Abstract
This cross-sectional study investigates the association between race and pulse oximeter accuracy in children in the US.
Several studies using large retrospective electronic health record (EHR) data sets have found that pulse oximetry may overestimate actual blood oxygen levels in Black patients with hypoxemia more often than in White patients.1,2,3 If true, a commonly used medical device could systematically mislead clinicians to undertreat hypoxemia in Black patients, a flaw with substantial implications for health care equity and outcomes.4 However, prior EHR-based studies are limited by imprecise linkages between pulse oximetry values and blood gas laboratory results obtained up to 10 minutes apart.1,2,3 There are also few studies of race and pulse oximetry in children.3
Here we aimed to address these limitations by comparing arterial blood oxygen saturation (SaO2) and pulse oximetry (SpO2) values in Black and White children using data from a pediatric cardiac catheterization laboratory where SpO2 is captured at 1-minute intervals in the EHR and is able to be linked to arterial blood gases processed immediately via co-oximeter.
Methods
We conducted this retrospective, EHR-based study at a free-standing children’s hospital. The Children’s Hospital of Philadelphia institutional review board deemed the study exempt and waived informed consent because this was secondary research. We included patients aged 1 to 17 years with self-reported Black or African American or White race who underwent a cardiac catheterization between 2016 and 2021. We included only cases where Sao2 was measured from a location reflective of systemic arterial saturation (descending aorta, femoral artery, systemic ventricle). This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
We included the first Sao2 measurement per patient matched with an SpO2 value within 1 minute of the Sao2 measurement. We calculated diagnostic test characteristics to examine detection of occult hypoxemia by race (SpO2 <92% as test for Sao2 <88%; 4% difference is consistent with prior studies1,2,3 and US Food and Drug Administration guidance5). We calculated standard metrics for assessing pulse oximetry accuracy: bias (SpO2 − Sao2) and accuracy root mean square (ARMS).5,6 We used multivariable linear regression to examine the association between race and bias while adjusting for clinical covariates (eMethods in Supplement 1). Statistical analyses were performed using R, version 4.1.2 (R Core Team).
Results
The study cohort included 774 patients (201 Black or African American [26.0%]; 51% female; 573 White [74.0%]; 43% female). Black or African American patients had a mean (SD) age of 6.6 (5.3) years. White patients had a mean (SD) age of 7.3 (5.3) years. The most common diagnoses in both groups included hypoplastic left heart syndrome/single ventricle, tetralogy of Fallot, and patent ductus arteriosus. The median (IQR) SpO2 value used in the analysis was 96% (90%-98%). Diagnostic test characteristics by race are shown in the Figure. Among patients with true hypoxemia (Sao2 <88%), 12% (7 of 57) of Black or African American patients vs 4% (4 of 110) of White patients had peripheral oxygen saturation levels suggesting normoxemia (SpO2 ≥92%) (false negatives). Conversely, among patients with peripheral oxygen saturation levels suggesting normoxemia (SpO2 ≥92%), 5% (7 of 139) of Black or African American patients vs 1% (4 of 407) of White patients had true hypoxemia (Sao2 <88%).
Figure. Scatterplots of Paired Pulse Oximetry (SpO2) and Arterial Blood Oxygen Saturation (SaO2) Observations for Black or African American Patients and White Patients.
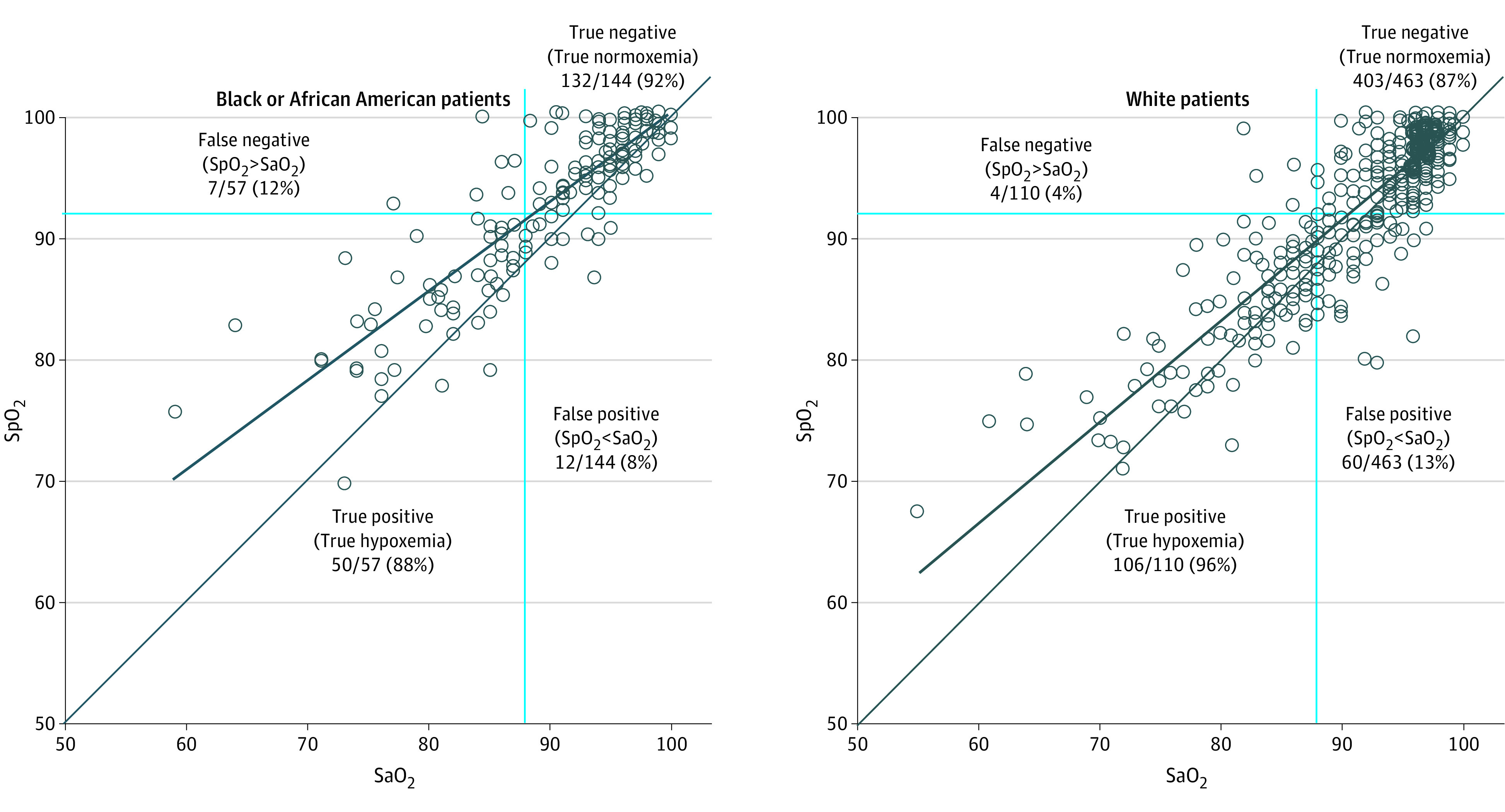
Black solid lines represent the line of equality and the trend line for the given set of paired data points. Blue solid lines denote the following quadrants: true positive includes patients whose paired SaO2 and SpO2 measurements both indicate hypoxemia (SpO2 <92% and SaO2 <88%). True negative includes patients whose SaO2 and SpO2 both indicate normoxemia. False positive includes patients whose SaO2 is normoxemic but whose SpO2 may suggest hypoxemia. False negative includes patients whose Sao2 is hypoxemic but whose SpO2 wrongly suggests normoxemia, placing the patient at risk of undertreatment (withholding supplemental O2).
The unadjusted bias for Black or African American patients was 2.58 (95% CI, 2.15-3.00) compared with 0.89 (95% CI, 0.64-1.15) for White patients (P < .001). Results adjusted for clinical covariates by categorized SpO2 range can be found in the Table.
Table. Bias and Accuracy Root Mean Square (ARMS) by Categorized Pulse Oximetry (SpO2) Rangea.
| Variable | Overall | SpO2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≥92% | 84%-91% | <84% | ||||||||||
| Black/African American | White | Between-group difference | Black/African American | White | Between-group difference | Black/African American | White | Between-group difference | Black/African American | White | Between-group difference | |
| No. | 201 | 573 | NA | 139 | 407 | NA | 44 | 117 | NA | 18 | 49 | NA |
| Adjusted bias (95% CI)b | 2.61 (2.19-3.04) | 0.88 (0.63-1.13) | 1.73 (1.24-2.22) | 2.46 (2.37-2.54) | 0.79 (0.74-0.85) | 1.66 (1.56-1.76) | 2.84 (2.65-3.04) | 1.07 (0.96-1.19) | 1.77 (1.54-2.00) | 2.88 (2.53-3.23) | 1.29 (1.08-1.50) | 1.59 (1.18-1.99) |
| ARMSc | 4.36 | 3.01 | NA | 3.60 | 2.55 | NA | 4.50 | 3.40 | NA | 7.93 | 5.00 | NA |
Abbreviations: NA, not applicable; SaO2, arterial blood oxygen saturation.
A multivariable linear regression model was used to model the association between race and bias, adjusting for patient characteristics (age, sex, blood pressure, temperature, hemoglobin, and medication use). Note: SpO2 was not included as a covariate in the regression model for bias. Predicted bias from the multivariable model was obtained for SpO2 categories.
Bias = SpO2 − SaO2.
 |
Discussion
Results of this cross-sectional study using data from a highly controlled clinical environment with tightly coupled Sao2 and SpO2 values suggest that pulse oximetry overestimated arterial oxygen saturation in children of Black or African American race.3 The discrepancy has been attributed to light absorption properties of melanin.5 Race is an imperfect proxy for skin pigmentation with the inherent assumption that Black or African American patients had darker skin and more melanin than White patients. Future studies in children should prospectively evaluate the association between SpO2 and SaO2 with reliable, direct measurement of skin pigmentation.
eMethods.
Data Sharing Statement
References
- 1.Sjoding MW, Dickson RP, Iwashyna TJ, Gay SE, Valley TS. Racial bias in pulse oximetry measurement. N Engl J Med. 2020;383(25):2477-2478. doi: 10.1056/NEJMc2029240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valbuena VSM, Seelye S, Sjoding MW, et al. Racial bias and reproducibility in pulse oximetry among medical and surgical inpatients in general care in the Veterans Health Administration 2013-2019: multicenter, retrospective cohort study. BMJ. 2022;378:e069775. doi: 10.1136/bmj-2021-069775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrist E, Nuppnau M, Barbaro RP, Valley TS, Sjoding MW. Association of race with pulse oximetry accuracy in hospitalized children. JAMA Netw Open. 2022;5(3):e224584-e224584. doi: 10.1001/jamanetworkopen.2022.4584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gottlieb ER, Ziegler J, Morley K, Rush B, Celi LA. Assessment of racial and ethnic differences in oxygen supplementation among patients in the intensive care unit. JAMA Intern Med. 2022;182(8):849-858. doi: 10.1001/jamainternmed.2022.2587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Food and Drug Administration . Pulse oximeter accuracy and limitations: FDA safety communication. Accessed August 30, 2022. https://www.fda.gov/medical-devices/safety-communications/pulse-oximeter-accuracy-and-limitations-fda-safety-communication
- 6.Batchelder PB, Raley DM. Maximizing the laboratory setting for testing devices and understanding statistical output in pulse oximetry. Anesth Analg. 2007;105(6)(suppl):S85-S94. doi: 10.1213/01.ane.0000268495.35207.ab [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
Data Sharing Statement


