Abstract
The communities of reproductive medicine and reproductive sciences have been witness to an enormous acceleration of interest in polycystic ovary syndrome (PCO) since the mid-19th century. Although progress has been increasingly palpable, the fundamentals of the etiology and pathophysiology of PCO remain as elusive as ever. Particularly lacking is a requisite understanding of events at the cellular and molecular levels. As we cross the millennial divide, it appears appropriate that an interim progress report be crafted. This treatise is attempting to meet this objective. What follows traces the chronology of the recorded history of PCO in 4 parts.
The communities of reproductive medicine and reproductive sciences have been witness to an enormous acceleration of interest in polycystic ovary syndrome (PCO) since the mid-19th century. Although progress has been increasingly palpable, the fundamentals of the etiology and pathophysiology of PCO remain as elusive as ever. Particularly lacking is a requisite understanding of events at the cellular and molecular levels. As we cross the millennial divide, it appears appropriate that an interim progress report be crafted. This treatise attempts to meet this objective. What follows traces the chronology of the recorded history of PCO in 4 parts:
The first part, the pre-Stein and Leventhal epoch, is dedicated to the period straddling the latter half of the 19th century and the beginning of the one just departed, the 20th. Interest in this epoch was motivated by the realization that most recent articles deem the recorded history of PCO to have its roots in the seminal 1935 contribution of Stein and Leventhal (1). In fact, several investigators sought to describe the typical morphology, the clinical manifestations, and the treatment of the disease decades earlier. Many of these observations were overlooked, going unrecognized for many years, only to be rediscovered and, at times, confirmed later. Stated differently, early pre-Stein–Leventhal contributions to the study of PCO may well have failed to galvanize the attention of the medical community. The Stein and Leventhal report did just that.
The second part of this treatise, the endocrine era, is launched coincident with the classical contribution of Drs. Stein and Leventhal and ends at the tail end of the 1970s. It is during this period that the endocrine origins of PCO were postulated and pursued with vigor.
The third period, the metabolic era, although not as sharply defined, spanning the last 2 decades of the 20th century, i.e., the 1980s and 1990s, is characterized by an intense interest in the metabolic abnormalities characterizing PCO.
The fourth period, the “molecular” era, although somewhat overlapping with its third counterpart, is ongoing. In more ways than one, this fourth period is emblematic of the future, of the 21st century, and the age of molecular reproductive medicine.
In preparing this article, every effort was made to acknowledge each and every important milestone in the history of PCO. However, the investigators are well aware that this report, as is true for any personalized historic summary, may not be all-encompassing. We, thus, wish to apologize to those clinicians and scientists who may not have been cited, inadvertently, in part or in whole, in this article, clinicians and scientists who, nevertheless, made noteworthy contributions to progress in this field.
The pre-Stein and leventhal epoch
Although one can reasonably, indeed safely assume that PCO has been around for as long as there has been a human race, the first published account of a clinical entity along these lines is often traced to Achille Chereau, M.D. (1817–1885) of France. In his 1844 ground-breaking book, one dedicated to the diseases of the ovaries (Maladies Des Ovaires), the segment addressing “acute ovaritis of the first degree” offers a fine description of the typical morphology of the polycystic ovaries (2). “Ovaries are enlarged in volume, elastic,… with smooth and shiny surface, containing many small cysts… located on the periphery of the organ.” (2) It is probably at that point in time that the gross ovarian morphology of PCO was formalized for the first time, a phenotype variably referred to thereafter as polycystic ovaries, sclerocystic ovaries, microcystic ovaries, follicular degeneration, or chronic cystic oophoritis.
It was in early 1895 that a careful description of a “cystic form of chronic oophoritis” was offered in “Clinical Gynecology, Medical, and surgical, for Students and Practitioners.” (3) The investigators included William Mecklenburg Polk, M.D. (1844–1918) of Cornell University Medical College, John Marie Keating, M.D. (1852–1893) of the University of Pennsylvania, and Henry Clarke Coe, M.D. (1856–1940) of the New York Polyclinic. In keeping with what was then a generally accepted inflammatory etiology of PCO, a relevant description of PCO was included in the portion of the book dedicated to inflammation of the female genital organs. After providing a detailed morphologic description of the “PCO” condition, the investigators state that “in the cystic form, the (tunica) albuginea is thickened, and the organ (ovary) is filled with cysts intermixed with normal follicles. The stroma of all such ovaries shows some degree of connective tissue increase leading to more or less induration.” (3) Chronic oophoritis is mentioned as one, albeit a rare cause of so-called “relative amenorrhea and infertility.” (3) The mention of a possible connection between PCO and menstrual dysfunction is noteworthy for the fact that it is lacking in many textbooks seeing the press even years later. As such, this 1895 text affords a unique insight later recaptured and amplified by Drs. Stein and Leventhal.
Two years later, in 1897, Albert Goldspohn, M.D. (1851–1929), Professor of Gynecology at the Post Graduate Medical School in Chicago, offered a possible noninflammatory etiology for “chronic oophoritis leading to cystic follicular degeneration.” (4) In so doing, Dr. Goldspohn reflected the opinion of many of his contemporaries who viewed the cystic ovarian phenotype as a complication of uterine retroversion that gave rise to ovarian congestion.
The relevance of the preceding reports notwithstanding, it is crystal clear that Drs. Stein and Leventhal’s subsequent report cannot be viewed as constituting the first true description of the ovarian morphology and, to a degree, the clinical symptomatology of the entity now recognized as “PCO.” Indeed, a most extensive macroscopic and microscopic analysis of some 180 cases of ovarian “follicular degeneration” was presented by Palmer Findley, M.D. (1868–1965) to the Chicago Gynecological Society as early as 1904 (5). Dr. Findley, a member of the faculty of both the Rush Medical College and the University of Nebraska College of Medicine, undertook a thorough microscopic examination of available pathologic material of ovarian “follicular degeneration.” Special note was made of the “scarcity of normal follicles with contained ova.” (5) Note was also made of the fact that “hyaline degeneration is a prominent feature in nearly all sections.” (5) Finally, Dr. Findley makes note of “fewer (follicles) in number than would appear to be normal. The explanation probably lies in atresia brought about by the addition of new connective tissue to the stroma and its subsequent contraction.” (5) The presumptive prevalence of the disease at the turn of the last century could be estimated by the fact that all of the cases reported by Dr. Findley were collected in only 22 months of practice. In Dr. Findley’s view, the cystic follicles in question did not arise from cell surface inclusions but rather were the result of passive congestion and hyperplasia of the stroma.
A complex chapter dedicated to “chronic ovaritis” can be found in 1905 in a medical textbook concerned with “The Practice of Gynecology for Practitioners and Students” by William Easterly Ashton, M.D. (1859–1933) of the Medico-Chirurgical College and the University of Pennsylvania. (6) It was Dr. Ashton’s objective to analyze the main clinical manifestations of what was referred to as “chronic ovaritis,” replete with pelvic pain, menstrual disturbances, and sterility. Assessment of the attendant prognosis by Dr. Ashton mirrored a familiar contemporary theme, i.e., that “chronic ovaritis is seldom cured spontaneously, and treatment, as a rule, only results in temporary relief.” The section dedicated to the therapy of “chronic ovaritis” reflects the uncertainties of the time. Still, many of the recommended therapies listed are worthy of mention. Specifically, Dr. Ashton suggests that “use of alcohol must be forbidden… the vagina should be douched every night and morning with a gallon or more of hot normal salt solution… a cotton-wool tampon saturated with glycerin should be inserted… diet should be nourishing and easily digested… plenty of pure water should be drunk… bowels should be opened daily… bromide or sodium should be given if the patient is restless or nervous while exercise in the open air and sunshine is beneficial.”
An outlook of PCO, not unlike that later espoused by Drs. Stein and Leventhal was suggested as early as 1907 by Clarence R. Hyde, M.D., of the Long Island College Hospital in New York. (7) As seen by Dr. Hyde, PCO was noteworthy for “a thickened tunic or cortex, the follicle is not allowed to penetrate the outside layer, or there is not enough vis-a-tergot to extrude it.”
As fine a description as any of the ovarian morphology of “PCO” saw press in 1911 in a peer-reviewed article coauthored by Julius Bartel, M.D. (1874–1925), a pathologist, and George Ernest Herman MB (1849–1914), an obstetrician gynecologist. (8) Whereas Dr. Bartel was associated with the Pathologisch-Anatomisches Institut in Vienna, Austria, Dr. Herman, the author of textbooks titled “Diseases of Women” and “Difficult Labour” practiced his craft in London, England. As noted by the investigators, “these ovaries were larger than average… had a thickened coat of dense fibrous tissue, and a strikingly smooth surface, devoid of normal ovulation wrinkles… Their increased size was due to the large number of atresic follicles, varying in size from a pea to a hazelnut that were either grouped in the poles or were distributed throughout the thickened subcortical layer.” (8) It does not get much better than this. The article by Professors Bartel and Herman also makes it clear that Drs. Stein and Leventhal did not pioneer the use of ovarian wedge resection. Indeed, as Professors Bartel and Herman suggest, the broad discussion of the conservative surgical treatment of ovaries afflicted with “follicular degeneration” preceded the classic contribution of Drs. Stein and Leventhal by at least 30 years. This outlook appears to have been supported by Dr. Hyde, whose 1907 article included an overview of surgical techniques such as the puncturing of ovarian cysts, puncturing, and cauterization of the interior of the cysts in question, as well as wedge excision and ablation (7). It would seem that the literature of that time offered almost the same variety of surgical interventions available to the contemporary obstetrician gynecologist, with the exception of laser technology.
It must be stated that the conservative surgical treatment of “chronic ovaritis” was not generally accepted at the turn of the 20th century for several reasons. For one, the reproductive axis, and particularly of ovaries, were viewed as organs of secondary importance of an uncertain role. This somewhat chauvinistic sentiment comes across as loud and clear in Dr. Goldspohn’s writing, who states that “…it is certain that ovaries are fully susceptible to surgical treatment and as such in need of it, as joints are, even though they be objects of lesser importance.” (4) Moreover, frequent recurrence of the presenting symptoms necessitating a high reoperation rate was referred to in some articles as a disincentive to conservative surgical therapy (7). The aforementioned sentiments were further emphasized in 1909 by John Osborn Polak, M.D. (1870–1931), a New York-based obstetrician gynecologist (9). On concluding his review of the literature, Dr. Polak proceeded to state that ovarian wedge resection has a very limited role in the treatment of cystic degeneration of the ovaries. Among the 300 cases reported by Dr. Polak, 41, or 12%, required further surgery, such as ablation of the remaining ovary or of the remaining portion of the previously resected ovary (9). Dr. Polak goes on to state that in his analysis, only 32 pregnancies could be documented in the wake of conservative surgery (9). Note is also made of the conclusion that “the avoidance of the artificially produced menopause is the only result that resection can absolutely promise… the field of ovarian resection is a very limited one.” (9)
The above notwithstanding, ovarian wedge resection was advocated by several authorities. Dr. Goldspohn, for his part, in a broad overview from 1914, put together a series of arguments in support of ovarian wedge resection (10). It was Dr. Goldspohn’s contention that “…surgical treatment eliminates…hyperemia as a usual cause of follicular degeneration” and that “… [satisfactory] results appear from the experience of the majority of operators…” Stated differently: “The evils that come to ovaries with descensus ovariorum reflect the hidden trap that is created by the thoroughly retroverted uterus and the traumata that ovaries experience in their helpless association with it.” (10) In so stating, Dr. Goldspohn reflected the opinion of many of his contemporaries who viewed cystic degeneration as a secondary complication of retroversion. Viewed in this light, wedge resection “relieves the ovary of its tension by enucleating or dissection out the growing cystic follicles by a most careful technique. Care must be taken not to impede the circulation.” (10) Dr. Goldspohn went on to state that “this small but punctilious operation may be best suited for those persons to whom constant wages are a necessity and who may be best served by the smaller risks of conservative surgery.” (10) As adjunctive therapy, Dr. Goldspohn offered “half-hour daily douches at 110 to 120°F in the recumbent posture, as well as vagino-abdominal applications of the galvanic current (40–75 mA) in seances of 30 minutes each, once a week…”(10).
Apart and distinct from the aforementioned observations, Dr. Goldspohn also reported his own experience with a total of 151 ovarian wedge resection procedures, which were performed from 1907–1912 (10). In reading this account, one is led to believe that not much has changed when it comes to the actual “wedging” procedure (10). “Follicle cysts are removed mostly by taking out a wedge-shaped section of the ovary which is so placed so that it will either remove or cut open the maximum number of follicles. The wound is usually closed by 2 rows of continuous sutures, one deep enough to control the bleeding, and the return row to co-apt the edges.” (10) Dr. Goldspohn went on to note that “there is still too much difference of opinion in our ranks about follicular degeneration of the ovaries, as to its pathological status, its clinical importance, and about the practical value of surgical efforts to preserve, reconstruct, or improve such ovaries.” (10) Remarkably, now more than 100 years later, this statement still rings true.
The endocrine era
It was at the 1935 meeting of the Central Association of Obstetricians and Gynecologists that Irving Freiler Stein, M.D. (1887–1976) and Michael Leo Leventhal, M.D. (1901–1971) described the clinical history of 7 women afflicted with menstrual disorders, hirsutism, and infertility (1). The ovaries of the women in question were deemed to be enlarged. The ovarian cortex proved hypertrophied, replete with a thick tunica albuginea. Wedge resection of the ovaries was recommended. That same year, Drs. Stein and Leventhal also published their seminal “report” wherein they describe the now well-recognized ovarian pathology and the distinct clinical characterization thereof. It would appear that the linkage of ovarian pathology with amenorrhea, infertility, hirsutism, and, at times, obesity has given the clinical entity in question the momentum it lacked, not to mention a framework for subsequent discourse and, of course, therapeutic intervention. The eponymic immortality achieved by Drs. Stein and Leventhal is attributed to Joe Vincent Meigs, M.D. (1892–1963) of Harvard Medical School, who reportedly coined the term “Stein–Leventhal syndrome” when discussing one of Dr. Stein’s articles at a national meeting. Importantly, at first, it was Drs. Stein and Leventhal’s contention that “bilateral polycystic ovaries are most likely the result of hormonal influences and not the result of inflammatory change” has frequently been suggested. By then, the alternative notions that follicular degeneration is attributable to inclusion cyst formation or uterine retroversion have been utterly rejected. It was Drs. Stein and Leventhal’s belief that putative endocrine dysfunction produced “a mechanical crowding of the (ovarian) cortex, by cysts, thus interfering with the progress of the normal Graafian follicles to the surface of the ovary.” In so doing, the Stein and Leventhal report has shifted the attention to potential endocrine-driven pathophysiology. The report was apparently the first to refer to a possible “central” (i.e., hypothalamic/pituitary) cause of the disease when stating that “PCO” is “…probably a result of some hormonal stimulation …very likely related to the anterior lobe of the pituitary gland.”
In contrast to earlier articles on the topic of ovarian wedge resection, Drs. Stein and Leventhal evaluated the outcome of the procedure by the resumption of regular menstrual cyclicity as well as by the number of subsequent pregnancies. Regular menstrual cycles resumed in 39 of 53 patients (11). In a subsequent article, Dr. Stein reported that over a period of 27 years, 87% of 69 married women conceived in the wake of their surgical therapy (12). The surprisingly high success rates of ovarian wedge resection in the hands of Drs. Stein and Leventhal likely reflected fine operative skills and, perhaps, most importantly, the strict patient selection criteria. Previous and subsequent studies, in turn, may well have included not only “bona-fide” subjects with PCO but also patients whose circumstance was compounded by unrelated pathology.
One of Dr. Stein’s most important contributions was the clear formulation of diagnostic criteria for PCO (11). Leading ingredients included primary or secondary amenorrhea, sterility, hirsutism, and of course, bilateral ovarian enlargement (11). It was Dr. Stein’s belief that the diagnosis of PCO should be established before surgery on the basis of clinical symptoms, hormonal assays, and the radiographic findings of pneumography, that is, the transvaginal installation of air into the peritoneal cavity (13). Also known as gynecography, this now obsolete technology relied on silhouetting the female organs by means of a pneumoperitoneum. It was Dr. Stein’s view that laparotomy was to be reserved for therapeutic intervention once the diagnosis had been made. The aforementioned diagnostic criteria laid out by Dr. Stein were repeatedly confirmed thereafter. A compelling demonstration of this truism was afforded by Joseph W. Goldzieher, M.D., in 1973 on the pages of Clinical Obstetrics and Gynecology (14). A high frequency of obesity, hirsutism, virilization, amenorrhea, and infertility was documented in more than 1079 putative cases of PCO in congruence with the pioneering observations of Drs. Stein and Leventhal.
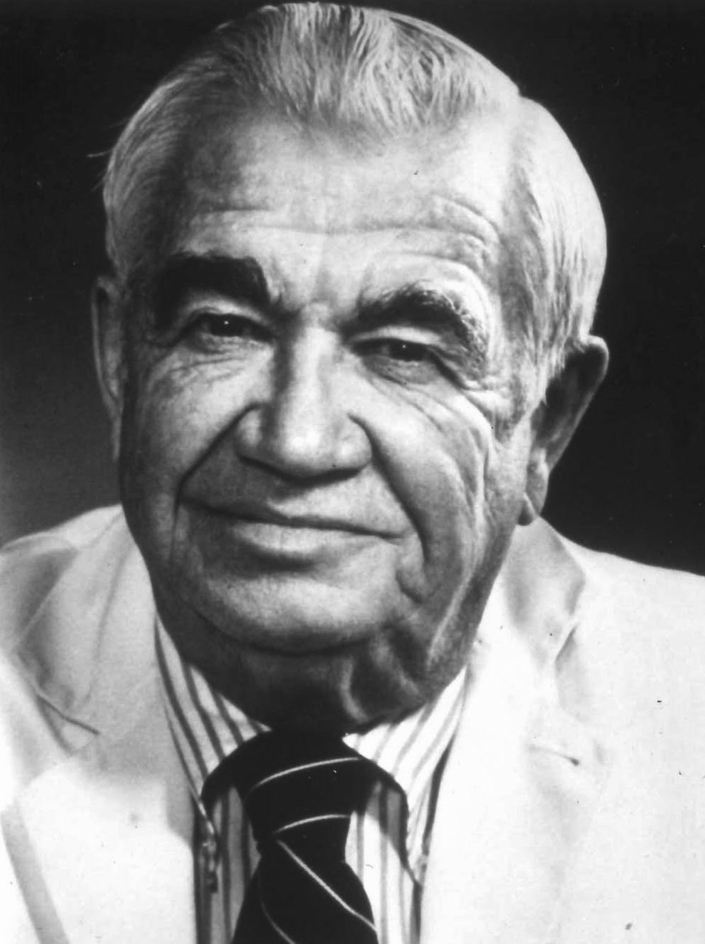
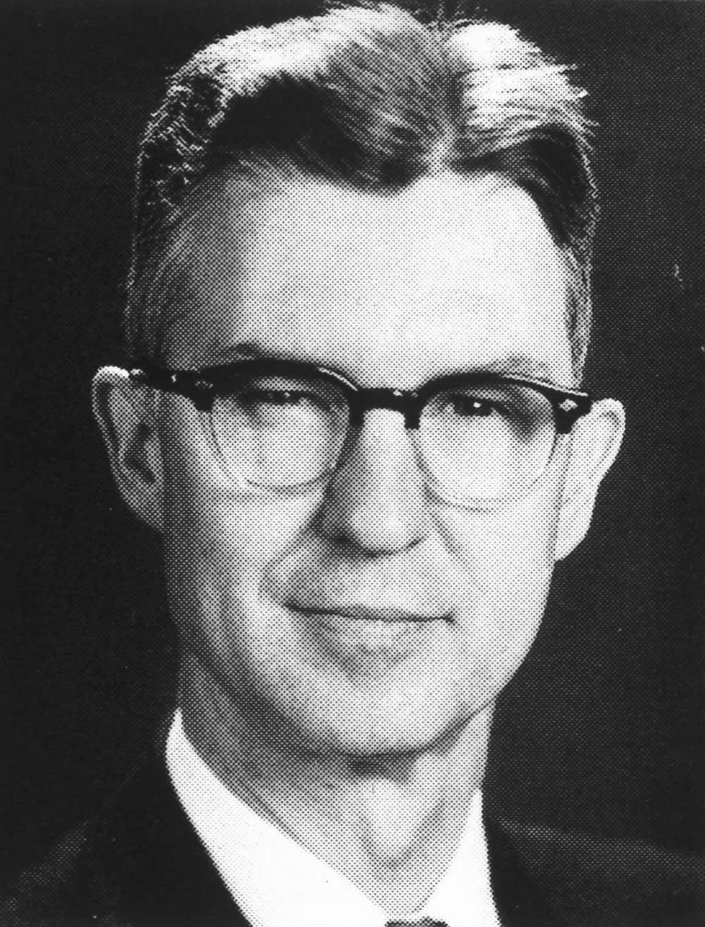
Both Chicago natives, Drs. Stein (Fig. 1) and Leventhal (Fig. 2) received their training at the Rush Medical College and at the Michael Reese Hospital. The 2 were joined in practice at the time that their seminal contribution was made. The association was severed, however, by World War II, during which time Dr. Leventhal served in the Mediterranean Theater. Dr. Stein went on to become a founding member and the 5th President of the American Society for the Study of Sterility, the precursor of the Fertility Society and its current incarnation, the American Society for Reproductive Medicine. Living acquaintances of Dr. Stein remember him as formal and proper, as well as impeccably dressed and groomed. Known for upholding high standards for the practice of medicine in general and for surgery in particular, Dr. Stein may have been perceived as demanding and perhaps imposing. By all accounts, Dr. Stein represented the best one would ascribe to a “gentleman of the old school.”
Figure 1.
Irving Freiler Stein, MD (1887–1976)
Figure 2.
Michael Leo Leventhal, M.D. (1901–1971)
It was in 1957, more than 2 decades past the Stein and Leventhal report, that the next milestone was to be achieved, in this case, from unexpected quarters. Reference is made to a publication by Drs. William C. Keetel, James T. Bradbury, and Frederick J. Stoddard, all from the Department of Obstetrics and Gynecology at the University of Iowa. Professor William C. Keetel, M.D. (Fig. 3) (1911–1981), served as the Chair of the Department. James T. Bradbury, Ph.D., comprised a prime example of the collaboration possible between scientists and clinicians in academic departments of Obstetrics and Gynecology. Frederick J. Stoddard, M.D., was a resident in training. Given the preliminary experience with PCO, the team set out to explore the responsiveness of the polycystic ovary to exogenous gonadotropins of porcine and ovine origin (15). The ovarian size of the patients under study was assessed by palpation and, at times, by laparotomy.
Figure 3.
William Charles Keetel, M.D. (1911–1981)
In detailing the background to the study in question, Dr. Keetel and associates stated that “unless one is constantly conscious of PCO, it is easy to overlook such patients.” (15). At the University of Iowa, the syndrome was not diagnosed until 1952. The first patient to be so diagnosed was treated by bilateral ovarian wedge resection, albeit without success. Because menstruation occurred only once since the operation, the suggestion was made that a course of treatment with a gonadotropic extract from the porcine pituitary is deployed to bring about ovulation. Within a few days of applying the aforementioned extract, the patient in question reported severe abdominal pain and a sense of fullness. Pelvic examination disclosed one ovary to be markedly enlarged. Two weeks have elapsed before the resolution of the aforementioned signs and symptoms. Viewed in hindsight, it would appear that Dr. Keetel and his associates, although possibly unaware of the significance of their observations, may have reported the first example of ovarian hyperstimulation.
A subsequent study by Keetel et al. (15) involved a cohort of subjects with PCO who reported amenorrhea (7 out 13), sterility, hirsutism (6 out 13), and enlargement of the ovaries (10 out 13). Control subjects were assessed as well. Keetel et al. (15) also noted that all but one of the subjects with PCO under study responded to the specific follicle stimulating hormone (“FSH”) preparation with a rapid and marked increase in the size of the ovaries because of the formation of many cystic follicles. In contrast, only one of the 36 control subjects responded in this fashion. One may wish to note that this pioneering undertaking also established, for the first time, the hypersensitivity of PCO ovaries to exogenous gonadotropin therapy, a phenomenon commonly noted in subjects with PCO. Notably, these early observations preceded by several years the more definitive work of Drs. Carl Axel Gemzell of Sweden (1910–2007) and Erwin M Rabau (1899–1983) of Israel who made pioneering use of pituitary and urinary gonadotropins of human origin, respectively (16, 17).
The study of Keetel et al. (15) may also be viewed as a breakthrough in the diagnosis of PCO in that the investigators also took to assessing the circulating levels of luteinizing hormone (LH) using a bioassay, i.e., the response of the pregnant mare serum gonadotropin—primed immature rat ovary—to an extract of the subject’s urine (15). The analysis suggested that the circulating levels of LH may have been elevated in subjects with PCO, thereby prompting the investigators to state that the altered level of serum LH is “a consistent finding and of definite diagnostic value.” Moreover, the investigators regarded the finding of the marked response of the polycystic ovaries to gonadotropic therapy as a characteristic feature of PCO, one that was also proposed as a diagnostic test (“...it seems that the use of ‘FSH’ offers a new diagnostic test”). As such, these observations of endocrine dysfunction in PCO likely constituted the first ever mention of potential diagnostic criteria of an endocrine nature.
On the heels of the preceding observations, the remarkable discovery of increased urinary excretion of LH in subjects with PCO saw press (18). The lead author of the article was Janet W. McArthur, M.D. (1914–2006) (Fig. 4) of Harvard Medical School. Her coauthor, Francis M. Ingersoll, M.D. (Fig. 5), was to become the 17th President of the American Fertility Society, now the American Society for Reproductive Medicine. The study in question, published in 1958, was designed to monitor changes in gonadotropin secretion in 11 women afflicted with menstrual cycle irregularities because of diseases of the reproductive system, including PCO (n = 5) (18). It was the primary objective of the study to quantify the circulating levels of LH as revealed by urinary excretion patterns. The bioassay relied on the effectuation of weight changes in the rat testis and in the ventral prostate. All told, strong evidence was presented to suggest an association between PCO and elevated circulating levels of LH.
Figure 4.
Janet W. MacArthur, M.D. (1914–2006)
Figure 5.
Francis M. Ingersoll, M.D. (1913–1991)
Ever the perfectionist, Dr. McArthur, expressed concern as to the limited number of samples that could be processed for the measurement of LH. It was this reality that prompted Dr. McArthur to conclude that “an ideal description of this (PCO) state would require serial studies…laborious and costly although such an undertaking would be, it appears essential if the full clinical potentialities of gonadotropin assays are to be realized.” (18) Dr. McArthur further summarized the results of her studies by stating that “…it seems fair to conclude that the excretion of one or more gonadotropic hormones fluctuates abnormally in the Stein–Leventhal syndrome and periodically reaches high levels.” (18)
The above advances notwithstanding, gynecologists had hitherto little to offer patients with PCO other than an invasive surgical procedure. Efforts were, thus, undertaken to bring about ovulation through the use of glucocorticoids, estrogens, or Clomiphene Citrate (19, 20, 21). Note must also be made of the tack taken by Abraham Edward Rakoff, M.D. (1913–1981) of the Jefferson Medical College in Philadelphia. As recently as 1953, Dr. Rakoff cautiously promoted “low dosage radiation to the ovaries and pituitary gland as effective in some cases of the Stein–Leventhal syndrome… in which the ovaries have not yet become much enlarged… and the patient has failed to respond to hormonal therapy.” (22)
By the early 1960s, note could be made of some meaningful advances in the medical treatment of PCO, primarily in the treatment of the attendant anovulatory infertility. Successful induction of ovulation in 4 patients with PCO with an experimental (never to be approved) nonsteroidal antiestrogen (MER-25) was reported by Robert W. Kistner, M.D. (1917–1990) and Olive W. Smith, Ph.D. (1901–1983) of Harvard Medical School (23). Pregnancy ensued in 3 of the patients in question. The effectiveness of a closely related nonsteroidal antiestrogen (Clomiphene Citrate) as an ovulation-inducing agent in the context of PCO was documented for the first time in 1961 by Robert Benjamin Greenblatt, M.D. (1906–1987) and associates from the Medical College of Georgia (Fig. 6) (24). Ovulation was restored in 78% of the 36 patients treated, a finding that was repeatedly confirmed thereafter (25). Taken together, the aforementioned observations established, for the first time, a potential noninvasive “chemical” option for the treatment of anovulatory infertility, including PCO (26, 27, 28, 29, 30, 31). The application of Clomiphene Citrate was accompanied and at times preceded by the first reports on the use of human pituitary or urinary gonadotropins to stimulate ovulation in subjects with PCO (16, 32, 33, 34, 35).
Figure 6.
Robert Benjamin Greenblatt, M.D. (1906–1987)
Yet other investigators focused their interest on the possibility of modulating the attendant hyperandrogenism. A decrease in testosterone secretion was demonstrated after ovarian wedge resection but also after the administration of estrogen-progestin-containing combination oral contraceptives (36, 37, 38, 39).
Concurrent with the aforementioned developments, interest persisted in the surgical treatment of PCO. Mostly, however, only modest modifications of previously established principles can be reported. An important step forward was the development of laparoscopic techniques. The first report describing the use of laparoscopic surgery in the context of PCO in 1967 was led by Raul Palmer, M.D. (1904–1985) in France (40). The investigators documented a 60% ovulation rate and a 20% pregnancy rate after multiple ovarian biopsies. Hemostasis was accomplished with unipolar electrocautery. Five years later, a case report, the first to see the press in the English-speaking medical literature, described the laparoscopic treatment of a presumptive case of PCO by Robert S. Neuwirth, M.D. (1933–2013) of Columbia University School of Medicine (41). The diagnosis of PCO rested on documented long-standing anovulatory infertility and on a high normal value for the urinary excretion of gonadotropins. No hyperandrogenism was evident either biochemically or clinically. The ovaries were not deemed polycystic but rather inactive. Ovulatory menstrual cycles were restored once the patient was subjected to a large ovarian biopsy. The investigators reportedly made use of the Palmer Drill Biopsy Forceps, which permits the stabilization of the ovary for the purpose of extracting a tissue core. Hemostasis was achieved with light coagulation. Conception followed in short order. In 1984, the first laparoscopic ovarian electrocauterization procedure in subjects with PCO was reported by Halvard Gjonnaess, M.D. et al. (42) from the Aker University Hospital in Oslo, Norway. The investigators reported a postprocedural ovulation rate of 92% and a pregnancy rate of 80%. A critical overview of the various surgical techniques for the induction of ovulation in PCO was published in 1995 by Drs. Barry W. Donesky and Eli Y. Adashi from the University of Maryland School of Medicine (43).
Lest we forget, although, the process of discovery proceeded unabated. Dr. McArthu, finally saw her wish come true in 1970, at which time the power of the newly developed radioimmunoassays was put to good use in the context of PCO. Having implemented technology acquired from A. Rees Midgley, M.D., from the University of Michigan, Samuel SC Yen, M.D., Sc.D. (1927–2006) (Fig. 7) of Case Western Reserve University, proceeded to convert his private practice office into a “mini CRC” (Clinical Research Center) wherein he subjected subjects with PCO to frequent blood sampling (30). In what remains a seminal contribution, Dr. Yen confirmed the abnormal gonadotropin secretion patterns in amenorrheic subjects, all of whom were noted to display the typical ovarian morphology of PCO by culdoscopy or laparotomy. As the investigators note, “…the cyclic pattern of FSH and LH is typically absent, and there is a disproportionately high secretion of LH with constant low FSH secretion.” (30) Dr. Yen goes on to state that “a disturbance in the hypothalamic regulation of pituitary gonadotropin secretion may be causally related to the chronic anovulation and abnormal steroidogenesis observed in subjects with PCO.” (30)
Figure 7.
Samuel S.C. Yen, M.D., Sc.D. (1927–2006)
The above studies served as an impetus to further evaluation of the regulation of gonadotropin secretion in subjects with PCO. In 1976, Robert W. Rebar, M.D. of the University of California, San Diego, published a landmark article on the effects of the administration of exogenous estrogen, antiestrogen (Clomiphene Citrate), or LH releasing factor (now referred to as gonadotropin-releasing hormone [GnRH]) on gonadotropin release in subjects with PCO (44). Consistent with other investigators, Dr. Rebar reported augmented pituitary sensitivity to stimulation with GnRH, a phenomenon correlated with the circulating levels of estrogens (45, 46, 47). A most important finding was that of the apparent normalcy of both the positive and negative feedback mechanisms at the hypothalamic-pituitary level. These observations led Rebar et al. (44) to suggest that “…in PCO patients, the abnormal regulation of gonadotropin secretion was not an inherent defect but represented a functional derangement consequent to inappropriate estrogen feedback.”
In addition to abnormal gonadotropin secretion, subjects with PCO have also been shown to display varying degrees of hyperandrogenism. Indeed, several articles demonstrated a significant increase in the circulating levels of testosterone, dihydrotestosterone, dihydrotestosterone-sulfate, and androstenedione in subjects with PCO (48, 49, 50). The diagnosis of PCO in the cases in question relied on the documentation of the typical ovarian morphology as confirmed by laparoscopy or laparotomy. In addition to the documentation of higher androgen production rates, note was made of low sex hormone binding globulin (SHBG) concentrations, the role of which in the enhancement of the hyperandrogenic state was carefully documented. Although ovarian androgen overproduction has been clearly established as a common feature of PCO, the adrenal contribution to the circulating pool of androgens in subjects with PCO was also assessed. Notably, the circulating levels of testosterone proved to be significantly more suppressible in response to the administration of dexamethasone in subjects with PCO compared with normal ovulatory controls (51). Equally important observations were made by Lachelin et al. (52) of the University of California, San Diego, who made note of the fact that subjects afflicted with PCO displayed increased adrenal capacity but not sensitivity to the adrenocorticotropin hormone. It was on the strength of these observations that Lachelin et al (52) suggested that the adrenal hyperresponsiveness to adrenocorticotropin hormone was a reflection of functional changes in adrenal steroidogenesis that was ascribable to excess circulating levels of androgens of presumed ovarian origin.
The imaging technology was not to be outdone. As early as 1981, efforts at the sonographic imaging of the ovaries were meeting with increasing success (53). The first relevant report to see press, by Mark G. Swanson, M.D. of the University of British Columbia Canada, made good use of an abdominal probe which was to give way, in due course, to a vaginal counterpart the product of which would prove far more informative. Most importantly, the reproductive endocrine community was apprised, for the first time, of the possibility that the sonographic ovarian phenotype need not necessarily be associated with a chronic anovulatory state. Indeed, seemingly asymptomatic (that is, normally cycling), if still gonadotropin-hypersensitive, subjects have been noted to display an identical sonographic ovarian phenotype (54). Equally important observations were made by Howard S. Jacobs, M.D., of the St. Mary's Hospital Medical School in London (55, 56). Special note was made of the observation that clinically asymptomatic women, replete with the sonographic phenotype of polycystic ovaries, displayed increased circulating basal and glucose-stimulated levels of insulin (57).
Concurrently, the early 1980s also saw a resurgence of interest in a possible hypothalamic etiology of PCO. The first in a series of such developments, the so-called “dopamine deficiency” theory, dates back to 1981 (58). According to this view, one promulgated with vigor by Dr. Yen of the University of California, San Diego, the.” alteration of the pulsatile pattern of GnRH release may be due (in subjects with PCO) to central dopaminergic deficiency.” Stated differently, PCO may constitute a state of diminished endogenous dopaminergic tone. Put yet another way, PCO could be viewed as the reproductive equivalent of Parkinson disease. Central to this hypothesis is the observation that subjects with PCO display increased sensitivity to exogenous dopaminergic inhibition of gonadotropin release (58).
Although the “dopamine deficiency” hypothesis is not without its detractors, additional lines of evidence would tend to support such a possibility. One such line of support is represented by the occasional concurrent presence of hyperprolactinemia in subjects with PCO, the decreased sensitivity to the dopaminergic blockade, and the occasional normalization of reproductive dysfunction with bromocriptine, a dopaminergic agonist (59, 60, 61, 62, 63, 64). Indeed, the superimposition of a dopaminergic agonist, such as bromocriptine, has sporadically been shown to convert a clomiphene-resistant circumstance to a clomiphene-sensitive state. Moreover, the provision of bromocriptine has also been reported to diminish the pituitary hypersensitivity to GnRH, circulating levels and pulse frequency of LH, and even the attendant hyperandrogenism (65).
Even more telling documentation of a possible primary hypothalamic pathology was put forth by Barnett Zumoff, M.D (1926–2021). and associates of the Albert Einstein College of Medicine (Fig. 8). It was in 1983 that Dr. Zumoff and his colleagues reported on the disordered chronobiology of LH release in adolescent subjects with PCO (66). The subjects under study, 5 girls aged 13–16 years, all oligomenorrheic or amenorrheic, displayed a marked midday surge of LH secretion. The core finding of the study was that whereas normal pubertal girls displayed a daily LH surge that is coterminous with the nocturnal sleep period, subjects with PCO proved grossly desynchronized in this regard in that their LH surge transpired in the daytime, that is, 7–8 hours later than normal. It was Dr. Zumoff’s conclusion that this finding points to the central nervous system as the probable primary locus of the pathophysiology of PCO.
Figure 8.
Barnett Zumoff, M.D. (1926–2021)
It took no more than 2 years before the aforementioned observation was complemented by the documentation of an apparent acceleration of the hypothalamic GnRH pulse generator in PCO. The first in a series of such reports was contributed by Johannes Schoemaker, M.D., Ph.D. of the Free University of Amsterdam (67). Confirmation of these findings followed in short order from the laboratories of William F. Crowley, M.D., of Harvard Medical School, and Samuel SC Yen, M.D., D.Sc. (68, 69). The significance of the preceding observations was inevitably bolstered by the finding that the acceleration of the frequency of pulsatile GnRH delivery in arcuate-lesioned rhesus monkeys resulted in an abnormal LH/FSH ratio, a finding not unlike that observed in subjects with PCO (70). Similar observations were made by Dr. Yen in GnRH-treated hypogonadotropic subjects in whom a PCO-like profile was induced on the initiation of pulsatile GnRH therapy (71).
The pendulum swung back again in 1987 when William C. Dodson, M.D. and Arthur F. Haney, M.D., both of Duke University School of Medicine, first demonstrated that the ovarian hypersensitivity to gonadotropic stimulation, a hallmark of PCO, was unaltered by prior short-term gonadotrophic deprivation brought about by a GnRH agonist (72). Compared with ovulation induction using human menopausal gonadotropins (hMGs) alone, the administration of leuprolide acetate (a GnRH agonist) before and during treatment with hMG prevented premature luteinization but was without effect on the hMG-induced increase in the circulating levels of l7β-estradiol. Although one could argue that the gonadotrophic deprivation, in this case, was relatively short-lived, this argument may not hold in the face of subsequent work led by Dr. Howard S. Jacobs (54). Importantly, note was made of a PCO-like ovarian phenotype as well as of gonadotropin hypersensitivity in the face of a lifetime of gonadotrophic deprivation. One cannot help but conclude that these observations make a compelling case for the ovary as the primary seat of pathology in PCO.
Finally, note must be made of the efforts of Robert L. Rosenfield, M.D., of the University of Chicago, to develop a dynamic, functional test of the hypothalamic/pituitary/ovarian axis (73). Applied to PCO, this approach (a GnRH agonist stimulation test) revealed subjects with PCO to display a masculinized pituitary and ovarian response to stimulation with nafarelin (a GnRH agonist) thereby suggesting dysregulation of 17 α-hydroxylase and 17–20 lyase activities. All told, these observations suggested that the PCO ovary was transformed in a manner conducive to the elaboration of androgens.
The Metabolic Era
A possible association between hyperandrogenism and a metabolic disease state was hinted at for the first time in 1921 by Emile Charles Achard, M.D., and Joseph Thiers, M.D. of France, when describing a case of diabetes in a bearded woman (74). Years later, Dorothy R. Hollingsworth, M.D. of Yale University School of Medicine, unaware of the preceding observation, identified a distinct subgroup of female subjects with obesity afflicted with acanthosis nigricans, hirsutism, and menstrual irregularities. Polycystic ovaries were diagnosed in one of the cases in question and suspected in the other 3 (75). Only 2 years later, note was made by James R. Givens, M.D. (1930–2005) of the University of Tennessee (Fig. 9) of the concurrence of insulin-resistant diabetes mellitus, acanthosis nigricans, and hyperandrogenism in 2 families afflicted with ovarian hyperthecosis, likely a more severe variety of PCO (76). Additional clues as to the metabolic roots of PCO were afforded by Ronald.C. Kahn, M.D., in 1976, then at the National Institutes of Health (77). Specifically, note was made of the combination of extreme insulin resistance, systemic hyperandrogenism (clitoromegaly, temporal balding, increased muscle mass, and deepening of the voice), and acanthosis nigricans in adolescent girls afflicted with the type A syndrome of extreme insulin resistance. Although the latter subjects could not be described as suffering from “primary” PCO, the documentation of hyperinsulinemic hyperandrogenism, i.e., the very linkage, proved instructive. By all accounts, the preceding and subsequent articles heralded the interest in PCO as an insulin-resistant state which, from here onward, comprised a new focus of investigative attention.
Figure 9.
James Robert Givens, M.D. (1930–2005)
It was not until 1980, however, that additional inklings of metabolic aberrations in PCO were described. It was here that Dr. Givens made his seminal observations on the apparent association between insulin resistance and PCO. A leading 1980 article senior-authored by Dr. Givens reported a correlation between basal and glucose-stimulated insulin secretion on one hand and the circulating levels of testosterone on the other (78). The PCO constellation described by the investigators comprised oligomenorrhea or amenorrhea, obesity, hirsutism, hyperandrogenism, and an elevated LH to FSH ratio. Not surprisingly, the article served to catalyze future interest in hyperinsulinemic hyperandrogenism as a facet of PCO (78). Thereafter, insulin resistance and apparent compensatory hyperinsulinemia were documented by multiple investigators for both obese and nonobese subjects with PCO of different ethnic origins (79, 80, 81, 82, 83, 84, 85, 86). In addition to decreased insulin sensitivity, note was also made of pancreatic β-cell dysfunction in subjects with PCO (87, 88, 89, 90). Impaired insulin secretion was later affirmed for both obese and nonobese subjects with PCO (90). Greater prevalence of this dysfunction was documented for subjects with PCO reporting a history of type 2 diabetes in a first degree relative (91). In that significant improvement of insulin resistance during weight loss was not followed by improved insulin secretory dynamics, the suggestion was made that the dysfunctional secretion of insulin may, in fact, constitute a “primary” attribute of PCO independent of the apparent peripheral insulin resistance (90).
In an effort to further elucidate the molecular defects underlying the aforementioned metabolic phenotypes, several investigators sought to focus on the cellular mechanisms underlying insulin resistance and abnormal insulin secretion. Although no mutations of the insulin receptor have been identified in subjects with PCO, putative defects in postreceptor signal transduction, i.e., in the recruitment of glucose transporter proteins, were demonstrated in subjects with PCO (85, 91, 92, 93). It is in this context that Andrea E. Dunaif, M.D. of Pennsylvania State University College of Medicine, reported a frequent defect in the autophosphorylation of the insulin receptor in subjects with PCO (94). Most recently, these same investigators observed diminished insulin-mediated disposition of glucose, decreased insulin receptor substrate 1-associated with PI-3-Kinase activity, but increased representation of insulin receptor substrate 2 in muscle tissue of subjects with PCO (95).
Expectedly, the discovery of impaired insulin economy as a feature of PCO raised questions as to its role in “triggering” the attendant ovarian hyperandrogenism. A compelling argument to this effect was offered by John E. Nestler, M.D. of the Medical College of Virginia, whose study entailed the monitoring of endocrine and metabolic parameters in subjects with PCO who were being treated with diazoxide, an inhibitor of pancreatic insulin secretion (96). As reported by the investigators, note was made of a decrease in the circulating levels of insulin and of a reduction in the circulating levels of total testosterone in the face of an unaltered gonadotropin economy. As such, this study furnished clinical in vivo evidence for a close, possibly causal association between the hyperinsulinemic and hyperandrogenic features of PCO. In contrast, suppression of androgen production or action did not completely reverse the insulin-resistant state, thereby arguing against a causal role for androgens in the induction of insulin resistance (97, 98, 99). A direct inhibitory effect of hyperinsulinemia on the circulating levels of serum SHBG levels in obese subjects with PCO was also noted to contribute to an increase in the free fraction of the circulating levels of testosterone (100).
The in vitro ability of insulin to promote human ovarian androgen production, by itself, but mostly in synergy with LH, was demonstrated by multiple investigators, albeit under insulin-sensitive as distinct from insulin-resistant circumstances (101, 102). Thus, the relationship between hyperinsulinemia and hyperandrogenism, although undeniable, remains incompletely understood. For example, how can insulin stimulate ovarian androgen biosynthesis or synergize with LH in this regard in the face of a systemic insulin-resistant state? Although multiple hypotheses have been put forth to explain away this apparent conundrum, a definitive resolution of this phenomenon is still pending. One possible explanation, however, may involve an insulin receptor-independent mechanism of action of insulin. It is in this context that Dr. Nestler, M.D. undertook to study a putatively novel signal transduction system activated by insulin, one that did not entail tyrosine phosphorylation of and by the insulin receptor (103). Using cultured human theca cells, the insulin receptor of which was immunologically neutralized, Dr. Nestler was able to show, with the aid of anti-inositolglycan antibodies, that insulin is capable of activating an inositolglycan signal transduction system. More recently, but along similar lines, Leonid Poretsky, M.D. of Albert Einstein College of Medicine, offered evidence in support of the notion of a PI-3-kinase-independent insulin signaling pathway in human ovarian cells (104).
Interest in the nonreproductive comorbidity experienced by subjects with PCO has been growing in light of the increasing appreciation of the metabolic aspects of the disease. The first relevant, if still uncontrolled, study by Dunaif et al. (105) suggested an increased risk of developing type 2 diabetes by 46 subjects with obesity and PCO. The prevalence of type 2 diabetes was also evaluated retrospectively in older perimenopausal women who were previously diagnosed as being afflicted with PCO (106). The results of the latter study disclosed a significantly higher prevalence of type 2 diabetes in subjects with PCO as compared with age-matched controls (15% vs. 2.3%). More recently, 2 additional controlled studies reported relevant data on the reality that subjects with PCO are at increased risk of developing type 2 diabetes (107, 108).
Acting on the presumption that obesity and insulin resistance constitute intrinsic features of PCO, other landmarks of the so-called “Syndrome X” (hypertension and dyslipidemia) were also sought. As early as 1985, Robert A. Wild, M.D., Ph.D., M.P.H. of the University of Oklahoma College of Medicine, observed lower circulating levels of high density lipoprotein cholesterol, low density lipoprotein/high density lipoprotein ratios, and triglyceride levels in subjects with PCO when compared with normally cycling women (109). An adverse lipid profile in association with PCO was affirmed by subsequent reports (110, 111, 112). More of the same was reported by Evelyn O. Talbott, Dr.P.H., M.P.H. from the University of Pittsburgh, who noted high circulating levels of low density lipoprotein cholesterol and total cholesterol (adjusted for body mass index and for the circulating levels of insulin) in subjects with PCO aged <45 years (113). Although one retrospective study revealed a higher incidence of hypertension in putative subjects with PCO compared with controls (39% vs. 11%), several other studies failed to confirm this association (106, 114, 115).
The possibility of an increased risk of coronary heart disease in subjects with PCO was also assessed. In this connection, Wild et al. (116) noted a high prevalence of hirsutism in patients with proven coronary artery lesions. Comparable observations were made by Birdsall et al. (117) who was able to demonstrate significantly increased carotid artery intima-media thickness in subjects with PCO. A significantly higher prevalence of coronary artery disease was also documented by David S. Guzick, M.D., Ph.D. from the University of Pittsburgh, for a limited number of postmenopausal women previously said to have been diagnosed with PCO (118). However, mortality and morbidity rates from coronary heart disease, as assessed by way of a retrospective cohort study, proved similar for subjects with PCO compared with women at large (119, 120).
The new insights as to the metabolic facets of PCO were implemented before too long with an eye toward advancing novel approaches to treatment. The frequent occurrence of compensatory hyperinsulinemia, attributed, in part, to peripheral insulin resistance, prompted efforts to reduce the circulating levels of insulin in an effort to normalize this facet of the condition. In that context, 1994 saw the publication of the first article assessing the effect of treatment with an “insulin-sensitizing” agent on the pathophysiology of PCO (121). Specifically, the administration of metformin, a biguanide capable of increasing peripheral glucose uptake and lowering hepatic glucose output, not only led to a reduction in the circulating levels of insulin but also gave rise to a decrease in the circulating levels of total and free testosterone while increasing the circulating levels of SHBG. A concomitant reduction of body weight was also noted. It remains unclear whether or not all of the aforementioned effects could be solely or even largely attributed to the treatment of subjects with PCO with metformin. Indeed, several other, mostly observational or short-term studies, reported inconsistent effects of metformin on the circulating levels of insulin or of androgens or on the restoration of regular menstrual cyclicity (122, 123, 124, 125, 126). It was not until 2000 when the first randomized, double-blind, placebo-controlled 6-month study on the utility of metformin in PCO was published (127). The latter effort revealed that the administration of metformin led to a significant reduction in the circulating levels of insulin, in insulin resistance, and in the attendant circulating levels of androgens. Encouraging results were also observed when using troglitazone of the thiazolidinedione class of oral hypoglycemic agents. This promising drug was launched in 1997, only to be withdrawn in Europe in the same year and in the United States in March of 2000 because of liver toxicity. Still, treatment of subjects with PCO with troglitazone improved insulin sensitivity, ameliorated insulin secretory dysfunction, and reduced the overall hyperandrogenic effect (123, 124, 125, 126, 127, 128, 129, 130). Another thiazolidinedione, Pioglitazone, was shown to inhibit early atherosclerosis at the level of the carotid artery through peroxisome proliferator-activated receptor-γ activation (131). The combination of an antiestrogen with an insulin-sensitizing agent, either Metformin or Troglitazone, was also shown to increase ovulation rates in infertile subjects with PCO (130, 132, 133).
The hypothesized deficiency in inositol phosphoglycans (putative mediators of insulin action) in subjects with PCO stimulated yet another therapeutic alternative. A double-blind study of 22 subjects with PCO led by Dr. Nestler documented improved insulin sensitivity after 6–8 weeks of treatment with D-chiro-inositol (a phosphoglycan mediator of insulin action) (134). This, in turn, was followed by a significant decrease in the circulating levels of (total or free) testosterone. Ovulation was restored in 19 (86%) of the cases. On balance, the efficacy of this approach was more than comparable with that of Metformin or Troglitazone. Clearly, although, larger studies of longer duration are needed to confirm the efficacy of inositol phosphoglycan replacement in the treatment of the anovulatory state or of the metabolic abnormalities of PCO.
The treatment of anovulatory infertility, a central feature of PCO, also witnessed some additional progress. Indeed, the early 1980s saw improvements in the induction of ovulation with the introduction of low-dose gonadotropin protocols, first reported by Kamrava et al. (135) of Harvard Medical School. Specifically, ovulatory cycles followed by pregnancy were achieved by the administration of low doses of FSH in 2 subjects afflicted with PCO. Based on this new concept, Polson et al. (136) of the Imperial College London were able to bring about ovulation in all of the clomiphene-resistant subjects with PCO under study using low doses of subcutaneously-administered purified urinary FSH. This approach made it possible to increase the likelihood of monofollicular development as well as reduce the incidence of ovarian hyperstimulation syndrome and of multiple gestation (137, 138, 139). Last but not least, mention must be made of the contribution of the field of Assisted Reproductive Technology to the treatment of the infertility component of PCO. Specifically, cumulative pregnancy rates achieved in in vitro fertilization-treated subjects with PCO proved comparable with those achieved in patients afflicted with other causes of infertility, such as tubal disease (140, 141, 142, 143).
The genomic era
The closure of the circle would not be complete without mentioning the continuing efforts to elucidate the pathobiology of PCO in the genetics arena. The 3rd millennium is, after all, the genetics millennium. High hopes persist that newly derived genetic insights will shed new light on the cellular and molecular pathology of PCO. Although initial reports of familial clustering of PCO were published as early as the 1960s, the last 10 years have seen a renewed interest in the genetic aspects of the disease (144, 145). Although various modes of inheritance have been proposed, no definitive genetic route has been established thus far (146, 147, 148, 149). Several possible parallel male phenotypes have been proposed as well, including premature male baldness (147, 150, 151). However, at the time of this writing, the definite male phenotype remains uncertain. Nearly 40 genes have been tested thus far in an effort to identify possible candidates which might be contributory to PCO. Early efforts focused on the CYP 17 gene, the gene encoding cytochrome P450c17α (17-α hydroxylase/17, 20 - lyase). (151, 152) However, linkage studies failed to confirm an association between a variant CYP17 allele and PCO (153, 154). A more recent effort in this arena was undertaken by Urbanek et al. (155), Ph.D. from the Feinberg School of Medicine. Relying on a retrospective cohort, the investigators assessed the degree of linkage of 37 candidate genes to the PCO phenotype in the families of presumptively affected women (155). The strongest evidence for linkage was reported for the Follistatin gene. However, the significance of this finding remains uncertain. Several candidate genes encoding steroidogenic enzymes were also investigated. In this context, an association was reported for a variation in the CYP11a gene and the PCO phenotype in general and serum testosterone in particular (156). The CYP11a gene encodes the enzyme cholesterol side-chain cleavage which catalyzes the first step in the steroidogenic cascade. No abnormalities were documented for the insulin or the type I insulin-like growth factor receptor genes. (92, 155). Finally, tandem repeat polymorphism at a minisatellite locus of the insulin gene (variable number tandem repeats [VNTRs]) on chromosome 11p15.5 was studied by Waterworth et al. (157) of the Imperial College School of Medicine in London, United Kingdom (157). Variation of this element has been implicated in the regulation of insulin secretory dynamics and thus in susceptibility to type 2 diabetes (158). A strong association between class III alleles (140–210 repeats) of the VNTR and anovulatory PCO was demonstrated in 3 different populations. Polymorphism of the VNTR locus of the insulin gene has been proposed as a contributor to the mechanism of hyperinsulinemia and to the higher risk of type 2 diabetes in PCO (157, 158).
Epilogue
By the end of the 2nd Millennium, unassailable clarity as to the precise pathophysiology of PCO remained out of reach. What, then, was a reproductive endocrinologist to do? Is PCO a primary hypothalamic or a primary ovarian disorder? And who is to arbitrate between the centrist (hypothalamic-pituitary) school and the one favoring the ovarian end organ of the reproductive axis?
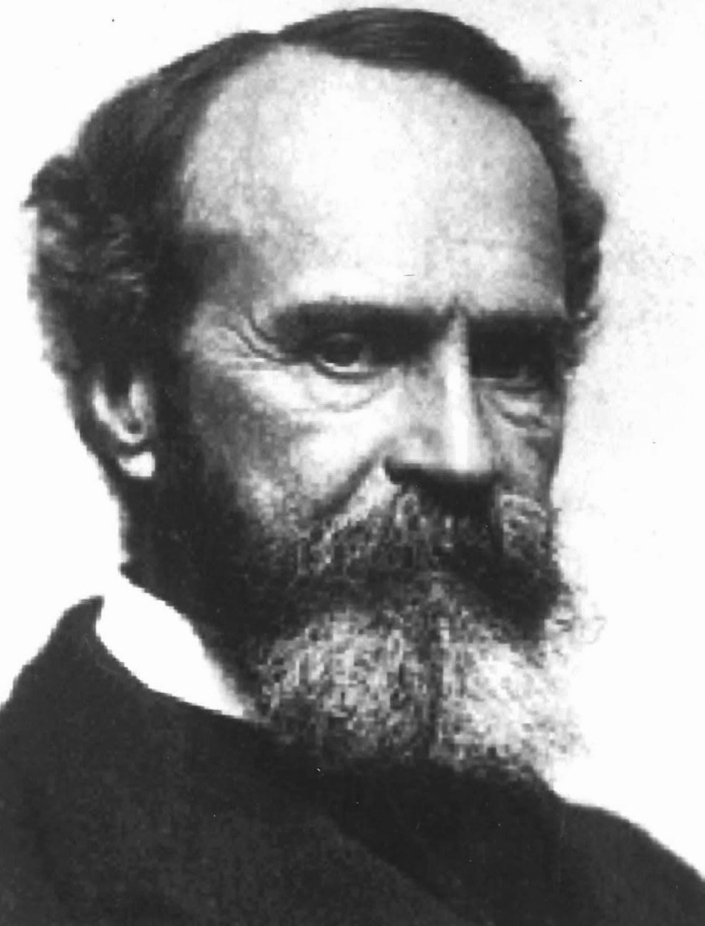
In many ways, the enigma of PCO is highly reminiscent of the experience of “going around the squirrel,” a conundrum communicated by the great American philosopher, historian, and psychologist William James (1842–1910) (Fig. 10). It seems James was out one day, and while looking at an oak tree, he heard the unmistakable sound of a squirrel scratching on the unseen side of the oak. James circled to his right, and the squirrel did as well. No matter how quickly James moved in a circle around the tree, the squirrel moved just as quickly and thus remained unseen by the philosopher. It would certainly appear that we, the collective discipline of women's health, not unlike William James, are still going around the tree in the belief of seeing the squirrel, which for all practical purposes, remains unseen.
Figure 10.
William James (1842–1910)
As seen from the vantage point of the turn of the 20th century, uncertainty reigned as to whether or not PCO constituted a primary hypothalamic disorder. Such a hypothesis would argue that the likely essence of the pathology is an alteration of the pulsatile pattern of GnRH release, the precise causation of which would have to be determined. Evidence to support this notion includes the documentation of the disordered chronobiology of GnRH release, the acceleration of the pulse generator, and the possible decrease in central dopaminergic priming. That said, at least some of the previously mentioned observations could potentially represent secondary phenomena.
At the opposing end of the spectrum, the reproductive community at large was left facing the alternative hypothesis, namely whether or not PCO constitutes a primary ovarian disorder. Evidence in support of this possibility includes the extensively documented ovarian hypersensitivity to gonadotropins, the realization that short-term, as well as long-term gonadotrophic deprivation, does not alter this seemingly intrinsic ovarian trait, and the existence of a sonographic ovarian phenotype in seemingly asymptomatic but still (gonadotropin) hypersensitive subjects.
Lest we forget, the future of and perhaps the key to the PCO conundrum may lie in the metabolic connection. While insulin is highly likely to play a role, it is unlikely to constitute the only culprit. At the point in time at the conclusion of 150 years of study of PCO, there is a growing awareness of the possibility that trophic pituitary factors other than gonadotropins may be involved. After all, gonadotrophic deprivation does not appear to reverse the apparent ovarian hypersensitivity. Might it be possible that enhanced growth hormone secretion, for example, maybe all it takes to amplify even the most modest gonadotrophic input? It is in this context that future studies of the genetic underpinning of PCO will deliver novel, relevant insights replete with the prospect of, heretofore, unrealized gonadotropic principles.
One hundred and fifty years of study have markedly enhanced the understanding of PCO. Still, as viewed from the vantage point of the year 2000, much remains to be done. Overriding it all is the imperative of pinpointing the precise etiologic origins of PCO and, thereby, its therapy. Clearly, a cure is not in the cards as yet. One must also admit that our therapeutic tools are still limited in scope, focusing mostly on palliation. Looking back at publications now a century old, one might be tempted to conclude that limited progress can be reported. The above notwithstanding, new discoveries will progressively eliminate the gaps in our knowledge and thereby render the jigsaw puzzle complete. Major advances, especially in the human genetics arena, are likely to permit the identification of variants of the syndrome and thus add insight into the PCO pathophysiology. Beneficial implications to the therapeutic possibilities are bound to follow. As it is, PCO remains an area where many important discoveries are likely to come our way.
Acknowledgments
The authors acknowledge the following individual for significant contributions to this work: Lawrence D. Longo, M.D., (1926–2016) and Jean Cohen, M.D. (1929–2007). They give special credit to Linda Tanner and Janine Calfo for their moral and technical support. Further assistance was rendered by Samuel SC Yen, M.D. (1927–2006), Robert W. Rebar, M.D., A. Rees Midgley, M.D., Paul McDonough, M.D. (1930–2021), Virendra Mahesh, M.D. (1932–2019), and James R. Givens, M.D. (1930–2005).
Footnotes
E.Y.A. has nothing to report. D.C. has nothing to report. C.M.P. has nothing to report. R.A. has nothing to report.
References
- 1.Stein I.F., Leventhal M.L. Amenorrhea associated with bilateral polycystic ovaries. Am J Obstet Gynecol. 1935;29:181–191. [Google Scholar]
- 2.Chereau A. Masson et Cie.; Paris: 1844. Memoires pour Servir a l'etude des maladies des ovaries. [Google Scholar]
- 3.Polk W.M. In: Clinical Gynecology Medical and Surgical for Students and Practitioners. Keating J.M., Coe H.C., editors. J.B. Lippincott Co.; Philadelphia: 1895. Inflammation of the female genital organs; p. 349. [Google Scholar]
- 4.Goldspohn A. The fate of ovaries in connection with retroversion and retroflexion of the uterus. Am J Obstet. 1897;36:439–447. [Google Scholar]
- 5.Findley P. Cystic degeneration of the ovary, an anatomical and clinical study of 180 cases. Am J Obstet. 1904;49:762–771. [Google Scholar]
- 6.Ashton W.E. In: A textbook on the practice of gynecology for practitioners and students. Ashton W.E., editor. W.B. Saunders and Company; Philadelphia and London: 1905. Chronic ovaritis; pp. 507–511. [Google Scholar]
- 7.Hyde C.R. Notes on conservative ovarian surgery. Am J Obstet Dis Women Child. 1907;56:145–159. [Google Scholar]
- 8.Bartel J., Herman E. Uber die weibliche Keimdruse bei Anornalie dere Konstitution. Gynecol Obstet. Investig. 1911;3:125–135. [Google Scholar]
- 9.Polak J.O. Final results in conservative surgery on the ovaries. JAMA. 1909;53:1382–1386. [Google Scholar]
- 10.Goldspohn A. Resection of ovaries. Trans Am Gyncecol Soc. 1914;27:71–84. [Google Scholar]
- 11.Stein I.F. Bilateral polycystic ovaries. Am J Obstet Gynecol. 1945;50:385–398. [Google Scholar]
- 12.Stein I.F. Ultimate results of bilateral ovarian wedge resection: twenty-five years follow-up. Int J Fertil. 1956;1:333–344. [Google Scholar]
- 13.Stein I.F. The Stein-Leventhal syndrome; a curable form of sterility. N Engl J Med. 1958;259:420–423. doi: 10.1056/NEJM195808282590904. [DOI] [PubMed] [Google Scholar]
- 14.Goldzieher J.W. Polycystic ovarian disease. Clin Obstet Gynecol. 1973;16:82–105. doi: 10.1097/00003081-197312000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Keetel W.C., Bradbury J.T., Stoddard F.J. Observations on the polycystic ovary syndrome. Am J Obstet Gynecol. 1957;73:954–965. [PubMed] [Google Scholar]
- 16.Gemzell C.A., Diczfallusy E., Tillinger G. Clinical effect of human pituitary follicle- stimulating hormone (FSH) J Clin Endocrinol Metab. 1958;18:1333–1348. doi: 10.1210/jcem-18-12-1333. [DOI] [PubMed] [Google Scholar]
- 17.Rabau E., David A., Serr D.M., Mashiach S., Lunenfeld B. Human menopausal gonadotropins for anovulation and sterility. Results of 7 years of treatment. Am J Obstet Gynecol. 1967;98:92–98. doi: 10.1016/0002-9378(67)90137-8. [DOI] [PubMed] [Google Scholar]
- 18.McArthur J.W., lngerssoll F.M., Worcester J. The urinary excretion of interstitial- cell and follicle-stimulating hormone activity by women with disease of the reproductive system. J Clin Endocrinol Metab. 1958;18:1202–1215. doi: 10.1210/jcem-18-11-1202. [DOI] [PubMed] [Google Scholar]
- 19.Smith K.D., Steinberger E., Perlof W.H. Polycystic ovarian disease. A report of 301 patients. Am J Obstet Gynecol. 1965;93:994–1001. doi: 10.1016/0002-9378(65)90161-4. [DOI] [PubMed] [Google Scholar]
- 20.Kirschner M.A., Bardin C.W., Hembree W.C., Ross G.T. Effect of estrogen administration on androgen production and plasma luteinizing hormone in hirsute women. J Clin Endocrinol Metab. 1970;30:727–732. doi: 10.1210/jcem-30-6-727. [DOI] [PubMed] [Google Scholar]
- 21.Beck P., Grayzel E.F., Young I.S., Kupperman H.S. Induction of ovulation with clomiphene. Report of a study including comparison with intravenous estrogen and human chorionic gonadotrophin. Obstet Gynecol. 1966;27:54–64. [PubMed] [Google Scholar]
- 22.Rakoff A.E. Hormonal changes following low-dosage irradiation of pituitary and ovaries in anovulatory women; further studies. Fertil Steril. 1953;4:263–271. doi: 10.1016/s0015-0282(16)31323-1. [DOI] [PubMed] [Google Scholar]
- 23.Kistner R.W., Smith O.W. Observations on the use of non-steroidal estrogen antagonist: MER-25. Fertil Steril. 1961;12:121–141. doi: 10.1016/s0015-0282(16)34082-1. [DOI] [PubMed] [Google Scholar]
- 24.Greenblatt R.B., Barfield W.E., Jungck E.C., Ray A.W. Induction of ovulation with MRL/41. Preliminary report. JAMA. 1961;178:101–104. doi: 10.1001/jama.1961.03040410001001. [DOI] [PubMed] [Google Scholar]
- 25.Adashi E.Y. Clomiphene citrate: mechanism(s) and site(s) of action--a hypothesis revisited. Fertil Steril. 1984;42:331–344. doi: 10.1016/s0015-0282(16)48069-6. [DOI] [PubMed] [Google Scholar]
- 26.Riley G.M., Evans T.N. Effects of clomiphene citrate on anovulatory ovarian function. Am J Obstet Gynecol. 1964;89:97–110. doi: 10.1016/s0002-9378(16)35046-3. [DOI] [PubMed] [Google Scholar]
- 27.Vorys N., Gantt C.L., Hamwi G.J., Copeland W.E., Uller J.C. Clinical utility of chemical induction of ovulation. Am J Obstet Gynecol. 1964;88:425–432. doi: 10.1016/0002-9378(64)90497-1. [DOI] [PubMed] [Google Scholar]
- 28.Naville A.H., Kistner R.W., Wheatley R.E., Rock J. Induction of ovulation with clomiphene-citrate. Fertil Steril. 1964;15:290–309. doi: 10.1016/s0015-0282(16)35225-6. [DOI] [PubMed] [Google Scholar]
- 29.Kistner R.W. Further observations on the effect of clomiphene citrate in anovulatory female. Am J Obstet Gynecol. 1965;92:380–420. doi: 10.1016/0002-9378(65)90393-5. [DOI] [PubMed] [Google Scholar]
- 30.Yen S.S., Vela P., Rankin J. Inappropriate secretion of follicle-stimulating hormone and luteinizing hormone in polycystic ovarian disease. J Clin Endocrinol Metab. 1970;30:435–442. doi: 10.1210/jcem-30-4-435. [DOI] [PubMed] [Google Scholar]
- 31.Rust L.A., Israel R., Mishell D.R., Jr. An individualized graduated therapeutic regimen for clomiphene citrate. Am J Obstet Gynecol. 1974;120:785–790. doi: 10.1016/0002-9378(74)90582-1. [DOI] [PubMed] [Google Scholar]
- 32.Jones G.S., De Moraes-Ruehsen M. Induction of ovulation with human gonadotropins and with clomiphene. Fertil Steril. 1965;16:461–484. doi: 10.1016/s0015-0282(16)35646-1. [DOI] [PubMed] [Google Scholar]
- 33.Raj S.G., Berger M.J., Grimes E.M., Taymor M.L. The use of gonadotropins for the induction of ovulation in women with polycystic ovarian disease. Fertil Steril. 1977;28:1280–1284. doi: 10.1016/s0015-0282(16)42969-9. [DOI] [PubMed] [Google Scholar]
- 34.Wang C.F. Gemzell C The use of human gonadotropins for the induction of ovulation in women with polycystic ovarian disease. Fertil Steril. 1980;33:479–486. doi: 10.1016/s0015-0282(16)44711-4. [DOI] [PubMed] [Google Scholar]
- 35.Schoemaker J., Wentz A.C., Jones G.S., Dubin N.H., Sapp K.C. Stimulation of follicular growth with “pure” FSH in patients with anovulation and elevated LH levels. Obstet Gynecol. 1978;51:270–277. doi: 10.1097/00006250-197803000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Judd H.L., Rigg L.A., Anderson D.C., Yen S.S. The effects of ovarian wedge resection on circulating gonadotropin and ovarian steroid levels in patients with polycystic ovary syndrome. J Clin Endocrinol Metab. 1976;43:347–355. doi: 10.1210/jcem-43-2-347. [DOI] [PubMed] [Google Scholar]
- 37.Mahesh V.B., Toledo S.P., Mattar E. Hormone levels following wedge resection in polycystic ovary syndrome. Obstet Gynecol. 1978;51 64s–9s. [PubMed] [Google Scholar]
- 38.Easterling W.E., Talbert L.M., Potter H.D. Serum testosterone levels in the polycystic ovary syndrome. Effect of an estrogen-progestin on protein binding of testosterone. Am J Obstet Gynecol. 1974;120:385–389. doi: 10.1016/0002-9378(74)90242-7. [DOI] [PubMed] [Google Scholar]
- 39.Talbert L.M., Sloan C. The effect of a low-dose oral contraceptive on serum testosterone levels in polycystic ovary disease. Obstet Gynecol. 1979;53:694–697. [PubMed] [Google Scholar]
- 40.Palmer R., de Brux J. Resultats histologiques, biochimiques et therapeutiques obtenus chez les femmes dont les ovaires avalent ete diagnostiques Stein-Leventhal a la coelioscopie. Bull Fed Gynec Obstet Franc. 1967;19:405–412. [PubMed] [Google Scholar]
- 41.Neuwirth R.S. A method of bilateral ovarian biopsy at laparoscopy in infertility and chronic anovulation. Fertil Steril. 1972;23:361–366. doi: 10.1016/s0015-0282(16)38948-8. [DOI] [PubMed] [Google Scholar]
- 42.Gjonnaess H. Polycystic ovarian syndrome treated by ovarian electrocautery through the laparoscope. Fertil Steril. 1984;41:20–25. doi: 10.1016/s0015-0282(16)47534-5. [DOI] [PubMed] [Google Scholar]
- 43.Donesky B.W., Adashi E.Y. Surgically induced ovulation in the polycystic ovary syndrome: wedge resection revisited in the age of laparoscopy. Fertil Steril. 1995;63:439–463. doi: 10.1016/s0015-0282(16)57408-1. [DOI] [PubMed] [Google Scholar]
- 44.Rebar R., Judd H.L., Yen S.S., Rakoff J., Vandenberg G., Naftolin F. Characterization of the inappropriate gonadotropin secretion in polycystic ovary syndrome. J Clin Invest. 1976;57:1320–1329. doi: 10.1172/JCI108400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shaw R.W., Duignan N.M., Butt W.R., Logan-Edwards R., London D.R. Modification by sex steroids of LHRH response in the polycystic ovary syndrome. Clin Endocrinol (Oxf) 1976;5:495–502. doi: 10.1111/j.1365-2265.1976.tb01978.x. [DOI] [PubMed] [Google Scholar]
- 46.Berger M.J., Taymor M.L., Patton W.C. Gonadotropin levels and secretory pattern in patients with typical and atypical polycystic ovary syndrome. Fertil Steril. 1975;26:619–626. [PubMed] [Google Scholar]
- 47.Duignan N.M., Shaw R.W., Rudd B.T., Holder G., Williams J.W., Butt W.R., et al. Sex hormone levels and gonadotropin release in the polycystic ovary syndrome. Clin Endocrinol (Oxf) 1975;4:287–295. doi: 10.1111/j.1365-2265.1975.tb01536.x. [DOI] [PubMed] [Google Scholar]
- 48.Anderson D.C. Sex-hormone-binding globulin. Clin Endocrinol (Oxf) 1974;3:69–96. doi: 10.1111/j.1365-2265.1974.tb03298.x. [DOI] [PubMed] [Google Scholar]
- 49.De Vane G.W., Czekala N.M., Judd H.L., Yen S.S. Circulating gonadotropins, estrogens, and androgens in polycystic ovarian disease. Am J Obstet Gynecol. 1975;121:496–500. doi: 10.1016/0002-9378(75)90081-2. [DOI] [PubMed] [Google Scholar]
- 50.Judd H.L., McPherson R.A., Rakoff J.S., Yen S.S. Correlation of the effects of dexamethasone administration on urinary 17-ketosteroid and serum androgen levels in patients with hirsutism. Am J Obstet Gynecol. 1977;128:408–417. doi: 10.1016/0002-9378(77)90560-9. [DOI] [PubMed] [Google Scholar]
- 51.Bardin C.W., Hembree W.C., Lipsett M.B. Suppression of testosterone and androstenedione production rates with dexamethasone in women with idiopathic hirsutism and polycystic ovaries. J Clin Endocrinol Metab. 1968;28:1300–1306. doi: 10.1210/jcem-28-9-1300. [DOI] [PubMed] [Google Scholar]
- 52.Lachelin G.C., Barnett M., Hopper B.R., Brink G., Yen S.S. Adrenal function in normal women and women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1979;49:892–898. doi: 10.1210/jcem-49-6-892. [DOI] [PubMed] [Google Scholar]
- 53.Swanson M., Sauerbrei E.E., Cooperberg P.L. Medical implications of ultrasonically detected polycystic ovaries. J Clin Ultrasound. 1981;9:219–222. doi: 10.1002/jcu.1870090504. [DOI] [PubMed] [Google Scholar]
- 54.Shoham Z., Conway G.S., Patel A., Jacobs H.S. Polycystic ovaries in patients with hypogonadotropic hypogonadism: similarity of ovarian response to gonadotropin stimulation in patients with polycystic ovarian syndrome. Fertil Steril. 1992;58:37–45. doi: 10.1016/s0015-0282(16)55134-6. [DOI] [PubMed] [Google Scholar]
- 55.Adams J., Franks S., Polson D.W., Mason H.D., Abdulwahid N., Tucker M., et al. Multifollicular ovaries: clinical and endocrine features and response to pulsatile gonadotropin releasing hormone. Lancet. 1985;2:1375–1379. doi: 10.1016/s0140-6736(85)92552-8. [DOI] [PubMed] [Google Scholar]
- 56.Tucker M., Adams J., Mason W.P., Jacobs H.S. Infertility, megalocystic and polycystic ovaries: differential response to LHRH therapy. Ups J Med Sci. 1984;89:43–46. doi: 10.3109/03009738409178461. [DOI] [PubMed] [Google Scholar]
- 57.Norman R.J., Hague W.M., Masters S.C., Wang X.J. Subjects with polycystic ovaries without hyperandrogenaemia exhibit similar disturbances in insulin and lipid profiles as those with polycystic ovary syndrome. Hum Reprod. 1995;10:2258–2261. doi: 10.1093/oxfordjournals.humrep.a136280. [DOI] [PubMed] [Google Scholar]
- 58.Quigley M.E., Rakoff J.S., Yen S.S. Increased luteinizing hormone sensitivity to dopamine inhibition in polycystic ovary syndrome. J Clin Endocrinol Metab. 1981;52:231–234. doi: 10.1210/jcem-52-2-231. [DOI] [PubMed] [Google Scholar]
- 59.Carmina E., Rosato F., Maggiore M., Gagliano A.M., Indovina D., Janni A. Prolactin secretion in polycystic ovary syndrome (PCO): correlation with the steroid pattern. Acta Endocrinol (Copenh) 1984;105:99–104. doi: 10.1530/acta.0.1050099. [DOI] [PubMed] [Google Scholar]
- 60.Luciano A.A., Chapler F.K., Sherman B.M. Hyperprolactinemia in polycystic ovary syndrome. Fertil Steril. 1984;41:719–725. [PubMed] [Google Scholar]
- 61.Cumming D.C., Reid R.L., Quigley M.E., Rebar R.W., Yen S.S. Evidence for decreased endogenous dopamine and opioid inhibitory influences on LH secretion in polycystic ovary syndrome. Clin Endocrinol (Oxf) 1984;20:643–648. doi: 10.1111/j.1365-2265.1984.tb00114.x. [DOI] [PubMed] [Google Scholar]
- 62.Barnes R.B., Lobo R.A. Central opioid activity in polycystic ovary syndrome with and without dopaminergic modulation. J Clin Endocrinol Metab. 1985;61:779–782. doi: 10.1210/jcem-61-4-779. [DOI] [PubMed] [Google Scholar]
- 63.Seppala M., Hirvonen E., Ranta T. Bromocriptine treatment of secondary amenorrhea. Lancet. 1976;1:1154–1156. doi: 10.1016/s0140-6736(76)91542-7. [DOI] [PubMed] [Google Scholar]
- 64.Barnes R.B., Mileikowsky G.N., Cha K.Y., Spencer C.A., Lobo R.A. Effects of dopamine and metoclopramide in polycystic ovary syndrome. J Clin Endocrinol Metab. 1986;63:506–509. doi: 10.1210/jcem-63-2-506. [DOI] [PubMed] [Google Scholar]
- 65.Falaschi P., Rocco A., del Pozo E. Inhibitory effect of bromocriptine treatment on luteinizing hormone secretion in polycystic ovary syndrome. J Clin Endocrinol Metab. 1986;62:348–351. doi: 10.1210/jcem-62-2-348. [DOI] [PubMed] [Google Scholar]
- 66.Zumoff B., Freeman R.A., Coupey S., Saenger P., Markowitz M., Kream J. A chronobiologic abnormality in luteinizing hormone secretion in teenage girls with the polycystic-ovary syndrome. N Engl J Med. 1983;309:1206–1209. doi: 10.1056/NEJM198311173092002. [DOI] [PubMed] [Google Scholar]
- 67.Burger C.W., Korsen T., van Kesse H., van Dop P.A., Caron F.J., Schoemaker J. Pulsatile luteinizing hormone patterns in the follicular phase of the menstrual cycle, polycystic ovarian disease (PCOD) and non-PCOD secondary amenorrhea. J Clin Endocrinol Metab. 1985;61:1126–1132. doi: 10.1210/jcem-61-6-1126. [DOI] [PubMed] [Google Scholar]
- 68.Waldstreicher J., Santoro N.F., Hall J.E., Filicori M., Crowley W.F., Jr. Hyperfunction of the hypothalamic-pituitary axis in women with polycystic ovarian disease: indirect evidence for partial gonadotroph desensitization. J Clin Endocrinol Metab. 1988;66:165–172. doi: 10.1210/jcem-66-1-165. [DOI] [PubMed] [Google Scholar]
- 69.Kazer R.R., Kessel B., Yen S.S. Circulating luteinizing hormone pulse frequency in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1987;65:233–236. doi: 10.1210/jcem-65-2-233. [DOI] [PubMed] [Google Scholar]
- 70.Wildt L., Hausler A., Marshall G., Hutchison J.S., Plant T.M., Belchetz P.E., et al. Frequency and amplitude of gonadotropin-releasing hormone stimulation and gonadotropin secretion in the rhesus monkey. Endocrinology. 1981;109:376–385. doi: 10.1210/endo-109-2-376. [DOI] [PubMed] [Google Scholar]
- 71.Reid R.L., Leopold G.R., Yen S.S. Induction of ovulation and pregnancy with pulsatile luteinizing hormone releasing factor: dosage and mode of delivery. Fertil Steril. 1981;36:553–559. doi: 10.1016/s0015-0282(16)45850-4. [DOI] [PubMed] [Google Scholar]
- 72.Dodson W.C., Hughes C.L., Whitesides D.B., Haney A.F. The effect of leuprolide acetate on ovulation induction with human menopausal gonadotropins in polycystic ovary syndrome. J Clin Endocrinol Metab. 1987;65:95–100. doi: 10.1210/jcem-65-1-95. [DOI] [PubMed] [Google Scholar]
- 73.Barnes R.B., Rosenfield R.L., Burstein S., Ehrmann D.A. Pituitary-ovarian responses to nafarelin testing in the polycystic ovary syndrome. N Engl J Med. 1989;320:559–565. doi: 10.1056/NEJM198903023200904. [DOI] [PubMed] [Google Scholar]
- 74.Achard C., Thiers J. Le virilisme pilaire et son association a l'insuffisance glycolytique (diabete des fammes a barb) Bull Acad Natl Med. 1921;86:51–64. [Google Scholar]
- 75.Hollingsworth D.R., Amatruda T.T., Jr. Acanthosis nigricans and obesity, an endocrine abnormality? Arch Intern Med. 1969;124:481–487. [PubMed] [Google Scholar]
- 76.Givens J.R., Wiser W.L., Coleman S.A., Wilroy R.S., Andersen R.N., Fish S.A. Familial ovarian hyperthecosis: a study of two families. Am J Obstet Gynecol. 1971;110:959–972. [Google Scholar]
- 77.Kahn C.R., Flier J.S., Bar R.S., Archer J.A., Gorden P., Martin M.M., et al. The syndromes of insulin resistance and acanthosis nigricans. Insulin-receptor disorders in man. N Engl J Med. 1976;294:739–745. doi: 10.1056/NEJM197604012941401. [DOI] [PubMed] [Google Scholar]
- 78.Burghen G.A., Givens J.R., Kitabchi A.E. Correlation of hyperandrogenism with hyperinsulinism in polycystic ovarian disease. J Clin Endocrinol Metab. 1980;50:113–116. doi: 10.1210/jcem-50-1-113. [DOI] [PubMed] [Google Scholar]
- 79.Chang R.J., Nakamura R.M., Judd H.L., Kaplan S.A. Insulin resistance in nonobese patients with polycystic ovarian disease. J Clin Endocrinol Metab. 1983;57:356–359. doi: 10.1210/jcem-57-2-356. [DOI] [PubMed] [Google Scholar]
- 80.Barbieri R.L., Ryan K.J. Hyperandrogenism, insulin resistance, and acanthosis nigricans syndrome: a common endocrinopathy with distinct pathophysiologic features. Am J Obstet Gynecol. 1983;147:90–101. doi: 10.1016/0002-9378(83)90091-1. [DOI] [PubMed] [Google Scholar]
- 81.Pasquali R., Casimirri F., Venturoli S., Paradisi R., Mattioli L., Capelli M., et al. Insulin resistance in patients with polycystic ovaries: its relationship to body weight and androgen levels. Acta Endocrinol (Copenh) 1983;104:110–116. doi: 10.1530/acta.0.1040110. [DOI] [PubMed] [Google Scholar]
- 82.Shoupe D., Kumar D.D., Lobo R.A. Insulin resistance in polycystic ovary syndrome. Am J Obstet Gynecol. 1983;147:588–592. doi: 10.1016/0002-9378(83)90023-6. [DOI] [PubMed] [Google Scholar]
- 83.Cotrozzi G., Matteini M., Relli P., Lazzari T. Hyperinsulinism and insulin resistance in polycystic ovarian syndrome: a verification using oral glucose, I.V. glucose and tolbutamide. Acta Diabetol Lat. 1983;20:135–142. doi: 10.1007/BF02624914. [DOI] [PubMed] [Google Scholar]
- 84.Dunaif A., Segal K.R., Futterweit W., Dobrjansky A. Profound peripheral insulin resistance, independent of obesity, in polycystic ovary syndrome. Diabetes. 1989;38:1165–1174. doi: 10.2337/diab.38.9.1165. [DOI] [PubMed] [Google Scholar]
- 85.Dunaif A., Segal K.R., Shelley D.R., Green G., Dobrjansky A., Licholai T. Evidence for distinctive and intrinsic defects in insulin action in polycystic ovary syndrome. Diabetes. 1992;41:1257–1266. doi: 10.2337/diab.41.10.1257. [DOI] [PubMed] [Google Scholar]
- 86.Dunaif A., Sorbara L., Delson R., Green G. Ethnicity and polycystic ovary syndrome are associated with independent and additive decreases in insulin action in Caribbean-Hispanic women. Diabetes. 1993;42:1462–1468. doi: 10.2337/diab.42.10.1462. [DOI] [PubMed] [Google Scholar]
- 87.O'Meara N.M., Blackman J.D., Ehrmann D.A., Barnes R.B., Jaspan J.B., Rosenfield R.L., et al. Defects in beta-cell function in functional ovarian hyperandrogenism. J Clin Endocrinol Metab. 1993;76:1241–1247. doi: 10.1210/jcem.76.5.8496316. [DOI] [PubMed] [Google Scholar]
- 88.Holte J., Bergh T., Berne C., Berglund L., Lithell H. Enhanced early insulin response to glucose in relation to insulin resistance in women with polycystic ovary syndrome and normal glucose tolerance. J Clin Endocrinol Metab. 1994;78:1052–1058. doi: 10.1210/jcem.78.5.8175959. [DOI] [PubMed] [Google Scholar]
- 89.Ehrmann D.A., Sturis J., Byrne M.M., Karrison T., Rosenfield R.L., Polonsky K.S. Insulin secretory defects in polycystic ovary syndrome. Relationship to insulin sensitivity and family history of non-insulin-dependent diabetes mellitus. J Clin Invest. 1995;96:520–527. doi: 10.1172/JCI118064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dunaif A., Finegood D.T. Beta-cell dysfunction independent of obesity and glucose intolerance in the polycystic ovary syndrome. J Clin Endocrinol Metab. 1996;81:942–947. doi: 10.1210/jcem.81.3.8772555. [DOI] [PubMed] [Google Scholar]
- 91.Sorbara L.R., Tang Z., Cama A., Xia J., Schenker E., Kohanski R.A., et al. Absence of insulin receptor gene mutations in three Insulin-resistant women with the polycystic ovary syndrome. Metabolism. 1994;43:1568–1574. doi: 10.1016/0026-0495(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 92.Talbot J.A., Bicknell E.J., Rajkhowa M., Krook A., O’Rahilly S.O., Clayton R.N. Molecular scanning of the Insulin receptor gene in women with polycystic ovarian syndrome. J Clin Endocrinol Metab. 1996;81:1979–1983. doi: 10.1210/jcem.81.5.8626868. [DOI] [PubMed] [Google Scholar]
- 93.Ciaraldi T.P., El-Roeiy A., Madar Z., Reichart D., Olefsky J.M., Yen S.S. Cellular mechanisms of insulin resistance in polycystic ovarian syndrome. J Clin Endocrinol Metab. 1992;75:577–583. doi: 10.1210/jcem.75.2.1322430. [DOI] [PubMed] [Google Scholar]
- 94.Dunaif A., Xia J., Book C.B., Schenker E., Tang Z. Excessive insulin receptor serine phosphorylation in cultured fibroblasts and in skeletal muscle. A potential mechanism for insulin resistance in the polycystic ovary syndrome. J Clin Invest. 1995;96:801–810. doi: 10.1172/JCI118126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dunaif A., Wu X., Lee A., Diamanti-Kandarakis E. Defects in insulin receptor signaling in vivo in the polycystic ovary syndrome (PCOS) Am J Physiol Endocrinol Metab. 2001;281:E392–E399. doi: 10.1152/ajpendo.2001.281.2.E392. [DOI] [PubMed] [Google Scholar]
- 96.Nestler J.E., Barlascini C.O., Matt D.W., Steingold K.A., Plymate S.R., Clore J.N., et al. Suppression of serum Insulin by diazoxide reduces serum testosterone levels in obese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1989;68:1027–1032. doi: 10.1210/jcem-68-6-1027. [DOI] [PubMed] [Google Scholar]
- 97.Dunaif A., Green G., Futterweit W., Dobrjansky A. Suppression of hyperandrogenism does not improve peripheral or hepatic insulin resistance in the polycystic ovary syndrome. J Clin Endocrinol Metab. 1990;70:699–704. doi: 10.1210/jcem-70-3-699. [DOI] [PubMed] [Google Scholar]
- 98.Elkind-Hirsh K.E., Valdes C.T., Malinak L.R. Insulin resistance improves in hyperandrogenic women treated with lupron. Fertil Steril. 1993;60:634–641. doi: 10.1016/s0015-0282(16)56213-x. [DOI] [PubMed] [Google Scholar]
- 99.Moghetti P., Tosi F., Castello R., Magnani C.M., Negri C., Brun E., et al. The insulin resistance in women with hyperandrogenism is partially reversed by antiandrogen treatment: evidence that androgens impair insulin action in women. J Clin Endocrinol Metab. 1996;81:952–960. doi: 10.1210/jcem.81.3.8772557. [DOI] [PubMed] [Google Scholar]
- 100.Nestler J.E., Powers L.P., Matt D.W., Steingold K.A., Plymate S.R., Rittmaster R.S., et al. A direct effect of hyperinsulinemia on serum sex hormone-binding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1991;72:83–89. doi: 10.1210/jcem-72-1-83. [DOI] [PubMed] [Google Scholar]
- 101.Barbieri R.L., Makris A., Randall R.W., Daniel G., Kistner R.W., Ryan K.J. Insulin stimulates androgen accumulation in incubations of ovarian stroma obtained from women with hyperandrogenism. J Clin Endocrinol Metab. 1986;62:904–910. doi: 10.1210/jcem-62-5-904. [DOI] [PubMed] [Google Scholar]
- 102.Willis D., Mason H., Gilling-Smith C., Franks S. Modulation by Insulin of follicle-stimulating hormone and luteinizing hormone actions in human granulosa cells of normal and polycystic ovaries. J Clin Endocrinol Metab. 1996;81:302–309. doi: 10.1210/jcem.81.1.8550768. [DOI] [PubMed] [Google Scholar]
- 103.Nestler J.E., Jakubowicz D.J., de Vargas A.F., Brik C., Quintero N., Medina F. Insulin stimulates testosterone biosynthesis by human thecal cells from women with polycystic ovary syndrome by activating its own receptor and using inositolglycan mediators as the signal transduction system. J Clin Endocrinol Metab. 1998;83 doi: 10.1210/jcem.83.6.4886. 2001–5. [DOI] [PubMed] [Google Scholar]
- 104.Poretsky L., Seto-Young D., Shrestha A., Dhillon S., Mirjany M., Liu H.C., et al. Phosphatidyl-inositol-3 kinase-independent insulin action pathway(s) in the human ovary. J Clin Endocrinol Metab. 2001;86:3115–3119. doi: 10.1210/jcem.86.7.7617. [DOI] [PubMed] [Google Scholar]
- 105.Dunaif A., Graf M., Mandeli J., Laumas V., Dobrjansky A. Characterization of groups of hyperandrogenic women with acanthosis nigricans, impaired glucose tolerance, and/or hyperinsulinemia. J Clin Endocrinol Metab. 1987;65:499–507. doi: 10.1210/jcem-65-3-499. [DOI] [PubMed] [Google Scholar]
- 106.Dahlgren E., Johansson S., Lindstedt G., Knutsson F., Oden A., Janson P.O., et al. Women with polycystic ovary syndrome wedge resected in 1956 to 1965: a long-term follow-up focusing on natural history and circulating hormones. Fertil Steril. 1992;57:505–513. doi: 10.1016/s0015-0282(16)54892-4. [DOI] [PubMed] [Google Scholar]
- 107.Ehrmann D.A., Barnes R.B., Rosenfeld R.L., Cavaghan M.K., Imperial J. Prevalence of impaired glucose tolerance and diabetes in women with polycystic ovary syndrome. Diabetes Care. 1999;22:141–146. doi: 10.2337/diacare.22.1.141. [DOI] [PubMed] [Google Scholar]
- 108.Legro R.S., Kunselman A.R., Dodson W.C., Dunaif A. Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: a prospective, controlled study in 254 affected women. J Clin Endocrinol Metab. 1999;84:165–169. doi: 10.1210/jcem.84.1.5393. [DOI] [PubMed] [Google Scholar]
- 109.Wild R.A., Painter P.C., Coulson P.B., Carruth K.B., Ranney G.B. Lipoprotein lipid concentration and cardiovascular risk in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1985;61:946–951. doi: 10.1210/jcem-61-5-946. [DOI] [PubMed] [Google Scholar]
- 110.Talbott E., Guzick D., Clerici A., Berga S., Detre K., Weimer K., et al. Coronary heart disease risk factors in women with polycystic ovary syndrome. Arterioscler Thromb Vasc Biol. 1995;15:821–826. doi: 10.1161/01.atv.15.7.821. [DOI] [PubMed] [Google Scholar]
- 111.Robinson S., Henderson A.D., Gelding S.V., Kiddy D., Niththyananthan R., Bush A., et al. Dyslipidaemia is associated with Insulin resistance in women with polycystic ovaries. Clin Endocrinol (Oxf) 1996;44:277–284. doi: 10.1046/j.1365-2265.1996.674495.x. [DOI] [PubMed] [Google Scholar]
- 112.Rajkhowa M., Neary R.H., Kumpatla P., Game F.L., Jones P.W., Obhrai M.S., et al. Altered composition of high-density lipoproteins in women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1997;82:3389–3394. doi: 10.1210/jcem.82.10.4318. [DOI] [PubMed] [Google Scholar]
- 113.Talbott E., Clerici A., Berga S.L., Kuller L., Guzick D., Detre K., et al. Adverse lipid and coronary heart disease risk profiles in young women with polycystic ovary syndrome: results of a case-control study. J Clin Epidemiol. 1998;51:415–422. doi: 10.1016/s0895-4356(98)00010-9. [DOI] [PubMed] [Google Scholar]
- 114.Sampson M., Kong C., Patel A., Unwin R., Jacobs H.S. Ambulatory blood pressure profiles and plasminogen activator inhibitor (PAI-1) activity in lean women with and without the polycystic ovary syndrome. Clin Endocrinol (Oxf) 1996;45:623–629. doi: 10.1046/j.1365-2265.1996.00863.x. [DOI] [PubMed] [Google Scholar]
- 115.Zimmerman S., Phillips R.A., Dunaif A., Finegood D.T., Wilkenfeld C., Ardeljan M., et al. Polycystic ovary syndrome: lack of hypertension despite profound insulin resistance. J Clin Endocrinol Metab. 1992;75:508–513. doi: 10.1210/jcem.75.2.1639952. [DOI] [PubMed] [Google Scholar]
- 116.Wild R.A., Grubb B., Hartz A., Van Nort J.J., Bachman W., Bartholomew M. Clinical signs of androgen excess as risk factors for coronary artery disease. Fertil Steril. 1990;54:255–259. doi: 10.1016/s0015-0282(16)53699-1. [DOI] [PubMed] [Google Scholar]
- 117.Birdsall M.A., Farquhar C.M., White H.D. Association between polycystic ovaries and extent of coronary artery disease in women having cardiac catheterization. Ann Intern Med. 1997;126:32–35. doi: 10.7326/0003-4819-126-1-199701010-00005. [DOI] [PubMed] [Google Scholar]
- 118.Guzick D.S., Talbott E.O., Sutton-Tyrrell K., Herzog H.C., Kuller L.H., Wolfson S.K., Jr. Carotid atherosclerosis in women with polycystic ovary syndrome: initial results from a case-control study. Am J Obstet Gynecol. 1996;174:1224–1229. doi: 10.1016/s0002-9378(96)70665-8. discussion 1229–32. [DOI] [PubMed] [Google Scholar]
- 119.Cibula D., Cifkova R., Fanta M., Poledne R., Zivny J., Skibova J. Increased risk of non-insulin dependent diabetes mellitus, arterial hypertension and coronary artery disease in perimenopausal women with a history of the polycystic ovary syndrome. Hum Reprod. 2000;15:785–789. doi: 10.1093/humrep/15.4.785. [DOI] [PubMed] [Google Scholar]
- 120.Wild S., Pierpoint T., McKeigue P., Jacobs H. Cardiovascular disease in women with polycystic ovary syndrome at long- term follow-up: a retrospective cohort study. Clin Endocrinol (Oxf) 2000;52:595–600. doi: 10.1046/j.1365-2265.2000.01000.x. [DOI] [PubMed] [Google Scholar]
- 121.Velazquez E.M., Mendoza S., Hamer T., Sosa F., Glueck C.J. Metformin therapy in polycystic ovary syndrome reduces hyperinsulinemia, insulin resistance, hyperandrogenemia, and systolic blood pressure, while facilitating normal menses and pregnancy. Metabolism. 1994;43:647–654. doi: 10.1016/0026-0495(94)90209-7. [DOI] [PubMed] [Google Scholar]
- 122.Nestler J.E., Jakubowicz D.J. Decreases in ovarian cytochrome P450c17 alpha activity and serum free testosterone after reduction of insulin secretion in polycystic ovary syndrome. N Engl J Med. 1996;335:617–623. doi: 10.1056/NEJM199608293350902. [DOI] [PubMed] [Google Scholar]
- 123.Velazquez E., Acosta A., Mendoza S.G. Menstrual cyclicity after metformin therapy in polycystic ovary syndrome. Obstet Gynecol. 1997;90:392–395. doi: 10.1016/s0029-7844(97)00296-2. [DOI] [PubMed] [Google Scholar]
- 124.Morin-Papunen L.C., Koivunen R.M., Ruokonen A., Martikainen H.K. Metformin therapy improves the menstrual pattern with minimal endocrine and metabolic effects in women with polycystic ovary syndrome. Fertil Steril. 1998;69:691–696. doi: 10.1016/s0015-0282(98)00011-9. [DOI] [PubMed] [Google Scholar]
- 125.Glueck C.J., Wang P., Fontaine R., Tracy T., Sieve-Smith L. Metformin-induced resumption of normal menses in 39 of 43 (91%) previously amenorrheic women with the polycystic ovary syndrome. Metabolism. 1999;48:511–519. doi: 10.1016/s0026-0495(99)90113-0. [DOI] [PubMed] [Google Scholar]
- 126.Ehrmann D.A., Cavaghan M.K., Imperial J., Sturis J., Rosenfield R.L., Polonsky K.S. Effects of metformin on insulin secretion, Insulin action, and ovarian steroidogenesis in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1997;82:524–530. doi: 10.1210/jcem.82.2.3722. [DOI] [PubMed] [Google Scholar]
- 127.Moghetti P., Castello R., Negri C., Tosi F., Perrone F., Caputo M., et al. Metformin effects on clinical features, endocrine and metabolic profiles, and insulin sensitivity in polycystic ovary syndrome: a randomized, double-blind, placebo-controlled 6-month trial, followed by open, long-term clinical evaluation. J Clin Endocrinol Metab. 2000;85:139–146. doi: 10.1210/jcem.85.1.6293. [DOI] [PubMed] [Google Scholar]
- 128.Dunaif A., Scott D., Finegood D., Quintana B., Whitcomb D.R. The Insulin-sensitizing agent troglitazone improves metabolic and reproductive abnormalities in the polycystic ovary syndrome. J Clin Endocrinol Metab. 1996;81:3299–3306. doi: 10.1210/jcem.81.9.8784087. [DOI] [PubMed] [Google Scholar]
- 129.Ehrmann D.A., Schneider D.J., Sobel B.E., Cavaghan M.K., Imperial J., Rosenfield R.L., et al. Troglitazone improves defects in insulin action, insulin secretion, ovarian steroidogenesis, and fibrinolysis in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1997;82:2108–2116. doi: 10.1210/jcem.82.7.4069. [DOI] [PubMed] [Google Scholar]
- 130.Hasegawa I., Murakawa H., Suzuki M., Yamamoto Y., Kurabayaski T., Tanaka K. Effect of troglitazone on endocrine and ovulatory performance in women with insulin resistance-related polycystic ovary syndrome. Fertil Steril. 1999;71:323–327. doi: 10.1016/s0015-0282(98)00454-3. [DOI] [PubMed] [Google Scholar]
- 131.Koshiyama H., Shimono D., Kuwamura N., Minamikawa J., Nakamura Y. Rapid communication: inhibitory effect of pioglitazone on carotid arterial wall thickness in type 2 diabetes. J Clin Endocrinol Metab. 2001;86:3452–3456. doi: 10.1210/jcem.86.7.7810. [DOI] [PubMed] [Google Scholar]
- 132.Nestler J.E., Jakubowicz D.J., Evans W.S., Pasquali R. Effects of metformin on spontaneous and clomiphene-induced ovulation in the polycystic ovary syndrome. N Engl J Med. 1998;338:1876–1880. doi: 10.1056/NEJM199806253382603. [DOI] [PubMed] [Google Scholar]
- 133.Mitwally M.F., Kuscu N.K., Yalcinkaya T.M. High ovulatory rates with use of troglitazone in clomiphene-resistant women with polycystic ovary syndrome. Hum Reprod. 1999;14:2700–2703. doi: 10.1093/humrep/14.11.2700. [DOI] [PubMed] [Google Scholar]
- 134.Nestler J.E., Jakubowicz D.J., Reamer P., Gunn R.D., Allan G. Ovulatory and metabolic effects of D-chiro-inositol in the polycystic ovary syndrome. N Engl J Med. 1999;340:1314–1320. doi: 10.1056/NEJM199904293401703. [DOI] [PubMed] [Google Scholar]
- 135.Kamrava M.M., Seibel M.M., Berger M.J., Thompson I., Taymor M.L. Reversal of persistent anovulation in polycystic ovarian disease by administration of chronic low-dose follicle-stimulating hormone. Fertil Steril. 1982;37:520–523. doi: 10.1016/s0015-0282(16)46159-5. [DOI] [PubMed] [Google Scholar]
- 136.Polson D.W., Mason H.D., Saldahna M.B., Franks S. Ovulation of a single dominant follicle during treatment with low-dose pulsatile follicle stimulating hormone in women with polycystic ovary syndrome. Clin Endocrinol (Oxf) 1987;26:205–212. doi: 10.1111/j.1365-2265.1987.tb00778.x. [DOI] [PubMed] [Google Scholar]
- 137.Shoham Z., Patel A., Jacobs H.S. Polycystic ovarian syndrome: safety and effectiveness of stepwise and low-dose administration of purified follicle-stimulating hormone. Fertil Steril. 1991;55:1051–1056. doi: 10.1016/s0015-0282(16)54351-9. [DOI] [PubMed] [Google Scholar]
- 138.Homburg R., Levy T., Ben-Rafael Z. A comparative prospective study of conventional regimen with chronic low-dose administration of follicle-stimulating hormone for anovulation associated with polycystic ovary syndrome. Fertil Steril. 1995;63:729–733. doi: 10.1016/s0015-0282(16)57473-1. [DOI] [PubMed] [Google Scholar]
- 139.Andoh K., Mizunuma H., Liu X., Kamijo T., Yamada K., Ibuki Y. A comparative study of fixed-dose, step-down, and low-dose step-up regimens of human menopausal gonadotropin for patients with polycystic ovary syndrome. Fertil Steril. 1998;70:840–846. doi: 10.1016/s0015-0282(98)00308-2. [DOI] [PubMed] [Google Scholar]
- 140.Salat-Baroux J., Alvarez S., Antoine J.M., Cornet D., Tibi C., Plachot M., et al. Results of IVF in the treatment of polycystic ovary disease. Hum Reprod. 1988;3:331–335. doi: 10.1093/oxfordjournals.humrep.a136704. [DOI] [PubMed] [Google Scholar]
- 141.Homburg R., Berkowitz D., Levy T., Feldberg D., Ashkenazi J., Ben-Rafael Z. In vitro fertilization and embryo transfer for the treatment of infertility associated with polycystic ovary syndrome. Fertil Steril. 1993;60:858–863. doi: 10.1016/s0015-0282(16)56287-6. [DOI] [PubMed] [Google Scholar]
- 142.Dale P.O., Tanbo T., Abyholm T. In-vitro fertilization in infertile women with the polycystic ovarian syndrome. Hum Reprod. 1991;6:238–241. doi: 10.1093/oxfordjournals.humrep.a137313. [DOI] [PubMed] [Google Scholar]
- 143.MacDougall M.J., Tan S.L., Balen A., Jacobs H.S. A controlled study comparing patients with and without polycystic ovaries undergoing in-vitro fertilization. Hum Reprod. 1993;8:233–237. doi: 10.1093/oxfordjournals.humrep.a138029. [DOI] [PubMed] [Google Scholar]
- 144.Cooper H.E., Spellacy W.N., Prem K.A., Cohen W.D. Hereditary factors in the Stein-Leventhal syndrome. Am J Obstet Gynecol. 1968;100:371–387. doi: 10.1016/s0002-9378(15)33704-2. [DOI] [PubMed] [Google Scholar]
- 145.Simpson J.L., Christakos A.C. Hereditary factors in obstetrics and gynecology. Obstet Gynecol Surv. 1969;24:580–601. doi: 10.1097/00006254-196907000-00002. [DOI] [PubMed] [Google Scholar]
- 146.Givens J.R. Familial polycystic ovarian disease. Endocrinol Metab Clin North Am. 1988;17:771–783. [PubMed] [Google Scholar]
- 147.Lunde O., Magnus P., Sandvik L., Hoglo S. Familial clustering in the polycystic ovarian syndrome. Gynecol Obstet Invest. 1989;28:23–30. doi: 10.1159/000293493. [DOI] [PubMed] [Google Scholar]
- 148.Carey A.H., Chan K.L., Short F., White D., Williamson R., Franks S. Evidence for a single gene effect causing polycystic ovaries and male pattern baldness. Clin Endocrinol (Oxf) 1993;38:653–658. doi: 10.1111/j.1365-2265.1993.tb02150.x. [DOI] [PubMed] [Google Scholar]
- 149.Govind A., Obhrai M.S., Clayton R.N. Polycystic ovaries are inherited as an autosomal dominant trait: analysis of 29 polycystic ovary syndrome and 10 control families. J Clin Endocrinol Metab. 1999;84:38–43. doi: 10.1210/jcem.84.1.5382. [DOI] [PubMed] [Google Scholar]
- 150.Ferriman D., Purdie A.W. The inheritance of polycystic ovarian disease and a possible relationship to premature balding. Clin Endocrinol (Oxf) 1979;11:291–300. doi: 10.1111/j.1365-2265.1979.tb03077.x. [DOI] [PubMed] [Google Scholar]
- 151.Carey A.H., Waterworth D., Patel K., White D., Little J., Novelli P., et al. Polycystic ovaries and premature male pattern baldness are associated with one allele of the steroid metabolism gene CYP17. Hum Mol Genet. 1994;3:1873–1876. doi: 10.1093/hmg/3.10.1873. [DOI] [PubMed] [Google Scholar]
- 152.Rosenfield R.L., Barnes R.B., Cara J.F., Lucky A.W. Dysregulation of cytochrome P450c 17 alpha as the cause of polycystic ovarian syndrome. Fertil Steril. 1990;53:785–791. [PubMed] [Google Scholar]
- 153.Gharani N., Waterworth D.M., Williamson R., Franks S. 5' polymorphism of the CYP17 gene is not associated with serum testosterone levels in women with polycystic ovaries. J Clin Endocrinol Metab. 1996;81:4174. doi: 10.1210/jcem.81.11.8923880. [DOI] [PubMed] [Google Scholar]
- 154.Techatraisak K., Conway G.S., Rumsby G. Frequency of a polymorphism in the regulatory region of the 17 alpha-hydroxylase-17,20-lyase (CYP17) gene in hyperandrogenic states. Clin Endocrinol (Oxf) 1997;46:131–134. doi: 10.1046/j.1365-2265.1997.8700880.x. [DOI] [PubMed] [Google Scholar]
- 155.Urbanek M., Legro R.S., Driscoll D.A., Azziz R., Ehrmann D.A., Norman R.J., et al. Thirty-seven candidate genes for polycystic ovary syndrome: strongest evidence for linkage is with follistatin. Proc Natl Acad Sci U S A. 1999;96:8573–8578. doi: 10.1073/pnas.96.15.8573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Gharani N., Waterworth D.M., Batty S., White D., Gilling-Smith C., Conway G.S., et al. Association of the steroid synthesis gene CYP l la with polycystic ovary syndrome and hyperandrogenism. Hum Mol Genet. 1997;6:397–402. doi: 10.1093/hmg/6.3.397. [DOI] [PubMed] [Google Scholar]
- 157.Waterworth D.M., Bennett S.T., Gharani N., McCarthy M.I., Hague S., Batty S., et al. Linkage and association of insulin gene VNTR regulatory polymorphism with polycystic ovary syndrome. Lancet. 1997;349:986–990. doi: 10.1016/S0140-6736(96)08368-7. [DOI] [PubMed] [Google Scholar]
- 158.Bennett S.T., Lucassen A.M., Gough S.C., Powell E.E., Undlien D.E., Pritchard L.E., et al. Susceptibility to human type l diabetes at IDDM2 is determined by tandem repeat variation at the Insulin gene minisatellite locus. Nat Genet. 1995;9:284–292. doi: 10.1038/ng0395-284. [DOI] [PubMed] [Google Scholar]