Abstract
Introduction
While COVID-19 pandemic is an ongoing threat for our lives, the rapid development of effective vaccines against COVID-19 provided us hopes for manageable disease control. However, vaccine hesitancy across the globe is a concern which could attenuate efforts of disease control. This study examined the extent and trend of vaccine hesitancy in Nigeria.
Methods
The COVID-19 National Longitudinal Phone Survey conducted between 2020 and 2021 was used for the analysis. The extent and trend of vaccine hesitancy across different zones within Nigeria, over time, as well as reasons of the hesitancy were evaluated.
Results
Vaccine hesitancy was more prevalent in southern zones, which on average have better socioeconomic status than northern zones. Overtime, vaccine hesitancy became more prevalent, and respondents became more resistant to the COVID-19 vaccine across the country.
Conclusion
While the nature of interventions to improve the uptake of COVID-19 vaccine should differ by regions due to differential barriers to vaccination, it might be important to prebunk and debunk any misinformation related to COVID-19 vaccine to mitigate the vaccine hesitancy across the country.
Keywords: COVID-19 vaccine, Vaccine hesitancy, Africa, Nigeria
1. Background
COVID-19 has been impacting our lives globally. There have been over 380 million cases of COVID-19 and about 5.7 million deaths due to COVID-19 worldwide as of September 2022 [17].
As a result of intensive scientific investments on the vaccine development, COVID-19 vaccines became available rapidly, first in developed country followed by the rest of the world. Recent studies confirmed the efficacy of COVID-19 vaccines in preventing people from contracting diseases as well as in reducing the risk of hospitalizations and deaths[14], [6], [10], [15].
Despite the availability of COVID-19 vaccines in developed countries, many countries observed that the vaccination coverage got stagnant. For example, in the U.S., the proportion of the population aged 18 or above who were fully vaccinated got stuck around 74 % [3]. Vaccine hesitancy against COVID-19 vaccine has been noted as a global issue [7], [12], [13].
In Nigeria, the study site, COVID-19 vaccines became available in early 2021 (March 5th, 2021) at no cost to recipients. However, the number of vaccines administered has been limited. By the end of April 2021, merely 1 million doses of vaccines have been administered. The limited number of vaccine administration was due to the limited scope in the eligible population: at the initial stage, the eligible recipients were only healthcare workers and other priority frontline workers [9]. Even almost one year later as of February 2022 by when all the adults over 18 years of age were eligible to receive the vaccine, however, only about 20 million doses of vaccines have been administered, which would cover around 5 % of the population with two doses [17], [11]. This low vaccination coverage might be due to various barriers. One important barrier is the insufficient supply of vaccine. It is estimated that among developing countries, the vaccines were available to cover about 20 % of the population at the end of 2021 [16].
Another potentially important barrier is vaccine hesitancy. Vaccine hesitancy is believed to be a critical issue in African countries, especially in Nigeria. For example, the Polio vaccination boycott in three northern Nigerian states in 2003, due to a suspicion about the safety of the vaccine, is a famous event that is considered to have resulted in the creation of persistent vaccine hesitancy in the region [5]. Some of recent studies pointed out the prevalence of vaccine hesitancy against COVID-19 vaccines within Nigerian context [4], [1]. These previous studies however utilized the sample that were not nationally representative. This study is the first to evaluate the extent of vaccine hesitancy against COVID-19 vaccine among the nationally-representative Nigerian sample. Furthermore, this is the first to study the change in vaccine hesitancy before and after the peak of COVID-19 cases.
2. Methods
2.1. Data
This study used COVID-19 National Longitudinal Phone Survey (NLPS) conducted in Nigeria by the National Bureau of Statistics (NBS) and the World Bank, between April 2020 to April 2021. This is a longitudinal study that followed the same respondents over time. The total of 1,950 households were followed-up from Round 1 to Round 12. Each cycle from Round 1 to Round 12 was conducted every month. The final sample at Round 12 was 1,238 households. Details on survey including sampling methods and questionnaires can be found in their website [18].
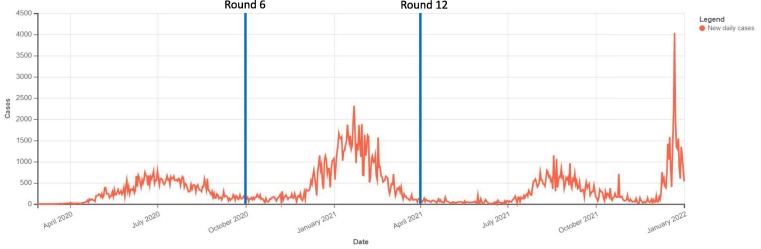
Although NLPS captured various aspects of the standard of living among respondents, this study focused on attitudes and perceptions of COVID-19 vaccines. Their perceptions and attitudes toward COVID-19 vaccine were asked only during Round 6 (2020 October), Round 10 (2021 February), and Round 12 (2021 April). In this study, we focused on Round 6 and Round 12. As presented in Fig. 1 , one of the largest peaks of COVID-19 cases occurred in between Round 6 and Round 12.
Fig. 1.
COVID-19 cases over time in Nigeria and the timing of National Longitudinal Phone Survey (NLPS).
2.2. Study design
We compared attitudes toward COVID-19 vaccine based on the geographical zones (North Central, North East, North West, South East, South South, South West), as well as over time (Round 6 vs Round 12). The number of respondents were roughly equally distributed across zones: 16.5 % in North Central, 17.6 % in North East, 16.0 % in North West, 17.9 % in South East, 13.2 % in South South, and 18.9 % in South West at Round 6. At Round 12, the distribution of respondents was as follows: 16.8 % in North Central, 22.9 % in North East, 18.5 % in North West, 13.2 % in South East, 9.6 % in South South, and 19.0 % in South West.
As this study compares the prevalence of vaccine hesitancy by geographical zones, it is important to ensure that the sample in each zone was representative. The sample frame of NLPS was based on the existing household survey called General Household Survey (GHS) conducted in 2018. In GHS, it was confirmed that the sample of households was representative nationally as well as across the geopolitical zones [18]. The response rate for NLPS based on GHS sampling was about 65 % overall, and it was confirmed that the sample in NLPS was representative at national as well as at zone level [18]. While NLPS omits many important information such as education and wealth level which might affect the vaccine hesitancy, some information around knowledge and wealth is available. To see any systematic difference in these sociodemographic characteristics by zones, Table 1 presents the difference in knowledge around coronavirus and Table 2 presents the prevalence of food security by zones. While it is widely believed that the northern Nigeria is on average less educated and less wealthy, these tables indicates that the knowledge around coronavirus is similar across zones. Food insecurity might be severer in the northern zones (Table 2; “went without eating a whole day”).
Table 1.
Knowledge of coronavirus by zone.
| Zone | To your knowledge, what measures can you adopt to reduce the risk of contracting coronavirus? (%) |
|||
|---|---|---|---|---|
| Handwashing | Use mask | Avoid crowded place | Maintain distance | |
| 1. North Central | 93.3 | 76.1 | 88.5 | 80.3 |
| 2. North East | 97.9 | 69.7 | 93.0 | 98.4 |
| 3. North West | 98.4 | 76.6 | 95.1 | 78.3 |
| 4. South East | 99.5 | 69.5 | 92.0 | 87.9 |
| 5. South South | 97.6 | 86.6 | 90.4 | 86.9 |
| 6. South West | 97.9 | 85.2 | 82.8 | 84.9 |
Table 2.
Food security by zone.
| Zone | Food security (past 30 days) |
||
|---|---|---|---|
| Needed to skip meal | Ran out of food | Went without eating a whole day | |
| 1. North Central | 70.5 | 54.9 | 21.6 |
| 2. North East | 68.4 | 52.3 | 32.8 |
| 3. North West | 65.4 | 52.8 | 28.1 |
| 4. South East | 75.6 | 59.4 | 21.0 |
| 5. South South | 76.9 | 67.6 | 17.4 |
| 6. South West | 79.2 | 55.5 | 25.6 |
We examined the answers to the following survey questions: 1) would you agree to be vaccinated against COVID-19 if available right now at no cost to you? 2) If the answer to 1. was no; then why would not you agree to be vaccinated? This is a descriptive study, and we did not conduct a statistical analysis. In other words, we observe trends mainly visually, but we did not test the statistical significance of differences.
3. Results
3.1. Prevalence of vaccine hesitancy
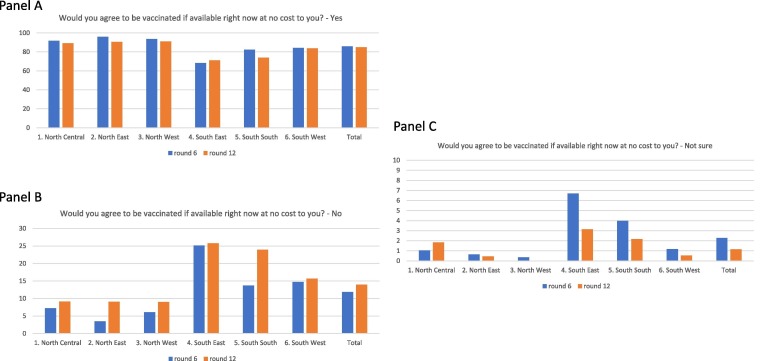
Overall, in the most recent round of survey (round 12), 84.9 % of respondents agreed to be vaccinated if the vaccine was available at no cost, while 14 % refused to agree and the remaining 1.1 % were unsure about the vaccination decision.
There exists a substantial geographical difference in the vaccine hesitancy within Nigeria. In general, northern zones have higher vaccine acceptance than southern zones. The proportion of respondents agreeing to get vaccinated in northern zones ranged from 90 to 91 %, while it ranged from 71 to 84 % in the southern zones. Similarly, we observed the higher prevalence of vaccine hesitancy in southern zones than in northern zones. The proportion of respondents refusing to get vaccinated in northern zones was about 9 %, while it ranged from 16 to 26 % in the southern zones.
Fig. 2 presents the change in vaccine acceptance and hesitancy overtime (from Round 6 to Round 12) by zone. Overtime, the proportion of respondents who agreed to get vaccinated slightly decreased for most of zones, except in South East zone. On the contrary, the proportion of respondents who refused to get vaccinated increased for all zones. The proportion of respondents who were uncertain about vaccination also mostly decreased, except for North Central zone.
Fig. 2.
Vaccine acceptance and hesitancy over time in each zone in Nigeria.
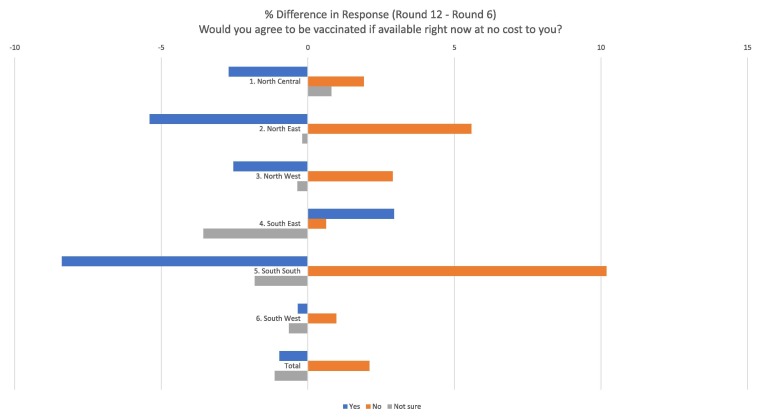
Fig. 3 presents the difference in the perception between Round 12 and Round 6. The magnitude of the increase in the vaccine hesitancy over time was generally larger than that of the decrease in the proportion of people who were uncertain of their decision.
Fig. 3.
Difference in response to "Would you agree to be vaccinated if the vaccine is available now at no cost" between Round 12 and Round 6.
3.2. Reasons of vaccine hesitancy
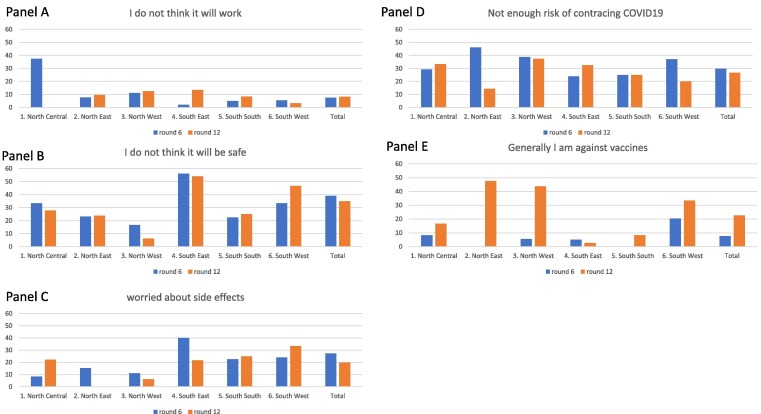
Overall, the most common reason of the vaccine hesitancy was the safety concern of COVID-19 vaccine, followed by the low-risk perception of contracting COVID-19 and concerns about side effects of COVID-19 vaccine.
Concerns around the COVID-19 vaccine itself, such as the safety concern and the concern of side effects were more prevalent in southern zones than in northern zones. For example, during Round 12, the proportion of vaccine refusers who mentioned the safety concern of COVID-19 vaccine ranged between 6 and 28 % in the northern zones, while it ranged from 25 to 54 % in the south. Similarly, the proportion of vaccine refusers who mentioned the concern for side effects of COVID-19 vaccine ranged between 0 and 22 % in the northern zones, while it ranged from 22 to 33 % in the south.
The proportion of vaccine refusers who had the low-risk perception of contracting COVID-19 vaccine was generally larger among the northern zone in the Round 6: 29 to 39 %, compared to 24 to 37 % in the south. However, this trend did not hold during the last survey, Round 12.
Fig. 4 presents reasons of vaccine hesitancy by zone, over time. The safety concern against COVID-19 vaccine became less prevalent over time, across Nigeria. However, in South South and South West, the safety concern rather increased. Similarly, the concern for the side effects of COVID-19 vaccine exhibited the similar pattern; while it became less prevalent overall, it became more prevalent in South South and South West.
Fig. 4.
Reasons of vaccine hesitancy by zone over time.
4. Discussion
This study investigated the geographical trend of vaccine acceptance and hesitancy of COVID-19 vaccine as well as reasons for hesitancy over time, based on the household survey conducted in Nigeria. This study is one of the first to investigate the trend of vaccine hesitancy over time by zone in Nigeria, using the nationally representative sample.
We found that the proportion of respondents who expressed vaccine hesitancy became higher over time, while the proportion of respondents who were uncertain about vaccination against COVID-19 and the proportion of people who could accept the vaccine decreased over time. More people who were uncertain about COVID-19 vaccine at Round 6 became hesitant to vaccine at Round 12. It is concerning to observe the upward trend of vaccine hesitancy overtime. It is concerning especially because, after experiencing the high peak of COVID-19 cases between Round 6 and Round 12 as shown in Fig. 1, respondents’ willingness to accept the COVID-19 vaccine did not improve.
We also found the substantial variations in the vaccine hesitancy geographically. We found that respondents in southern zones had higher vaccine hesitancy than those in northern zones. Historically, the average population in the southern zones are wealthier, more educated, and have higher vaccination coverage [2], [8].
The positive association between higher income level and higher prevalence of vaccine hesitancy found in this study is consistent with the country-level study which compared the prevalence of vaccine hesitancy between high income countries and low- and middle- income countries [13].
At the same time, northern zones usually have lower coverage of children’s vaccination than southern zones. For example, in Nigeria, the coverage of measles vaccination in southern zones reached 70 %, while none of the northern zones reached 60 % [8]. In other words, northern zones suffer from lower vaccination coverage although they have less prevalence of vaccine hesitancy than southern zones. These results might imply that the low vaccine uptake in the northern zones is not due to vaccine hesitancy, but rather due to other constrains, such as the weak supply chain and difficult access to the health facilities.
This study has important policy implications. The study found that the vaccine hesitancy against COVID-19 vaccine due to doubts on COVID-19 vaccine efficacy was more prevalence in southern zones than in northern zones. It is important to differentiate the type of interventions aiming for the enhanced vaccine uptake, depending on the reasons of non-vaccination. Information interventions to assure the safety of COVID-19 vaccine, as well as to debunk the misinformation around the disease and vaccine, is important to tackle the vaccine hesitancy issues in southern zones. On the other hand, easing the access barriers and improving their perceived importance of vaccines to prevent diseases might be more effective in northern zones.
At the same time, it is a concerning trend that the proportion of people who refused to receive COVID-19 vaccine increased over time, even in the northern zones. This result might imply that information regarding the COVID-19 vaccine, including the misinformation to discredit the COVID-19 vaccine efficacy might be spreading across Nigeria over time. If so, information interventions to prebunk and debunk such misinformation across the country might play a critical role.
There are several limitations in the study. First, the dropout rate of respondents from round 6 to round 12 in each zone differed substantially. This differential attrition might have created the selection bias. Results should be interpreted with caution. Second, while it might be important to compare the trend of vaccine hesitancy in Nigeria with the global trend, this comparison was not possible due to the lack of data availability. Third, the survey did not ask the information on the actual uptake of COVID-19 vaccine, thus it was not possible to analyze data based on the actual vaccination status.
5. Conclusion
The study found that vaccine hesitancy is more prevalent in the southern Nigeria where the socioeconomic status is better than the north, and the proportion of vaccine refusers increased across Nigeria over time. While the nature of interventions to improve the uptake of COVID-19 vaccine should differ by regions due to differential barriers to vaccination, it might be important to prebunk and debunk any misinformation related to COVID-19 vaccine to mitigate the vaccine hesitancy across the country.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability
The authors do not have permission to share data.
References
- 1.Adigwe O.P. COVID-19 vaccine hesitancy and willingness to pay: Emergent factors from a cross-sectional study in Nigeria. Vaccine: X. 2021;9 doi: 10.1016/j.jvacx.2021.100112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arndt C., McKay A., Tarp F. Oxford University Press; 2016. Growth and poverty in sub-Saharan Africa. [Google Scholar]
- 3.Center for Disease Control. “COVID Data Tracker” https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-people-onedose-pop-5yr accessed on Feb 3, 2022.
- 4.Iliyasu Z., Umar A.A., Abdullahi H.M., Kwaku A.A., Amole T.G., Tsiga-Ahmed F.I., et al. “They have produced a vaccine, but we doubt if COVID-19 exists”: correlates of COVID-19 vaccine acceptability among adults in Kano, Nigeria. Hum Vaccin Immunother. 2021:1–8. doi: 10.1080/21645515.2021.1974796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jegede A.S. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med. 2007;4(3):e73. doi: 10.1371/journal.pmed.0040073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin D.-Y., Yu G.u., Wheeler B., Young H., Holloway S., Sunny S.-K., et al. Effectiveness of Covid-19 Vaccines over a 9-Month Period in North Carolina. N Engl J Med. 2022 doi: 10.1056/NEJMoa2117128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Machingaidze S., Wiysonge C.S. Understanding COVID-19 vaccine hesitancy. Nat Med. 2021;27(8):1338–1339. doi: 10.1038/s41591-021-01459-7. [DOI] [PubMed] [Google Scholar]
- 8.National Population Commission - NPC/Nigeria and ICF. 2019. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF.
- 9.Nomhwange T., Wariri O., Nkereuwem E., Olanrewaju S., Nwosu N., Adamu U., et al. COVID-19 vaccine hesitancy amongst healthcare workers: An assessment of its magnitude and determinants during the initial phase of national vaccine deployment in Nigeria. EClinicalMedicine. 2022;50 doi: 10.1016/j.eclinm.2022.101499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pilishvili T., Gierke R., Fleming-Dutra K.E., Farrar J.L., Mohr N.M., Talan D.A., et al. Effectiveness of mRNA Covid-19 vaccine among US health care personnel. N Engl J Med. 2021;385(25):e90. doi: 10.1056/NEJMoa2106599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reuters. “COVID-19 Tracker” https://graphics.reuters.com/world-coronavirus-tracker-and-maps/countries-and-territories/nigeria/ accessed on Feb 3, 2022.
- 12.Siegler A.J., Luisi N., Hall E.W., Bradley H., Sanchez T., Lopman B.A., et al. Trajectory of COVID-19 vaccine hesitancy over time and association of initial vaccine hesitancy with subsequent vaccination. JAMA Netw Open. 2021;4(9):e2126882–e. doi: 10.1001/jamanetworkopen.2021.26882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Solís Arce J.S., Warren S.S., Meriggi N.F., et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27:1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson M.G., Stenehjem E., Grannis S., Ball S.W., Naleway A.L., Ong T.C., et al. Effectiveness of Covid-19 vaccines in ambulatory and inpatient care settings. N Engl J Med. 2021;385(15):1355–1371. doi: 10.1056/NEJMoa2110362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tregoning J.S., Flight K.E., Higham S.L., Wang Z., Pierce B.F. Progress of the COVID-19 vaccine effort: viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat Rev Immunol. 2021;21(10):626–636. doi: 10.1038/s41577-021-00592-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Bank “New Data Illuminates Acute Vaccine Supply & Delivery Gaps for Developing Countries” https://blogs.worldbank.org/health/new-data-illuminates-acute-vaccine-supply-delivery-gaps-developing-countries accessed on Feb 3, 2022.
- 17.World Health Organization. “WHO Coronavirus (COVID-19) Dashboard” https://covid19.who.int/ accessed Feb 3, 2022.
- 18.World Bank “COVID-19 National Longitudinal Phone Survey 2020-2021” available at https://microdata.worldbank.org/index.php/catalog/3712 accessed on Feb 7, 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.