Abstract
In the last 20 years, noninvasive serum biomarkers to identify liver fibrosis in patients with non-alcoholic fatty liver disease (NAFLD) have been developed, validated against liver biopsy (the gold standard for determining the presence of liver fibrosis) and made available for clinicians to use to identify ≥F3 liver fibrosis. The aim of this review is firstly to focus on the current use of widely available biomarkers and their performance for identifying ≥F3. Secondly, we discuss whether noninvasive biomarkers have a role in identifying F2, a stage of fibrosis that is now known to be a risk factor for cirrhosis and overall mortality. We also consider whether machine learning algorithms offer a better alternative for identifying individuals with ≥F2 fibrosis. Thirdly, we summarise the utility of noninvasive serum biomarkers for predicting liver related outcomes (e.g., ascites and hepatocellular carcinoma) and non-liver related outcomes (e.g., cardiovascular-related mortality and extra hepatic cancers). Finally, we examine whether serial measurement of biomarkers can be used to monitor liver disease, and whether the use of noninvasive biomarkers in drug trials for non-alcoholic steatohepatitis can accurately, compared to liver histology, monitor liver fibrosis progression/regression. We conclude by offering our perspective on the future of serum biomarkers for the detection and monitoring of liver fibrosis in NAFLD.
Keywords: NAFLD, Liver fibrosis, Biomarker
INTRODUCTION
The global prevalence of nonalcoholic fatty liver disease (NAFLD) has been rising steadily since 2006 [1] and NAFLD is estimated to affect a quarter of the world’s adult population [2]. NAFLD represents a spectrum of liver fat-associated conditions that begins with liver fat accumulation and progresses to steatohepatitis, liver fibrosis and cirrhosis. Within that spectrum of liver disease, it is patients with F3 [3] fibrosis and F4 [3] cirrhosis who are at substantial risk of death from end-stage liver disease and liver cancer. However, the earlier stages of liver fibrosis lend themselves well to therapeutic interventions to either attenuate or ameliorate progression and potentially reverse liver damage [4-7]. Thus, managing patients with NAFLD necessitates identification of F1 [3] and F2 [3] stages and estimation of the risk of progression to a more advanced stage of fibrosis/cirrhosis. However, liver disease can be hard to identify before it has reached a very advanced stage because it usually progresses without signs or symptoms [8].
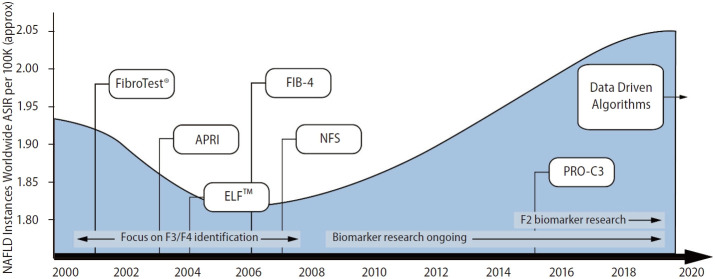
In the last 20 years significant advances have been made in the development of noninvasive serum biomarkers for the identification of liver fibrosis. In this brief review, we describe these biomarkers and discuss their current utility and their potential future use in clinical practice. We consider whether liver fibrosis biomarkers have a role in: a) identifying F2 (that might be amenable to treatment as a relatively early stage of fibrosis), b) predicting patient outcomes and c), whether biomarkers can be used to help track progression or amelioration of liver fibrosis.
INITIAL AND CURRENT USE OF NONINVASIVE SERUM BIOMARKERS FOR NAFLD
Liver fibrosis is one of the most relevant prognostic factors for important clinical outcomes in NAFLD [9], yet liver fibrosis often remains undiagnosed until it has progressed to cirrhosis. With the global prevalence of NAFLD estimated to be between 31.6% and 40.8% of the population [10], it is important to be able to detect liver fibrosis early in the disease process, so that effective interventions can be implemented before the disease becomes too advanced. The gold standard for identification and staging of liver fibrosis is liver biopsy, however, it is a diagnostic procedure that is time consuming, costly, invasive, subject to sampling error [11], and not scalable considering the magnitude of the global health care burden imposed by NAFLD.
Noninvasive serum biomarkers for fibrosis were initially developed by and for secondary care physicians, to use as a diagnostic assessment tool to detect patients who have advanced liver fibrosis and/or cirrhosis, offering an alternative and potential replacement to liver biopsy. A number of noninvasive serum biomarkers have been developed over the last 20 years and we now have tests, that have been validated against liver biopsy, such as the enhanced liver fibrosis (ELFTM) test [12], fibrosis-4 (FIB-4) index [13], NAFLD fibrosis score (NFS) [14], aspartate aminotransferase to platelet radio index (APRI) [15] and FibroTest® [16] (FibroSURETM in the USA). These relatively common tests are widely available for use in both primary and secondary care and offer a variable degree of accuracy and reliability (Table 1).
Table 1.
Summary of the performance comparison of five widely available and frequently used noninvasive serum biomarkers for diagnosing ≥F3 liver fibrosis in NAFLD
| Performance | Noninvasive blood biomarker |
|||||
|---|---|---|---|---|---|---|
| ELF™ [35] | FIB-4 [32] | NFS [32] | APRI [32] | FibroTest® [33] | ||
| AUC value | 0.83 | 0.80 | 0.78 | 0.75 | 0.77 | |
| Sensitivity | 0.42 | 0.32 | 0.43 | 0.33 | 0.72 | |
| Specificity | 0.95 | 0.96 | 0.88 | 0.91 | 0.69 | |
| PPV | 0.85 | 0.66 | 0.67 | 0.56 | NR | |
| NPV | 0.71 | 0.85 | 0.89 | 0.79 | NR | |
| Notable differences | ||||||
| Age included in algorithm | √ | √ | √ | √ | ||
| Score calculated from routine blood and anthropometric measurements* | √ | √ | √ | |||
| Additional costs beyond routine blood tests incurred | √ | √ | ||||
| Utility for high prevalence setting only | √ | √ | √ | √ | √ | |
NAFLD, non-alcoholic fatty liver disease; AUC, area under the curve; PPV, positive predictive value; NPV, negative predictive value; NR, not reported; ELF™, enhanced liver fibrosis; FIB-4, fibrosis-4; NFS, nonalcoholic fatty liver disease fibrosis score; APRI, aspartate transaminase to platelet ratio index. *Online calculators for FIB-4, NFS, and APRI are available: FIB-4: e.g., https://gps.northcentrallondon.icb.nhs.uk/fib-4-calculator and https://www.hepatitisc.uw.edu/page/clinical-calculators/fib-4.
APRI: e.g., https://www.hepatitisc.uw.edu/page/clinical-calculators/apri and https://www.omnicalculator.com/health/apri.
Combining noninvasive serum biomarkers has been shown to further improve diagnostic performance compared with single biomarker performance alone [17,18]. Nevertheless, the current use of noninvasive serum biomarkers focuses on excluding disease, e.g., stratification of patients into those who have a high probability of ≥F3 fibrosis versus those who have a low probability of ≥F3 fibrosis. The utility of noninvasive serum biomarkers is therefore limited because even though they have been used to identify someone with a high probability of ≥F3 fibrosis, additional tests are required to confirm this. For example, in UK primary care, the biomarkers NFS, FIB-4 and ELFTM are recommended for use to identify patients with a high probability of ≥F3 fibrosis [19] but as the biomarker itself is not informative enough as a basis for intervention, the recommendation is to follow biomarker testing with vibration controlled transient elastography (VCTE) [20], to confirm the stage of fibrosis. In Korea, the recommendation is to assess for fibrosis using radiological examinations such as VCTE [21]. If this is not feasible then NFS or FIB-4 are the recommended tests [21].
DO BIOMARKERS HAVE A ROLE IN IDENTIFYING F2 FIBROSIS?
We now know that F2 fibrosis has important consequences for patients [22,23]. F2 fibrosis is a risk factor for cirrhosis and overall mortality and F2 increases the risk of extra hepatic complications including cardio vascular disease [22,23]. Approximately 20% of patients diagnosed with low-levels of liver fibrosis (F1–F2) will progress to F3, or F4, within 5 years [24]. F2 is a stage of fibrosis that is easily managed in primary care and it is potentially treatable and maybe halted or reversed through lifestyle changes [6,25,26]. Alternatively, medications such as anti-fibrotic therapeutic drugs (currently in phase 3 trials [27]) or glucagon-like peptide-1 agonist medication [28] may have beneficial effects on the early stages of liver fibrosis. It is therefore important for clinicians to be able to identify F2 accurately, precisely, quickly and easily, which noninvasive serum biomarkers have the potential to do. However, there are difficulties in determining the optimum cut-off value to use to differentiate intermediate states of fibrosis from the more advanced stages [29,30]. To date no one biomarker is recommended for the detection of F2 [13,31].
Recent systematic reviews evaluating the five widely available noninvasive biomarkers concluded that APRI [32], FIB-4 [32], FibroTest® [33] and NFS [32] showed a fair [34] performance for identifying ≥F2 fibrosis (Table 2). The performance of ELFTM [35] however was evaluated as good [34], although it should be noted that ELFTM may produce a high number of false positive tests (specificity=12%). In another systematic review, PRO-C3 [36] (N-terminal type III collagen pro-peptide) a less widely available noninvasive blood biomarker, has been shown to match the performance of ELFTM and outperform APRI, FIB-4, FibroTest®, and NFS [32]. In this study PRO-C3 had a sensitivity and specificity of 68% (95% confidence interval [CI], 0.50–0.82) and 79% (95% CI, 0.71–0.86) respectively, with an area under the curve (AUC) of 0.81 (95% CI, 0.77–0.84) [36]. However, the availability of PRO-C3 is limited. Currently, the PRO-C3 assay is exclusively produced by a pharmaceutical company and at present is only used for research purposes and is not recommended for clinical use [36].
Table 2.
Comparison of the performance of ELF™, FIB-4, APRI, FibroTest®, and NFS for identifying ≥F2 fibrosis
| Biomarkers | Cut-off values | AUC | Summary sensitivity (%) | Summary specificity (%) | Summary PPV (%) | Summary NPV (%) |
|---|---|---|---|---|---|---|
| APRI [32] | 0.43–1.50 | 0.70 | 59.3 (33.3–71.1) | 77.1 (66.2–90.6) | 67.5 (61.1–74.3) | 70.6 (57.6–87.5) |
| FIB-4 [32] | 0.37–3.25 | 0.75 | 64.4 (54.4–77.8) | 70.0 (60.0–87.5) | 73.3 (66.2–77.8) | 60.6 (40.5–74.2) |
| FibroTest® [33] | 0.30–0.75 | 0.77 | 56.0 (45.0–66.0) | 77.0 (74.0–80.0) | NR | NR |
| NFS [32],* | –1.1 | 0.72 | 66.5 (60.9–70.1) | 82.5 (68.7–96.3) | 81.7 (76.6–86.7) | 73.6 (61.1–86.0) |
| ELF™ [35] | 7.7† | 0.81 | Sensitivity=0.96 | Specificity=0.12 | PPV=0.42 | NPV=0.83 |
Values are presented as mean (range).
ELF™, enhanced liver fibrosis test; FIB-4, fibrosis-4; APRI, aspartate transaminase to platelet ratio index; NFS, nonalcoholic fatty liver disease fibrosis score; AUC, area under the curve; PPV, positive predictive value; NPV, negative predictive value; NR, not recorded.
Two studies were used for to assess the performance of NFS for significant fibrosis. One cut point was reported.
Manufacturers recommended cut-off value for moderate fibrosis. [50]
Ideally, clinicians should be able to quickly and easily assess their patients for ≥F2 fibrosis without having to request additional costly blood tests that require specialist evaluation (e.g., ELFTM and FibroTest®). Sripongpun et al. [37] developed and validated a biomarker (Steatosis-Associated Fibrosis Estimator, SAFE) specifically to identify ≥F2 fibrosis. SAFE has seven variables (sex, body mass index [BMI], diabetes status, aspartate transaminase [AST], alanine transaminase [ALT], platelet and globulin) [37]. SAFE is therefore similar to the NFS that includes age, BMI, platelet count, AST and ALT ratio [14]. SAFE was shown to outperform NFS [37], suggesting that the coefficients applied to SAFE maybe a better fit for identifying ≥F2 fibrosis in modern NAFLD patients [37].
The use of machine learning from serum biomarker data has been found to offer a good performance for identifying ≥F2 fibrosis, AUC 0.86 [38]. A recently published study utilised routinely available data to develop and validate six algorithms (LiverAID XXS, XS, S, M, L, and 4XL) to identify ≥F2 [38]. The diagnostic performance of all the LiverAID models for detecting ≥F2 outperformed FIB-4 and APRI, and in all cases was statistically significant (P≤0.001): the AUC of LiverAID-XXS=0.86, the AUC of LiverAID-XS=0.89, the AUC of LiverAID-S=0.91, the AUC of LiverAID-M=0.92, the AUC of LiverAID-L=0.92, the AUC of LiverAID-4XL=0.94, the AUC of FIB-4=0.70 and the AUC of APRI=0.74. This demonstrates how machine learning models can utilise data and very quickly learn to identify liver fibrosis. However, the performance of machine learning algorithms is dependent on the quantity and quality of the input data and using liver biopsy as the reference standard. To date, the data available from liver histology studies are not sufficient to develop and guide the algorithms and available datasets are currently far too small [39]. At present, the use of machine learning to identify fibrosis is still in its infancy. That said, machine learning is well positioned to deal with this type of dynamic data in the future (Fig. 1) [40].
Figure 1.
Timeline showing the global rise in NAFLD and the emergence of noninvasive biomarkers for fibrosis in NAFLD. NAFLD, non-alcoholic fatty liver disease; ASIR, age-standardised incidence rate per 100,000 persons; ELFTM, enhanced liver fibrosis; FIB-4, fibrosis-4; NFS, nonalcoholic fatty liver disease fibrosis score; APRI, aspartate transaminase to platelet ratio index; PRO-C3, type III collagen marker of the N-terminal pro-peptide.
CAN A SINGLE BIOMARKER TEST PREDICT PATIENT OUTCOMES?
Observational studies have shown biopsy-confirmed liver fibrosis is a prognostic factor for patients with NAFLD [41,42]. A single biomarker that can predict patient outcomes as well as, or better, than liver biopsy would be a useful tool for clinicians managing patients with liver disease. However, there is conflicting evidence [43-45] and this may be in part due to the ethnicity of populations studied, the length of follow-up period, or inadequate sample sizes and the limited power of the studies to address these questions [43-45].
A medium sized study (n=153) based in Israel [43], with a follow-up period of 100 months, has shown that FIB-4 and NFS, but not APRI, when compared with liver biopsy, are good predictors of overall mortality. Higher FIB-4, NFS and APRI scores were also associated with hepatic and extra-hepatic malignancies [43]. A larger sized study (n=301) in Japan with a follow-up period of 84 months, has shown that FIB-4 and NFS are useful for predicting the occurrence of liver-related complications (e.g., varices, ascites or encephalopathy) [44]. However, these scores were limited in their ability to predict extrahepatic malignancies [44]. A recent systematic review concluded that in secondary care, FIB-4, NFS and APRI show limited performance in predicting changes in fibrosis (as evaluated by biopsy) [45]. However, these scores consistently predicted liver-related morbidity (e.g., ascites, esophageal varices or hepatocellular carcinoma), and also liver-related mortality [45].
A more recent (2022) systematic review and meta-analysis has reaffirmed that NFS and FIB-4 are reliable and comparable to liver biopsy as prognostic markers of all-cause mortality in NAFLD patients. Additionally, NFS may be useful for predicting risk of cardiovascular death [46]. Further, a large retrospective study (n=5,123) in America [47] found that the risk of progression to cirrhosis and decompensation increased by FIB-4 strata at NAFLD diagnosis [47]. In Individuals with FIB-4 <1.3, the risk of NAFLD progression was higher than for those with 1.30-2.67 (hazard ratio [HR]=3.67; 95% CI=1.65–8.15; P=0.0014) and FIB-4 >2.67 (HR=56.26; 95% CI=25.77–122.83; P<0.001) [47]. Also, the risk of death was higher in individuals with FIB-4 >2.67 (HR, 3.26; P<0.001) [47]. In a different study, it has been shown that ELFTM predicts clinical outcomes more accurately than liver biopsy [48]. A one-point increase in ELFTM score was associated with a twofold increase in risk of liver-related clinical outcome (defined as liver-related death or episode of decompensated cirrhosis e.g., ascites or esophageal variceal hemorrhage) [48]. Therefore, noninvasive serum biomarkers for liver fibrosis in NAFLD, e.g., NFS, FIB-4, and ELFTM may help predict non-liver-related outcomes e.g., cardiovascular-related mortality [46], and extra-hepatic cancers [43,44]; thus demonstrating their utility beyond simply diagnosing liver disease.
In the US, ELFTM has been granted marketing authorization by the American Food and Drug Administration (FDA) for use as a prognostic risk assessment tool for assessing the likelihood of fibrosis progression in patients with advanced fibrosis [49]. The guidance from the manufacturers of ELFTM is that in patients with F3 bridging fibrosis, an ELFTM score of ≥9.8 indicates an increased risk of progression to cirrhosis in 1–5 years [50]. The guidance also states that in patients with compensated cirrhosis, an ELFTM score of ≥9.8 indicates an increased risk of progression within 5 years to a liver-related event (e.g., development of hepatocellular carcinoma, liver failure or death) [50]. The manufacturers of ELFTM do not, however, quantify how great the risk of progression is. In our opinion, a more accurate interpretation of their guidance should be that after a liver biopsy has diagnosed F3 bridging fibrosis, an ELFTM score of ≥9.8 indicates a risk of progression to cirrhosis in 1–5 years. In the UK, the ELFTM test is the recommended noninvasive blood biomarker test, to identify advanced fibrosis in patients diagnosed with NAFLD [20]. The guidelines are to repeat ELFTM every three years [20], and not to use serial ELFTM measurements to monitor disease progression. Rather, the test should be used at any single moment in time to predict risk of prevalent ≥F3 liver fibrosis.
CAN SERIAL MEASUREMENT OF LIVER FIBROSIS BIOMARKERS HELP TRACK OR MONITOR DISEASE PROGRESSION?
As it is often uncertain how quickly liver disease will progress, a reliable noninvasive test to monitor progression over time is needed. Noninvasive serum biomarkers have the potential to monitor disease progression or amelioration over time. Having a baseline biomarker result that is repeated at regular intervals to monitor liver health would be useful for both patients and clinicians. However, repeating a biomarker and relying on the result to inform a prognosis requires the change in biomarker score to be independently validated against the change in liver biopsy, the gold standard for determining the presence and degree of liver fibrosis.
An alternative to using liver biopsy to validate biomarker score changes would be to examine retrospective biomarker scores over time in relation to liver disease progression, as was undertaken by Hagström et al. [51]. These investigators used data from a retrospective population based cohort (1986–1996) and showed that repeating FIB-4 within a 5-year period can, in comparison to a single measurement, help identify individuals who are at a higher risk of developing severe liver disease [51]. These authors noted that repeating FIB-4 is only recommended for individuals at a low risk of worsening fibrosis. The recommendation for a high risk patients was that these individuals should undergo additional diagnostic testing, e.g., VCTE, without repeat testing of FIB-4 [51]. In another retrospective analysis, Balkhed et al. [52] examined data from a high prevalence of liver disease setting and showed the accuracy of FIB-4 (and APRI) is only weakly associated with disease progression. The authors concluded that the biomarkers have limited clinical utility in monitoring the course of NAFLD progression [52].
Metabolomics analysis has been used as a promising method in NAFLD to investigate novel biomarkers involved in the pathogenesis of the disease [53]. In particular, serum lipocalin 2 has been identified as a key molecule participating in transport of fatty acids [54], that may serve as a valuable NAFLD biomarker for monitoring the initiation and progression of fibrosis [54].
Currently, there is still no licensed drug treatment for NAFLD. In the last decade, there have been many clinical trials testing new drugs for the treatment of liver disease in NAFLD. However, data obtained from these trials have shown suboptimal results, particularly for treatment of liver fibrosis [55]. In clinical trials for NAFLD treatment, liver biopsy is the reference standard used to assess liver fibrosis, which means that participants are required to have at least two (baseline and end of study) invasive procedures to assess the efficacy of a drug. In therapeutic drug trials for non-alcoholic steatohepatitis (NASH), noninvasive serum biomarkers are often (but not always) included to assess for changes in liver fibrosis. Therefore, when the liver biopsy findings in a drug trial show a change in the staging of fibrosis, the performance of biomarkers can be compared against the changes in liver histology.
We reviewed all 21 of the NASH drug trials from a recent systematic review and meta-analysis by Ampuero et al. [55] (Supplementary Table 1). Five [27,56-59] studies did not use any widely available noninvasive biomarker to assess changes in liver fibrosis, one [60] study stated that the data is not publicly available, and two [61,62] were conference reports/poster presentations. We tabulated the remaining 13 studies [63-75], (Supplementary Table 2) and an abridged version shown as Table 3, to illustrate the biopsy-observed changes in liver fibrosis and the changes that occurred in serum biomarker scores (ELFTM, NFS, APRI, FIB-4, FibroTest® , and PRO-C3) between baseline and follow-up assessment. It should be noted that the primary aim of the drug trials shown in the tables was to evaluate the efficacy of a therapeutic drug treatment for NASH, rather than to investigate the ability of noninvasive serum biomarkers to monitor change in histological measurement of fibrosis. As such, the value of the data reported and available from the published research papers is limited to address the question of whether biomarkers can be used to monitor changes in fibrosis attributed to a therapeutic intervention. For example, the biomarker scores at baseline and follow-up for ELFTM, NFS, APRI, FIB-4, FibroTest®, and PRO-C3 in all the trials were all reported as an average score observed changes between baseline and follow up. Nine [63-71] of the studies included participants with F1 and F2 (and in some studies F0); yet the serum biomarkers used to assess fibrosis (ELFTM, NFS, APRI, FIB-4, and FibroTest®) are currently only validated for ≥F3 fibrosis. The participant eligibility criteria for the remaining four [72-75] studies was F3 at baseline. Therefore a comparison of biomarker performance against changes in liver histology should be possible. However, only one of the studies (Harrison et al. [74], 2020) provided sufficient data to make this comparison. Therefore, the utility of noninvasive biomarkers to track changes in liver fibrosis needs further study in therapeutic trials targeting treatment of fibrosis.
Table 3.
Comparison between change in noninvasive serum biomarkers and change in liver fibrosis assessed by liver histology, in therapeutic trials of nonalcoholic steatohepatitis (NASH)
| Study | Study design, duration & numbers recruited | Relevant drug for NASH | Patient group | Fibrosis marker | Baseline | Follow-up | Change in mean | Change in serum biomarker score |
|---|---|---|---|---|---|---|---|---|
| Newsome et al. [63] (2021) | Phase 2, double-blind, randomised, placebo-controlled; 72 weeks; n=320 | Semaglutide | 0.4 mg | Mean fibrosis stagea,* (SD) | 2.2 (0.6) | 1.7 (0.4) | –0.5 | |
| Mean ELF™ scored,f | 9.9±1.0 | 9.2b | –0.56c | |||||
| Mean VCTE reading, kPae | 11.5±87.1 | 7.68g | –3.82 | |||||
| Placebo | Mean fibrosis stagea,* (SD) | 2.2 (0.6) | 2.0 (0.4) | –0.2 | ||||
| Mean ELF™ scored,f | 9.6±0.9 | 9.77b | 0.01c | |||||
| Mean VCTE reading, kPae | 8.7±90.0 | 10.84g | 2.14b | |||||
| Friedman et al. [64] (2018) | Phase 2b, double- blind, randomised, placebo-controlled; 52 weeks; n=288 | Cenicriviroc | 150 mg | Mean fibrosis stage* (SD) | 2.1 (0.5) | 1.9 (0.4) | –0.2 | |
| Median NFS score (min, max) | –0.942 (–4.55, 1.27) | –0.942 (–4.55, 1.27) | –0.942 (–4.55, 1.27) | |||||
| Median FIB-4 score (min, max) | 1.239 (0.38, 4.20) | 1.375 (0.42, 5.26) | 0.080 (–1.81, 2.38) | |||||
| Median APRI score, (min, max) | 0.470 (0.20, 3.12) | 0.539 (0.15, 3.45) | 0.024 (–1.30, 1.49) | |||||
| Median ELF™§ (min, max) | –0.892 (–2.70, 1.27) | –0.828 (–2.50, 1.08) | 0.023 (–1.98, 1.65) | |||||
| Placebo | Mean fibrosis score* (SD) | 2.0 (0.5) | 2.1 (0.4) | 0.1 | ||||
| Median NFS score (min, max) | –1.223 (–4.81, 2.46) | –1.190 (–4.27, 2.34) | 0.102 (–1.74, 1.37) | |||||
| Median FIB-4 score (min, max) | 1.303 (0.40, 4.14) | 1.242 (0.36, 5.32) | 0.006 (–1.18, 3.11) | |||||
| Median APRI score, (min, max) | 0.568 (0.15, 2.26) | 0.538 (0.13, 3.71) | –0.031 (–0.82, 3.46) | |||||
| Median ELF™§(min, max) | –0.893 (–2.20, 1.62) | –1.003 (–2.53, 2.07) | –0.113 (–1.21, 1.60) | |||||
| Francque et al. [65] (2021) | Phase 2b, double-blind, randomised, placebo-controlled; 24 weeks; n=247 | Lanifibranor | 1,200 mg | Mean fibrosis score (SD)d,h,* | 2.1±0.8 | NR | NR | |
| Median ELF™ scorei (IQR) | NR | NR | 0.11 (–0.04 to 0.26) | |||||
| Median FIB-4 (IQR) | NR | NR | 0.03 (–0.13 to 0.19) | |||||
| Median PRO-C3, μg/L (IQR) | NR | NR | –1.79 (–3.07 to –0.52) | |||||
| Mean VCTE reading, kPa (SD) | 9.99 (5.46) | NR | –1.01 (3.88) | |||||
| Placebo | Mean fibrosis score (SD)d,h,* | 2.0±0.8 | NR | NR | ||||
| Median ELF™ scorei (IQR) | NR | NR | –0.08 (–0.23 to 0.06) | |||||
| Median FIB-4 (IQR) | NR | NR | 0.03 (–0.19 to 0.13) | |||||
| Median PRO-C3, μg/L (IQR) | NR | NR | –1.01 (–2.30 to 0.28) | |||||
| Mean VCTE reading, kPa (SD) | 9.96 (4.89) | NR | –0.66 (3.04) | |||||
| Harrison et al. [66] (2020) | Phase 2b, double-blind, randomised, placebo-controlled; 52 weeks; n=392 | MSDC-0602K | 250 mg | Mean fibrosis stagea,* (SD) | 2.10 (0.53) | NR | –0.1 | Reported as: the average effect of the combined highest doses relative to placebo on ELF™ FIB-4, FibroTest®, and CK-18 was a reduction of 0.21 (95% CI −0.39 to −0.03) SDs at 6 months and 0.17 (95% CI −0.37 to 0.02) SDs at 12 months. |
| Mean APRI score (SD) | 0.604 (0.4385) | NR | ||||||
| Mean ELF™ score (SD) | 9.80 (1.052) | NR | ||||||
| Mean FIB-4 score (SD) | 1.58 (0.909) | NR | ||||||
| Mean FibroTest® (SD) | 0.33 (0.192) | NR | ||||||
| Placebo | Mean fibrosis stagea,* (SD) | 2.2 (0.6) | NR | 0.1 | ||||
| Mean APRI score (SD) | 0.540 (0.2896) | NR | ||||||
| Mean ELF™ score (SD) | 9.6 (0.850) | NR | ||||||
| Mean FIB-4 score (SD) | 1.38 (0.688) | NR | ||||||
| Mean FibroTest® (SD) | 0.31 (0.197) | NR | ||||||
| Armstrong et al. [67] (2016) | Phase 2, double-blind, randomised, placebo-controlled; 48 weeks; n=52 | Liraglutide | 1.8 mg | Mean fibrosis stage† (SD) | 2.3 (0.9) | NR | –0.2 (0.8) | |
| Mean ELF™ score (SD) | 9.3 (SD) | NR | –0.3 (0.8) | |||||
| Placebo | Mean fibrosis stage† (SD) | 2.3 (1.3) | NR | 0.2 (1.0) | ||||
| Mean ELF™ score (SD) | 9.4 (1.3) | NR | 0.1 (0.8) | |||||
| Chalasani et al. [72] (2020) | Phase 2b, double-blind, randomised, placebo-controlled; 52 weeks; n=162 | Belapectin | 8 mg/kg | Mean fibrosis stagea,‡ (SD) | 4.0b | 3.75a (1.3) | –0.25b | |
| Mean ELF™ score (SD) | 10.64 (1.16) | NR | 0.50 (0.78) | |||||
| Mean FibroTest® score (SD) | NR | NR | 0.01 (0.02) | |||||
| Mean VCTE reading, kPa (SD) | 29.3 (14.9) | NR | –2.34 (10.8) | |||||
| Placebo | Mean fibrosis stagea,‡ (SD) | 4.0b | 3.7a (1.3) | –0.3b | ||||
| Mean ELF™ score (SD) | 10.81 (1.1) | NR | 0.37 (0.63) | |||||
| Mean FibroTest® score (SD) | NR | NR | 0.03 (0.02) | |||||
| Mean VCTE reading, kPa (SD) | 29.9 (17.8) | NR | –0.47 (18.6) | |||||
| Harrison et al. [68] (2021) | Phase 2, double blind, randomised, placebo-controlled; 24 weeks; n=78 | Aldafermin | 1 mg | Mean fibrosis stagea,* (SD) | 2.5a (0.7) | NR | NRj | |
| Mean ELF™ score (SD) | 9.8 (0.8) | NR | –0.2 (0.5) | |||||
| Mean PRO-C3 score, μg/L (SD) | 17.5 (8.4) | NR | –5.4 (6.2) | |||||
| Placebo | Mean fibrosis stagea,* (SD) | 2.4 (0.7) | NR | NRj | ||||
| Mean ELF™ score (SD) | 9.9 (1.0) | NR | 0 (0.6) | |||||
| Mean PRO-C3 score, μg/L (SD) | 17.1 (7.0) | NR | –1.2 (6.2) | |||||
| Harrison et al. [69] (2021) | Phase 2a, double blind, randomised, placebo-controlled; 12 weeks; n=80 | Efruxifermin | 70 mg | Mean fibrosis stagea,* (SD) | 2.0 (0.4) | NR | NR | |
| Mean ELF™ score (SD) | 9.5 (0.8) | NR | 9.3b,k | |||||
| Mean PRO-C3 score, μg/L (SD) | 17.2 (5.9) | NR | 10.0b,k | |||||
| Placebo | Mean fibrosis stagea,* (SD) | 2.0 (0.5) | NR | NR | ||||
| Mean ELF™ score (SD) | 9.5 (1.0) | NR | 9.5b,k | |||||
| Mean PRO-C3 score, μg/L (SD) | 16.1 (6.7) | NR | 15.0b,k | |||||
| Loomba et al. [73] (2021) | Phase 2b, double blind, randomised, placebo-controlled; 48 weeks; n=392 | Cilofexor Firsocostat | Cilofexor 30 mg | Biopsy confirmed F3/F4* | n=76 (98%) | NR | NR | |
| Firsocostat 20 mg | Median ELF™ score (IQR) | 10.0 (9.4, 10.7) | NR | –0.0 (–0.2, 0.20) | ||||
| Median VCTE reading, kPa (IQR) | 15.7 (10.9, 22.2) | NR | –4.2 (–6.5, –1.9) | |||||
| Harrison et al. [70] (2019) | Phase 2, double blind, randomised, placebo-controlled; 36 weeks; n=125 | Resmetriom | 80 mg | Mean fibrosis stagea,* (SD) | 1.6 (0.3) | NR | NR | |
| Mean ELF™ score (SD) | 9.2 (0.9) | NR | –0.38m (0.09) | |||||
| Mean PRO-C3 score, μg/L (SD) | 17.8 (10.3) | NR | –2.2p (2.1); –6.5q (3.5) | |||||
| Placebo | Mean fibrosis stagea,* (SD) | 1.6 (0.3) | NR | NR | ||||
| Mean ELF™ score (SD) | 9.2 (1.0) | NR | 0.02l (0.12) | |||||
| Mean PRO-C3 score, μg/L (SD) | 16.2 (59.0) | NR | 7.4n (3.1); 14.9o (5.6) | |||||
| Ratziu et al. [71] (2016) | Phase 2, double blind, randomised, placebo-controlled; 52 weeks; n=276 | Elafibranor | 120 mg | Mean fibrosis stage* (SD) | 1.7 (0.9) | NR | NR | |
| Mean NFS score (SD) | NR | NR | –0.25b | |||||
| Mean FibroTest® (SD) | NR | NR | –0.07b | |||||
| Placebo | Mean fibrosis stage* (SD) | 1.5 (1.0) | NR | NR | ||||
| Mean NFS score (SD) | NR | NR | –0.01b | |||||
| Mean FibroTest® (SD) | NR | NR | –0.01b | |||||
| Harrison et al. [74] (2020) | Phase III (STELLAR-4), double blind, randomised, placebo-controlled; 48 weeks; n=877 | Selonsertib | 18 mg | Mean fibrosis stagea,* (SD) | 4.0 (1.8) | 3.7 (1.4) | –0.3b | |
| Median ELF™ score (IQR) | 10.61 (10.04 to 11.34) | 10.73 (10.07 to 10.51) | 0.10b | |||||
| Median FibroTest® (IQR) | 0.58 (0.44 to 0.73) | 0.58 (0.40 to 0.75) | NC | |||||
| Median APRI score (IQR) | 0.8 (0.6 to 1.2) | 0.8 (0.5 to 1.3) | NC | |||||
| Median FIB-4 score (IQR) | 2.55 (1.76 to 3.62) | 2.65 (1.74 to 3.76) | 0.10b | |||||
| Median NFS score (IQR) | 0.659 (–0.119 to 1.472) | 0.816 (0.031 to 1.574) | 0.157b | |||||
| Median VCTE reading, kPa (IQR) | 21.10 (14.7 to 28.8) | 19.4 (14.3 to 27.3) | –1.7b | |||||
| Placebo | Mean fibrosis stagea,* (SD) | 3.7 (1.4) | 3.8 (1.5) | 0.10b | ||||
| Median ELF™ score (IQR) | 10.67(10.05 to 11.16) | 10.66 (10.14 to 11.26) | –0.01b | |||||
| Median FibroTest® (IQR) | 0.59 (0.40 to 0.77) | 0.57 (0.39 to 0.73) | –0.02b | |||||
| Median APRI score (IQR) | 0.8 (0.6 to 1.2) | 0.7 (0.5 to 1.2) | –0.1b | |||||
| Median FIB-4 score (IQR) | 2.50 (1.81 to 3.66) | 2.50 (1.65 to 3.67) | NC | |||||
| Median NFS score (IQR) | 0.682 (–0.304 to 1.450) | 0.774 (–0.241 to 1.595) | 0.092b | |||||
| Median VCTE reading, kPa (IQR) | 20.00 (14.4 to 26.7) | 19.30 (13.8 to 26.7) | 0.70b | |||||
| Loomba et al. [75] (2018) | Phase 2, double blind, randomised, de facto placebo-controlled; 24 weeks; n=72 | Selonsertib±Simtuzumab | Selonsertib 18 mg±Simtuzumab | Biopsy confirmed F3* | n=21 (66%) | Improvement n=13 (43%); Cirrhosis n=1 (3%) | ||
| Median ELF™ score (IQR) | NR | NR | 0.02 (–0.34 to 0.52) | |||||
| Median FibroTest® (IQR) | NR | NR | –0.01 (–0.03 to 0.03) | |||||
| Median VCTE reading, kPa (IQR) | NR | NR | 0.2 (–3.50 to 1.40) | |||||
| Simtuzumab | Biopsy confirmed F3* | n=6 (60%) | Improvement n=2 (20%); Cirrhosis n=2 (20%) | |||||
| Median ELF™ score (IQR) | NR | NR | –0.13 (–0.35 to 0.05) | |||||
| Median FibroTest® (IQR) | NR | NR | 0.01 (–0.04 to 0.05) | |||||
| Median VCTE reading, kPa (IQR) | NR | NR | –0.50 (–3.80 to 3.4) |
NR, not reported; NC, no change; ELF™, enhanced liver fibrosis; FIB-4, fibrosis-4; NFS, NAFLD fibrosis score; APRI, aspartate transaminase to platelet ratio index; PRO-C3, Type III collagen marker of the N-terminal pro-peptide; SD, standard deviation; IQR, interquartile range; VCTE, vibration controlled transient elastography.
Mean not provided, calculation made using data provided in the manuscript tables and supplementary information.
No standard deviation/IQR reported.
Change in biomarker score is the change reported in the research paper and not the exact difference between baseline and follow-up.56
Plus-minus values are means±SD.
Plus-minus values are geometric means±coefficient of variation.
An ELF™ score greater than 9.8 indicates a moderate risk of advanced fibrosis, and a score of greater than 11.3 denotes a high risk of advanced fibrosis.
No geometric means±coefficient of variation reported.
Fibrosis stage was classified according to the SAF-NASH CRN staging system.
An ELF™ score of less than 7.7 indicates none to mild fibrosis, and a score of 11.3 or greater indicates cirrhosis.
Improvement/no improvement or worsening reported, unable to calculate changes in fibrosis stage as data is not provided.
Estimated values only, exact values not recorded, data taken from manuscript62 Figure 3, (F) and (G).
Mean difference reported for subjects with ELF™ ≥9.0 only (n=21) at week 12.
Mean difference reported for subjects with ELF™ ≥9.0 only (n=40) at week 12.
Mean difference reported for subjects with baseline ≥10.00 ng/mL (n=25).
Mean difference reported for subjects with baseline ≥17.50 ng/mL (n=12).
Mean difference reported for subjects with baseline ≥10.00 ng/mL (n=53).
Mean difference reported for subjects with baseline ≥17.50 ng/mL (n=29).
Biopsy confirmed fibrosis stages using NASH CRN scoring system.
Biopsy confirmed fibrosis stages using Kleiner scoring system.
Biopsy confirmed cirrhosis using Ishak scoring system.
Data for baseline, follow up and change in ELF™ score taken from Supplementary Table 6.57
CONCLUSION
The current use of widely available noninvasive serum biomarkers for fibrosis in NAFLD continues to be used to identify patients who have a high probability of ≥F3 fibrosis in settings where there is a high prevalence of more severe liver disease. It remains uncertain whether biomarkers have sufficient sensitivity and specificity to be able to monitor progression in fibrosis, or amelioration of fibrosis with therapeutic interventions. Although there is a recognized need to identify fibrosis earlier in the disease process, no single biomarker has been shown to be accurate or precise enough to identify patients with F2 liver fibrosis. Increased liver fibrosis biomarker scores are associated with liver-related morbidity and mortality and also associated with an increased risk of non-liver related patient outcomes. Currently, there is an insufficient evidence to demonstrate that a change in a biomarker score allows prediction of a change in liver fibrosis. Finally, we consider that it is now crucial to develop biomarkers that accurately and precisely identify F2, and to continue to investigate whether biomarkers can be used for assessing and monitoring disease progression/regression with therapeutic interventions that include both drugs and lifestyle change (Fig. 2).
Figure 2.
The future of noninvasive serum biomarkers for fibrosis in NAFLD. NAFLD, non-alcoholic fatty liver disease.
Acknowledgments
For the purpose of Open Access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising from this submission. The authors would like to thank the NIHR Southampton Biomedical Research Centre and the University of Southampton for their support.
CDB and RMB are supported in part by the Southampton NIHR Biomedical Research Centre (IS-BRC-20004), UK.
Abbreviations
- APRI
aspartate transaminase to platelet ratio index
- AUC
area under the curve
- CI
confidence interval
- CVD
cardio vascular disease
- ELF™
enhanced liver fibrosis test
- FDA
Food and Drug Administration
- FIB-4
fibrosis-4 index
- GLP-1
glucagon-like peptide-1
- METAVIR
meta-analysis of histological data in viral hepatitis
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steohepatitis
- NFS
NAFLD fibrosis score
- NPV
negative predictive value
- PPV
positive predictive value
- PRO-C3
type III collagen marker of the N-terminal pro-peptide
- VCTE
vibration controlled transient elastography
Footnotes
Authors’ contribution
All authors (Tina Reinson, Ryan M. Buchanan, and Christopher D. Byrne) contributed to the review structure and concept; drafting of the manuscript and its critical revision; and approved the final version.
Conflicts of Interest
The authors have no conflicts to disclose.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Clinical and Molecular Hepatology website http://www.e-cmh.org).
Brief summary of the 21 therapeutic drug trials examined in Ampuero et al.’s 2022 meta-analysis of variables influencing the interpretation of clinical trial results in NAFLD[22]
Comparison between change in noninvasive serum biomarkers and change in liver fibrosis assessed by liver histology, in therapeutic trials of nonalcoholic steatohepatitis (NASH)
REFERENCES
- 1.Wu W, Feng A, Ma W, Li D, Zheng S, Xu F, et al. Worldwide longterm trends in the incidence of nonalcoholic fatty liver disease during 1990-2019: a joinpoint and age-period-cohort analysis. Front Cardiovasc Med. 2022;9:891963. doi: 10.3389/fcvm.2022.891963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-metaanalytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 3.Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 4.Thoma C, Day CP, Trenell MI. Lifestyle interventions for the treatment of non-alcoholic fatty liver disease in adults: a systematic review. J Hepatol. 2012;56:255–266. doi: 10.1016/j.jhep.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Katsagoni CN, Georgoulis M, Papatheodoridis GV, Panagiotakos DB, Kontogianni MD. Effects of lifestyle interventions on clinical characteristics of patients with non-alcoholic fatty liver disease: a meta-analysis. Metabolism. 2017;68:119–132. doi: 10.1016/j.metabol.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Romero-Gómez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67:829–846. doi: 10.1016/j.jhep.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Lee KC, Wu PS, Lin HC. Pathogenesis and treatment of nonalcoholic steatohepatitis and its fibrosis. Clin Mol Hepatol. 2012 Oct 13; doi: 10.3350/cmh.2022.0237. doi: 10.3350/cmh.2022.0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newsome PN, Cramb R, Davison SM, Dillon JF, Foulerton M, Godfrey EM, et al. Guidelines on the management of abnormal liver blood tests. Gut. 2018;67:6–19. doi: 10.1136/gutjnl-2017-314924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gheorghe G, Bungău S, Ceobanu G, Ilie M, Bacalbaşa N, Bratu OG, et al. The non-invasive assessment of hepatic fibrosis. J Formos Med Assoc. 2021;120:794–803. doi: 10.1016/j.jfma.2020.08.019. [DOI] [PubMed] [Google Scholar]
- 10.Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, et al. The prevalence and incidence of NAFLD worldwide:a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2022;7:851–861. doi: 10.1016/S2468-1253(22)00165-0. [DOI] [PubMed] [Google Scholar]
- 11.Gaidos JK, Hillner BE, Sanyal AJ. A decision analysis study of the value of a liver biopsy in nonalcoholic steatohepatitis. Liver Int. 2008;28:650–658. doi: 10.1111/j.1478-3231.2008.01693.x. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberg WM, Voelker M, Thiel R, Becka M, Burt A, Schuppan D, et al. Serum markers detect the presence of liver fibrosis: a cohort study. Gastroenterology. 2004;127:1704–1713. doi: 10.1053/j.gastro.2004.08.052. [DOI] [PubMed] [Google Scholar]
- 13.Vallet-Pichard A, Mallet V, Nalpas B, Verkarre V, Nalpas A, Dhalluin-Venier V, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology. 2007;46:32–36. doi: 10.1002/hep.21669. [DOI] [PubMed] [Google Scholar]
- 14.Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–854. doi: 10.1002/hep.21496. [DOI] [PubMed] [Google Scholar]
- 15.Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38:518–526. doi: 10.1053/jhep.2003.50346. [DOI] [PubMed] [Google Scholar]
- 16.Poynard T, Imbert-Bismut F, Munteanu M, Messous D, Myers RP, Thabut D, et al. Overview of the diagnostic value of biochemical markers of liver fibrosis (FibroTest, HCV FibroSure) and necrosis (ActiTest) in patients with chronic hepatitis C. Comp Hepatol. 2004;3:8. doi: 10.1186/1476-5926-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anstee QM, Lawitz EJ, Alkhouri N, Wong VW, Romero-Gomez M, Okanoue T, et al. Noninvasive tests accurately identify advanced fibrosis due to NASH: baseline data from the STELLAR trials. Hepatology. 2019;70:1521–1530. doi: 10.1002/hep.30842. [DOI] [PubMed] [Google Scholar]
- 18.Petta S, Wong VW, Cammà C, Hiriart JB, Wong GL, Vergniol J, et al. Serial combination of non-invasive tools improves the diagnostic accuracy of severe liver fibrosis in patients with NAFLD. Aliment Pharmacol Ther. 2017;46:617–627. doi: 10.1111/apt.14219. [DOI] [PubMed] [Google Scholar]
- 19. National institute for Health and Care Excellence (NICE). How should I assess a person with NAFLD 2021. NICE website, < https://cks.nice.org.uk/topics/non-alcoholic-fatty-liverdisease-nafld/diagnosis/assessment/>. Accessed 25 Oct 2022. System Requirements: NICE website has only been made available to people living in the UK.
- 20. National Institute for Health and Care Excellence (NICE). Nonalcoholic fatty liver disease (NAFLD): assessment and management. NICE website, < https://www.nice.org.uk/guidance/ng49>. Accessed 25 Oct 2022.
- 21.Kang SH, Lee HW, Yoo JJ, Cho Y, Kim SU, Lee TH, et al. KASL clinical practice guidelines: Management of nonalcoholic fatty liver disease. Clin Mol Hepatol. 2021;27:363–401. doi: 10.3350/cmh.2021.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Byrne CD, Targher G. Non-alcoholic fatty liver disease-related risk of cardiovascular disease and other cardiac complications. Diabetes Obes Metab. 2022;24(Suppl 2):28–43. doi: 10.1111/dom.14484. [DOI] [PubMed] [Google Scholar]
- 23.Mantovani A, Byrne CD, Targher G. Efficacy of peroxisome proliferator-activated receptor agonists, glucagon-like peptide-1 receptor agonists, or sodium-glucose cotransporter-2 inhibitors for treatment of non-alcoholic fatty liver disease: a systematic review. Lancet Gastroenterol Hepatol. 2022;7:367–378. doi: 10.1016/S2468-1253(21)00261-2. [DOI] [PubMed] [Google Scholar]
- 24.Reinson T, Byrne CD, Patel J, El-Gohary M, Moore M. Transient elastography in patients at risk of liver fibrosis in primary care: a follow-up study over 54 months. BJGP Open. 2021;5:BJGPO.2021.0145. doi: 10.3399/BJGPO.2021.0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Asbaghi O, Choghakhori R, Ashtary-Larky D, Abbasnezhad A. Effects of the Mediterranean diet on cardiovascular risk factors in non-alcoholic fatty liver disease patients: a systematic review and meta-analysis. Clin Nutr ESPEN. 2020;37:148–156. doi: 10.1016/j.clnesp.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 26.Baker CJ, Martinez-Huenchullan SF, D’Souza M, Xu Y, Li M, Bi Y, et al. Effect of exercise on hepatic steatosis: are benefits seen without dietary intervention? a systematic review and metaanalysis. J Diabetes. 2021;13:63–77. doi: 10.1111/1753-0407.13086. [DOI] [PubMed] [Google Scholar]
- 27.Younossi ZM, Ratziu V, Loomba R, Rinella M, Anstee QM, Goodman Z, et al. Obeticholic acid for the treatment of nonalcoholic steatohepatitis: interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial. Lancet. 2019;394:2184–2196. doi: 10.1016/S0140-6736(19)33041-7. [DOI] [PubMed] [Google Scholar]
- 28.Rezaei S, Tabrizi R, Nowrouzi-Sohrabi P, Jalali M, Atkin SL, AlRasadi K, et al. GLP-1 receptor agonist effects on lipid and liver profiles in patients with nonalcoholic fatty liver disease: systematic review and meta-analysis. Can J Gastroenterol Hepatol. 2021;2021:8936865. doi: 10.1155/2021/8936865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Soon G, Wee A. Updates in the quantitative assessment of liver fibrosis for nonalcoholic fatty liver disease: histological perspective. Clin Mol Hepatol. 2021;27:44–57. doi: 10.3350/cmh.2020.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reinson T. Performance of the enhanced liver fibrosis (ELF) score, comparison with vibration-controlled transient elastography (VCTE) data, and development of a simple algorithm to predict significant liver fibrosis in a community-based liver service: a retrospective evaluation. Journal of Clinical and Translational Hepatology. doi: 10.14218/JCTH.2022.00335. Forthcoming 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317–1325. doi: 10.1002/hep.21178. [DOI] [PubMed] [Google Scholar]
- 32.Xiao G, Zhu S, Xiao X, Yan L, Yang J, Wu G. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: a meta-analysis. Hepatology. 2017;66:1486–1501. doi: 10.1002/hep.29302. [DOI] [PubMed] [Google Scholar]
- 33.Vali Y, Lee J, Boursier J, Spijker R, Verheij J, Brosnan MJ, et al. FibroTest for evaluating fibrosis in non-alcoholic fatty liver disease patients: a systematic review and meta-analysis. J Clin Med. 2021;10:2415. doi: 10.3390/jcm10112415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Critical Appraisal Lowdown (CAL). Likelihood ratios & area under the curve. CAL website, < https://www.criticalappraisallowdown.co.uk/lessons/likelihood-ratios-area-under-the-curve/>. Accessed 25 Oct 2022.
- 35.Vali Y, Lee J, Boursier J, Spijker R, Löffler J, Verheij J, et al. Enhanced liver fibrosis test for the non-invasive diagnosis of fibrosis in patients with NAFLD: a systematic review and metaanalysis. J Hepatol. 2020;73:252–262. doi: 10.1016/j.jhep.2020.03.036. [DOI] [PubMed] [Google Scholar]
- 36.Mak AL, Lee J, van Dijk AM, Vali Y, Aithal GP, Schattenberg JM, et al. Systematic review with meta-analysis: diagnostic accuracy of Pro-C3 for hepatic fibrosis in patients with non-alcoholic fatty liver disease. Biomedicines. 2021;9:1920. doi: 10.3390/biomedicines9121920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sripongpun P, Kim WR, Mannalithara A, Charu V, Vidovszky A, Asch S, et al. The steatosis-associated fibrosis estimator (SAFE) score: a tool to detect low-risk NAFLD in primary care. Hepatology. 2022 Apr 28; doi: 10.1002/hep.32545. doi: 10.1002/hep.32545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blanes-Vidal V, Lindvig KP, Thiele M, Nadimi ES, Krag A. Artificial intelligence outperforms standard blood-based scores in identifying liver fibrosis patients in primary care. Sci Rep. 2022;12:2914. doi: 10.1038/s41598-022-06998-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carteri RB, Grellert M, Borba DL, Marroni CA, Fernandes SA. Machine learning approaches using blood biomarkers in non-alcoholic fatty liver diseases. Artif Intell Gastroenterol. 2022;3:80–87. [Google Scholar]
- 40.Wong GL, Yuen PC, Ma AJ, Chan AW, Leung HH, Wong VW. Artificial intelligence in prediction of non-alcoholic fatty liver disease and fibrosis. J Gastroenterol Hepatol. 2021;36:543–550. doi: 10.1111/jgh.15385. [DOI] [PubMed] [Google Scholar]
- 41.Angulo P, Kleiner DE, Dam-Larsen S, Adams LA, Bjornsson ES, Charatcharoenwitthaya P, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149:389–397. doi: 10.1053/j.gastro.2015.04.043. e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taylor RS, Taylor RJ, Bayliss S, Hagström H, Nasr P, Schattenberg JM, et al. Association between fibrosis stage and outcomes of patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis. Gastroenterology. 2020;158:1611–1625. doi: 10.1053/j.gastro.2020.01.043. e12. [DOI] [PubMed] [Google Scholar]
- 43.Peleg N, Sneh Arbib O, Issachar A, Cohen-Naftaly M, Braun M, Shlomai A. Noninvasive scoring systems predict hepatic and extra-hepatic cancers in patients with nonalcoholic fatty liver disease. PLoS One. 2018;13:e0202393. doi: 10.1371/journal.pone.0202393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ito T, Ishigami M, Ishizu Y, Kuzuya T, Honda T, Hayashi K, et al. Utility and limitations of noninvasive fibrosis markers for predicting prognosis in biopsy-proven Japanese non-alcoholic fatty liver disease patients. J Gastroenterol Hepatol. 2019;34:207–214. doi: 10.1111/jgh.14448. [DOI] [PubMed] [Google Scholar]
- 45.Lee J, Vali Y, Boursier J, Spijker R, Anstee QM, Bossuyt PM, et al. Prognostic accuracy of FIB-4, NAFLD fibrosis score and APRI for NAFLD-related events: a systematic review. Liver Int. 2021;41:261–270. doi: 10.1111/liv.14669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cianci N, Subhani M, Hill T, Khanna A, Zheng D, Sheth A, et al. Prognostic non-invasive biomarkers for all-cause mortality in non-alcoholic fatty liver disease: a systematic review and metaanalysis. World J Hepatol. 2022;14:1025–1037. doi: 10.4254/wjh.v14.i5.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Allen AM, Therneau TM, Ahmed OT, Gidener T, Mara KC, Larson JJ, et al. Clinical course of non-alcoholic fatty liver disease and the implications for clinical trial design. J Hepatol. 2022;77:1237–1245. doi: 10.1016/j.jhep.2022.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Parkes J, Roderick P, Harris S, Day C, Mutimer D, Collier J, et al. Enhanced liver fibrosis test can predict clinical outcomes in patients with chronic liver disease. Gut. 2010;59:1245–1251. doi: 10.1136/gut.2009.203166. [DOI] [PubMed] [Google Scholar]
- 49. Bloomberg. FDA grants marketing authorization to siemens healthineers ELF test for NASH prognostic assessment. Bloomberg website, < https://www.bloomberg.com/press-releases/2021-08-24/fda-grants-marketing-authorization-to-siemens-healthineers-elf-test-for-nash-prognostic-assessment>. Accessed 25 Oct 2022.
- 50. Siemens Healthineers. The ELF test as a universally available prognostic tool for enhancing NASH patient care. Siemens Healthineers website, < https://www.siemens-healthineers.com/laboratory-diagnostics/assays-by-diseases-conditions/liver-disease/elf-test-educational-videos/elf-test-as-universallyavailable-prognostic-tool-for-enhancing-nash-patient-care>.Accessed 25 October 2022.
- 51.Hagström H, Talbäck M, Andreasson A, Walldius G, Hammar N. Repeated FIB-4 measurements can help identify individuals at risk of severe liver disease. J Hepatol. 2020;73:1023–1029. doi: 10.1016/j.jhep.2020.06.007. [DOI] [PubMed] [Google Scholar]
- 52.Balkhed W, Åberg FO, Nasr P, Ekstedt M, Kechagias S. Repeated measurements of non-invasive fibrosis tests to monitor the progression of non-alcoholic fatty liver disease: a long-term follow-up study. Liver Int. 2022;42:1545–1556. doi: 10.1111/liv.15255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim HY. Recent advances in nonalcoholic fatty liver disease metabolomics. Clin Mol Hepatol. 2021;27:553–559. doi: 10.3350/cmh.2021.0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu G, Wang YM, Ying MM, Chen SD, Li ZR, Ma HL, et al. Serum lipocalin-2 is a potential biomarker for the clinical diagnosis of nonalcoholic steatohepatitis. Clin Mol Hepatol. 2021;27:329–345. doi: 10.3350/cmh.2020.0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ampuero J, Gallego-Durán R, Maya-Miles D, Montero R, Gato S, Rojas Á, et al. Systematic review and meta-analysis: analysis of variables influencing the interpretation of clinical trial results in NAFLD. J Gastroenterol. 2022;57:357–371. doi: 10.1007/s00535-022-01860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Harrison SA, Goodman Z, Jabbar A, Vemulapalli R, Younes ZH, Freilich B, et al. A randomized, placebo-controlled trial of emricasan in patients with NASH and F1-F3 fibrosis. J Hepatol. 2020;72:816–827. doi: 10.1016/j.jhep.2019.11.024. [DOI] [PubMed] [Google Scholar]
- 57.Neuschwander-Tetri BA, Loomba R, Sanyal AJ, Lavine JE, Van Natta ML, Abdelmalek MF, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebocontrolled trial. Lancet. 2015;385:956–965. doi: 10.1016/S0140-6736(14)61933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sanyal AJ, Chalasani N, Kowdley KV, McCullough A, Diehl AM, Bass NM, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;362:1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cusi K, Orsak B, Bril F, Lomonaco R, Hecht J, Ortiz-Lopez C, et al. Long-term pioglitazone treatment for patients with nonalcoholic steatohepatitis and prediabetes or type 2 diabetes mellitus: a randomized trial. Ann Intern Med. 2016;165:305–315. doi: 10.7326/M15-1774. [DOI] [PubMed] [Google Scholar]
- 60.Ratziu V, de Guevara L, Safadi R, Poordad F, Fuster F, FloresFigueroa J, et al. One-year results of the global phase 2b randomized placebo-controlled ARREST trial of aramchol, a stearoyl CoA desaturasemodulator in NASH patients. The Liver Meeting 2018. 2018 Nov;:9–13. San Francisco, CA. [Google Scholar]
- 61.Harrison SA, Ratziu V, Bedossa P, Dufour JF, Kruger F, Schattenberg M, et al. RESOLVE-IT phase 3 of elafibranor in NASH: final results of the week 72 interim surrogate efficacy analysis. The Liver Meeting Digital Experience 2020. 2020 Nov;:11–16. [Google Scholar]
- 62.Harrison SA, Gunn NT, Khazanchi A, Guy CD, Brunt EM, Moussa S, et al. A 52-week multi-center double-blind randomized phase 2 study of seladelpar, a potent and selective peroxisome proliferator- activated receptor delta (PPAR-delta) agonist, in patients with nonalcoholic steatohepatitis (NASH) The Liver Meeting Digital Experience 2020. 2020 Nov;:11–16. [Google Scholar]
- 63.Newsome PN, Buchholtz K, Cusi K, Linder M, Okanoue T, Ratziu V, et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med. 2021;384:1113–1124. doi: 10.1056/NEJMoa2028395. [DOI] [PubMed] [Google Scholar]
- 64.Friedman SL, Ratziu V, Harrison SA, Abdelmalek MF, Aithal GP, Caballeria J, et al. A randomized, placebo-controlled trial of cenicriviroc for treatment of nonalcoholic steatohepatitis with fibrosis. Hepatology. 2018;67:1754–1767. doi: 10.1002/hep.29477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Francque SM, Bedossa P, Ratziu V, Anstee QM, Bugianesi E, Sanyal AJ, et al. A randomized, controlled trial of the Pan-PPAR agonist lanifibranor in NASH. N Engl J Med. 2021;385:1547–1558. doi: 10.1056/NEJMoa2036205. [DOI] [PubMed] [Google Scholar]
- 66.Harrison SA, Alkhouri N, Davison BA, Sanyal A, Edwards C, Colca JR, et al. Insulin sensitizer MSDC-0602K in non-alcoholic steatohepatitis: a randomized, double-blind, placebo-controlled phase IIb study. J Hepatol. 2020;72:613–626. doi: 10.1016/j.jhep.2019.10.023. [DOI] [PubMed] [Google Scholar]
- 67.Armstrong MJ, Gaunt P, Aithal GP, Barton D, Hull D, Parker R, et al. Liraglutide safety and efficacy in patients with nonalcoholic steatohepatitis (LEAN): a multicentre, doubleblind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387:679–690. doi: 10.1016/S0140-6736(15)00803-X. [DOI] [PubMed] [Google Scholar]
- 68.Harrison SA, Neff G, Guy CD, Bashir MR, Paredes AH, Frias JP, et al. Efficacy and safety of aldafermin, an engineered FGF19 analog, in a randomized, double-blind, placebo-controlled trial of patients with nonalcoholic steatohepatitis. Gastroenterology. 2021;160:219–231. doi: 10.1053/j.gastro.2020.08.004. e1. [DOI] [PubMed] [Google Scholar]
- 69.Harrison SA, Ruane PJ, Freilich BL, Neff G, Patil R, Behling CA, et al. Efruxifermin in non-alcoholic steatohepatitis: a randomized, double-blind, placebo-controlled, phase 2a trial. Nat Med. 2021;27:1262–1271. doi: 10.1038/s41591-021-01425-3. [DOI] [PubMed] [Google Scholar]
- 70.Harrison SA, Bashir MR, Guy CD, Zhou R, Moylan CA, Frias JP, et al. Resmetirom (MGL-3196) for the treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2019;394:2012–2024. doi: 10.1016/S0140-6736(19)32517-6. [DOI] [PubMed] [Google Scholar]
- 71.Ratziu V, Harrison SA, Francque S, Bedossa P, Lehert P, Serfaty L, et al. Elafibranor, an agonist of the peroxisome proliferatoractivated receptor-α and -δ, induces resolution of nonalcoholic steatohepatitis without fibrosis worsening. Gastroenterology. 2016;150:1147–1159. doi: 10.1053/j.gastro.2016.01.038. e5. [DOI] [PubMed] [Google Scholar]
- 72.Chalasani N, Abdelmalek MF, Garcia-Tsao G, Vuppalanchi R, Alkhouri N, Rinella M, et al. Effects of belapectin, an inhibitor of galectin-3, in patients with nonalcoholic steatohepatitis with cirrhosis and portal hypertension. Gastroenterology. 2020;158:1334–1345. doi: 10.1053/j.gastro.2019.11.296. e5. [DOI] [PubMed] [Google Scholar]
- 73.Loomba R, Noureddin M, Kowdley KV, Kohli A, Sheikh A, Neff G, et al. Combination therapies including cilofexor and firsocostat for bridging fibrosis and cirrhosis attributable to NASH. Hepatology. 2021;73:625–643. doi: 10.1002/hep.31622. [DOI] [PubMed] [Google Scholar]
- 74.Harrison SA, Wong VW, Okanoue T, Bzowej N, Vuppalanchi R, Younes Z, et al. Selonsertib for patients with bridging fibrosis or compensated cirrhosis due to NASH: results from randomized phase III STELLAR trials. J Hepatol. 2020;73:26–39. doi: 10.1016/j.jhep.2020.02.027. [DOI] [PubMed] [Google Scholar]
- 75.Loomba R, Lawitz E, Mantry PS, Jayakumar S, Caldwell SH, Arnold H, et al. The ASK1 inhibitor selonsertib in patients with nonalcoholic steatohepatitis: a randomized, phase 2 trial. Hepatology. 2018;67:549–559. doi: 10.1002/hep.29514. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Brief summary of the 21 therapeutic drug trials examined in Ampuero et al.’s 2022 meta-analysis of variables influencing the interpretation of clinical trial results in NAFLD[22]
Comparison between change in noninvasive serum biomarkers and change in liver fibrosis assessed by liver histology, in therapeutic trials of nonalcoholic steatohepatitis (NASH)