Abstract
Non-alcoholic fatty liver disease (NAFLD) is a chronic liver disease characterized by excess fat accumulation in the liver. It is closely associated with metabolic syndrome, and patients with NAFLD often have comorbidities such as obesity, type 2 diabetes mellitus, and dyslipidemia. In addition to liver-related complications, NAFLD has been associated with a range of non-liver comorbidities, including cardiovascular disease, chronic kidney disease, and sleep apnea. Cardiovascular disease is the most common cause of mortality in patients with NAFLD, and patients with NAFLD have a higher risk of developing cardiovascular disease than the general population. Chronic kidney disease is also more common in patients with NAFLD, and the severity of NAFLD is associated with a higher risk of developing chronic kidney disease. Sleep apnea, a disorder characterized by breathing interruptions during sleep, is also more common in patients with NAFLD and is associated with the severity of NAFLD. The presence of non-liver comorbidities in patients with NAFLD has important implications for the management of this disease. Treatment of comorbidities such as obesity, type 2 diabetes mellitus, and dyslipidemia may improve liver-related outcomes in patients with NAFLD. Moreover, treatment of non-liver comorbidities may also improve overall health outcomes in patients with NAFLD. Therefore, clinicians should be aware of the potential for non-liver comorbidities in patients with NAFLD and should consider the management of these comorbidities as part of the overall management of this disease.
Keywords: Nonalcoholic fatty liver disease, Comorbidity
INTRODUCTION
As the incidence and prevalence of nonalcoholic fatty liver disease (NAFLD) continues to increase worldwide, the association of NAFLD with other comorbid conditions is an area of increasing interest and research [1-9]. In several studies, NAFLD has been found to be an independent risk factor for adverse outcomes, including mortality [10], even after controlling for other known risk factors. However, the relationship of NAFLD to other comorbid conditions is still under investigation, especially when trying to understand whether these conditions coexist or if one causes the other. Furthermore, the presence of fibrosis complicates this relationship as when fibrosis is present, it becomes the number one predictor of mortality [11-19]. Nonetheless, having an understanding of what comorbidities are often associated with NAFLD is important so that proper treatment can be forthcoming. Therefore, the following will provide a brief review of these conditions (Fig. 1) and the current evidence regarding each association.
Figure 1.
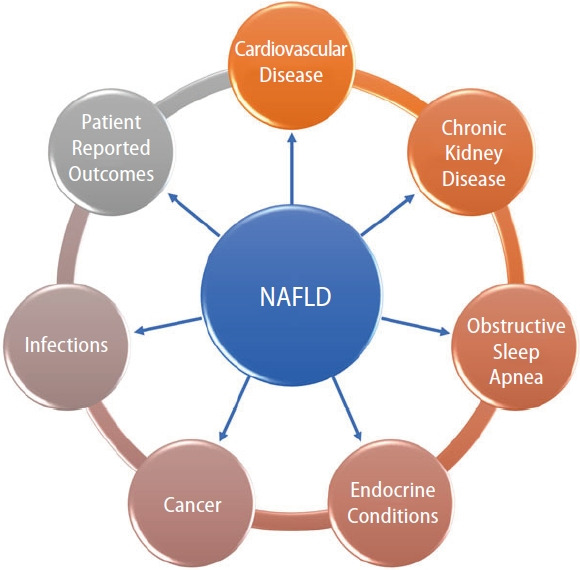
The Multisystem Impact of nonalcoholic fatty liver disease (NAFLD).
CARDIOVASCULAR DISEASE
Ischemic heart disease
The most common cause of death in patients with NAFLD is the spectrum of cardiovascular disease (CVD) comprising coronary artery disease, angina, and ischemic stroke. The incidence of CVD in NAFLD has been estimated to be as high as 100.6 per 1,000 person-years [20]. Though it appears clear that the two conditions are associated, the proof for NAFLD being an independent cause of CVD has not been borne out by the evidence [21]. The absence of a causative link, however, may be due to a lack of data in stratifying CVD in relation to the level of fibrosis. NAFLD does appear to increase the overall risk of CVD, but it is not yet clear if it increases mortality caused by CVD. A meta-analysis of 16 studies showed that NAFLD significantly increased the risk of non-fatal cardiovascular events with an odds ratio (OR) of 2.52 when compared to patients without NAFLD, but no significant relationship was found between NAFLD and the risk of fatal cardiovascular outcomes. However, if severe NAFLD was assessed, as defined by fatty liver on imaging with either increased gamma-glutamyltransferase (GGT) or elevated NAFLD fibrosis score or positron emission tomography showing increased fluorodeoxyglucose (FDG) uptake or worsening fibrosis on pathology, then there was a higher risk of CVD mortality with an OR of 3.28 when compared to patients without NAFLD [22].
Pathophysiologically, the metabolic syndrome inflicts widespread end-organ damage which manifests as CVD and NAFLD. The mechanism is thought to be related to the accumulation of visceral and ectopic fat leading to the production and release of fat-derived toxic metabolites. These metabolites trigger systemic and local inflammation ultimately resulting in the progression of both NAFLD and CVD [23].
As the mechanisms are similar, the treatment guidelines are shared among the diseases. The American Heart Association has released the “Life’s Simple 7” guidelines with a stated goal of reducing deaths from CVD and stroke by 20%. A recent study conducted among patients with NAFLD using Life’s Simple 7 guidelines did find that if all NAFLD subjects achieved an ideal rating on all 7 of the health metrics, 66% of all-cause deaths and 83% of cardiovascular (CV) deaths were preventable. In fact, among NAFLD subjects, lack of glycemic control (adjusted population attributable fraction [PAF] =28.3% all-cause; 38.1% CV) and hypertension (adjusted PAF of 23% all-cause; 52.8% CV) were the largest mortality contributors while obtaining ideal physical activity level provided an adjusted PAF=13.9% all-cause and 13.8% CV mortality [24].
A Mediterranean style diet has also been proposed as an intervention that may help decrease the incidence of both NAFLD and CVD [25].
However, just recently, the American Health Association updated their Life Simple 7 guidelines to include sleep as a new metric (Life’s Simple 8 guidelines) [26] as well as updating their diet recommendations to include more food groups such as what is found in a Mediterranean style diet and to use non-high density lipoprotein (HDL) cholesterol measurement for lipid quantification. In this light, a recently published study looked at both sleep and fatigue and their impact on NAFLD mortality. Investigators reported that adults with NAFLD and fatigue experienced 2.3-fold higher mortality than adults with NAFLD but without fatigue. In addition, depression, sleep disturbance and CVD were all major predictors of fatigue, while not having a sleep disturbance had an inverse relationship with mortality [27]. As such, the association between NAFLD and CVD is complex which requires a systematic treatment approach as outlined in several recent guidelines [28-35].
Congestive heart failure
As the end-stage phenotype of multiple cardiac conditions, congestive heart failure (CHF) is a widespread threat. Associations have been drawn between the presence of NAFLD and CHF. The risk of incident heart failure in patients with NAFLD is higher than patients without NAFLD with an estimated hazard ratio of 1.75, according to a study from Sweden looking at 10,422 patients over a median follow-up period of 13.6 years [36]. Increased epicardial fat in patients diagnosed with fatty liver leads to abnormal energy metabolism, especially in the left ventricle, despite seemingly normal systolic and diastolic function as measured by echocardiography [37]. Positive correlations are seen between hepatic and myocardial triglyceride content as measured by magnetic resonance. Rijzewijk et al. [38] showed that greater amounts of myocardial fat deposition contribute to left ventricular (LV) diastolic dysfunction, predisposing to heart failure with preserved ejection fraction [38].
In the other well-known phenotype of CHF, heart failure with reduced ejection fraction, NAFLD appears to be an independent risk factor. Even after accounting for obesity, insulin resistance and a suboptimal diet, the presence of NAFLD remains an independent factor contributing to a lower ejection fraction [39]. Using ultrasound and echocardiography, Trovato et al. [39] performed multiple linear regression to compare the presence of fatty liver with ejection fraction and found a statistically significant negative correlation. This deeply concerning finding brings into perspective the much greater risk that these patients with NAFLD face. Further complicating the picture is the population that is not obese yet has underlying fatty liver. High clinical suspicion would be required at the frontlines to find these “lean NAFLD” patients and ensure adequate cardiovascular risk stratification in this population.
The prevalence of NAFLD is 36% in patients with, heart failure with reduced ejection fraction (HFrEF), significantly higher than in the general population. The combination of NAFLD and HFrEF may be particularly troublesome, as these patients are on average younger and have a higher body-mass index, larger LV mass, and greater fibrosis in the LV myocardium [40]. The changes are not all morphologic, as these patients with NAFLD in addition to HFrEF have higher rates of in-hospital and post-discharge all-cause mortality. Advanced fibrosis due to NAFLD is a specific cause of even greater all-cause mortality [41].
Valvular heart disease
Studies have examined the presence of increased cardiac valvular calcification with NAFLD prevalence. Coexisting sclerosis of the aortic valve (AVS) along with calcification of the mitral annulus (MAC) appears to have the strongest correlation, while patients without any valvular calcification are the least likely to have NAFLD. Isolated AVS and isolated MAC have an intermediate probability [42]. These associations are present independent of diabetes, kidney disease, medications and even echocardiographic values. Along with valvular calcification, suboptimal glycemic control and advancing kidney disease were the other independent predictors of valvular calcification, implying common causative pathways [43].
Treatment of valvular heart disease may also become more complicated. Anticoagulants like warfarin are frequently indicated in these patients to prevent thromboembolic events. Patients with NAFLD along with valvular disease are seen to require higher doses of warfarin and even then, they are less likely to stay in the therapeutic range as compared to patients without NAFLD [44].
Ischemic stroke
NAFLD appears to increase the frequency of ischemic stroke though the evidence for it being a potential causative factor has been conflicting. Some earlier smaller studies had not shown a clear association between the two entities [45,46]. However, according to a study from Sweden by Simon et al. [36], patients with NAFLD have a significantly increased risk of incident stroke when compared to patients without NAFLD (hazard ratio of 1.58). A large meta-analysis published in 2022 looking at 64 studies from 1998 to 2016 showed that the more advanced the NAFLD, the higher the risk of ischemic stroke. Mild NAFLD had an OR of 1.47 when compared to ischemic stroke, while moderate NAFLD had an OR of 1.67 and severe NAFLD had an OR of 1.79. Mild, moderate, and severe NAFLD were assessed with the degree of hepatic echogenicity on ultrasound. The authors felt that the data was conclusive enough to suggest the use of carotid intima-media thickness (CIMT), assessed by duplex ultrasonography, as a screening tool for NAFLD [47]. While CIMT is not yet being used by clinicians to check for NAFLD, the relationship does bring into perspective the close ties shared by these conditions.
A smaller study from Korea suggests that the assessment of steatosis alone may not adequately predict risk. It concludes that fibrosis specifically, and not necessarily the degree of steatosis, is what increases the risk of ischemic stroke [48]. The association does not seem to differ based on ethnicity or the type of ischemic stroke [49], though hemorrhagic stroke does not seem to have any relationship with the presence of NAFLD [47].
It does appear that patients who present with an ischemic stroke are more likely to have underlying NAFLD. A recent study from Japan reports that the frequency of NAFLD is nearly 40% in patients with stroke but only 26.4% in the general Japanese population [50]. From a clinical standpoint, patients who have been diagnosed with a new ischemic stroke should have closer follow-up regarding the status of their liver function, as this follow-up is not routinely done at present.
Specific phenotypes of ischemic stroke caused by NAFLD have been considered. Large artery atherosclerosis and small vessel occlusions are most commonly seen in stroke patients with NAFLD, whereas a cardioembolic etiology is less commonly found [51]. Brainstem infarctions may also be more common in this patient population and have a higher risk of progression even after adjusting for comorbidities [52].
Atrial fibrillation
An arrhythmia with already high prevalence in the general population, a diagnosis of NAFLD appears to push it higher. A prospective study from Finland on the Observational Pharmaco-Epidemiology Research & Analysis (OPERA) cohort looked at nearly 1,000 patients and established an independent association between the two conditions even after adjusting for age, sex and the presence of diabetes. The increase in risk was found to be nearly two-fold [53]. Though not directly assessing NAFLD, the Framingham study of 3,700 patients found that higher liver enzymes (aspartate transaminase and alanine transaminase) did correlate with an increased risk of incident atrial fibrillation [54]. At least 4 studies from 2014 to 2017 did suggest that elevated GGT levels were also independently associated with the development of atrial fibrillation. A review on the topic looking at 14 studies and 3 meta-analyses found one study that did not show an association between NAFLD and atrial fibrillation, while all the others suggested that NAFLD is associated with an increased risk of developing atrial fibrillation [55].
Ventricular arrhythmias
Other more immediately dangerous arrhythmias are also being linked to the presence of NAFLD. An excessively prolonged corrected QT (QTc) interval on electrocardiography can often degenerate into ventricular tachyarrhythmias and has been associated with sudden cardiac death [56]. Interestingly, the degree of NAFLD has been found to increase the QTc interval on patient EKGs. A large study of over 30,000 patients from Taiwan found that mild NAFLD increased QTc intervals by 2.55 ms and severe NAFLD increased it by 12.13 ms [57]. Smaller studies have confirmed this association in other parts of the world [58,59]. Clearly, patients with NAFLD would benefit from having a lower threshold for undergoing rhythm monitoring if symptomatic though the evidence does not yet support screening for arrhythmias in NAFLD.
Impact of dyslipidemia treatment
Contrary to what one may hope, treatment of dyslipidemia has not been found to improve NAFLD, though newer targets in the pipeline may be able to alter disease progression. In a study of 2,566 patients, traditional antidyslipidemic treatment, including hydroxy-methyl-glutaryl-coenzyme A reductase (HMG-CoA) reductase inhibitors, did not improve mortality or major adverse cardiovascular events in NAFLD [60]. It is possible that traditional therapies do not account for the specific phenotype of dyslipidemia that exists in NAFLD. A higher plasma apolipoprotein B to apolipoprotein A1 ratio has been found in patients with NAFLD even after taking obesity into account. Patients with NAFLD also have smaller low-density lipoprotein (LDL) particle size.
It is thought that these patients may require different treatment targets, which are currently being researched. Specifically, increasing hepatic fat metabolism is the proposed mechanism of action of resmetirom (MGL-3196), a selective thyroid hormone receptor agonist. This oral medication has shown increased reduction of hepatic fat as measured by magnetic resonance imaging (MRI) in phase 2 clinical trials though a clear mortality benefit is not yet evident [61]. Phase 3 trials confirm that resmetirom is as safe and as well tolerated as placebo while significantly improving liver transaminases and fibrosis biomarkers in addition to proton-density fat fraction on MRI [62].
Though PCSK9 inhibitors such as alirocumab and evolocumab are coming into more widespread use, these medications have not yet been shown to improve NAFLD. However, studies have shown that specific gene variants of PCSK7 have been associated with higher levels of inflammation in the liver along with higher transaminases [63]. Specifically targeting PCSK7 may be able to target NAFLD and its downstream deleterious effects [64].
CHRONIC KIDNEY DISEASE
Much research has been done into the risk of incident chronic kidney disease and nonalcoholic fatty liver disease. A 2018 meta-analysis including a total of 96,595 patients concluded that NAFLD did increase the risk of incident chronic kidney disease with a hazard ratio of 1.37. Multiple confounding factors including age, sex, body mass index, serum lipids, hypertension, tobacco use, baseline kidney function, and diabetes were assessed and the association persisted. Statistical analysis confirmed that the risk of developing chronic kidney disease increased as NAFLD advanced [65]. Cross-sectional analysis showed a patient with liver fibrosis has a 2.5 times greater likelihood of having CKD and is twice as likely to have albuminuria then a patient without NAFLD [66]. It is hoped that medications that would target inflammation and fibrosis in nonalcoholic steatohepatitis (NASH) and chronic kidney disease may delay the disease progression of both these conditions.
OBSTRUCTIVE SLEEP APNEA
Most studies have concluded that a greater degree of hepatic steatosis increases the severity of chronic intermittent hypoxia on polysomnography (Table 1).
Table 1.
Studies Assessing the Relationship between NAFLD and OSA
| Author | Year | Sample size | NAFLD diagnosis | OSA diagnosis | Significant findings |
|---|---|---|---|---|---|
| Tanne et al. | 2005 | 163 | Liver biopsy and liver enzymes | PSG | AHI predicted liver histology independent of age and BMI |
| Turkay et al. | 2012 | 112 | Ultrasound and liver enzymes | PSG | Increased prevalence and severity of steatosis in OSA |
| AHI independently predicted presence of NAFLD | |||||
| Minville et al. | 2014 | 226 | Biochemical markers | PSG | Steatosis increased with the severity of CIH |
| Qi et al. | 2015 | 175 | Ultrasound | PSG | Steatosis increased with the severity of CIH |
| Lin et al. | 2015 | 85 | Ultrasound | PSG | Steatosis increased with the severity of CIH |
| Angrawal et al. | 2015 | Liver enzymes and elastography | PSG | Fibrosis increased with the severity of CIH and higher AHI | |
| Petta et al. | 2018 | 126 | Liver biopsy | PSG and questionnaires | Fibrosis increased with the severity of CIH |
| Trzepizur et al. | 2018 | 1,285 | Liver enzymes and biochemical markers | PSG or home sleep study | Steatosis increased with the severity of OSA |
| Severe OSA associated with 2.5 folds higher risk of liver fibrosis |
NAFLD, nonalcoholic fatty liver disease; OSA, obstructive sleep apnea; BMI, body mass index; PSG, polysomnography; AHI, apnea-hypopnea index; CIH, chronic intermittent hypoxia.
More concerningly, obstructive sleep apnea may contribute to the development of insulin resistance and it may trigger the development of nonalcoholic fatty liver disease [67]. Highlighting the need for multimodal therapy in NAFLD, chronic positive airway pressure treatment decreases the concentrations of liver enzymes, specifically alanine transaminase and aspartate transaminase [68].
ENDOCRINE CONDITIONS
Diabetes mellitus
The interest surrounding NAFLD and its predisposition to diabetes has been extensive. Patients with NAFLD generally have hepatic insulin resistance, which then increases the likelihood of developing diabetes mellitus. On a molecular level, it is thought that insulin resistance causes mitochondrial dysfunction which disrupts fatty acid beta oxidation and leads to lipid deposition in the liver [69]. Addressing NAFLD early on would decrease incident diabetes mellitus and its myriad associated complications. Measures aimed at weight loss, limiting saturated fats in the diet, and becoming physically active all increase insulin sensitivity and decrease hepatic steatosis [70]. Medications used for diabetes mellitus like pioglitazone are among the first line agents in the medical management of NASH [71].
Polycystic ovarian syndrome
The hallmark feature of polycystic ovarian syndrome (PCOS), androgen excess, has been related to insulin resistance. It is well recognized that higher rates of diabetes, central obesity, and dyslipidemia are observed in patients with PCOS [72]. NAFLD has also been shown to affect 34 to 70% of women with PCOS, when NAFLD affects only 14 to 34% of women in the general population [73].
Hyperandrogenism may independently increase the risk of NAFLD. A case-control study compared 275 non-obese women with PCOS to 892 non-obese women without PCOS. The PCOS cohort was found to have a NAFLD prevalence of 5.8%, while only 2.8% of women without PCOS had NAFLD. The study found that increased levels of free testosterone correlated to a higher risk for NAFLD even after adjusting for age, body-mass index, insulin resistance, and lipid profile [74].
Specific treatment of PCOS has not been shown to improve NAFLD. A common treatment for PCOS, oral contraceptives, have not had a clear benefit in NAFLD. A cross-sectional study looking at NHANES data did find lower rates of NAFLD in women currently on oral contraceptives when compared to women who had used them in the past or had never used them [75]. A biopsy-based study, however, showed increased lobular inflammation, a histologic feature of NASH, in patients taking oral contraceptives [76].
Weight loss, on the other hand, appears to be a more surefire way to ameliorate both conditions. Liraglutide 1.8 mg daily led to decreased rates of NAFLD along with downtrends in hepatic fat fraction and visceral adipose tissue [77]. The increased availability of glucagon-like peptide-1 receptor agonists worldwide remains a goal of clinicians invested in public health.
Hypothyroidism
The exact pathophysiological mechanisms for the development of NAFLD in the presence of hypothyroidism are yet to be elucidated. However, the most accepted mechanism of action is that hepatic steatosis results from decreased serum levels of thyroid hormone (TH). The decrease in TH stimulates lipolysis from fat stores in white adipose tissue and from dietary fat sources (high-fat diets) to generate free fatty acids that enter the hepatic cells via protein transporters causing an induction of de novo lipogenesis (DNL). In addition, TH indirectly controls the transcriptional regulation of hepatic DNL by regulating the expression and activities of other transcription factors such as sterol associated with NAFLD through increased levels of thyroid stimulating hormone (TSH) whereby high levels of TSH stimulate lipogenesis in the liver causing hepatosteatosis [78]. Disturbingly, hypothyroidism has been found to be more common in those with NASH and NAFLD related hepatocellular carcinoma [79-82]. Currently, there are no additional treatments recommended for this condition [83].
Growth hormone deficiency
Ever since Takano et al published their case report of a 17 years old boy who presented with panhypopituitarism and fatty liver in 1997 [84], the therapeutic use of growth hormone (GH) in NAFLD has been explored by researchers around the world. In the case report, the patient was treated with GH and their fatty liver subsequently improved, as measured by ultrasound echogenicity and liver size. Numerous studies over the years looking at the relationship between NAFLD and GH deficiency are summarized in Table 2.
Table 2.
Studies Assessing the Relationship between NAFLD and Growth Hormone Deficiency
| Author | Year | Study design | Sample size | NAFLD diagnosis | Significant findings |
|---|---|---|---|---|---|
| Adams et al. | 2004 | Retrospective; single center | 21 | 10 based on liver biopsy and 11 based on imaging | NAFLD developed rapidly (on average 6.4 years) after the diagnosis of pituitary/hypothalamic dysfunction, and liver disease was severe; 60% of those biopsied had cirrhosis, and 14.3% (three) of the 21 received liver transplants or died. |
| Fukuda et al. | 2008 | Retrospective: single center | 42 | Ultrasound and elevated transaminases | Rate of NAFLD increased progressively after stopping GH therapy. The prevalence of NAFLD at 10 and 20 years after the cessation of GH was 22%/10% (M/F) and 33%/25% (M/F). |
| Hong et al. | 2011 | Cross-sectional; single center | 34 males with 40 controls | Ultrasound | The degree of fatty liver on abdominal ultrasonography correlated with the degree of GH deficiency even after adjusting for BMI. |
| Nishizawa et al. | 2012 | Retrospective; single center | 66 patients with 83 controls | Ultrasound; 16 had liver biopsy | GH replacement therapy significantly improved liver enzymes, histology, and levels of fibrotic markers in patients with NASH. |
| Gardner et al. | 2012 | Cross-sectional; single center | 28 patients with 24 controls | Magnetic resonance spectroscopy | NAFLD was equally prevalent in patients with GH deficiency and matched controls. GH replacement significantly decreased abdominal subcutaneous and visceral fat though it did not reduce liver fat. |
| Meienberg et al. | 2016 | Cross-sectional | 22 patients with 44 controls | Proton magnetic resonance spectroscopy | Liver fat content and the prevalence of NAFLD were similar in patients with GH deficiency and matched controls. GH-deficient patients had greater total and visceral fat mass. GH replacement therapy did not decrease hepatic fat fractions. |
| Kang et al. | 2021 | Cross-sectional | 76 patients with 74 controls | Transient elastography and MRI | 71% of patients with hypopituitarism had NAFLD, compared with 31% of controls. |
NAFLD, nonalcoholic fatty liver disease; GH, growth hormone; BMI, body mass index; M/F, males/females; MRI, magnetic resonance imaging; NASH, nonalcoholic steatohepatitis.
In patients with proven GH deficiency, replacing GH does decrease body fat content while increasing lean muscle mass [85]. Efforts at using GH in patients without GH deficiency with the aim of treating NAFLD have had mixed results so far. In a small pilot study, treatment with recombinant human growth hormone did not decrease liver fat content as assessed by magnetic resonance spectroscopy (MRS), though a lower body mass index was achieved [86].
NON-LIVER CANCER
Colon cancer
The links being found between NAFLD and cancer are alarming. Allen et al. [87] longitudinally followed a population of 4,722 patients with NAFLD and compared them to 14,441 controls and found that NAFLD doubled the risk of developing cancer while obesity alone did not (incidence rate ratio [IRR]=2.0, 95% confidence interval [CI] 1.5–2.9 vs. IRR=1.0, 95% CI 0.8–1.4). This data raises the concern that NAFLD may play a role in mediating cancer development. One theory proposes that visceral adipose tissue produces adipocytokines that lead to tumor proliferation. Gastrointestinal cancers appear to have the strongest correlation with NAFLD. Colon cancer specifically had an IRR of 1.8 in the study by Allen et al. [87]. A large meta-analysis of 15 studies confirms a similar degree of association, with a pooled OR of 1.7 when looking at NAFLD and the risk of colorectal cancer [88].
NAFLD appears to not only increase the risk of colon cancer, but precancerous lesions, as well. Adenomatous polyps, polyps with villous morphology, and lesions with high-grade dysplasia are all more common in patients with NAFLD [89]. The need for strict adherence to the recommended guidelines for colon cancer screening in patients with NAFLD are evident, though increased or earlier screening has not yet been suggested.
Gastric cancer
Another gastrointestinal cancer with links to NAFLD is stomach cancer. Data from six studies assessing the risk of incident stomach cancer in NAFLD showed a pooled random effects hazard ratio of 1.81 [90]. It is likely that similar pathways of tumorigenesis play a role in the development of these gastrointestinal cancers.
Breast cancer
The presence of NAFLD may also be associated with extragastrointestinal cancers. A pooled OR of 1.69 was found when assessing the risk of breast cancer in patients with NAFLD [88]. Some of the relevant studies are noted in Table 3.
Table 3.
Studies Assessing the Relationship between NAFLD and Breast Cancer
| Author | Year | Study design | Sample size | NAFLD diagnosis | Cancer diagnosis | Significant findings |
|---|---|---|---|---|---|---|
| Nseir et al. | 2017 | Cohort | 73 patients | CT imaging | Pathology | Odds ratio of 2.82 (breast cancer in NAFLD vs. in controls) |
| Kim et al. | 2018 | Longitudinal cohort | 25,947 patients | Ultrasound | Pathology and radiology | Incidence rate ratio of 1.77 (breast cancer in NAFLD vs. in controls) |
| Allen et al. [87] | 2019 | Longitudinal cohort | 4,722 patients with 14,441 controls | ICD-9 | ICD-9 | Incidence rate ratio of 1.6 (breast cancer in NAFLD vs. in obese controls) |
| Kwak et al. | 2019 | Case-control | 270 patients with 270 controls | Ultrasound | Mammography and pathology | Odds ratio of 1.63 (breast cancer in nonobese NAFLD vs. in nonobese controls); no association between NAFLD and breast cancer was detected in the obese group |
NAFLD, nonalcoholic fatty liver disease; CT, computerized tomography; ICD-9, International Classification of Diseases, ninth revision.
Uterine cancer
Gynecologic cancers appear to be more prevalent in patients with NAFLD. In a pooled analysis of 85,827 patients, of which 23% had NAFLD, patients with NAFLD had an approximately 60% greater risk of developing uterine cancer than the general population [90].
INFECTIONS
Helicobacter pylori
Gastrointestinal-specific infections have been associated with NAFLD. Helicobacter pylori increases the generation of inflammatory markers like interleukin-1β and tumor necrosis factor-α, levels of which are increased in patients testing positive for H. pylori. These markers may increase hepatic inflammation and predispose patients to developing NAFLD. Indeed, studies have shown a 36% greater risk of NAFLD in patients diagnosed with H. pylori infection [91] though the data does not universally affirm the risk (Table 4).
Table 4.
Studies Assessing the Relationship between NAFLD and H. pylori
| Authors | Year | Study design | Sample size | NAFLD diagnosis | H. pylori diagnosis | Significant findings |
|---|---|---|---|---|---|---|
| Abdel-Razik et al. [92] | 2018 | Cohort; multi-center | 369 adults without NAFLD | Ultrasound | Fecal antigen | -the presence of H. pylori was an independent risk variable for the presence of NAFLD |
| -After therapy of H. pylori infection, there was a significant reduction in NAFLD-LFS | ||||||
| Kang et al. | 2018 | Retrospective; NHANES data | 5,404 patients | Ultrasound | H. pylori serology | -H. pylori infection was significantly associated with NAFLD in non-Hispanic black patients |
| -CagA negative H. pylori was associated with an increased risk for NAFLD in the non-Hispanic white and non-Hispanic black populations | ||||||
| Alvarez et al. | 2020 | Cross-sectional; community | 424 patients | Fatty Liver Index and Hepatic Steatosis Index | H. pylori multiplex serology | -No significant associations between H. pylori, H. bilis, or H. hepaticus and NAFLD or other metabolic or liver conditions |
| -Seropositivity for H. pylori antigens, CagA and VacA, and H. hepaticus antigen HH0713 were each associated with a 2 to 3-fold increased prevalence of NAFLD |
NAFLD, nonalcoholic fatty liver disease; H. pylori, Helicobacter pylori; LFS, liver fibrosis score, CagA, cytotoxin associated gene A; VacA, vacuolating cytotoxin A; H. bilis, Helicobacter bilis; H. hepaticus, Helicobacter hepaticus; NHANES, National Health and Nutrition Examination Survey.
Data has been encouraging that treating H. pylori infection in patients with NAFLD does appear to improve fibrosis scores [92]. Clinicians should have a lower threshold for diagnosing and curing patients of H. pylori in cases of NAFLD.
Clostridium difficile
Altered gut microbiome in patients with NAFLD is also being explored. Patients with NASH are found to have increased amounts of Bacteroides and decreased amounts of Prevotella in their gastrointestinal flora, while Ruminococcus was associated with increased liver fibrosis [93]. It follows that patients with NAFLD have a higher risk of infection with Clostridium difficile, even after adjusting for the presence of diabetes and obesity (Table 5).
Table 5.
Studies Assessing the Relationship between NAFLD and Clostridium difficile
| Authors | Year | Study design | Sample size | NAFLD diagnosis | Clostridium difficile diagnosis | Significant findings |
|---|---|---|---|---|---|---|
| Papić et al. [113] | 2020 | Retrospective cohort; single-center | 314 patients | Ultrasound | Screening GDH test confirmed with toxin A/B PCR | -OR 3.27 (P=0.04) - association of NAFLD with C difficile infection. Appears to be independent of other components of metabolic syndrome, such as obesity and diabetes mellitus |
| Nseir et al. | 2020 | Retrospective cross-sectional; single-center | 115 patients | Ultrasound or abdominal CT | Positive stool test for CD Toxin A/B by enzyme immunoassay or PCR for CD | -OR 1.51 (P=0.05) - association of NAFLD with C difficile infection. |
| -Majority of patients with NAFLD (63%) had a fibrosis score of more than two points. Consequently, it seems that NAFLD patients with liver fibrosis are at more risk for acquiring CDI | ||||||
| Šamadan et al. | 2021 | Retrospective cohort; single-center | 329 patients | Ultrasound | Screening GDH test confirmed with toxin A/B PCR | -OR 1.81 (P=0.005) - association of NAFLD with recurrent C difficile infection. |
| -DM and obesity were not associated with rCDI in this study | ||||||
| -Statin use was associated with lower rCDI in patients both with and without NAFLD |
NAFLD, nonalcoholic fatty liver disease; C. difficile and CD, Clostridium difficile; rCDI, recurrent C difficile infection; GDH, glumatate dehydrogenase; CT, computerized tomography; OR, odds ratio; PCR, polymerase chain reaction.
COVID-19
During the global pandemic of our time, front-line clinicians early on saw the increased mortality rates among patients with obesity. NAFLD by itself appears to increase the risk further, even after adjusting for the presence of obesity, especially in severe COVID-19 disease [94]. NAFLD also increases the duration of viral shedding [95], a finding with public health implications. The liver is thought to be especially prone to this virus as SARS-COV-2 enters cells through the angiotensin-converting enzyme 2 (ACE2). These enzymes are abundant in both the liver and in the biliary epithelium [96]. Fighting NAFLD on all fronts may very well decrease the rapid spread of any future viral respiratory-borne infections.
Bacterial pneumonia
The increased inflammation associated with NAFLD may increase the susceptibility to certain infections. Bacterial pneumonia has been examined and some associations have been found (Table 6).
Table 6.
Studies Assessing the Relationship between NAFLD and Bacterial Pneumonia
| Authors | Year | Study design | Sample size | NAFLD diagnosis | Significant findings |
|---|---|---|---|---|---|
| Nseir et al. [71] | 2017 | Retrospective case-control | 141 patients with 141 controls | Ultrasound or abdominal CT | NAFLD (odds ratio 2.5, P=0.023) was associated with CAP. 40.4% of the study group showed evidence of NAFLD compared to 27.6% in controls |
| Bailey et al. [72] | 2017 | Retrospective | 147 trauma ICU patients with VAP and 130 trauma ICU patients without VAP | Abdominal CT | The presence of NAFLD on admission CT was significantly higher in ICU patients with post-traumatic VAP compared to the baseline trauma population |
| Nseir et al. [73] | 2019 | Retrospective cohort | 561 patients | Ultrasound | NAFLD was independently associated with increased 30-day all-cause mortality in patients with CAP, especially in patients with advanced liver fibrosis |
NAFLD, nonalcoholic fatty liver disease; CAP, community-acquired pneumonia; VAP, ventilator-associated pneumonia; CT, computerized tomography; ICU, intensive care unit.
OVERALL PATIENT REPORTED OUTCOMES (PROs)
The presence of NAFLD or NASH is associated with decreased PROs which is more evident in those with NASH and advanced fibrosis. Among the studies completed on health-related quality of life, results have consistently shown that patients with NAFLD and NASH report low physical functioning scores, fatigue and higher rates of depression and anxiety than the general population which can result in decreased productivity at work if employed (presenteeism) and/or performing their activities of daily living [97-100]. On the other hand, treatment of NAFLD or NASH that causes a regression in the disease state patients may show an improvement in their PROs.
Health care utilization for both inpatient and outpatient care is increased for those with NAFLD especially when the comorbidities of CVD, hypertension, and obesity were present for inpatients and CVD, diabetes mellitus, hypertension were present as outpatients. However, the presence of cirrhosis increased costs significantly among inpatients and outpatients. In addition, NAFLD has a significant economic impact on countries, as well [101-113].
CONCLUSION
NAFLD is a complex metabolically based liver disease that is associated with a number of comorbidities. Through an increased awareness of the extrahepatic complications of NAFLD, clinicians can embark on a multi-pronged approach to tackle this insidious, mostly asymptomatic condition [27-34]. As more research is completed on finding patients with NAFLD who are at the highest risk for adverse outcomes, further study is required to determine the preventative screening guidelines to be implemented due to their demonstrably greater risk in several conditions. Due to its multifaceted nature, effective treatments of NAFLD may be generated in other fields not directly related to hepatology, and these developments will be followed with interest by hepatologists worldwide.
Abbreviations
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
- CVD
cardiovascular disease
- HFpEF
heart failure with preserved ejection fraction
- HFrEF
heart failure with reduced ejection fraction
- AVS
aortic valve sclerosis
- MAC
mitral annular calcification
- OR
odds ratio
- CIMT
carotid intima-media thickness
- AST
aspartate transaminase
- ALT
alanine transaminase
- GGT
gamma-glutamyltransferase
- HMG-CoA reductase
hydroxy-methyl-glutaryl-coenzyme A reductase
- PCSK 9 and 7
proprotein convertase subtilisin/kexin type 9 and 7
- CKD
chronic kidney disease
- OSA
obstructive sleep apnea
- BMI
body mass index
- PSG
polysomnography
- AHI
apnea-hypopnea index
- CIH
chronic intermittent hypoxia
- GH
growth hormone
- BMI
body mass index
- M/F
males/females
- US
ultrasound
- MRI
magnetic resonance imaging
- CT
computerized tomography
- DM
diabetes mellitus
- PCOS
polycystic ovarian syndrome
- OCP
oral contraceptive pills
- LDL
low-density lipoprotein
- GLP- 1
glucagon-like peptide-1
- TH
thyroid hormones
- TSH
thyroid stimulating hormone
- rhGH
recombinant human growth hormone
- ICD-9
International Classification of Diseases
- H. pylori
Helicobacter pylori
- LFS
liver fibrosis score
- CagA
cytotoxin associated gene A
- VacA
vacuolating cytotoxin A
- CAP
communityacquired pneumonia
- VAP
ventilator-associated pneumonia
- CT
computerized tomography
- ICU
intensive care unit
- C. difficile and CD
Clostridium difficile
- rCDI
recurrent C. difficile infection
- GDH
glumatate dehydrogenase
- PCR
polymerase chain reaction
- ACE2
angiotensin-converting enzyme 2
- COVID-19
coronavirus disease 2019
- SARS-COV-2
severe acute respiratory syndrome coronavirus 2
- PROs
patient-reported outcomes
Footnotes
Authors’ contribution
RM: study design, data collection, data synthesis and interpretation, and drafting of the manuscript. MHN: study concept, study supervision, data interpretation, and revision of the manuscript. All authors approved the final draft of the manuscript as well as the authorship list.
Conflicts of Interest
Mindie H. Nguyen: Research support: Pfizer, Enanta, Gilead, Glycotest, Vir, B.K. Kee Foundation, National Cancer Institute. Advisory board/consulting: Janssen, Spring Bank, Gilead, Novartis, Bayer, Eisai, Eli Lilly, Exact Sciences, Laboratory of Advanced Medicine, Helio Health, Intercept. Other authors have no disclosures.
REFERENCES
- 1.Ye Q, Zou B, Yeo YH, Li J, Huang DQ, Wu Y, et al. Global prevalence, incidence, and outcomes of non-obese or lean nonalcoholic fatty liver disease: a systematic review and metaanalysis. Lancet Gastroenterol Hepatol. 2020;5:739–752. doi: 10.1016/S2468-1253(20)30077-7. [DOI] [PubMed] [Google Scholar]
- 2.Zou B, Yeo YH, Nguyen VH, Cheung R, Ingelsson E, Nguyen MH. Prevalence, characteristics and mortality outcomes of obese, nonobese and lean NAFLD in the United States, 1999-2016. J Intern Med. 2020;288:139–151. doi: 10.1111/joim.13069. [DOI] [PubMed] [Google Scholar]
- 3.Li J, Ha A, Rui F, Zou B, Yang H, Xue Q, et al. Meta-analysis: global prevalence, trend and forecasting of non-alcoholic fatty liver disease in children and adolescents, 2000-2021. Aliment Pharmacol Ther. 2022;56:396–406. doi: 10.1111/apt.17096. [DOI] [PubMed] [Google Scholar]
- 4.Yu EL, Golshan S, Harlow KE, Angeles JE, Durelle J, Goyal NP, et al. Prevalence of nonalcoholic fatty liver disease in children with obesity. J Pediatr. 2019;207:64–70. doi: 10.1016/j.jpeds.2018.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newton KP, Wilson LA, Crimmins NA, Fishbein MH, Molleston JP, Xanthakos SA, et al. Nonalcoholic Steatohepatitis Clinical Research Network Incidence of type 2 diabetes in children with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2022 Jun 13; doi: 10.1016/j.cgh.2022.05.028. doi: [DOI] [Google Scholar]
- 6.Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 7.Paik JM, Golabi P, Younossi Y, Mishra A, Younossi ZM. Changes in the global burden of chronic liver diseases from 2012 to 2017: the growing impact of NAFLD. Hepatology. 2020;72:1605–1616. doi: 10.1002/hep.31173. [DOI] [PubMed] [Google Scholar]
- 8.Golabi P, Paik JM, AlQahtani S, Younossi Y, Tuncer G, Younossi ZM. Burden of non-alcoholic fatty liver disease in Asia, the Middle East and North Africa: Data from Global Burden of Disease 2009-2019. J Hepatol. 2021;75:795–809. doi: 10.1016/j.jhep.2021.05.022. [DOI] [PubMed] [Google Scholar]
- 9.Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol. 2019;71:793–801. doi: 10.1016/j.jhep.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 10.Golabi P, Paik JM, Arshad T, Younossi Y, Mishra A, Younossi ZM. Mortality of NAFLD according to the body composition and presence of metabolic abnormalities. Hepatol Commun. 2020;4:1136–1148. doi: 10.1002/hep4.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loomba R, Friedman SL, Shulman GI. Mechanisms and disease consequences of nonalcoholic fatty liver disease. Cell. 2021;184:2537–2564. doi: 10.1016/j.cell.2021.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanyal AJ, Van Natta ML, Clark J, Neuschwander-Tetri BA, Diehl A, Dasarathy S, et al. NASH Clinical Research Network (CRN) Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N Engl J Med. 2021;385:1559–1569. doi: 10.1056/NEJMoa2029349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hagström H, Nasr P, Ekstedt M, Hammar U, Stål P, Hultcrantz R, et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol. 2017;67:1265–1273. doi: 10.1016/j.jhep.2017.07.027. [DOI] [PubMed] [Google Scholar]
- 14.Kleiner DE, Brunt EM, Wilson LA, Behling C, Guy C, Contos M, et al. Nonalcoholic Steatohepatitis Clinical Research Network Association of histologic disease activity with progression of nonalcoholic fatty liver disease. JAMA Netw Open. 2019;2:e1912565. doi: 10.1001/jamanetworkopen.2019.12565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reddy YK, Marella HK, Jiang Y, Ganguli S, Snell P, Podila PSB, et al. Natural history of non-alcoholic fatty liver disease: a study with paired liver biopsies. J Clin Exp Hepatol. 2020;10:245–254. doi: 10.1016/j.jceh.2019.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wong VW, Wong GL, Choi PC, Chan AW, Li MK, Chan HY, et al. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut. 2010;59:969–974. doi: 10.1136/gut.2009.205088. [DOI] [PubMed] [Google Scholar]
- 17.McPherson S, Hardy T, Henderson E, Burt AD, Day CP, Anstee QM. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol. 2015;62:1148–1155. doi: 10.1016/j.jhep.2014.11.034. [DOI] [PubMed] [Google Scholar]
- 18.Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 2015;13:643–654.e1-9. doi: 10.1016/j.cgh.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adams LA, Sanderson S, Lindor KD, Angulo P. The histological course of nonalcoholic fatty liver disease: a longitudinal study of 103 patients with sequential liver biopsies. J Hepatol. 2005;42:132–138. doi: 10.1016/j.jhep.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 20.Park J, Lee EY, Li J, Jun MJ, Yoon E, Ahn SB, et al. NASH/Liver fibrosis prevalence and incidence of nonliver comorbidities among people with NAFLD and incidence of NAFLD by metabolic comorbidities: lessons from South Korea. Dig Dis. 2021;39:634–645. doi: 10.1159/000514953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Targher G, Byrne CD, Tilg H. NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut. 2020;69:1691–1705. doi: 10.1136/gutjnl-2020-320622. [DOI] [PubMed] [Google Scholar]
- 22.Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Nonalcoholic fatty liver disease and risk of incident cardiovascular disease: A meta-analysis. J Hepatol. 2016;65:589–600. doi: 10.1016/j.jhep.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 23.Kasper P, Martin A, Lang S, Kütting F, Goeser T, Demir M, et al. NAFLD and cardiovascular diseases: a clinical review. Clin Res Cardiol. 2021;110:921–937. doi: 10.1007/s00392-020-01709-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oni E, Ogunmoroti O, Allen N, A-Mallah MH, Blankstein R, Martin SS, et al. Life’s simple 7 and nonalcoholic fatty liver disease: the multiethnic study of atherosclerosis. Am J Med. 2021;134:519–525. doi: 10.1016/j.amjmed.2020.09.023. [DOI] [PubMed] [Google Scholar]
- 25.Plaz Torres MC, Aghemo A, Lleo A, Bodini G, Furnari M, Marabotto E, et al. Mediterranean diet and NAFLD: what we know and questions that still need to be answered. Nutrients. 2019;11:2971. doi: 10.3390/nu11122971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lloyd-Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, et al. American Heart Association Life’s essential 8: updating and enhancing the American Heart Association’s construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation. 2022;146:e18–e43. doi: 10.1161/CIR.0000000000001078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Younossi ZM, Paik JM, Golabi P, Younossi Y, Henry L, Nader F. The impact of fatigue on mortality of patients with nonalcoholic fatty liver disease: Data from National Health and nutrition examination survey 2005-2010 and 2017-2018. Liver Int. 2022;42:2646–2661. doi: 10.1111/liv.15437. [DOI] [PubMed] [Google Scholar]
- 28.Lazarus JV, Anstee QM, Hagström H, Cusi K, Cortez-Pinto H, Mark HE, et al. Defining comprehensive models of care for NAFLD. Nat Rev Gastroenterol Hepatol. 2021;18:717–729. doi: 10.1038/s41575-021-00477-7. [DOI] [PubMed] [Google Scholar]
- 29.Kanwal F, Shubrook JH, Adams LA, Pfotenhauer K, Wai-Sun Wong V, Wright E, et al. Clinical care pathway for the risk stratification and management of patients with nonalcoholic fatty liver disease. Gastroenterology. 2021;161:1657–1669. doi: 10.1053/j.gastro.2021.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong VWS, Zelber-Sagi S, Cusi K, Carrieri P, Wright E, Crespo J, et al. Management of NAFLD in primary care settings. Liver Int. 2022;42:2377–2389. doi: 10.1111/liv.15404. [DOI] [PubMed] [Google Scholar]
- 31.Cusi K, Isaacs S, Barb D, Basu R, Caprio S, Garvey WT, et al. American Association of Clinical Endocrinology Clinical Practice Guideline for the diagnosis and management of nonalcoholic fatty liver disease in primary care and endocrinology clinical settings: co-sponsored by the American Association for the Study of Liver Diseases (AASLD) Endocr Pract. 2022;28:528–562. doi: 10.1016/j.eprac.2022.03.010. [DOI] [PubMed] [Google Scholar]
- 32.Younossi ZM, Corey KE, Alkhouri N, Noureddin M, Jacobson I, Lam B, et al. US Members of the Global Nash Council Clinical assessment for high-risk patients with non-alcoholic fatty liver disease in primary care and diabetology practices. Aliment Pharmacol Ther. 2020;52:513–526. doi: 10.1111/apt.15830. [DOI] [PubMed] [Google Scholar]
- 33.Srivastava A, Gailer R, Tanwar S, Trembling P, Parkes J, Rodger A, et al. Prospective evaluation of a primary care referral pathway for patients with non-alcoholic fatty liver disease. J Hepatol. 2019;71:371–378. doi: 10.1016/j.jhep.2019.03.033. [DOI] [PubMed] [Google Scholar]
- 34.Long MT, Noureddin M, Lim JK. AGA clinical practice update: diagnosis and management of nonalcoholic fatty liver disease in lean individuals: expert review. Gastroenterology. 2022;163:764–774.e1. doi: 10.1053/j.gastro.2022.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Younossi ZM, Corey KE, Lim JK. AGA clinical practice update on lifestyle modification using diet and exercise to achieve weight loss in the management of nonalcoholic fatty liver disease: expert review. Gastroenterology. 2021;160:912–918. doi: 10.1053/j.gastro.2020.11.051. [DOI] [PubMed] [Google Scholar]
- 36.Simon TG, Roelstraete B, Hagström H, Sundström J, Ludvigsson JF. Non-alcoholic fatty liver disease and incident major adverse cardiovascular events: results from a nationwide histology cohort. Gut. 2022;71:1867–1875. doi: 10.1136/gutjnl-2021-325724. [DOI] [PubMed] [Google Scholar]
- 37.Perseghin G, Lattuada G, De Cobelli F, Esposito A, Belloni E, Ntali G, et al. Increased mediastinal fat and impaired left ventricular energy metabolism in young men with newly found fatty liver. Hepatology. 2008;47:51–58. doi: 10.1002/hep.21983. [DOI] [PubMed] [Google Scholar]
- 38.Rijzewijk LJ, van der Meer RW, Smit JW, Diamant M, Bax JJ, Hammer S, et al. Myocardial steatosis is an independent predictor of diastolic dysfunction in type 2 diabetes mellitus. J Am Coll Cardiol. 2008;52:1793–1799. doi: 10.1016/j.jacc.2008.07.062. [DOI] [PubMed] [Google Scholar]
- 39.Trovato FM, Martines GF, Catalano D, Musumeci G, Pirri C, Trovato GM. Echocardiography and NAFLD (non-alcoholic fatty liver disease) Int J Cardiol. 2016;221:275–279. doi: 10.1016/j.ijcard.2016.06.180. [DOI] [PubMed] [Google Scholar]
- 40.Zhang Z, Wang P, Guo F, Liu X, Luo T, Guan Y, et al. Chronic heart failure in patients with nonalcoholic fatty liver disease: prevalence, clinical features, and relevance. J Int Med Res. 2018;46:3959–3969. doi: 10.1177/0300060518782780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Valbusa F, Agnoletti D, Scala L, Grillo C, Arduini P, Bonapace S, et al. Non-alcoholic fatty liver disease and increased risk of all-cause mortality in elderly patients admitted for acute heart failure. Int J Cardiol. 2018;265:162–168. doi: 10.1016/j.ijcard.2018.04.129. [DOI] [PubMed] [Google Scholar]
- 42.Mantovani A, Pernigo M, Bergamini C, Bonapace S, Lipari P, Valbusa F, et al. Heart valve calcification in patients with type 2 diabetes and nonalcoholic fatty liver disease. Metabolism. 2015;64:879–887. doi: 10.1016/j.metabol.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 43.Bonapace S, Valbusa F, Bertolini L, Pichiri I, Mantovani A, Rossi A, et al. Nonalcoholic fatty liver disease is associated with aortic valve sclerosis in patients with type 2 diabetes mellitus. PLoS One. 2014;9:e88371. doi: 10.1371/journal.pone.0088371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wen X, Wang S, Taveira TH, Akhlaghi F. Required warfarin dose and time in therapeutic range in patients with diagnosed Nonalcoholic Fatty Liver Disease (NAFLD) or Nonalcoholic Steatohepatitis (NASH) PLoS One. 2021;16:e0251665. doi: 10.1371/journal.pone.0251665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moshayedi H, Ahrabi R, Mardani A, Sadigetegad S, Farhudi M. Association between non-alcoholic fatty liver disease and ischemic stroke. Iran J Neurol. 2014;13:144–148. [PMC free article] [PubMed] [Google Scholar]
- 46.Tziomalos K, Giampatzis V, Bouziana SD, Spanou M, Papadopoulou M, Pavlidis A, et al. Association between nonalcoholic fatty liver disease and acute ischemic stroke severity and outcome. World J Hepatol. 2013;5:621–626. doi: 10.4254/wjh.v5.i11.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tang ASP, Chan KE, Quek J, Xiao J, Tay P, Teng M, et al. Nonalcoholic fatty liver disease increases risk of carotid atherosclerosis and ischemic stroke: An updated meta-analysis with 135,602 individuals. Clin Mol Hepatol. 2022;28:483–496. doi: 10.3350/cmh.2021.0406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim SU, Song D, Heo JH, Yoo J, Kim BK, Park JY, et al. Liver fibrosis assessed with transient elastography is an independent risk factor for ischemic stroke. Atherosclerosis. 2017;260:156–162. doi: 10.1016/j.atherosclerosis.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 49.Hu J, Xu Y, He Z, Zhang H, Lian X, Zhu T, et al. Increased risk of cerebrovascular accident related to non-alcoholic fatty liver disease: a meta-analysis. Oncotarget. 2017;9:2752–2760. doi: 10.18632/oncotarget.22755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mori T, Yoshioka K, Tanno Y. Non-alcoholic fatty liver disease frequency and associated factors at admission of acute stroke. Hepatol Int. 2022;16:81–88. doi: 10.1007/s12072-021-10253-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu M, Zha M, Lv Q, Xie Y, Yuan K, Zhang X, et al. Non-alcoholic fatty liver disease and stroke: A Mendelian randomization study. Eur J Neurol. 2022;29:1534–1537. doi: 10.1111/ene.15277. [DOI] [PubMed] [Google Scholar]
- 52.Li H, Hu B, Wei L, Zhou L, Zhang L, Lin Y, et al. Non-alcoholic fatty liver disease is associated with stroke severity and progression of brainstem infarctions. Eur J Neurol. 2018;25:577–e34. doi: 10.1111/ene.13556. [DOI] [PubMed] [Google Scholar]
- 53.Käräjämäki AJ, Pätsi OP, Savolainen M, Kesäniemi YA, Huikuri H, Ukkola O. Non-alcoholic fatty liver disease as a predictor of atrial fibrillation in middle-aged population (OPERA Study) PLoS One. 2015;10:e0142937. doi: 10.1371/journal.pone.0142937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mantovani A. Nonalcoholic fatty liver disease (NAFLD) and risk of cardiac arrhythmias: a new aspect of the liver-heart axis. J Clin Transl Hepatol. 2017;5:134–141. doi: 10.14218/JCTH.2017.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen Z, Liu J, Zhou F, Li H, Zhang XJ, She ZG, et al. Nonalcoholic fatty liver disease: an emerging driver of cardiac arrhythmia. Circ Res. 2021;128:1747–1765. doi: 10.1161/CIRCRESAHA.121.319059. [DOI] [PubMed] [Google Scholar]
- 56.Straus SM, Kors JA, De Bruin ML, van der Hooft CS, Hofman A, Heeringa J, et al. Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J Am Coll Cardiol. 2006;47:362–367. doi: 10.1016/j.jacc.2005.08.067. [DOI] [PubMed] [Google Scholar]
- 57.Hung CS, Tseng PH, Tu CH, Chen CC, Liao WC, Lee YC, et al. Nonalcoholic fatty liver disease is associated with QT prolongation in the general population. J Am Heart Assoc. 2015;4:e001820. doi: 10.1161/JAHA.115.001820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mantovani A, Ballestri S, Lonardo A, Targher G. Cardiovascular disease and myocardial abnormalities in nonalcoholic fatty liver disease. Dig Dis Sci. 2016;61:1246–1267. doi: 10.1007/s10620-016-4040-6. [DOI] [PubMed] [Google Scholar]
- 59.Mantovani A, Rigamonti A, Bonapace S, Bolzan B, Pernigo M, Morani G, et al. Nonalcoholic fatty liver disease is associated with ventricular arrhythmias in patients with type 2 diabetes referred for clinically indicated 24-hour Holter monitoring. Diabetes Care. 2016;39:1416–1423. doi: 10.2337/dc16-0091. [DOI] [PubMed] [Google Scholar]
- 60.Shahab O, Biswas R, Paik J, Bush H, Golabi P, Younossi ZM. Among patients with NAFLD, treatment of dyslipidemia does not reduce cardiovascular mortality. Hepatol Commun. 2018;2:1227–1234. doi: 10.1002/hep4.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Harrison SA, Bashir MR, Guy CD, Zhou R, Moylan CA, Frias JP, et al. Resmetirom (MGL-3196) for the treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2019;394:2012–2024. doi: 10.1016/S0140-6736(19)32517-6. [DOI] [PubMed] [Google Scholar]
- 62.Harrison SA, Alkhouri N, Taub RA, Neff GW, Kowdley KV, Noureddin M. A 52-week phase 3 clinical trial of resmetirom in 180 patients with well-compensated NASH cirrhosis. Hepatology. 2022;76:S90–S92. [Google Scholar]
- 63.Dongiovanni P, Meroni M, Baselli G, Mancina RM, Ruscica M, Longo M, et al. PCSK7 gene variation bridges atherogenic dyslipidemia with hepatic inflammation in NAFLD patients. J Lipid Res. 2019;60:1144–1153. doi: 10.1194/jlr.P090449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kawashiri MA. Can PCSK7 be a new pharmaceutical target? J Atheroscler Thromb. 2022;29:1265–1267. doi: 10.5551/jat.ED188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mantovani A, Zaza G, Byrne CD, Lonardo A, Zoppini G, Bonora E, et al. Nonalcoholic fatty liver disease increases risk of incident chronic kidney disease: A systematic review and metaanalysis. Metabolism. 2018;79:64–76. doi: 10.1016/j.metabol.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 66.Ciardullo S, Ballabeni C, Trevisan R, Perseghin G. Liver stiffness, albuminuria and chronic kidney disease in patients with NAFLD: a systematic review and meta-analysis. Biomolecules. 2022;12:105. doi: 10.3390/biom12010105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ahmed MH, Byrne CD. Obstructive sleep apnea syndrome and fatty liver: association or causal link? World J Gastroenterol. 2010;16:4243–4252. doi: 10.3748/wjg.v16.i34.4243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chin K, Nakamura T, Takahashi K, Sumi K, Ogawa Y, Masuzaki H, et al. Effects of obstructive sleep apnea syndrome on serum aminotransferase levels in obese patients. Am J Med. 2003;114:370–376. doi: 10.1016/s0002-9343(02)01570-x. [DOI] [PubMed] [Google Scholar]
- 69.Koo SH. Nonalcoholic fatty liver disease: molecular mechanisms for the hepatic steatosis. Clin Mol Hepatol. 2013;19:210–215. doi: 10.3350/cmh.2013.19.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tilg H, Moschen AR, Roden M. NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol. 2017;14:32–42. doi: 10.1038/nrgastro.2016.147. [DOI] [PubMed] [Google Scholar]
- 71.Kang SH, Lee HW, Yoo JJ, Cho Y, Kim SU, Lee TH, et al. Korean Association for the Study of the Liver (KASL) KASL clinical practice guidelines: Management of nonalcoholic fatty liver disease. Clin Mol Hepatol. 2021;27:363–401. doi: 10.3350/cmh.2021.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vassilatou E. Nonalcoholic fatty liver disease and polycystic ovary syndrome. World J Gastroenterol. 2014;20:8351–8363. doi: 10.3748/wjg.v20.i26.8351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paschou SA, Polyzos SA, Anagnostis P, Goulis DG, KanakaGantenbein C, Lambrinoudaki I, et al. Nonalcoholic fatty liver disease in women with polycystic ovary syndrome. Endocrine. 2020;67:1–8. doi: 10.1007/s12020-019-02085-7. [DOI] [PubMed] [Google Scholar]
- 74.Kim JJ, Kim D, Yim JY, Kang JH, Han KH, Kim SM, et al. Polycystic ovary syndrome with hyperandrogenism as a risk factor for non-obese non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2017;45:1403–1412. doi: 10.1111/apt.14058. [DOI] [PubMed] [Google Scholar]
- 75.Liu SH, Lazo M, Koteish A, Kao WH, Shih MH, Bonekamp S, et al. Oral contraceptive pill use is associated with reduced odds of nonalcoholic fatty liver disease in menstruating women: results from NHANES III. J Gastroenterol. 2013;48:1151–1159. doi: 10.1007/s00535-012-0715-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yang JD, Abdelmalek MF, Guy CD, Gill RM, Lavine JE, Yates K, et al. Nonalcoholic Steatohepatitis Clinical Research Network Patient sex, reproductive status, and synthetic hormone use associate with histologic severity of nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2017;15:127–131.e2. doi: 10.1016/j.cgh.2016.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Frøssing S, Nylander M, Chabanova E, Frystyk J, Holst JJ, Kistorp C, et al. Effect of liraglutide on ectopic fat in polycystic ovary syndrome: A randomized clinical trial. Diabetes Obes Metab. 2018;20:215–218. doi: 10.1111/dom.13053. [DOI] [PubMed] [Google Scholar]
- 78.Sinha RA, Singh BK, Yen PM. Direct effects of thyroid hormones on hepatic lipid metabolism. Nat Rev Endocrinol. 2018;14:259–269. doi: 10.1038/nrendo.2018.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liangpunsakul S, Chalasani N. Is hypothyroidism a risk factor for non-alcoholic steatohepatitis? J Clin Gastroenterol. 2003;37:340–343. doi: 10.1097/00004836-200310000-00014. [DOI] [PubMed] [Google Scholar]
- 80.Pagadala MR, Zein CO, Dasarathy S, Yerian LM, Lopez R, McCullough AJ. Prevalence of hypothyroidism in nonalcoholic fatty liver disease. Dig Dis Sci. 2012;57:528–534. doi: 10.1007/s10620-011-2006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kim D, Kim W, Joo SK, Bae JM, Kim JH, Ahmed A. Subclinical hypothyroidism and low-normal thyroid function are associated with nonalcoholic steatohepatitis and fibrosis. Clin Gastroenterol Hepatol. 2018;16:123–131.e1. doi: 10.1016/j.cgh.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 82.Hassan MM, Kaseb A, Li D, Patt YZ, Vauthey JN, Thomas MB, et al. Association between hypothyroidism and hepatocellular carcinoma: a case-control study in the United States. Hepatology. 2009;49:1563–1570. doi: 10.1002/hep.22793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tanase DM, Gosav EM, Neculae E, Costea CF, Ciocoiu M, Hurjui LL, et al. Hypothyroidism-Induced Nonalcoholic Fatty Liver Disease (HIN): mechanisms and emerging therapeutic options. Int J Mol Sci. 2020;21:5927. doi: 10.3390/ijms21165927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Takano S, Kanzaki S, Sato M, Kubo T, Seino Y. Effect of growth hormone on fatty liver in panhypopituitarism. Arch Dis Child. 1997;76:537–538. doi: 10.1136/adc.76.6.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hazem A, Elamin MB, Bancos I, Malaga G, Prutsky G, Domecq JP, et al. Body composition and quality of life in adults treated with GH therapy: a systematic review and meta-analysis. Eur J Endocrinol. 2012;166:13–20. doi: 10.1530/EJE-11-0558. [DOI] [PubMed] [Google Scholar]
- 86.Pan CS, Weiss JJ, Fourman LT, Buckless C, Branch KL, Lee H, et al. Effect of recombinant human growth hormone on liver fat content in young adults with nonalcoholic fatty liver disease. Clin Endocrinol (Oxf) 2021;94:183–192. doi: 10.1111/cen.14344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Allen AM, Hicks SB, Mara KC, Larson JJ, Therneau TM. The risk of incident extrahepatic cancers is higher in non-alcoholic fatty liver disease than obesity - A longitudinal cohort study. J Hepatol. 2019;71:1229–1236. doi: 10.1016/j.jhep.2019.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Liu SS, Ma XF, Zhao J, Du SX, Zhang J, Dong MZ, et al. Association between nonalcoholic fatty liver disease and extrahepatic cancers: a systematic review and meta-analysis. Lipids Health Dis. 2020;19:118. doi: 10.1186/s12944-020-01288-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wong VW, Wong GL, Tsang SW, Fan T, Chu WC, Woo J, et al. High prevalence of colorectal neoplasm in patients with nonalcoholic steatohepatitis. Gut. 2011;60:829–836. doi: 10.1136/gut.2011.237974. [DOI] [PubMed] [Google Scholar]
- 90.Mantovani A, Petracca G, Beatrice G, Csermely A, Tilg H, Byrne CD, et al. Non-alcoholic fatty liver disease and increased risk of incident extrahepatic cancers: a meta-analysis of observational cohort studies. Gut. 2022;71:778–788. doi: 10.1136/gutjnl-2021-324191. [DOI] [PubMed] [Google Scholar]
- 91.Ning L, Liu R, Lou X, Du H, Chen W, Zhang F, et al. Association between Helicobacter pylori infection and nonalcoholic fatty liver disease: a systemic review and meta-analysis. Eur J Gastroenterol Hepatol. 2019;31:735–742. doi: 10.1097/MEG.0000000000001398. [DOI] [PubMed] [Google Scholar]
- 92.Abdel-Razik A, Mousa N, Shabana W, Refaey M, Elhelaly R, Elzehery R, et al. Helicobacter pylori and non-alcoholic fatty liver disease: A new enigma? Helicobacter. 2018;23:e12537. doi: 10.1111/hel.12537. [DOI] [PubMed] [Google Scholar]
- 93.Boursier J, Mueller O, Barret M, Machado M, Fizanne L, AraujoPerez F, et al. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota. Hepatology. 2016;63:764–775. doi: 10.1002/hep.28356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sachdeva S, Khandait H, Kopel J, Aloysius MM, Desai R, Goyal H. NAFLD and COVID-19: a pooled analysis. SN Compr Clin Med. 2020;2:2726–2729. doi: 10.1007/s42399-020-00631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ji D, Qin E, Xu J, Zhang D, Cheng G, Wang Y, et al. Non-alcoholic fatty liver diseases in patients with COVID-19: A retrospective study. J Hepatol. 2020;73:451–453. doi: 10.1016/j.jhep.2020.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Adenote A, Dumic I, Madrid C, Barusya C, Nordstrom CW, Rueda Prada L. NAFLD and infection, a nuanced relationship. Can J Gastroenterol Hepatol. 2021;2021:5556354. doi: 10.1155/2021/5556354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Younossi ZM, Stepanova M, Anstee QM, Lawitz EJ, Wai-Sun Wong V, Romero-Gomez M, et al. Reduced patient-reported outcome scores associate with level of fibrosis in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2019;17:2552–2560.e10. doi: 10.1016/j.cgh.2019.02.024. [DOI] [PubMed] [Google Scholar]
- 98.Younossi ZM, Wong VW, Anstee QM, Romero-Gomez M, Trauner MH, Harrison SA, et al. Fatigue and pruritus in patients with advanced fibrosis due to nonalcoholic steatohepatitis: the impact on patient-reported outcomes. Hepatol Commun. 2020;4:1637–1650. doi: 10.1002/hep4.1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Younossi ZM, Anstee QM, Wai-Sun Wong V, Trauner M, Lawitz EJ, Harrison SA, et al. The association of histologic and noninvasive tests with adverse clinical and patient-reported outcomes in patients with advanced fibrosis due to nonalcoholic steatohepatitis. Gastroenterology. 2021;160:1608–1619.e13. doi: 10.1053/j.gastro.2020.12.003. [DOI] [PubMed] [Google Scholar]
- 100.Weinstein AA, Kallman Price J, Stepanova M, Poms LW, Fang Y, Moon J, et al. Depression in patients with nonalcoholic fatty liver disease and chronic viral hepatitis B and C. Psychosomatics. 2011;52:127–132. doi: 10.1016/j.psym.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 101.Zou B, Yeo YH, Jeong D, Park H, Sheen E, Lee DH, et al. A nationwide study of inpatient admissions, mortality, and costs for patients with cirrhosis from 2005 to 2015 in the USA. Dig Dis Sci. 2020;65:1520–1528. doi: 10.1007/s10620-019-05869-z. [DOI] [PubMed] [Google Scholar]
- 102.Nguyen AL, Park H, Nguyen P, Sheen E, Kim YA, Nguyen MH. Rising inpatient encounters and economic burden for patients with nonalcoholic fatty liver disease in the USA. Dig Dis Sci. 2019;64:698–707. doi: 10.1007/s10620-018-5326-7. [DOI] [PubMed] [Google Scholar]
- 103.Younossi ZM, Zheng L, Stepanova M, Henry L, Venkatesan C, Mishra A. Trends in outpatient resource utilizations and outcomes for Medicare beneficiaries with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2015;49:222–227. doi: 10.1097/MCG.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 104.Sayiner M, Otgonsuren M, Cable R, Younossi I, Afendy M, Golabi P, et al. Variables associated with inpatient and outpatient resource utilization among medicare beneficiaries with nonalcoholic fatty liver disease with or without cirrhosis. J Clin Gastroenterol. 2017;51:254–260. doi: 10.1097/MCG.0000000000000567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gordon SC, Fraysse J, Li S, Ozbay AB, Wong RJ. Disease severity is associated with higher healthcare utilization in nonalcoholic steatohepatitis medicare patients. Am J Gastroenterol. 2020;115:562–574. doi: 10.14309/ajg.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 106.Romero-Gomez M, Kachru N, Zamorano MA, Darba J, Shreay S. Disease severity predicts higher healthcare costs among hospitalized nonalcoholic fatty liver disease/nonalcoholic steatohepatitis (NAFLD/NASH) patients in Spain. Medicine (Baltimore) 2020;99:e23506. doi: 10.1097/MD.0000000000023506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Petta S, Ting J, Saragoni S, Degli Esposti L, Shreay S, Petroni ML, et al. LHUs group Healthcare resource utilization and costs of nonalcoholic steatohepatitis patients with advanced liver disease in Italy. Nutr Metab Cardiovasc Dis. 2020;30:1014–1022. doi: 10.1016/j.numecd.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 108.Canbay A, Meise D, Haas JS. Substantial comorbidities and rising economic burden in real world non-alchoholic fatty liver disease (NAFLD)/non-alcoholic steatohepatitis (NASH) patients with compensated cirrhosis (CC): a large German claims database study [Abstract] J Hepatol. 2018;68(Supp 1):S32. Abstract no. PS-057. [Google Scholar]
- 109.Hagström H, Nasr P, Ekstedt M, Hammar U, Widman L, Stål P, et al. Health care costs of patients with biopsy-confirmed nonalcoholic fatty liver disease are nearly twice those of matched controls. Clin Gastroenterol Hepatol. 2020;18:1592–1599.e8. doi: 10.1016/j.cgh.2019.10.023. [DOI] [PubMed] [Google Scholar]
- 110.Younossi ZM, Blissett D, Blissett R, Henry L, Stepanova M, Younossi Y, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64:1577–1586. doi: 10.1002/hep.28785. [DOI] [PubMed] [Google Scholar]
- 111.Younossi ZM, Tampi R, Priyadarshini M, Nader F, Younossi IM, Racila A. Burden of illness and economic model for patients with nonalcoholic steatohepatitis in the United States. Hepatology. 2019;69:564–572. doi: 10.1002/hep.30254. [DOI] [PubMed] [Google Scholar]
- 112.Tampi RP, Wong VW, Wong GL, Shu SS, Chan HL, Fung J, et al. Modelling the economic and clinical burden of non-alcoholic steatohepatitis in East Asia: Data from Hong Kong. Hepatol Res. 2020;50:1024–1031. doi: 10.1111/hepr.13535. [DOI] [PubMed] [Google Scholar]
- 113.Papić N, Jelovčić F, Karlović M, Marić LS, Vince A. Nonalcoholic fatty liver disease as a risk factor for Clostridioides difficile infection. Eur J Clin Microbiol Infect Dis. 2020;39:569–574. doi: 10.1007/s10096-019-03759-w. [DOI] [PubMed] [Google Scholar]


