Abstract
Few studies and almost exclusively from the USA have recently investigated mobile phone and computer use among users of psychiatric services, which is of high relevance regarding the increasing development of digital health applications and services.
Objective, design and setting
In a cross-sectional patient survey, we examined (a) rates and purposes of mobile phone, computer, internet and social media use, and (b) the role of social and clinical predictors on rates of utilisation among psychiatric inpatients in Berlin, Germany.
Participants and results
Descriptive analyses showed that among 496 participants, 84.9% owned a mobile phone and 59.3% a smartphone. Among 493 participants, 68.4% used a computer regularly. Multivariate logistic regression models revealed being homeless, diagnosis of a psychotic illness, being of older age and a lower level of education to be significant predictors for not owning a mobile phone, not using a computer regularly or having a social media account, respectively.
Conclusions
Users of psychiatric services may have access to mobile phones and computers, although rates are lower than in the general population. However, key barriers that need to be addressed regarding the development of and engagement with digital health interventions are factors of social exclusion like marginalised housing as well as clinical aspects like psychotic illness.
Keywords: mental health, psychiatry, adult psychiatry
STRENGTHS AND LIMITATIONS OF THIS STUDY.
In this study, a rather large study population has been investigated.
This is one of the first studies in Europe to examine the possession and use of digital devices among users of psychiatric services.
Our study sample included patients living in Berlin with rather lower socioeconomic status. However, the districts included in the present study are generally comparable with other urban areas not only in Germany, but also with other metropolitan areas in Europe or in western countries.
Introduction
Surveys investigating access to technology indicate that of the worldwide population, 79.8% own a smartphone and 47.1% own a computer.1 In western countries like Germany, rates are even higher: 96.7% of German households own a mobile phone,2 3 88.8% use a smartphone and 90.4% have access to a computer, which is necessary to possibly benefit from digital health interventions and keep on with the ongoing process of digitalisation in healthcare. Such interventions can improve treatment processes for patients and healthcare providers, especially in mental health.4 While there is increasing research and development of digital health interventions in people with common mental disorders like anxiety or depression, people with serious mental illness, who often receive inpatient psychiatric treatment, have scarcely been in the focus of research so far.5 6 One reason is the continuing uncertainty about the extent to which people with serious mental illness use mobile phones, smartphones or computers, and which factors influence mobile phone use, especially regarding healthcare interventions. This is important because the implementation of digital interventions for people with serious mental illness could open new forms of care overcoming existing barriers of healthcare services, for example, via an anonymous healthcare supply.7 8 Additionally, an inpatient setting might be a point of care at which patients could be introduced to digital interventions—especially patients who face higher barriers in access to care like people experiencing precarious housing. The role of precarious housing in the use of digital devices and services among people who use inpatient or outpatient psychiatric services is also not well understood.9
Most studies on mobile phone use among people with serious mental illness or users of psychiatric services date back to the time before the fast dissemination of smartphones. More recent studies solely stem from US samples. In a recent study among 249 people with serious mental illness in US clinics, mobile phone use was high with 85%, including 60% using a smartphone.10 Mobile phones were used for messaging by 81%, internet by 52%, email by 47% and apps by 45%.10 People were less likely to use a smartphone if they were older, had a persistent psychotic disorder, received disability income or had lower neurocognitive functioning.10 Another US study among psychiatric outpatients (n=100) with serious mental illness revealed that 85% of participants owned a mobile phone and were using it regularly, but only 37% owned a smartphone.11 In contrast, another recent US study (n=50) showed 94% of psychiatric inpatients owned a smartphone with a data plan, which was comparable with nationally representative samples.12 Participants with psychotic disorders especially expressed difficulty in using a mobile app for mental health purposes.12 Further, people with serious mental illness used their smartphones less frequently for health-related purposes than the general population (27% vs 84%).12
To our knowledge, this is the first study assessing different forms of technology use like mobile phones, computers and social media among users of psychiatric inpatient services in Europe. Furthermore, evidence about specific clinical or social factors influencing the use of smartphones and computers among people using psychiatric services is still scarce but could be relevant for the tailoring of and engagement in digital health interventions. Therefore, we examined (1) the access and use of mobile phones, computers, internet, as well as social media platforms, and (2) clinical and sociodemographic factors as predictors for access and use among users of inpatient psychiatric services in Berlin, Germany—a region comparable with other western urban areas.13
Methods
Study design and participants
The study was part of the ‘WOHIN Project’,14 which is a cross-sectional patient survey designed to investigate the housing situation, psychiatric morbidity and service use among psychiatric inpatients and day-clinic patients treated in the catchment area of the Psychiatric University Hospital Charité at St Hedwig Hospital over 6 months (15 March–15 September 2016). The hospital provides psychiatric treatment for all inhabitants living in the Berlin central districts of Wedding, Tiergarten and Moabit. The hospital offers inpatient treatment for 192 people spread out on three general psychiatric wards and four specialised wards (addiction, depression, geriatric-psychiatry, ‘Soteria’ (treatment of people with early psychosis)) as well as five day-clinics. In the study period, a total number of 1251 patients were admitted (excluding outpatients and readmissions).
Trained interviewers contacted patients as soon as possible after admission. All participants gave written informed consent before participation. Inclusion criteria were being of age and giving informed consent. A monetary incentive (€5) was offered for participation. Over 6 months, 1251 patients were admitted to the hospital. We had no exclusion criteria regarding mental disorder, but patients who could not consent due to their symptoms and patients who did not want to participate. For inclusion, patients had to be admitted as inpatients or day-clinic patients in the set time period.
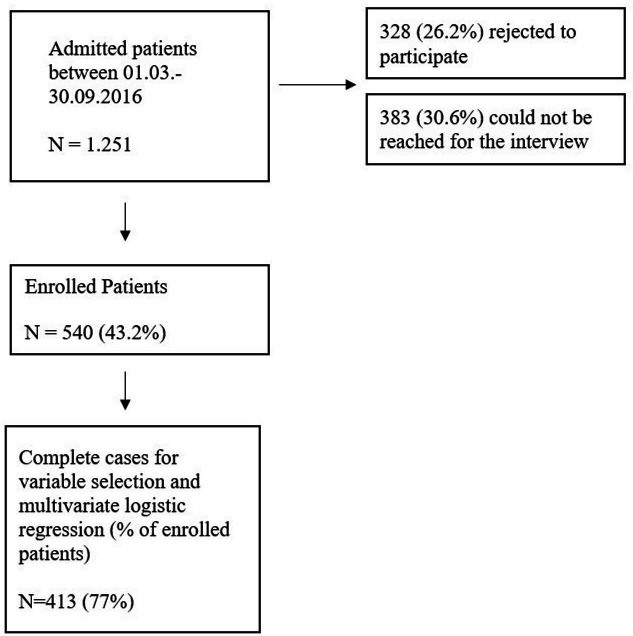
The interview had been evaluated before study start by 10 patients regarding comprehensibility and fitting of outcome measures to patients’ experience and priorities. Items then were adapted accordingly (mainly linguistic changes). In total, 540 participants (43.2%) were willing to participate in the interview, of which 496 gave information about mobile phones, 493 about computer usage and 531 participants gave information about social media accounts (see figure 1). Sociodemographic variables included sex, age, education, housing status and income, and were assessed by a structured interview. Diagnoses of mental disorders were obtained based on discharge records and provided by psychiatric clinicians based on International Statistical Classification of Diseases and Related Health Problems 10 criteria.15 Information about mobile phone, computer, internet and social media use was assessed by questions, which were included in the structured interview but not part of a validated questionnaire (eg, ‘Do you own a smartphone?’, ‘Do you use the computer regularly?’ or ‘Do you have an account on a social media platform?’). Patients were also asked about the purpose and frequency of use. The compilation of the items was based on the expertise of different professional groups and in a short test phase, during which patients evaluated the items regarding comprehensibility and meaningfulness.
Figure 1.
Flow chart of the progress of the cross-sectional study from patient recruitment to selection of complete cases.
Statistical analysis
After descriptive analysis, comparative analyses (Mann-Whitney U test and Χ2 test) were performed to determine whether the relationship between mobile phone or internet use and the considered variables was significant. We performed a multivariate binary logistic regression of sociodemographic factors associated with owning a mobile phone, using a computer regularly or possession of a social media account. After excluding variables missing not at random (salary and social benefits), we conducted a predictor selection for the regression models performed via the least absolute shrinkage and selection operator (LASSO). This predictor selection technique allows for the determination of the importance of predictor variables and thus incorporates the intercorrelation of the predictor variables. Due to a significant proportion of missing data (23,5%), we also conducted a multiple imputation (30 data sets were imputed) without aggregating LASSO results afterwards. In current research, there is no satisfying approach on how to aggregate after multiple imputation for LASSO regression, as the LASSO selects slightly different predictors in every imputed data set and constraints the parameters of all other predictors to zero. Nevertheless, we analysed, if any of the predictors occurred more often in multiple statistical runs after imputation. All tests of significance were based on a p<0.05 level and a CI of 95%. Data were analysed with SPSS version 29.016 and R (R Core Team (2013)).
Patient and public involvement
No patient involved.
Results
Mobile phone use
Among 496 participants, 84.9% (421 of 496) owned a mobile phone and 59.3% (294 of 496) owned a smartphone (table 1). Among participants with a mobile phone, 74.6% (337 of 452) used it to stay in contact with family and friends, only 1.5% (7 of 452) used it for contacting professionals of the support systems. Here, multiple and free-text answers were possible. Among free-text answers, participants mostly reported internet use on their smartphone for consumption of music and movies, work, managing finances, online shopping, job applications and job as well as flat search. Predictor selection in logistic regression revealed that homeless people are 77% less likely to own a mobile phone (OR 0.23, 95% CI (0.12–0.45)), whereas psychosis goes along with a 68% reduced probability of owning a phone (OR 0.32, 95% CI (0.18–0.58)). People of older age are 4% less likely to have a mobile phone (OR 0.96, 95% CI (0.95–0.98); table 2).
Table 1.
Differences in sociodemographic and clinical variables between participants owning a mobile phone, using a computer and having a social media account
| Mobile phone N/mean |
No mobile phone N/mean |
P value | Regular PC use N/mean | No regular PC use N/mean |
P value | Social media account N/mean |
No social media account N/mean |
P value | |
| N=496 (% or SD) | N=493 (% or SD) | N=531 (% or SD) | |||||||
| N | 421 (84.9) | 75 (15.1) | 337 (68.4) | 156 (31.6) | 275 (51.8) | 256 (48.2) | |||
| Male | 244 (62.7) | 47 (62.7) | 0.271 | 195 (58.0) | 94 (60.3) | 0.642 | 154 (56.2) | 153 (59.8) | 0.407 |
| Age (median Q1–Q3) | 40 (30–50) | 46 (33–63) | 0.002 | 38 (30–49) | 48 (36–59) | <0.001 | 37 (28–45) | 49 (37–57) | <0.001 |
| Years of education (median Q1–Q3) |
14 (12–17) | 13 (10–17) | 0.028 | 15 (12–17) | 13 (10–15) | 0.001 | 14 (12–16) | 14 (12–17) | 0.708 |
| Housing status | <0.001 | 0.002 | 0.003 | ||||||
| Own apartment/property | 260 (62.5) | 36 (49.3) | 215 (64.4) | 80 (52.3) | 170 (62.7) | 151 (59.7) | |||
| Sociotherapeutic facilities | 66 (15.9) | 17 (23.3) | 44 (13.2) | 38 (24.8) | 37 (13.7) | 48 (19.0) | |||
| Homeless | 41 (9.9) | 19 (26.0) | 36 (10.8) | 24 (15.7) | 24 (8.9) | 37 (14.6) | |||
| With friends/family | 49 (11.8) | 1 (1.4) | 39 (11.7) | 11 (7.2) | 40 (14.8) | 17 (6.7) | |||
| Income | 0.227 | 0.572 | 0.275 | ||||||
| Salary or pension | 103 (27.1) | 22 (32.4) | 85 (28.7) | 39 (26.2) | 65 (26.7) | 72 (31.3) | |||
| Social benefits | 277 (72.9) | 46 (67.6) | 211 (71.3) | 110 (73.8) | 178 (73.3) | 158 (68.7) | |||
| Official psychosocial support in the last 6 months* | 192 (45.6) | 39 (52.0) | 0.306 | 143 (42.4) | 86 (55.1) | 0.009 | 157 (57.1) | 130 (50.8) | 0.145 |
| Other psychosocial support in the last 6 months† | 196 (46.6) | 33 (44.0) | 0.683 | 161 (47.8) | 66 (42.3) | 0.257 | 149 (54.2) | 141 (55.1) | 0.84 |
| In a relationship or married | 115 (27.6) | 17 (23.3) | 0.439 | 94 (28.2) | 37 (24.2) | 0.351 | 75 (28.1) | 72 (28.5) | 0.926 |
| Psychiatric conditions | |||||||||
| Organic mental disorders | 16 (3.8) | 11 (14.7) | <0.001 | 10 (3.0) | 17 (10.9) | <0.001 | 4 (1.5) | 24 (9.4) | <0.001 |
| Psychosis | 103 (24.5) | 31 (41.3) | 0.002 | 89 (26.4) | 44 (28.2) | 0.676 | 76 (27.6) | 68 (26.6) | 0.781 |
| Any substance dependence | 198 (47.0) | 31 (41.3) | 0.362 | 150 (44.5) | 77 (49.4) | 0.315 | 116 (42.2) | 118 (46.1) | 0.364 |
| Any substance abuse | 88 (20.9) | 8 (10.7) | 0.039 | 69 (20.5) | 27 (17.3) | 0.409 | 54 (19.6) | 44 (17.2) | 0.467 |
| Mood disorders | 133 (31.6) | 17 (22.7) | 0.121 | 111 (32.9) | 38 (24.4) | 0.054 | 96 (34.9) | 77 (30.1) | 0.235 |
| Personality disorders | 93 (22.1) | 6 (8.0) | 0.005 | 69 (20.5) | 29 (18.6) | 0.626 | 65 (23.6) | 37 (14.5) | <0.001 |
| Intellectual disabilities | 9 (2.1) | 4 (5.3) | 0.111 | 7 (2.1) | 6 (3.8) | 0.254 | 4 (1.5) | 9 (3.5) | 0.125 |
Significant p values are presented in bold.
*Guardianship and other forms of psychosocial support, which have to be applied for and are supported by the social code.
†For example, religious helpers, support groups, drug counselling, soup kitchen, etc.
PC, personal computer.
Table 2.
Multivariate binary logistic regression (after variable selection and multiple imputation) of sociodemographic factors associated with owning a mobile phone, using a computer regularly or possession of a social media account
| Mobile phone | P value | PC | P value | Social media account | P value | |
| OR (95% CI) N=540 |
OR (95% CI) N=540 |
OR (95% CI) N=540 |
||||
| Constant | 61.26 (22.57–179.78) | <0.001 | 1.42 (0.54–3.72) | 0.48 | 18.56 (9.31–38.46) | <0.001 |
| Age | 0.96 (0.95–0.98) | <0.001 | 0.95 (0.93–0.96) | <0.001 | 0.92 (0.91–0.94) | <0.001 |
| Education years | 1.19 (1.12–1.27) | <0.001 | ||||
| Housing situation* | ||||||
| Homeless | 0.23 (0.12–0.45) | <0.001 | 0.54 (0.29–0.98) | 0.04 | ||
| With friends/family | ||||||
| Own apartment | 1.73 (1.06–2.83) | 0.03 | ||||
| Official psychosocial support in the last 6 months† | 1.46 (0.92–2.32) | 0.10 | ||||
| Organic mental disorders | 0.38 (0.14–1.03) | 0.05 | ||||
| Psychosis | 0.32 (0.18–0.58) | <0.001 |
Significant p values are presented in bold.
*In reference to own apartment.
†Legal guardianship and other forms of psychosocial support, which have to be applied for and are supported by the social code.
PC, personal computer.
Computer, internet and social media use
Among 493 participants giving information on computer usage, 68.4% (337 of 493) used a computer regularly. Concerning general internet use, 35% (158 of 451) reported use of fewer than 2 hours per week, 16.9% (76 of 451) of 10–19 hours per week and 12.4% (56 of 451) of 2–5 hours; 6.4% (29 of 451) reported internet use of more than 50 hours. Multivariate logistic regression revealed a 73% more likely computer use among people who owned an apartment (OR 1.73, 95% CI (1.06–2.83)). Similarly, being of older age reduced the probability of using a computer by 5% (OR 0.95, 95% CI (0.93–0.96)). Patients with higher education were 19% more likely to use a computer (OR 1.19, 95% CI (1.12–1.27)). Among 531 participants answering the item on having a social media account, 48.2% (256 of 531) did not have an account, 37.7% (200 of 531) had a Facebook account, 3.8% (20 of 531) a Twitter account and 10.4% (55 of 531) others. Multivariate logistic regression revealed that study participants who were homeless were 46% less likely to have a social media account (OR 0.54, 95% CI (0.29–0.98)), and older age was associated with an 8% reduced likelihood of having a social media account (OR 0.92, 95% CI (0.91–0.94); table 2).
Discussion
To our knowledge, this is the first study assessing different forms of technology use like mobile phones, computers and social media among users of psychiatric inpatient services in Europe. Our results reveal that 84.9% (421 of 496) of psychiatric inpatients owned a mobile phone and 59.3% (294 of 496) owned a smartphone, which is lower than rates in the general population at the respective time in Germany (95.1% owned a mobile phone, 74% used a smartphone in 2016).3 17 Our results are comparable with recent studies from the USA investigating samples of users of inpatient and outpatient psychiatric services with serious mental illness with rates of owning a mobile phone between 85% and 94% and owning a smartphone between 37% and 94%.11 12
Furthermore, 68.4% (377 of 493) of participants used a computer regularly, which is also below the rate of computer usage in Germany’s general population of 84%.18 Data on regular computer use among users of psychiatric services are scarce. So far, published studies from the USA report comparable rates: one study among 403 patients with serious mental illness reported a slightly lower computer usage of 53.6%19; a study among 80 inpatients and outpatients with schizophrenia or schizoaffective disorder reported a rate of 54%.20 Comparable studies investigating slightly different subgroups from Europe show similar rates: a study from Finland including 311 inpatients with schizophrenia spectrum disorders reported a computer usage of 55%.21 The only German study investigated the general internet use without specifying the device for internet surfing and found rates of 79.5% internet use among 337 inpatients of a university hospital in an urban city area.22 Compared with the worldwide general population, all studies, either in an outpatient or inpatient setting and from different regions, show a lower frequency of internet use in psychiatric service users, although data from the general population are limited.23
These data illustrate a structural key barrier associated with digital healthcare interventions, for which smartphones and computers are of need. It might also reflect worries about cost, privacy and security concerning the use of digital devices and apps.24 Next to lower rates of mobile phone and computer use, our regression results revealed social and clinical factors like precarious housing (homelessness) and a lower level of education as well psychosis and older age to be significant predictors for not owning a mobile phone, using a computer or having a social media account, respectively.
This is the first study among psychiatric service users identifying precarious housing as a significant predictor for not owning a mobile phone or using a computer. In two of three regression models, homelessness presented as a predictor with the strongest effects. Possible explanations might be economic factors and competing priorities, higher chances of theft and losing one’s phone on the street as well as possible mistrust in technology. Since the healthcare delivery for homeless people still depicts a major healthcare challenge, digital interventions might still be promising in overcoming these struggles.
On this note, it is worth mentioning that among our participants, 68.3% of homeless participants still owned a mobile phone. These results are in line with a range of studies on rates of mobile phone use among people in different forms of precarious housing: one US study found that 94% of the respondents in permanent supportive housing possessed a phone,25 whereas studies among non-sheltered people reported that between 44% and 62% possessed a mobile phone.26 27 So far, studies with digital interventions among homeless people in general only exist with small sample sizes and in the form of pilot studies, and not specifically for homeless people with mental illness, although prevalence among homeless people is high.28 For example, a US study with 35 young homeless people, who were contacted in a homeless shelter network, investigated the feasibility of a digital intervention providing emotional support and coping skills over 1 month and found high rates of engagement and satisfaction.29 Since homeless people often experience no continuity in their care path, reaching people at the point of care of an inpatient setting could be a possibility to address topics of availability, digital health literacy and engagement to support a more continuous healthcare system use after discharge.
Next to precarious housing, a psychotic illness reduced the likeliness of owning a mobile phone about 70% but showed no effect on social media or computer use. A recent US study examined inpatients with serious mental illness and reported that higher age and psychosis were significant predictors for not owning a smartphone.10 Several factors might contribute to a reduced digital affinity in people with psychosis: first, sensory gating in patients with schizophrenia can be impaired, often resulting in a feeling of sensory flooding.30 Furthermore, psychotic symptoms themselves, as well as social isolation and economic factors, are also discussed to play a role.31 32 Here, future research is needed to understand if digital interventions can improve treatment processes and outcomes and if the provision of mobile devices and data plans as well as promotion of digital health literacy can lead to higher engagement in digital mental healthcare, since people with psychotic disorders are still confronted with a high burden of unmet needs. This development is also picked up by pharmaceutical companies like Boehringer Ingelheim, which announced developing a digital therapeutic to aid the treatment of schizophrenia in cooperation with Click Therapeutics.33 Interestingly, we found homelessness as well as psychosis to be significant predictors independently for not owning a mobile phone, although a psychotic illness itself increases the likelihood of becoming homeless. One might argue that both factors might contribute to a decreased chance of owning a mobile phone, especially if occurring together.
Higher education turned out to be a significant predictor for using a computer, with no significant effect on mobile or social media use. This is comparable with one small US study among 28 psychiatric outpatients who used cocaine showing lower education to be associated with less computer use.34 Although a significant predictor in all three of our regression models, older age resulted in small effects. Two other studies also reported less frequent smartphone ownership among patients of higher age: one study examined 403 participants with serious mental illness being treated at mental health centres in the USA, the other study surveyed 1592 people with serious mental illness via a mental health and rehabilitation agency in Chicago.19 32 Older age is often discussed to eventually be associated with reduced digital literacy skills or a higher resistance towards technology,35 resulting in a risk of exclusion from healthcare processes if digitalised. However, the potential of digital devices for healthcare delivery for older adults has been reported numerous times.36 For example, a recent systematic review on telehealth for mental healthcare among older adults found a positive impact of telehealth on depressive symptoms and healthcare utilisation (fewer emergency visits and fewer hospital admissions).37 In addition, educational programmes regarding digital competencies could be beneficial not only for older people,38 but also for people with mental illness or in precarious social situations.
Interestingly, lower rates regarding the use of social media platforms were also revealed among our participants: other studies among 403 and 70 participants in the USA reported a social media usage (Facebook) of 67.9% and 71% in especially younger (<50 years) study samples with serious mental illness in community mental health centres in urban areas.19 39 This difference goes along with the number of Facebook users in the general German and US population.40 This is of clinical interest since studies, for example, among people with bipolar disorders using self-help forums, report online social networking as an important factor in coping with their illness mostly benefiting from aspects of ‘disclosure’, ‘friendship’ and ‘online group cohesion’ as main self-help mechanisms.41 Another US study with 1323 members of ‘PatientsLikeMe’, an online research platform for patients with chronic diseases, showed that users reported profiting from learning about their symptoms, or possible treatment options and side effects.42 More than half of the patients reported finding another patient, who helped them understand more about their condition.42
Our study highlights the need to address questions of availability, accessibility and engagement of people in psychiatric treatment with digital tools and interventions. The rise of digital health interventions could increase the ‘digital divide’ and accelerate social inequalities for groups already at risk of social exclusion like people with serious mental illness or experiencing homelessness.43
Limitations
The following limitations should be mentioned. First, our study sample included psychiatric inpatients and day-clinic patients living in districts of Berlin with rather lower socioeconomic status (Tiergarten, Moabit, Wedding). These districts struggle with comparable problems with larger cities in Germany due to partially low living standards and high rates of migrants. Therefore, the generalisability of our findings is limited especially with rural areas. However, the districts included in the present study are generally comparable with other urban areas not only in Germany, but also with other metropolitan areas in Europe or in western countries. Second, existing studies show some methodological differences, limiting its comparability like (a) different study populations (inpatient vs outpatient services, subpopulations like people with serious mental illness), (b) different time points and (c) different assessments/instruments. The present study used specific questions assessing phone or computer possession and use, which were included in the structured interview but not part of a validated questionnaire (eg, ‘Do you own a smartphone?’, ‘Do you use the computer regularly?’ or ‘Do you have an account on a social media platform?’). Therefore, no reliability or validity testing has been conducted. Future research should include standardised questionnaires, for example, the E-Health Literacy Scale44 or Digital Health Literacy Instrument.45 Third, the present study was conducted in 2016. At that time, the ownership and use rates of mobile devices might have been lower than today. For example, smartphone ownership rates in the general population of Germany increased from 74% in 2016 to 88.8% in 2021.3 Thus, results of our study need to be interpreted carefully. Nevertheless, factors associated with a lower use and ownership of mobile devices among psychiatric service users can be considered as still relevant, even more so considering the increasing importance of digital health today. Consequently, more studies investigating the use of digital devices among psychiatric inpatients, especially after the COVID-19 pandemic and the ongoing digitisation, are needed.
Conclusion
The use of technology among users of psychiatric inpatient and day clinic services is clearly lower compared with Germany’s general population and shows that creating structures to guarantee access to technology is a key factor in order not to exclude people from the possible benefit of digital healthcare interventions. Risk factors for lower technology use identified in this study are the clinical aspect of a psychotic illness as well as social factors, especially precarious housing and with only a smaller effect older age. These risk factors should be considered in designing and creating digital healthcare interventions. It is important to detect further barriers in the process of implementing and engaging people with mental health problems with digital health services. Vulnerable subgroups like people struggling with homelessness and mental health problems should not be excluded from processes of digital transformation of the healthcare system.
Supplementary Material
Acknowledgments
We want to thank all patients for their participation and talking freely about their challenges and sharing their experiences. We also want to thank Dr Daniel Schulze for his statistical advice.
Footnotes
Contributors: SS and SG are the authors responsible for the overall content as the guarantors.
SS and SG were responsible for drafting and revising the original study protocol; they were the chief investigators and had overall responsibility for the management of the trial; and they delivered the training to the interviewers. SS and DM wrote the analysis plan and cleaned and analysed the data under the supervision of SG, DF, SL, DS, LK and HK. DM and SS wrote the first draft of the report and revised the subsequent draft. All authors contributed to and approved the final report.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available. No data sharing plan has been included with the trial registry. No additional data available.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and was approved by Charité University Hospital local ethics committee (number: EA1/291/15).
References
- 1. Ericsson mobility visualizer [online]. n.d. Available: https://www.ericsson.com/en/reports-and-papers/mobility-report/mobility-visualizer?f=1&ft=3&r=1&t=8&s=1&u=1&y=2020,2027&c=1
- 2. German Federal Statistical Office . Ausstattung privater haushalte mit informations- und kommunikationstechnik - deutschland. n.d. Available: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Einkommen-Konsum-Lebensbedingungen/Ausstattung-Gebrauchsgueter/Tabellen/liste-infotechnik-d.html;jsessionid=58BEC3B00671E22B6814859EDBB4303F.live741
- 3. Research VB. Anteil der smartphonenutzer*in in deutschlang in den jahren 2012 bis 2021. 2021. Available: https://de.statista.com/statistik/daten/studie/585883/umfrage/anteil-der-smartphone-nutzer-in-deutschland/
- 4. Miralles I, Granell C, Díaz-Sanahuja L, et al. Smartphone apps for the treatment of mental disorders: systematic review. JMIR Mhealth Uhealth 2020;8:e14897. 10.2196/14897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berry N, Lobban F, Emsley R, et al. Acceptability of interventions delivered online and through mobile phones for people who experience severe mental health problems: a systematic review. J Med Internet Res 2016;18:e121. 10.2196/jmir.5250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ernsting C, Dombrowski SU, Oedekoven M, et al. Using smartphones and health apps to change and manage health behaviors: a population-based survey. J Med Internet Res 2017;19:e101. 10.2196/jmir.6838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chan S, Torous J, Hinton L, et al. Psychiatric apps: patient self-assessment, communication, and potential treatment interventions. 2016:217–29.
- 8. Luxton DD, McCann RA, Bush NE, et al. MHealth for mental health: integrating smartphone technology in behavioral healthcare. Profess Psychol: Res Pract 2011;42:505–12. 10.1037/a0024485 [DOI] [Google Scholar]
- 9. Polillo A, Gran-Ruaz S, Sylvestre J, et al. The use of ehealth interventions among persons experiencing homelessness: a systematic review. Digit Health 2021;7:2055207620987066. 10.1177/2055207620987066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Young AS, Cohen AN, Niv N, et al. Mobile phone and smartphone use by people with serious mental illness. Psychiatr Serv 2020;71:280–3. 10.1176/appi.ps.201900203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Glick G, Druss B, Pina J, et al. Use of mobile technology in a community mental health setting. J Telemed Telecare 2016;22:430–5. 10.1177/1357633X15613236 [DOI] [PubMed] [Google Scholar]
- 12. Asuzu K, Rosenthal MZ. Mobile device use among inpatients on a psychiatric unit: a preliminary study. Psychiatry Res 2021;297:S0165-1781(21)00017-2. 10.1016/j.psychres.2021.113720 [DOI] [PubMed] [Google Scholar]
- 13. Federal Institute for Research on Building UA and SD . Metropolitan areas in europe - abstract of a new BBSR study. 2010. Available: https://www.bbsr.bund.de/BBSR/EN/publications/BerichteKompakt/Issues/DL_7_2010.pdf?__blob=publicationFile&v=1
- 14. Schreiter S, Heidrich S, Zulauf J, et al. Housing situation and healthcare for patients in a psychiatric centre in Berlin, Germany: a cross-sectional patient survey. BMJ Open 2019;9:e032576. 10.1136/bmjopen-2019-032576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Graubner B, Auhuber T. ICD-10-GM (internationale statistische klassifikationen der krankheiten und verwandter gesundheitsprobleme). Deutscher Ärzteverlag, 2013. [Google Scholar]
- 16. IBM Corp . Released 2010. IBM SPSS statistics for windows, version 19.0. Armonk, NY: IBM Corp, 2010. [Google Scholar]
- 17. German Federal Statistical . Anteil der privaten haushalte in deutschland mit einem mobiltelefon von 2000 bis 2021. 2021. Available: https://de.statista.com/statistik/daten/studie/198642/umfrage/anteil-der-haushalte-in-deutschland-mit-einem-mobiltelefon-seit-2000/
- 18. German Federal Statistical Office . Anteil der computernutzer* in deutschland von 2004 bis 2017 [online]. 2018. Available: https://de.statista.com/statistik/daten/studie/3102/umfrage/quote-der-computernutzer-in-deutschland-seit-2004/
- 19. Brunette MF, Achtyes E, Pratt S, et al. Use of smartphones, computers and social media among people with SMI: opportunity for intervention. Community Ment Health J 2019;55:973–8. 10.1007/s10597-019-00431-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miller BJ, Stewart A, Schrimsher J, et al. How connected are people with schizophrenia? cell phone, computer, email, and social media use. Psychiatry Res 2015;225:458–63. 10.1016/j.psychres.2014.11.067 [DOI] [PubMed] [Google Scholar]
- 21. Välimäki M, Kuosmanen L, Hätönen H, et al. Connectivity to computers and the Internet among patients with schizophrenia spectrum disorders: a cross-sectional study. Neuropsychiatr Dis Treat 2017;13:1201–9. 10.2147/NDT.S130818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kalckreuth S, Trefflich F, Rummel-Kluge C. Mental health related Internet use among psychiatric patients: a cross-sectional analysis. BMC Psychiatry 2014;14:368. 10.1186/s12888-014-0368-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Agentur für Arbeit Statistik . Statistiken nach regionen [online]. n.d. Available: https://statistik.arbeitsagentur.de/DE/Navigation/Statistiken/Statistiken-nach-Regionen/Statistiken-nach-Regionen-Nav.html
- 24. Bauer M, Glenn T, Geddes J, et al. Smartphones in mental health: a critical review of background issues, current status and future concerns. Int J Bipolar Disord 2020;8:2. 10.1186/s40345-019-0164-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rhoades H, Wenzel SL, Rice E, et al. No digital divide? technology use among homeless adults. J Soc Distress Homeless 2017;26:73–7. 10.1080/10530789.2017.1305140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Eyrich-Garg KM. Mobile phone technology: a new paradigm for the prevention, treatment, and research of the non-sheltered “street” homeless? J Urban Health 2010;87:365–80. 10.1007/s11524-010-9456-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rice E, Lee A, Taitt S. Cell phone use among homeless youth: potential for new health interventions and research. J Urban Health 2011;88:1175–82. 10.1007/s11524-011-9624-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gutwinski S, Schreiter S, Deutscher K, et al. The prevalence of mental disorders among homeless people in high-income countries: an updated systematic review and meta-regression analysis. PLoS Med 2021;18:e1003750. 10.1371/journal.pmed.1003750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Schueller SM, Glover AC, Rufa AK, et al. A mobile phone-based intervention to improve mental health among homeless young adults: pilot feasibility trial. JMIR Mhealth Uhealth 2019;7:e12347. 10.2196/12347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Javitt DC, Freedman R. Sensory processing dysfunction in the personal experience and neuronal machinery of schizophrenia. Am J Psychiatry 2015;172:17–31. 10.1176/appi.ajp.2014.13121691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Firth J, Cotter J, Torous J, et al. Mobile phone ownership and endorsement of “mhealth” among people with psychosis: a meta-analysis of cross-sectional studies. Schizophr Bull 2016;42:448–55. 10.1093/schbul/sbv132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ben-Zeev D, Davis KE, Kaiser S, et al. Mobile technologies among people with serious mental illness: opportunities for future services. Adm Policy Ment Health 2013;40:340–3. 10.1007/s10488-012-0424-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ruckel L. Boehringer ingelheim and click therapeutics enter into collaboration to develop and commercialize CT-155, a novel prescription digital therapeutic to aid in the treatment of schizophrenia [online]. 2020. Available: https://www.boehringer-ingelheim.us/press-release/boehringer-ingelheim-and-click-therapeutics-enter-collaboration-develop
- 34. Black AC, Serowik KL, Schensul JJ, et al. Build a better mouse: directly-observed issues in computer use for adults with SMI. Psychiatr Q 2013;84:81–92. 10.1007/s11126-012-9229-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. McDonough CC, University of Massachusetts Lowell . The effect of ageism on the digital divide among older adults. GGM 2016;2:1–7. 10.24966/GGM-8662/100008 [DOI] [Google Scholar]
- 36. Martínez-Alcalá CI, Rosales-Lagarde A, Alonso-Lavernia M de los Á, et al. Digital inclusion in older adults: a comparison between face-to-face and blended digital literacy workshops. 2018. Available: https://www.frontiersin.org/article/10.3389/fict.2018.00021
- 37. Harerimana B, Forchuk C, O’Regan T. The use of technology for mental healthcare delivery among older adults with depressive symptoms: A systematic literature review. Int J Ment Health Nurs 2019;28:657–70. 10.1111/inm.12571 [DOI] [PubMed] [Google Scholar]
- 38. McCosker A, Critchley C, Walshe J, et al. Accounting for diversity in older adults’ digital inclusion and literacy: the impact of a national intervention. Ageing and Society 2021:1–21. 10.1017/S0144686X21001550 [DOI] [Google Scholar]
- 39. Naslund JA, Aschbrenner KA, Bartels SJ. How people with serious mental illness use smartphones, mobile apps, and social media. Psychiatr Rehabil J 2016;39:364–7. 10.1037/prj0000207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. DataReportal . Leading countries based on facebook audience size as of january 2021 [online]. 2021. Available: https://www.statista.com/statistics/268136/top-15-countries-based-on-number-of-facebook-users/
- 41. Bauer R, Bauer M, Spiessl H, et al. Cyber-support: an analysis of online self-help forums (online self-help forums in bipolar disorder). Nord J Psychiatry 2013;67:185–90. 10.3109/08039488.2012.700734 [DOI] [PubMed] [Google Scholar]
- 42. Wicks P, Massagli M, Frost J, et al. Sharing health data for better outcomes on patientslikeme. J Med Internet Res 2010;12:e19. 10.2196/jmir.1549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. McAuley A. Digital health interventions: widening access or widening inequalities? Public Health 2014;128:1118–20. 10.1016/j.puhe.2014.10.008 [DOI] [PubMed] [Google Scholar]
- 44. Norman CD, Skinner HA. EHEALS: the ehealth literacy scale. J Med Internet Res 2006;8:e27. 10.2196/jmir.8.4.e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. van der Vaart R, Drossaert C. Development of the digital health literacy instrument: measuring a broad spectrum of health 1.0 and health 2.0 skills. J Med Internet Res 2017;19:e27. 10.2196/jmir.6709 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data are available. No data sharing plan has been included with the trial registry. No additional data available.