Abstract
Objectives
The aim of this study was to map existing emergency medical services (EMS) and palliative care literature by answering the question, what literature exists concerning EMS and palliative care? The sub-questions regarding this literature were, (1) what types of literature exist?, (2) what are the key findings? and (3) what knowledge gaps are present?
Design
A scoping review of literature was performed with an a priori search strategy.
Data sources
MEDLINE via Pubmed, Web of Science, CINAHL, Embase via Scopus, PsycINFO, the University of Cape Town Thesis Repository and Google Scholar were searched.
Eligibility criteria for selecting studies
Empirical, English studies involving human populations published between 1 January 2000 and 24 November 2022 concerning EMS and palliative care were included.
Data extraction and synthesis
Two independent reviewers screened titles, abstracts and full texts for inclusion. Extracted data underwent descriptive content analysis and were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews guidelines.
Results
In total, 10 725 articles were identified. Following title and abstract screening, 10 634 studies were excluded. A further 35 studies were excluded on full-text screening. The remaining 56 articles were included for review. Four predominant domains arose from included studies: (1) EMS’ palliative care role, (2) challenges faced by EMS in palliative situations, (3) EMS and palliative care integration benefits and (4) proposed recommendations for EMS and palliative care integration.
Conclusion
EMS have a role to play in out-of-hospital palliative care, however, many challenges must be overcome. EMS provider education, collaboration between EMS and palliative systems, creation of EMS palliative care guidelines/protocols, creation of specialised out-of-hospital palliative care teams and further research have been recommended as solutions. Future research should focus on the prioritisation, implementation and effectiveness of these solutions in various contexts.
Keywords: accident & emergency medicine, health services administration & management, palliative care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
A thorough search string was piloted and employed in conjunction with a wide range of databases, meeting recommendations for optimal combinations and providing a comprehensive view of contemporary literature.
The performance and report of this review was completed according to the quality standards of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews guidelines.
Limitations to this review include those common to scoping reviews such as human error in article selection.
A formal risk of bias assessment was not performed; therefore, data reliability lacks evaluation.
Introduction
Emergency medical services (EMS) and palliative care function with unique respective aims. EMS are designed to preserve life and limb in out-of-hospital emergency situations by immediate intervention and hospital conveyance.1 2 Palliative care is, according to the WHO, ‘an approach that improves the quality of life (QoL) of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.’3 This includes a variety of situations such as chronic/life-limiting illnesses, end-of-life (EoL) care and any condition (physical, psychosocial, spiritual) causing suffering.3 Thus, the EMS approach is curative, whereas the palliative approach is supportive.
Despite these seemingly conflicting approaches, EMS and palliative care often intersect.4–7 As they progress towards EoL, patients with palliative needs experience worsening symptoms for which EMS are often contacted.8 9 Furthermore, the role of EMS has expanded in recent years to include more intricate forms of healthcare beyond emergency care such as community-based primary care and palliative care.10 Global ageing populations and subsequent increases in chronic non-communicable diseases are well-documented reasons for this expanded role as demand for palliative care rises and EMS are more frequently confronted with these patients.11
Contemporary EMS and palliative care literature recommends integration between the two fields to improve palliative care provision as their differing aims may, in fact, complement one another.12 Nevertheless, a lack of integration persists. Typically, EMS are not trained in palliative care nor do palliative care systems make formal use of EMS to deliver care.13 This results in disregarding of patient autonomy, performance of aggressive, futile interventions and overall poor management of those requiring a palliative approach to care by EMS providers.12–14 However, should the two fields integrate, potential benefits include early palliative care delivery, provision of homecare, respect for patient autonomy, improved patient and family satisfaction, confidence and quality of life (QoL), decreased healthcare costs and setting correct trajectories of care.5 15 16
Given the growing body of EMS and palliative care literature, and potential integration benefits, a need exists to review current evidence. Previous reviews have focused on singular aspects such as specialised community paramedic roles in the provision of palliative care in patient homes,11 however, a more extensive review of EMS in the broader out-of-hospital setting is lacking. Thus, this review aimed to map existing EMS and palliative care literature by answering the question, what literature exists concerning EMS and palliative care? The sub-questions regarding this literature were (1) what types of literature exist?, (2) what are the key findings? and (3) what knowledge gaps are present? For the purposes of this study, EMS are defined as those systems and personnel providing medical care in the out-of-hospital setting using ambulance-based services. The out-of-hospital setting includes all areas to which EMS may be called, from patient homes to any public space.
Methods
Design
A scoping review of EMS and palliative care literature was performed, the protocol for which has been published previously,17 detailing the methodological framework of Arksey and O’Malley used for this review.18 The steps of this employed framework were (1) identifying the research question, (2) identifying relevant studies, (3) selecting eligible studies, (4) charting data and (5) collating, summarising and reporting results.18 The optional sixth step of expert consultation was not included as this review forms the first part of an overarching investigation in which expert consultation will be subsequently performed. As this review aimed to simply map existing literature, in-depth quality appraisal of eligible studies was not performed, though limitations were noted.
Search strategy and eligibility criteria
An a priori search strategy, developed in line with the recommendations of Aromataris and Riitano, was used.19 This strategy employed keyword combinations and their synonyms (see online supplemental material 1). The following databases were originally searched on 28 September 2021 with an updated search on 24 November 2022: MEDLINE via Pubmed, Web of Science, CINAHL, Embase via Scopus and PsycINFO. The University of Cape Town Thesis Repository and Google Scholar were searched to identify grey literature. These databases met the recommendation of Bramer et al for optimal database combinations.20 Furthermore, Embase, CINAHL and PsycINFO provided access to unique palliative care literature not indexed in MEDLINE as highlighted by Tieman et al.21 Additional articles were sought from hand-searching reference lists of eligible studies. This search strategy was piloted to ensure appropriateness of keyword combinations in the selected databases.
bmjopen-2022-071116supp001.pdf (65.9KB, pdf)
Eligible studies were selected based on the following criteria:
Inclusion: empirical, English studies involving human populations published between 1 January 2000 and 24 November 2022 concerning EMS and palliative care. The EMS and palliative care interface was the primary focus for eligibility.
Exclusion: studies involving the in-hospital setting, including emergency departments (EDs), those where the full text was unobtainable, editorial and discussion articles, opinion papers and studies involving exclusively EMS or palliative care.
Data management
All identified studies were uploaded to Mendeley reference software22 and duplicates removed. Remaining studies were exported to the Rayyan web application23 where two authors (CHG, CS) independently screened titles and abstracts for inclusion. CHG and CS then screened the full texts of included studies for final inclusion in the review. Agreement achieved between authors was >99%. On discussion, complete agreement was reached for all studies. This process was overseen by LG and WS. All authors agreed on the final inclusion list.
Data extraction and analysis
An a priori data extraction matrix was used to gather the following data from each included study which were charted by CHG using Microsoft Word (Microsoft Corporation, Redmond, Washington, USA): title, authorship, publication year, setting, including country income status divided into high-income countries (HICs) and low-to-middle income countries (LMICs), aims, population and sample, EMS palliative care training, methodology, conclusions, significant findings, limitations. To ensure consistency in application of this extraction matrix, CS double coded 10% of included articles. In line with the recommendations of Arksey and O’Malley, extracted data underwent basic numerical analysis concerning the distribution of studies and descriptive content analysis where the literature was organised according to major domains.18 These domains were identified through an inductive-dominant approach. Findings are presented in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews.24 25
Patient and public involvement
No patients were involved in this study.
Results
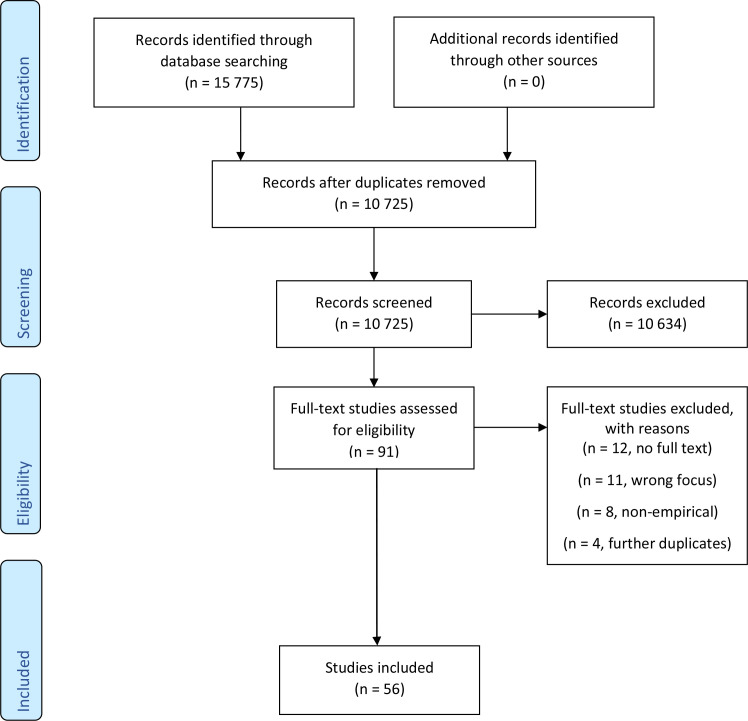
After duplication removal, 10 725 studies were identified. Following title and abstract screening, 10 634 studies were excluded. A further 35 studies were excluded on full-text screening. Of the full-text exclusions, 12 full texts were unavailable, the EMS and palliative care interface was not the primary focus in 11 studies, 8 studies presented non-empirical evidence and the remaining 4 studies were previously undetected duplicates. Hand-searching of included reference lists revealed no further studies. No grey literature fitting inclusion criteria was identified. In total, 56 studies were included for analysis. Figure 1 details the selection process while a summary of included studies is provided in online supplemental material 2.
Figure 1.
PRISMA selection process flow diagram.25 PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
bmjopen-2022-071116supp002.pdf (174.1KB, pdf)
Study characteristics
Included studies were performed in the USA (n=16),1 6 26–39 the UK (n=9),7 14 40–46 Germany (n=10),8 47–55 Australia (n=8),2 4 11 56–60 Canada (n=4),15 61–63 France (n=1),5 Switzerland (n=1),13 New Zealand (n=2),64 65 Finland (n=2),66 67 Czech Republic (n=1),68 Brazil (n=1)69 and South Africa (n=1)16 between 2002 and 2022. The majority of studies (96%, n=54) were performed in HICs with only Brazil and South Africa representing LMICs, and most (63%, n=35) were published between 2018 and 2022.
Methodologically, most studies were quantitative (55%, n=31) while the remainder used a qualitative (27%, n=15) or mixed-methods (18%, n=10) approach. Quantitative studies comprised of surveys (n=12),1 8 30 32 38 41 43 48 49 51 56 58 retrospective cohorts (n=9),5 33 34 40 52 54 55 57 66 literature reviews (n=5),11 46 61 64 68 case series/reports (n=3),6 13 35 a pre-intervention and post-intervention study (n=1)29 and a prospective cohort (n=1).8 Qualitative studies contained individual interviews (n=12),7 14 16 26–28 31 42 44 47 65 69 focus group interviews (n=2)2 63 and deliberative dialogues (n=1),62 while the mixed-methods studies4 15 36 37 39 45 50 59 60 67 made use of various survey and interview combinations.
EMS providers were the primary population in most studies (52%, n=29)1 2 4 7 8 14 16 26–31 36–39 41 43–45 47–49 51 56 58 67 69 including paramedics, doctors and nurses involved in out-of-hospital emergency care dependant on EMS system model: paramedic-led (Anglo-American), physician-led (Franco-German).11 Other investigations were performed using patient records (n=10),5 8 33 34 40 52 54 55 57 66 published literature (n=5),11 46 61 64 68 case reports/series (n=3),6 13 35 stakeholders and experts (n=3),42 50 62 mixed populations including patients, families, paramedics, caregivers, palliative providers and patient records (n=3),15 59 63 EMS agencies (n=2)32 60 and family caregivers (n=1).65
Study categories were EMS provider knowledge and perspectives (54%, n=30),1 2 4 7 8 14 16 26–28 30 31 36–39 41–45 47–49 51 56 58 63 67 69 EMS–palliative integration (23%, n=13),5 6 15 29 32 34 35 40 50 59 60 62 66 EMS–palliative intersection (14%, n=8)8 13 33 52 54 55 57 65 and literature reviews (9%, n=5).11 46 61 64 68 Studies concerning EMS provider knowledge and perspectives vis à vis palliative care focused on EMS management and decision making (n=9),8 26 27 37 44 48 49 51 58 roles and barriers in palliative situations (n=11),2 14 16 28 31 42 43 45 47 63 69 understanding and education (n=6),1 4 30 38 39 67 identification of patients with palliative needs (n=2)36 41 and potential solutions to overcome barriers (n=2).7 56 Studies concerning EMS and palliative care integration focused on effects of integration on patient transport, patient/family satisfaction and EMS provider confidence (n=7),5 15 34 35 40 59 66 recommendations for integration (n=4)6 29 50 62 and EMS palliative care protocols (n=2).32 60 Studies concerning EMS and palliative care intersection focused on the characteristics and frequency of patients with palliative needs encountered by EMS providers (n=4),8 33 55 57 EMS provider treatment of these patients (n=3)13 52 54 and the experience of family caregivers.65 Literature reviews focused on attitudes and perceptions of paramedics concerning EoL care (n=1),46 EMS role in EoL care (n=1),68 EMS palliative provision in community-based settings (n=1)11 and rapid reviews of EMS and palliative care literature in Canada (n=1)61 and New Zealand (n=1).64
Four predominant domains arose from included studies: (1) EMS’ palliative care role, (2) challenges faced by EMS in palliative situations, (3) EMS and palliative care integration benefits and (4) proposed recommendations for EMS and palliative care integration.
EMS’ palliative care role
Numerous studies (66%, n=37)1 2 6 8 11 14–16 26–28 31 34 35 37 41–46 48 51 53–55 57 59–61 63–69 discussed the potential role of EMS in palliative care. Most EMS providers viewed palliative care positively, regarding it as important to their role as demonstrated in studies performed in the UK,43 Australia,59 Canada15 and South Africa.16 The EMS’s palliative care role was frequently highlighted due to the intersection between EMS and patients with palliative needs.8 54 57 For example, an Australian study found palliative situations comprised 0.5% (n=4348) of the annual EMS caseload.57 Other studies, found palliative situations may represent up to 10% of caseload and most EMS providers had previously encountered palliative situations.8 47 Commonly documented reasons for EMS calls to palliative situations were sudden, unexpected patient deterioration, caregiver exhaustion and alarming signs and symptoms: dyspnoea, pain, convulsions, severe anxiety.15 26 47 These calls often occurred out-of-office hours or during holidays when the usual patient caregivers were unavailable.13 Specific EMS palliative care roles included complex care provision,68 adjusting patient trajectory,16 decision-making within limited information environments,14 therapeutic interventions,54 24/7 availability, provision of homecare66 and improving patient and family QoL, comfort and confidence.15
Challenges faced by EMS in palliative situations
Most studies (63%, n=35)1 2 6–8 11 13 14 16 26 27 30–33 36–38 40 41 43–47 49 51–54 58 61 67–69 highlighted various challenges EMS providers face in palliative situations. These challenges were EMS provider mindset,1 the out-of-hospital environment,16 EMS systems,14 lack of education,68 medico-legal confusion49 and inter-personal conflicts.2 The EMS provider mindset is to ‘save lives’ through a curative approach to care, whereas the palliative approach is primarily supportive through prevention and relief of suffering.1–3 Other common challenges were related to the complex out-of-hospital environment: lack of information, limited time, consequent difficult decision-making.47
EMS system barriers to palliative provision were mandated hospital transport,16 limited scope of practice47 and lack of alternative care pathways.14 Despite patient and family wishes and better clinical judgement, EMS providers often conveyed palliative patients to hospital due to system rigidity, fear of consequences and a lack of alternative care pathways.14 Hospital transport was described as a safety net for EMS providers and, thus, their default decision in palliative situations.44
Many studies identified a lack of EMS provider education concerning palliative care2 16 36 43 47 and only five studies mentioned EMS providers with additional palliative or hospice care training in their samples.4 8 36 53 56 The additional palliative training ranged from short course to postgraduate diploma level. This lack of education was identified in both physician and paramedic-led EMS systems.8 16
Highlighted medico-legal challenges for EMS providers in palliative situations were fear of litigation47 and confusion surrounding legal documentation such as advance directives.13 38 49 EMS providers were sometimes unaware of the presence of legal documentation due to lack of available information at incidents.6 26 27 Furthermore, where legal documentation was presented, EMS providers were uncertain of legal implications in emergencies.2 49
Finally, EMS providers described various conflicts requiring management in palliative situations. Conflicts arose with other healthcare providers, patients, families and within EMS providers themselves.2 These conflicts were due to competing interests: patient wishes, family wishes, EMS protocols, EMS provider clinical judgement, medico-legal considerations.16 26
EMS and palliative care integration benefits
Many studies (36%, n=20)5 6 8 11 15 16 29 34 35 40–42 47 53 54 59 61–63 66 described benefits of EMS and palliative care integration: early palliative provision, home-based care, respect of patient autonomy, improved patient and family QoL, increased patient and family satisfaction and confidence, improved EMS provider confidence and decreased healthcare costs. Conversely, the consequences of non-integration were disregard of patient autonomy, performance of aggressive or futile interventions and poor management of palliative patients by EMS.13 14
Provision of early, home-based palliative care by EMS was found to improve patient and family QoL, satisfaction and confidence as demonstrated by Carter et al.15 This study found high patient and family satisfaction with palliative provision from EMS providers, observing their compassion and skill in symptom management.15 Furthermore, knowledge of the 24/7 availability of EMS providers in this programme provided confidence and peace of mind.15 Paramedic comfort and confidence in palliative provision likewise improved during the study.15
Collaboration between EMS and palliative care networks was found to improve respect of patient autonomy.5 An example was provided in a case study by Clemency et al where a terminally ill patient was transported home from hospital, extubated and allowed to die at home according to her wishes.35 This was facilitated by EMS under the guidance of palliative care specialists and in conjunction with a broader multidisciplinary team.35
Several studies discussed the potential decreased healthcare costs resulting from EMS and palliative integration.41 59 61 66 The decreased costs would, theoretically, result from provision of homecare, thus avoiding expensive and unnecessary hospital admissions.61 A Finnish study evaluating the integration of paramedics in EoL care argued that healthcare costs may be diminished through provision of homecare by paramedics in particular.66
Proposed recommendations for EMS and palliative care integration
All 56 included studies made recommendations for EMS and palliative care integration. These were EMS provider education,4 EMS and palliative system collaboration,5 EMS palliative care guideline/protocol creation,16 specialised out-of-hospital palliative care teams34 and further research.57 The following topics were highlighted as areas for EMS provider education: identifying patients with palliative needs,41 palliative therapeutic goals,44 legal documentation and advance care planning, ethics,13 withholding and withdrawing treatment,38 51 patient and family communication (including caregiver support),47 symptom management,54 interdisciplinary teamwork59 and current palliative system structures.58
Lamba et al detailed four steps for EMS and palliative care integration: (1) identify EMS ‘champions’, (2) review protocols and literature, (3) perform a needs assessment and (4) create an action plan.6 The authors argued that optimal palliative care begins out-of-hospital and, therefore, palliative and EMS systems should collaborate.6 Such collaborations between palliative and EMS systems, making use of newly developed palliative care guidelines and protocols for EMS providers, were successfully deployed in Canada,15 Finland66 and the USA.34
Concerning further research, the following areas were recommended: educational interventions,46 development of EMS palliative care protocols,16 defining the role of EMS in palliative situations,2 development of EMS palliative care policies and clarifying palliative care referral pathways,2 cost-effectiveness of EMS and palliative care integration.40 59 66
Discussion
This scoping review aimed to map existing EMS and palliative literature by identifying study types, extracting key findings and noting limitations, thereby providing a summary of current evidence, context for EMS and palliative care integration and identifying knowledge gaps for future research.
The topic of EMS and palliative care has gathered momentum in recent years as the role of EMS systems in out-of-hospital care has expanded; most studies included in this review (63%, n=35) being published between 2018 and 2022. While the body of literature has grown, there remains a relative dearth of empirical evidence, with only 56 such studies identified here since the turn of the millennium. Many of these studies are small in scale, presenting limited findings. Common limitations include small sample sizes, limited external validity, use of unvalidated survey instruments, self-selection bias, recall bias and those resulting from retrospective approaches.
Despite these limitations, the literature, when aggregated, is consistent across various contexts. For example, similar challenges to EMS palliative provision, such as a lack of on-scene patient information, have been documented in both paramedic26 and physician-led systems.47 Moreover, findings regarding EMS role, challenges and integration benefits in palliative situations appear similar across HICs68 and LMICs,16 demonstrating the ubiquitous nature of the out-of-hospital environment.
Of importance, only two studies in this review (3.5%) were performed in LMICs,16 69 revealing a significant knowledge gap. Due to disproportionately high burdens of disease and contemporaneous resource constraints, challenges and integration benefits in LMICs may be amplified when compared with HICs.70 71 HICs have reported that 0.5%–10% of EMS caseload comprises palliative situations.47 57 With their greater disease burdens, this proportion is likely much larger within LMICs.16 LMICs require novel approaches to this problem given their resource constraints. The development of new, specialised out-of-hospital palliative care teams, for example, may not be feasible in LMICs. Capacitating already existing structures, EMS and palliative, to collaborate via alternative means may represent a more efficient use of scarce resources to achieve integration benefits.59 Simply improving communication between the two systems may confer benefit as demonstrated by Dent et al where palliative telephonic advice provided to EMS resulted in decreased rates of hospital conveyance.40 Similar integrative approaches have been successfully employed in HICs for mental health emergencies, linking mental healthcare workers with EMS and police to provide consult at point of care.72
The 1990 Commission on Health Research for Development affirmed that strengthening LMIC research capacity is ‘one of the most powerful, cost-effective, and sustainable means of advancing health and development’.73 Not only would LMICs benefit greatly from further research, but the cost-effective solutions developed would likewise benefit HICs where increasing healthcare costs remain a challenge.74 Considering amplified LMIC problems, solutions and the need for contextually suitable approaches, the need for, and yet lack of, EMS palliative care LMIC research is striking.
While further research is needed, the existing literature supports, and indeed recommends, the integration of EMS and palliative care services whatever the context (paramedic vs physician-led, HIC vs LMIC).5 16 Such integration would be congruous with the multidisciplinary approach espoused by palliative care3 and recommended by the WHO.75 The WHO has noted a growing demand for palliative care worldwide, with an insufficient corresponding supply of specialist palliative services.75 Integration between palliative services and other disciplines is required to meet the need. Given the multidisciplinary requirement of palliative care and the significant EMS palliative care intersection, integration between the two appears essential.
Though a need for integration exists the question as to precise EMS roles in palliative situations remains. Whatever the specifics, several unique features of EMS may compliment palliative care provision: first-responder role, 24/7 availability, homecare provision and emergency capabilities.6 10 76 77 The earlier palliative care is implemented, the greater its efficacy.78 EMS have the capability to both identify palliative needs and initiate palliative care immediately in their role as first responders.6 76 Often patients with palliative needs wish to be treated at home but lack this option.15 They may also suffer deleterious symptoms at any time of day or night requiring a hospital visit.15 Out-of-hospital palliative care services frequently function exclusively during office hours leaving these patients without support.13 The 24/7 availability of EMS, coupled with their homecare expertise, could ameliorate these gaps within palliative care provision and, in the not unlikely event of patient deterioration, EMS expertise in emergencies would be beneficial.66
Various recommendations to promote EMS and palliative care integration have been made. However, the priorities of these recommendations have not been established. It is likewise unclear from the literature whether EMS and palliative care integration itself is of high priority within individual countries or globally. Further research is required not only to prioritise recommendations for integration, but to prioritise EMS and palliative care integration within unique healthcare systems. Priorities will likely vary across disparate contexts; however, the literature suggests integration should be favourably considered as it has potential to be a low-cost, high impact intervention aligned with WHO priorities. Such integration would result in improved palliative care provision and access,16 providing these vulnerable patients with dignity through protection of their autonomy and avoidance of non-beneficial treatment. In addition, EMS and palliative care integration may result in cost and resource savings by decreasing hospital burdens.61 66 This in turn would free resources for additional healthcare interventions. Other causal-sequence benefits may result including a unified healthcare approach and bringing together of siloed systems (EMS, palliative, in-hospital), which would result in further improved patient experience across the healthcare spectrum.
A concern regarding this integration is that this expanded role would strain EMS resources by increasing caseload and time spent per incident.77 Further investigation into this concern is needed across various contexts. However, existing evidence has shown no increased strain on caseload66 and while time spent on scene does appear increased in certain palliative situations, these involve provision of homecare without conveyance.66 76 Total time spent per incident appears to decrease in these situations due to time-saving from avoidance of transport, hospital handover, ambulance cleaning and restocking.76
Research priorities regarding palliative care in the ED setting have been established by Quest et al79: (1) which patients are in greatest need of palliative care services in the ED?, (2) what is the optimal role of emergency clinicians in caring for patients along a chronic trajectory of illness?, (3) what are the educational priorities for emergency clinical providers in the domain of palliative care? As EMS represent the out-of-hospital branch of emergency medicine, such priorities are germane.
Based on the included literature of this review, several specific EMS palliative care research gaps exist. There is a need for further epidemiological study, on a larger scale, across various contexts, particularly LMICs, to more accurately describe the impact of patients requiring palliative care on EMS systems. Further intervention-based studies are required to test the effectiveness of various forms of EMS and palliative care integration, including their cost-effectiveness. The potential benefit of decreased healthcare costs remains theoretical and requires investigation. Educational interventions require particular analysis as many questions remain unanswered: What EMS qualifications should be targeted? What content is most relevant? What level and type of intervention is required (ie, undergraduate vs postgraduate, informal vs formal)? Qualitative interview studies with palliative patients, family members and palliative specialists concerning EMS use in palliative care are largely lacking and would be beneficial as these are primary role players. Finally, both quantitative and qualitative data are needed from other stakeholders such as medical insurance companies which often cover the costs of both EMS and palliative services.
Limitations
This review is not without limitation. Some relevant studies, including grey literature, may have been missed due to the selection criteria, databases searched, search string employed and researcher finitude. Furthermore, only English studies were selected. However, it is unlikely many relevant studies were omitted as a comprehensive search string was developed, piloted and employed in conjunction with a broad database range, meeting recommendations for an optimal search strategy. Finally, the conclusions of this review should be observed with equipoise given the potential risk of bias, limited external validity of many included studies and the need for further contextual and empirical evidence.
Conclusion
Current literature suggests EMS and palliative care systems should integrate to improve palliative care provision. EMS have a role to play in out-of-hospital palliative care however, the specifics of this role require further investigation and are likely to differ across disparate contexts. Currently, when performing various functions in palliative situations, EMS providers are faced with several challenges which must be overcome to provide appropriate care. EMS provider education, collaboration between EMS and palliative systems, creation of EMS palliative care guidelines/protocols, creation of specialised out-of-hospital palliative care teams and further research have been recommended as solutions. Future research should focus on the prioritisation, implementation and effectiveness of these solutions cross-contextually; particularly in LMICs where the need and potential impact are most significant.
Supplementary Material
Footnotes
Twitter: @willem_stassen
Contributors: CHG, LG and WS designed the protocol. CHG and CS collected data. CHG drafted the manuscript with input from CS, LG and WS. All authors reviewed and gave final approval of the manuscript. CHG is the guarantor and accepts full responsibility for the study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. No additional data available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Waldrop D, Clemency B, Maguin E, et al. Prehospital providers’ perceptions of emergency calls near life’s end. Am J Hosp Palliat Care 2015;32:198–204. 10.1177/1049909113518962 [DOI] [PubMed] [Google Scholar]
- 2.Lord B, Récoché K, O’Connor M, et al. Paramedics’ perceptions of their role in palliative care: analysis of focus group transcripts. J Palliat Care 2012;28:36–40. [PubMed] [Google Scholar]
- 3.WHO.int [internet]. 2022. Available: www.who.int/cancer/palliative/definition/en/ [Accessed 13 Dec 2022].
- 4.Rogers IR, Shearer FR, Rogers JR, et al. Paramedics’ perceptions and educational needs with respect to palliative care. Australasian Journal of Paramedicine 2015;12:1–7. 10.33151/ajp.12.5.218 [DOI] [Google Scholar]
- 5.Burnod A, Lenclud G, Ricard-Hibon A, et al. Collaboration between prehospital emergency medical teams and palliative care networks allows a better respect of a patient’s will. Eur J Emerg Med 2012;19:46–7. 10.1097/MEJ.0b013e328347fa9c [DOI] [PubMed] [Google Scholar]
- 6.Lamba S, Schmidt TA, Chan GK, et al. Integrating palliative care in the out-of-hospital setting: four things to jump-start an EMS-palliative care initiative. Prehosp Emerg Care 2013;17:511–20. 10.3109/10903127.2013.811566 [DOI] [PubMed] [Google Scholar]
- 7.Patterson R, Standing H, Lee M, et al. Paramedic information needs in end-of-life care: a qualitative interview study exploring access to a shared electronic record as a potential solution. BMC Palliat Care 2019;18:108. 10.1186/s12904-019-0498-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiese CHR, Bartels UE, Marczynska K, et al. Quality of out-of-hospital palliative emergency care depends on the expertise of the emergency medical team -- a prospective multi-centre analysis. Support Care Cancer 2009;17:1499–506. 10.1007/s00520-009-0616-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schrijvers D, van Fraeyenhove F. Emergencies in palliative care. Cancer J 2010;16:514–20. 10.1097/PPO.0b013e3181f28a8d [DOI] [PubMed] [Google Scholar]
- 10.Long D. Paramedic delivery of community-based palliative care: an overlooked resource? Progress in Palliative Care 2019;27:289–90. 10.1080/09699260.2019.1672414 [DOI] [Google Scholar]
- 11.Juhrmann ML, Vandersman P, Butow PN, et al. Paramedics delivering palliative and end-of-life care in community-based settings: a systematic integrative review with thematic synthesis. Palliat Med 2022;36:405–21. 10.1177/02692163211059342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duchateau FX. Palliative care and prehospital emergency medicine -- apparently conflicting approaches? Eur J Emerg Med 2012;19:1. 10.1097/MEJ.0b013e32834d0d93 [DOI] [PubMed] [Google Scholar]
- 13.Carron P-N, Dami F, Diawara F, et al. Palliative care and prehospital emergency medicine: analysis of a case series. Medicine (Baltimore) 2014;93:e128. 10.1097/MD.0000000000000128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoare S, Kelly MP, Prothero L, et al. Ambulance staff and end-of-life hospital admissions: a qualitative interview study. Palliat Med 2018;32:1465–73. 10.1177/0269216318779238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carter AJE, Arab M, Harrison M, et al. Paramedics providing palliative care at home: a mixed-methods exploration of patient and family satisfaction and paramedic comfort and confidence. CJEM 2019;21:513–22. 10.1017/cem.2018.497 [DOI] [PubMed] [Google Scholar]
- 16.Gage CH, Geduld H, Stassen W. South African paramedic perspectives on prehospital palliative care. BMC Palliat Care 2020;19:153. 10.1186/s12904-020-00663-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gage CH, Stander C, Gwyther L, et al. Emergency medical services and palliative care: protocol for a scoping review. BMJ Open 2022;12:e062054. 10.1136/bmjopen-2022-062054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 19.Aromataris E, Riitano D. Constructing a search strategy and searching for evidence. A guide to the literature search for a systematic review. Am J Nurs 2014;114:49–56. 10.1097/01.NAJ.0000446779.99522.f6 [DOI] [PubMed] [Google Scholar]
- 20.Bramer WM, Rethlefsen ML, Kleijnen J, et al. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev 2017;6:245. 10.1186/s13643-017-0644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tieman JJ, Sladek RM, Currow DC. Multiple sources: mapping the literature of palliative care. Palliat Med 2009;23:425–31. 10.1177/0269216309102727 [DOI] [PubMed] [Google Scholar]
- 22.Mendeley.com [internet]. 2022. Available: www.mendeley.com/download-reference-manager/ [Accessed 13 Dec 2022].
- 23.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016;5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prisma-statement.org [internet]. 2021. Available: www.prisma-statement.org/documents/PRISMA-ScR-Fillable-Checklist_11Sept2019.pdf [Accessed 7 Jun 2021].
- 25.Page MJ, Moher D. Evaluations of the uptake and impact of the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and extensions: a scoping review. Syst Rev 2017;6:263. 10.1186/s13643-017-0663-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waldrop DP, Clemency B, Lindstrom HA, et al. “We are strangers walking into their life-changing event”: how prehospital providers manage emergency calls at the end of life. J Pain Symptom Manage 2015;50:328–34. 10.1016/j.jpainsymman.2015.03.001 [DOI] [PubMed] [Google Scholar]
- 27.Waldrop DP, McGinley JM, Dailey MW, et al. Decision-making in the moments before death: challenges in prehospital care. Prehosp Emerg Care 2019;23:356–63. 10.1080/10903127.2018.1518504 [DOI] [PubMed] [Google Scholar]
- 28.Waldrop DP, McGinley JM, Clemency B. Mediating systems of care: emergency calls to long-term care facilities at life’s end. J Palliat Med 2018;21:987–91. 10.1089/jpm.2017.0332 [DOI] [PubMed] [Google Scholar]
- 29.Fitzpatrick S, Somers S, Stryckman B, et al. Improving hospice and palliative care through nurse practitioner engagement in a community paramedicine program. The Journal for Nurse Practitioners 2022;18:769–773. 10.1016/j.nurpra.2022.04.011 [DOI] [Google Scholar]
- 30.Wenger A, Potilechio M, Redinger K, et al. Care for a dying patient: EMS perspectives on caring for hospice patients. J Pain Symptom Manage 2022;64:e71–6. 10.1016/j.jpainsymman.2022.04.175 [DOI] [PubMed] [Google Scholar]
- 31.Breyre AM, Benesch T, Glomb NW, et al. EMS experience caring and communicating with patients and families with a life-limiting-illness. Prehosp Emerg Care 2022;26:708–15. 10.1080/10903127.2021.1994674 [DOI] [PubMed] [Google Scholar]
- 32.Ausband SC, March JA, Brown LH. National prevalence of palliative care protocols in emergency medical services. Prehosp Emerg Care 2002;6:36–41. 10.1080/10903120290938751 [DOI] [PubMed] [Google Scholar]
- 33.Breyre AM, Bains G, Moore J, et al. Hospice and comfort care patient utilization of emergency medical services. J Palliat Med 2022;25:259–64. 10.1089/jpm.2021.0143 [DOI] [PubMed] [Google Scholar]
- 34.Breyre A, Taigman M, Salvucci A, et al. Effect of a mobile integrated hospice healthcare program on emergency medical services transport to the emergency department. Prehosp Emerg Care 2022;26:364–9. 10.1080/10903127.2021.1900474 [DOI] [PubMed] [Google Scholar]
- 35.Clemency BM, Grimm KT, Lauer SL, et al. Transport home and terminal extubation by emergency medical services: an example of innovation in end-of-life care. J Pain Symptom Manage 2019;58:355–9. 10.1016/j.jpainsymman.2019.03.007 [DOI] [PubMed] [Google Scholar]
- 36.Barnette Donnelly C, Armstrong KA, Perkins MM, et al. Emergency medical services provider experiences of hospice care. Prehosp Emerg Care 2018;22:237–43. 10.1080/10903127.2017.1358781 [DOI] [PubMed] [Google Scholar]
- 37.McGinley J, Waldrop DP, Clemency B. Emergency medical services providers’ perspective of end-of-life decision making for people with intellectual disabilities. J Appl Res Intellect Disabil 2017;30:1057–64. 10.1111/jar.12363 [DOI] [PubMed] [Google Scholar]
- 38.Stone SC, Abbott J, McClung CD, et al. Paramedic knowledge, attitudes, and training in end-of-life care. Prehosp Disaster Med 2009;24:529–34. 10.1017/s1049023x00007469 [DOI] [PubMed] [Google Scholar]
- 39.Waldrop DP, Clemency B, Maguin E, et al. Preparation for frontline end-of-life care: exploring the perspectives of paramedics and emergency medical technicians. J Palliat Med 2014;17:338–41. 10.1089/jpm.2013.0442 [DOI] [PubMed] [Google Scholar]
- 40.Dent T, Tipping I, Anderson R, et al. Hospice advice and rapid response service for ambulance clinicians. BMJ Support Palliat Care 2020;10:296–9. 10.1136/bmjspcare-2019-001911 [DOI] [PubMed] [Google Scholar]
- 41.Eaton-Williams P, Barrett J, Mortimer C, et al. A national survey of ambulance paramedics on the identification of patients with end of life care needs. Br Paramed J 2020;5:8–14. 10.29045/14784726.2020.12.5.3.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goodwin L, Proctor A, Kirby K, et al. Staff stakeholder views on the role of UK paramedics in advance care planning for patients in their last year of life. Progress in Palliative Care 2021;29:76–83. 10.1080/09699260.2021.1872140 [DOI] [Google Scholar]
- 43.Kirk A, Crompton PW, Knighting K, et al. Paramedics and their role in end-of-life care: perceptions and confidence. Journal of Paramedic Practice 2017;9:71–9. 10.12968/jpar.2017.9.2.71 [DOI] [Google Scholar]
- 44.Murphy-Jones G, Timmons S. Paramedics’ experiences of end-of-life care decision making with regard to nursing home residents: an exploration of influential issues and factors. Emerg Med J 2016;33:722–6. 10.1136/emermed-2015-205405 [DOI] [PubMed] [Google Scholar]
- 45.Pease NJ, Sundararaj JJ, O’Brian E, et al. Paramedics and serious illness: communication training. BMJ Support Palliat Care 2022;12:e248–55. 10.1136/bmjspcare-2018-001734 [DOI] [PubMed] [Google Scholar]
- 46.Pentaris P, Mehmet N. Attitudes and perceptions of paramedics about end-of-life care: a literature review. Journal of Paramedic Practice 2019;11:206–15. 10.12968/jpar.2019.11.5.206 [DOI] [Google Scholar]
- 47.Kamphausen A, Roese H, Oechsle K, et al. Challenges faced by prehospital emergency physicians providing emergency care to patients with advanced incurable diseases. Emerg Med Int 2019;2019:3456471. 10.1155/2019/3456471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leibold A, Lassen CL, Lindenberg N, et al. Is every life worth saving: does religion and religious beliefs influence paramedic’s end-of-life decision-making? A prospective questionnaire-based investigation. Indian J Palliat Care 2018;24:9–15. 10.4103/IJPC.IJPC_128_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taghavi M, Simon A, Kappus S, et al. Paramedics experiences and expectations concerning advance directives: a prospective, questionnaire-based, bi-centre study. Palliat Med 2012;26:908–16. 10.1177/0269216311419885 [DOI] [PubMed] [Google Scholar]
- 50.Wiese CH, Lassen CL, Bartels UE, et al. International recommendations for outpatient palliative care and prehospital palliative emergencies-a prospective questionnaire-based investigation. BMC Palliat Care 2013;12:10. 10.1186/1472-684X-12-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wiese CH, Taghavi M, Meyer N, et al. Paramedics’ ‘end-of-life’ decision making in palliative emergencies. Journal of Paramedic Practice 2012;4:413–9. 10.12968/jpar.2012.4.7.413 [DOI] [Google Scholar]
- 52.Wiese CHR, Bartels UE, Zausig YA, et al. Prehospital emergency treatment of palliative care patients with cardiac arrest: a retrolective investigation. Support Care Cancer 2010;18:1287–92. 10.1007/s00520-009-0746-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wiese CHR, Bartels UE, Ruppert D, et al. Treatment of palliative care emergencies by prehospital emergency physicians in Germany: an interview based investigation. Palliat Med 2009;23:369–73. 10.1177/0269216309102987 [DOI] [PubMed] [Google Scholar]
- 54.Wiese CHR, Barrels UE, Graf BM, et al. Out-of-hospital opioid therapy of palliative care patients with “ acute dyspnoea ”: a retrospective multicenter investigation. J Opioid Manag 2009;5:115–22. 10.5055/jom.2009.0013 [DOI] [PubMed] [Google Scholar]
- 55.Hauch H, El Mohaui N, Wolff JEA, et al. Out-of-hospital emergencies in children under palliative home care. Front Pediatr 2021;9:734181. 10.3389/fped.2021.734181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.James HSE, Smith AC, Thomas EE, et al. Exploring paramedics’ intention to use a specialist palliative care telehealth service. Progress in Palliative Care 2021;29:106–13. 10.1080/09699260.2020.1852657 [DOI] [Google Scholar]
- 57.Lord B, Andrew E, Henderson A, et al. Palliative care in paramedic practice: a retrospective cohort study. Palliat Med 2019;33:445–51. 10.1177/0269216319828278 [DOI] [PubMed] [Google Scholar]
- 58.Mott C, Herbert A, Malcolm K, et al. Emergencies in pediatric palliative care: a survey of ambulance officers to understand the interface between families and ambulance services. J Palliat Med 2020;23:1649–52. 10.1089/jpm.2019.0299 [DOI] [PubMed] [Google Scholar]
- 59.Swetenham K, Grantham H, Glaetzer K. Breaking down the silos: collaboration delivering an efficient and effective response to palliative care emergencies. Progress in Palliative Care 2014;22:212–8. 10.1179/1743291X13Y.0000000076 [DOI] [Google Scholar]
- 60.Juhrmann ML, Anderson NE, Boughey M, et al. Palliative paramedicine: comparing clinical practice through guideline quality appraisal and qualitative content analysis. Palliat Med 2022;36:1228–41. 10.1177/02692163221110419 [DOI] [PubMed] [Google Scholar]
- 61.Rosa A, Dissanayake M, Carter D, et al. Community paramedicine to support palliative care. Progress in Palliative Care 2022;30:11–5. 10.1080/09699260.2021.1912690 [DOI] [Google Scholar]
- 62.Carter AJE, Harrison M, Kryworuchko J, et al. Essential elements to implementing a paramedic palliative model of care: an application of the consolidated framework for implementation research. J Palliat Med 2022;25:1345–54. 10.1089/jpm.2021.0459 [DOI] [PubMed] [Google Scholar]
- 63.Carter AJE, Harrison M, Goldstein J, et al. Providing palliative care at home aligns with the professional identity of paramedics: a qualitative study of paramedics and palliative health care providers. Can J Emerg Med 2022;24:751–9. 10.1007/s43678-022-00369-y [DOI] [PubMed] [Google Scholar]
- 64.McCormick G, Thompson SR. The provision of palliative and end-of-life care by paramedics in new zealand communities: a review of international practice and the New Zealand context. Whitireia Nurs Heal J 2019:51–7. [Google Scholar]
- 65.Anderson NE, Robinson J, Goodwin H, et al. ’mum, I think we might ring the ambulance, okay?’ A qualitative exploration of bereaved family members’ experiences of emergency ambulance care at the end of life. Palliat Med 2022;36:1389–95. 10.1177/02692163221118204 [DOI] [PubMed] [Google Scholar]
- 66.Surakka LK, Peake MM, Kiljunen MM, et al. Preplanned participation of paramedics in end-of-life care at home: a retrospective cohort study. Palliat Med 2021;35:584–91. 10.1177/0269216320981713 [DOI] [PubMed] [Google Scholar]
- 67.Surakka LK, Hökkä M, Törrönen K, et al. Paramedics’ experiences and educational needs when participating end-of-life care at home: a mixed method study. Palliat Med 2022;36:1217–27. 10.1177/02692163221105593 [DOI] [PubMed] [Google Scholar]
- 68.Peran D, Uhlir M, Pekara J, et al. Approaching the end of their lives under blue lights and sirens - scoping review. J Pain Symptom Manage 2021;62:1308–18. 10.1016/j.jpainsymman.2021.04.023 [DOI] [PubMed] [Google Scholar]
- 69.Boaventura JR, Pessalacia JDR, Ribeiro AA, et al. Palliative care in the pre-hospital service in Brazil: experiences of health professionals. BMC Palliat Care 2022;21:4. 10.1186/s12904-021-00890-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gov.uk [internet]. 2022. Available: https://assets.publishing.service.gov.uk/media/5d42be4eed915d09d8945db9/SRIA_-_REA_final__Dec_2019_Heart___003_.pdf [Accessed 14 Dec 2022].
- 71.Franzen SRP, Chandler C, Lang T. Health research capacity development in low and middle income countries: reality or rhetoric? A systematic meta-narrative review of the qualitative literature. BMJ Open 2017;7:e012332. 10.1136/bmjopen-2016-012332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Huppert D, Griffiths M. Police mental health partnership project: police ambulance crisis emergency response (PACER) model development. Australas Psychiatry 2015;23:520–3. 10.1177/1039856215597533 [DOI] [PubMed] [Google Scholar]
- 73.Binns CW. Health research-essential link to equity in development. Asia Pac J Public Health 1990;4:278. 10.1177/101053959000400420 [DOI] [Google Scholar]
- 74.WHO.int [internet]. 2022. Available: www.who.int/publications/i/item/who-his-hgf-hfworkingpaper-19.4 [Accessed 14 Dec 2022].
- 75.WHO.int [internet]. 2022. Available: https://apps.who.int/iris/handle/10665/345532 [Accessed 14 Dec 2022].
- 76.Helmer J, Baranowski L, Armour R, et al. Developing a paramedic approach to palliative emergencies. Progress in Palliative Care 2021;29:72–5. 10.1080/09699260.2020.1852656 [DOI] [Google Scholar]
- 77.Pekarsky B, Seymour-Walsh A, Wright C, et al. The role of ambulance services in reducing the gaps in access to end-of-life care: from conversations to policy. Progress in Palliative Care 2021;29:98–105. 10.1080/09699260.2020.1871174 [DOI] [Google Scholar]
- 78.Rowland K, Schumann S-A. PURLs. palliative care: earlier is better. J Fam Pract 2010;59:695–8. [PMC free article] [PubMed] [Google Scholar]
- 79.Quest TE, Asplin BR, Cairns CB, et al. Research priorities for palliative and end-of-life care in the emergency setting. Acad Emerg Med 2011;18:e70–6. 10.1111/j.1553-2712.2011.01088.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-071116supp001.pdf (65.9KB, pdf)
bmjopen-2022-071116supp002.pdf (174.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. No additional data available.