Abstract
Objective: In a secondary prevention of coronary artery disease (CAD), nutritional management is an integral part of lifestyle optimisation. However, few studies have investigated the potential of remote nutritional follow-up using digital solutions. This study investigates the effectiveness of a smartphone application for nutrition education and feedback with pictures of meals by a dietitian for patients with CAD. Methods: Sixty participants with CAD were randomised to either a TeleDiet group or a control group. Participants in the TeleDiet group participated in dietary education using a messaging application. The primary outcome was the change of the Mediterranean diet score (MedDietScore). The Nutrition-Score, a modification of the MedDietScore, blood tests (blood lipids, blood glucose and kidney function), body mass index, self-efficacy, medication adherence and health-related quality of life during the observation period were analysed as secondary outcomes. Results: Sixty participants participated in the study. The difference in the MedDietScore in the TeleDiet group was greater than in the control group, but not significant (2.0 [−1.0, 4.0] vs. 0.0 [−3.0, 1.5], p = 0.066). The difference in the Nutrition-Score in the TeleDiet group was significantly greater than in the control group (3.0 [1.0, 3.5] vs. 0.0 [−3.0, 2.0], p = 0.029). Nutrition knowledge of the TeleDiet group improved significantly compared to the control group (1.9 ± 1.7 vs. 0.8 ± 2.1, p = 0.048). Conclusions: A feedback system using a simple messaging application that allows patients with CAD to simply send a picture of their food has a positive effect on nutrition knowledge. It could be a hint for the implementation of the Mediterranean diet.
Keywords: Dietary follow-up, nutrition, secondary prevention, coronary artery disease, telerehabilitation, MedDietScore
Introduction
The European Society of Cariology (ESC) Guidelines published in 20211 indicate that patients considered at high cardiovascular disease (CVD) risk are often inadequately treated for atherosclerotic CVD risk factors and that prevention of recurrent CVD, including coronary artery disease (CAD), is important. One of the leading methods of CVD prevention is cardiac rehabilitation (CR), which consists of several components. Nutrition management is one essential component of lifestyle optimisation to correct coronary risk factors and prevent rehospitalization.1,2 Recent digital health solutions have great potential for application in the field of nutrition. A past randomised controlled trial (RCT) includes the ‘TEXT ME’ trial published from Australia in 2015,3 which showed improvements in several CVD risk factors. Subsequent mobile health (mHealth) trials using text messaging have also shown improvements in CVD risk factors.4–6 MHealth means can be defined as the use of wireless technology to deliver health services and information in mobile communication devices such as mobile phones, tablet computers, monitoring devices, smartphones, etc.7 Advances in mHealth technology have led to the development of several smartphone applications. In previous studies,8,9 in addition to dietary education, counselling and feedback from nurses, physicians and dietitians, patients with CVD risk (e.g. obesity, smoking, hypertension, type 2 diabetes), were asked to record their diet on an application to improve their diet. However, few studies have reported the effectiveness of using a smartphone application to send photos of meals and communicate directly with a dietitian for patients with CVD, such as CAD. One of the common patient-level barriers of digital health technology is the difficulty of using the technology.10 As described in the Methods section, the system in this study uses a smartphone application to send messages and images to the dietitians and receive feedback messages from them. This system requires very few steps for patients with CVD, including the elderly, compared to the number of things patients do with the multifunctional applications that have been developed in recent years. This study examines the effectiveness of a smartphone application that uses photos of meals of patients with CAD to provide nutrition education and feedback from a dietitian.
Methods
Study design
The TeleDiet study (NCT05071495) is a single-centre, prospective RCT with two parallel groups and a 12-week follow-up period. The study was conducted at Jessa Hospital and Hasselt University in Belgium. After determining eligibility and obtaining informed consent, participants were randomised 1:1 to either an intervention group (TeleDiet group) or a control group. The participants were randomised 1:1 using the sealed envelope method.
Study population
Participants were patients with CAD (myocardial infarction, unstable or stable angina pectoris as diagnostic criteria for CAD) 20 years of age or older who had undergone coronary revascularization (percutaneous coronary intervention and/or coronary artery bypass grafting during the index hospitalisation) and were scheduled to start CR at Jessa Hospital. The exclusion criteria were as follows. (1) participants with malignant tumours, liver cirrhosis, or other serious diseases other than the target CAD; (2) participants whose life expectancy was less than 6 months or whose follow-up was impossible; (3) participants for whom informed consent could not be obtained; (4) participants for whom CR was impossible (e.g. advanced dementia) and (5) participants with chronic conditions that required them to follow a strict organ-specific diet not compatible with the Mediterranean diet (e.g. pancreatic insufficiency, end-stage renal disease). Participants were recruited in the interview with a dietitian after discharge.
Study procedures
Control group
The control group received the usual dietary treatment by a dietitian and a physician for 12 weeks. Under usual care, dietary guidance by a dietitian was provided at least once after discharge, and additional sessions were planned by the dietitian as needed. In follow-up outpatient visits, physicians provided dietary guidance.
Intervention group (TeleDiet group)
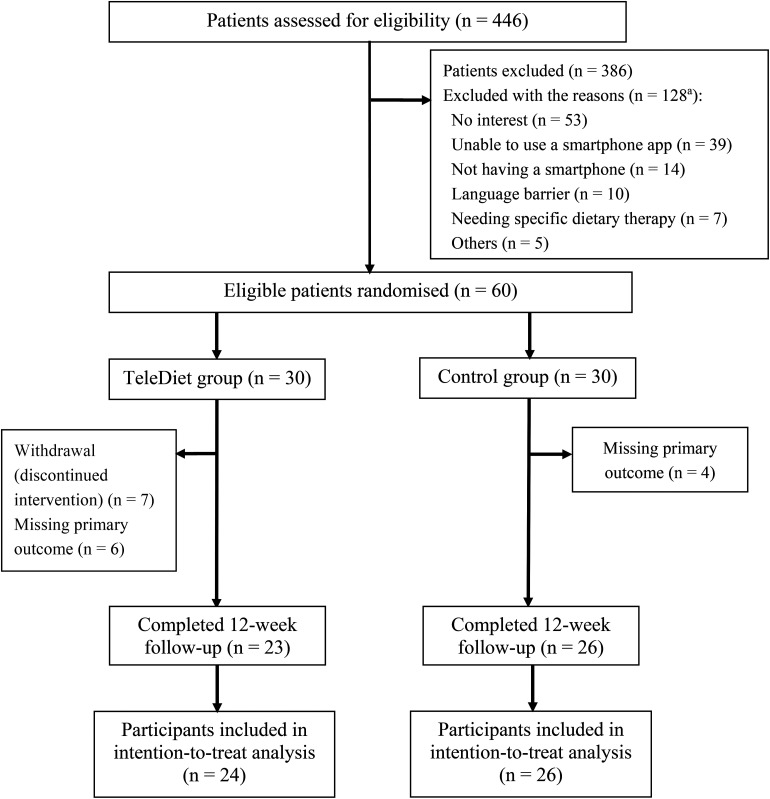
In addition to this usual procedure, the TeleDiet group was asked to install ‘Signal’ (Signal Foundation, Mountain View, CA), a smartphone application which provides messaging services. It was chosen because it offers greater data anonymity and security than ‘WhatsApp’. Participants could use signal to send messages containing files, voice memos, images and videos. The participants were asked to take pictures of every meal, including alcoholic and other beverages, for one week in a row during the month and send them to the dietitians to receive feedback messages from the dietitians. All participants in the CR received a 2-hour lecture on healthy nutrition from one of the dietitians participating in the study. The emphasis of this practical lecture was on how to adhere as much as possible to the Mediterranean diet advocated in the ESC guidelines for prevention.1 All participants underwent a personal interview with the dietitian to obtain information about their actual nutritional patterns and how to improve them. The scientific content of the responses by the dietitians was also based on the dietary guideline.11 During the intervention period, the dietitians provided regular feedback via the application on food components that should be avoided or increased in the diet. The tone of the messages was rather friendly and advisory, not angry or aggressive. Although the dietitians were asked to send feedback as soon as possible, it is up to the dietitians when to check the photos and at what time interval. The feedback included several points about the participant's diet (food types, preparation, calories, approval) (Supplemental material 1). For the next 3 weeks following this week, they did not need to send in any photos, but they could get advice from the dietitians if needed. This process was repeated 3 times during the 12-week observation period (photos were taken and sent at weeks 1, 5 and 9) (Figure 1).
Figure 1.
Study design and randomisation to either the TeleDiet group or the control group.
Measures
Questionnaires on diet, self-efficacy, medication adherence and quality of life
The participants in both the groups were asked to complete questionnaires on diet (including the Mediterranean diet score [MedDietScore]12), self-efficacy (questionnaire of Generalized Self-Efficacy Scale [GSES],13 which assesses the strength of an individual's belief in his or her ability to cope with new and difficult situations), medication adherence (identification of medication adherence barriers [IMAB],14 which is designed to identify barriers to patients taking medication [as opposed to measuring actual adherence]), and quality of life (a core heart disease health-related quality of life questionnaire [HRQoL]15) at weeks 0 and 12 (participants who did not complete the questionnaire at week 12 were reminded to do so as soon as possible) using the website Qualitics.com.
Blood tests
Blood tests including low-density lipoprotein (LDL)-cholesterol, high-density lipoprotein (HDL)-cholesterol, estimated glomerular filtration rate (eGFR) and haemoglobin A1c (HbA1c) were measured at weeks 0 and 6.
Cardiopulmonary exercise testing
Cardiopulmonary exercise testing (CPET) (Ergo 1500 cycle; Ergofit GmbH, Pirmasens, Germany) was performed at weeks 0 and 6 (if CPET could not be performed at week 6 for any reason, it was performed at week 12 instead).
CoroPrevention Nutrition-Score
The Nutrition-Score is a nutritional intake score that was developed in the setting of the Horizons 2020 CoroPrevention project.16 It is a modification of the MedDietScore in which parameters about salt and sugar intake are added to the score, and an intake of zero alcohol is considered positive (in contrast to the MedDietScore, which uses the old knowledge that limiting alcohol was beneficial). The score was developed by the CoroPrevention research team (see Supplemental material 2).
Nutrition knowledge score
The nutrition knowledge questionnaire is a questionnaire that was developed by the CR research team including specialised CR dietitians in Jessa Hospital and Hasselt University. The questionnaire assesses knowledge about heart-healthy food (see Supplemental material 3).
Study outcomes
All outcomes were obtained at Jessa Hospital during the protocol. The primary outcome was the difference in the MedDietScore between baseline and week 12. The secondary outcomes were differences in the Nutrition-Score, GSES, IMAB, HRQoL, and the nutrition knowledge score at baseline and week 12. Also examined as secondary outcomes, differences in LDL-cholesterol, HDL-cholesterol, HbA1c, eGFR on blood tests at baseline and week 6, and body mass index and peak oxygen consumption on CPET at baseline and week 6 (or week 12) were also examined. A semi-structured interview was also conducted to understand the acceptability, feasibility and appropriateness of the intervention,17 and participants’ satisfaction, perceptions and experiences in the intervention group (Supplemental material 4). Withdrawal was defined as discontinuation of sending pictures of meal during the study period.
Statistical analysis
All statistical analyses were performed using SPSS for Windows version 27.0 (SPSS Inc, Chicago, IL). For the sensitivity analysis considering missing data in the dataset, a single imputation method was used in which the missing values were embedded with the mean (median) values of the non-missing observations. Data are presented as mean (standard deviation), median (interquartile range) or percentages. The chi-square test was carried out to calculate proportions. Unpaired t tests or Mann–Whitney U tests were used to compare parameters between the two groups. A two-tailed p-value < 0.05 was considered statistically significant. Our prospective power analysis showed that an effect size of 0.8, alpha error probability of 0.05 and the power of 0.8 would require at least 26 participants in each group.
Results
Participants
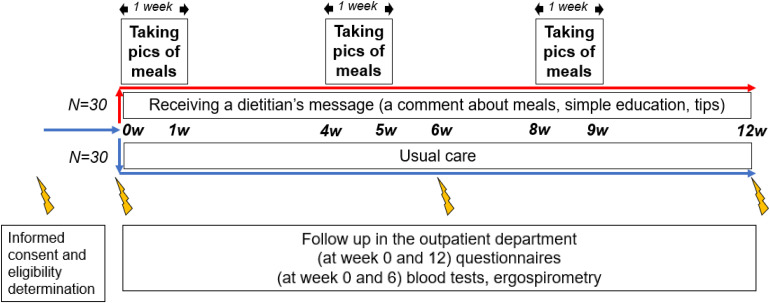
Between March 2021 and April 2022, 446 patients with consecutive CAD were evaluated for eligibility and 60 patients agreed to participate in the study. They were randomly assigned to the TeleDiet group (n = 30) and the control group (n = 30). Finally, 24 participants in the TeleDiet group and 26 participants in the control group were included in the intention-to-treat analysis taking into account those with missing outcome (Figure 2). Baseline characteristics are shown in Table 1. There were no significant differences between the two groups. In the TeleDiet group, a total of seven participants stopped sending any photos in the middle of the intervention period (withdrawal). There were no differences in baseline characteristics between the withdrawals and the rest.
Figure 2.
Study flow diagram.
Table 1.
Baseline characteristics of patients.
| TeleDiet group (n = 30) | Control group (n = 30) | p-value | ||
|---|---|---|---|---|
| Age, years | 58 (7) | 60 (10) | 0.519 | |
| Male sex | 27 (90) | 27 (90) | 1.000 | |
| Body mass index, kg/m2 | 28.2 [25.8, 30.9] | 28.0 [24.4, 30.1] | 0.395 | |
| Current smoker | 11 (37) | 5 (17) | 0.080 | |
| Coronary artery disease | STEMI | 7 (23) | 8 (27) | 0.764 |
| NSTEMI/UAP | 12 (40) | 10 (33) | 0.588 | |
| Procedure performed | PCI | 27 (90) | 28 (93) | 1.000 |
| CABG | 4 (13) | 3 (10) | 1.000 | |
| Comorbidities | Hypertension | 17 (57) | 15 (50) | 0.605 |
| Dyslipidaemia | 28 (93) | 23 (77) | 0.145 | |
| Diabetes | 6 (20) | 8 (27) | 0.542 | |
| Blood tests | LDL-cholesterol, mg/dL | 102 (49) | 106 (42) | 0.718 |
| HDL-cholesterol, mg/dL | 49 (16) | 51 (18) | 0.588 | |
| HbA1c, %b | 5.8 [5.5, 6.1] | 5.7 [5.5, 6.4] | 0.691 | |
| Estimated GFR, mL/min | 80 [72, 97] | 84 [75, 98] | 0.539 | |
| Echocardiographya | Normal ejection fraction (≥ 50%) | 22 (73) | 23 (77) | 0.708 |
| Cardiopulmonary exercise testing | Peak VO2, mL/min/kg | 20.5 [18.1, 23.6] | 21.1 [16.6, 25.9] | 0.833 |
| Medications | ACEi/ARB, ARNI | 19 (63) | 18 (60) | 0.791 |
| Beta blockers | 23 (77) | 16 (53) | 0.058 | |
| Statins | 26 (87) | 28 (93) | 0.671 | |
| Antiplatelets | 30 (100) | 29 (97) | 1.000 | |
| Mediterranean diet score | 32 [30, 37] | 33 [29, 38] | 0.915 |
Values are mean (standard deviation), median [interquartile range] or n (%).
Data were obtained from the most recent (up to 6 months prior) echocardiogram at the time of inclusion.
n = 55.
ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; ARNI, angiotensin receptor-neprilysin inhibitor; CABG, coronary artery bypass grafting; GFR, glomerular filtration rate; HbA1c, haemoglobin A1c; HDL, high-density lipoprotein; LDL, low-density lipoprotein; NSTEMI, non-ST-elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction; UAP, unstable angina pectoris; VO2, oxygen consumption.
Primary outcome
The difference in the MedDietScore from baseline to week 12 in the TeleDiet group was greater than in the control group, but not significant (between-group difference 2.0 [−1.0, 4.0] vs. 0.0 [−3.0, 1.5], p = 0.066). However, there was a significant difference in the within-group analysis for the MedDietScore in the TeleDiet group (32 [30, 38] at baseline vs. 36 [33, 41] at week 12, p = 0.045) but not in the control group (33 [28, 38] at baseline vs. 34 [27, 37] at week 12, p = 0.582) (Table 2).
Table 2.
Differences in the questionnaires from baseline to week 12 and blood tests and CPET from baseline to week 6.
| N | TeleDiet group | Control group | p-value | ||
|---|---|---|---|---|---|
| Primary outcome | Mediterranean diet score | 50 | 2.0 [−1.0, 4.0]a | 0.0 [−3.0, 1.5] | 0.066 |
| Secondary outcomes | CoroPrevention Nutrition-Score | 50 | 3.0 [1.0, 3.5] | 0.0 [−3.0, 2.0] | 0.029 |
| GSES | 53 | 0.0 [−3.5, 1.0] | 0.0 [−1.0, 1.5] | 0.659 | |
| IMAB score | 53 | −0.2 (3.5) | −0.2 (3.1) | 0.968 | |
| HRQoL score | 53 | 7.4 (8.9) | 3.2 (7.0) | 0.063 | |
| Nutrition knowledge score | 53 | 1.9 (1.7) | 0.8 (2.1) | 0.048 | |
| LDL-cholesterol, mg/dL | 53 | −39 (53) | −44 (42) | 0.689 | |
| HDL-cholesterol, mg/dL | 53 | −2.2 (7.1) | −0.1 (7.7) | 0.303 | |
| HbA1c, % | 34 | 0.1 [0.0, 0.2] | −0.1 [−0.2, 0.2] | 0.457 | |
| Estimated GFR, mL/min | 52 | −6.0 [−8.5, 0.0] | −6.5 [−13.0, −0.5] | 0.819 | |
| Body mass index, kg/m2 | 56 | −0.3 [−1.0, 0.0] | 0.0 [−0.7, 0.3] | 0.679 | |
| Peak VO2, mL/min/kg | 44 | 1.3 [0.0, 3.2] | 1.9 [−0.3, 4.0] | 0.830 |
Values are mean (standard deviation) or median [interquartile range].
In the within-group analysis, there was a significant difference only in the TeleDiet group (p = 0.045).
CPET, cardiopulmonary exercise testing; GFR, glomerular filtration rate; GSES, General Self-Efficacy Scale; HbA1c, haemoglobin A1c; HDL, high-density lipoprotein; HRQoL, Health-related quality of life; IMAB, Identification of Medication Adherence Barriers; LDL, low-density lipoprotein; VO2, oxygen consumption.
Secondary outcomes
The difference in the Nutrition-Score in the TeleDiet group from baseline to week 12 was significantly greater than in the control group (3.0 [1.0, 3.5] vs. 0.0 [−3.0, 2.0], p = 0.029). From baseline to week 12, the nutrition knowledge score of the TeleDiet group improved significantly over the control group (1.9 ± 1.7 vs. 0.8 ± 2.1, p = 0.048). There was no significant increase in HRQoL score in the TeleDiet group compared to the control group (7.4 ± 8.9 vs. 3.2 ± 7.0, p = 0.063). There were no significant differences between the two groups for other parameters such as blood tests and CPET (Table 2). Sensitivity analysis was performed on missing data using the single imputation method (Supplementary material 5). The primary outcome and HbA1c showed significant differences between the intervention and the control groups, but the other results remained the same. The results of the semi-structured interviews are presented in Supplemental material 6. Thirteen participants in the TeleDiet group finished the Acceptability of Intervention Measure, Intervention Appropriateness Measure, and Feasibility of Intervention Measure questionnaires. All three questionnaire scores are above 4 out of 5. Although the interpretation of the cut-off score is debatable, higher scores indicate greater acceptability, appropriateness, and feasibility, and these results represent good values.
Detailed analysis of ‘Signal’ application
Data only from participants in the TeleDiet group who transmitted photographic data (n = 21) were examined for correlations between the three parameters and differences in the MedDietScore (Table 3). The total word counts of affirmative comments (Dutch) including praise, encouragement and dietary guidance by the dietitians, was positively related to the difference in the MedDietScore (r = 0.546, p = 0.013). The higher response time between sending a photo and receiving a message was negatively correlated with the change in the MedDietScore (r = −0.468, p = 0.037). The difference in the number of photos sent between the first (week 1) and the third (week 9) was not associated with the MedDietScore (r = 0.175, p = 0.462). In the TeleDiet group, the average number of responses by the dietitians was 63 ± 24 for a total of 3 weeks (weeks 1, 5 and 9) and the average number of pictures taken per participant per day was 4.2 ± 1.6.
Table 3.
Correlation between signal application parameters and differences in the MedDietScore in the TeleDiet group (n = 20).
| Mean/median | Correlation coefficient | p-value | |
|---|---|---|---|
| Total word counts of affirmative comments made by dietitians during the intervention period (in Dutch) | 1171 (398) | 0.546 | 0.013 |
| Average response time from photo transmission to message reception (minutes) | 432 [374, 773] | −0.468 | 0.037 |
| Difference between the number of photos sent at week 9 (3rd time) and at week 1(1st time) | −11 [−15, −5] | 0.175 | 0.462 |
Values are mean (standard deviation) or median [interquartile range].
Discussion
The results of this study can be summarised as the following main findings. (i) The intervention resulted in a non-significant difference in the MedDietScore in the TeleDiet group compared to the control group. There was a small non-significant difference which could be considered as a trend. The Nutrition-Score, including data on salt, sugar and alcohol however did show significantly better scores in the TeleDiet group. (ii) Improvement in Nutrition-related knowledge was significantly higher in the TeleDiet group compared to the control group. (iii) HRQoL improved more in the TeleDiet group than in the control group (but not significant). (iv) The amount of positive information provided and the time required to respond by dietitians were significantly associated with difference in the MedDietScore.
This study shows that communication between the patient and the dietician by sending pictures of their daily meals and drinks, with feedback can improve dietary knowledge. In addition, an earlier paper showed that nutrition knowledge is related to the achievement of the Mediterranean diet.18 The intervention using this application is characterised by two features: a relatively fast response time by dietitians and the use of pictures. First, in usual clinical practice, dietitians cannot advise patients until their next outpatient appointment at a hospital. In this study, however, it takes only about 7 hours on average. As the results shows, the shorter the average response time, the higher the MedDietScore. Second, the dietitians can see the participants’ diet directly in the photos. This helps the dietitians to advise the participants because the dietitians have a realistic picture of the participants’ diet. This follow-up mechanism could be useful in promoting nutritional knowledge and the Mediterranean diet. Furthermore, an RCT on salt intake and hypertension19 has shown that improving dietary knowledge is one of the key goals in achieving outcomes. A previous systematic review20 has stated that the higher degree of patient engagement with a smartphone application, such as self-monitoring (in this study, taking pictures), is associated with improved risk factor outcomes. These previous studies also support the importance of gaining nutritional knowledge and knowing one's own diet. Improvements in the MedDietScore showed only a non-significant trend, so there may be a gap between improved nutritional knowledge and implementation of the Mediterranean diet. The decrease in the number of photos sent from weeks 1 to 9 is debatable and could be interpreted as the participant becoming more familiar with the application or a gradual decrease in adherence to photography.
This intervention tended to enhance HRQoL. A previous study21 has shown that a smartphone application to incorporate secondary prevention into the daily lives of patients with CAD can improve QoL. One of the key words in the paper is personalisation. It is generally accepted that personalised medicine improves patient satisfaction, empowerment and QoL. The high degree of personalisation is achieved by providing rapid feedback on each picture. A previous review22 has indicated that personalised feedback is essential for behavioural change and lifestyle improvement, supporting the present findings. Another meta-analysis23 finds that mHealth is a meaningful strategy because it is customisable and can send time-sensitive messages. This also suggests the importance of personalisation. In addition, the total word counts of affirmative comments, such as praise from the dietitians, were moderately associated with higher MedDietScores. Positive feedback may be related to behaviour change.
The study found a significant impact of the intervention on the Nutrition-Score. Since the MedDietScore does not include salt and sugar intake as recommended by the European Society of Cardiology, American Heart Association, and World Health Organization, the Nutrition-Score was created to include the basic components of salt and sugar intake. The results showed that the intervention had a positive impact on salt and sugar intake. This result is important because it is clear that high intakes are associated with hypertension and diabetes. The score will also be used in the EU-funded CoroPrevention project,16 which aims to discover long-term behavioural changes, lifestyle modifications and necessary drug therapies for patients with CAD.
No significant differences in lipid profiles such as LDL-cholesterol were found in the present study; the previous systematic review on smartphone applications for CVD risk factor management20 and RCTs using a smartphone application24 and text messages6 for patients with CVD also showed no significant differences. The difference between the two groups in this study may have been smaller because both groups received statins and other medications and general education by nurses.
Finally, questionnaires were sent to participants in the TeleDiet group regarding usability and feasibility of this system. Many positive comments were made about the system. On the other hand, there were also comments comparing the system to traditional methods. The key to future adoption of digital cardiology seems to be not only to develop more applications, but also to combine applications with face-to-face communication.25 Furthermore, the dietitians scored lower on feasibility than the participants. In the recent published guideline, reducing the burden on healthcare professionals is one of the key points for the implementation of digital cardiology.26 In this regard, the development of artificial intelligence, such as automatic image analysis and automatic advice response systems, is desirable. In the future, efforts should be made to incorporate this developed system into daily clinical practice.
Study limitations
The trial has several limitations. First, although a power analysis was performed before the study began, the number of all participants followed up in week 12 and the number of participants who had a smartphone, could use it, and could take and send photos was lower than expected because of the withdrawal. Therefore, some results may reflect an inadequate sample size. Second, this trial is a preliminary study of the mHealth for dietary therapy in patients with CAD. Recent trials in the field of mHealth have increasingly included smartphone applications with ‘all-in-one’ capabilities that include many elements for CR. However, the system tested in the current study is low-cost and requires only a few simple steps. Along with a multifunctional application, attention should be paid to such a small and simple application so that digital cardiology can be widely used by older patients. Third, 90% of the participants in both the groups in this study were male. This could be the so-called ‘gender digital divide’27 and may bias the results. Fourth, the lack of significant results in the primary outcome still raises the question of whether this procedure, which uses a smartphone application, is worth implementing in patients’ real lives. Further trials should be conducted in the future. Fifth, there were no parameters for sociodemographic characteristics (e.g. highest education or household income indicators). Sixth, the usefulness of the application is limited to those who own and can use a smartphone. Finally, the dietitians cannot provide feedback at all hours and the average time between sending a photo and the dietitian providing feedback (about 7 hours) may not indicate that the diet will be changed immediately. However, this is only an average, and it is also true that feedback before the next meal can provide useful advice for changing the content from one meal to the next.
Conclusion
A feedback system using a simple messaging application that allows participants to simply send a picture of their food is associated with improvements in nutrition knowledge. This supports the implementation of the Mediterranean diet.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076231164101 for The impact of dietary education and counselling with a smartphone application on secondary prevention of coronary artery disease: A randomised controlled study (the TeleDiet study) by Toshiki Kaihara, Maarten Falter, Martijn Scherrenberg, Linqi Xu, Jana Maes, Elise Meesen and Paul Dendale in Digital Health
Acknowledgements
The authors would like to thank the entire staff of the rehabilitation centre at Jessa Hospital for their dedication and understanding of this study. Special thanks go to Lara Dobbels, our social nurse, and two dietitians, Anne Gijbels and Inge Gielen.
Footnotes
Authors’ contributions: TK, MF, MS and PD contributed to the conception or design of the work. TK, MF, MS, LX and JM contributed to the acquisition, analysis or interpretation of the dataset. TK drafted the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work ensuring integrity and accuracy.
Availability of data and materials: All dataset analysed are included in this manuscript and supplementary materials.
Human and animal rights and Informed consent: The protocol, informed consent form and other study-related documents received approval from the Ethics Committee (EC) of the Jessa Hospital Hasselt and University of Hasselt. The study is implemented according to the Declaration of Helsinki (Appendix III) and Good Clinical Practice.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study received funding by Daiichi-Sankyo, Inc. PD received funding through the Horizons 2020 CoroPrevention project, project number 848056. MF received funding through the Flanders Research Foundation FWO, file number 1SE1222N.
ORCID iD: Toshiki Kaihara https://orcid.org/0000-0003-0941-8035
Supplemental material: Supplemental material for this article is available online.
References
- 1.Visseren FLJ, MacH F, Smulders YM, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021; 42: 3227–3337. [DOI] [PubMed] [Google Scholar]
- 2.Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 2019; 140: E69–E89. [DOI] [PubMed] [Google Scholar]
- 3.Chow CK, Redfern J, Hillis GS, et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA 2015; 314: 1255–1263. [DOI] [PubMed] [Google Scholar]
- 4.Santo K, Hyun K, Keizer L De, et al. The effects of a lifestyle-focused text- messaging intervention on adherence to dietary guideline recommendations in patients with coronary heart disease : an analysis of the TEXT ME study. Int J Behav Nutr Phys Act 2018; 15: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farmer A, Bobrow K, Leon N, et al. Digital messaging to support control for type 2 diabetes (StAR2D): a multicentre randomised controlled trial. BMC Public Health 2021; 21: 1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bae JW, Woo S Il, Lee J, et al. MHealth interventions for lifestyle and risk factor modification in coronary heart disease: randomized controlled trial. JMIR mHealth uHealth 2021; 9: e29928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De La Torre-Diéz I, López-Coronado M, Vaca C, et al. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemed e-Health 2015; 21: 81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alonso-Domínguez R, García-Ortiz L, Patino-Alonso MC, et al. Effectiveness of a multifactorial intervention in increasing adherence to the Mediterranean diet among patients with diabetes mellitus type 2: a controlled and randomized study (EMID study). Nutrients 2019; 11: 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Recio-Rodriguez JI, Conde CA, Calvo-Aponte MJ, et al. The effectiveness of a smartphone application on modifying the intakes of macro and micronutrients in primary care: a randomized controlled trial. The EVIDENT II study. Nutrients 2018; 10: 1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whitelaw S, Pellegrini DM, Mamas MA, et al. Barriers and facilitators of the uptake of digital health technology in cardiovascular care: a systematic scoping review. Eur Hear J - Digit Heal 2021; 2: 62–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lichtenstein AH, Appel LJ, Vadiveloo M, et al. 2021 Dietary guidance to improve cardiovascular health: a scientific statement from the American Heart Association. Circulation 2021; 144: e472–e487. [DOI] [PubMed] [Google Scholar]
- 12.Panagiotakos DB, Milias GA, Pitsavos C, et al. Meddietscore: a computer program that evaluates the adherence to the Mediterranean dietary pattern and its relation to cardiovascular disease risk. Comput Methods Programs Biomed 2006; 83: 73–77. [DOI] [PubMed] [Google Scholar]
- 13.Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In: Measures in health psychology: a user’s portfolio. Causal and control beliefs. Windsor, UK: NFER-NELSON, 1995, pp. 35–37. [Google Scholar]
- 14.Easthall C, Wright D, Taylor N, et al. Developing the ‘Identification of Medication Adherence Barriers’ (IMAB) instrument: a novel application of behaviour change theoretical frameworks. In: United Kingdom Society of Behavioural Medicine. 2012, p. 48.
- 15.Oldridge N, Saner H, Mcgee HM. The Euro Cardio-QoL Project. An international study to develop a core heart disease health-related quality of life questionnaire, the HeartQoL. Eur J Prev Cardiol 2005; 12: 87–94. [DOI] [PubMed] [Google Scholar]
- 16.CoroPrevention project. CoroPrevention: personalised prevention for coronary heart disease, https://coroprevention.eu/ (accessed 5 May 2022).
- 17.Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Heal Ment Heal Serv Res 2011; 38: 65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bonaccio M, Castelnuovo Di, Costanzo A. S, et al. Nutrition knowledge is associated with higher adherence to Mediterranean diet and lower prevalence of obesity. Results from the Moli-sani study. Appetite 2013; 68: 139–146. [DOI] [PubMed] [Google Scholar]
- 19.Riches SP, Piernas C, Aveyard P, et al. A mobile health salt reduction intervention for people with hypertension: results of a feasibility randomized controlled trial corresponding author. JMIR Med Informatics 2021; 9: e26233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spaulding EM, Marvel FA, Piasecki RJ, et al. User engagement with smartphone apps and cardiovascular disease risk factor outcomes: systematic review corresponding author. JMIR Cardio 2021; 5: e18834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eckardt I, Buschhaus C, Nickenig G, et al. Smartphone-guided secondary prevention for patients with coronary artery disease. J Rehabil Assist Technol Eng 2021; 8: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrier S, Blanchard CM, Vallis M, et al. Behavioural interventions to increase the physical activity of cardiac patients : a review. Eur J Cardiovasc Prev Rehabil 2011; 18: 15–32. [DOI] [PubMed] [Google Scholar]
- 23.Sequi-dominguez I, Alvarez-bueno C, Martinez-vizcaino V. Effectiveness of mobile health interventions promoting physical activity and lifestyle interventions to reduce cardiovascular risk among individuals with metabolic syndrome: systematic review corresponding author. J Med Internet Res 2020; 22: e17790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi BG, Dhawan T, Metzger K, et al. Image-based mobile system for dietary management in an American cardiology population: pilot randomized controlled trial to assess the efficacy of dietary coaching delivered via a smartphone app versus traditional counseling. JMIR mHealth uHealth 2019; 7: e10755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eiland L, Drincic A. Far apart, but close at heart: the importance of understanding patient barriers to telehealth and potential solutions. Circulation 2022; 146: 147–149. [DOI] [PubMed] [Google Scholar]
- 26.Tromp J, Jindal D, Redfern J, et al. World heart federation roadmap for digital health in cardiology. Glob Heart 2022; 17: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Picatoste X, Mesquita A, González-Laxe F. Gender wage gap, quality of earnings and gender digital divide in the European context. Empirica 2022; 1–21. Epub ahead of print. DOI: 10.1007/s10663-022-09555-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076231164101 for The impact of dietary education and counselling with a smartphone application on secondary prevention of coronary artery disease: A randomised controlled study (the TeleDiet study) by Toshiki Kaihara, Maarten Falter, Martijn Scherrenberg, Linqi Xu, Jana Maes, Elise Meesen and Paul Dendale in Digital Health