Abstract
Background:
The primary objective of this paper was to examine perspectives and experiences of individuals with cognitive impairment who received an amyloid PET scan and their care partners, with regard to the process, logistics, and decision-making associated with receiving an amyloid PET scan and its results.
Methods:
Structured telephone interviews were conducted with 200 randomly sampled scan recipient/care partner dyads from the CARE IDEAS study. The audio-recorded, transcribed responses were analyzed using an inductive qualitative content analytic approach.
Results:
Participating individuals and care partners described their experiences in seeking a diagnosis for memory issues, including decision-making and logistics involved with receiving an amyloid PET scan. Participants discussed the factors contributing to their decision to seek a diagnosis for their memory issues and their hopes and expectations in completing the scan. Participants also described the trajectory of this process, and although some described relatively straightforward trajectories, others described problems associated with identifying appropriate providers and coordinating care across numerous providers to obtain a diagnosis for their memory issues. Participants described an additional challenge of physicians attributing cognitive decline to normal aging, rather than signs of a neurodegenerative disorder.
Conclusions:
Findings shed light on the barriers and delays that individuals and care partners experience in connecting with physicians and obtaining a comprehensive evaluation for cognitive problems. Results from this study have implications for physicians who provide care to older adults, and specifically highlight the need for greater care coordination and clearer communication with and systems of referral for patients.
Keywords: amyloid PET scan, Alzheimer’s disease and related dementias, diagnosis, care seeking
Introduction
Alzheimer’s disease and related dementias (ADRD) affect an estimated 11% of people 65 or older in the United States.1 Individuals with ADRD typically require significant health services, and particularly long-term services and supports, as the disease progresses. The gold standard diagnosis of Alzheimer’s disease (AD) is based on postmortem neuropathological examination. During life, the clinical diagnosis is based on examination of cognitive and functional decline, personality and behavioral changes, neurological signs, standard blood labs, and structural neuroimaging. Recent advances in AD biomarkers that measure beta-amyloid and tau levels via specialized positron emission tomography (PET) scans, cerebrospinal fluid, and peripheral blood have shown value in the differential diagnosis of cognitive impairment, especially for atypical AD clinical phenotypes.2 However, as amyloid PET scans are not typically covered by major insurers, including Medicare, they are generally not available as part of the routine dementia evaluation.
Given limited therapeutic options, early detection and diagnosis of ADRD is considered critical to planning for the future.2 Early diagnosis also allows for greater inclusion in clinical trials designed to develop efficacious treatments for AD. Despite the importance of a timely diagnosis of AD, limited research has examined individuals’ and caregivers’ experiences in seeking a diagnosis and related treatment. Existing research has found that the diagnosis of AD is typically delayed for reasons including: lack of individual seeking a diagnosis and caregiver knowledge about dementia,3–7 failure of the individual, their family, and physicians to identify that symptoms are outside the range of normal aging,8,9 attributing symptoms to other comorbidities,10,11 challenges accessing physicians,12,13 and slow systems of referral to appropriate specialists.6,14 Further, most people with dementia are never seen by a dementia care specialist (only 36 percent after five years of diagnosis), and 85 percent are diagnosed by a non-dementia specialist, typically their primary care provider.6,15
While quantitative methods have been used in prior research to identify how long a diagnosis may take and how many providers are ultimately involved in the diagnostic process, very little research has taken a qualitative approach to examine and describe the experiences of persons with ADRD and their caregivers. Early research in this area conducted with caregivers found that persons with ADRD encountered delays in receiving a diagnosis; obtaining a diagnosis often took multiple years, visits to numerous providers, required persistence, and resulted in dissatisfaction with providers and with the diagnosis disclosure.16 More recent work tends to include both individuals with ADRD and caregivers. One such study of people with mild cognitive impairment (MCI) and care partners highlighted individuals’ need for information and a diagnosis, but also reported the anxiety and fear associated with receiving that diagnosis.17 Another study of people with dementia and caregivers found that although individuals were satisfied with their primary care providers, they were dissatisfied with access to other providers and services.18 Similarly, a study of people with fronto-temporal dementia found that patients and caregivers faced challenging trajectories to receiving a diagnosis, and were satisfied with the physicians who provided the ultimate diagnosis; however, they reported these physicians had limited awareness of available services in the community for follow-up and referral.19
These challenges highlight the value of research that seeks to understand individual and family member experiences in seeking a diagnosis for cognitive problems and receiving amyloid PET scan results. Although previous research highlighted above demonstrates difficulties with regard to obtaining a dementia diagnosis, much of this research is limited to small sample sizes within specific locations, and often outside the United States. The purpose of the present study is to examine open-ended responses to questions from a large sample of Medicare beneficiaries and their care partners from across the United States to describe experiences accessing and receiving an amyloid PET scan along the diagnostic pathway for memory issues. Results have the potential to inform improvements in care delivery for individuals with cognitive impairment.
Methods
Study Sample
The study sample was drawn from the Imaging Dementia-Evidence for Amyloid Scanning (IDEAS) study. IDEAS is a cohort study that examined the impact of amyloid PET scans on clinical management and outcomes for Medicare beneficiaries with dementia or MCI. This paper uses data from CARE-IDEAS, a supplemental study associated with IDEAS. CARE-IDEAS recruited a subset of IDEAS participants and their care partners who indicated they were willing to participate in this additional study. Those who indicated willingness were contacted by mail, with a letter that explained the study, informed the individual that they would be contacted by a survey research firm, and requested that they share the information with their care partner. Only individuals who identified a care partner were included. Of the 3,717 participants of the IDEAS study who agreed to be contacted, 2,228 scan recipients and 1,872 of their care partners individually participated in the 30 to 45-minute structured telephone surveys. Of these, a subset of 1,013 scan recipients and 794 care partners were asked open-ended questions and had their answers audio recorded. Participants in the current analyses were drawn from this group, as described below. The median time between recipients’ amyloid PET scans, conducted as part of the IDEAS study, and the CARE-IDEAS survey was 4.5 months. This paper used data from the CARE-IDEAS surveys and the original scan results from the IDEAS study.
Measures
Structured telephone survey questionnaires were administered to scan recipients and care partners separately. Scan recipient surveys included validated measures of cognition, wellbeing, and socio-demographics, and close-ended questions about healthcare decision-making and planning for the future (estate planning, long-term care planning, advance care planning), among other topics. The survey also included four open-ended questions prompting scan recipients to share their experiences in seeking a diagnosis for memory problems, how they interpret the results of the scan, how the results impact their future planning, and what they had hoped to achieve in having the scan. Care partner surveys included the same items that were in the scan recipient surveys, as well as an additional open-ended question that asked how the care partner became aware of the scan recipient’s memory impairment. Open-ended questions from the survey protocols are included in Supplementary Text S1. Of note, although participants were recruited into the IDEAS study to receive an amyloid PET scan, the open-ended questions asked about their experiences with regard to both the scan and seeking a diagnosis for memory problems, and participants tended to discuss these concepts somewhat interchangeably. This study was approved by the [Brown University] Institutional Review Board (#1606001534).
Data Collection and Analysis
Of the 1,013 scan recipients and 794 care partners who were asked the open-ended questions, responses from subsequent random samples (using a random number generator) of 50 recipient/care partner dyads were transcribed for analysis. These transcripts were initially analyzed by two authors (EB, TW) using a content analysis approach,20 and differences in coding were discussed until consensus was reached. The two coders agreed after analyzing 200 dyads that saturation had been reached and no relevant new information was present.21 Following this analysis, the two coders met with the larger research team to discuss preliminary themes and patterns in the data. With these potential themes in mind, the first author re-analyzed the qualitative data focusing on reported experiences and decision-making in seeking and receiving an amyloid PET scan. Thus, the analytic approach included both a priori codes based on the interview guides, as well as de novo codes that emerged from the data. NVivo 12 (QSR International Pty Ltd., Melbourne, Australia) was used to facilitate data analysis.
Results
Table 1 presents the characteristics describing the random sample of 200 dyads analyzed in this study. As is the case for the larger CARE IDEAS study,22 this sample of scan recipients was primarily male, while the care partners were primarily female. Scan recipients and care partners were almost entirely white, non-Hispanic, and married, and were highly educated. About three-quarters of the scan recipients had MCI, while one-quarter had dementia at the time they had the scan. Two-thirds of the sample of scan recipients had an elevated level of amyloid plaques, which indicates a high probability that their cognitive impairment was due to AD.
Table 1.
Descriptive Characteristics of Respondents to Open-Ended Survey Questions, N (%)
| Qualitative Sample | CARE Survey Sample | |||
|---|---|---|---|---|
| Scan Recipients N=196 | Care Partners N=196 | Scan Recipients N= 2,228 | Care Partners N= 1,872 | |
| Age | ||||
| Below 65 | 0 | 30 (15.3) | 0 | 358 (19.1) |
| 65–74 | 102 (52.0) | 93 (47.4) | 1,173 (52.7) | 870 (46.5) |
| 75+ | 92 (46.9) | 73 (37.2) | 1,047 (47.0) | 633 (33.8) |
| Gender | ||||
| Male | 121 (61.7) | 62 (31.7) | 1,283 (57.6) | 599 (32.0) |
| Female | 75 (38.3) | 134 (68.4) | 945 (42.4) | 1,273 (68.0) |
| Race/Ethnicity * | ||||
| White, Non-Hispanic | 187 (95.4) | 186 (94.9) | 2,055 (92.2) | 1,749 (93.4) |
| Marital status | ||||
| Married / Domestic Partner | 181 (92.4) | 186 (94.4) | 1,925 (86.4) | 1,773 (94.7) |
| Education | ||||
| High School or Less | 33 (16.8) | 29 (14.8) | 356 (16.0) | 264 (14.1) |
| Some College | 47 (24.0) | 55 (28.1) | 570 (25.6) | 521 (27.8) |
| College Degree | 44 (22.5) | 44 (22.5) | 500 (22.4) | 511 (27.3) |
| Post-secondary | 69 (35.2) | 68 (34.7) | 780 (35.0) | 564 (30.1) |
| Level of Impairment | ||||
| MCI | 148 (75.5) | N/A | 1,660 (74.5) | N/A |
| Dementia | 48 (24.5) | N/A | 568 (25.5) | N/A |
| Amyloid PET Scan Results | ||||
| Elevated Amyloid | 133 (67.9) | N/A | 1,461 (65.6) | N/A |
| Not Elevated Amyloid | 62 (31.6) | N/A | 759 (34.1) | N/A |
Percentages have some missing values and may not add to 100%.
Note: There are 196 complete recipient/care partner dyads, as there was some missing data.
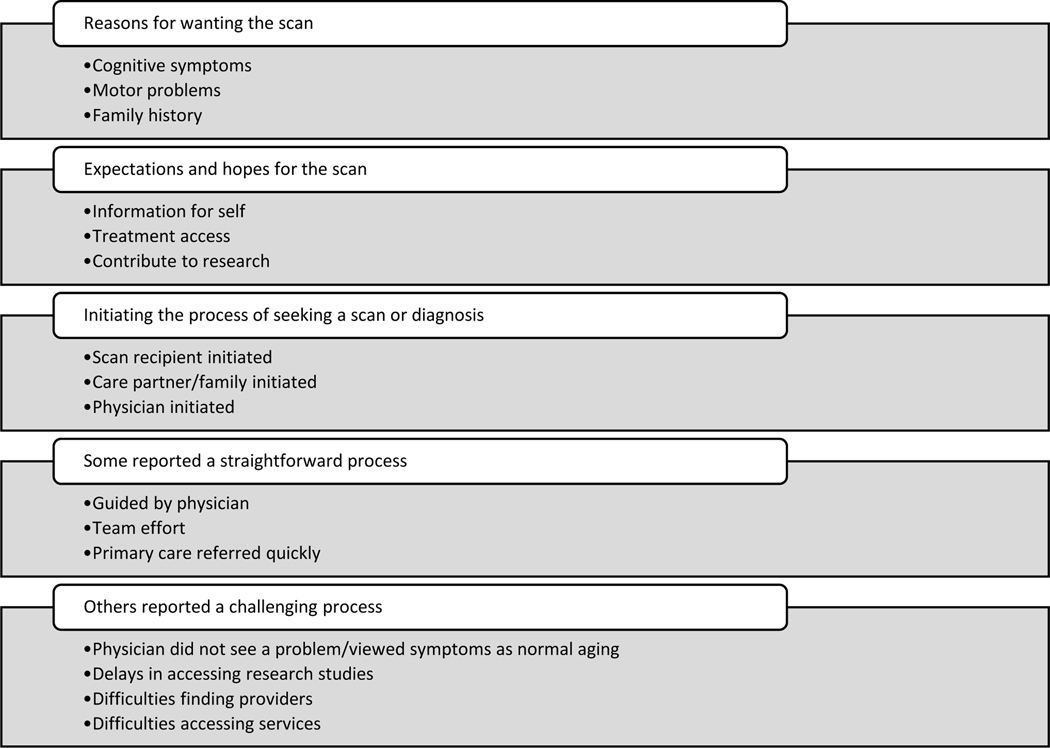
Survey respondents described their experiences getting an amyloid PET scan, including their hopes and expectations for what the scan results would mean and the steps it took to receive the scan. See Figure 1 for a visual representation of these findings. These themes and example quotes reflect content that was recurrent in the data, and are presented below.
Figure 1.
Themes Identified from Scan Recipient and Care Partner Responses
Rationale and Expectations for Receiving an Amyloid PET Scan
Amyloid PET scan recipients and care partners described their decision-making around seeking and receiving an amyloid PET scan and the potential diagnosis for memory problems. Reasons for wanting the scan or seeking care most commonly included concerns about cognitive symptoms, motor problems, and/or a family history of Alzheimer’s disease. These reasons are exemplified by one scan recipient, who said:
On my mother’s side there’s a history of Alzheimer’s. So based on that and based on my knowledge of myself, the last two or three years I realized that I was, you know, kind of forgetting things, and so I talked to my family doctor about it and he mentioned at the [University] they have a neurology center that I could do tests, to determine if there is an early onset of Alzheimer’s. (scan recipient, elevated amyloid, MCI)
Participants expressed their hopes that the scan would provide information about their symptoms and treatment access for themselves, and would also benefit others by contributing to research. Participants, such as this care partner, also hoped the scan would remove the “constant uncertainty” associated with not having a diagnosis:
The doctor had discussed with us whether we thought it would be helpful if there were a medical procedure or test that would say definitely whether he had Alzheimer’s disease or did not, and we both thought that that would be an excellent idea to have this knowledge….I think that the definitive diagnosis, it’s nothing but helpful. I mean, it’s taken away the constant uncertainty about what it is…that’s affecting my husband. So we now at least have something to call it and something to look up and study more about. (care partner, elevated amyloid, MCI)
Others expressed that they hoped a scan would help them “find answers” (care partner, elevated amyloid, MCI) that would enable them to make decisions, and also “even if it didn’t…give us any answers, that maybe for someone else in the future it would.” (care partner, not elevated amyloid, dementia) Representative quotes, such as these, are presented in Table 2.
Table 2.
Rationale and Expectations for Receiving an Amyloid PET Scan
| Representative Quotes (participant type, result of scan, impairment level) |
|---|
| Reasons for Wanting the Scan or Diagnosis |
| Cognitive symptoms, family history: “She initiated the contact with the doctor because she was concerned about her memory. Partially, and probably the major portion of it was because of her experience with her sister’s Alzheimer’s.” (care partner, elevated amyloid, dementia) |
| Motor problems, family history: “I go to an internist also. First, I went and he sent me to the neurologist because I kept falling…I was dropping things a lot…And so he sent me to the neurologist…and he’s had to do a lot of different testing…And then mom died this year, and my uncle also got Alzheimer’s. Yeah, so they were thinking that it’s in the family maybe.” (scan recipient, not elevated amyloid, MCI) |
| Cognitive symptoms: “I was having serious problems with, in particular the thing that was most obvious was proper nouns, names. I simply didn’t know anybody’s name. I can’t remember the names of many members of my family who were close enough that it shocks people that I don’t remember them…I was then, referring to them by categories. My mother’s brother said, because mother and brother are words that I have lots and lots of threads running through in my brain, whereas Uncle [Name], I don’t have an Uncle [Name]. You know it’s one thread to one person and I was very aware of that.” (scan recipient, elevated amyloid, dementia) |
| Expectations and Hopes for the Scan |
| Information for self: “I was glad that he was doing something about it to find answers. And sometimes he’s reluctant to participate or go to an appointment, but I remind him, I said ‘by not going doesn’t change anything, it gives information and you and I will both be better prepared for what’s going to happen’” (care partner, elevated amyloid, MCI) |
| Treatment access: “When I heard of the study [IDEAS], I had my mind set that because if I had the neurological, psychological tests for two years in a row and I saw that my results were getting worse with that, I had in my mindset that I was going to fight this.” (scan recipient, elevated amyloid, MCI) |
| Treatment access: “But that’s why we had the PET scan to rule out that it was Alzheimer’s because there would have been a chance of him having some medication that could have slowed down the process. And without the amyloids he was much more convinced that it was frontotemporal lobe.” (care partner, not elevated amyloid, MCI) |
| Information for self, contribute to research: “We just thought that, you know, there’s the opportunity to have some direction or understanding of what’s happening, why wouldn’t we purchase it? And even if it didn’t do any…give us any answers, that maybe for someone else in the future it would.” (care partner, not elevated amyloid, dementia) |
| Information for self, contribute to research: “The doctor thought that my husband would be a very good candidate because at that point the neurologist didn’t know whether or not he had Alzheimer’s. My husband was very willing to do it. We’re both educators and we believe in education and research and trying to really understand things and do the right thing. [We] just think that’s best not only for us individually but for us as a family and for others, even people that we don’t know.” (care partner, not elevated amyloid, MCI) |
Experiences Throughout the Process of Seeking a Scan and Diagnosis
Scan recipients and their care partners described differing trajectories in their efforts to receive the scan and obtain a diagnosis. Participants discussed who first noticed symptoms and initiated the process of seeking a diagnosis, including the scan recipient, care partners or family members, and physicians. This care partner described a process initiated by their neurologist:
We happened to have a neurologist who is a very, very sharp MD. And after two visits with him, he ordered the scan done and then he followed up with getting us the results. And I just feel fortunate that we have such a talented physician, that he is in tune with the potential for folks as we age. (care partner, not elevated amyloid, MCI)
Like this care partner, some interview participants described a straightforward process, in which the scan recipient, a family member, or their doctor became aware of the scan recipient’s symptoms, and their doctors connected them with the appropriate specialists. Such interview participants noted that they “had a good doctor that guided me through it,” (scan recipient, not elevated amyloid, MCI) and “it was not difficult. I talked to my primary care physician about having, being aware of short term memory loss and he connected to the doctor very quickly.” (scan recipient, elevated amyloid, MCI)
Others described more difficult processes that sometimes included the challenge of convincing doctors that their symptoms were different from normal aging; it frequently took working with multiple doctors to obtain answers. One such care partner described attempting to convince a primary care provider:
For the past two years I’ve been talking to his primary care doctor and insisting that I had seen a lot of changes and he didn’t agree with me. He just thought it was normal aging and I wanted to pursue that because I thought it was much more than just normal aging. (care partner, not elevated amyloid, MCI)
These participants expressed that “it took a long time to find a doctor that actually believed her,” (care partner, elevated amyloid, MCI) and that primary care physicians “need to be more aware” (care partner, elevated amyloid, MCI) of dementia, its diagnosis, and follow-up options. Other interview participants commented that they experienced logistical challenges associated with finding appropriate specialists. This care partner described their experience:
It was just time-consuming, because we did a lot of digging…We wanted to find the best neurologist we could find, and we did a lot of inquiring from people who would know…Our family doctor…I don’t go to him anymore…Just felt ho-hum…Maybe this was just everybody had memory loss as they got older, and if it was more than just normal memory loss, there was nothing we could do about it anyway. So we just on our own tried to find the best neurologist that we could find. And then asked the family doctor to please give us a referral to him, and we had to wait at least four months to get in to see him. So that was probably the most difficult part of finding someone to help. (care partner, elevated amyloid, MCI)
Such participants said the process required “perseverance,” (care partner, not elevated amyloid, MCI) and “the whole way, it was a fight.” (care partner, elevated amyloid, dementia) Representative quotes of these experiences are listed in Table 3. Implications of these results are discussed below.
Table 3.
Experiences Throughout the Process of Seeking a Scan and Diagnosis
| Representative Quotes (participant type, result of scan, impairment level) |
|---|
| Initiating the Process of Seeking a Scan or Diagnosis |
| Scan recipient, physician initiated: “I had been starting to not remember stuff and it bothered me, and so, when I went in for a physical, I mentioned it to my doctor and he set an appointment up with the doc that I go to now for the Alzheimer’s, and he sent me for a PET scan and he is now treating me.” (scan recipient, elevated amyloid, MCI) |
| Physician initiated: “I had an interview with my doctor about another ailment I had and I told her that I couldn’t remember some things she told me earlier in the discussion. This caused her to be concerned, because I’m not normally at that disposition. So she arranged for me to go on to a Memory Clinic.” (scan recipient, elevated amyloid, MCI) |
| Care partner initiated: “I knew that I was having memory problems, but I kept telling myself, and all my friends were telling me, ‘Oh, that’s normal. Everyone has it.’ My husband was the one who said, ‘I think you should ask the doctor if they could see if there’s anything wrong here,’ and so I did.” (scan recipient, elevated amyloid, MCI) |
| Family initiated: “She would forget to lock the door when she was leaving the house, and I would tell her something and then she would ask a question and I’d tell her, and then that would come up again. The girls, our two daughters, noticed it more than I did because we’re together, and I thought, well, she just, you know, it’s her age and that sort of thing, but the girls kept pushing…We talked to our regular doctor and he said, ‘Well, let’s send you to a neurologist,’ and it was the neurologist who did some tests on her.” (care partner, elevated amyloid, MCI) |
| Straightforward Process |
| Guided by doctor: “It wasn’t really difficult because I had a good doctor that guided me through it.” (scan recipient, not elevated amyloid, MCI) |
| Team effort: “I don’t think it was difficult to get the diagnosis. It was difficult to get a good doctor. But once he got to Dr. [Name], a neurologist, after that, things got better because she was knowledgeable, educated, caring of her patients. So, then we pretty much had her make those decisions. We felt that she really cared personally for [Scan Recipient] and was thinking about what to do for him as we were too. So it was kind of a team effort, all three of us.” (care partner, not elevated amyloid, MCI) |
| Primary care referred quickly: “It certainly was not difficult to get the diagnosis. I talked to my family doctor about my concern of what I thought was the short term memory loss and he and his office made an appointment for me to go to a specialist.” (scan recipient, not elevated amyloid, MCI) |
| Challenging Process |
| Physician did not believe problem: “It took a long time to find a doctor that actually believed her or believed this was enough of a problem to kind of pursue it.” (care partner, elevated amyloid, MCI) |
| Physician did not pick up on problem: “I don’t think family physicians pick it up right away. I think they need to be more aware of things like this. That slowed us down a lot in the beginning.” (care partner, elevated amyloid, MCI) |
| Physician thought normal aging: “Well, I feel as though I wasted a year because our primary physician sent us to a neurologist in the group that she practices in. And he after doing some paper testing and talking to [Scan Recipient], who is very, very high functioning, was very high functioning, said ‘oh, it’s nothing. It’s just that you’re retiring and it’s a change of life,’ and so on and so forth. And then we went back and saw someone else in that office, his assistant and the same thing twice. And meanwhile I noticed negative changes, and I called a friend of mine who is a neurologist…and asked for a recommendation. And she sent us to where we are now at the [City] Neurology Center, which is part of the [Hospital]. And the difference was day and night, as to the questions they asked, the way they went about it. So I don’t know that it would’ve made any difference one way or the other but I felt that the year with the other neurologist was a total waste. And I told my primary physician.” (care partner, elevated amyloid, dementia) |
| Delays in accessing research studies: “It was somewhat difficult to … it took us right at a year to even get to the point that we could get into a study. Of course, that caused anxiety on my part because I felt that everything I had read, they said that working on something and getting [Scan Recipient] on medication, the more possibility of it stabilizing and not progressing so quickly.” (care partner, elevated amyloid, MCI) |
| Difficulties finding providers: “Well, it took some perseverance. We went to our primary care first, several times…He suggested that we find a neuropsychologist and that was probably the hardest part, trying to figure out where the heck to go. And so we found out through a friend, of a doctor who was doing research on Parkinson’s…and that he had recently switched to early-onset Alzheimer’s research….But finding a person to help you out is the hardest part.” (care partner, not elevated amyloid, MCI) |
| Difficulties accessing services: “I had to fight with the VA [Veteran’s Affairs] to get even the neurologist makeup done on him… The whole way, it was a fight. My dermatologist is the one that said, ‘Get him in the neurology section there.’ I must’ve called 15 different numbers…He [Scan Recipient] actually was put on the drugs I think too late. He went to the VA and the VA then said after doing testing, like four hours worth of neurology testing and an MRI, they said early Alzheimer’s. Yet the neurologist there said, ‘Oh, he’s fine. I don’t need to see him anymore.’ We missed probably two years of treatment. This has meant everything to us.” (care partner, elevated amyloid, dementia) |
Discussion
Amyloid PET scan recipients and their care partners described their experiences in seeking a diagnosis and receiving an amyloid PET scan as part of the IDEAS research study. These experiences included how the decision to seek a diagnosis came about and what the process and associated logistics involved. In describing these trajectories, participants discussed which factors contributed to their decision and what the recipient and care partners hoped to achieve by completing the scan. Participant discussion of the process and logistics varied, with some describing relatively straightforward trajectories and others describing considerable difficulties engaging with providers, as well as their problems associated with identifying appropriate providers, and their challenges coordinating care across numerous providers.
These findings align with and extend prior literature. Consistent with existing research, we found delays and challenges in connecting with physicians who were dementia specialists,6,12–14 as well as the difficulty that individuals seeking care, care partners, and physicians have in distinguishing between cognitive decline that is part of normal aging versus a neurodegenerative disorder.8,9,23 We also found that these challenges are associated with negative experiences overall, including the perspective of “the whole way, it was a fight,” (care partner, elevated amyloid, dementia) as one care partner described the frustration. Some participants described the process of seeking a diagnosis as one that took years of perseverance and hard work. Our findings offer a broader perspective than those of prior research, as we benefitted from a large sample size that includes both amyloid PET scan recipients and their care partners.
Some participants described whether and how the amyloid PET scan results met their expectations. This was largely in the context of their hopes for the scan, and many viewed receiving the results as a favorable outcome, regardless of the result or of their difficulty in accessing the scan. Generally, more information was described as helpful. However, participants also expressed negative aspects of seeking and receiving the scan, including challenges in convincing providers that symptoms were outside of “normal aging,” as well as in accessing follow-up care. These results may have implications for providers, and highlight the value of engaging with patients and care partners actively in seeking diagnoses. This recommendation is consistent with those provided by a workgroup of dementia experts (particularly clinical neurologists) for communicating MCI diagnoses with patients and families.23 Explicitly, the workgroup called for research like ours, which sought to understand logistics of amyloid PET scan and results receipt, learning directly from the patients and care partners.
The issues identified by interview participants raise several implications for practice. First, findings suggest a need for greater care coordination. Although some discussed a straightforward process of care seeking, others described long wait times to see physicians they were referred to, that they had a hard time “trying to figure out where the heck to go,” (care partner, not elevated amyloid, MCI) and being sent back and forth between doctors. Of note, participants who reported difficulties or long wait times were almost exclusively care partners, and not the scan recipients themselves. Future research into this question is needed, but this finding may be due in part to the role of cognitive impairment in participants’ abilities to recount a more long-term, negative experience. Findings also highlight the need for improved dementia training and education about screening for pathological cognitive decline for primary care providers. Some participants expressed that while they started their search for a diagnosis with their primary care provider, their doctors tended to minimize their symptoms and assess their memory loss as a normal part of aging. One care partner in particular suggested: “I don’t think family physicians pick it up right away. I think they need to be more aware of things like this. That slowed us down a lot in the beginning.” (care partner, elevated amyloid, MCI) Further, there may be a need for targeted training of providers in primary and family care practices regarding the value that persons with dementia and their care partners place on a diagnosis.
This research has a few limitations. First, although the sample size is relatively large for a qualitative study, findings are not intended to be generalizable. Our findings provide depth of understanding about the perspectives of a selected sample who participated in the IDEAS study. Of note, our sample, similar to the overall IDEAS sample, consists of primarily white, highly educated, Medicare beneficiaries. An additional limitation is that, because the sample includes amyloid PET scan recipients with MCI or some form of cognitive impairment, the reported findings may skew towards representing those who were less impaired and better able to comment on and discuss their experiences. However, since it is less likely that individuals with advanced dementia would get an amyloid PET scan as part of the traditional diagnostic trajectory, our sample likely includes those for whom a scan may be most indicated in practice. Also, because our sample is derived from those who received an amyloid PET scan as part of a research study, we were unable to include perspectives from those who were not referred for the scan, and who may have more challenging and negative experiences to share. It is important to note that there are substantial barriers to timely referral to research studies and services.3–14
Despite these limitations, this study gathered perspectives and experiences from individuals who, due to their cognitive status, are often excluded from qualitative research that is relevant to their interests and outcomes. These participants help fill in an important gap in our knowledge of how individuals at the early stages of dementia and memory loss experience their situation. As some participants discussed, the ability to contribute to research that may aid others in the future was part of their motivation to even complete an amyloid PET scan.
This study presents the experiences of a sample of Medicare beneficiaries who received amyloid PET scans and their care partners with regard to seeking a diagnosis for cognitive problems and the receipt of the amyloid PET scan. Participants described their motivation for seeking a scan, and discussed in detail the process that led to their obtaining a diagnosis. Although some reported a straightforward process, many described challenges that led to delays in a diagnosis and the ability to plan for the future, which may have had significant effects on ultimate outcomes. These findings indicate how providers, patients, and care partners may benefit from improved processes for seeking answers for their cognitive symptoms and more easily obtain a diagnosis for their condition.
Supplementary Material
Supplementary Text S1: Open-ended questions asked of amyloid PET scan recipients and care partners
Key Points:
Amyloid PET scan recipients and their care partners describe their motivations for seeking a diagnosis for memory issues, as well as their experiences during and the logistics of this process.
While some report straightforward trajectories in receiving a diagnosis, others describe challenging experiences characterized by problems associated with identifying appropriate providers and coordinating care across numerous providers to obtain a diagnosis for their memory issues.
Participants described an additional challenge of physicians attributing cognitive decline to normal aging or to other causes, rather than signs of a neurodegenerative disorder.
Why does this matter?
Results highlight the need for greater care coordination and clearer communication with and systems of referral for patients.
Acknowledgements
Funding source:
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under award number R01AG053934 and by the American College of Radiology Imaging Network and the Alzheimer’s Association. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the American College of Radiology Imaging, or the Alzheimer’s Association.
Sponsor’s Role:
The sponsor had no role in the design, methods, subject recruitment, data collections, analysis, or preparation of the paper.
Footnotes
Conflict of Interest: The authors have no conflicts.
Data Accessibility:
Data are accessible on the Brown Digital Repository (https://doi.org/10.26300/74bs-dw33) which includes a CARE-IDEAS codebook.
References
- 1.Hudomiet P, Hurd M, Rohwedder S. Dementia prevalence in the United States in 2000 and 2012: Estimates based on a nationally representative study. J Gerontol B Psychol Sci Soc Sci 2018;73(Suppl 1)S10–S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.How Is Alzheimer’s Disease Diagnosed? National Institute on Aging (online). Available at: https://www.nia.nih.gov/health/how-alzheimers-disease-diagnosed. Accessed December 3, 2021. [Google Scholar]
- 3.Juarez-Cedillo T, Jarillo-Soto EC, Rosas-Carrasco O. Social Representation of Dementia and Its Influence on the Search for Early Care by Family Member Caregivers. Am J Alzheimers Dis Other Demen 2014;29(4):344–353. doi: 10.1177/1533317513517041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koehn S, McCleary L, Garcia L, Spence M, Jarvis P, Drummond N. Understanding Chinese-Canadian pathways to a diagnosis of dementia through a critical-constructionist lens. J Aging Stud 2012;26(1):44–54. doi: 10.1016/j.jaging.2011.07.002. [DOI] [Google Scholar]
- 5.Prorok JC, Horgan S, Seitz DP. Health care experiences of people with dementia and their caregivers: a meta-ethnographic analysis of qualitative studies. CMAJ 2013;185(14):E669–E680. doi: 10.1503/cmaj.121795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teel CS, Carson P. Family Experiences in the Journey Through Dementia Diagnosis and Care. J Fam Nurs 2003;9(1):38–58. doi: 10.1177/1074840702239490. [DOI] [Google Scholar]
- 7.Willis R, Zaidi A, Balouch S, Farina N. Experiences of People With Dementia in Pakistan: Help-Seeking, Understanding, Stigma, and Religion. Gerontologist 2020;60(1):145–154. doi: 10.1093/geront/gny143. [DOI] [PubMed] [Google Scholar]
- 8.Chrisp TA, Tabberer S, Thomas BD, Goddard WA. Dementia early diagnosis: triggers, supports and constraints affecting the decision to engage with the health care system. Aging Ment Health 2012;16(5):559–565. doi: 10.1080/13607863.2011.651794. [DOI] [PubMed] [Google Scholar]
- 9.Mukadam N, Cooper C, Livingston G. A systematic review of ethnicity and pathways to care in dementia. Int J Geriatr Psychiatry 2011;26(1):12–20. doi: 10.1002/gps.2484. [DOI] [PubMed] [Google Scholar]
- 10.McCleary L, Persaud M, Hum S, et al. Pathways to dementia diagnosis among South Asian Canadians. Dementia (London) 2013;12(6):769–789. doi: 10.1177/1471301212444806. [DOI] [PubMed] [Google Scholar]
- 11.Leung KK, Finlay J, Silvius JL, et al. Pathways to diagnosis: exploring the experiences of problem recognition and obtaining a dementia diagnosis among Anglo-Canadians. Health Soc Care Community 2011;19(4):372–381. doi: 10.1111/j.1365-2524.2010.00982.x. [DOI] [PubMed] [Google Scholar]
- 12.Clark PC, Kutner NG, Goldstein FC, et al. Impediments to timely diagnosis of Alzheimer’s disease in African Americans. J Am Geriatr Soc 2005;53(11):2012–2017. doi: 10.1111/j.1532-5415.2005.53569.x. [DOI] [PubMed] [Google Scholar]
- 13.Connell CM, Roberts JS, McLaughlin SJ, Carpenter BD. Black and white adult family members’ attitudes toward a dementia diagnosis. J Am Geriatr Soc 2009;57(9):1562–1568. doi: 10.1111/j.1532-5415.2009.02395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilkinson D, Stave C, Keohane D, Vincenzino O. The role of general practitioners in the diagnosis and treatment of Alzheimer’s disease: a multinational survey. J Int Med Res 2004;32(2):149–159. doi: 10.1177/147323000403200207. [DOI] [PubMed] [Google Scholar]
- 15.Drabo EF, Barthold D, Joyce G, Ferido P, Chang Chui H, Zissimopoulos J. Longitudinal analysis of dementia diagnosis and specialty care among racially diverse Medicare beneficiaries. Alzheimers Dement 2019;15(11):1402–1411. doi: 10.1016/j.jalz.2019.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinton L, Franz C, Friend J. Pathways to dementia diagnosis: evidence for cross-ethnic differences. Alzheimer Dis Assoc Disord 2004;18(3):134–144. doi: 10.1097/01.wad.0000127444.23312.ff. [DOI] [PubMed] [Google Scholar]
- 17.Morris JL, Hu L, Hunsaker A, Liptak A, Seaman JB, Lingler JH. Patients’ and Family Members’ Subjective Experiences of a Diagnostic Evaluation of Mild Cognitive Impairment. J Patient Exp 2020;7(1):124–131. doi: 10.1177/2374373518818204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khanassov V, Rojas-Rozo L, Sourial R, Yang XQ, Vedel I. Needs of patients with dementia and their caregivers in primary care: lessons learned from the Alzheimer plan of Quebec. BMC Fam Pract 2021;22(1):186. Published 2021 Sep 15. doi: 10.1186/s12875-021-01528-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Besser LM, Galvin JE. Diagnostic experience reported by caregivers of patients with frontotemporal degeneration. Neurol Clin Pract 2020;10(4):298–306. doi: 10.1212/CPJ.0000000000000738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 21.Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018;52(4):1893–1907. doi: 10.1007/s11135-017-0574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.James HJ, Van Houtven CH, Lippmann S, et al. How Accurately Do Patients and Their Care Partners Report Results of Amyloid-β PET Scans for Alzheimer’s Disease Assessment?. J Alzheimers Dis 2020;74(2):625–636. doi: 10.3233/JAD-190922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Miranda LFJR Matoso RO, Rodrigues MV, et al. Factors influencing possible delay in the diagnosis of Alzheimer’s disease: Findings from a tertiary Public University Hospital. Dement Neuropsychol 2011;5(4):328–331. doi: 10.1590/S1980-57642011DN05040011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grill JD, Apostolova LG, Bullain S, et al. Communicating mild cognitive impairment diagnoses with and without amyloid imaging. Alzheimers Res Ther 2017;9(35). doi: 10.1186/s13195-017-0261-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Text S1: Open-ended questions asked of amyloid PET scan recipients and care partners
Data Availability Statement
Data are accessible on the Brown Digital Repository (https://doi.org/10.26300/74bs-dw33) which includes a CARE-IDEAS codebook.