Abstract
Introduction
Total knee arthroplasty (TKA) is currently regarded as an effective treatment for knee osteoarthritis, relieving patients’ pain and significantly enhancing their quality of life and activity levels, allowing them to return to work and daily life after surgery. However, some TKA patients suffer from varying degrees of postoperative residual pain and opioid abuse, which negatively impacts their recovery and quality of life. It has been reported that preoperative treatment with multimodal analgesics improves postoperative pain and reduces opioid consumption. However, there is no conclusive evidence that pre-emptive analgesia provides the same benefits in TKA. In order to inform future research, this protocol focuses on the efficacy and safety of oral analgesics used in TKA pre-emptive analgesia.
Methods and analysis
We will search the literature on the involvement of pre-emptive analgesia in the management of pain in TKA from the PubMed, EMBASE, MEDLINE, the Cochrane Central Register of Controlled Trials and the Cochrane Database of Systematic Reviews, from their inception to 1 February 2023. Additionally, clinical registry platforms will be investigated to collect data for ongoing studies. Using the Cochrane Risk of Bias Tool, the quality assessment will be conducted. RevMan V.5.4 will be used for the meta-analysis. The statistic I2 will be used to measure the percentage of total variability due to heterogeneity between studies. Where appropriate, subgroup and sensitivity analyses, assessment of evidence quality and publication bias will be conducted.
Ethics and dissemination
No ethical approval and consent is required for this systematic review. Moreover, the results of this systematic review will be disseminated through peer-reviewed publications and conference presentations.
PROSPERO registration number
CRD42022380782.
Keywords: Knee, Anaesthesia in orthopaedics, Pain management
Strengths and limitations of this study.
This is a protocol for a systematic review and meta-analysis of oral multimodal analgesics and postoperative pain after total knee arthroplasty.
A subgroup analyses of confounding factors including age, type of analgesic, duration of treatment, anaesthetic dose, duration of operation, amount of blood loss and duration of follow-up will be performed.
This review protocol is reported referring to the recommendations of the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols.
The inclusion of studies in databases containing only English-language entries may result in potential bias.
Introduction
As the world’s population grows and inevitably ages, the number of people diagnosed with osteoarthritis is expected to rise by 40% by 2035.1 Knee osteoarthritis is a common condition that causes significant pain and disability among patients. According to Murphy et al,2 the lifetime risk of symptomatic knee osteoarthritis is estimated to be approximately 45%. As a result, this patient group constitutes a significant proportion of potential total knee arthroplasty (TKA) candidates. TKA is currently regarded as an effective treatment for knee osteoarthritis, relieving patients’ pain and significantly enhancing their quality of life and activity levels, allowing them to return to work and daily activities after surgery.3 Given the substantial medium-term or long-term benefits of TKA, both clinicians and patients have embraced the procedure.
However, not every patient will recover well. Despite the fact that the success rate of TKA is between 80% and 90%, up to 30% of patients are reported to be dissatisfied. The level of dissatisfaction with pain relief among these individuals ranged from 14% to 28%.4 5 This was primarily due to the persistent postoperative knee pain. Due to the significance of the knee in daily activities, even when mobility is commensurate with activity levels, some TKA patients report significant residual pain, which frequently develops into chronic pain.6 7 Managing pain following knee surgery is another inevitable challenge for clinicians. Because pain is considered a subjective sensation, the degree and threshold of perception vary from person to person; this, combined with the complexity of factors affecting postoperative pain, makes it challenging to analyse and manage pain through specific pain mechanisms.8–10
The various adverse effects of opioid abuse include nausea, vomiting, sedation, intestinal obstruction, respiratory depression and itchiness. Three weeks after hospital discharge, over 70% of post-TKA patients are still taking opioids, according to a survey conducted by the health services.11 According to research conducted in the USA, patients undergoing joint replacement surgery are more likely to consume opioids than those undergoing other surgical procedures.12 13 Both postoperative knee pain and opioid abuse may delay the recovery process, diminish the patient’s postoperative quality of life and even increase the TKA revision rate, thereby increasing the patient’s financial burden. Adoption of a high-quality pain management model is thus an urgent requirement for initial functional recovery after TKA.
Pre-emptive analgesia is an efficient method for achieving rapid postoperative recuperation and optimising pain management. Pre-emptive refers to analgesic interventions administered prior to the onset of noxious stimuli to prevent the development of central sensitisation, incision and inflammatory damage and has been shown to be more effective than the same interventions administered after surgery.14 15 By preventing the sensitisation of the central nervous system caused by painful stimuli, appropriate interventions can attenuate the response to future injurious sensory input and reduce the sensitisation of the central nervous system, so that normally painful stimuli become less painful or even painless. The mechanism of action may involve the inhibition of cytokine and prostaglandin release-induced modifications in central sensory processes, as well as the suppression of inflammatory reactions.16–18 Current research indicates that pre-emptive analgesia can minimise the chance of developing chronic pain, improve pain management and boost the efficacy of other treatment modalities.19 The network meta-analysis (NMA) revealed that various preventive analgesic medicines or strategies reduced postoperative pain, opioid intake and postoperative side effects to diverse degrees.20 As the notion of pre-emptive analgesia has acquired widespread recognition in the field of surgery, the investigation of preemptive analgesia to improve the overall benefit to the postoperative patient has become one of the clinical and scientific hotspots of the moment. Diverse techniques, such as epidural analgesia, peripheral nerve blocks, local infiltration analgesia, opioids, NMDA receptor antagonists and non-steroidal anti-inflammatory drugs, are used for pre-emptive analgesia.21 22 This study focuses on the role of oral medicine as a preventative multimodal analgesic.
Nevertheless, there is debate in the existing literature regarding the efficacy and safety of preventive analgesics. Wang et al examined the efficacy and safety of preoperative selective COX-2 inhibitor administration in TKA patients. A meta-analysis discovered that selective COX-2 inhibitors decreased postoperative pain and opioid intake in TKA patients, but there were no significant differences in time to operation or adverse effects.23 However, in another randomised controlled trial (RCT), Wang et al24 reported that the opioid oxycodone did not produce a substantial pre-emptive analgesic effect in TKA patients. Similar contradictory results were observed in investigations of medications such as gabapentins and acetaminophen.25 Evidently, a rigorous clinical review and evidence validating the efficacy and advantages of pre-emptive analgesia in TKA are still lacking.
The objective of this systematic review and meta-analysis was to evaluate the efficacy of several oral pre-emptive analgesics for the management of pain in TKA patients.
Methods
Eligibility criteria
Protocol for meta-analysis registered with International Prospective Register of Systematic Review (Prospero CRD 42022380782). In addition, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols guidelines will be used to report this protocol.26
Study design
We will include RCTs that reported the efficacy of pre-emptive analgesia in TKA. The use of quasi-RCTs and non-RCTs, including sequentially assigned RCTs within the clinic, retrospective studies, letters, review articles, case reports, editorials and animal experimental research, will be eliminated.
Type of participants/populations
All participants/populations with an indication for TKA surgery as determined by physicians and undergoing the procedure will be included. The participants in this study will not be limited by age, gender, race, surgery history, primary or revision TKA or underlying condition.
Type of interventions
In RCTs aimed at pre-emptive analgesia, any oral pre-emptive analgesic chosen prior to TKA will be permitted. The sample size, perioperative care and underlying treatment of the study will not be restricted. However, non-pharmacological pre-emptive analgesia methods will be excluded.
Type of comparator groups
Comparator groups may employ a different type or method of oral preoperative analgesic medication, a placebo or no preoperative analgesic medication. Studies with other types of interventions in the comparator groups will be excluded.
Types of outcome measures
Primary outcomes
Primary outcomes included the degree of improvement in knee pain and activity and the use of perioperative analgesics.
The visual analogue scale (VAS) dynamic pain score from 24 to 72 hours after surgery.
The numerical pain rating scale (NRS) score from 24 to 72 hours after surgery.
The Knee Society Score (KSS) will be used to assess postoperative knee function.
Consumption of analgesics from 24 to 72 hours after surgery.
Secondary outcomes
The following data will be collected for analysis as secondary outcomes: blood loss, length of hospitalisation, adverse events, duration of surgery, postoperative nausea and vomiting, time to first mobilisation, quality of life (QoL), readmission rates or perioperative care.
Search strategy
A systematic search of the PubMed, EMBASE, MEDLINE, the Cochrane Central Register of Controlled Trials and the Cochrane Database of Systematic Reviews, from their inception to 1 February 2023. There will be no restrictions on country, publication status or year of publication in the search of the previous databases. Included in the list of predefined search terms are TKA, pre-emptive analgesia, RCTs and similar topics. The search strategy will be modified for each individual database. Take PubMed as an example, the detailed search strategy was shown in table 1.
Table 1.
Search strategy used in the PubMed database
| Number | Search terms |
| #1 | Total knee arthroplasty [Mesh] |
| #2 | Total knee arthroplasty(Title/Abstract)OR Knee Replacement Arthroplasty(Title/Abstract)OR Total Knee Replacement(Title/Abstract)OR Arthroplasties, Replacement, Knee(Title/Abstract)OR Arthroplasty, Knee Replacement(Title/Abstract)OR Arthroplasty, Total Knee(Title/Abstract)OR Knee Arthroplasty, Total(Title/Abstract)OR Replacement, Total Knee(Title/Abstract)OR Knee Replacement, Total(Title/Abstract) |
| #3 | #1 OR #2 |
| #4 | Analgesia [Mesh) |
| #5 | Analgesia(Title/Abstract)OR Analgesics(Title/Abstract)OR Anodynes(Title/Abstract)OR Analgesic Drugs(Title/Abstract)OR Analgesic(Title/Abstract)OR Analgesic Agents(Title/Abstract)OR Antinociceptive Agents(Title/Abstract)OR Analgesics, Non-Narcotic(Title/Abstract)OR Analgesics, Short-Acting(Title/Abstract)OR Analgesics, Opioid(Title/Abstract)OR Anti-Inflammatory Agents, Non-Steroidal(Title/Abstract) |
| #6 | #4 OR #5 |
| #7 | Preoperative Period(Title/Abstract)OR Preoperative(Title/Abstract)OR Preemptive(Title/Abstract) |
| #8 | Randomized controlled trial [Publication Type) |
| #9 | Controlled clinical trial [Publication Type) |
| #10 | Randomized(Title/Abstract) |
| #11 | Randomly(Title/Abstract) |
| #12 | Trial(Title/Abstract) |
| #13 | #8 OR #9 OR #10 OR #11 OR #12 |
| #14 | #3 AND #6 AND #7 AND #13 |
As a supplement, the following clinical registry platforms will be searched to collect data from ongoing studies: WHO International Clinical Trial Registration Platform (http://www.who.int/trialsearch/), Australian New Zealand Clinical Trials (http://www.anzctr.org.au/) and National Institutes of Health clinical registry (http://www.clinicaltrials.gov/). The detailed retrieval search strategies we have developed for each database are in online supplemental file 1. If there is missing data, we will contact the correspondent or first author to complete it.
bmjopen-2022-070998supp001.pdf (70.6KB, pdf)
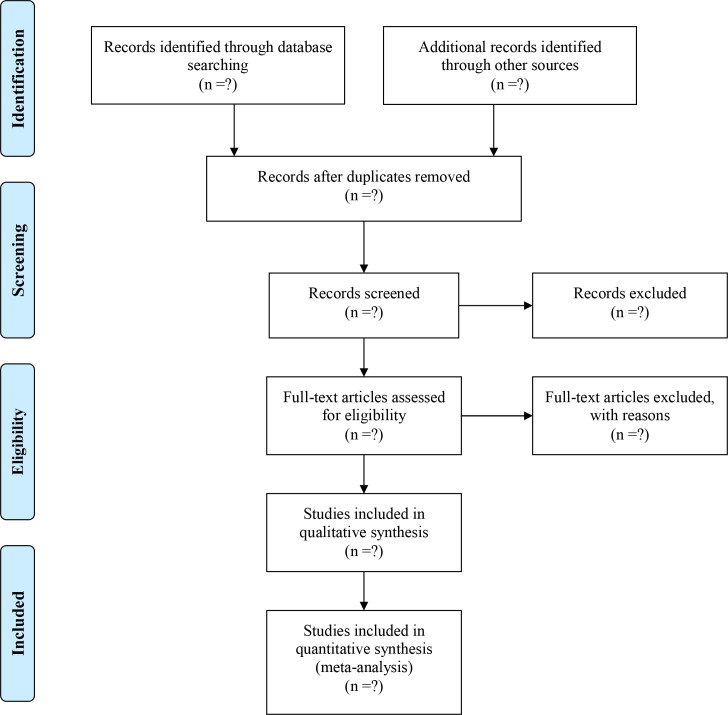
Study selection process
EndNote X9 (Thomson Reuters, New York, USA) software will be used to manage the literature and perform filtering and categorise the document and remove duplicates. After classifying the literature and removing duplicates, two independent reviewers (FX and WZ) will review the titles and abstracts of the identified studies to exclude irrelevant parts. The full text will then be downloaded and submitted to two reviewers (SJ and XH) for the whole-length articles screening to identify studies that are ultimately suitable for meta-analysis. Throughout the procedure, any disagreement will be resolved by a third researcher (KS). Figure 1 is a schematic diagram of literature selection in this study.
Figure 1.
PRISMA flow diagram of study identification and selection. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Data extraction and management
Two independent reviewers (XL and HP) will use Microsoft Excel to independently extract and manage the data. The extracted data items include:
Study characteristics: title, first author name, publication year, country of publication and funding source.
Participants: sample size, gender, average age, race, disease course and preoperative pain score/knee function score.
Interventions/comparator groups: types of the treatment, types of analgesics, timing of intervention, clinical dosage and course of treatment.
Outcomes: data relating to the primary and secondary outcomes at each measurement time will be recorded.
Before the formal data extraction, 10 studies were randomly selected to test and modify the predesigned table. All data will be cross-checked. In addition, during the data extraction process, if there is any objection can be negotiated, or by a third reviewer (YL) accuracy and consistency checking of data.
Risk of bias assessment
According to the current version of the Cochrane Risk of Bias Tool, two reviewers (FX and WZ) will independently assess the risk of bias, which included the seven specific domains: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome data, (5) incomplete outcome data, (6) selective reporting and (7) other bias.27 If required, the third reviewer (YL) will resolve divergent opinions.
Data synthesis and meta-analysis
Due to the study’s exclusive reliance on RCTs, it may be susceptible to bias. Therefore, the outcomes of this study’s data analysis should be carefully assessed.
Selection of effect measure
In this study, continuous outcome variables including VAS score, NRS score, KSS score, consumption of analgesics, blood loss, length of hospitalisation, duration of surgery, time to first mobilisation and QoL will use the standardised mean difference as the effect measure. Dichotomous variables including adverse events, postoperative nausea and vomiting, readmission rates and perioperative care will use relative ratio to evaluate the effect measure. All effect measure will be expressed with 95% CIs.
Statistical heterogeneity
The statistic I2 will be used to measure the percentage of total variability due to heterogeneity between studies.28 When the I2 range is 0%–30%, it indicates that heterogeneity may not be important. When the I2 range is 30%–75%, it indicates that moderate or substantial heterogeneity may present.29 If I2 over 75%, a descriptive analysis using a best-evidence synthesis approach will be performed without meta-analysis. In addition, we will evaluate clinical heterogeneity by assessing potential differences in the included studies, as it may still exist even in the absence of statistical heterogeneity.
Subgroup and sensitivity analyses
When the heterogeneity is excessive, we will investigate the potential origins of major inconsistencies or heterogeneity by meta-regression analysis and grouping. Age, primary or revision TKA, types of analgesics, duration of treatment, anaesthetic dosage, duration of operation, blood loss and follow-up time are among the complicating factors that need to be analysed. To uncover sources of bias and check the consistency of the meta-analysis conclusions, we will conduct a sensitivity analysis by excluding each study individually.
Meta-analysis
When we considered the included studies to be sufficiently similar, we will further conduct a meta-analysis of the outcomes of each RCT individually. When multiple outcomes were available from a single study, the value was used that was thought to be best correlated to that time interval. A random effect model will be used for all analyses based on the DerSimonian and Laird approach.30 RevMan V.5.4 (The Nordic Cochrane Center, The Cochrane Collaboration, Denmark) will be used to perform the meta-analysis.
Publication bias
If more than 10 studies are ultimately included, we will draw the Begg funnel plot to assess publication bias. The Egger test was then used to assess the asymmetry of the funnel plot.31 32
Quality of evidence
On the basis of the five components (limitations of design, inconsistency of results, indirectness, imprecision and other factors), we will assess the quality of the evidence for all outcomes. The quality of evidence is divided into four levels: very low, low, model and high. GRADE profiler software will be used for the above evidence quality grading.33
Patient and public involvement
There will be no patients involved in this study.
Ethics and dissemination
No ethical approval and consent is required for this systematic review. Moreover, the results of this systematic review will be disseminated through peer-reviewed publications and conference presentations.
Discussion
The majority of studies believe that pre-emptive analgesia is essential for promoting rapid recovery in TKA patients. The pre-emptive analgesic regimen for TKA is a combination of different types of drugs and routes of administration, including mainly epidural analgesia, peripheral nerve blocks, local infiltration analgesia, intravenous analgesia and oral analgesics (opioid/non-opioid). Although the main thrust of all the pre-emptive analgesia methods is to provide better postoperative pain relief and reduce opioid consumption, we found that the different methods differed in terms of strengths and limitations. According to the 2019 International Consensus on Anaesthesia-Related Outcomes after Surgery group consensus recommendation on anaesthetic care for TKA that primary neuraxial anaesthetic techniques including epidural analgesia are the preferred choice for TKA.34 Its main drawback, however, is the unintentional motor nerve block, which delays physiotherapy and rehabilitation.35 Peripheral nerve blocks, represented by femoral nerve blocks, are a common analgesic technique for TKA, but there is a risk of damage to adjacent blood vessels and nerves, as well as damage to local muscle strength.36 As an alternative analgesic option to femoral nerve blocks, local infiltration analgesia is less likely to produce the above-mentioned risks, but its disadvantage is that there is no consensus on its optimal composition and infiltration technique and it remains to be further investigated.37 Intravenous glucocorticoids are currently an element of multimodal salvage analgesia and have shown equally positive results in reducing pain and opioid consumption, but given the long-term safety risks associated with glucocorticoids, more evidence is still required to support them in clinical practice.38 Oral analgesics, however, are widely used and well tolerated as an pre-emptive analgesic option that optimises cost-effectiveness to a higher extent and helps to improve patient compliance and reduce the risk of anaesthesia. This is the main reason why we are concerned about oral analgesia.
However, existing research on the role of oral analgesics in TKA pain treatment have generally concentrated on the efficacy of the medications, lacking a comprehensive evaluation of the overall benefits and safety of these drugs and neglecting the influence of confounding factors on clinical study outcomes.39 A recent big NMA assessed the efficacy of oral pre-emptive analgesics on perioperative pain, showing the superiority of pre-emptive analgesia over traditional pain management methods. However, the study did not account for variability between procedures and did not conduct additional subgroup analyses of drug doses, which may have been a major source of heterogeneity.20 In our study, it is of considerable interest to undertake a novel and systematic investigation of TKA. It can enrich the evidence-based evidence for pre-emptive analgesia in TKA and provide a more convincing reference for pain management to surgeons. As only English-language database reports were considered for inclusion in this protocol, the exclusion of other databases may pose a risk of bias.
Supplementary Material
Footnotes
F-jX and WZ contributed equally.
Contributors: FX and WZ conceptualised the study and contributed equally to this work. SJ obtained funding, and together with FX, WZ and YL designed the study and drafted the initial manuscript. XH, XL, HP and KS were involved in the review and revision of the protocol. The grammar of this protocol has been improved by HP. YL supervised the study. All authors read and approved the final version of the manuscript.
Funding: Science and technology Research Special project of Sichuan Administration of Traditional Chinese Medicine (2020LC0050).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 2008;58:26–35. 10.1002/art.23176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy L, Schwartz TA, Helmick CG, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum 2008;59:1207–13. 10.1002/art.24021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Becker R. Total knee arthroplasty 2010. Knee Surg Sports Traumatol Arthrosc 2010;18:851–2. 10.1007/s00167-010-1178-1 [DOI] [PubMed] [Google Scholar]
- 4.Moonot P, Mu S, Railton GT, et al. Tibiofemoral kinematic analysis of knee flexion for a medial pivot knee. Knee Surg Sports Traumatol Arthrosc 2009;17:927–34. 10.1007/s00167-009-0777-1 [DOI] [PubMed] [Google Scholar]
- 5.Canovas F, Dagneaux L. Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res 2018;104:S41–6. 10.1016/j.otsr.2017.04.017 [DOI] [PubMed] [Google Scholar]
- 6.Behrend H, Zdravkovic V, Giesinger J, et al. Factors predicting the forgotten joint score after total knee arthroplasty. J Arthroplasty 2016;31:1927–32. 10.1016/j.arth.2016.02.035 [DOI] [PubMed] [Google Scholar]
- 7.Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 2017;10:2287–98. 10.2147/JPR.S144066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wylde V, Beswick A, Bruce J, et al. Chronic pain after total knee arthroplasty. EFORT Open Rev 2018;3:461–70. 10.1302/2058-5241.3.180004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korean Knee Society . Guidelines for the management of postoperative pain after total knee arthroplasty. Knee Surg Relat Res 2012;24:201–7. 10.5792/ksrr.2012.24.4.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coghill RC. Individual differences in the subjective experience of pain: new insights into mechanisms and models. Headache 2010;50:1531–5. 10.1111/j.1526-4610.2010.01763.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tran T, Castello J, Taylor SE, et al. Opioid use and appropriateness of supply after total knee or hip arthroplasty: an Australian perspective. J Am Acad Orthop Surg 2020;28:e980–9. 10.5435/JAAOS-D-19-00789 [DOI] [PubMed] [Google Scholar]
- 12.Dailiana ZH, Papakostidou I, Varitimidis S, et al. Patient-reported quality of life after primary major joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Musculoskelet Disord 2015;16:366. 10.1186/s12891-015-0814-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Kefraoui C, Olleik G, Chay M-A, et al. Opioid versus opioid-free analgesia after surgical discharge: protocol for a systematic review and meta-analysis. BMJ Open 2020;10:e035443. 10.1136/bmjopen-2019-035443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kissin I. Preemptive analgesia. Anesthesiology 2000;93:1138–43. 10.1097/00000542-200010000-00040 [DOI] [PubMed] [Google Scholar]
- 15.Kissin I. Preemptive analgesia: terminology and clinical relevance. Anesth Analg 1994;79:809–10. 10.1213/00000539-199410000-00037 [DOI] [PubMed] [Google Scholar]
- 16.Woolf CJ. Evidence for a central component of post-injury pain hypersensitivity. Nature 1983;306:686–8. 10.1038/306686a0 [DOI] [PubMed] [Google Scholar]
- 17.Woolf CJ. Recent advances in the pathophysiology of acute pain. Br J Anaesth 1989;63:139–46. 10.1093/bja/63.2.139 [DOI] [PubMed] [Google Scholar]
- 18.Kehlet H. Surgical stress: the role of pain and analgesia. Br J Anaesth 1989;63:189–95. 10.1093/bja/63.2.189 [DOI] [PubMed] [Google Scholar]
- 19.Woolf CJ, Chong MS. Preemptive analgesia -- treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg 1993;77:362–79. 10.1213/00000539-199377020-00026 [DOI] [PubMed] [Google Scholar]
- 20.Xuan C, Yan W, Wang D, et al. Efficacy of preemptive analgesia treatments for the management of postoperative pain: a network meta-analysis. Br J Anaesth 2022;129:946–58. 10.1016/j.bja.2022.08.038 [DOI] [PubMed] [Google Scholar]
- 21.Yang L, Zhang J, Zhang Z, et al. Preemptive analgesia effects of ketamine in patients undergoing surgery. A meta-analysis. Acta Cir Bras 2014;29:819–25. 10.1590/S0102-86502014001900009 [DOI] [PubMed] [Google Scholar]
- 22.Rosaeg OP, Krepski B, Cicutti N, et al. Effect of preemptive multimodal analgesia for arthroscopic knee ligament repair. Reg Anesth Pain Med 2001;26:125–30. 10.1053/rapm.2001.20982 [DOI] [PubMed] [Google Scholar]
- 23.Wang C, Fu H, Wang J, et al. Preemptive analgesia using selective cyclooxygenase-2 inhibitors alleviates postoperative pain in patients undergoing total knee arthroplasty: a protocol for PRISMA guided meta-analysis of randomized controlled trials. Medicine (Baltimore) 2021;100:e24512. 10.1097/MD.0000000000024512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Q, Zhang W, Xiao T, et al. Efficacy of opioids in preemptive multimodal analgesia for total knee arthroplasty: A prospective, double-blind, placebo-controlled, randomized trial. J Arthroplasty 2023;38:65–71. 10.1016/j.arth.2022.08.001 [DOI] [PubMed] [Google Scholar]
- 25.Golladay GJ, Balch KR, Dalury DF, et al. Oral multimodal analgesia for total joint arthroplasty. J Arthroplasty 2017;32:S69–73. 10.1016/j.arth.2017.05.002 [DOI] [PubMed] [Google Scholar]
- 26.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 27.Sterne JAC, Savović J, Page MJ, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 28.Rücker G, Schwarzer G, Carpenter JR, et al. Undue reliance on I (2) in assessing heterogeneity may mislead. BMC Med Res Methodol 2008;8:79. 10.1186/1471-2288-8-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions version 6.3. Cochrane, 2022. Available: www.training.cochrane.org/handbook [Google Scholar]
- 30.DerSimonian R, Laird N. Meta-Analysis in clinical trials. Control Clin Trials 1986;7:177–88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 31.Begg CB, Mazumdar M. Operating characteristics of a RANK correlation test for publication bias. Biometrics 1994;50:1088–101. 10.2307/2533446 [DOI] [PubMed] [Google Scholar]
- 32.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burkhoff D, Mirsky I, Suga H. Assessment of systolic and diastolic ventricular properties via pressure-volume analysis: a guide for clinical, translational, and basic researchers. Am J Physiol Heart Circ Physiol 2005;289:H501–12. 10.1152/ajpheart.00138.2005 [DOI] [PubMed] [Google Scholar]
- 34.Memtsoudis SG, Cozowicz C, Bekeris J, et al. Anaesthetic care of patients undergoing primary hip and knee arthroplasty: consensus recommendations from the international consensus on anaesthesia-related outcomes after surgery group (ICAROS) based on a systematic review and meta-analysis. Br J Anaesth 2019;123:269–87. 10.1016/j.bja.2019.05.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Koh JC, Song Y, Kim SY, et al. Postoperative pain and patient-controlled epidural analgesia-related adverse effects in young and elderly patients: a retrospective analysis of 2,435 patients. J Pain Res 2017;10:897–904. 10.2147/JPR.S133235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chan E-Y, Fransen M, Parker DA, et al. Femoral nerve blocks for acute postoperative pain after knee replacement surgery. Cochrane Database Syst Rev 2014;2014:CD009941. 10.1002/14651858.CD009941.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li JW, Ma YS, Xiao LK. Postoperative pain management in total knee arthroplasty. Orthop Surg 2019;11:755–61. 10.1111/os.12535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hartman J, Khanna V, Habib A, et al. Perioperative systemic glucocorticoids in total hip and knee arthroplasty: a systematic review of outcomes. J Orthop 2017;14:294–301. 10.1016/j.jor.2017.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krishna Prasad GV. Post-Operative analgesia techniques after total knee arthroplasty: a narrative review. Saudi J Anaesth 2020;14:85–90. 10.4103/sja.SJA_494_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-070998supp001.pdf (70.6KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study.