Abstract
Diabetic foot (DF) has become a serious health problem in modern society, and it has been a hotspot of research for a long time. However, little scientometric analysis has been carried out on DF. In the present study, we analysed 8633 literature reports on DF in the Web of Science Core Collection from database inception until April 23, 2022. VOSviewer (Centre for Science and Technology Studies at Leiden University, Leiden, the Netherlands) and CiteSpace (College of Computing and Informatics, Drexel University, Philadelphia, United States) were employed to address high‐impact countries and institutions, journals, references, research hotspots, and key research fields in DF research. Our analysis findings indicated that publications on DF have increased markedly since 2016 and were primarily published in the United States of America. The recent studies focus on the amniotic membrane, foot ulcers, osteomyelitis, and diabetic wound healing. The five keyword clusters, which included DF ulcer and wound healing therapies, management and guidelines, neuropathy and plantar pressure, amputation and ischemia, and DF infection and osteomyelitis, are helpful for enhancing prevention, standardising treatment, avoiding complications, and improving prognosis. These findings indicated a method for future therapies and research in DF.
Keywords: CiteSpace, diabetic foot, scientometrics analysis, visualisation, VOSviewer
1. INTRODUCTION
Diabetic foot (DF) is defined as foot infection, ulceration, or tissue destruction in a person with diabetes mellitus (DM), accompanied by peripheral neuropathy and/or peripheral artery disease (PAD) in the lower extremity. 1 DF is one of the most common complications in patients with DM and directly affects the life quality of patients and leads to a 12% to 15% increase in disease‐related costs. 2 DF‐related morbidity, mortality, and health care costs have become a significant burden. 3 To summarise the hotspots and difficulties systematically is likely to improve prevention and therapeutic strategies to promote the efficacy of DF treatment.
Scientometrics analysis provides quantitative insights into the development of a given topic, including trends of outputs and focuses, collaboration networks, thematic research clusters, historic evolution patterns, and co‐citation networks. 4 Compared with descriptive reviews, scientometrics has the advantage of quickly identifying key issues of interest and guiding future research. In recent years, an increasing number of studies have applied scientometrics methods to investigate various aspects of DM and obtained important information. Studies on diabetic peripheral neuropathic pain have primarily focused on endocrinology, metabolism, and clinical neurology with the recent emerging keywords of “inflammation,” “activation,” “phenotype,” “adult,” and “receptor”. 5 The hotspots of diabetic neuropathy (DN) studies from 2016 to 2020 include micro‐ribonucleic acids, signal transduction pathways, single‐nucleotide polymorphisms, mesangial cells and podocytes, plant extracts, and hypoglycemic drug treatment. 6 Bibliometrics analysis revealed that lower limb amputation, diabetic foot infection (DFI), and the treatment and management of diabetic foot ulcer (DFU) were the hotspots of global DFU research. 7 In studies of genome‐wide association studies in diabetes, deoxyribonucleic acid methylation and genetic variation are two hotspots, and the identification of genetic phenotypes associated with adiposity, metabolic memory, pancreatic islets, and inflammation is the leading trend in research. 8 An analysis of DF research in New Zealand indicated that the focus on indigenous Māori was limited and that the incidence of diabetes‐related amputations was higher for these individuals, which indicates that future research must focus on reducing inequalities in diabetes‐related outcomes for the Māori. 9 The findings of all the aforementioned studies suggest that the United States has occupied a leading position in DM studies. 5 , 6 , 7 , 8 , 9 To date, no analysis has focused on DF; therefore, scientometrics analysis may help scientists understand the current situation and the developing trends of DF and display the hotspot themes, key documents, and key authors. 10
In this study, we conducted a scientometrics analysis of DF and proposed future research directions. We analysed and summarised the clusters of co‐occurring keywords in DF, including management and guidelines, therapies to treat DFU and achieve wound healing, DN and plantar pressure, amputation and ischemia, and DFI and osteomyelitis. This is the first extensive scientometrics analysis of DF research. The results of the present scientometrics analysis help scientists explore key evidence and highlight the emerging trends in DF research.
2. METHODS
2.1. Literature source and search strategy
The data utilised in scientometrics analysis were downloaded from the Science Citation Index Expanded database in the Web of Science Core Collection (WoSCC) from database inception until April 23, 2022. The workflow of scientometrics research is shown in Figure 1. We searched WoSCC using the topical retrieval terms: (“diabetic foot” OR “diabetes foot” OR “diabetes feet” OR “diabetic feet”) NOT (“comment” OR “commentary”). No language or time refinements were applied. Duplication was removed using CiteSpace.
FIGURE 1.
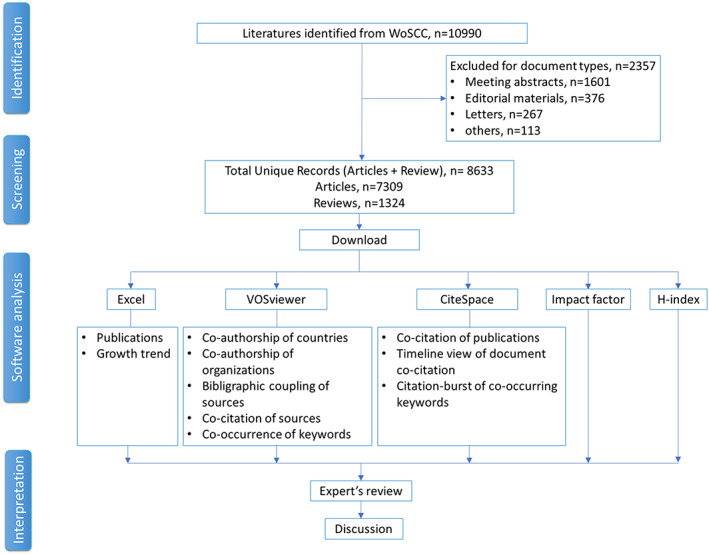
Flow chart of the scientometrics analysis
2.2. Methods of analysis
We aimed to address the hotspots and future trends of DF by analysing the co‐citation of documents and co‐occurring keywords. However, we attempted to provide a measure of the DF research network, which included countries, institutions, authors, journals, and publications.
VOSviewer (1.6.18; Centre for Science and Technology Studies at Leiden University, Leiden, the Netherlands) was utilised for bibliometric analysis, including co‐authorship of countries and organisations, bibliographic coupling of sources, co‐citation of sources, and co‐occurrence of keywords. CiteSpace (5.8.R3; College of Computing and Informatics, Drexel University, Philadelphia, United States) was utilised for co‐citation of publications, timeline view of document co‐citation network, and co‐occurring keywords citation‐burst analysis. In the visualisation maps, the node size represents the number of publications, and the node colour represents a cluster. The impact factors (IFs) of the journals were extracted from the journal citation report from Web of Science (WoS) (Clarivate, Philadelphia, PA), and the high citation indexes (H‐indexes) were downloaded from Scimago Journal and Country Rank (https://www.scimagojr.com/journalrank.php).
3. RESULTS
3.1. Yearly publication of diabetic foot studies
Literature reports on DF (n = 8633) were identified and included 7309 articles and 1324 reviews. Based on the search results of DF in WoSCC, the growth of publications on this topic can be divided into three stages: the beginning stage from 1955 to 1998, the slow growth stage from 1999 to 2015, and the fast growth stage from 2016 to 2022 (Figure 2A). In the first 44 years, 519 papers were published, and the annual publication accounted for less than 1% of the total publications each year. Since 2016, the annual publications on DF have numbered over 500 papers, and the rapid growth in DF can be explained by two factors. First, DM is a leading global health concern in an ageing society, 11 and the incidence of DFU is increasing among elderly patients with DM. 12 Second, in 2021, the World Health Organisation (WHO) launched the Global Diabetes Compact, published during the 100th anniversary of the discovery of insulin, in response to the growing burden of diabetes(https://www.who.int/publications/m/item/the-global-diabetes-compact), and on October 25, 2016, the State Council of China released the Healthy China 2030 plan. 13 Multiple countries have launched a series of plans on public health strategies. For bibliometrics analysis, more data may lead to more reliable results.
FIGURE 2.
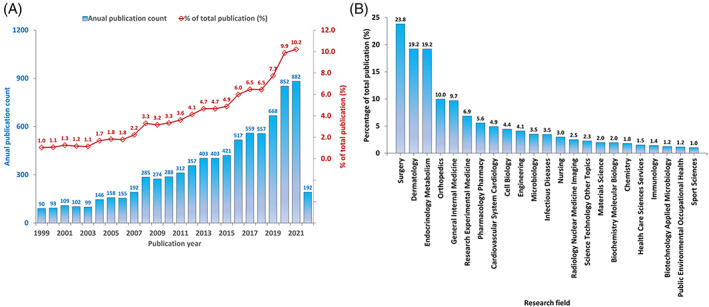
Publication data on diabetic foot research from 1955 to 2022. A, Annual publication of diabetic foot studies. B, The research fields of diabetic foot studies
As shown in Figure 2B, the top five research fields included surgery, dermatology, endocrinology, metabolism, orthopaedics, and general internal medicine. Among these fields, surgery accounts for 23.8% of the published articles regarding DF. Refractory wounds caused by DF are a challenge for clinical surgery. 14 The current treatment of DF aims to heal the wound, reduce complications, and avoid amputation, and timely surgical treatment of patients with DF may prevent foot ulcers and amputation. 15 Dermatology accounted for 19.2% of publications. The skin protects individuals from the outside environment, and any damage to the skin allows microbes to enter the body and can lead to infection. 16 DFU in diabetics is a wound that penetrates the dermis of the skin below the ankle. 17 Endocrinology, metabolism, and general internal medicine accounted for 28.9% of the publications. The treatment of DF primarily includes blood glucose control, supportive therapy, anti‐infection, maintenance of internal environmental stability, and wound management. 18 A systematic analysis of nine randomised controlled trials (RCTs) revealed that intensive glycemic control led to a 35% reduction in amputation risk in patients with DF. 19 These results highlight the complexity of DF and indicate that DF treatment requires comprehensive consideration.
3.2. Cooperation of countries/regions and institutions
In the collaboration network obtained through VOSviewer, the node size represents the number of publications, based on the country/region, institution, or author. Based on observation, 52 countries/regions had published more than 20 articles, among which the United States ranked first with 2529 (29.29%) articles (Figure 3A). The United States is followed by England, China, Germany, Italy, the Netherlands, Australia, India, Spain, France, and Turkey with 4558 (52.80%) publications collectively. Furthermore, various countries entered into close collaborations, which emphasises that DF is a global challenge. Developed countries have a larger share of total publications, which may be explained by objective and subjective factors. With regard to objective factors, developed countries spend more money on scientific research. With regard to subjective factors, the incidence of DM in developed countries is higher; thus, it is an urgent problem that needs to be solved.
FIGURE 3.
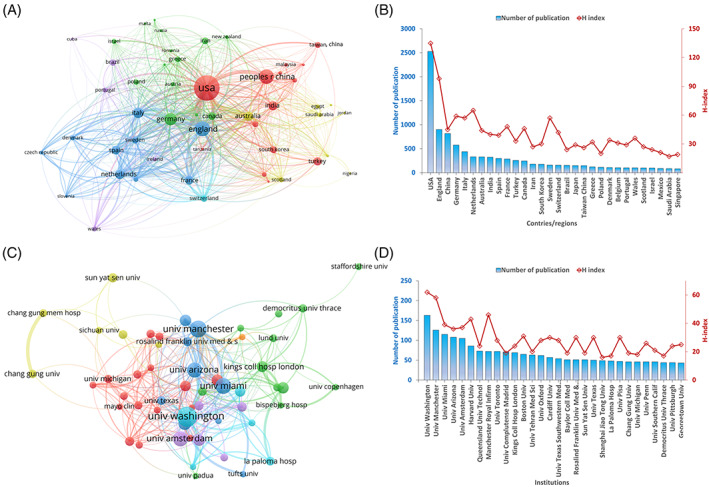
Cooperation between countries/regions and institutions. A, The countries/regions co‐authorship network contains 52 nodes and 648 links. The size of the nodes and lines represent the number of publications and cooperation, respectively, in a country/region. Different coloured lines represent six different clusters. B, The number of publications and the H‐index scores, based on countries/regions. C, The institution co‐authorship network contains 55 nodes and 358 links. The node size and line represent the number of publications from the institution and their cooperation, respectively. Different coloured lines represent seven different clusters. D, The number of publications and the H‐index scores of the institutions
Sixty institutions have each published more than 30 articles One‐half of the top 10 institutions are from the United States, with the University of Washington (Seattle, WA; 163 articles) ranking first (Figure 3C), which indicates the great scientific strength of the United States. Other institutions in the top 10 were the University of Amsterdam (Amsterdam, Netherlands), Queensland University of Technology (Brisbane City, Queensland, Australia), Manchester Royal Infirmary (Manchester, England), the University of Toronto (Toronto, Ontario, Canada), and Complutense University of Madrid (Madrid, Spain). The impact of individual scientific achievements is measured by different bibliometrics such as the H‐index, journal impact factor (IF), number of publications, and number of citations. 20 The H‐index is accessed from WoS through the “citation report.” The H‐index of researchers revealed that they have at most H papers cited at least H times. 21 The total H‐index of DF studies is 167. The United States has an H‐index of 135 and has several world‐famous institutions. Compared with other countries/regions, the United States has obvious advantages and makes outstanding contributions to the research on DF. England (H‐index = 98), the Netherlands (H‐index = 65), and Germany (H‐index = 59) have also made outstanding contributions to the study of DF.
3.3. Journals and journal co‐citation
The top 20 journals in the DF field are listed in Table 1. The top journal is the International Journal of Lower Extremity Wounds with 336 documents, and the second top journal is the International Wound Journal with 269 documents. Of the top 20 journals, 13 journals are from the United States, six journals are from the United Kingdom, and one journal is from Ireland. One‐half of the top 20 journals have an IF >3.0, and nine journals have an H‐index >100. The journal with the highest IF and an H‐index is Diabetes Care, with an IF of 19.112 and H‐index of 363.
TABLE 1.
The top 20 journals publishing articles on diabetic foot
| Rank | Journal Name | No. of documents | No. of citations | IF (2020) | H‐index (2021) |
|---|---|---|---|---|---|
| 1 | International Journal of Lower Extremity Wounds | 336 | 3010 | 2.057 | 42 |
| 2 | International Wound Journal | 269 | 5022 | 3.315 | 70 |
| 3 | Journal of Wound Care | 259 | 2689 | 2.072 | 68 |
| 4 | Diabetic Medicine | 230 | 10 955 | 4.359 | 152 |
| 5 | Wounds: A Compendium of Clinical Research and Practice | 218 | 2192 | 1.546 | 42 |
| 6 | Journal of the American Podiatric Medical Association | 197 | 2923 | 0.675 | 60 |
| 7 | Wound Repair and Regeneration | 189 | 11 433 | 3.617 | 117 |
| 8 | Diabetes Care | 180 | 18 882 | 19.112 | 380 |
| 9 | Diabetes/Metabolism Research and Reviews | 175 | 8064 | 4.876 | 117 |
| 10 | Diabetes Research and Clinical Practice | 158 | 3460 | 5.602 | 122 |
| 11 | Foot and Ankle International | 109 | 3194 | 2.827 | 114 |
| 12 | Journal of Diabetes and Its Complications | 109 | 2962 | 2.852 | 88 |
| 13 | Journal of Foot and Ankle Surgery | 105 | 1190 | 1.286 | 70 |
| 14 | Journal of Foot and Ankle Research | 94 | 1077 | 2.303 | 45 |
| 15 | Advances in Skin and Wound Care | 93 | 1085 | 2.347 | 64 |
| 16 | PloS One | 79 | 2128 | 3.240 | 367 |
| 17 | Journal of Vascular Surgery | 78 | 6577 | 4.268 | 202 |
| 18 | Plastic and Reconstructive Surgery | 69 | 2910 | 4.730 | 188 |
| 19 | Ostomy Wound Management | 67 | 1611 | 2.629 | 0 |
| 20 | Advances in Wound Care | 62 | 1876 | 4.730 | 31 |
Abbreviations: H‐index, high citation index; IF, impact factor.
The top 20 co‐cited journals in the DF field are listed in Table 2. Based on the number of cited publications, the top three journals are Diabetes Care (23 003 citations), Diabetic Medicine (8374 citations), and Wound Repair and Regeneration (6360 citations). Five journals have an IF >10.0 and eight journals have an IF >5.0. Of the top 20 journals, 11 journals are from the United States; seven journals, from the United Kingdom, one journal, from Germany; and one journal is from Ireland.
TABLE 2.
The top 20 co‐cited journals for studies on diabetic foot
| Rank | Source | No. of citations | IF (2020) | H‐index (2021) |
|---|---|---|---|---|
| 1 | Diabetes Care | 23 003 | 19.112 | 380 |
| 2 | Diabetic Medicine | 8374 | 4.359 | 152 |
| 3 | Wound Repair and Regeneration | 6360 | 3.617 | 117 |
| 4 | Diabetes/Metabolism Research and Reviews | 5760 | 4.876 | 117 |
| 5 | Journal of Vascular Surgery | 5663 | 4.268 | 202 |
| 6 | Diabetologia | 4880 | 10.122 | 241 |
| 7 | International Wound Journal | 4280 | 3.315 | 70 |
| 8 | Clinical Infectious Diseases | 4217 | 9.079 | 353 |
| 9 | Lancet | 3892 | 79.321 | 807 |
| 10 | New England Journal of Medicine | 3528 | 91.245 | 1079 |
| 11 | Plastic and Reconstructive Surgery | 3353 | 4.730 | 188 |
| 12 | Journal of Wound Care | 3246 | 2.072 | 68 |
| 13 | Diabetes Research and Clinical Practice | 3033 | 5.602 | 122 |
| 14 | Foot and Ankle International | 2776 | 2.827 | 114 |
| 15 | Journal of Foot and Ankle Surgery | 2773 | 1.286 | 70 |
| 16 | JAMA Journal of the American Medical Association | 2760 | 56.272 | 709 |
| 17 | Journal of the American Podiatric Medical Association | 2690 | 0.675 | 60 |
| 18 | PLoS One | 2683 | 3.240 | 367 |
| 19 | Diabetes | 2401 | 9.461 | 345 |
| 20 | Journal of Diabetes and Its Complications | 2295 | 2.852 | 88 |
Abbreviations: H‐index, high citation index; IF, impact factor.
Many studies on DF are published in low‐IF journals, which suggests that high‐quality research is required in DF studies. The cited journals generally have a higher IF, which indicates that the cited research is closer to the basics or the theory is stronger.
3.4. Analysis of co‐cited references
Co‐cited references are references that are co‐cited in one or more publications. The top 20 commonly cited references for DF are listed in Table 3. The highest number of co‐citations is 529, seven references are co‐cited 100–250 times, and other references are co‐cited 70–100 times. Topics covered by highly cited papers include guidelines, 22 , 23 , 24 , 25 epidemiology, 26 burden of DF, 27 , 28 and meta‐analysis. 29 Five articles are published in the top journals with an IF >10, and they include the New England Journal of Medicine, the Journal of the American Medical Association (JAMA), Lancet, Diabetes Care, and Diabetologia.
TABLE 3.
The top 20 cited articles related to diabetic foot
| Rank | Cited number | Title of the article | Year | Journal name | Impact factor (2020) | H‐index (2021) |
|---|---|---|---|---|---|---|
| 1 | 529 | Diabetic foot ulcers and their recurrence | 2017 | New England Journal of Medicine | 91.245 | 1079 |
| 2 | 250 | Global epidemiology of diabetic foot ulceration: a systematic review and meta‐analysis | 2017 | Annals of Medicine | 4.709 | 117 |
| 3 | 237 | Executive summary: 2012 infectious diseases society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections | 2012 | Clinical Infectious Diseases | 9.079 | 353 |
| 4 | 187 | IWGDF guidance on the diagnosis and management of foot infections in persons with diabetes | 2016 | Diabetes‐Metabolism Research and Reviews | 4.876 | 117 |
| 5 | 124 | Preventing foot ulcers in patients with diabetes | 2005 | JAMA Journal of the American Medical Association | 56.272 | 709 |
| 6 | 118 | Medical treatment of diabetic foot infections | 2004 | Clinical Infectious Diseases | 9.079 | 353 |
| 7 | 116 | The management of diabetic foot: a clinical practice guideline by the society for vascular surgery in collaboration with the American podiatric medical association and the society for vascular medicine | 2016 | Journal of Vascular Surgery | 4.268 | 202 |
| 8 | 113 | Association of diabetic foot ulcer and death in a population‐based cohort from the United Kingdom | 2016 | Diabetic Medicine | 4.359 | 152 |
| 9 | 98 | Practical guidelines on the management and prevention of the diabetic foot 2011 | 2012 | Diabetes‐Metabolism Research and Reviews | 4.876 | 117 |
| 10 | 97 | The global burden of diabetic foot disease | 2005 | Lancet | 79.321 | 807 |
| 11 | 96 | Burden of diabetic foot ulcers for Medicare and private insurers | 2014 | Diabetes Care | 19.112 | 380 |
| 12 | 90 | The 2015 IWGDF guidance documents on prevention and management of foot problems in diabetes: development of an evidence‐based global consensus | 2016 | Diabetes/Metabolism Research and Reviews | 4.876 | 117 |
| 13 | 88 | IWGDF guidance on the prevention of foot ulcers in at‐risk patients with diabetes | 2016 | Diabetes/Metabolism Research and Reviews | 4.876 | 117 |
| 14 | 85 | Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update) | 2020 | Diabetes/Metabolism Research and Reviews | 4.876 | 117 |
| 15 | 83 | Prevention and management of foot problems in diabetes: a summary guidance for daily practice 2015, based on the IWGDF guidance documents | 2016 | Diabetes/Metabolism Research and Reviews | 4.876 | 117 |
| 16 | 83 | Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE study | 2008 | Diabetologia | 10.122 | 241 |
| 17 | 80 | The society for vascular surgery lower extremity threatened limb classification system: risk stratification based on wound, ischemia, and foot infection (WIFI) | 2014 | Journal of Vascular Surgery | 4.268 | 202 |
| 18 | 78 | Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update) | 2020 | Diabetes/Metabolism Research and Reviews | 4.876 | 117 |
| 19 | 74 | Burden of infected diabetic foot ulcers on hospital admissions and costs | 2016 | Annals of Vascular Surgery | 1.466 | 75 |
| 20 | 72 | Challenges in the treatment of chronic wounds | 2015 | Advances in Wound Care | 4.73 | 31 |
Abbreviations: H‐index, high citation index; IF, impact factor.
Figure 4 shows the timeline map of co‐cited references from 1999 to 2022. The reference network map has 1940 nodes and 9923 links. All references form 14 clusters, and positive co‐citation exists among the references. The early literature focused on rehabilitation, offloading, dressings, and granulocyte colony‐stimulating factor (G‐CSF). Co‐citations in G‐CSF reduced quickly after the year 2004, and a meta‐analysis of RCTs using G‐CSF therapy demonstrated no benefits in infection eradication. 30 The co‐citation of offloading persisted for a longer time. Pressure analyses are required to understand the pressures that result in DF and improve the effectiveness of interventions., 31 The finite element method has been utilised to study plantar pressure. 32 Proper pressure offloading may stabilise soft tissues and accelerate healing of a DFU. 33
FIGURE 4.
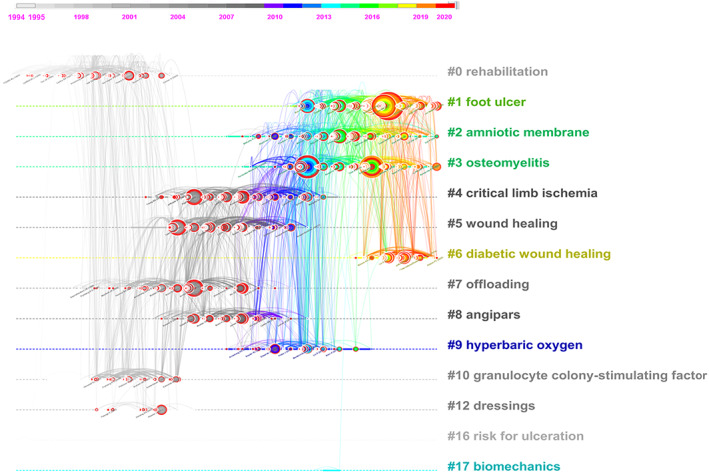
Timeline view of co‐cited references. The node size represents the total number of references, and the node colour represents the time slice. Different coloured lines indicate that two articles were co‐cited in one article
Later co‐cited references were in critical limb ischemia, wound healing, and semelil (Angipars; Pars Roos Drug Company, Tehran, Iran). Angipars is an herbal formulation capable of reducing skin ageing and inducing microvascularization and anti‐inflammation. 34 Angipars have been reported to improve the distal latency and amplitude of the motor ulnar nerve in DF, 35 but the evidence remains limited.
Recent co‐cited references focused on foot ulcers, amniotic membrane, osteomyelitis, and diabetic wound healing. A multicenter, double‐blinded RCT demonstrated that human amniotic membrane preparation is safe and promising for DF treatment. 36 Amniotic membrane allografts could facilitate wound closure with standard therapy in chronic ulcers that are resistant to closure, 37 which indicates that amniotic membrane allografts are promising for improving wound healing. Various modalities such as human amniotic membrane preparations, growth factors, stem cells, cultured fibroblasts, keratinocytes were applied to treat difficult‐to‐heal ulcers. 38
3.5. Keywords analysis and citation burstness
Keywords indicate the hot spots and future trends in the DF research field. Keyword clustering is formed by keywords with similar research topics, and each cluster is marked by frequently used keywords in the articles. Keywords with a co‐occurrence >50 were included in the keyword clustering map (Figure 5A). The keywords were classified into five clusters, which included 218 nodes and 13 991 links. Cluster 1 (75 items) referred to DFU and wound healing; cluster 2 (48 items) referred to prevention, care, management, and guidelines of diabetes complications; cluster 3 (35 items) referred to risk of DF; cluster 4 (32 items) referred to amputation; and cluster 5 (28 items) referred to osteomyelitis and infections. We summarised the top 15 keywords of each cluster to systematically understand DF and provide suggestions for future research (Figure 6).
FIGURE 5.
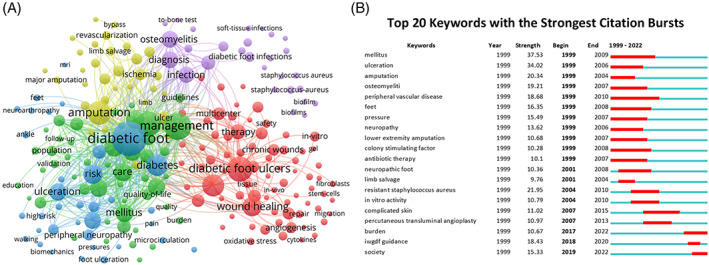
Co‐occurrence of keywords. A, The keywords co‐occurrence clustering network. Node size and node colour represent the number of keywords and clusters. Different coloured lines indicate that the two keywords appeared in an article. B, The top 20 keywords with the strongest citation bursts. The red bars indicate that certain keywords are frequently referenced at a certain time
FIGURE 6.
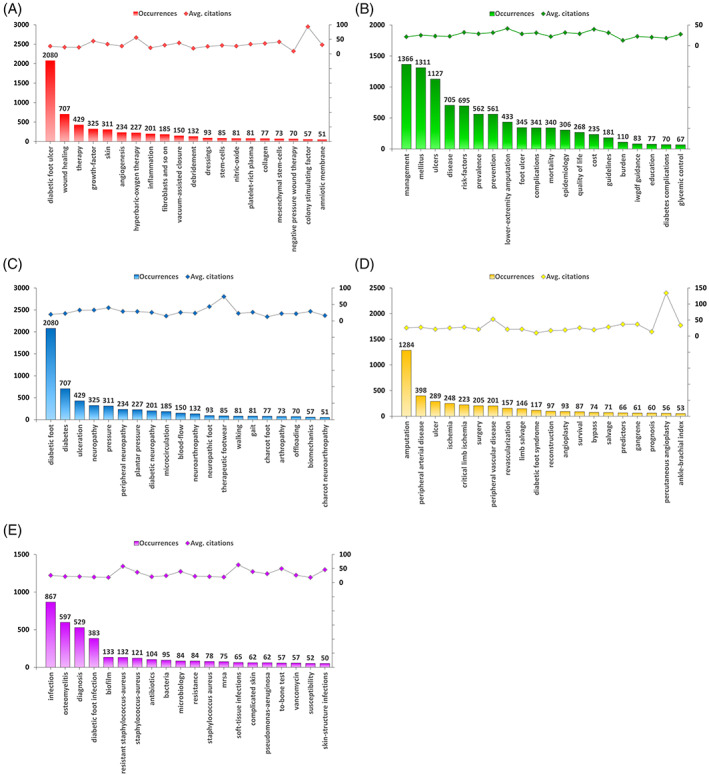
The top 20 keywords of five co‐occurrence keywords clusters. A, Therapies to achieve wound healing. B, Management and guidelines. C, Neuropathy and plantar pressure. D, Amputation and ischemia. E, Infection and osteomyelitis
Keywords with citation bursts have a higher citation rate within a certain period, which can test whether a research area is popular at that time. In all, 270 keywords had citation bursts in the field of DF from 1999 to 2022. The top 20 are listed in Figure 5B. Much burstness occurred in the earlier times and included DFU amputation and limb salvage. The type of DFU was classified as neuropathic ischemic or neuroischemic ulcers based on the International Working Group on the Diabetic Foot (IWGDF) consensus. 39 Hyperbaric oxygen therapy combined with standard management to treat DFU may promote wound healing and decrease the risk of major amputation. 40 Recent bursts focused on the burden of DF on society and IWGDF guidance. Recent studies have tended to adopt the IWGDF guidelines for risk evaluation. 41 , 42 IWGDF DFI guidelines were published in 1999 and were utilised to classify FD states with the Perfusion Extent Depth Infection and Sensation classification, which can be utilised to assess clinical practise and help improve patient care 43
4. DISCUSSION
In this study, we conducted a scientometrics analysis of DF and analysed clusters of co‐occurring keywords in DF, including management and guidelines, therapies to treat DFU and achieve wound healing, DN and plantar pressure, amputation and ischemia, and DFI and osteomyelitis.
4.1. Therapies of DFU and wound healing
Epidemiological studies have revealed that 15% to 25% of diabetics develop DFU during their lifetime. 44 DFU is a major health risk for DM patients and leads to limb loss and mortality. In the absence of intact skin covering, these wounds can be reopened and gradually spread, which may result in sepsis and amputations. 45 Thus, the treatment of chronic wounds to promote healing is a major area of research in DFU. 46 The top 15 keywords related to therapies for DFU are shown in Figure 6A.
The standard therapies of DFUs include offloading and controlling the blood glucose level, thorough wound debridement, negative pressure drainage, and infection management. 47 , 48 Offloading is the primary intervention for healing DFUs. 49 Debridement removes necrotic debris, senescent cells, infected tissue, and biofilms to transform chronic ulcers into biologically active acute wounds and accelerate healing. 50
Furthermore, strategically designed wound dressings can facilitate wound healing. Therefore, a series of new dressings have been reported recently for treating DF, such as an injectable glucose‐responsive multifunctional metal–organic drug‐loaded hydrogel, 51 an asiaticoside‐loaded multifunctional biomimetic nanofibrous scaffold, 52 and bioactive agent‐loaded polymer‐based wound dressing materials. 53 Three‐dimensional scaffolds can be fabricated through bioprinting and electrospinning, offer excellent biocompatibility and mechanical properties, and promote cell adhesion and proliferation. 54 Natural polymers such as collagen, gelatin, alginate, and fibrin, and synthetic polymers are employed for bioprinting. Antibiotics, growth factors, 55 colony‐stimulating factors, 56 stem cells, 57 fibroblasts, 58 keratinocytes, 59 endothelial progenitor cells, 60 and platelet‐rich plasma 61 can be supplemented to stimulate healing. Furthermore, some systems have been developed to incorporate and release bioactive nanoparticles on demand. 62
DFU involves damage to multiple tissues. Therefore, distraction osteogenesis is utilised to induce new bone, angiogenesis, and local perfusion, and proximal tibial cortex transverse distraction is a promising surgical method. 47 , 48 Hyperbaric oxygen therapy may increase cell proliferation, collagen deposition, angiogenesis, and host defence to reduce cases of infection and promote the healing of chronic or severe wounds. 63
4.2. Management and guidelines
One study reviewed 22 DM clinical practise guidelines and summarised the recommendations for DF complications, such as DFU, Charcot neuropathy (CN), and diabetic foot osteomyelitis. 64 The four recommendations for standard care for DFU and six recommendations for diagnosis and treatment of CN are consistent. 64 The care standard for DFU involves four principles—decompression, debridement, infection management, and revascularization—and adjuvant therapies such as negative pressure wound therapy and hyperbaric oxygen therapy. 65 Five clinical practise guidelines were developed by five independent working groups of the IWGDF, 66 , 67 which covered the five aspects of DF: prevention, 68 offloading, 69 infection, 70 peripheral arterial disease, 71 and wound management. 14 Multidisciplinary guidelines for the prevention and management of DF suggest a whole course of patient care and multidisciplinary teamwork, which includes endocrinology, burns, vascular surgery, orthopaedics, foot and ankle surgery, and cardiology. 72
The risk of DF has always been a research hotspot. A study 73 in New South Wales (Australia) found that, among people with DM aged ≥45 years, the prevalence of diabetes‐related foot disease was 10.8%; DFU, 5.4%; DFI, 5.2%; diabetic gangrene, 0.4%; and diabetes‐related lower extremity amputation (DLEA), 0.9%. Older age, male sex, single status, having an ethnicity from English‐speaking countries, a low socioeconomic position, low physical activity, history of diabetes for >15 years, and cardiovascular disease were risk factors for diabetes‐related foot disease, DFU, and DFI. 74 A case–control study 75 from Egypt found that three or more comorbidities, two or more diabetic complications, callus, and flatfoot are risk predictors of DFUs, whereas diet control, oral hypoglycemic drugs, insulin, and an intact vibration sense are protective predictors. A cohort study 76 in South Korea found that DFU among people of low socioeconomic position was strongly associated with increased rates of amputation and mortality. A systematic review suggested that barefoot plantar pressure and adherence were associated with DFU. 77 A meta‐analysis suggests that in Ethiopia, socio‐demographic factors, body weight, and health care practise are risk factors for DFU. 78 Identifying the risk factors is helpful for the effective prevention and treatment of DF.
4.3. Neuropathy and plantar pressure
DN is the presence of certain physical signs or specific symptoms suggestive of neuropathy in DM patients after excluding other causes of neuron damage. The risks of DN increase with age and diabetes duration, poor glycemic control, hyperlipidemia, hypertension, obesity, and reduced physical activity. Early diagnosis and management of DN may limit or delay disease progression. 79 The temperature perception test and pinprick pain perception test are utilised to evaluate thin nerve fibre function, and the vibration perception test, monofilament touch perception test, and ankle reflexes test are utilised to evaluate long nerve fibre function. A DN diagnosis requires at least two semi‐quantitative tests. 80 A nerve conduction study is one of the gold standards of DN diagnosis, and quantitative sensory measurement, the neurological function scoring system, confocal microscopy, and high‐frequency ultrasound may be utilised for early DN screening. 81
Patients with DN tend to have an increased forefoot‐to‐rearfoot plantar pressure ratio 82 and plantar pressure. 83 Owing to the loss of the protective sensation of pain in the feet, patients with DM may load their feet too heavily, which leads to the development of DFU. Therefore, increased plantar pressure is a main mechanical trigger for DF, and the reduction of plantar pressure is an important part of the management of DF. In patients with DM, weight‐bearing exercise is associated with better plantar microcirculation and lower plantar tissue hardness and is not associated with the risk of DFUs. 84 Monitoring temperature and pressure as a whole may help predict DFU in clinical practice; various technologies have been developed to measure in‐shoe plantar pressures and skin temperatures. 85 Smart wearable devices have been developed to prevent DF by monitoring pressure, humidity, and temperature. 86 Some researchers tried to employ a low‐cost three‐dimensional printing technique to monitor overloading of the foot in daily life. 87 Suitable exercises and footwear may provide effective offloading interventions to prevent the occurrence of DF.
4.4. Amputation and ischemia
DFU is a serious health care problem worldwide, and minor traumas can have catastrophic consequences. 88 Patients with diabetes should be classified based on their risks of developing DFU and should be screened for risk factors for DFU at least annually. The risk classification system developed by the IWGDF is very useful in daily clinical practise. 89 The healing of a DF wound is frequently complicated by critical limb‐threatening ischemia, which may require amputation. Imminent arterial revascularization is an option to avoid amputation. 90 More than 80% of lower extremity amputations are secondary to dysvascular disease resulting from PAD, DM, or both. 91
The incidence of dysvascular lower extremity amputation has not decreased greatly, though the treatment of DM has improved. A multidisciplinary team approach is critical for amputation prevention. 88 Limb‐preservation teams are believed to be beneficial for DF management, and a team comprises vascular surgeons, podiatrists, foot and orthopaedic surgeons, vascular medicine specialists, endocrinologists, infectious diseases specialists, plastic surgeons, physical medicine specialists, pedorthists and orthotists, dietitians, and nurses experienced in wound care. 92
4.5. DFI and osteomyelitis
The top 15 keywords related to DFI are shown in Figure 6E. Approximately 2.2% to 6.3% of patients with DM may experience DFI annually, 50% to 60% cases of DFU may progress to DFI, and 20% to 66% cases of DFI are complicated with diabetic foot osteomyelitis. 22 The Infectious Diseases Society of America (IDSA) classification system is commonly used to classify DFI and includes four grades: “no infection,” “mild infection,” “moderate infection,” and “severe infection.” Patients with osteomyelitis have worse outcomes. 93 , 94 Therefore, the IDSA classification has been modified and now includes group 1 (“no infection”), group 2 (“mild soft tissue infection”), group 3 (“moderate or severe soft tissue infection”), and group 4 (“moderate or severe bone infection”). 94
The management of DFI relies on a combination of effective surgical and antimicrobial treatment. 95 The microbiology of DFI is diverse. Staphylococcus aureus (S. aureus) is the organism most commonly identified, and methicillin‐resistant S. aureus (MRSA) represents 18.0% of S. aureus infection cases. 96 The incidence of Pseudomonas aeruginosa and multidrug‐resistant gram‐negative bacilli is growing. 97 The choice of antibiotics to treat DFI is highly individualised, based on the site, extent, severity of infection, pathogens involved, presence of concomitant osteomyelitis, and comorbidities. 95 Ten principles for antimicrobial stewardship exist and include preventing DFI, diagnosing DFI correctly, excluding non‐infectious causes of DVI, identifying causative pathogens, differentiating between soft tissue and bone infection, ensuring specialist consultation for most moderate and all severe infections, choosing an effective antibiotic regimen with the narrowest spectrum, optimising patient‐related effectiveness of antibiotic therapy, medical therapy, and surgical treatment. 98 For diabetic foot osteomyelitis treatment, using antibiotics that penetrate the bone and are active against biofilms is important. 99 Researchers have suggested that the maximum duration of antibiotic therapy should be no more than 4 to 6 weeks. 100
4.6. Strengths and limitations
Data from the WoSCC were analysed in the present study. The literature in the WoSCC provides high‐quality research results on DF; therefore, it is ideal for bibliometric analysis. 101 The WoSCC database covers a substantial amount of data to study the topic of DF, which ensured the results obtained in this study were highly reliable. However, at present, the bibliometrics software is unable to distinguish between authors with the same abbreviations; therefore, some incorrect conclusions about authors may be included in this paper. This scientometrics study helps researchers to quickly understand the research hotspots and future trends in the field of DF.
5. CONCLUSIONS
In the present study, we utilised scientometrics to analyse DF research in the Science Citation Index Expanded database. Our results revealed the high‐impact countries and institutions, journals, references, research hotspots, and key research fields in DF research. Following the increasing incidences of DM and the health strategies in response to the growing burden of DM, publications on DF have increased remarkably since 2016. The United States leads the research on DF. The recent studies focus on the amniotic membrane, foot ulcers, osteomyelitis, and diabetic wound healing. The hotspots of DF studies include DFU and wound healing therapies, management and guidelines, neuropathy and plantar pressure, amputation and ischemia, DFI, and osteomyelitis. Our results revealed the high impact countries and institutions, journals, references, research hotspots, and key research fields in DF research and the directions for further research.
Shen J‐M, Chen J, Feng L, Feng C. A scientometrics analysis and visualisation of diabetic foot research from 1955 to 2022. Int Wound J. 2023;20(4):1072‐1087. doi: 10.1111/iwj.13964
Jin‐Ming Shen and Jie Chen contributed equally to this work.
Funding information National Natural Science Foundation of China, Grant/Award Number: 82171690; Natural Science Foundation of Zhejiang Province, Grant/Award Numbers: LY22H040002, LY21H040004
DATA AVAILABILITY STATEMENT
Data derived from public domain resources. [Web of Science (https://www.webofscience.com/); Scimago Journal & Country Rank (https://www.scimagojr.com/journalrank.php)].
REFERENCES
- 1. van Netten JJ, Bus SA, Apelqvist J, et al. Definitions and criteria for diabetic foot disease. Diabetes Metab Res Rev. 2020;36:e3268. [DOI] [PubMed] [Google Scholar]
- 2. de Sousa GP, Fontenele M, da Rocha RB, Cardoso VS. Update of topical interventions for healing diabetic ulcers—a systematic review. Int J Low Extrem Wounds. 2021;1‐13. [DOI] [PubMed] [Google Scholar]
- 3. Zhang Y, Lazzarini PA, McPhail SM, van Netten JJ, Armstrong DG, Pacella RE. Global disability burdens of diabetes‐related lower‐extremity complications in 1990 and 2016. Diabetes Care. 2020;43(5):964‐974. [DOI] [PubMed] [Google Scholar]
- 4. Li J, Goerlandt F, Reniers G. An overview of scientometric mapping for the safety science community: methods, tools, and framework. Safety Sci. 2021;134:105093. [Google Scholar]
- 5. Du SH, Zheng YL, Zhang YH, Wang MW, Wang XQ. The Last Decade Publications on Diabetic Peripheral Neuropathic Pain: A Bibliometric Analysis. Front Mol Neurosci. 2022;15:854000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shao Y. Bibliometric study of trends in the diabetic nephropathy research space from 2016 to 2020. Oxid Med Cell Longev. 2022;2022:8050137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Deng P, Shi HS, Pan XY, et al. Worldwide research trends on diabetic foot ulcers (2004–2020): suggestions for researchers. J Diabetes Res. 2022;2022:7991031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu Y, Wang Y, Qin S, et al. Insights into genome‐wide association study for diabetes: a bibliometric and visual analysis from 2001 to 2021. Front Endocrinol (Lausanne). 2022;13:817620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Carroll M, Al‐Busaidi IS, Coppell KJ, et al. Diabetes‐related foot disease research in Aotearoa New Zealand: a bibliometric analysis (1970‐2020). J Foot Ankle Res. 2022;15(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Goerlandt F, Li J, Reniers G. The landscape of risk communication research: a scientometric analysis. Int J Environ Res Public Health. 2020;17(9):3255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen KC, Chung CH, Lu CH, et al. Association between the use of dipeptidyl peptidase 4 inhibitors and the risk of dementia among patients with type 2 diabetes in Taiwan. J Clin Med. 2020;9(3):660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xu Y, Ouyang L, He L, Qu Y, Han Y, Duan D. Inhibition of exosomal miR‐24‐3p in diabetes restores angiogenesis and facilitates wound repair via targeting PIK3R3. J Cell Mol Med. 2020;24(23):13789‐13803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yang J, Siri JG, Remais JV, et al. The Tsinghua‐lancet commission on healthy cities in China: unlocking the power of cities for a healthy China. Lancet. 2018;391(10135):2140‐2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Game FL, Attinger C, Hartemann A, et al. IWGDF guidance on use of interventions to enhance the healing of chronic ulcers of the foot in diabetes. Diabetes Metab Res Rev. 2016;32(Suppl 1):75‐83. [DOI] [PubMed] [Google Scholar]
- 15. Lazaro‐Martinez JL, Alvaro‐Afonso FJ, Sevillano‐Fernandez D, Garcia‐Alvarez Y, Sanz‐Corbalan I, Garcia‐Morales E. Cellular proliferation, dermal repair, and microbiological effectiveness of ultrasound‐assisted wound debridement (uaw) versus standard wound treatment in complicated diabetic foot ulcers (dfu): an open‐label randomized controlled trial. J Clin Med. 2020;9(12):4032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhang M, Wang G, Wang D, et al. Ag@MOF‐loaded chitosan nanoparticle and polyvinyl alcohol/sodium alginate/chitosan bilayer dressing for wound healing applications. Int J Biol Macromol. 2021;175:481‐494. [DOI] [PubMed] [Google Scholar]
- 17. Bakker K, Apelqvist J, Lipsky BA, Netten JJ, Schaper NC. The 2015 IWGDF guidance documents on prevention and management of foot problems in diabetes: development of an evidence‐based global consensus. Diabetes Metab Res Rev. 2016;32:2‐6. [DOI] [PubMed] [Google Scholar]
- 18. Lin CJ, Yuan Y, Ji LQ, Yang XP, Yin GS, Lin SD. The amputation and survival of patients with diabetic foot based on establishment of prediction model. Saudi J Biol Sci. 2020;27(3):853‐858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fesseha BK, Abularrage CJ, Hines KF, et al. Association of hemoglobin a(1c) and wound healing in diabetic foot ulcers. Diabetes Care. 2018;41(7):1478‐1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jalipa F, Sy M, Espiritu AI, Jamora R. Bibliometric analysis of bacterial central nervous system infection research in Southeast Asia. BMC Neurol. 2021;21(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gershoni A, Vainer I, Reitblat O, et al. Research productivity across different ophthalmic subspecialties in the United States. BMC Health Serv Res. 2019;19(1):778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lipsky BA, Berendt AR, Cornia PB, et al. Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54(12):1679‐1684. [DOI] [PubMed] [Google Scholar]
- 23. Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA‐J Am Med Assoc. 2005;293(2):217‐228. [DOI] [PubMed] [Google Scholar]
- 24. Apelqvist J, Bakker K, van Houtum WH, Schaper NC. Practical guidelines on the management and prevention of the diabetic foot ‐ based upon the international consensus on the diabetic foot (2007) prepared by the international working group on the diabetic foot. Diabetes Metab Res Rev. 2008;24:S181‐S187. [DOI] [PubMed] [Google Scholar]
- 25. Lipsky BA, Senneville E, Abbas ZG, et al. Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3280. [DOI] [PubMed] [Google Scholar]
- 26. Walsh JW, Hoffstad OJ, Sullivan MO, Margolis DJ. Association of diabetic foot ulcer and death in a population‐based cohort from the United Kingdom. Diabet Med. 2016;33(11):1493‐1498. [DOI] [PubMed] [Google Scholar]
- 27. Rice JB, Desai U, Cummings A, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care. 2014;37(3):651‐658. [DOI] [PubMed] [Google Scholar]
- 28. Hicks CW, Selvarajah S, Mathioudakis N, et al. Burden of infected diabetic foot ulcers on hospital admissions and costs. Ann Vasc Surg. 2016;33:149‐158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhang PZ, Lu J, Jing YL, Tang S, Zhu DL, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta‐analysis. Ann Med. 2017;49(2):106‐116. [DOI] [PubMed] [Google Scholar]
- 30. Mahdipour E, Sahebkar A. The role of recombinant proteins and growth factors in the management of diabetic foot ulcers: a systematic review of randomized controlled trials. Journal of Diabetes Research. 2020;2020:6320514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chatwin KE, Abbott CA, Boulton A, Bowling FL, Reeves ND. The role of foot pressure measurement in the prediction and prevention of diabetic foot ulceration—a comprehensive review. Diabetes Metab Res Rev. 2020;36(4):e3258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ghazali MJ, Ren X, Rajabi A, Zamri W, Mustafah NM, Ni J. Finite element analysis of cushioned diabetic footwear using ethylene vinyl acetate polymer. Polymers. 2021;13(14):2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Al Khalifa A, Al Khalifa M, Khan RM, et al. Offloading plantar pressures in healthy adults: stirrup cast vs total contact cast. Foot Ankle Int.2022;43(5):6 [DOI] [PubMed] [Google Scholar]
- 34. Chorepsima S, Tentolouris K, Dimitroulis D, Tentolouris N. Melilotus: contribution to wound healing in the diabetic foot. J Herb Med. 2013;3(3):81‐86. [Google Scholar]
- 35. Bakhshayeshi S, Madani SP, Hemmatabadi M, Heshmat R, Larijani B. Effects of Semelil (ANGIPARS [TM]) on diabetic peripheral neuropathy: a randomized, double‐blind placebo‐controlled clinical trial. DARU‐J Pharm Sci. 2011;19(1):65‐70. [PMC free article] [PubMed] [Google Scholar]
- 36. Game F, Gray K, Davis D, et al. The effectiveness of a new dried human amnion derived membrane in addition to standard care in treating diabetic foot ulcers: a patient and assessor blind, randomised controlled pilot study. Int Wound J. 2021;18(5):692‐700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lakmal K, Basnayake O, Hettiarachchi D. Systematic review on the rational use of amniotic membrane allografts in diabetic foot ulcer treatment. BMC Surg. 2021;21(1):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Eleftheriadou I, Samakidou G, Tentolouris A, Papanas N, Tentolouris N. Nonpharmacological management of diabetic foot ulcers: an update. Int J Lower Extrem Wounds. 2021;20(3): 188‐197. [DOI] [PubMed] [Google Scholar]
- 39. Granado‐Casas M, Martinez‐Gonzalez D, Martinez‐Alonso M, et al. Psychometric validation of the cardiff wound impact schedule questionnaire in a Spanish population with diabetic foot ulcer. J Clin Med. 2021;10(17):4023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Da Cruz D, Oliveira‐Pinto J, Mansilha A. The role of hyperbaric oxygen therapy in the treatment of diabetic foot ulcers: a systematic review with meta‐analysis of randomized controlled trials on limb amputation and ulcer healing. Int Angiol. 2022;41(1):63‐73. [DOI] [PubMed] [Google Scholar]
- 41. Mineoka Y, Ishii M, Hashimoto Y, et al. Nutritional status assessed with objective data assessment correlates with a high‐risk foot in patients with type 2 diabetes. J Clin Med. 2022;11(5):1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Stotl I, Blagus R, Urbancic‐Rovan V. Individualised screening of diabetic foot: creation of a prediction model based on penalised regression and assessment of theoretical efficacy. Diabetologia. 2022;65(2):291‐300. [DOI] [PubMed] [Google Scholar]
- 43. Malone M, Erasmus A, Schwarzer S, Lau NS, Ahmad M, Dickson HG. Utilisation of the 2019 IWGDF diabetic foot infection guidelines to benchmark practice and improve the delivery of care in persons with diabetic foot infections. J Foot Ankle Res. 2021;14(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pouget C, Dunyach‐Remy C, Pantel A, Schuldiner S, Sotto A, Lavigne JP. Biofilms in diabetic foot ulcers: significance and clinical relevance. Microorganisms. 2020;8(10):1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Eriksson E, Liu PY, Schultz GS, et al. Chronic wounds: treatment consensus. Wound Repair Regen. 2022;30(2):156‐171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dixon D, Edmonds M. Managing diabetic foot ulcers: pharmacotherapy for wound healing. Drugs. 2021;81(1):29‐56. [DOI] [PubMed] [Google Scholar]
- 47. Chen Y, Kuang XC, Zhou J, et al. Proximal tibial cortex transverse distraction facilitating healing and limb salvage in severe and recalcitrant diabetic foot ulcers. Clin Orthop Relat Res. 2020;478(4):836‐851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yuan YS, Ding XF, Jing ZW, et al. Modified tibial transverse transport technique for the treatment of ischemic diabetic foot ulcer in patients with type 2 diabetes. J Orthopaed Transl. 2021;29:100‐105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bus SA, Armstrong DG, Gooday C, et al. Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3274. [DOI] [PubMed] [Google Scholar]
- 50. Lavery LA, Niederauer MQ, Papas KK, Armstrong DG. Does debridement improve clinical outcomes in people with diabetic foot ulcers treated with continuous diffusion of oxygen. Wounds Compend Clin Res Pract. 2019;31(10):246‐251. [PubMed] [Google Scholar]
- 51. Yang JX, Zeng WN, Xu P, et al. Glucose‐responsive multifunctional metal‐organic drug‐loaded hydrogel for diabetic wound healing. Acta Biomater. 2022;140:206‐218. [DOI] [PubMed] [Google Scholar]
- 52. Anand S, Rajinikanth PS, Arya DK, et al. Multifunctional biomimetic nanofibrous scaffold loaded with asiaticoside for rapid diabetic wound healing. Pharmaceutics. 2022;14(2):273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Alven S, Peter S, Mbese Z, Aderibigbe BA. Polymer‐based wound dressing materials loaded with bioactive agents: potential materials for the treatment of diabetic wounds. Polymers. 2022;14(4):724e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Glover K, Stratakos AC, Varadi A, Lamprou DA. 3D scaffolds in the treatment of diabetic foot ulcers: new trends vs conventional approaches. Int J Pharm. 2021;599:120423. [DOI] [PubMed] [Google Scholar]
- 55. Augustine R, Hasan A, Dalvi YB, et al. Growth factor loaded in situ photocrosslinkable poly(3‐hydroxybutyrate‐co‐3‐hydroxyvalerate)/gelatin methacryloyl hybrid patch for diabetic wound healing. Mater Sci Eng C Mater Biol Appl. 2021;118:111519. [DOI] [PubMed] [Google Scholar]
- 56. Lopes L, Setia O, Aurshina A, et al. Stem cell therapy for diabetic foot ulcers: a review of preclinical and clinical research. Stem Cell Res Ther. 2018;9(1):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Santarella F, Sridharan R, Marinkovic M, et al. Scaffolds functionalized with matrix from induced pluripotent stem cell fibroblasts for diabetic wound healing. Adv Healthc Mater. 2020;9(16):2000307. [DOI] [PubMed] [Google Scholar]
- 58. Rai V, Moellmer R, Agrawal DK. The role of CXCL8 in chronic nonhealing diabetic foot ulcers and phenotypic changes in fibroblasts: a molecular perspective. Mol Biol Rep. 2022;49(2):1565‐1572. [DOI] [PubMed] [Google Scholar]
- 59. Sakamoto M, Nakano T, Tsuge I, et al. Dried human cultured epidermis accelerates wound healing in diabetic mouse skin defect wounds. Sci Rep. 2022;12(1):3184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tanaka R, Fujimura S, Kado M, et al. Phase I/IIa feasibility trial of autologous quality‐ and quantity‐cultured peripheral blood mononuclear cell therapy for non‐healing extremity ulcers. Stem Cells Transl Med. 2022;11(CHEMIA; DIABETIC FOOT; TOE PRESSURE; BONE‐MARROW:146‐158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Hirase T, Ruff E, Surani S, Ratnani I. Topical application of platelet‐rich plasma for diabetic foot ulcers: a systematic review. World J Diabetes. 2018;9(10):172‐179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ahmad T, McGrath S, Sirafim C, et al. Development of wound healing scaffolds with precisely‐triggered sequential release of therapeutic nanoparticles. Biomater Sci. 2021;9(12):4278‐4288. [DOI] [PubMed] [Google Scholar]
- 63. DeFrates KG, Franco D, Heber‐Katz E, Messersmith PB. Unlocking mammalian regeneration through hypoxia inducible factor one alpha signaling. Biomaterials. 2021;269:120646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Sun Y, Gao Y, Chen J, et al. Evidence mapping of recommendations on diagnosis and therapeutic strategies for diabetes foot: an international review of 22 guidelines. Metab Clin Exp. 2019;100:153956. [DOI] [PubMed] [Google Scholar]
- 65. Aldana PC, Khachemoune A. Diabetic foot ulcers: appraising standard of care and reviewing new trends in management. Am J Clin Dermatol. 2020;21(2):255‐264. [DOI] [PubMed] [Google Scholar]
- 66. Zhang PY, Lu Q, Li HJ, et al. The quality of guidelines for diabetic foot ulcers: a critical appraisal using the AGREE II instrument. PLoS One. 2019;14(9):e0217555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Tan M, Goodall R, Hughes W, Langridge B, Shalhoub J, Davies AH. A methodological assessment of diabetic foot syndrome clinical practice guidelines. Eur J Vasc Endovasc Surg. 2020;60(2):274‐281. [DOI] [PubMed] [Google Scholar]
- 68. Bus SA, van Netten JJ, Lavery LA, et al. IWGDF guidance on the prevention of foot ulcers in at‐risk patients with diabetes. Diabetes Metab Res Rev. 2016;32(Suppl 1):16‐24. [DOI] [PubMed] [Google Scholar]
- 69. Bus SA, Armstrong DG, van Deursen RW, Lewis JE, Caravaggi CF, Cavanagh PR. IWGDF guidance on footwear and offloading interventions to prevent and heal foot ulcers in patients with diabetes. Diabetes Metab Res Rev. 2016;32(Suppl 1):25‐36. [DOI] [PubMed] [Google Scholar]
- 70. Lipsky BA, Aragon‐Sanchez J, Diggle M, et al. IWGDF guidance on the diagnosis and management of foot infections in persons with diabetes. Diabetes Metab Res Rev. 2016;32:45‐74. [DOI] [PubMed] [Google Scholar]
- 71. Hinchliffe RJ, Brownrigg JR, Apelqvist J, et al. IWGDF guidance on the diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers in diabetes. Diab Metab Res Rev. 2016;32(Suppl 1):37‐44. [DOI] [PubMed] [Google Scholar]
- 72. Wang AP, Lv GZ, Cheng XB, et al. Guidelines on multidisciplinary approaches for the prevention and management of diabetic foot disease (2020 edition). Burns Trauma. 2020;8:tkaa017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ahmed MU, Tannous WK, Agho KE, Henshaw F, Turner D, Simmons D. Prevalence and burden of diabetes‐related foot disease in New South Wales, Australia: evidence from the 45 and up study survey data linked with health services data. Int J Environ Res Publ Health. 2021;18(21):11528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ahmed MU, Tannous WK, Agho KE, Henshaw F, Turner D, Simmons D. Social determinants of diabetes‐related foot disease among older adults in New South Wales, Australia: evidence from a population‐based study. J Foot Ankle Res. 2021;14(1):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Galal YS, Khairy WA, Taha AA, Amin TT. Predictors of foot ulcers among diabetic patients at a tertiary care center, Egypt. Risk Manag Healthc Policy. 2021;14:3817‐3827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ha JH, Jin H, Park JU. Association between socioeconomic position and diabetic foot ulcer outcomes: a population‐based cohort study in South Korea. BMC Public Health. 2021;21(1):1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Hulshof CM, van Netten JJ, Pijnappels M, Bus SA. The role of foot‐loading factors and their associations with ulcer development and ulcer healing in people with diabetes: a systematic review. J Clin Med. 2020;9(11):3591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Tolossa T, Mengist B, Mulisa D, Fetensa G, Turi E, Abajobir A. Prevalence and associated factors of foot ulcer among diabetic patients in Ethiopia: a systematic review and meta‐analysis. BMC Public Health. 2020;20(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ponirakis G, Elhadd T, Chinnaiyan S, et al. Prevalence and risk factors for diabetic neuropathy and painful diabetic neuropathy in primary and secondary healthcare in Qatar. J Diabetes Investig. 2021;12(4):592‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Bondar A, Popa AR, Papanas N, et al. Diabetic neuropathy: a narrative review of risk factors, classification, screening and current pathogenic treatment options (Review). Exp Ther Med. 2021;22(1):690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Yu YC. Gold standard for diagnosis of DPN. Front Endocrinol. 2021;12:719356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Caselli A, Pham H, Giurini JM, Armstrong DG, Veves A. The forefoot‐to‐rearfoot plantar pressure ratio is increased in severe diabetic neuropathy and can predict foot ulceration. Diabetes Care. 2002;25(6):1066‐1071. [DOI] [PubMed] [Google Scholar]
- 83. Allan D, Chatzistergos PE, Mahadevan S, et al. Increased exposure to loading is associated with decreased plantar soft tissue hardness in people with diabetes and neuropathy. Diabetes Res Clin Pract. 2022;187:109865. [DOI] [PubMed] [Google Scholar]
- 84. Ren WY, Duan YJ, Jan YK, et al. Effect of exercise volume on plantar microcirculation and tissue hardness in people with type 2 diabetes. Front Bioeng Biotechnol. 2021;9:732628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Thorne CS, Gatt A, DeRaffaele C, Bazena A, Formosa C. Digital foot health technology and diabetic foot monitoring: a systematic review. Diabetes Res Clin Pract. 2021;175:108783. [DOI] [PubMed] [Google Scholar]
- 86. Moulaei K, Malek M, Sheikhtaheri A. A smart wearable device for monitoring and self‐management of diabetic foot: a proof of concept study. Int J Med Inform. 2021;146:104343. [DOI] [PubMed] [Google Scholar]
- 87. Chatzistergos PE, Chockalingam N. A novel concept for low‐cost non‐electronic detection of overloading in the foot during activities of daily living. R Soc Open Sci. 2021;8(6):202035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Doğruel H, Aydemir M, Balci MK. Management of diabetic foot ulcers and the challenging points: an endocrine view. World J Diabetes. 2022;13(1):27‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Bus SA, Lavery LA, Monteiro‐Soares M, et al. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3269. [DOI] [PubMed] [Google Scholar]
- 90. Ruemenapf G, Morbach S, Sigl M. Therapeutic alternatives in diabetic foot patients without an option for revascularization: a narrative review. J Clin Med. 2022;11(8):2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Hussain MA, Al‐Omran M, Salata K, et al. Population‐based secular trends in lower‐extremity amputation for diabetes and peripheral artery disease. CMAJ. 2019;191(35):E955‐E961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Bernatchez J, Mayo A, Kayssi A. The epidemiology of lower extremity amputations, strategies for amputation prevention, and the importance of patient‐centered care. Semin Vasc Surg. 2021;34(CHEMIA):54‐58. [DOI] [PubMed] [Google Scholar]
- 93. Wukich DK, Hobizal KB, Raspovic KM, Rosario BL. SIRS is valid in discriminating between severe and moderate diabetic foot infections. Diabetes Care. 2013;36(11):3706‐3711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Lavery LA, Ryan EC, Ahn J, et al. The infected diabetic foot: re‐evaluating the Infectious Diseases Society of America diabetic foot infection classification. Clin Infect Dis. 2020;70(8):1573‐1579. [DOI] [PubMed] [Google Scholar]
- 95. Saeed K, Esposito S, Akram A, et al. Hot topics in diabetic foot infection. Int J Antimicrob Agents. 2020;55(6):105942. [DOI] [PubMed] [Google Scholar]
- 96. Macdonald KE, Boeckh S, Stacey HJ, Jones JD. The microbiology of diabetic foot infections: a meta‐analysis. BMC Infect Dis. 2021;21(1):770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Hawkins BK, Barnard M, Barber KE, et al. Diabetic foot infections: a microbiologic review. Foot (Edinb). 2022;51:101877. [DOI] [PubMed] [Google Scholar]
- 98. Uckay I, Berli M, Sendi P, Lipsky BA. Principles and practice of antibiotic stewardship in the management of diabetic foot infections. Curr Opin Infect Dis. 2019;32(2):95‐101. [DOI] [PubMed] [Google Scholar]
- 99. Rotman SG, Thompson K, Grijpma DW, et al. Development of bone seeker‐functionalised microspheres as a targeted local antibiotic delivery system for bone infections. J Orthop Transl. 2020;21:136‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Maurer SM, Hepp ZS, McCallin S, et al. Short and oral antimicrobial therapy for diabetic foot infection: a narrative review of current knowledge. J Bone Jt Infect. 2022;7(2):61‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Barbosa W, Prado T, Batista C, et al. Electric vehicles: bibliometric analysis of the current state of the art and perspectives. Energies. 2022;15(2):395. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data derived from public domain resources. [Web of Science (https://www.webofscience.com/); Scimago Journal & Country Rank (https://www.scimagojr.com/journalrank.php)].


