause IPD.22,24,42 In addition, immune responses to the 13 serotypes shared by PCV13 and V114 were generally comparable between the two vaccination groups 30 days following PCV vaccination, regardless of the number of baseline risk factors. Taken together, this suggests that V114 may be able to provide expanded protection against these two additional serotypes in at-risk adults while also maintaining immune responses to the 13 serotypes shared with PCV13. Sequential administration of PPSV23 6 months after V114 induced immune responses to all 15 serotypes, regardless of the number of baseline risk factors for pneumococcal disease; these responses were generally comparable with those elicited with PPSV23 administered 6 months after PCV13. V114 administered alone or sequentially with PPSV23 also had a comparable safety profile to that of PCV13 administered alone or sequentially with PPSV23, with no apparent effect of risk factors on vaccine-related AEs. Of note, when compared with PCV13, vaccination with V114 was associated with higher OPA GMTs for serotype 3 at Day 30 and up to Month 6 post-vaccination, which is consistent with the results of other studies.27,28 The clinical impact of higher immune responses to serotype 3 compared with the response to PCV13 is not currently known. Furthermore, following vaccination with PPSV23, antibody responses to serotype 3 were more similar between both vaccination groups. The lack of a consistent booster response to sequential vaccination was also evident for other serotypes. For serotype 33F, PPSV23 induced immune responses in the PCV13 arm that were higher than those after sequential administration of V114 and PPSV23. Similar findings have been described in a previous study that evaluated sequential administration of PCV13 and PPSV23 in older adults (60–64 years of age) using a 1-year interval between vaccinations. Antibody levels for some serotypes were not numerically higher post-vaccination with PCV13/PPSV23 than those measured after PCV13 or PPSV23 administered alone.43 Longer intervals between vaccinations may improve the immune response to serotypes shared between the PCV and PPSV23.44 In a study evaluating the administration of PPSV23 8 weeks after PCV13, immune responses for PPSV23-unique serotypes were superior while responses to shared serotypes were non-inferior at Week 12, compared with PCV13 given alone.45 In the absence of accepted immune correlates of protection, as well as head-to-head studies comparing shorter (<1 year) versus longer (>1 year) time intervals, the potential benefit for earlier protection against PPSV23-unique serotypes with a shorter time interval should be considered in at-risk populations. The strength of this study is that participants had well-defined chronic risk conditions, disease stages, and treatment plans, and, therefore, the results support the use of the V114/PPSV23 sequential regimen in at-risk adults. The importance of this approach is now reflected in the updated ACIP recommendation for pneumococcal vaccination of at-risk adults ≥19 years of age with either V114 followed by PPSV23 or a single dose of PCV20.32
The study was descriptive and was not powered to assess noninferiority or superiority with respect to immune responses, thus limiting the interpretability of between-group comparisons; a formal statistical comparison between V114 and PCV13 was conducted in a larger study in adults ≥50 years of age.27 The heterogeneity of underlying medical conditions in this population also limits the interpretability of comparisons between the risk factor groups. However, comparisons made between vaccination groups and risk factor groups in this study regarding immunogenicity refer to observed trends of OPA and IgG responses and the totality of the observed immunogenicity results, which do not suggest clinically meaningful differences. Regarding safety, absolute differences in the proportions of participants with specific AEs were small and most AEs were mild to moderate in intensity.
Conclusions
In immunocompetent adults 18–49 years of age with one or more risk factors for pneumococcal disease, including chronic liver, lung, and heart disease, diabetes mellitus, and tobacco or alcohol use, V114 administered alone or sequentially with PPSV23 was well tolerated and had a comparable safety profile to PCV13 administered alone or sequentially with PPSV23. V114 administered either alone or sequentially with PPSV23 6 months later was immunogenic for all 15 serotypes in V114, regardless of the number of baseline risk factors. V114 has the potential to broaden serotype coverage and protect against pneumococcal disease caused by serotypes not contained in PCV13 for at-risk adults.
Supplementary Material
Acknowledgments
We would like to thank all the participants, study staff, and investigators in the V114-017 (PNEU-DAY) study group for their invaluable contributions to this study. Medical writing support, including assisting authors with the development of the initial draft and incorporation of comments, was provided by Cindy Cheung, MBBS (MD), and Suparna Abraham, PharmD, of Scion, London; and editorial support, including figure preparation, formatting, proofreading, and submission, was provided by Ian Norton, PhD, of Scion, London, UK, supported by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA, according to Good Publication Practice guidelines (Link). The sponsor was involved in the study design and collection, analysis, and interpretation of data, as well as data checking of information provided in the manuscript. However, ultimate responsibility for opinions, conclusions, and data interpretation lies with the authors.
Funding Statement
This study was supported by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Disclosure statement
L.L.H. has received research grants paid to her institution from AstraZeneca, CDC, Merck & Co., Inc., NIH, and Pfizer. E.J. has received grants from Axella, CymaBay, Dr. Falk, Exelixis, GSK, Janssen-Cilag, Merck & Co., Inc., and Novo Nordisk, and honoraria from AbbVie, and Roche. F.J.P. has received consulting fees from Boehringer Ingelheim, Dexcom, Medscape, and Merck & Co., Inc., honoraria from Medscape, and research grants paid to his institution from Merck & Co., Inc., Dexcom, and Insulet. K.R.R. has received consulting fees from Genfit, Gilead, Mallinckrodt, Merck & Co., Inc., Novo Nordisk, and Spark Therapeutics, served on an advisory board for AstraZeneca and Novartis-DSMB, and received research support paid to his institution from AbbVie, BioVie, BMS, Exact Sciences, Gilead, Grifols, HCC-TARGET, Intercept, Mallinckrodt, Merck & Co., Inc., NASH-TARGET, and Sequana. R. Dagan has received research grants from MedImmune/AstraZeneca, Merck & Co., Inc., and Pfizer, consulting fees from Merck & Co., Inc. and Pfizer, and honoraria from Merck & Co., Inc., Pfizer, and Sanofi Pasteur. R. Dawson was an employee of Merck & Co., Inc. at the time of this study, and is currently an employee of Moderna. A.P., G.T., J.M., K.C., L.M., T. Shekar, T. Sterling, U.K.B., and W.F. are employees of Merck Sharp & Dohme LLC., a subsidiary of Merck & Co., Inc., Rahway, NJ, USA and may own stock and/or stock options in Merck & Co., Inc., Rahway, NJ, USA. All other authors report no potential conflicts of interest.
Author contributions
L.L.H.: conceptualization, design, or planning of the study, acquisition of the data, interpretation of the results, drafting of the manuscript, and reviewing or revising the manuscript for important intellectual content. D.Q.: acquisition of the data and reviewing or revising the manuscript for important intellectual content. E.J., K.A.: acquisition of the data, interpretation of the results, and reviewing or revising the manuscript for important intellectual content. F.J.P., R.T.: interpretation of the results and drafting of the manuscript. K.R.R.: interpretation of results and reviewing or revising the manuscript for important intellectual content. I.M.K.: analysis of the data and drafting of the manuscript. R. Dagan, T. Shekar: interpretation of the results, drafting of the manuscript, and reviewing or revising the manuscript for important intellectual content. R. Dawson: analysis of the data, interpretation of the results, and critically reviewing or revising the manuscript for important intellectual content. J.M.: conceptualization, design, or planning of the study, drafting of the manuscript, and critically reviewing or revising the manuscript for important intellectual content. W.F.: analysis of the data and reviewing or revising the manuscript for important intellectual content. A.P.: conceptualization, design, or planning of the study, analysis of the data, interpretation of the results, and reviewing or revising the manuscript for important intellectual content. T. Sterling, G.T.: conceptualization, design, or planning of the study, and reviewing or revising the manuscript for important intellectual content. L.M.: conceptualization, design, or planning of the study, analysis of the data, interpretation of the results, drafting of the manuscript, and reviewing or revising the manuscript for important intellectual content. U.K.B.: conceptualization, design, or planning of the study, analysis of the data, acquisition of the data, interpretation of the results, drafting of the manuscript, and reviewing or revising the manuscript for important intellectual content.
Data availability statement
The data sharing policy, including restrictions, of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA is available at http://engagezone.msd.com/ds_documentation.php through the EngageZone site or via e-mail to dataaccess@merck.com.
Supplementary data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2177066.
References
- 1.Curcio D, Cane A, Isturiz R.. Redefining risk categories for pneumococcal disease in adults: critical analysis of the evidence. Int J Infect Dis. 2015;37:30–11. doi: 10.1016/j.ijid.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Torres A, Blasi F, Dartois N, Akova M.. Which individuals are at increased risk of pneumococcal disease and why? Impact of COPD, asthma, smoking, diabetes, and/or chronic heart disease on community-acquired pneumonia and invasive pneumococcal disease. Thorax. 2015;70(10):984–89. doi: 10.1136/thoraxjnl-2015-206780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention, Advisory Committee on Immunization Practices . Updated recommendations for prevention of invasive pneumococcal disease among adults using the 23-valent pneumococcal polysaccharide vaccine (PPSV23). MMWR. 2010;59(34):1102–06. [PubMed] [Google Scholar]
- 4.Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 diabetes and its impact on the immune system. Curr Diabetes Rev. 2020;16(5):442–49. doi: 10.2174/1573399815666191024085838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhat TA, Panzica L, Kalathil SG, Thanavala Y. Immune dysfunction in patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2015;12(Suppl 2):S169–75. doi: 10.1513/AnnalsATS.201503-126AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Inghammar M, Engstrom G, Kahlmeter G, Ljungberg B, Lofdahl CG, Egesten A. Invasive pneumococcal disease in patients with an underlying pulmonary disorder. Clin Microbiol Infect. 2013;19(12):1148–54. doi: 10.1111/1469-0691.12182. [DOI] [PubMed] [Google Scholar]
- 7.Burgos J, Lujan M, Larrosa MN, Fontanals D, Bermudo G, Planes AM, Puig M, Rello J, Falco V, Pahissa A. Risk factors for respiratory failure in pneumococcal pneumonia: the importance of pneumococcal serotypes. Eur Respir J. 2014;43(2):545–53. doi: 10.1183/09031936.00050413. [DOI] [PubMed] [Google Scholar]
- 8.Corrales-Medina VF, Musher DM, Wells GA, Chirinos JA, Chen L, Fine MJ. Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality. Circulation. 2012;125(6):773–81. doi: 10.1161/CIRCULATIONAHA.111.040766. [DOI] [PubMed] [Google Scholar]
- 9.Sicras-Mainar A, Ibanez-Nolla J, Cifuentes I, Guijarro P, Navarro-Artieda R, Aguilar L. Retrospective epidemiological study for the characterization of community- acquired pneumonia and pneumococcal pneumonia in adults in a well-defined area of Badalona (Barcelona, Spain). BMC Infect Dis. 2012;12(1):283. doi: 10.1186/1471-2334-12-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weycker D, Farkouh RA, Strutton DR, Edelsberg J, Shea KM, Pelton SI. Rates and costs of invasive pneumococcal disease and pneumonia in persons with underlying medical conditions. BMC Health Serv Res. 2016;16(1):182. doi: 10.1186/s12913-016-1432-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morton JB, Morrill HJ, LaPlante KL, Caffrey AR. Risk stacking of pneumococcal vaccination indications increases mortality in unvaccinated adults with Streptococcus pneumoniae infections. Vaccine. 2017;35(13):1692–97. doi: 10.1016/j.vaccine.2017.02.026. [DOI] [PubMed] [Google Scholar]
- 12.Zhang D, Petigara T, Yang X. Clinical and economic burden of pneumococcal disease in US adults aged 19–64 years with chronic or immunocompromising diseases: an observational database study. BMC Infect Dis. 2018;18(1):436. doi: 10.1186/s12879-018-3326-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shea KM, Edelsberg J, Weycker D, Farkouh RA, Strutton DR, Pelton SI. Rates of pneumococcal disease in adults with chronic medical conditions. Open Forum Infect Dis. 2014;1(1):ofu024. doi: 10.1093/ofid/ofu024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pelton SI, Bornheimer R, Doroff R, Shea KM, Sato R, Weycker D. Decline in pneumococcal disease attenuated in older adults and those with comorbidities following universal childhood PCV13 immunization. Clin Infect Dis. 2019;68(11):1831–38. doi: 10.1093/cid/ciy800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GBD 2016 Lower Respiratory Infections Collaborators . Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18:1191–210. doi: 10.1016/S1473-3099(18)30310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watt JP, O’brien KL, Benin AL, McCoy SI, Donaldson CM, Reid R, Schuchat A, Zell ER, Hochman M, Santosham M, et al. Risk factors for invasive pneumococcal disease among Navajo adults. Am J Epidemiol. 2007;166(9):1080–87. doi: 10.1093/aje/kwm178. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization . Pneumococcal disease. 2021. [Accessed 2021 Nov 29]. https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccine-standardization/pneumococcal-disease.
- 18.Niederman MS, Folaranmi T, Buchwald UK, Musey L, Cripps AW, Johnson KD. Efficacy and effectiveness of a 23-valent polysaccharide vaccine against invasive and noninvasive pneumococcal disease and related outcomes: a review of available evidence. Expert Rev Vaccines. 2021;20(3):243–56. doi: 10.1080/14760584.2021.1880328. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization . WHO vaccine-preventable diseases: monitoring system. 2020 global summary. 2020. [Accessed Nov 7]. https://immunizationdata.who.int/pages/schedule-by-disease/pneumo.html?ISO_3_CODE=&TARGETPOP_GENERAL=.
- 20.Merck Sharp & Dohme Corp . Pneumovax 23 prescribing information. 2021. [Accessed 2021 Aug 16]. https://www.merck.com/product/usa/pi_circulars/p/pneumovax_23/pneumovax_pi.pdf.
- 21.Pfizer . PREVNAR 13 (Pneumococcal 13-valent conjugate vaccine [Diphtheria CRM197 protein]). 2017. [Accessed Sept 29]. https://www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM574852.pdf.
- 22.Waight PA, Andrews NJ, Ladhani SN, Sheppard CL, Slack MP, Miller E. Effect of the 13-valent pneumococcal conjugate vaccine on invasive pneumococcal disease in England and Wales 4 years after its introduction: an observational cohort study. Lancet Infect Dis. 2015;15(5):535–43. doi: 10.1016/S1473-3099(15)70044-7. [DOI] [PubMed] [Google Scholar]
- 23.Tin Tin Htar M, Morato Martinez J, Theilacker C, Schmitt HJ, Swerdlow D. Serotype evolution in Western Europe: perspectives on invasive pneumococcal diseases (IPD). Expert Rev Vaccines. 2019;18(11):1145–55. doi: 10.1080/14760584.2019.1688149. [DOI] [PubMed] [Google Scholar]
- 24.Moore MR, Link-Gelles R, Schaffner W, Lynfield R, Lexau C, Bennett NM, Petit S, Zansky SM, Harrison LH, Reingold A, et al. Effect of use of 13-valent pneumococcal conjugate vaccine in children on invasive pneumococcal disease in children and adults in the USA: analysis of multisite, population-based surveillance. Lancet Infect Dis. 2015;15(3):301–09. doi: 10.1016/S1473-3099(14)71081-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amin-Chowdhury Z, Groves N, Sheppard CL, Litt D, Fry NK, Andrews N, Ladhani SN. Invasive pneumococcal disease due to 22F and 33F in England: a tail of two serotypes. Vaccine. 2021;39(14):1997–2004. doi: 10.1016/j.vaccine.2021.02.026. [DOI] [PubMed] [Google Scholar]
- 26.Owusu-Edusei Ad K, Kelly DJ. Estimates of the health and economic burden of pneumococcal infections attributable to the 15-valent pneumococcal conjugate vaccine serotypes in the USA. Infect Dis Ther. 2022;11(3):987–99. doi: 10.1007/s40121-022-00588-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Platt HL, Cardona JF, Haranaka M, Schwartz HI, Narejos Perez S, Dowell A, Chang CJ, Dagan R, Tamms GM, Sterling T, et al. A phase 3 trial of safety, tolerability, and immunogenicity of V114, 15-valent pneumococcal conjugate vaccine, compared with 13-valent pneumococcal conjugate vaccine in adults 50 years of age and older (PNEU-AGE). Vaccine. 2022;40(1):162–72. doi: 10.1016/j.vaccine.2021.08.049. [DOI] [PubMed] [Google Scholar]
- 28.Song JY, Chang CJ, Andrews C, Diez-Domingo J, Oh MD, Dagan R, Hartzel J, Pedley A, Li J, Sterling T, et al. Safety, tolerability, and immunogenicity of V114, a 15-valent pneumococcal conjugate vaccine, followed by sequential PPSV23 vaccination in healthy adults aged ≥50 years: a randomized phase III trial (PNEU-PATH). Vaccine. 2021;39(43):6422–36. doi: 10.1016/j.vaccine.2021.08.038. [DOI] [PubMed] [Google Scholar]
- 29.Hammitt LL, Quinn D, Janczewska E, Pasquel FJ, Tytus R, Reddy KR, Abarca K, Khaertynova IM, Dagan R, McCauley J, et al. Immunogenicity, safety, and tolerability of V114, a 15-valent pneumococcal conjugate vaccine, in immunocompetent adults aged 18–49 years with or without risk factors for pneumococcal disease: a randomized phase 3 trial (PNEU-DAY). Open Forum Infect Dis. 2021. doi: 10.1093/ofid/ofab605. [DOI] [PMC free article] [PubMed]
- 30.European Medicines Agency. Vaxneuvance Summary of Product Characteristics . 2022. [Accessed Nov 29]. https://www.ema.europa.eu/en/documents/product-information/vaxneuvance-epar-product-information_en.pdf.
- 31.Food and Drug Administration . VAXNEUVANCE™ (Pneumococcal 15-valent conjugate vaccine) prescribing information. 2021. [Accessed Aug 10]. https://www.fda.gov/vaccines-blood-biologics/vaccines/vaxneuvance.
- 32.Kobayashi M, Farrar JL, Gierke R, Britton A, Childs L, Leidner AJ, Campos-Outcalt D, Morgan RL, Long SS, Talbot HK, et al. Use of 15-valent pneumococcal conjugate vaccine and 20-valent pneumococcal conjugate vaccine among U.S. adults: updated recommendations of the advisory committee on immunization practices — United States, 2022. MMWR. 2022;71(4):109–17. doi: 10.15585/mmwr.mm7104a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zimmermann P, Curtis N. Factors that influence the immune response to vaccination. Clin Microbiol Rev. 2019;32(2). doi: 10.1128/CMR.00084-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hare ND, Smith BJ, Ballas ZK. Antibody response to pneumococcal vaccination as a function of preimmunization titer. J Allergy Clin Immunol. 2009;123(1):195–200. doi: 10.1016/j.jaci.2008.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zaccaro DJ, Wagener DK, Whisnant CC, Staats HF. Evaluation of vaccine-induced antibody responses: impact of new technologies. Vaccine. 2013;31(25):2756–61. doi: 10.1016/j.vaccine.2013.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eibl N, Spatz M, Fischer GF, Mayr WR, Samstag A, Wolf HM, Schernthaner G, Eibl MM. Impaired primary immune response in type-1 diabetes: results from a controlled vaccination study. Clin Immunol. 2002;103(3):249–59. doi: 10.1006/clim.2002.5220. [DOI] [PubMed] [Google Scholar]
- 37.Davis AL, Aranda CP, Schiffman G, Christianson LC. Pneumococcal infection and immunologic response to pneumococcal vaccine in chronic obstructive pulmonary disease. A pilot study. Chest. 1987;92(2):204–12. doi: 10.1378/chest.92.2.204. [DOI] [PubMed] [Google Scholar]
- 38.Mathews CE, Brown EL, Martinez PJ, Bagaria U, Nahm MH, Burton RL, Fisher-Hoch SP, McCormick JB, Mirza S. Impaired function of antibodies to pneumococcal surface protein a but not to capsular polysaccharide in Mexican American adults with type 2 diabetes mellitus. Clin Vaccine Immunol. 2012;19(9):1360–69. doi: 10.1128/CVI.00268-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Restrepo MI, Reyes LF. Pneumonia as a cardiovascular disease. Respirology. 2018;23(3):250–59. doi: 10.1111/resp.13233. [DOI] [PubMed] [Google Scholar]
- 40.Fountoulaki K, Tsiodras S, Polyzogopoulou E, Olympios C, Parissis J. Beneficial effects of vaccination on cardiovascular events: myocardial infarction, stroke, heart failure. Cardiology. 2018;141(2):98–106. doi: 10.1159/000493572. [DOI] [PubMed] [Google Scholar]
- 41.Ignatova GL, Avdeev SN, Antonov VN. Comparative effectiveness of pneumococcal vaccination with PPV23 and PCV13 in COPD patients over a 5-year follow-up cohort study. Sci Rep. 2021;11(1):15948. doi: 10.1038/s41598-021-95129-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.European Centre for Disease Prevention and Control . Invasive pneumococcal disease. ECDC. Annual epidemiological report for 2018. 2020. [Accessed September 30]. https://www.ecdc.europa.eu/sites/default/files/documents/AER_for_2018_IPD.pdf.
- 43.Greenberg RN, Gurtman A, Frenck RW, Strout C, Jansen KU, Trammel J, Scott DA, Emini EA, Gruber WC, Schmoele-Thoma B. Sequential administration of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine in pneumococcal vaccine–naïve adults 60–64 years of age. Vaccine. 2014;32(20):2364–74. doi: 10.1016/j.vaccine.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 44.Jackson LA, Gurtman A, van Cleeff M, Frenck RW, Treanor J, Jansen KU, Scott DA, Emini EA, Gruber WC, Schmoele-Thoma B. Influence of initial vaccination with 13-valent pneumococcal conjugate vaccine or 23-valent pneumococcal polysaccharide vaccine on anti-pneumococcal responses following subsequent pneumococcal vaccination in adults 50 years and older. Vaccine. 2013;31(35):3594–602. doi: 10.1016/j.vaccine.2013.04.084. [DOI] [PubMed] [Google Scholar]
- 45.Buchwald UK, Andrews CP, Ervin J, Peterson JT, Tamms GM, Krupa D, Ajiboye P, Roalfe L, Krick AL, Sterling TM, et al. Sequential administration of Prevnar 13™ and PNEUMOVAX™ 23 in healthy participants 50 years of age and older. Hum Vaccin Immunother. 2021;17(8):2678–90. doi: 10.1080/21645515.2021.1888621. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sharing policy, including restrictions, of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA is available at http://engagezone.msd.com/ds_documentation.php through the EngageZone site or via e-mail to dataaccess@merck.com.


