Abstract
Isthmic spondylolisthesis is a condition characterized by the subluxation of one vertebral body over the adjacent inferior vertebral body, secondary to a defect in the pars interarticularis. This paper reports two cases of young acrobatic gymnasts who presented with long-term, progressive lumbosciatic pain and lower limb dysesthesia. One gymnast presented with additional neurogenic bladder dysfunction. Diagnostic testing revealed L5-S1 spondylolisthesis due to bilateral isthmic lysis in both gymnasts. Both underwent L4-S2 fixation followed by L5-S1 transdiscal arthrodesis with Rialto sacroiliac fusion system (Medtronic®, Minneapolis, MN, USA). Favorable evolution of neuromotor symptoms was observed after rehabilitation, with less residual neurological impairment in the case of higher-grade spondylolisthesis. This case series aims to emphasize the importance of recognizing this pathology in athletes as well as its correct management. Early surgical intervention can prevent the onset and progression of neurological deficits.
Keywords: rehabilitation, orthopedic procedures, spondylolisthesis, neurogenic bladder, sciatica
Introduction
Spondylolisthesis results from an anterior, posterior, or lateral translation of a vertebral body relative to its caudal vertebral body [1]. Isthmic spondylolisthesis (IS) corresponds to an injury of the pars interarticularis (PI) which can occur from stress fractures (type IIA), elongation (type IIB), or acute fractures (type IIC) [2-4]. The result is a progressive anterior slippage, most commonly at the L5-S1 vertebral level [1,2].
The degree of the subluxation is categorized according to Meyerding’s classification (grade I: <25%; grade II: 25-50%; grade III: 50-75%; grade IV: 75-100%; grade V: >100%). This scale allows the distinction between low-grade spondylolisthesis (grades I and II), high-grade spondylolisthesis (grades III and IV), and spondyloptosis (grade V) [5]. The Wiltse classification is based on etiology and anatomical factors and may be divided into I - dysplastic; II - isthmic; III - degenerative; IV - traumatic; V - pathological; and VI - iatrogenic [4].
Clinical presentation includes lower back pain with or without radicular symptoms and, rarely, bladder and/or bowel dysfunction [1-3]. There is no clear consensus regarding management, with treatment options ranging from conservative measures for asymptomatic patients or those with mild symptoms to surgical treatment in the face of neurological compromise [2]. Spondylolysis and IS can cause significant morbidity in adolescent gymnasts, occurring in approximately 11%, with repeated trauma and hyperextension of the lumbar spine as the likely injury mechanism [1,3,6,7]. This paper describes two cases of sports-related IS at L5-S1 with partial recovery of neurological deficits.
Case presentation
Case one
An 18-year-old female acrobatic gymnast presented with chronic low back pain radiating to the lower limbs (asymmetrical radiation with left predominance) and dysesthesia in the L5 territory for four years. She had normal osteotendinous reflexes, absence of motor deficits, and positive Lasègue’s sign on the left lower limb. Dynamic radiography (DR) revealed grade V spondylolisthesis at L5-S1 and the presence of instability (Figure 1). Magnetic resonance imaging (MRI) showed grade V anterolisthesis at L5 with bilateral isthmic lysis (Figure 2). Electroneuromyography confirmed radiculopathy of the left L5 nerve root (Appendices). The patient underwent surgical intervention using a posterior approach for fixation of L4-S2 with transpedicular screws, L5 laminectomy, insertion of reduction screws, L5-S1 discectomy, and placement of an autologous bone graft. The Rialto sacroiliac fusion system (Medtronic®, Minneapolis, MN, USA) [8] was used to promote L5-S1 fusion (Figures 2, 3). The patient subsequently showed significant improvement in self-reported pain; however, she maintained hypoesthesia in the territory of L5, S1, and S2 on the left lower limb. Pregabalin (150 mg per day) was introduced to manage dysesthesia, and discontinuation of acrobatic gymnastics was recommended.
Figure 1. Dynamic radiography with evidence of lumbar hyperlordosis and spondyloptosis in case one.
A: Hyperextension. B: Neutral position. C: Hyperflexion.
Figure 2. Case one. A: Magnetic resonance imaging of the lumbosacral spine showing grade V spondylolisthesis (circle). B: Postoperative control computed tomography with an illustration of the Rialto sacroiliac arthrodesis system (Medtronic®, Minneapolis, MN, USA).
Figure 3. Postoperative control lumbosacral radiographs in case one.
A: Anteroposterior view. B: Lateral view.
Case two
A 19-year-old female acrobatic gymnast presented with left lumbosciatic pain associated with dysesthesia in L5 and S1 territories as well as urinary urgency episodes for the past three years. She presented a positive Lasègue’s sign on the left lower limb and sensory deficits in the corresponding regions. DR (Figure 4) and MRI (Figure 5) showed grade III spondylolisthesis at L5-S1 due to bilateral isthmic lysis, compromise of the S1 roots, and an occult spina bifida. Electroneuromyography confirmed radiculopathy of the left S1 root with signs of active denervation. The urodynamic study evidenced a neurogenic bladder with the presence of uninhibited detrusor contraction; however, it demonstrated preserved bladder sensitivity and capacity (Appendices). Transpedicular instrumentation of L4-S1 was subsequently performed, with the placement of bilateral sacroiliac screws at S2, L5 laminectomy, and L5-S1 transdiscal arthrodesis with Rialto cylinder (Medtronic®) [8]. As with the first case, the correct positioning of the osteosynthesis material was verified on imaging examination (Figures 3, 6). The patient maintained hypoesthesia in the left gluteal region, and a rehabilitation program with home exercises and suspension of sports practice was recommended.
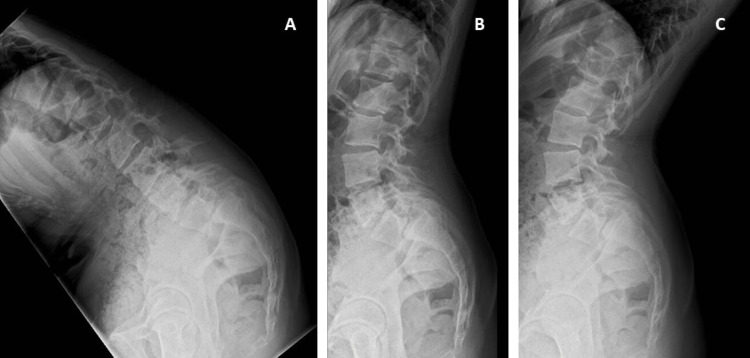
Figure 4. Dynamic radiography with accentuation of lumbar curvature and grade III spondylolisthesis in case two.
A: Hyperflexion. B: Neutral position. C: Hyperextension.
Figure 5. Case 2. A: Magnetic resonance imaging of the lumbosacral spine showing grade III spondylolisthesis (circle). B: Postoperative control computed tomography with an illustration of the Rialto sacroiliac arthrodesis system ((Medtronic®, Minneapolis, MN, USA)).
Figure 6. Postoperative control lumbosacral radiographs in case two.
A: Anteroposterior view. B: Lateral view.
Discussion
IS affects 4-8% of the general population [9,10], with a higher prevalence in gymnasts [7,11], especially female athletes (11%) [11,12]. It is usually found at the L5-S1 vertebral level due to the instability of the PI, as described in the presented cases [1]. A defect in this structure leads to anterior subluxation and, consequently, stress fractures [1,4].
The most common clinical symptom is mechanical lower back pain [1-3,10]. Acute IS may also present with impaired bowel and/or bladder function, in addition to motor/sensory deficits of the lower limbs, as observed in case two. On the other hand, in chronic IS, radicular symptoms are more frequent, which is consistent with the clinical presentation of case one [3].
Diagnosis is generally performed with DR, allowing for assessment of spondylolisthesis severity, but MRI is the gold standard in patients with neurological symptoms, possibly requiring surgical intervention [2]. The decision for surgical intervention depends on the severity and persistence of symptoms, neurological impairment, degree of subluxation, inherent instability, and impact on function [2]. In both athletes, the pain was affecting their ability to walk, limiting their practice of gymnastics. Despite the lower degree of spondylolisthesis in case two, her bladder function was also compromised.
Several surgical techniques are available for the treatment of spondylolisthesis, but there is still no consensus regarding which is most effective [3,13]. In the above cases, in addition to L4-S2 fixation and L5 laminectomy, the cylindrical Rialto device (Medtronic®) was used to promote L5-S1 arthrodesis (Figure 6). Although this material was initially designed to facilitate sacroiliac joint arthrodesis, it has already demonstrated its utility in the surgical treatment of this pathology. The authors found two cases of grade III spondylolisthesis reported in the literature in which this arthrodesis system was adopted [14]. The results were positive in terms of symptoms, sagittal balance, deformity correction, and complication rate [14].
Curiously, the patient with greater neurological impairment (radicular symptoms and neurogenic bladder) had a less severe anatomical lesion (grade III vs. grade V). Both patients participated in a rehabilitation program integrating physiotherapy and hydrotherapy, with significant improvement in pain and sensory deficits. They performed daily physiotherapy for four weeks, which consisted of neurosensory and proprioceptive stimulation of the lower limbs, strengthening of the dorsolumbar muscles, postural re-education exercises, and desensitization massage of the surgical scar. In the following three weeks, they started hydrotherapy every two days. It included water gait training with progressive loads for strengthening the core and lower limb muscles, proprioceptive training, and effort reconditioning.
Conclusions
Sports-related IS can result in serious clinical sequelae. This case series intends to highlight the importance of early diagnosis in the management of IS in gymnasts. Early intervention may prevent the onset and progression of neurological deficits, as well as promote functional recovery. Additionally, further evidence is required to determine the best approach for the management of IS, and the novel surgical technique used in this case series, using the Rialto system to promote healing, should be investigated as an alternative surgical strategy.
Appendices
Figure 7. Electroneuromyography in case one.
Figure 8. Urodynamic study in case two.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.High-grade lumbar spondylolisthesis. Beck AW, Simpson AK. Neurosurg Clin N Am. 2019;30:291–298. doi: 10.1016/j.nec.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Management of high-grade spondylolisthesis. Kasliwal MK, Smith JS, Kanter A, Chen CJ, Mummaneni PV, Hart RA, Shaffrey CI. Neurosurg Clin N Am. 2013;24:275–291. doi: 10.1016/j.nec.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Spondylolysis and spondylolisthesis in children and adolescents: I. Diagnosis, natural history, and nonsurgical management. Cavalier R, Herman MJ, Cheung EV, Pizzutillo PD. J Am Acad Orthop Surg. 2006;14:417–424. doi: 10.5435/00124635-200607000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Classification of spondylolisis and spondylolisthesis. Wiltse LL, Newman PH, Macnab I. https://pubmed.ncbi.nlm.nih.gov/1277669/ Clin Orthop Relat Res. 1976:23–29. [PubMed] [Google Scholar]
- 5.Classification in brief: the Meyerding classification system of spondylolisthesis. Koslosky E, Gendelberg D. Clin Orthop Relat Res. 2020;478:1125–1130. doi: 10.1097/CORR.0000000000001153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lumbar spondylolysis. A study of natural progression in athletes. Congeni J, McCulloch J, Swanson K. Am J Sports Med. 1997;25:248–253. doi: 10.1177/036354659702500220. [DOI] [PubMed] [Google Scholar]
- 7.Prevalence of spondylolisthesis in a population of gymnasts. Toueg CW, Mac-Thiong JM, Grimard G, Parent S, Poitras B, Labelle H. Stud Health Technol Inform. 2010;158:132–137. [PubMed] [Google Scholar]
- 8.Medtronic. [ Nov; 2022 ]. 2023. https://www.medtronic.com/us-en/index.html https://www.medtronic.com/us-en/index.html
- 9.Isthmic spondylolisthesis. Ganju A. Neurosurg Focus. 2002;13:0. doi: 10.3171/foc.2002.13.1.2. [DOI] [PubMed] [Google Scholar]
- 10.Spondylolysis: a critical review. Standaert CJ, Herring SA. Br J Sports Med. 2000;34:415–422. doi: 10.1136/bjsm.34.6.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Current evidence regarding the etiology, prevalence, natural history, and prognosis of pediatric lumbar spondylolysis: a report from the Scoliosis Research Society Evidence-Based Medicine Committee. Crawford CH 3rd, Ledonio CG, Bess RS, et al. Spine Deform. 2015;3:12–29. doi: 10.1016/j.jspd.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 12.Spondylolysis in the female gymnast. Jackson DW, Wiltse LL, Cirincoine RJ. https://pubmed.ncbi.nlm.nih.gov/132328/ Clin Orthop Relat Res. 1976:68–73. [PubMed] [Google Scholar]
- 13.Surgical treatment of high-grade spondylolisthesis: technique and results. Rivollier M, Marlier B, Kleiber JC, Eap C, Litre CF. J Orthop. 2020;22:383–389. doi: 10.1016/j.jor.2020.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sacro-iliac joint fusion system for high-grade spondylolisthesis using "Reverse Bohlman technique": a technical report and overview of the literature. Sharma M, Aljuboori Z, Clouse JW, Rodgers R, Altstadt T. World Neurosurg. 2019;124:331–339. doi: 10.1016/j.wneu.2019.01.041. [DOI] [PubMed] [Google Scholar]