Abstract
Providing critical nursing care for conscious mechanically ventilated patients is mediated via effective communication. This study aimed to identify and map the antecedents, attributes, consequences, and definition of nurse–conscious mechanically ventilated patient communication (N-CMVPC). This scoping review was conducted by searching the Cochrane Library and the CINAHL, Embase, PubMed, Web of Science, and Scopus databases, between 2001 and 2021. The keywords queried included "nurses," "mechanically ventilated patients," "mechanical ventilation," "intubated patients," "communication," "interaction," "relationships," "nurse–patient communication," "nurse–patient relations," "intensive care units," and "critical care." Studies related to communication with healthcare personnel or family members were excluded. The results indicated that N-CMVPC manifests as a set of attributes in communication experiences, emotions, methods, and behaviors of the nurse and the patient and is classified into three main themes, nurse communication, patient communication, and quantitative-qualitative aspects. N-CMVPC is a complex, multidimensional, and multi-factor concept. It is often nurse-controlled and can express itself as questions, sentences, or commands in the context of experiences, feelings, and positive or negative behaviors involving the nurse and the patient.
Keywords: communication, critical care, intensive care units, mechanically ventilated patients, nurse
INTRODUCTION
Mechanical ventilation (MV) is used widely to treat critically ill patients in intensive care units (ICUs) [1]. Evidence indicates that MV is necessary for over 90% of adult patients with critical illness in ICUs [2]. The application of MV has increased due to recent advancements in invasive medical or surgical procedures, neurological and oncological treatments, treatment of chronic diseases, population aging, and emergence of new diseases, as observed during the coronavirus disease 2019 (COVID-19) pandemic [3]. The nursing care of invasive mechanically ventilated (IMV) patients is mediated through effective communication [4]. This communication is increasingly recognized as an integral part of patient-centered and value-based nursing care; however, many of its dimensions remain to be fully described, determined, or understood [5].
Nurse–conscious mechanically ventilated patient communication (N-CMVPC) faces many challenges [6], including physiological, psychological, and technological barriers, such as the presence of artificial airways (e.g., tracheostomy), the critical condition of the patient, level of consciousness or sedation, delirium, and neurological disease preventing the IMV patient from speaking, being understood, and sharing their needs or thoughts with nurses [7]. Martinho and Rodrigues [8] reported that communication between nurses and IMV patients in 71% of cases was “quite hard” from the perspective of the patient. In such situations, non-verbal communication and use of augmentative and alternative communication (AAC) are basic requirements and must be considered when communicating with patients [9]. AAC strategies refer to a group of approaches, tools, and low- or high-tech technologies such as the use of body language, eye or physical contact, touching, pen and paper, communication boards, alphabet charts, and touch screen devices [10]. These strategies are used to solve communication difficulties for voiceless patients [7].
Communication difficulties are a significant source of distress, potentially causing negative emotions such as anxiety, fear, anger, loss of control, depersonalization, depression, frustration, and dissatisfaction [11,12]. Some IMV patients have described their experiences as “being trapped in a dysfunctional body” after weaning [8]. In such circumstances, effective N-CMVPC is important to inform nurses about the needs or concerns of the patients so that they may adjust to their condition [11].
Recent trends in ICUs toward light-sedation or no-sedation protocols have increased the IMV patient level of consciousness [13]. Evidence suggests that patients with a Glasgow coma scale of 9/15 and higher were able to communicate with nurses nonverbally [14]. One study found that basic communication criteria (i.e., alert, awake, and responsive at least for 12 hours) were met by more than half of the IMV patients [15]. Nursing communication with conscious IMV patients differs from communication with sedated patients. It requires more time, non-verbal methods, continuity, and close attention of nurses [4]. Further studies are needed to explore nurse–patient communication in non-sedated IMV patients and to define it as the essence of nursing care [13].
A thorough review of the studies indicates that the concept of N-CMVPC has not been clearly defined. In addition, the definitions provided in the nursing literature are different, context-based, and abstract, and they lack a clear theoretical definition, which complicates application of this concept [16]. Therefore, given the significance of communication in enhancing the quality of care [17], this study was conducted to provide a theoretical definition and identify the antecedents, attributes, and consequences of N-CMVPC for a better understanding of this concept and its application for quality care.
MATERIALS AND METHODS
The present study was approved by the Institutional Review Board of Shahid Beheshti University of Medical Sciences of Iran (No. IR.SBMU.RETECH.REC.1399.906).
This study was conducted based on the methodological framework of scoping reviews by Arksey and O’Malley [18] and further developments by the Joanna Briggs Institute [19]. Scoping reviews can be used to map underlying concepts and clarify definitions and conceptual borders of a research field. The five stages of scoping reviews in this research were (1) Identifying the research question, (2) Identifying relevant studies, (3) Study selection, (4) Charting the data, and (5) Collating, summarizing, and reporting the results. In addition, we used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist [20] to report our findings (Supplementary Table 1).
Identifying the Research Questions
This scoping review aimed to determine the antecedents, attributes, consequences, and definitions of the concept of N-CMVPC. The primary research question for this review was (1) How is the concept of N-CVPMC defined in various studies? This question led to the following complementary questions: (2) In the studies, what attributes are used to describe the concept of N-CMVPC? (3) What are the antecedents of the concept of N-CMVPC? (4) What are the consequences of this type of communication, according to the evidence? Research questions were based on the PCC aspects of population, concept, and context [21]. In the current research, the population (P) included ICU nurses and conscious patients under MV. The concept (C) was the N-CMVPC, and the context (C) was ICUs.
Identifying Relevant Studies
Between June and October 2021, an advanced search was performed on Web of Science, CINAHL, Embase, PubMed, Cochrane Library, and Scopus for articles published between January 2000 and June 2021. Also, full-text articles published in the main Persian databases, including IranMedex, MagIran, IranDoc, and the Scientific Information Database, were searched. The key terms were nurses, mechanically ventilated patients, MV, intubated patients, communication, interaction, relationships, nurse–patient communication, nurse–patient relations, ICUs, critical care, and their Persian equivalents. Numerous combinations of these keywords were created using the Boolean operators “AND” and “OR.” In addition, references at the end of each paper were reviewed to complete the research. An information technologist was consulted to validate the search. An overview of the search strategy is shown in Supplementary Table 2.
Study Selection
Preliminary data included full-text articles published in English, focusing on communication between nurses and conscious adult patients (older than 18 years) under MV. All quantitative, qualitative, and mixed-method designs were eligible. Studies with only a small number of findings related to the study concept, such as communication with other health care personnel or family members, experiences of nurses caring for mechanically ventilated patients, and experiences of patients being mechanically ventilated were excluded. Also, studies focusing on interventions not led by nurses or strategies describing the technical aspects of AACs other than nurse–patient communication were excluded.
After all articles were identified in all databases, duplicates were excluded, eligible articles were selected, and the articles were reviewed and screened independently by the members of two research teams (AM and MH). The final decision to include the evidence was based on agreement; in cases of disagreement, a third party (FAS) was consulted. No methodological quality assessment was performed, which was consistent with the guidance provided in the scoping review methodology [19]. As the international Prospective Register of Systematic Reviews (PROSPERO) does not accept scoping review protocols for publication, it was not registered [22].
Charting the Data
Data from eligible studies were charted in a data extraction form, including author, year, country, design, the aim of the study, and main findings of the study related to antecedents, attributes, consequences, and definitions of the concept of N-CMVPC. The full text of the included articles was reviewed several times to ensure that all study objectives were considered. The methods and tools developed to measure the concept of N-CMVPC were also investigated. One researcher (AMG) extracted data, and the second researcher (MH) validated the data.
Collating, Summarizing, and Reporting Results
Applying the qualitative content analysis method through a conventional approach [23] helped us collate, summarize, and report results. The analysis process started with examining the entire text for meaning units. The meaning units in this study were sub-aspects related to antecedents, attributes, and consequences of N-CMVPC. Meaning units were coded and analyzed considering the study objectives in MAXQDA version 10 (Udo Kuckartz). Similar codes were classified into subcategories, which were grouped to form the main categories and themes. Findings were clarified and mapped as a comprehensive collection of antecedents, attributes, and consequences that characterize and define N-CMVPC in the ICU.
RESULTS
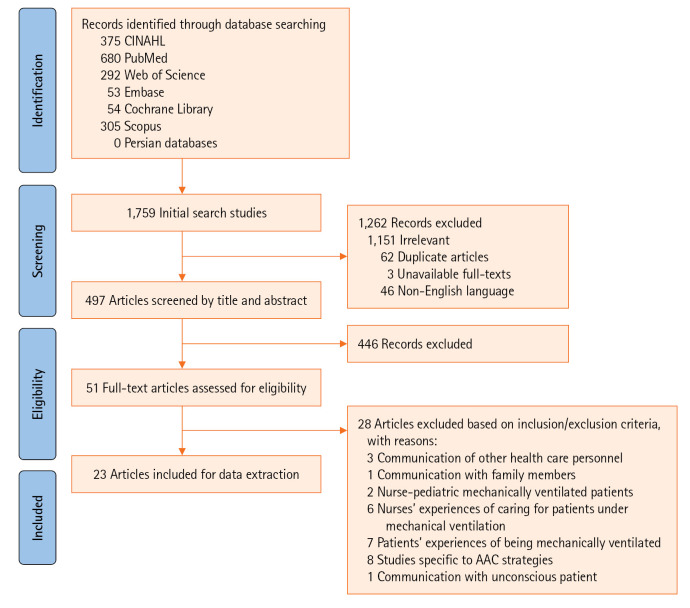
The search identified 1,759 articles, of which 1,262 were excluded based on non-English language (n=46), unavailable full-text (n=3), duplicate articles (n=62), and irrelevant objectives (n=1,151). After reading the titles and abstracts, 446 articles were excluded. Finally, 51 full-text articles were examined for eligibility, and 23 studies that met the inclusion criteria were included in this review. Figure 1 shows a summary of this process based on the PRISMA flowchart.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart for selecting articles. AAC: augmentative and alternative communication.
Characteristics of Studies
A total of 23 articles met the inclusion criteria, of which 4 used a qualitative design, 16 used a quantitative design, and 3 used a mixed-method design. Geographically, most of the selected articles were from Europe (n=8) and Asia (n=6), with a few articles from the USA (n=5), Africa (n=3), and Australia (n=1). With regard the time of publication, most of the articles (60%) were conducted between 2016 and 2020, though 40% of them were conducted between 2011 and 2015. Table 1 presents the included studies [4,6,7,9,12,14,17,24-39].
Table 1.
Summary of included articles
| Study | Country | Design | Aim of study |
|---|---|---|---|
| Holm et al. (2020) [12] | Denmark | Umbrella review | To describe the interaction between ICU patients and the ICU environment |
| Gorzin et al. (2020) [39] | Iran | Quasi‑experimental study with pretest-posttest design | To evaluate the effect of education on function and communication skills of nurses with IMV patients |
| Bayog et al. (2020) [30] | Philippines | Cross-sectional, choice-based conjoint analysis | To explicate the communication preferences of registered nurses towards IMV patients |
| Momennasab et al. (2019) [31] | Iran | Observational study | To describe the quality of the relationship between nurses and IMV patients |
| Wallander Karlsen et al. (2019) [26] | Norway | Observational study | To explore the interaction between IMV patients and healthcare personnel |
| Karlsen et al. (2019) [25] | Norway | Scoping review | To examine previous knowledge about interaction between health care personnel and conscious IMV patients |
| Noguchi et al. (2019) [38] | Japan | Mixed method | To examine changes in the practice of nurses who received an intervention designed to increase their awareness of endotracheally intubated, lightly sedated IMV patients’ intent to communicate |
| Salem and Ahmad (2018) [29] | Jordan | Integrative review | To assess available evidence about existing skills, knowledge, and perceptions and barriers for IMV patients to communicate |
| Carruthers et al. (2017) [9] | UK | Systematic review | To assess the effectiveness of AAC strategies to enable IMV patients to communicate |
| Dithole et al. (2017) [36] | South Africa | Qualitative study | To describe nurses’ experience of a communication skills training intervention |
| Dithole et al. (2016) [6] | South Africa | Structured review | To identify communication challenges existing between nurses and IMV patients |
| Dithole et al. (2016) [14] | South Africa | A retrospective descriptive and explorative research design with a quantitative approach | To determine the existing knowledge and skills of intensive care nurses working with MV patients |
| Ten Hoorn et al. (2016) [34] | Netherlands | Systematic review | To summarize the current evidence regarding communication methods with IMV patients |
| Foà et al. (2016) [7] | Italy | Qualitative study | To investigate how the ICU nurses manages communications and relationships |
| Tembo et al. (2015) [24] | Australia | Qualitative, phenomenological | Describe the lived experiences of people who experienced critical ill patients in the ICU and how it affects the participants' continued existence beyond ICU and hospitalization |
| hermeneutical research | |||
| Happ et al. (2014) [37] | USA | Quasi-experimental design | To assess the effect of two levels of intervention on communication ease, quality, frequency, and success between nurses and IMV patients |
| Nilsen et al. (2014) [17] | USA | Descriptive correlational design | To describe interaction behaviors between nurses and IMV patients and factors which could affect communication |
| To assess relationship between interaction behaviors and nursing care quality | |||
| Nilsen et al. (2013) [32] | USA | Secondary analysis of data from a quasi-experimental study | To examine the association between nurse and patient characteristics, and duration of nurse talk |
| Meriläinen et al. (2013) [28] | Finland | Mixed method study | To describe the interaction between IMV patients and the ICU environment from the perspective of the patients’ memories |
| Karlsson et al. (2012) [4] | Sweden | Qualitative, phenomenological | To observe, interpret, and describe nurses’ communication with conscious IMV patients |
| hermeneutical research | |||
| Happ et al. (2011) [27] | USA | Quantitative (descriptive study) | To describe communication interactions, methods, and assistive techniques between nurses and nonspeaking patients in the ICU |
| Khalaila et al. (2011) [33] | Israel | Cross-sectional study | To investigate the relationship between communication characteristics and psycho-emotional distress among IMV patients, and identify factors predictive of psychological outcomes |
| Grossbach et al. (2011) [35] | Minneapolis | Review article | To review various strategies to promote effective communication between IMV patients, health care staff, and patients’ family members |
ICU: intensive care unit; IMV: invasive mechanically ventilated; AAC: augmentative and alternative communication; MV: mechanical ventilation.
Attributes of the Concept
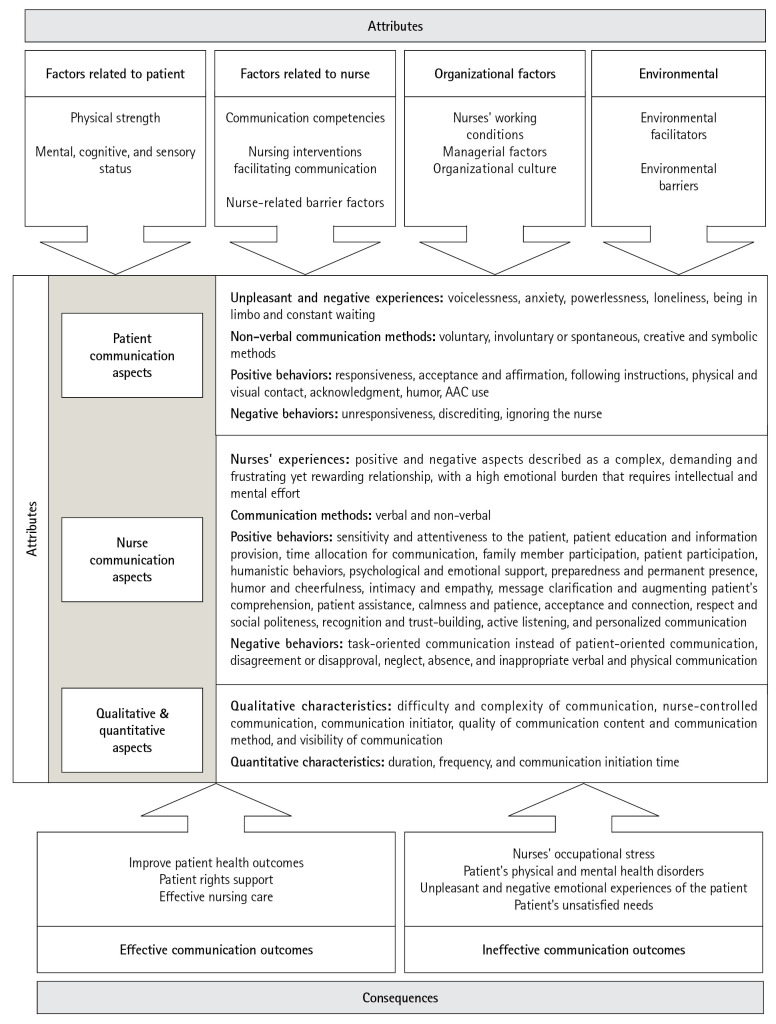
The current study results indicate that the attributes of N-CMVPC can be summarized into three main themes: nurse communication, patient communication, and quantitative-qualitative aspects.
Patient communication
The attributes of this type of communication in patients manifested in their communication experiences, emotions or feelings, methods, actions, or behaviors. Patients' experiences of voicelessness, anxiety, powerlessness, loneliness, being in limbo, and constant waiting were frequently repeated in the literature and were unpleasant and negative [12,24,25]. One of the other extracted attributes of the N-CMVPC was the variety of verbal and non-verbal communication methods. Three subcategories of patient non-verbal communication methods were identified. These methods were voluntary, involuntary or spontaneous, and creative and symbolic non-verbal communication.
Other extracted attributes of the N-CMVPC were the positive and negative communication behaviors of nurses and patients. A literature review showed positive patient communication behaviors such as responsiveness [26], acceptance and affirmation [27], following instructions [17], physical contact, visual contact [17,27], acknowledgment [26,27], humor [17], and use of the AAC strategies [27]. The negative patient behaviors were unresponsiveness [26,27], discrediting, and ignoring the nurse [17,27].
Nurse communication
The attributes of the N-CMVPC from the perspective of nurses were also determined by their communication experiences, emotions, methods, and behaviors. The communication experiences of nurses with mechanically ventilated patients include positive and negative aspects, described as a complex, demanding, and frustrating yet rewarding relationship, with a high emotional burden that requires intellectual and mental effort [7,12,25]. Nurses used different verbal and non-verbal methods to communicate. According to the literature, positive nurse communication behaviors include sensitivity and attentiveness to the patient [4,28], patient education and information provision [6,17,25,29], time allocation for communication [7], family member participation [7,30], patient participation, humanistic behaviors [4], psychological and emotional support [4,7,27], preparedness and permanent presence [4,7], humor and cheerfulness [4,7,27], intimacy and empathy [4,7], message clarification and augmentation of patient comprehension [4,27], patient assistance [27], calmness and patience [4,7], acceptance and connection, respect and social politeness [4,27], recognition and trust-building [7,27], active listening [4], and personalized communication [4,27]. In contrast, behaviors such as task-oriented communication instead of patient-oriented communication [12], disagreement or disapproval, neglect, absence, and inappropriate verbal and physical communication were negative communication behaviors of the nurse [4,17,27].
Qualitative and quantitative aspects
The theoretical data identified five qualitative and three quantitative characteristics of the N-CMVPC. The qualitative characteristics were difficulty and complexity of communication [12,25,27,28], nurse-controlled communication [12,25,28], communication initiator [25,27,30,31], quality of communication content, and communication method [4,26,27,31]. The quantitative characteristics of N-CMVPC were duration [25,27-29,32], frequency [25,27-29], and communication initiation time [28].
Antecedents of the Concept
Four themes were identified as antecedents of the N-CMVPC concept: (1) Factors related to the patient, including physical strength and mental, cognitive, and sensory status; (2) Factors related to the nurse, including communication competencies, interventions facilitating communication, and barrier factors; (3) Organizational factors, including working conditions, managerial factors, and organizational culture; and (4) Environmental factors including facilitators and barriers (Table 2) [6,7,12,14,25,27-30,32,34-38].
Table 2.
Antecedents of the N-CMVPC concept in the ICUs
| Theme | Category | Subcategory |
|---|---|---|
| Factor related to patient | Physical strength | ▪ Physical condition [12,28,32,34] |
| ▪ Clinical condition [6,12,27,28] | ||
| Mental, cognitive and sensory status | ▪ Mental and cognitive status [6,12,34] | |
| ▪ Level of consciousness [6,12,27,32] | ||
| ▪ Patients' sensory status [12,34] | ||
| Factor related to nurse | Communication competency | ▪ Nurses' skills in controlling and directing communication [6,36] |
| ▪ Nurses' skills in communication methods [6,36] | ||
| ▪ Nurses' skills in communicating with accuracy, sensitivity, and attention [6,36] | ||
| ▪ Nurses' commitment, knowledge and communication experiences [6,36] | ||
| Nursing interventions facilitating communication | ▪ Paying attention to the communication duration [6,32,35] | |
| ▪ Maintaining a proper distance from the patient [6,14,35] | ||
| ▪ Paying attention to the patient needs [7,35] | ||
| ▪ Considering nurses' preferences to communicate [30] | ||
| ▪ Use of para-verbal communication [6,7,14,35] | ||
| ▪ Evaluate the patient's conditions, needs and communication barriers [6,12,14,35] | ||
| Nurse-related barrier factor | ▪ Inadequate knowledge [34] | |
| ▪ Task-oriented communication [6] | ||
| ▪ Communication at an inappropriate time [6,14] | ||
| Organizational factor | Nurses’ working condition | ▪ Work load pressure [7] |
| ▪ Lack of time [7] | ||
| Managerial factor | ▪ Development of communication tools and AAC technologies [29,36] | |
| ▪ Recruiting helpful human resources specialized in communication [7,29,37] | ||
| ▪ Development, application and evaluation of communication standards, tools, and algorithms [12,14,34] | ||
| ▪ Developing nursing education and training [7,12,14,29,35-38] | ||
| ▪ Evaluating and developing nurses' communication skills [36] | ||
| ▪ Improving communication documentation [12,34] | ||
| Organizational culture | ▪ Team work [25,35] | |
| ▪ Inter-professional participation [29,35] | ||
| ▪ Sharing experiences [7] | ||
| Environmental factor | Environmental facilitator | ▪ Appropriate physical environment [7] |
| ▪ Friendly and comfortable communication environment [7,35] | ||
| Environmental barrier | ▪ Unfamiliar environment [7,28] | |
| ▪ Noisy environment [6,35] |
N-CMVPC: nurse–conscious mechanically ventilated patient communication; ICU: intensive care unit; AAC: augmentative and alternative communication.
Consequences of the Concept
The consequences of the concept of N-CMVPC can be classified into effective and ineffective communication outcomes. Effective N-CMVPC improves the health outcomes of the patient, supports the rights of the patient, and leads to effective nursing care. Conversely, ineffective N-CMVPC may lead to occupational stress in the nurses and physical and mental health disorders in the patients, as well as unpleasant and negative emotional experiences and unsatisfied needs (Table 3) [7,9,12,14,17,24-31,37,38].
Table 3.
Consequences of the N-CMVPC concept in the ICUs
| Theme | Category | Subcategory |
|---|---|---|
| Effective communication outcomes | Improving the patients' health outcomes | ▪ Promoting the patient's health and recovery [25,29] |
| ▪ Promoting the patient comfort and convenience [29,37] | ||
| ▪ Prevent adverse medical outcomes [17,25,30] | ||
| Supporting patient rights | ▪ Patient satisfaction [38] | |
| ▪ Patient participation [25-27,29] | ||
| ▪ Patient respect ▪ Patient satisfaction [38] | ||
| ▪ Improving the quality of medical decisions [7,25,28] | ||
| Effective nursing care | ▪ Development of individual care quality [28,29] | |
| ▪ Identifying and meet the patient needs [7,29] | ||
| ▪ Improving patient abilities and safety [25,29] | ||
| Ineffective communication outcomes | Nurse's occupational stress | ▪ Nurse's frustration and dissatisfaction [7,31] |
| ▪ Nurse's feeling of failure and role inadequacy [7] | ||
| Patient's physical and mental health disorders | ▪ Incidence of anxiety disorders in the patient [9,14,25] | |
| ▪ Patient emotional instability [12,24,27] | ||
| ▪ Patient's body image disturbance [24,27] | ||
| ▪ Impaired patient's health and recovery [14,27,28,30] | ||
| Unpleasant and negative emotional experiences of the patient | ▪ Feeling of dependency and vulnerability [12] | |
| ▪ Patient's experience of being in a bad situation between life and death [12,24] | ||
| ▪ Patient's sense of captivity [12] | ||
| ▪ Patient's feeling of despair and dissatisfaction [9,12,25,31] | ||
| ▪ Patient's feeling of suffering and disorientation due to unmet needs[12] | ||
| Patient's unsatisfied needs | ▪ Unmet patient's needs [12] | |
| ▪ Unknown patient's needs [12] | ||
| ▪ Unevaluated patient's needs [30] |
N-CMVPC: nurse–conscious mechanically ventilated patient communication; ICU: intensive care unit.
DISCUSSION
There is an urgent need to define and identify antecedents, attributes, and consequences of the N-CMVPC concept in ICUs [12]. In this scoping review, various articles regarding N-CMVPC were explored, and the attributes, antecedents, and consequences were determined to clarify and define the concept for wider practical application in nursing education, training, and practice (Figure 2).
Figure 2.
Mapping of attributes, antecedents, and consequences of the nurse–conscious mechanically ventilated patient communication. AAC: augmentative and alternative communication.
Walker and Avant [40] defined attributes as features that continually appear in a concept that help researchers distinguish the occurrence of a specific phenomenon from a similar phenomenon. The first defining attributes of the concept of N-CMVPC were "patient communication" and "nurse communication," which were reflected in their communication experiences, emotions, methods, and behaviors. Unpleasant and negative feelings of patients are frequent in the literature. Communication difficulties due to intubation are the main factors of distress, leading to high levels of psycho-emotional distress and negative emotions in patients [27,33,34]. Likewise, nurses become frustrated when they communicate with patients under MV, as the conditions allow minimal communication. Such communication difficulties lead nurses to experience many negative emotions while communicating with patients [6]. Nurses routinely use traditional communication methods like lip reading, gestures, and nods to converse with IMV patients [33,35]. This makes N-CMVPC difficult, complex, time-consuming, frustrating, inefficient in meeting patient needs, and demanding yet rewarding for nurses. Therefore, it is necessary to emphasize the need for an effective communication strategy for N-CMVPC in ICUs [30]. Enhanced nurse awareness of the needs and experiences of IMV patients would be useful in developing effective interventions to facilitate communication with them [29].
In this study, the communication methods of nurses and IMV patients were shown as a category of communication attributes. N-CMVPC includes a variety of verbal and non-verbal communication methods, with non-verbal communication playing a greater role [28]. IMV patients are speechless due to intubation. They are unable to communicate verbally. They communicate with nurses through various non-verbal methods. In this study, three types of non-verbal communication by patients were identified: voluntary, involuntary or spontaneous, and creative and symbolic methods.
Mouthing words, facial expressions, gestures, body language, and pointing are some examples of non-verbal communication by patients and are often performed voluntarily to express their needs. Other communication techniques derived from the literature were spontaneous and involuntary communication efforts, such as involuntary muscle contractions or cringes [12,28]. Another type of non-verbal communication found in patients is the initiative to express themselves and their creativity by creating individual communication strategies, labeled creative and symbolic communication. Wallander Karlsen et al. [26] describe this method as "attention-seeking actions" and define it as "the act of seeking attention and understanding without a voice, with a variety of content, forms, and non-verbal methods." For example, creating sound by tapping on the bedside, tongue clicking, or even breathing hard to produce an alarm from the ventilator, or symbolic gestures such as a thumbs up that means everything is good. Such strategies are the basis for the N-CMVPC because IMV patients can only convey their message to the nurse if they have attracted their attention [26]. However, nurses frequently use verbal methods to communicate with IMV patients [25]. The results revealed that talking, negotiation, commands, and yes/no questions were verbal methods, and the use of symbols and physical and visual contact were non-verbal methods frequently used by nurses. Nurses need to be self-aware of their communication methods [41]. Also, they must spend more time and be more attentive and sensitive to the bodies or symbolic gestures of IMV patients to understand their needs [26].
Another category of communication attributes was communication behaviors. Nurses and IMV patients perform positive and negative behaviors when interacting, which is consistent with the results of previous studies. Nilsen et al. [17] defined behaviors as verbal and non-verbal, shared by nurses and patients, and affecting interpersonal communication. Every communication behavior of IMV patients, even their silence, has a message of value for nurses [25]. Therefore, critical nurses need to identify and recognize the communication behaviors of patients. Effective N-CMVPC entails a nurse or patient displaying positive communication behaviors [30]. The communication behaviors of nurses can motivate patients to participate in the exchange and help establish a therapeutic relationship [17].
The second defining attribute of the concept of N-CMVPC was "qualitative-quantitative aspects," which include the five qualitative characteristics of communication difficulty and complexity, quality of communication content and method, communication visibility, communication initiator, and nurse-controlled communication and the three quantitative characteristics of duration, frequency, and communication initiation time. N-CMVPC is a complex concept, with the content of sentences, questions, instructions, methods, positive and negative behaviors, actions, and reactions visible in different nursing care situations [4,27]. Holm et al. [12] argued that the complexity of the communication is rooted, first, in the difficulty of capturing the interaction through communication; second, in the different tools and methods applied to optimize communication; and third, in the differences in local and national contexts. The other characteristic, the communication initiator, focuses on the person who starts the communication, consisting of two levels, patient-initiated or nurse-initiated. Happ et al. [27] noted that most communications are started by nurses and followed by patients. It was mentioned that the initiative of nurses to communicate was vital to meeting the needs of patients [4]. Nurses recognize the inability of IMV patients to communicate verbally, so they prefer to initiate communication in different ways to provide vital nursing care [30]. Another characteristic of the N-CMVPC, nurse-controlled communication, refers to the critical role of nurses in directing and controlling the topic, time, duration, frequency, and method of communication in the ICU [12,25,29]. Nurses must acquire sufficient knowledge and skills to establish effective communication [14].
Antecedents include various factors taken from the literature that precedes the concept occurrence [40]. For IMV patients, physical readiness and mental, cognitive, and sensory status include the condition of their illness and their mood during the hospital stay, which are linked with the ability to communicate [42]. Before N-CMVPC, nurses must assess the physical, mental, cognitive, and sensory status of the patient and measure whether it is appropriate to attempt communication at that time or not [43]. Assessing the communication ability of IMV patients is essential to effectively address the physiological and psychological needs of the patients [14,35].
The results indicate that the communication competencies of the nurses, including characteristics such as knowledge, skills, commitment, and experiences, are important predisposing factors in communication [36]. Additionally, as noted in previous studies, the results of the current study suggest that some nursing interventions are effective in facilitating communication; these include the use of para-verbal communication [7,14,35], paying attention to the needs of the patients [6,7,14,35], considering the communication preferences of nurses [30], paying attention to the communication duration [6,32,35], maintaining a proper distance from the patient [6,14,35], and evaluating the conditions, needs, and communication barriers of the patients [6,12,14,35]. On the contrary, inadequate knowledge among nurses [34], task-oriented communication [6], and communication at an inappropriate time [6,14] were nurse-related communication barriers. At the organizational level, appropriate facilities such as communication tools and AAC strategies should be provided to facilitate N-CMVPC [12-14]. The use of AAC strategies is highly recommended for reducing the communication difficulties of IMV patients and improving patient satisfaction in communication [9,33]. Moreover, reducing the workload of the nurses [7]; recruiting helpful human resources specialized in communication such as speech-language pathologists [7,29,37]; developing, applying, and evaluating communication standards, tools, and algorithms [12,14,34]; developing nursing education and training [7,12,14,29,35-38]; evaluating and developing the communication skills of nurses [36], improving communication documentation [12,34], and developing an organizational culture to promote teamwork [25,35], encourage inter-professional participation [29,35], and share experiences [7] may be beneficial.
Walker and Avant [40] have defined consequences as those events that arise from the occurrence of the concept. Consistent with the results of other studies, improving the health outcomes of patients, supporting patient rights, and the effectiveness of nursing care were consequences of effective N-CMVPC. In addition, the literature shows that ineffective N-CMVPC may lead to the occupational stress of nurses and physical and mental health disorders of patients, unpleasant and negative emotional experiences, and unsatisfied needs.
Studies have revealed that effective N-CMVPC may reduce the time patients spend on MV [25], reduce the duration of patient hospitalization in the ICU [29], and prevent adverse medical outcomes such as pain and delirium [17,25,30]. According to Guttormson et al. [44], inefficient communication can increase the stress of IMV patients and impact nursing care during and after admission to the ICU.
Effective communication of nurses can support the rights of patients by increasing patient satisfaction [38], participation [25,27-29], and respect [38] and improving the quality of medical decisions during treatment [7,25,28]. Meriläinen et al. [28] stated that effective N-CMVPC fosters individualized care. Effective communication is essential for conveying the physiological and psychological needs of the patient, plan of care, and end-of-life decisions. ICU nurses play a critical therapeutic role in mechanically ventilated patients. Therefore, effective communication skills are essential when caring for such patients [14]. Nurse awareness of communication strategies and their training in this field can improve the quality of care by increasing patient satisfaction, comfort, and participation in care plans [29].
STRENGTHS AND LIMITATIONS OF THE STUDY
This study makes a valuable contribution to the field. To the best of our knowledge, this is the first scoping review that summarizes current studies by providing an overview and comprehensive set of attributes, antecedents, and consequences for the N-CMVPC concept in ICUs. This is the most significant strength of the current study. However, like any review study, this scoping review might have missed some relevant sources of information. Due to a lack of access, the review depended on limited information to assess the review question, the chosen search strategy, and electronic databases. For further studies, it could be interesting to survey the attributes, antecedents, and consequences of the N-CMVPC concept provided in this study from the point of view of IMV patients and their family members, critical care nurses, and even other healthcare members to provide a more comprehensive definition of this concept.
IMPLICATIONS AND RECOMMENDATIONS FOR PRACTICE
The results can be used to develop empirical indicators, such as assessment tools, and they can also increase the knowledge, awareness, and skills of nurses in communicating with mechanically ventilated patients and meeting their diverse needs.
CONCLUSIONS
The N-CMVPC is a complex, multidimensional, and multifactorial concept. It is often nurse-controlled and observable, with the content of brief and short answer questions, sentences, or commands. This relationship includes a variety of verbal and voluntary, involuntary or spontaneous, and creative or symbolic attention-seeking non-verbal communication methods. It also includes a variety of positive and negative actions-reactions in communicating feelings and experiences. This communication can be evaluated through a series of qualitative and quantitative characteristics. The concept of N-CMVPC includes a set of converging underlying factors, including factors related to the patient, to the nurse, and to the organization, management, and environment. Effective N-CMVPC allows patients to progress toward preventing and reducing the severity and complications of the disease, increasing their feelings of comfort and recovery, and ultimately promoting their health outcomes by overcoming psychological problems and unpleasant emotions. Such a system will enable nurses to support the rights of patients by improving their participation, respect, satisfaction, and quality of medical decisions. Also, it will help nurses provide effective care by identifying and addressing the needs of the patient, increasing the abilities and safety of the patient, and promoting the uniqueness and quality of their care. The current research results were based on theoretical data and a literature review. Such antecedents, attributes, and consequences must be analyzed in the future from the perspective of nurses, IMV patients, and their family members to achieve a more comprehensive definition of the concept.
KEY MESSAGES
▪ The findings from this research can be utilized to create empirical indicators, such as assessment tools, with the aim of enhancing the knowledge, awareness, and communication skills of nurses when working with mechanically ventilated patients.
▪ This will help to address the diverse needs of these patients.
Acknowledgments
None.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Methodology: MH, FA. Writing–original draft: AM. Writing–review & editing: AM, FA.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4266/acc.2022.01039.
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist
The search strategy of the study
REFERENCES
- 1.He Q, Wang W, Zhu S, Wang M, Kang Y, Zhang R, et al. The epidemiology and clinical outcomes of ventilator-associated events among 20,769 mechanically ventilated patients at intensive care units: an observational study. Crit Care. 2021;25:44. doi: 10.1186/s13054-021-03484-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Namadian M, Taran Z. The effect of sedation protocol on sedation level and pharmacological and non-pharmacological interventions on mechanically ventilated patients. Iran J Nurs Midwifery Res. 2021;26:316–23. doi: 10.4103/ijnmr.IJNMR_165_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zisk-Rony RY, Weissman C, Weiss YG. Mechanical ventilation patterns and trends over 20 years in an Israeli hospital system: policy ramifications. Isr J Health Policy Res. 2019;8:20. doi: 10.1186/s13584-019-0291-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karlsson V, Forsberg A, Bergbom I. Communication when patients are conscious during respirator treatment: a hermeneutic observation study. Intensive Crit Care Nurs. 2012;28:197–207. doi: 10.1016/j.iccn.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Blackstone SW, Pressman H. Patient communication in health care settings: new opportunities for augmentative and alternative communication. Augment Altern Commun. 2016;32:69–79. doi: 10.3109/07434618.2015.1125947. [DOI] [PubMed] [Google Scholar]
- 6.Dithole K, Sibanda S, Moleki MM, Thupayagale-Tshweneagae G. Exploring communication challenges between nurses and mechanically ventilated patients in the intensive care unit: a structured review. Worldviews Evid Based Nurs. 2016;13:197–206. doi: 10.1111/wvn.12146. [DOI] [PubMed] [Google Scholar]
- 7.Foà C, Cavalli L, Maltoni A, Tosello N, Sangilles C, Maron I, et al. Communications and relationships between patient and nurse in intensive care unit: knowledge, knowledge of the work, knowledge of the emotional state. Acta Biomed. 2016;87:71–82. [PubMed] [Google Scholar]
- 8.Martinho CI, Rodrigues IT. Communication of mechanically ventilated patients in intensive care units. Rev Bras Ter Intensiva. 2016;28:132–40. doi: 10.5935/0103-507X.20160027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carruthers H, Astin F, Munro W. Which alternative communication methods are effective for voiceless patients in intensive care units? A systematic review. Intensive Crit Care Nurs. 2017;42:88–96. doi: 10.1016/j.iccn.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 10. Burkhart LJ. What is AAC? [Internet]. International Society for Augmentative and Alternative Communication; 2018 [cited 2022 Dec 1]. Available from: https://www.isaac-online.org/english/what-is-AAC.
- 11.Leung CC, Pun J, Lock G, Slade D, Gomersall CD, Wong WT, et al. Exploring the scope of communication content of mechanically ventilated patients. J Crit Care. 2018;44:136–41. doi: 10.1016/j.jcrc.2017.10.044. [DOI] [PubMed] [Google Scholar]
- 12.Holm A, Viftrup A, Karlsson V, Nikolajsen L, Dreyer P. Nurses' communication with mechanically ventilated patients in the intensive care unit: umbrella review. J Adv Nurs. 2020;76:2909–20. doi: 10.1111/jan.14524. [DOI] [PubMed] [Google Scholar]
- 13.Holm A, Dreyer P. Intensive care unit patients' experience of being conscious during endotracheal intubation and mechanical ventilation. Nurs Crit Care. 2017;22:81–8. doi: 10.1111/nicc.12200. [DOI] [PubMed] [Google Scholar]
- 14.Dithole KS, Sibanda S, Moleki MM, Thupayagale-Tshweneagae G. Nurses' communication with patients who are mechanically ventilated in intensive care: the Botswana experience. Int Nurs Rev. 2016;63:415–21. doi: 10.1111/inr.12262. [DOI] [PubMed] [Google Scholar]
- 15.Happ MB. Giving voice: nurse-patient communication in the intensive care unit. Am J Crit Care. 2021;30:256–65. doi: 10.4037/ajcc2021666. [DOI] [PubMed] [Google Scholar]
- 16.Fleischer S, Berg A, Zimmermann M, Wüste K, Behrens J. Nurse-patient interaction and communication: A systematic literature review. J Pub Health. 2009;17:339–53. [Google Scholar]
- 17.Nilsen ML, Sereika SM, Hoffman LA, Barnato A, Donovan H, Happ MB. Nurse and patient interaction behaviors' effects on nursing care quality for mechanically ventilated older adults in the ICU. Res Gerontol Nurs. 2014;7:113–25. doi: 10.3928/19404921-20140127-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 19.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141–6. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 20.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 21.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Page MJ, Shamseer L, Tricco AC. Registration of systematic reviews in PROSPERO: 30,000 records and counting. Syst Rev. 2018;7:32. doi: 10.1186/s13643-018-0699-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today. 2017;56:29–34. doi: 10.1016/j.nedt.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Tembo AC, Higgins I, Parker V. The experience of communication difficulties in critically ill patients in and beyond intensive care: findings from a larger phenomenological study. Intensive Crit Care Nurs. 2015;31:171–8. doi: 10.1016/j.iccn.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Karlsen MW, Ølnes MA, Heyn LG. Communication with patients in intensive care units: a scoping review. Nurs Crit Care. 2019;24:115–31. doi: 10.1111/nicc.12377. [DOI] [PubMed] [Google Scholar]
- 26.Wallander Karlsen MM, Heggdal K, Finset A, Heyn LG. Attention-seeking actions by patients on mechanical ventilation in intensive care units: a phenomenological-hermeneutical study. J Clin Nurs. 2019;28:66–79. doi: 10.1111/jocn.14633. [DOI] [PubMed] [Google Scholar]
- 27.Happ MB, Garrett K, Thomas DD, Tate J, George E, Houze M, et al. Nurse-patient communication interactions in the intensive care unit. Am J Crit Care. 2011;20:e28–40. doi: 10.4037/ajcc2011433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meriläinen M, Kyngäs H, Ala-Kokko T. Patients' interactions in an intensive care unit and their memories of intensive care: a mixed method study. Intensive Crit Care Nurs. 2013;29:78–87. doi: 10.1016/j.iccn.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Salem A, Ahmad MM. Communication with invasive mechanically ventilated patients and the use of alternative devices: integrative review. J Res Nurs. 2018;23:614–30. doi: 10.1177/1744987118785987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bayog KM, Bello DM, Benabaye JM, Benegas TM, Benito AL, Berioso MA, et al. A conjoint analysis of the communication preferences of registered nurses towards mechanically ventilated patients. Int J Nurs Pract. 2020;26:e12809. doi: 10.1111/ijn.12809. [DOI] [PubMed] [Google Scholar]
- 31.Momennasab M, Ardakani MS, Rad FD, Dokoohaki R, Dakhesh R, Jaberi A. Quality of nurses' communication with mechanically ventilated patients in a cardiac surgery intensive care unit. Invest Educ Enferm. 2019;37:e02. doi: 10.17533/udea.iee.v37n2e02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nilsen ML, Sereika S, Happ MB. Nurse and patient characteristics associated with duration of nurse talk during patient encounters in ICU. Heart Lung. 2013;42:5–12. doi: 10.1016/j.hrtlng.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khalaila R, Zbidat W, Anwar K, Bayya A, Linton DM, Sviri S. Communication difficulties and psychoemotional distress in patients receiving mechanical ventilation. Am J Crit Care. 2011;20:470–9. doi: 10.4037/ajcc2011989. [DOI] [PubMed] [Google Scholar]
- 34.Ten Hoorn S, Elbers PW, Girbes AR, Tuinman PR. Communicating with conscious and mechanically ventilated critically ill patients: a systematic review. Crit Care. 2016;20:333. doi: 10.1186/s13054-016-1483-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grossbach I, Stranberg S, Chlan L. Promoting effective communication for patients receiving mechanical ventilation. Crit Care Nurse. 2011;31:46–60. doi: 10.4037/ccn2010728. [DOI] [PubMed] [Google Scholar]
- 36.Dithole KS, Thupayagale-Tshweneagae G, Akpor OA, Moleki MM. Communication skills intervention: promoting effective communication between nurses and mechanically ventilated patients. BMC Nurs. 2017;16:74. doi: 10.1186/s12912-017-0268-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Happ MB, Garrett KL, Tate JA, DiVirgilio D, Houze MP, Demirci JR, et al. Effect of a multi-level intervention on nurse-patient communication in the intensive care unit: results of the SPEACS trial. Heart Lung. 2014;43:89–98. doi: 10.1016/j.hrtlng.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Noguchi A, Inoue T, Yokota I. Promoting a nursing team's ability to notice intent to communicate in lightly sedated mechanically ventilated patients in an intensive care unit: an action research study. Intensive Crit Care Nurs. 2019;51:64–72. doi: 10.1016/j.iccn.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 39.Gorzin K, Sanagoo A, Jouybari L, Pahlavanzadeh B, Jesmi AA. The effect of education on function and communication skill of nurse with intubated patient in intensive care unit. J Nurs Midwifery Sci. 2020;7:84–7. [Google Scholar]
- 40.Walker LO, Avant KC. Strategies for theory construction in nursing. Pearson; 2005. [Google Scholar]
- 41.Wanko Keutchafo EL, Kerr J, Jarvis MA. Evidence of nonverbal communication between nurses and older adults: a scoping review. BMC Nurs. 2020;19:53. doi: 10.1186/s12912-020-00443-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abdolrahimi M, Ghiyasvandian S, Zakerimoghadam M, Ebadi A. Therapeutic communication in nursing students: a Walker & Avant concept analysis. Electron Physician. 2017;9:4968–77. doi: 10.19082/4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xue W, Heffernan C. Therapeutic communication within the nurse-patient relationship: a concept analysis. Int J Nurs Pract. 2021;27:e12938. doi: 10.1111/ijn.12938. [DOI] [PubMed] [Google Scholar]
- 44.Guttormson JL, Bremer KL, Jones RM. "Not being able to talk was horrid": a descriptive, correlational study of communication during mechanical ventilation. Intensive Crit Care Nurs. 2015;31:179–86. doi: 10.1016/j.iccn.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist
The search strategy of the study