Abstract
Aim of our study was to report unusual presentation of mucormycosis in patients, who were recovered from COVID-19 infection. This was a prospective observational study, undertaken at Ravindra Nath Tagore Medical College, Udaipur, India, over a period of last 3 months (April-June 2021). All patients with maxillofacial and dental mucormycosis were included in the study. All patients either have COVID-19 infection or recovered from it. Eight (40%) patients had history of use of corticosteroids for COVID1-19 infection, fifteen patients had either known case of diabetes or newly diagnosed diabetes with uncontrolled blood sugar at the time of presentation, three (15%) patients were in pre-diabetic state with HbA1c between 6.0 and 6.5% and two patients had no diabetes. None of patients had diabetic ketoacidosis and only one patient reported complete loss of vision with dental symptoms. There was unusual presentation of mucormycosis in form of loosening of teeth in uncontrolled diabetes. Injudicious use of steroids and uncontrolled diabetes are two main risk factors, so eyes should be kept on both of these.
Keywords: COVID-19, Maxillofacial, Mucormycosis, Uncontrolled diabetes, Unusual
We know mucormycosis have been declared notifiable disease in eleven states of India. Fungi which are responsible for Mucormycosis belong to the order Mucorales like Rhizopus, Mucor, Rhizomucor, Cunninghamella and Absidia. The most common species isolated was Rhizopus species, with an overall mortality of 46% [1]. India has high prevalence of mucormycosis approximately 0.14 cases per 1000 population, which is 80 times more than developed countries [2]. In covid-19 infection immunity of patients is severely compromised due to use of corticosteroids. Uncontrolled diabetes is commonly associated with covid-19 infection and predisposes to individual for mucormycosis. Diabetes mellitus is most common risk factor for development of mucormycosis [3]. Rhino cerebral form of mucormycosis is most common presentation in diabetes but in covid-19 infected patients, pain and loosening of tooth is now most common presenting symptom along with facial and eye swelling. There is limited literature available on mucormycosis in covid-19 patients. Here, we want to report our 20 cases of maxillofacial and dental mucormycosis, which were presented to our institute with chief complaints of teeth ache and loosening of teeth with facial numbness. Mucormycosis has high mortality, so prompt diagnosis and treatment with a team work of physician, ophthalmologist, otorhinolaryngologist, neurosurgeon, maxillofacial surgeon and microbiologist is needed. Despite best medical and surgical management, fatality rate of mucormycosis is very high [4].
Materials and Methods
Informed written consent was taken from all the patients. This was a prospective observational study, undertaken at Ravindra Nath Tagore Medical College, Udaipur, India, over a period of last 3 months (April-June 2021). Ethical clearance was taken from the ethical committee of the institute. All patients with maxillofacial and dental mucormycosis were included in the study. All patients either have COVID-19 infection or recovered from it. There was organization of a committee by the institute, which includes general physician, general surgeon, otorhinolaryngologist, ophthalmologist, maxillofacial surgeon, neurosurgeon, neuro-physician, endocrinologist and microbiologist, for prompt diagnosis and management. Mucormycosis have been declared as notifiable disease in Rajasthan along with eleven states of India. We followed guidelines of Indian Council of Medical Research (ICMR) for management of mucormycosis.
First diagnosis of mucormycosis was done on basis of Magnetic Resonance Imaging (MRI) (Fig. 1). Cone beam computed tomography of maxilla (Fig. 2) done to know the extension of disease along with any bony erosion. Microbiological diagnosis was done by potassium hydroxide (KOH) wet mount of tissue obtained from gums and palate (Fig. 3) with scrapping during oral cavity examination. Data in form of presentation details of patients, comorbities or risk factor, imaging, diagnostic nasal endoscopy findings and management details were recorded and analyzed (Table 1). All patients had undergone surgical debridement and tissue sent for KOH mount, fungal culture and histopathological examination (Table 2). Post-operative cleaning was done every 5th day for 45 days and patients were discharged after three consecutive cleaning becomes negative for KOH mount and on examination healthy tissue was seen.
Fig. 1.
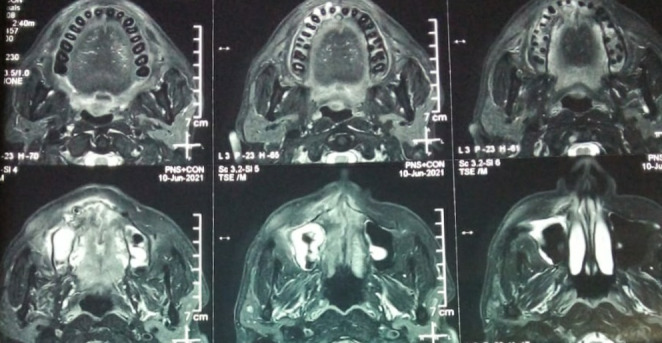
T2W Magnetic resonance imaging showing involvement of right maxillary sinus and maxillary alveolus
Fig. 2.
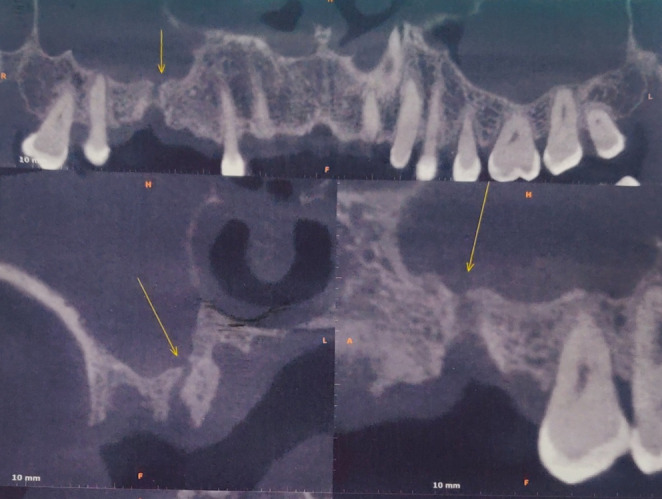
Cone beam computed tomography showing erosion of right maxillary alveolus
Fig. 3.

Formation of pustules seen over right maxillary alveolus
Table 1.
Clinical presentation, risk factor and association with COVID 19 infection
MRI = Magnetic resonance imaging, KOH = potassium hydroxide, U/L = Unilateral. B/L = Bilateral
| Case No. |
Age/ Sex |
Dental symptom at presentation | Risk factor | COVID status at presentation | |
|---|---|---|---|---|---|
| U/L | B/L | ||||
| 1 | 46Y/M | - | B/L loosening of teeth | Newly diagnosed diabetes mellitus HbA1c 9.3% | Recovered |
| 2 | 42Y/M | Pain and loosening in right upper teeth | - | Prediabetic state HbA1c 6.2% |
No history of COVID-19 infection. Brother had history of covid-19 infection and hospitalization |
| 3 | 43Y/M | - | Loosening of teeth on right side and pain on left side | Diabetes mellitus since last 2 year | Recovered |
| 4 | 35Y/M | Loosening and pain in left upper teeth | - |
Diabetes mellitus since last 2 year HbA1c 12.3%, prolonged corticosteroid use(> 2week) |
Recovered |
| 5 | 50Y/F | Bilateral loosening of teeth with right side facial pain | - | Diabetes from last 16 years, HbA1c 13.35% | recovered |
| 6. | 45Y/M | Right side facial and dental pain | - | Newly diagnosed diabetes mellitus, HbA1c 9.0% | recovered |
| 7 | 60Y/M | Right side facial and dental pain with pus draining sinuses over gingiva | - | Diabetes mellitus from last 12–13 year, HbA1c 10.80% | recovered |
| 8 | 52Y/M | Left sided loosening of teeth | - | Pre-diabetic state HbA1c 6.4% use of corticosteroids for 1 week | recovered |
| 9 | 40Y/M | - | B/L dental pain |
Diabetes from last 2 year, HbA1c 7.5% Use of corticosteroids > 2week |
recovered |
| 10 | 67Y/M | Dental pain on left side | - |
Use of corticosteroids > 2 week No diabetes |
recovered |
| 11 | 31Y/M | Multiple pus draining sinuses over upper gingiva on right side | - | Newly diagnosed diabetes mellitus, HbA1c 11.4% | recovered |
| 12 | 53Y/M | - | B/L Dental pain with Right side facial swelling |
Diabetes mellitus from 20 years Hospitalization for Covid-19 pneumonia > 1 month Corticosteroids use > 2week Oxygen inhalation > 10 days |
recovered |
| 13 | 64 Y/M | Right facial and dental pain with facial swelling | - |
Prolonged corticosteroids use > 2 week Prediabetic state, blood glucose level normal, HbA1c 6.5% |
recovered |
| 14 | 34Y/M | Loosening of upper teeth on left side | - | Newly diagnosed diabetes, 11.1% | recovered |
| 15 | 35Y/F | Right facial and dental pain with facial swelling | - |
Use of corticosteroids for 1 week No diabetes mellitus |
recovered |
| 16 | 40Y/F | Right side facial pain, dental pain with decreased vision | - |
Newly diagnosed diabetes, HbA1c Prolonged use of corticosteroids > 2 week |
recovered |
| 17 | 51Y/M | Left side facial and dental pain with facial paresis | - |
Diabetes from 12 years Corticosteroids use > 2 week Oxygen supplementation for 1 week |
recovered |
| 18 | 57Y/M | Right eye complete loss of vison along with facial and dental pain | - | Diabetes mellitus from last 1 year, HbA1c 10.91 | recovered |
| 19 | 40Y/M | - | B/L dental and facial pain | Newly diagnosed diabetes, HbA1c 9.2 | recovered |
| 20 | 40 Y/F | Left side dental and facial pain | - | Diabetes mellitus from 1 year, HbA1c 10.7% | recovered |
Note: Loosening of teeth and dental pain in all mentioned cases was on upper alveolus.
Table 2.
Radiological, Microbiological, histopathological finding, surgical procedure and final outcome of patients V2 = maxillary division of trigeminal nerve, ITF = infratemporal fossa, PPF = pterygopalatine fossa
| Case No. |
Important imaging finding (MRI) | KOH Mount | Tissue biopsy | Fungal culture | Surgical procedure | Outcome |
|---|---|---|---|---|---|---|
| 1 | Right cheek, hard palate | Aseptate fungal hyphae seen | Suggestive of mucormycosis | Rhizopus grown on culture | Right Infrastructure maxillectomy and left upper alveolectomy | Discharged |
| 2 | Erosion of floor of right maxillary sinus & perialveloar fluid collection at para median aspect | Septate and aseptate both fungal hyphae seen | Suggestive of mucormycosis and aspergillus both | Rhizopus grown on culture | Right upper alveolectomy | Discharged |
| 3 | B/L cheeks, Right hard palate, and bilateral sphenoid | Broad aseptate fungal hyphae seen |
Suggestive of mucormycosis Angioinvasion seen |
Rhizopus grown | Right Infrastructure Maxillectomy, Left Caldwell luc with B/L clearance of sphenoid sinuses | Discharged |
| 4 | Left maxillary sinus, left cheek, left inferior rectus muscle, left alveolus with right maxillary sinus involvement | Broad aseptate fungal hyphae seen |
Suggestive of mucormycosis Angioinvasion seen |
Rhizopus grown on culture | Left total maxillectomy with removal of coronoid process of mandible and right Caldwell luc with clearance of maxillary sinus | Discharged |
| 5 | Bilateral disease with right side hard palate, orbital floor | Broad aseptate fungal hyphae seen |
Suggestive of mucormycosis Angioinvasion seen |
Rhizopus grown on culture | Right total maxillectomy with clearance up to maxillary division of trigeminal and anterior skull base with clearance of bilateral sphenoid sinuses with left upper alveolectomy | Deceased |
| 6 | Right cheek with loosening of tooth | Broad aseptate fungal hyphae seen |
Suggestive of mucormycosis Angioinvasion seen |
Rhizopus grown on culture | Right open antrostomy with removal of canine and incisor teeth | Discharged |
| 7 | Involvement of right cheek, hard palate, orbital floor with left maxillary sinus | Broad aseptate fungal hyphae seen |
Suggestive of mucormycosis Angioinvasion seen |
Rhizopus grown on culture | Right total maxillectomy with left side Caldwell luc and extraction of two molar tooth | Discharged |
| 8 | Erosion of left para median aspect of hard palate, floor of left maxillary sinus | Broad aseptate fungal hyphae seen |
Suggestive of mucormycosis Angioinvasion seen |
Rhizopus grown on culture | Left upper alveolectomy | Discharged |
| 9 | Erosion of alveolar process of left maxilla | Broad aseptate fungal hyphae seen | Suggestive of mucormycosis | Rhizopus grown on culture | Left open antrostomy with upper alveolectomy and removal of one canine one incisor tooth | Discharged |
| 10 | Erosion of left side hard palate and floor of maxillary sinus | Broad aseptate fungal hyphae seen | Suggestive of mucormycosis | Rhizopus grown on culture | Left upper alveolectomy | Discharged |
| 11 | Involvement of Right side PPF ,ITF, pterygo maxillary fissure, hard palate with erosion of floor of maxillary sinus and alveolar process of maxilla | Broad aseptate fungal hyphae seen | Suggestive of mucormycosis | Rhizopus grown on culture | Right infrastructure maxillectomy with clearance of PPF, ITF | Discharged |
| 12 | Erosion of anterior wall and floor of left maxillary sinus, maxillary alveolus, hard palate is seen with preseptal & perialveolar collection seen with adjacent edematous change on left side | Broad aseptate fungal hyphae seen | Suggestive of mucormycosis | Rhizopus grown on culture | left infrastructure maxillectomy with right upper alveolectomy | Discharged |
| 13 | Involvement of right maxillary sinus, right cheek | No fungal hyphae seen | Acute suppuration on nonspecific chronic granulomatous inflammation | No fungus grown on culture | Right open antrostomy with clearance of floor of maxillary sinus | Discharged |
| 14 | Erosion of floor of left maxillary sinus | Broad aseptate fungal hyphae seen | Suggestive of mucormycosis | Rhizopus grown on culture | Left infrastructure maxillectomy | Discharged |
| 15 | Involvement of right cheek, maxillary sinus and perialveolar fluid collection | Broad aseptate fungal hyphae seen |
-Suggestive of mucormycosis -Tuft of fungal hyphae seen |
Rhizopus grown on culture | Right infrastructure maxillectomy | Discharged |
| 16 | Involvement of all sinuses on right side with extension of disease in ITF, retro antral fat and cheek | Aseptate fungal hyphae seen |
-Suggestive of mucormycosis -Tuft of aseptate fungal hyphae seen -Angioinvasion present |
Rhizopus grown on culture | Right total maxillectomy with clearance of ITF, Pterygoid ridge, V2 and endoscopic clearance of ethmoid and sphenoid sinus. | Discharged |
| 17 | Erosion of anterior and posterolateral wall of left maxillary sinus with erosion of adjacent left maxillary alveolus with loculated perialveolar collection | Aseptate fungal hyphae seen |
-Suggestive of mucormycosis -Tuft of aseptate fungal hyphae seen -Angioinvasion present |
Rhizopus grown on culture | Left total maxillectomy with clearance of ITF | Discharged |
| 18 | Involvement of right maxillary, sphenoid, ethmoid and frontal sinus hard palate, masticator space, retro antral fat with disease extension up to orbital apex | Aseptate fungal hyphae seen |
-Suggestive of mucormycosis -Tuft of aseptate fungal hyphae seen -Angioinvasion present |
Rhizopus grown on culture | Right total maxillectomy with orbital exenteration with clearance of ITF, pterygoid ridge, maxillary division of trigeminal nerve and endoscopic clearance of ethmoid, sphenoid and frontal sinus | Discharged |
| 19 | Involvement of B/L maxillary sinus with right nasal cavity, hard palate | Aseptate fungal hyphae seen |
-Suggestive of mucormycosis -Tuft of fungal hyphae seen |
Rhizopus grown on culture |
-Left infrastructure maxillectomy -Right upper alveolectomy |
Discharged |
| 20 | Involvement of left cheek, retro antral fat, masticator space and erosion of floor of left maxillary sinus | Broad aseptate fungal hyphae seen |
-Suggestive of mucormycosis seen -Angioinvasion present |
Rhizopus grown on culture | Left total maxillectomy with ITF clearance | Discharged |
Results
There was total 20 patients in our study among them 16 were male and 4 were female. Average age was 41.65 year. In our study all patients had history of COVID 19- infection. In our study, nineteen patients were confirmed cases of mucormycosis with microbiological (KOH mount & fungal culture) and histopathological finding. Eight (40%) patients had taken corticosteroids for COVID1-19 infection. Fifteen (75%) patients had either known case of diabetes or newly diagnosed diabetes with uncontrolled blood sugar at the time of presentation. Three (15%) patients were in pre-diabetic state with HbA1c between 6.0 and 6.5% and two patients had no diabetes. There was bilateral disease in five (25%) patients. Maxillary sinus involvement was present in all cases. None of patients had diabetic ketoacidosis. Two patients had history of oxygen inhalation. One patient had hospitalization of more than one month with oxygen inhalation for more than 15 days. In our study only one patient had complete loss of vison with extensive disease into infratemporal fossa, pterygoid ridge and up to maxillary division of trigeminal nerve. One patient was died on same postoperative day and rest all patients were discharged for home.
Discussion
T-cell count alteration in COVID-19 infection is associated with pathogenesis of fungal infection. Early diagnosis and antifungal therapy along with surgical debridement have crucial role in decreasing mortality and to prevent damage of the affected part.
COVID-19 management includes use of steroids, monoclonal antibody and broad spectrum antibiotics, due to which there is high chances of new onset fungal infection [5]. There is extensive pulmonary disease and subsequent alveolo‑interstitial pathology in COVID-19 infection, which itself predispose to invasive fungal infection of the airways including sinuses and lungs [5, 6]. Most commonly mucormycosis is caused by 2 orders Mucorales and Entomophthorales. There are 4 genera within the Mucorales which have been mostly equated with disease in humans, are Rhizopus, Mucor, Absidia, and Cunninghamella. Conidiobolus and Basidiobolus (Entomophthorales) genera are clinically and genetically distinct from the Mucorales. In invasive fungal infection, mucormycosis is on third position after candidiasis and aspergillosis. Rhizopus is most frequently associated with mucormycosis with overall 46% mortality [7, 8]. Maxillofacial or rhino maxillary mucormycosis begins with inhalation of the fungus by an immunocompromised individual [9]. There is only few reported rhino-ocular-cerebral mucormycosis associated with COVID-19 infection [5, 10, 11]. One study of odontogenic mucormycosis was described by Saidha PK et al. [12] with six histo-pathologically proven cases and association with poorly controlled diabetes. In our study all patients had dental symptoms in form of loosening teeth or pain in upper teeth. Only 40% had history of use of corticosteroids and 10% had history of oxygen inhalation. So we can say there was no use of immunosuppressants in 60% patients and none of patient had diabetic ketoacidosis and only 10% had history of oxygen inhalation then what is the proposed mechanism of pathogenesis which induces mucormycosis in these COVID-19 recovered patients. Main limitation of our study was less number of patients.
Learning and Unanswered Points
Second wave of COVID-19 infection was associated with sudden rise of mucormycosis all over in India.
As we studied that only 40% patients had history of use of corticosteroids, none of patient had diabetic ketoacidosis and only in two patients, history of oxygen inhalation was present than what was the inciting factor for mucormycosis in these COVID 19 recovered patients.
Is the delta variant of COVID-19 infection is responsible for this dangerous addition of mucormycosis in this pandemic?
Why first wave of COVID-19 infection was not associated with mucormycosis?
Why odontogenic mucormycosis only affects maxillary sinus.
Why there is orbital involvement in odontogenic mucormycosis( only in one patient had loss of vision).
Conclusion
We had observed unusual presentation of mucormycosis in form of loosening of teeth, in uncontrolled diabetes and newly diagnosed diabetes. In all of these cases had rapidly developing fungal infection with history of covid-19 infection. Injudicious use of steroids and uncontrolled diabetes are two main risk factors, which makes patient vulnerable for the disease, so eyes should be kept on both of these.
Author Contribution
Navneet Prasad Mathur was the main surgeon in our study. First draft of the manuscript was written by Manju Silu and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Not applicable.
Data Availability
Data of this study is original and not copied from any other source available. This is an original research done in a premier government institute. Data of this study has not been submitted anywhere else in the past for the purpose of publication. The data used to support the findings of this study are included within the article.
Code Availability
Not applicable.
Declarations
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Ethical Statement
Here we are declaring that laws which are applicable to our article are followed. Ethical committee approval was taken before commencing this study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Navneet Prasad Mathur, Email: entrnt11@gmail.com.
Manju Silu, Email: manjusilu35@gmail.com.
References
- 1.Jeong W, Keighley C, Wolfe R et al (2019) The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect 25:26–34. 10.1016/j.cmi.2018.07.011 [DOI] [PubMed]
- 2.Skiada A, Pavleas I, Drogari-Apiranthitou M. Epidemiology and diagnosis of mucormycosis: an update. J Fungi. 2020;6:265. doi: 10.3390/jof6040265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prakash H, Chakrabarti A. Global epidemiology of mucormycosis. J Fungi. 2019;5:26. doi: 10.3390/jof5010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ballester DG, González-García R, García CM, Ruiz-Laza L, Gil FM. Mucormycosis of the head and neck: report of five cases with different presentations. J Craniomaxillofac Surg. 2012;40:584–591. doi: 10.1016/j.jcms.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 5.Mehta S, Pandey A. Rhino–orbital mucormycosis associated with COVID–19. Cureus. 2020;12:e10726. doi: 10.7759/cureus.10726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gangneux JP, Bougnoux ME, Dannaoui E, Cornet M, Zahar JR. Invasive fungal diseases during COVID–19: we should be prepared. J Mycol Med. 2020;30:100971. doi: 10.1016/j.mycmed.2020.100971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bouza E, Munoz P, Guinea J. Mucormycosis: an emerging˜ disease? Clin Microbiol Infect. 2006;12(7):7–236. doi: 10.1111/j.1469-0691.2006.01604. [DOI] [Google Scholar]
- 8.Jeong W, Keighley C, Wolfe R, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25:26–34. doi: 10.1016/j.cmi.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Greenberg MS. Ulcerative vesicular and bullous lesions. In: Greenberg MS, Glick M, editors. Burket’s oral medicine diagnosis and treatment. Amsterdam: Elsevier; 2003. [Google Scholar]
- 10.Mekonnen ZK, Ashraf DC, Jankowski T, et al. Acute invasive rhino-orbital mucormycosis in a patient with COVID-19-associated acute respiratory distress syndrome. Ophthalmic Plast Reconstr Surg. 2021;37:40–80. doi: 10.1097/IOP.0000000000001889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Werthman-Ehrenreich A (2021) Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am J Emerg Med 42. 264.e5–264.e8 [DOI] [PMC free article] [PubMed]
- 12.Saidha PK, Kapoor S, Das P, et al. Mucormycosis of Paranasal Sinuses of Odontogenic Origin Post COVID19 infection: a Case Series. Indian J of Otolaryngol and Head and Neck Surg http//doi. 2021 doi: 10.1007/s12070-021-02638-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data of this study is original and not copied from any other source available. This is an original research done in a premier government institute. Data of this study has not been submitted anywhere else in the past for the purpose of publication. The data used to support the findings of this study are included within the article.
Not applicable.


