Abstract
Purpose of Review
Health literacy is fundamental to primary and primordial prevention of atherosclerotic vascular disease (ASCVD) in children and adolescents. Here we summarize essential components of interventions which address health literacy challenges to reduce ASCVD risk in youth.
Recent Findings
There is a global pandemic of suboptimal health behaviors among youth that may contribute to the increasing rates of ASCVD worldwide. Deficiencies in youth cardiovascular health have promoted increased attention to health education that incorporates health literacy. Studies conducted in both the child (0 to 9 years) and adolescent (10 to 17 years) population have shown improvement in health knowledge, health behaviors such as physical activity and eating habits, and objective measures such as body mass index (BMI), blood pressure, and serum lipid levels. The available literature affirms that the involvement of family and community members in young people’s surroundings—including parents, teachers, and peers—can influence educational interventions’ protective effects.
Summary
Educational interventions which incorporate health literacy have demonstrated potential to address ASCVD risk factors in youth and may be augmented by caregiver and community involvement.
Keywords: Primordial prevention, Primary prevention, Atherosclerosis, Cardiovascular disease, Health literacy, Youth
Introduction
Atherosclerosis is a lifelong disease, with vascular remodeling occurring throughout the lifespan [1–4]. Individuals with cardiovascular risk factors have 6 to 12 times greater likelihood of having or being diagnosed with atherosclerotic cardiovascular disease (ASCVD) in their lifetime [4]. Commonly recognized ASCVD risk factors include obesity, smoking, poor diet, low physical activity levels, inadequate sleep, elevated cholesterol, hypertension, and elevated blood glucose [5, 6]. The pathogenesis of atherosclerosis may even initiate in utero, as exposure to maternal pre-eclampsia is associated with ASCVD in offspring [7, 8]. Postmortem data show over 50% of youth by the ages 2 to 15 years have evidence of early ASCVD [2, 9]. Given the prevalence of ASCVD at an early age, prevention efforts in youth are paramount.
The presence and severity of ASCVD risk factors may be exacerbated by an individual’s social context, including level of education and health literacy [10–12]. Health literacy, as defined by the World Health Organization, is the “degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” [11] Therefore, knowledge-based or behavior modification interventions designed to prevent the development of ASCVD must be implemented in ways that are feasible and appropriate for an individual’s social context [10, 13]. Data suggest that the implementation of accessible educational interventions that are appropriate to the participants’ level of health literacy can effectively reduce ASCVD risk and its development. In this review, we assess the central role of health literacy in educational and behavioral modification interventions targeting primordial and primary prevention in youth.
Health Literacy as a Social Determinant of Health
Social deprivation contributes to ASCVD risk in youth and towards limited opportunities for health-related education and health literacy. Youth health literacy is shaped by educational access, financial limitations, and other social determinants of health (SDOH). Data from China demonstrate decreased number of ideal cardiovascular health factors in children from families of lower education and lower income levels [14]. In a cross-sectional study conducted in a European cohort of 2100 adolescents, those that pursued apprenticeships rather than vocational or general academic high schools had poorer diets (43.6% vs. 35.7% vs 26.6%; p < 0.001) and were more likely to have BMI > 95th percentile (16.2% vs. 8.9% and 4.2%; p < 0.001) [5, 15]. Adverse childhood experiences such as physical or psychological abuse, caregiver substance use disorders, and intimate partner violence in the home are additionally associated with suboptimal health behaviors, thereby exacerbating ASCVD risk [16•, 17]. Children with 4 or greater adverse childhood experiences, in comparison to those with none, are twice as likely to smoke (OR 2.2; CI, 1.7–2.9), 1.6 times more likely to have a BMI ≥ 35 kg/m2 (OR 1.6; CI, 1.2–2.1), and twice as likely to be diagnosed with ischemic heart disease (OR 2.2; CI, 1.3–3.7) in adulthood [17]. Children from families with lower incomes are also more likely to experience an increased number of adverse childhood experiences than children from families with middle or higher incomes [18]. Associations between social determinants of health and ASCVD risk factors further emphasize the need for risk mitigation in youth through targeted, educationally appropriate programming.
Health Literacy Affects Youths’ Health Knowledge and Behaviors
Knowledge and awareness of ASCVD are fundamentally limited in youth. In a survey of 331 young women 15 to 24 years old, only 10% correctly identified heart disease as the leading cause of death for women [19]. A qualitative study conducted in the UK found that although most adolescents had heard of cardiovascular disease, and all knew the risk of disease was augmented by unhealthy lifestyle practices, some thought that lifestyle changes did not need to occur until they were older as participants perceived ASCVD as a disease acquired in middle age [20]. Participants also had difficulty specifically describing how lifestyle behaviors were associated with ASCVD. Integral gaps in ASCVD knowledge, the prominence of risk factors, and suboptimal health behaviors emphasize the need for educational interventions in youth.
Deficiencies in youth health behaviors and objective health factors have been well-established globally [14, 15, 21, 22]. In an analysis of data from the National Health and Nutrition Examination Survey from 2005 to 2010, none of 4673 participants ages 12 to 19 reported having an ideal Healthy Diet Score [23]. Additionally, more than one-third had poor smoking status and a BMI that did not fit the ideal benchmark. Such rates of cardiovascular health behaviors are similar to data obtained from Chinese, European, and Caribbean cohorts [14, 15, 21, 22]. The presence of ASCVD risk factors in youth has been predictive of physiologic markers of ASCVD [24]. An analysis of data from 387 healthy Italian adolescents showed inverse associations between cardiovascular health scores and carotid-femoral pulse wave velocity, a validated marker of atherosclerosis [24].
Interventions Considering Health Literacy in Children
Beginning in 2009, an international group of three cluster-randomized controlled trials ranging in size from 500 to 2000 children was sequentially conducted using a structured preschool-based educational intervention designed to reduce ASCVD development [25–27, 28••]. The trials were conducted in Bogotá, Colombia, Madrid, Spain, and New York, New York. All three trials assessed the effect of a program focused on changing knowledge, attitudes, and habits towards healthy nutrition and physical activity. The intervention consisted of 30–50 h of structured curricula focused on physiology, nutrition, and physical activity. Each intervention was designed for participants’ current level of level of education. Activities included age-appropriate stories, videos, games, and songs [29]. Parents and families also attended school-wide events and were encouraged to participate in take-home exercises. Preschools in Bogotá were chosen specifically prior to randomization to ensure representation of migrant Colombian unprivileged communities [26]. The Spanish trial was designed using stratified randomization based to accommodate for varied immigrant backgrounds and household incomes at each of the preschools [30]. The American trialists chose to conduct the intervention in the Harlem neighborhood of New York, an underserved, urban, ethnically, and racially diverse community. Hence, the investigators assessed the intervention in socially diverse preschools where students encountered additional challenges of social determinants of health.
Knowledge, attitude, and habits were measured using standardized instruments administered by trained professionals. Questionnaire items included “location of the heart,” “recognizes a variety of possibilities for carrying out physical activity,” identifying inappropriate nutrition “once in a while foods,” and quantifying recent type of food consumption and physical activity [26]. In all three trials, children in the intervention groups demonstrated statistically significant increases in knowledge, attitude, or habit sub-scores immediately post-intervention. Analyses conducted in the Colombian cohort at 3 years post-intervention showed improvements in composite knowledge, attitude, and habit scores. The American cohort showed a dose–response effect of the educational intervention, as children who participated in > 75% of modules had a larger change in scores than those who participated in 50–75%, and those with < 50% completion showed the least improvement. The Spanish and American cohorts noted an increase in composite knowledge, attitude, and habit scores in children from families from higher educational backgrounds and higher incomes, reflective of an association between socioeconomic status and ideal health [28••, 30]. In the Colombian cohort, at the 3-year timepoint, 540 children underwent additional physiologic measurements. BMI ranges were defined using Centers for Disease Control and Prevention growth charts. Sixty-two children went from the underweight to normal weight category, and 91 went from being overweight/obese to normal weight category. The Spanish and American cohorts did not show such changes in BMI. All three trials demonstrated meaningful and sustained improvements in awareness of ASCVD and risk factor modification.
Another educational trial conducted in Brazil among older children showed similar results [31]. The educational intervention, tailored towards children 7–11 years old, consisted of an 8-week after-school workshop series with sessions lasting 30 to 90 min each. The workshops included art activities, games, music, dance, and real-life simulations that all centered around healthy habits and cardiovascular health at an appropriate literacy level. Baseline questionnaires assessed cardiovascular knowledge, and participant knowledge was reassessed after completion of the intervention. The 79 participants were all enrolled from an after-school program for children of lower income backgrounds. The results of this study showed that children in the intervention group had a 1.4-point increase in knowledge of health habits immediately post-intervention on a 5-point scale, which was sustained at a 1-point increase at 3 months (1.4, CI 0.9–2.0 vs 1.0, CI 0.3–1.6; p < 0.001). This trial affirms the use of educational programming in children in an older age range.
Interventions Considering Health Literacy in Adolescents
Educational interventions in adolescents demonstrate similar shifts in ASCVD risk factor management as those in children. Project Healthy Schools, an initiative from the University of Michigan and local community organizations, is a school-based program designed to promote healthier choices to reduce youth obesity and long-term ASCVD risk [32, 33]. The 10-week program focuses on diet and physical activity behavior change through ten 20-min interactive educational modules during the school day. Prospective studies of the intervention recorded outcomes of health behavior change after program completion, including dietary habits, physical activity, sedentary activity, and physiological outcomes including serum lipid levels, blood pressure, random blood glucose, and BMI.
Separately, two prospective studies of 1100–4000 middle school students in Michigan showed post-participation improvement in physical activity, with the larger study showing increases in participation in both moderate (3.16 to 3.54 days per week; p < 0.001) and vigorous (4.13 to 4.52 days per week; p < 0.001) physical activity [32]. In the larger of the two studies, significant dietary improvement defined as improved fruit and vegetable intake was shown as well. Among objective measures, improvement in serum cholesterol markers were noted in both studies. The larger study also found significant decreases in random blood glucose (97.51 ± 16.00 to 94.94 ± 16.62; p < 0.001), systolic blood pressure (109.47 ± 15.26 mm Hg to 107.76 ± 10.87 mm Hg; p < 0.001), and diastolic blood pressure (64.78 ± 8.57 mm Hg to 63.35 ± 7.81 mm Hg; p < 0.001) [32]. The median income of families whose children participated in the larger study ranged from $28,610 to $56,612. Project Healthy Schools, in successfully teaching students from economically limited backgrounds, reaffirms the importance of accessible and grade-relevant programming in ASCVD prevention.
Similar to Project Healthy Schools, the “Wizards of Motion Cardiovascular Disease Prevention Module” focused on ASCVD and its prevention, but did so through experimental learning [34]. The educational module was designed to introduce basic cardiac physiology to 5th grade students to help them identify relationships between the cardiovascular system and health habits, such as healthy food intake, smoking avoidance, and regular physical exercise. Students were randomized to either the intervention group that received the educational module or a control group that received standard school curriculum. After an age-appropriate educational presentation, students participated in a model-based laboratory activity designed to simulate restriction of coronary artery flow using rubber tubing, flow valves, clamps, and colored water. Assessment of knowledge and attitudes towards ASCVD prevention followed the educational intervention. Students who participated in the module had a greater than 60% increase in knowledge test (28.21% vs 94.87%; p < 0.01) as well as greater than 10% increase in the attitude test score (72.67% vs 83.15%; p < 0.01) [34].
Need for Family and Community Integration
Parental health literacy has a crucial contribution towards health of children and adolescents and is associated with the cardiovascular health of youth. In children with type 1 diabetes mellitus, data have demonstrated an almost 2-point increase in mean hemoglobin A1c percentage in children with caregivers of limited health literacy (10.4 ± 2.2% vs 8.6 ± 1.7%; p < 0.001) [35]. Family-based conversation about ASCVD is associated with improvements in health-related knowledge among children and adults [36]. Limited parental health literacy is associated with increased ASCVD risk factor prevalence in youth, such as increased rates of adolescent obesity [37]. Health literacy of both caregivers and youth are instrumental in ASCVD prevention, as outlined in the proposed mechanism in Fig. 1, and should be targeted in future education-based interventions.
Fig. 1.
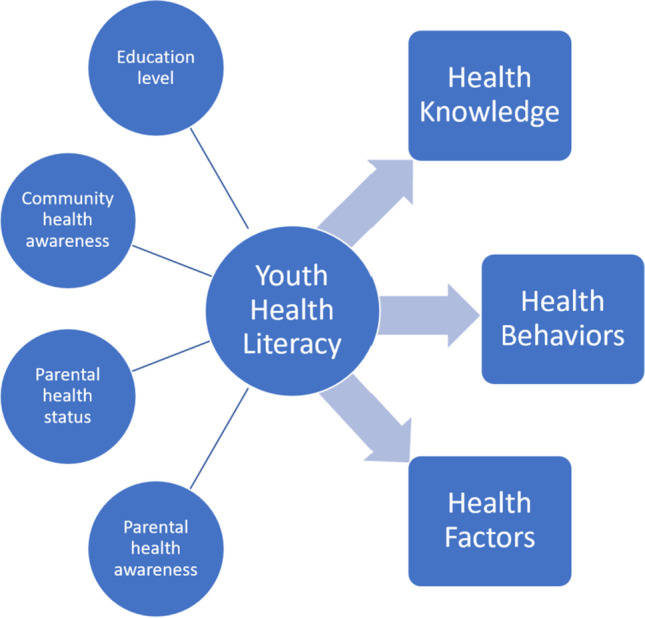
Conceptual framework for youth health literacy
Educational programs for youth which include family members have shown stronger lifestyle changes in both caregivers and youth [38]. For example, in a study from China of 603 5th graders, a 3.5-month school-based salt-reduction education program was conducted [39]. The aim of this study was to examine the educational intervention’s effect on the adolescents’ salt-related behaviors, as well as examine associations between the adolescents’ salt-related behaviors and behaviors of those within their social network, including their family members, teachers, and peers. Salt-related behaviors were measured by a survey validated by 24-urine collection in 135 of the participants. The survey asked questions regarding frequency of eating salty snacks and whether participants’ families were incorporating salt reduction practices in their lifestyles, with a max score of 9 indicating the highest-number of salt-reduction behaviors.
Results collected 9 months after completion of the educational program demonstrated that adolescents from families less supportive of salt reduction had lower salt-reduction behavior scores (− 1.1, 95% CI − 1.6 to − 0.6; p < 0.0001) [39]. The approach of family integration may apply to the broader unit of community as well. Youth at schools with teachers and principals who received additional education and training about salt-reduction also had higher salt-reduction behaviors, in comparison to youth at schools whose teachers and principals did not participate in additional training (+ 0.33; 95% CI 0.01 to 0.64; p = 0.043) [39]. In an associated study conducting the same intervention among 832 youth and 553 family members, family members who received educational programming regarding salt intake and hypertension at the same time as adolescents had a 2.9 g decreased salt intake as calculated by 24-h urinary sodium in comparison to families in the control group who received a standard school curriculum (− 2.9, CI − 3.7 to − 2.2; p < 0.001) [40]. These studies suggests that the optimal educational intervention to bolster ASCVD prevention in youth focuses not only on the health literacy of the child, but of the parent and their surrounding community too.
Conclusion
Health literacy contributes to cardiovascular risk in children and adolescents. Programs that provide accessible education with appropriate tailoring to participants’ level of education have demonstrated success in increasing ASCVD knowledge, healthy behaviors, and healthy habits. Further adding to the known associations of sociodemographic factors such as health literacy and other SDOH, the available data suggest that caregiver and community involvement in educational interventions can enhance the interventions’ effects on children and adolescent’s lifestyle behaviors.
Funding
Harnoor K. Mann reports a research grant NHLBI R38HL150207-03.
Jared W. Magnani reports a research grant NHLBI R33HL144669.
Amber E. Johnson reports a research grant NHLBI R33HL144669.
Compliance with Ethical Standards
Conflict of Interest
Amber E. Johnson reports a Research Award from Women as One Foundation. She also reports consulting fees from Sanofi, payment or honoraria from Howard University, and leadership or fiduciary role for Clue by Biowink, Medical Board Member. Other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Harnoor K. Mann, Email: mannhk@upmc.edu
Jared W. Magnani, Email: magnanij@pitt.edu
Amber E. Johnson, Email: johnsonae2@upmc.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Hong YM. Atherosclerotic cardiovascular disease beginning in childhood. 2010; (1738–5555 (Electronic)). [DOI] [PMC free article] [PubMed]
- 2.Berenson GS, Wattigney Wa Fau - Tracy RE, Tracy Re Fau - Newman WP, 3rd, Newman Wp 3rd Fau - Srinivasan SR, Srinivasan Sr Fau - Webber LS, Webber Ls Fau - Dalferes ER, Jr., et al. Atherosclerosis of the aorta and coronary arteries and cardiovascular risk factors in persons aged 6 to 30 years and studied at necropsy (The Bogalusa Heart Study). 1992; (0002–9149 (Print)). [DOI] [PubMed]
- 3.McGill HC, Jr., McMahan CA. Determinants of atherosclerosis in the young. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. 1998; (0002–9149 (Print)). [DOI] [PubMed]
- 4.Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PWF, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113(6):791–798. doi: 10.1161/Circulationaha.105.548206. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd-Jones Dm Fau - Hong Y, Hong Y Fau - Labarthe D, Labarthe D Fau - Mozaffarian D, Mozaffarian D Fau - Appel LJ, Appel Lj Fau - Van Horn L, Van Horn L Fau - Greenlund K, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010; (1524–4539 (Electronic)) 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed]
- 6.Lloyd-Jones Dm Fau - Allen NB, Allen Nb Fau - Anderson CAM, Anderson Cam Fau - Black T, Black T Fau - Brewer LC, Brewer Lc Fau - Foraker RE, Foraker Re Fau - Grandner MA, et al. Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health: a presidential advisory from the American Heart Association. 2022; (1524–4539 (Electronic)). [DOI] [PMC free article] [PubMed]
- 7.Andraweera PA-O, Gatford KA-O, Care AS, Bianco-Miotto T, Lassi ZS, Dekker GA, et al. Mechanisms linking exposure to preeclampsia in utero and the risk for cardiovascular disease. 2020; (2040–1752 (Electronic)). [DOI] [PubMed]
- 8.Nahum Sacks K, Friger M, Shoham-Vardi I, Spiegel E, Sergienko R, Landau D, et al. Prenatal exposure to preeclampsia as an independent risk factor for long-term cardiovascular morbidity of the offspring. 2018; (2210–7797 (Electronic)). [DOI] [PubMed]
- 9.Stary HC. Evolution and progression of atherosclerotic lesions in coronary arteries of children and young adults. 1989; (0276–5047 (Print)). [PubMed]
- 10.Magnani Jw Fau - Mujahid MS, Mujahid Ms Fau - Aronow HD, Aronow Hd Fau - Cené CW, Cené Cw Fau - Dickson VV, Dickson Vv Fau - Havranek E, Havranek E Fau - Morgenstern LB, et al. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. 2018; (1524–4539 (Electronic)). [DOI] [PMC free article] [PubMed]
- 11.Parker R, Ratzan SC. Health literacy: a second decade of distinction for Americans. 2010; (1087–0415 (Electronic)). [DOI] [PubMed]
- 12.Schillinger D. The intersections between social determinants of health, health literacy, and health disparities. 2020; (1879–8365 (Electronic)). [DOI] [PMC free article] [PubMed]
- 13.Arnett Dk Fau - Blumenthal RS, Blumenthal Rs Fau - Albert MA, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. 2019; (1524–4539 (Electronic)).
- 14.Dong H, Yan Y, Liu J, Zhao X, Cheng H, Hou D, et al. Alarming trends in ideal cardiovascular health among children and adolescents in Beijing, China, 2004 to 2014. Int J Cardiol. 2017;231:264–270. doi: 10.1016/j.ijcard.2016.12.027. [DOI] [PubMed] [Google Scholar]
- 15.Gande N, Pechlaner R, Bernar B, Staudt A, Stock K, Hochmayr C, et al. Cardiovascular health behaviors and associations of sex, age, and education in adolescents - Results from the EVA Tyrol study. Nutr Metab Cardiovasc Dis. 2021;31(4):1286–1292. doi: 10.1016/j.numecd.2020.11.002. [DOI] [PubMed] [Google Scholar]
- 16.•.Suglia Sf Fau - Koenen KC, Koenen Kc Fau - Boynton-Jarrett R, Boynton-Jarrett R Fau - Chan PS, Chan Ps Fau - Clark CJ, Clark Cj Fau - Danese A, Danese A Fau - Faith MS, et al. Childhood and adolescent adversity and cardiometabolic outcomes: a scientific statement from the American Heart Association. 2018; (1524–4539 (Electronic)). Scientific statement from the American Heart Assciation outlining the effects of adverse childhood experiences oncardiometabolic outcomes. [DOI] [PMC free article] [PubMed]
- 17.Felitti VJ, Anda Rf Fau - Nordenberg D, Nordenberg D Fau - Williamson DF, Williamson Df Fau - Spitz AM, Spitz Am Fau - Edwards V, Edwards V Fau - Koss MP, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Adverse Child Experiences (ACE) Study. 1998; (0749–3797 (Print)). [DOI] [PubMed]
- 18.Slopen N, Shonkoff JP, Albert MA, Yoshikawa H, Jacobs A, Stoltz R, et al. Racial disparities in child adversity in the U.S.: interactions with family immigration history and income. 2016; (1873–2607 (Electronic)). [DOI] [PubMed]
- 19.Gooding HC, Brown CA, Liu J, Revette AC, Stamoulis C, de Ferranti SD. Will teens go red? Low cardiovascular disease awareness among young women. J Am Heart Assoc. 2019;8(6):e011195. doi: 10.1161/JAHA.118.011195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Newby K, Varnes L, Yorke E, Meisel SF, Fisher A. Illness risk representation beliefs underlying adolescents’ cardiovascular disease risk appraisals and the preventative role of physical activity. Br J Health Psychol. 2020;25(1):171–188. doi: 10.1111/bjhp.12400. [DOI] [PubMed] [Google Scholar]
- 21.Pengpid S, Peltzer K. Ideal cardiovascular health behaviours in nationally representative school-based samples of adolescents in the Caribbean. Vasc Health Risk Manag. 2021;17:187–194. doi: 10.2147/VHRM.S302168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Henriksson P, Henriksson H, Gracia-Marco L, Labayen I, Ortega FB, Huybrechts I, et al. Prevalence of ideal cardiovascular health in European adolescents: the HELENA study. Int J Cardiol. 2017;240:428–432. doi: 10.1016/j.ijcard.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 23.Shay CM, Ning H Fau - Daniels SR, Daniels Sr Fau - Rooks CR, Rooks Cr Fau - Gidding SS, Gidding Ss Fau - Lloyd-Jones DM, Lloyd-Jones DM. Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005–2010. 2013; (1524–4539 (Electronic)). [DOI] [PubMed]
- 24.Pucci G, Bisogni V, Battista F, D’Abbondanza M, Anastasio F, Crapa ME, et al. Association between ideal cardiovascular health and aortic stiffness in Italian adolescents The MACISTE study. Nutri Metab Cardiovasc Dis : NMCD. 2021;31(9):2724–32. doi: 10.1016/j.numecd.2021.05.035. [DOI] [PubMed] [Google Scholar]
- 25.Cespedes J, Briceno G, Farkouh ME, Vedanthan R, Baxter J, Leal M, et al. Promotion of cardiovascular health in preschool children: 36-month cohort follow-up. Am J Med. 2013;126(12):1122–1126. doi: 10.1016/j.amjmed.2013.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cespedes J, Briceno G, Farkouh ME, Vedanthan R, Baxter J, Leal M, et al. Targeting preschool children to promote cardiovascular health: cluster randomized trial. Am J Med. 2013;126(1):27–35.e3. doi: 10.1016/j.amjmed.2012.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Penalvo JL, Santos-Beneit G, Sotos-Prieto M, Martinez R, Rodriguez C, Franco M, et al. A cluster randomized trial to evaluate the efficacy of a school-based behavioral intervention for health promotion among children aged 3 to 5. BMC Public Health. 2013;13:656. doi: 10.1186/1471-2458-13-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.••.Fernandez-Jimenez R, Jaslow R, Bansilal S, Santana M, Diaz-Munoz R, Latina J, et al. Child health promotion in underserved communities: the FAMILIA trial. J Am Coll Cardiol. 2019;73(16):2011–2021. doi: 10.1016/j.jacc.2019.01.057. [DOI] [PubMed] [Google Scholar]
- 29.Peñalvo JL, Sotos-Prieto M Fau - Santos-Beneit G, Santos-Beneit G Fau - Pocock S, Pocock S Fau - Redondo J, Redondo J Fau - Fuster V, Fuster V. The Program SI! intervention for enhancing a healthy lifestyle in preschoolers: first results from a cluster randomized trial. 2013;(1471–2458 (Electronic)). [DOI] [PMC free article] [PubMed]
- 30.Penalvo JL, Santos-Beneit G, Sotos-Prieto M, Bodega P, Oliva B, Orrit X, et al. The SI! program for cardiovascular health promotion in early childhood: a cluster-randomized trial. J Am Coll Cardiol. 2015;66(14):1525–1534. doi: 10.1016/j.jacc.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 31.Cecchetto FH, Pena DB, Pellanda LC. Playful interventions increase knowledge about healthy habits and cardiovascular risk factors in children: the CARDIOKIDS randomized study. Arq Bras Cardiol. 2017;109(3):199–206. doi: 10.5935/abc.20170107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eagle TF, Gurm R, Smith CA, Corriveau N, DuRussell-Weston J, Palma-Davis L, et al. A middle school intervention to improve health behaviors and reduce cardiac risk factors. Am J Med. 2013;126(10):903–908. doi: 10.1016/j.amjmed.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 33.Corriveau N, Eagle T, Jiang Q, Rogers R, Gurm R, Aaronson S, et al. Sustained benefit over four-year follow-up of Michigan’s project healthy schools. Am J Public Health. 2015;105(12):e19–25. doi: 10.2105/AJPH.2015.302835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Montelpare WJ, McPherson MN, Boardman K, Zerpa CE. Evaluating the wizards of motion cardiovascular disease prevention module. J School Nurs : the official publication of the National Association of School Nurses. 2018;34(5):350–358. doi: 10.1177/1059840517709074. [DOI] [PubMed] [Google Scholar]
- 35.Hassan K, Heptulla RA. Glycemic control in pediatric type 1 diabetes: role of caregiver literacy. (1098–4275 (Electronic)). [DOI] [PubMed]
- 36.Bartlo P, Irion G, Voorhees J. Assessment of the knowledge level regarding cardiovascular disease risk factors: comparison across age groups. 2020; (1573–3610 (Electronic)). [DOI] [PubMed]
- 37.Chari R, Warsh J, Ketterer T, Hossain J, Sharif I. Association between health literacy and child and adolescent obesity. 2014; (1873–5134 (Electronic)). [DOI] [PubMed]
- 38.Hopper CA, Munoz KD, Gruber MB, MacConnie S, Schonfeldt B, Shunk T. A school-based cardiovascular exercise and nutrition program with parent participation: an evaluation study. Children’s Health Care. 1996;25(3):221–235. doi: 10.1207/s15326888chc2503_5. [DOI] [Google Scholar]
- 39.Ma Y, Feng X, Ma J, He FJ, Wang H, Zhang J, et al. Social support, social network and salt-reduction behaviours in children: a substudy of the School-EduSalt trial. BMJ open. 2019;9(6):e028126. doi: 10.1136/bmjopen-2018-028126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.He FJ, Wu Y, Feng XX, Ma J, Ma Y, Wang H, et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): cluster randomised controlled trial. 2015; (1756–1833 (Electronic)). [DOI] [PMC free article] [PubMed]


