Abstract
Objectives:
Improving family-centered outcomes is a priority in oncologic critical care. As part of the Intensive Care Unit Patient-Centered Outcomes Research ICU Collaborative, we implemented patient and family-centered initiatives in a comprehensive cancer center.
Methods:
A multidisciplinary team was created to implement the initiatives. We instituted an open visitation policy (OVP), revamped the use of the two-way communication boards, and enhanced the waiting room experience by hosting ICU family-centered events. To assess the initiatives’ effects, we carried out pre-intervention (PRE) and post-intervention (POST) family/caregiver and ICU practitioner surveys.
Results:
A total of 159 (PRE=79, POST=80) family members and 147 (PRE=95, POST=52) ICU practitioners participated. Regarding the decision-making process, family members felt more included (40.5% vs 68.8%, p<0.001), and more supported (29.1% vs 48.8%, p=0.011) after the implementation of the initiatives. The caregivers also felt more control over the decision-making process in the POST survey (34.2% vs 56.3%, p=0.005). Although 33% of the ICU staff considered OVP beneficial for the ICU, 41% disagreed and 26% were neutral. Only half of them responded that OVP was beneficial for patients, and 63% agreed that OVP was beneficial for families. Half of the practitioners agreed that OVP resulted in additional work for staff.
Significance of results:
Our project effectively promoted patient and family-centered care. The families expressed satisfaction with the communication of information and the decision-making process. However, the ICU staff felt the initiatives increased their work load. Further research is needed to understand whether making this project universal or introducing additional novel practices would significantly benefit patients admitted to the ICU and their family.
Keywords: Intensive care unit, critical care, family engagement, family centered care, quality improvement
Introduction
Caregivers of cancer patients suffer a profound impact on their well-being and quality of life (Girgis et al., 2013; Sun et al., 2019). Their emotional burden worsens when their loved one is hospitalized and requires an intensive care unit (ICU) admission. Moreover, as the cancer population is at high risk of developing life-threatening events that require intensive care treatment (Cuenca et al., 2020; Gutierrez et al., 2018; Wallace et al., 2016), developing and enacting better family-centered care strategies for critically ill cancer patients is paramount. Increasing family engagement has been associated with a shorter ICU stay (Lee et al., 2019), decreased cardio-circulatory complications (Fumagalli et al., 2006), and reduced patient falls (Dupree et al., 2014) without increasing infections rate or adverse events (Adams et al., 2011; Bishop et al., 2013).
Historically, ICUs have maintained strict policies about visitation and family-centered care (Liu et al., 2013). However, the belief that patients in the ICU benefit from restricted visitation has been contradicted by evidence that social isolation can increase morbidity and mortality (Cacioppo et al., 2011). The COVID-19 pandemic has highlighted the various deleterious psychological effects that prohibiting visitation can generate in patients, families, and healthcare providers (Azoulay et al., 2021). The Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU suggest that family members of critically ill patients be “offered open or flexible family presence at the bedside” (Davidson et al., 2017). Despite this, hospitals’ visitation policies in their ICUs still vary widely (Liu et al., 2013). Strict visitation policies cause the families to stay mainly in the ICU waiting room, making them feel less engaged with the care of their loved ones (Davidson et al., 2017). For these reasons, waiting rooms should be a place of comfort with nearby restrooms and places to eat, and should post easily read signage to help family members navigate around (Deitrick et al., 2005; Karlsson et al., 2011).
To enhance the ICU family engagement and overall satisfaction of care by patients and their families, we participated in a national performance improvement study called the Patient-Centered Outcomes Research (PCOR) Collaborative (Kleinpell et al., 2019). We implemented a multilevel patient and family-centered initiatives that were focused on (1) applying an open visitation policy, (2) using daily two-way communication boards, and (3) enhancing the ICU waiting room experience. Here, we report the perspectives of both the families and the ICU practitioners on these performance improvement initiatives.
Methods
Study Design and Setting
This “before and after” performance improvement multilevel intervention study was approved by the Qualitative Institutional Review Board and was conducted in the 34-bed medical and 18-bed surgical ICUs at the University of Texas MD Anderson Cancer Center. A multidisciplinary workgroup consisting of physicians, nurses, advanced practice providers, pharmacists, physical therapists, occupational therapists, dieticians, patient educators, patient advocates, chaplains, social workers, ethicists, and volunteer services was formed. The workgroup was involved in planning, addressing concerns, enabling information dissemination, and implementing patient and family-centered care initiatives. In order to achieve a substantial improvement in family-centered care, the team decided to execute multiple initiatives simultaneously in a multilevel fashion.
To be considered eligible to participate in the study, respondents must have been caregivers of a patient admitted to the ICU or a healthcare provider who primarily worked in the ICU. We conducted pre-intervention (PRE) and the post-intervention (POST) surveys for families of patients admitted to the ICU and for ICU practitioners. The PRE surveys were carried out one month before the implementation period. At the same time, the institution renovated the ICUs and waiting rooms following the SCCM ICU design guidelines (Thompson et al., 2012). After a 6-month implementation period, the POST surveys were conducted. Consequently, there were two separate groups of family members who responded to the surveys (Figure 1). Potential participants were approached by the research team, only those who were willing to participate in the study were offered the links to the survey. The web secure database REDCap was used to anonymously collect and store all the survey data.
Figure 1.
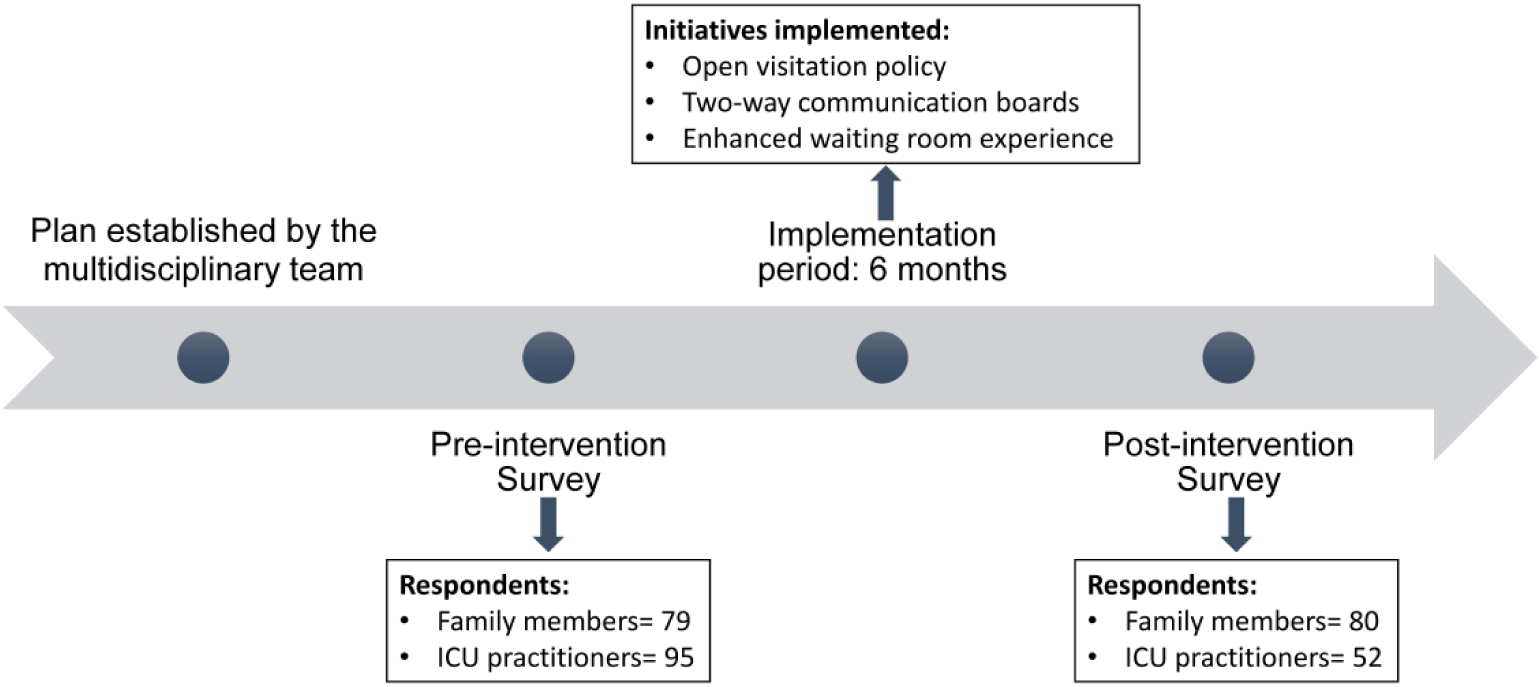
Study schema.
Initiatives
Open visitation policy:
A visitor pass system was implemented that allowed each family to have two passes to the ICU. One was a 24-hour pass, allowing one family member to stay in the patient’s room at any time during the day or night. The second pass allowed a second family member to be in the patient’s room between 10:00 AM and 10:00 PM.
Two-way communication boards:
We implemented this initiative early to optimize communication between patients, families, and caregivers. Daily goals were established for every patient during multidisciplinary rounds in the morning. Nurses updated the daily goals board with a minimum of two to three goals to be accomplished for the day, and subsequently, with a multidisciplinary approach, the ICU team addressed the goals with patients and families. Audits were performed daily to identify and overcome potential barriers. Patients and families were encouraged to write questions or concerns to the ICU team on the board.
Enhanced waiting room experience:
We worked with Volunteer Services to provide therapeutic coloring books and daily coffee services to the waiting room. A comprehensive calendar was created to inform family members of events they could participate in free of charge. We held events such as ICU family celebrations, card-making sessions, and holiday music therapy sessions directed by a certified Music Therapist. The calendar also included MD Anderson’s Integrative Medicine Program events such as yoga meditation, drumming sessions, Tai Chi, group singing, and cooking lessons.
Surveys
The PCOR collaborative leadership provided the surveys for this study (Kleinpell et al., 2019). The family/caregiver participants’ surveys were based on the Family Satisfaction with Care in the ICU Survey (Wall et al., 2007), which has well-established reliability and validity (Kleinpell et al., 2019). The questions addressed demographic information, staff competence, treatment of family, communication, waiting area environment, and overall family satisfaction. The ICU practitioners responded to The Patient- and Family-Centered Adult Intensive Care: A Self-Assessment Inventory (A Self-Assessment Inventory, 2019). The questions inquired about demographics such as age, sex, ICU practitioner role, years of practice, experience in the ICU, personal and professional experience with family presence, and family-centered care integration. Additionally, both the caregivers’ and practitioners’ POST surveys also included specific questions evaluating the implemented local initiatives (Kleinpell et al., 2019). All surveys were based on a Likert scale.
Statistical Analysis
Descriptive analyses were performed for patients’ family and ICU practitioner demographics and responses. For categorical variables, counts and frequencies were reported. Frequencies were calculated based on the non-missing values. For continuous variables, mean and standard deviation were reported. Differences between the PRE and POST intervention surveys were calculated using the Chi square test. All statistical analyses were performed using the statistical software IBM SPPS Statistics for Windows, version 25 (SPSS Inc., Chicago, USA).
Results
A total of 159 (PRE=79 and POST=80) family members completed the surveys. Table 1 describes the demographics and basic information of the participants. The families’/caregivers’ roles included daughter (21%), wife (17%), son (13%), parent (8%), husband (5%). “Others” involved extended family members (partner, brother, sister, other) (18%). Almost half of the caregivers (50.9%) had previous experience caring for a family member in the ICU. Approximately 42% of the caregivers lived with the patients. A total of 147 (PRE=95 and POST=52) ICU practitioners participated in the surveys. Most of them were nurses (43%), followed by advanced practice providers (12%), clinical pharmacists (12%), physicians (9%), respiratory therapists (9%), and others such as occupational therapists, speech therapists, and dieticians (15%).
Table 1.
Demographics and basic information of the participants.
| Family members | PRE N= 79 | % | POST N= 80 | % |
|
| ||||
| Age (years), Mean (SD) | 47.98 | (±15.23) | 47.1 | (±14.86) |
| Sex | ||||
| Female | 54 | 68.35 | 48 | 60 |
| Male | 25 | 31.65 | 32 | 40 |
| Relationship to patient | ||||
| Husband | 6 | 7.59 | 3 | 3.75 |
| Wife | 21 | 26.58 | 6 | 7.5 |
| Partner | 1 | 1.27 | 1 | 1.25 |
| Brother | 5 | 6.33 | 9 | 11.25 |
| Sister | 4 | 5.06 | 8 | 10 |
| Daughter | 16 | 20.25 | 18 | 22.5 |
| Son | 8 | 10.13 | 12 | 15 |
| Father | 3 | 3.80 | 0 | 0 |
| Mother | 4 | 5.06 | 6 | 7.5 |
| Other | 11 | 13.92 | 17 | 21.25 |
| Before this most recent event, have you been involved as a family member of a patient in an ICU? | ||||
| Yes | 45 | 56.96 | 36 | 45 |
| No | 34 | 43.04 | 44 | 55 |
| Do you live with the patient? | ||||
| Yes | 38 | 48.1 | 28 | 35 |
| No | 41 | 51.9 | 52 | 65 |
|
| ||||
| ICU practitioners | PRE N= 95 | % | POST N= 52 | % |
|
| ||||
| Age in years, Mean (SD) | 38.86 | (±10.54) | 41.13 | (±12.10) |
| Sex | ||||
| Female | 74 | 77.89 | 37 | 71.15 |
| Male | 13 | 13.68 | 9 | 17.31 |
| Prefer not to answer | 8 | 8.42 | 6 | 11.54 |
| Clinical role | ||||
| Advanced practice nurse | 6 | 6.45 | 7 | 13.21 |
| Nurse | 40 | 43.01 | 28 | 52.83 |
| Clinical pharmacist | 11 | 11.83 | 3 | 5.66 |
| Physician | 8 | 8.6 | 9 | 16.98 |
| Physician assistant | 5 | 5.38 | 1 | 1.89 |
| Occupational therapist | 8 | 8.60 | 1 | 1.89 |
| Other | 17 | 16.13 | 3 | 7.55 |
| Total years working in an ICU setting, Mean (SD) | 9.28 | (±8.08) | 10.73 | (±7.25) |
| Years working in the current ICU, Mean (SD) | 6.06 | (±5.67) | 6.8 | (±5.46) |
ICU: Intensive Care Unit
Family members’ perspectives
Overall, in the 159 caregivers (PRE and POST combined), the “excellent” to “very good” response for “ease of getting information” was 72%. The “fair” to “poor” response was 8%. The “excellent” to “very good” responses for “understanding of information” were 74%, and the “fair” to “poor” responses were 5%. Regarding their understanding of information, 74% of the participants rated it as “excellent” or “very good”, and just 5% considered it “fair” or “poor”. About 73% of caregivers responded “excellent” to “very good” with regard to the “completeness of information,” indicating that most family members were satisfied with how well the information regarding their loved ones was conveyed to them by the care team. A much lower percentage of respondents (8%) reported that “completeness of information” was “fair” to “poor.” Most (71%) of the families were satisfied with the “consistency of information,” indicating that they received similar messages from doctors and nurses, etc. A very small portion of relatives (9%) responded “fair” to “poor.” About 59% of families responded “excellent” to “very good” about the “frequency with which ICU doctors communicated information.” A few families (15%) felt less satisfied, responding “fair” to “poor.” The “excellent” to “good” response for family care and concern by ICU staff was 91%. The responses of the family members by PRE and POST are summarized in Table 2. Overall, the “excellent” response rate increased from PRE to POST, however, none of the improvements were statistically significant.
Table 2.
Family members’ perspectives on information dissemination and decision making process.
| PRE N= 79 | % | POST N= 80 | % | |
|---|---|---|---|---|
|
| ||||
| Ease of getting information | ||||
| Excellent | 31 | 39.2 | 38 | 48.7 |
| Very good | 25 | 31.6 | 19 | 24.4 |
| Good | 14 | 17.7 | 17 | 21.8 |
| Fair | 8 | 10.1 | 3 | 3.8 |
| Poor | 1 | 1.3 | 1 | 1.3 |
| N/A | 0 | - | 2 | - |
| Understanding of information | ||||
| Excellent | 33 | 41.8 | 37 | 47.4 |
| Very good | 27 | 34.2 | 19 | 24.4 |
| Good | 15 | 19 | 18 | 23.1 |
| Fair | 4 | 5.1 | 3 | 3.8 |
| Poor | 0 | 0 | 1 | 1.3 |
| N/A | 0 | - | 2 | - |
| Completeness of information | ||||
| Excellent | 33 | 41.8 | 44 | 56.4 |
| Very good | 24 | 30.4 | 14 | 17.9 |
| Good | 15 | 19.0 | 14 | 17.9 |
| Fair | 7 | 8.9 | 4 | 5.1 |
| Poor | 0 | 0.0 | 2 | 2.6 |
| N/A | 0 | - | 2 | - |
| Consistency of information | ||||
| Excellent | 30 | 38.5 | 35 | 46.1 |
| Very good | 24 | 30.8 | 20 | 26.3 |
| Good | 17 | 21.8 | 14 | 18.4 |
| Fair | 6 | 7.7 | 6 | 7.9 |
| Poor | 1 | 1.3 | 1 | 1.3 |
| N/A | 1 | - | 4 | - |
| Did you feel included in decision making process? | ||||
| Very included | 32 | 40.5 | 55 | 68.8 |
| Somewhat included | 28 | 35.4 | 12 | 15 |
| I felt neither included nor excluded | 12 | 15.2 | 6 | 7.5 |
| Somewhat excluded | 3 | 3.8 | 4 | 5 |
| Very excluded | 4 | 5.1 | 3 | 3.8 |
| Did you feel supported during the decision making process? | ||||
| I felt very supported | 23 | 29.1 | 39 | 48.8 |
| I felt supported | 35 | 44.3 | 27 | 33.8 |
| I felt neither overwhelmed nor supported | 15 | 19 | 8 | 10 |
| I felt somewhat overwhelmed | 4 | 5.1 | 5 | 6.3 |
| I felt totally overwhelmed | 2 | 2.5 | 1 | 1.3 |
| Did you feel you had control over the care of your family member? | ||||
| I felt I had good control | 27 | 34.2 | 45 | 56.3 |
| I felt I had some control | 28 | 35.4 | 20 | 25 |
| I felt neither in control nor out of control | 16 | 20.3 | 9 | 11.3 |
| I felt somewhat out of control | 5 | 6.3 | 4 | 5 |
| I felt really out of control | 3 | 3.8 | 2 | 2.5 |
| Did you have adequate time to have your concern addressed and questions answered? | ||||
| I had adequate time | 72 | 91.1 | 66 | 82.5 |
| I could have used more time | 7 | 8.9 | 14 | 17.5 |
ICU: Intensive Care Unit. N/A responses were excluded from the frequency calculations.
Most of the relatives (80%) felt included in the decision-making process (“very” 55%, “somewhat included” 25%). Fewer relatives felt excluded (9%). There was a statistically significant increase in the rate of “very included” in the decision-making process from the PRE to POST (p<0.001). A considerable number (78%) felt supported during the process, whereas 8% felt totally or somewhat overwhelmed. A significantly higher rate of participants felt very supported (p=0.011) after the implementation of the initiatives. About half (45%) of the relatives believed that they had good control of the process, whereas 30% felt less in control, and just 9% felt that the process was somewhat or completely out of their control. The proportion of respondents who felt in control of the process in the POST survey was higher than in the PRE survey (p=0.005). About 13% of the caregivers believed that they needed more time to make decisions or to discuss or address their concerns.
Caregivers’ perspectives regarding the ICU waiting room areas, OVP, and daily goal boards are presented in the Supplemental Table 1. Among the 159 caregivers (PRE and POST combined) who responded to the survey, 71% considered their satisfaction with the ICU waiting area environment to be “excellent” or “very good”. Most respondents described access to the kitchen (69%), nutritious snacks (75%), and laundry facilities (77%) as “very well” to “ok”. Regarding access to place for prayer or reflection, the majority (95%) reported “very well” to “ok” responses. Overall, the “excellent” and “very well” responses rate increased from PRE to POST, however only access to kitchen facilities (p<0.001) and nutritious snacks (p=0.008) were statistically significant. In the POST survey, the families evaluated the OVP and daily board goals. Over half of the respondents knew that the visitation policies had relaxed recently (60.7%), most of them were satisfied with the OVP (89%) and believed the OVP was helpful for them and their loved ones (87.6%). Likewise, the majority of the participants (77.4%) were aware of the use of the daily goal boards, liked it (81.9%), and agreed that it was helpful for them and their loved ones (81.9%).
ICU practitioners’ perspectives
The ICU practitioners’ perspectives regarding the initiatives are presented in Table 3. Among the 147 respondents (PRE and POST combined), 38% preferred an OVP in the ICU, whereas 42% were in disagreement, and 19% were neutral. Regarding communication with family, 42% of providers believed that the OVP improved it, while 31% disagreed. Almost a quarter of the practitioners (23%) thought that patient care was improved with OVP, whereas 37% disagreed and 40% were neutral. Although 33% responded that OVP was beneficial for the ICU, 41% disagreed and 26% were neutral. In addition, half of them responded that OVP was beneficial for patients, whereas 29% disagreed and 21% were neutral. Most (63%) practitioners agreed that OVP was beneficial for families despite over half of them (51%) believing that it could result in additional work for staff.
Table 3.
ICU practitioners’ perspectives about the initiatives
| Open visitation policy | Communication board | |||
|---|---|---|---|---|
| N= 52 | % | N= 52 | % | |
|
| ||||
| Preference for the initiative | ||||
| Strongly agree | 9 | 17.3 | 19 | 38 |
| Somewhat agree | 11 | 21.2 | 16 | 32 |
| Neutral | 10 | 19.2 | 13 | 26 |
| Somewhat disagree | 12 | 23.1 | 1 | 2 |
| Strongly disagree | 10 | 19.2 | 1 | 2 |
| N/A | 0 | - | 2 | - |
| Communication with family improves | ||||
| Strongly agree | 8 | 15.4 | 8 | 15.7 |
| Somewhat agree | 14 | 26.9 | 16 | 31.4 |
| Neutral | 14 | 26.9 | 15 | 29.4 |
| Somewhat disagree | 9 | 17.3 | 8 | 15.7 |
| Strongly disagree | 7 | 13.5 | 4 | 7.8 |
| N/A | 0 | - | 1 | - |
| Patient care improves | ||||
| Strongly agree | 3 | 5.8 | 7 | 13.5 |
| Somewhat agree | 9 | 17.3 | 11 | 21.1 |
| Neutral | 21 | 40.4 | 15 | 28.9 |
| Somewhat disagree | 12 | 23.1 | 14 | 26.9 |
| Strongly disagree | 7 | 13.5 | 5 | 9.6 |
| Beneficial for ICU | ||||
| Strongly agree | 5 | 9.8 | 10 | 19.2 |
| Somewhat agree | 12 | 23.5 | 21 | 40.4 |
| Neutral | 13 | 25.5 | 11 | 21.2 |
| Somewhat disagree | 15 | 29.4 | 7 | 13.5 |
| Strongly disagree | 6 | 11.8 | 3 | 5.8 |
| N/A | 1 | - | 0 | - |
| Beneficial for patients | ||||
| Strongly agree | 9 | 17.3 | 11 | 21.6 |
| Somewhat agree | 17 | 32.7 | 20 | 39.2 |
| Neutral | 11 | 21.2 | 12 | 23.5 |
| Somewhat disagree | 11 | 21.2 | 5 | 9.8 |
| Strongly disagree | 4 | 7.7 | 3 | 5.9 |
| N/A | 0 | - | 1 | - |
| Beneficial for families | ||||
| Strongly agree | 14 | 26.9 | 8 | 15.7 |
| Somewhat agree | 19 | 36.5 | 30 | 58.8 |
| Neutral | 12 | 23.1 | 9 | 17.7 |
| Somewhat disagree | 4 | 7.7 | 2 | 3.9 |
| Strongly disagree | 3 | 5.8 | 2 | 3.9 |
| N/A | 0 | - | 1 | - |
| More work for staff | ||||
| Strongly agree | 13 | 25.5 | 3 | 5.8 |
| Somewhat agree | 13 | 25.5 | 16 | 30.8 |
| Neutral | 15 | 29.4 | 10 | 19.2 |
| Somewhat disagree | 7 | 13.7 | 16 | 30.8 |
| Strongly disagree | 3 | 5.9 | 7 | 13.5 |
| N/A | 1 | - | 0 | - |
ICU: Intensive Care Unit. N/A responses were excluded from the frequency calculations.
The use of the two-way communication boards was supported by 70% of the 147 responders, 26% were neutral and only 4% were in disagreement. While almost half of the ICU practitioners (47%) believed that the board improved communication with patients’ families, only 23% disagreed. More than a third (35%) of the clinicians agreed that patient care improved; however, 65% were either neutral or in disagreement. Even though most of the responders believed it was beneficial for the unit (60%), the patients (61%) and the families (75%); a third agreed that the two-way communication boards created more work for the staff.
Discussion
Our findings suggest that the implementation of OPV, the two-way communication board, and a revamped waiting room experience enhanced communication and engagement between the family members/caregivers and the medical team. For instance, family members felt significantly more included and supported during the clinical decision-making process, which leads to a higher perception of control over medical decisions. Additionally, the three studied initiatives were well received by the family members. On the other hand, among ICU practitioners, the two-way communication board was more accepted than the OVP. More than half of the ICU practitioners believed the two-way communication boards were beneficial for the unit and the patients. Even though half of the practitioners believed OVP created additional work for the staff, nearly two-thirds of them also considered this initiative beneficial for the family members. Interestingly, 61.5% of the clinicians (16 out of 26) who believed OVP created more work also considered it beneficial to the families.
Improving patient and family-centered outcomes requires a multidisciplinary and coordinated effort. A multilevel approach was selected for this study due to the various facets involved, such as individual caregiver characteristics, medical team interactions, organizational logistics, and institutional policies. Each intervention aimed to improve a different level of influence. For instance, from an organizational level, we enacted an open visitation policy; from a healthcare team level, we implemented the two-way communication boards; and from the families’ environmental level, we renovated the waiting room areas. Despite the potential advantages of conducting multilevel intervention research, interpreting its results is challenging (Clauser et al., 2012; Paskett et al., 2016).
This project resulted in several steps toward improved patient and family-centered intensive care management in cancer patients. Our experience correlates with the growing interest and acceptance of empowering and engaging families and patients by ICU staff (Kleinpell et al., 2018; Naef et al., 2020, 2021). Despite the beneficial effects, we encountered barriers with our project. Notably, the ICU staff expressed concerns that the initiatives added additional work strain. There might be some potential explanations for the ICU staff’s perception regarding the OVP. First, the use of the ICU visitation passes required the staff to keep track of whether the caregivers were authorized to enter the ICU. Second, sometimes the family members who stayed overnight would accidentally forget to hand over the pass to the following designated caregiver. Dealing with this created unplanned discussions with the family to solve the issue. Third, some caregivers gained entrance to the unit through other entrances not available to the public, which could have made the practitioners feel that their efforts to provide a structured OVP were futile. This phenomenon is not unique to our project. Previous studies have reported the nursing staff concerns that more liberal visitation policies may interfere with their ability to provide excellent patient care (Berti et al., 2007; Kozub et al., 2017). However, ICUs with open visitation reported that families were highly satisfied with the policy (Chapman et al., 2016; Soury-Lavergne et al., 2012). Physicians and nurses in open visitation ICUs tended to view the policy positively as well (Chapman et al., 2016; Giannini et al., 2013).
We also faced difficulties implementing the two-way communication boards. The most commonly reported difficulty by the nursing staff was when other patients occasionally required their attention during rounds, precluding the nurse from writing down that particular patient’s goal or taking the extra time to talk to the team and address the family. Despite these issues, family members felt more included in the discussions, which is consistent with the literature. Pronovost et al. carried out a prospective study in which the implementation of daily goals form resulted in all staff having a better understanding of the goals for individual patients and improved information traffic and communication between families and staff (Pronovost et al., 2003). Additionally, another study reported that implementing ICU daily goals boards decreased the hospital length of stay and reduced errors of omission (Binnekade et al., 2010).
In light of the obstacles we faced, there is a need to promote the higher acceptance of patient and family-centered outcomes among the ICU staff. Addressing logistical and operational hurdles expressed by the staff should be a priority. Failing to show willingness to hear their input to improve the initiatives’ workflow could lead to a loss of support from the staff. Another potential action that should be considered is conducting educational sessions about patient-centered outcomes, as this seems to be a viable alternative to reach wider acceptance among the practitioners (Coyne and Dieperink, 2017; Nguyen et al., 2017).
Other initiatives to improve patients’ and families’ experience in the critical care-related facilities are currently being analyzed before introduction in our unit. For instance, specialized care packages could be provided to the family/caregiver when transitioning to comfort care. This gesture can be used to educate and offer a more empathetic environment for patients, families, and staff during the bereavement process (Oliver et al., 2010). Another strategy is introducing the ICU diary to help support patients and families during their ICU stay. The ICU diary can provide resources for caregiver support and the prevention and management of ICU delirium (Rogan et al., 2020). Furthermore, the implementation of ICU diaries could also nurture communication and journaling tools that facilitate mental and physical wellness. Future potential interventions must integrate family-centered outcomes with new technologies such as developing a mobile device application that allows easy access to technological education and frequent ICU questions posed by patients and their caregivers. Due to the wide variability between acceptance and integration of various initiatives, further research on different strategies to successfully increase patient and family engagement is essential.
The present study has several limitations. First, we encountered resistance to cultural change when staff put up barriers to engagement with two-way communication boards. Second, the multilevel implementation of concurrent patient-centered interventions at once made it difficult to isolate the potential beneficial effects of any single measure. Our study could have benefitted from a multilevel regression analysis that could in part isolate the effect of each intervention. Third, due to the nature of the study, different families were surveyed before and after the program was enacted. Thus, differences found between the PRE and POST surveys could have arisen from individual inherent factors of the two groups of respondents rather than being a product of the interventions. Fourth, our institution already had high interaction between patient families and ICU practitioners. Thus, this high baseline engagement could have skewed the observed effect. Therefore, our findings should be cautiously interpreted. For instance, the improvement in family communication and engagement and the higher work burden expressed by practitioners in our study might not be similar if the interventions were implemented in different settings such as community nonspecialized cancer centers. Further research should address these concerns.
Conclusions
Our project effectively promoted patient and family-centered care. The families expressed satisfaction with the communication of information and the decision-making process. Even though more than half of the practitioners agreed that an OVP was beneficial for families, there was a concern that it could create an additional burden to the staff. Practitioners were generally against implementing an OVP and did not believe it would help in patient care. The majority of practitioners supported the use of the two-way communication board which helped transfer information to families and improved their satisfaction. Finally, the added features in the ICU waiting room led to positive changes in family satisfaction. However, due to our limitations, further research is needed to understand whether making this project universal or introducing additional novel practices would significantly benefit patients and families in the ICU.
Supplementary Material
Acknowledgements:
Disclosures and acknowledgements
We appreciate the contributions of Mary Ann Oler, education program coordinator of the Department of Critical Care and Respiratory Care at The University of Texas MD Anderson Cancer Center, and Tamara K. Locke from the office of Scientific Publications at The University of Texas MD Anderson Cancer Center for their valuable editorial contributions. Part of this work was presented as an abstract in the 49th Annual Critical Care Congress of the Society of Critical Care Medicine, 16–19th February 2020.
Funding:
Supported by the NIH/NCI award number P30CA016672. Dr. Nates’ work is supported by the George Sweeney Fellowship, The University of Texas MD Anderson Cancer Center Grant Resources.
Footnotes
Conflicts of interest: The authors declare no conflict of interest directly applicable to this research.
References
- (2019). A Self-Assessment Inventory. Institute for Patient- and Family-Centered Care: Patient- and Family- Centered Adult Intensive Care. 2019 Available at https://www.ipfcc.org/resources/assessment.html (accessed June 17, 2021). [Google Scholar]
- Adams S, Herrera A, Miller L, and Soto R (2011). Visitation in the Intensive Care Unit. Crit Care Nurs Q 34:3–10. [DOI] [PubMed] [Google Scholar]
- Azoulay É, Curtis JR, and Kentish-Barnes N (2021). Ten reasons for focusing on the care we provide for family members of critically ill patients with COVID-19. Intensive Care Med 47:230–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berti D, Ferdinande P, and Moons P (2007). Beliefs and attitudes of intensive care nurses toward visits and open visiting policy. Intensive Care Med 33:1060–1065. [DOI] [PubMed] [Google Scholar]
- Binnekade JM, Brunsveld A, Arbous S, Dijkgraaf MG, Horn J, Sloot J, Balzereit A, and Vroom MB (2010). Implementation of daily goals in the ICU reduces length of ICU stay and errors of omission in patient care. Crit Care 14:P466. [Google Scholar]
- Bishop SM, Walker MD, and Mark Spivak I (2013). Family presence in the adult burn intensive care unit during dressing changes. Crit Care Nurse 33:14–24. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Norman GJ, and Berntson GG (2011). Social isolation. Ann N Y Acad Sci 1231:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DK, Collingridge DS, Mitchell LA, Wright ES, Hopkins RO, Butler JM, and Brown SM (2016). Satisfaction With Elimination of all Visitation Restrictions in a Mixed-Profile Intensive Care Unit. Am J Crit Care 25:46–50. [DOI] [PubMed] [Google Scholar]
- Clauser SB, Taplin SH, Foster MK, Fagan P, and Kaluzny AD (2012). Multilevel intervention research: Lessons learned and pathways forward. J Natl Cancer Inst - Monogr 2012:127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne E and Dieperink KB (2017). A qualitative exploration of oncology nurses’ family assessment practices in Denmark and Australia. Support Care Cancer 25:559–566. [DOI] [PubMed] [Google Scholar]
- Cuenca JA, Laserna A, Reyes MP, Nates JL, and Botz GH (2020). Critical Care Admission of an HIV Patient with Diabetic Ketoacidosis Secondary to Pembrolizumab. Case Reports Crit Care 2020:8671530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, Cox CE, Wunsch H, Wickline MA, Nunnally ME, Netzer G, Kentish-Barnes N, Sprung CL, Hartog CS, Coombs M, Gerritsen RT, Hopkins RO, Franck LS, Skrobik Y, Kon AA, Scruth EA, Harvey MA, Lewis-Newby M, White DB, Swoboda SM, Cooke CR, Levy MM, Azoulay E, and Curtis JR (2017). Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU. Crit Care Med 45:103–128. [DOI] [PubMed] [Google Scholar]
- Deitrick L, Ray D, Stern G, Fuhrman C, Masiado T, Yaich SL, and Wasser T (2005). Evaluation and recommendations from a study of a critical‐care waiting room. J Healthc Qual 27:17–25. [DOI] [PubMed] [Google Scholar]
- Dupree E, Fritz-Campiz A, and Musheno D (2014). A new approach to preventing falls with injuries. J Nurs Care Qual 29:99–102. [DOI] [PubMed] [Google Scholar]
- Fumagalli S, Boncinelli L, Lo Nostro A, Valoti P, Baldereschi G, Di Bari M, Ungar A, Baldasseroni S, Geppetti P, Masotti G, Pini R, and Marchionni N (2006). Reduced cardiocirculatory complications with unrestrictive visiting policy in an intensive care unit: Results from a pilot, randomized trial. Circulation 113:946–952. [DOI] [PubMed] [Google Scholar]
- Giannini A, Miccinesi G, Prandi E, Buzzoni C, and Borreani C (2013). Partial liberalization of visiting policies and ICU staff: a before-and-after study. Intensive Care Med 39:2180–2187. [DOI] [PubMed] [Google Scholar]
- Girgis A, Lambert S, Johnson C, Waller A, and Currow D (2013). Physical, psychosocial, relationship, and economic burden of caring for people with cancer: A review. J Oncol Pract 9:197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez C, McEvoy C, Mead E, Stephens RS, Munshi L, Detsky ME, Pastores SM, and Nates JL (2018). Management of the Critically Ill Adult Chimeric Antigen Receptor-T Cell Therapy Patient: A Critical Care Perspective. Crit Care Med 46:1402–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson C, Tisell A, Engstrom A, and Andershed B (2011). Family members’ satisfaction with critical care: a pilot study. Nurs Crit Care 16:11–18. [DOI] [PubMed] [Google Scholar]
- Kleinpell R, Heyland DK, Lipman J, Sprung CL, Levy M, Mer M, Koh Y, Davidson J, Taha A, and Curtis JR (2018). Patient and family engagement in the ICU: Report from the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care 48:251–256. [DOI] [PubMed] [Google Scholar]
- Kleinpell R, Zimmerman J, Vermoch KL, Harmon LA, Vondracek H, Hamilton R, Hanson B, and Hwang DY (2019). Promoting Family Engagement in the ICU: Experience from a National Collaborative of 63 ICUs∗. Crit Care Med. [DOI] [PubMed] [Google Scholar]
- Kozub E, Scheler S, Necoechea G, and O’Byrne N (2017). Improving nurse satisfaction with open visitation in an adult intensive care unit. Crit Care Nurs Q 40:144–154. [DOI] [PubMed] [Google Scholar]
- Lee HW, Park Y, Jang EJ, and Lee YJ (2019). Intensive care unit length of stay is reduced by protocolized family support intervention: a systematic review and meta-analysis. Intensive Care Med 45:1072–1081. [DOI] [PubMed] [Google Scholar]
- Liu V, Read J, Scruth E, and Cheng E (2013). Visitation policies and practices in US ICUs. Crit Care 17:R71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naef R, Massarotto P, and Petry H (2020). Family and health professional experience with a nurse-led family support intervention in ICU: A qualitative evaluation study. Intensive Crit Care Nurs 61:102916. [DOI] [PubMed] [Google Scholar]
- Naef R, von Felten S, Petry H, Ernst J, and Massarotto P (2021). Impact of a nurse-led family support intervention on family members’ satisfaction with intensive care and psychological wellbeing: A mixed-methods evaluation. Aust Crit Care. [DOI] [PubMed] [Google Scholar]
- Nguyen TK, Bauman GS, Watling CJ, and Hahn K (2017). Patient- and family-centered care: a qualitative exploration of oncologist perspectives. Support Care Cancer 25:213–219. [DOI] [PubMed] [Google Scholar]
- Oliver MA, Hillock S, Moore C, Goble H, and Asbury N (2010). Comfort care packs: A little bit of hospice in hospital? Int J Palliat Nurs. [DOI] [PubMed] [Google Scholar]
- Paskett E, Thompson B, Ammerman AS, Ortega AN, Marsteller J, and Richardson DJ (2016). Multilevel interventions to address health disparities show promise in improving population health. Health Aff 35:1429–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronovost P, Berenholtz S, Dorman T, Lipsett PA, Simmonds T, and Haraden C (2003). Improving communication in the ICU using daily goals. J Crit Care 18:71–75. [DOI] [PubMed] [Google Scholar]
- Rogan J, Zielke M, Drumright K, and Boehm LM (2020). Institutional Challenges and Solutions to Evidence-Based, Patient-Centered Practice: Implementing ICU Diaries. Crit Care Nurse 40:47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soury-Lavergne A, Hauchard I, Dray S, Baillot ML, Bertholet E, Clabault K, Jeune S, Ledroit C, Lelias I, Lombardo V, Maetens Y, Meziani F, Reignier J, Souweine B, Tabah A, Barrau K, and Roch A (2012). Survey of caregiver opinions on the practicalities of family-centred care in intensive care units. J Clin Nurs 21:1060–1067. [DOI] [PubMed] [Google Scholar]
- Sun V, Raz DJ, and Kim JY (2019). Caring for the informal cancer caregiver. Curr Opin Support Palliat Care 13:238–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson DR, Hamilton DK, Cadenhead CD, Swoboda SM, Schwindel SM, Anderson DC, Schmitz EV, St. Andre AC, Axon DC, Harrell JW, Harvey MA, Howard A, Kaufman DC, and Petersen C (2012). Guidelines for intensive care unit design. Crit Care Med 40:1586–1600. [DOI] [PubMed] [Google Scholar]
- Wall RJ, Engelberg RA, Downey L, Heyland DK, and Curtis RJ (2007). Refinement, scoring, and validation of the Family Satisfaction in the Intensive Care Unit (FS-ICU) survey*. Crit Care Med 35:271–279. [DOI] [PubMed] [Google Scholar]
- Wallace SK, Rathi NK, Waller DK, Ensor JE, Haque SA, Price KJ, Piller LB, Tilley BC, and Nates JL (2016). Two decades of ICU utilization and hospital outcomes in a comprehensive cancer center. Crit Care Med 44:926–933. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


